Abstract
Purpose
To evaluate the clinical and radiological features and the risk of middle ear disease in the contralateral ears of unilateral cholesteatoma with clinical and radiological assessment.
Methods
Fifty-two patients with unilateral cholesteatoma and 30 control subjects underwent otoscopic and audiologic examination. Temporal bone computed tomography was performed to evaluate the pneumatization of the temporal bones, the status of anterior epitympanic space and eustachian tube. Then, the parameters of the temporal bone pneumatization were calculated.
Results
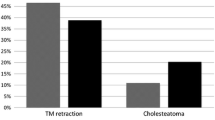
28 % of the contralateral ears in the cholesteatoma patients showed abnormal tympanic membrane findings. In the audiologic examination, 10 % of the contralateral ears showed moderate hearing loss and 3 % showed severe hearing loss. Aeration areas were 1.81 ± 1.01, 2.50 ± 1.31 and 4.49 ± 1.45 cm2, aeration ratios were 24, 28 and 42 %, in cholesteatoma, contralateral and control ears, respectively. Development of the anterior epitympanic space and eustachian tube patency was reduced in contralateral ears relative to control ears.
Conclusions
The degree of temporal bone pneumatization, eustachian tube function, and development of the anterior epitympanic space are significantly decreased in the contralateral ears of unilateral cholesteatoma patients, and there is an increased risk of middle ear diseases. Continuous monitoring of the contralateral ear is crucial for early detection and optimal treatment of middle ear disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of chronic otitis media in South Korea is reported to be 2.19 %. Of those cases, 22.8 % are diagnosed with cholesteatoma [4]. Cholesteatoma is a chronic inflammatory disease caused by intrusion and proliferation of keratinized stratified squamous cells in the middle ear cavity. It may result in a number of serious complications due to erosion of adjacent bony structures [7].
Several theories exist which may explain the pathogenesis of cholesteatoma. One is that cholesteatoma could arise from the accumulation of keratin debris in a retraction pocket. Formation of a retraction pocket could be associated with the pneumatization and gas exchange of temporal bone. Mastoid pneumatization occurs to varying degrees in individuals and it is widely accepted that it is strongly associated with the status of the eustachian tube and the middle ear cavity [15]. This supports that gas exchange in the middle ear cavity and the degree of mastoid pneumatization are related [8, 14]. In addition, our previous study on mastoid pneumatization and anterior epitympanic space suggested that underdevelopment of epitympanic space might be involved in the pathogenesis of chronic otitis media, especially in cholesteatoma [6].
After many studies about the relationship between otitis media and mastoid pneumatization, lots of attention has been paid to the development of otitis media of the contralateral ear in unilateral cholesteatoma patients [2, 3, 5, 11]. Prior studies were conducted with plain X-ray and temporal bone computed tomography (CT) [2, 5, 11]. However, few studies have adopted an easy method for measuring the degree of mastoid pneumatization.
In this study, we aimed to evaluate the risk of middle ear disease in the contralateral ears of unilateral cholesteatoma patients, according to the status of eustachian tube, anterior epitympanic space and the mastoid pneumatization, which was measured in our own technique.
Materials and methods
Subjects
We retrospectively reviewed the medical records of patients with a pathologically confirmed diagnosis of cholesteatoma in Hanyang university Hospital between January 2008 and December 2009. From such patients, we selected 52 who completed course of treatment for unilateral cholesteatoma. As a control group, we selected 30 patients who underwent temporal bone CT scanning for minor temporal bone trauma (Table 1). All candidates for the control group had normal hearing levels and tympanic membrane findings. Patients with histories of chronic otitis media or surgical treatment of otitis media were excluded.
Physical examination and audiologic tests
A thorough examination of the tympanic membrane was performed using an otoscope, otoendoscope and otomicroscope. The tympanic membrane was graded according to the degree of retraction using a modified version of Sade’s staging system [9]. Grade I was defined as mild retraction of the membrane, grade II as retraction in contact with the incus or stapes, and grade III as contact with the promontory or creation of adhesions with the middle ear cavity. Other features of tympanic membranes included evidence of granulation tissues, perforation and other defects (Fig. 1).
For audiology test, pure tone audiometry with modified ascending–descending technique was used. Hearing thresholds were set at 500, 1,000 and 2,000 Hz. The average degree of hearing loss measured using these tests was calculated for cholesteatoma patients and for control subjects, and the figures were compared.
Temporal bone computed tomography
All patients and control subjects underwent temporal bone CT using both axial and coronal sections with a slice thickness of 1 mm (using a Siemens Somatom Plus 16 machine, Erlangen, Germany). The axis of the scanned image was set parallel to the orbitomeatal line. The obtained images were converted to Digital Imaging Communication in Medicine (DICOM) files and transferred to a personal computer.
Based on these images, three assessments were made. First, temporal bone pneumatization was estimated. This measurement was performed in the axial plane, which is the best view of the lateral semicircular canal, and the window was set between −1,024 Hounsfield unit (HU) and −200 HU. Temporal bone CT scan was manipulated with image processing program, Image J 1.38x (National institutes of Health, USA). In the CT scan, soft tissue densities were extracted through modification of the CT image to the binary form in which bony and pneumatized part of the temporal bone were easily distinguished. Size of the total temporal bone area (T mm2) and pneumatized area (A mm2 = T−area of bony structure) were measured. According to these results, the aeration ratio (A/T) was calculated (Fig. 2) Secondly, the anterior epitympanic space was classified into one of three categories, undeveloped, consisting of one air cell or consisting of multiple air cells (Fig. 3). Finally, the status of eustachian tube was evaluated in temporal bone CT. The eustachian tube was considered to be obstructed when an abnormal soft tissue shadow was shown in the protympanum or the lumen of the tube seemed to be collapsed in chasing the eustachian tube from protympanum to its nasopharyngeal opening in the CT scan. When the protympanum appeared normal and the lumen of the eustachian tube was easily visible in serial temporal bone CT scan, the eustachian tube was considered to be patent radiologically (Fig. 4).
Axial CT sections of temporal bone at the level of the lateral semicircular canal. a Measurement of total area of temporal bone, b Image after binary transformation, measurement of aerated area, T mm2 = total area of temporal bone (shed area), A mm2 = T−area of bony structure (blue colored area), aeration ratio = A/T
Statistical analysis
Data were analyzed using SPSS for windows, version 12.0 (SPSS Inc., Chicago, IL, United States). For continuous variables such as aeration area and aeration ratio, data are presented as mean ± standard deviation. Categorical data are expressed as the number of cases in each category. Paired t tests, ANOVA, Chi square tests and linear by linear association were used, where appropriate. A p value less than 0.05 was considered statistically significant.
Results
Tympanic membrane findings and audiology tests
The affected ears of cholesteatoma patients displayed various tympanic membrane abnormalities. Contralateral ears displayed tympanic membrane abnormalities, of which grade I tympanic membrane retraction was the most common (Table 2).
In pure tone audiometry, 56 % of affected ears showed moderate or moderate to severe hearing losses. In contrast, 60 % of contralateral ears had normal hearing levels (Table 3). The air-bone gaps in the affected ears were found to be normal in 9 cases (17 %), 15–24 dB in 12 cases (23 %), 25–34 dB in 15 cases (29 %), 35–44 dB in 9 cases (17 %), above 45 dB in 7 cases (17 %), whereas the contralateral ears had normal air-bone gaps in 33 cases (65 %), 15–24 dB in 14 cases (27 %), 25–34 dB in 4 cases (7 %) and 35–44 dB in 1 case (1 %).
Mastoid pneumatization
The mean pneumatized areas in the affected and the contralateral ears of the cholesteatoma patients were 1.97 and 2.72 mm2, respectively, and the corresponding aeration ratios were 22.6 and 29.4 % (Table 4). In cholesteatoma patients with normal tympanic membranes in the contralateral ears, the mean pneumatized area of the affected and contralateral were 2.16 and 3.06 mm2, respectively, and the corresponding aeration ratios were 24.5 and 32.2 %. In the control group, the mean pneumatized area was 4.45 mm2 and the mean aeration ratio was 42 %. The means of aeration ratio in three groups were significantly different (ANOVA, p < 05).
Development of the anterior epitympanic space
The categories used to assess the development of the anterior epitympanic space were undeveloped (A), consisting of one air cell (B), and consisting of multiple air cells (C). In the affected ears of cholesteatoma patients, the numbers of cases in categories A, B and C were 1 (2 %), 19 (37 %) and 32 (62 %), respectively, while in the contralateral ears the figures were, 7 (13 %), 26 (50 %) and 19 (37 %) (Table 5). In control group, 22 (43 %), 26 (50 %) and 4 (7 %) cases were classified as categories A, B, and C, respectively. All results were statistically significant (Chi square test, p < 0.05).
Eustachian tube patency
In the cholesteatoma patients, 36 (69 %) affected ears and 48 (92 %) contralateral ears were found to have patent eustachian tubes, while 16 (31 %) affected ears and 4 (8 %) contralateral ears were found to have obstructed eustachian tubes (Table 6). In the control group all 30 subjects (100 %) had open eustachian tubes. All results are statistically significant (linear by linear association, p < 0.05). The mean pneumatized areas in all subjects with opened and closed eustachian tubes were 2.96 ± 1.50 and 2.01 ± 1.05 mm2, respectively, and the corresponding aeration ratios were 30 ± 12 and 25 ± 10 %. All results were statistically significant (student t test, p < 0.05).
Discussions
We found that the contralateral ears of cholesteatoma patients were likely to have abnormal tympanic membranes and had a higher degree of hearing loss and larger air-bone gaps than control ears. Contralateral ears were also significantly different from control ears in terms of pneumatization of mastoid antrum (evaluated by calculating pneumatized areas and aeration ratios), development of the anterior epitympanic space, and eustachian tube patency.
The possible development of middle ear problems in the contralateral ear in patients with unilateral cholesteatoma patients is a very interesting theme in otology. It seems to be associated with the pathogenesis of otitis media and cholesteatoma.
Paparella et al. [8] argued that the chronic otitis media grows sequentially, since the initial development of disease, to serous or purulent types, granulation tissue, cholesterol granuloma, cholesteatoma, and bony destruction. A major cause of cholesteatoma is functional disability of the eustachian tube, which maintains the ventilation of the middle ear cavity [1, 10]. The ventilation of the middle ear plays a role in pneumatization of the mastoid antrum and ultimately controls the size of the air cell in the antrum [15]. Development of middle ear disease and mastoid pneumatization are strongly associated.
Many studies have been conducted on the risk of middle ear disease in unilateral cholesteatoma patients. Sato et al. reported a significant decrease in the area of the mastoid process in unilateral cholesteatoma patients based on plain mastoid X-ray images [5]. Tsuji et al. [16] reported that patients with a history of patulous eustachian tubes had smaller mastoid air cells than control subjects, again based on plain mastoid X-ray images. Khalil et al. reported that the contralateral ears of unilateral cholesteatoma patients were normal in only 28 % of cases, and hearing levels were significantly different from those in normal control subjects. They also reported a volume of the mastoid air cell between affected contralateral and control ear, based on temporal bone CT images [3]. Deguine found that the tympanic membrane in the contralateral ears of unilateral cholesteatoma patients was normal in only one-third of cases [2].
In this study, we focused on the development of the anterior epitympanic space and the patency of eustachian tube in unilateral cholesteatoma patients, as well as mastoid pneumatization. And, we suggested a new method and parameters for measuring the mastoid pneumatization. The temporal bone CT scan of the same level with lateral semicircular canal could provide a lot of information such as development of sigmoid sinus, size of mastoid antrum and the status of aditus ad antrum. Thus, the value of pneumatization area might include these parameters associated with mastoid aeration and could be an objective parameter which represented pneumatization of whole mastoid bone. This method might be an easy to follow technique rather than the measurements of pneumatization through the plain mastoid X-ray or temporal bone CT with three-dimensional reconstructions [2, 3, 5].
The increased risk of developing cholesteatoma in the contralateral ears in unilateral cholesteatoma patients is still controversial. Similar with our results, a few studies suggested that the pneumatization failure leads to the development of cholesteatoma in the contralateral ears [2, 13], but further studies are required to establish whether there was a casual relationship between mastoid pneumatization and cholesteatoma in the contralateral ear of unilateral cholesteatoma.
However, we might suggest that the findings for the contralateral ears of cholesteatoma patients were significantly different from those in the normal control group. This was consistent with many previous studies that supported the theory that there was an increased risk of cholesteatoma in the contralateral ear of unilateral cholesteatoma patients [12], and demonstrated the importance of early treatment of any suspicious lesions and continuous follow-up, even though cholesteatoma treatment of affected ear had been finished.
Conclusion
The contralateral ears of unilateral cholesteatoma patients showed various signs of clinical and radiologic abnormalities. The contralateral ears also exhibit a value between those of affected and control ears for aeration area and aeration ratio, calculated by the method we suggested. To sum up, it is evident that the contralateral ears of unilateral cholesteatoma patients have characteristics of both non-pathological and diseased states. This suggests an increased risk of middle ear disease, and emphasizes the importance of continuous follow-up and close observation of contralateral ear of the unilateral cholesteatoma patients.
References
Austin DF (1977) On the function of the mastoid. Otolaryngol Clin North Am 10:541–547
Deguine C (1990) The contralateralear in cholesteatoma. Rev Laryngol Otol Rhinol (Bord) 11(5):463–468
Khalil HM, Saleh MA, Sakr A (2004) A clinico-radiological study of the contralateral ear in acquired unilateral cholesteatoma. Rev Laryngol Otol Rhinol 125(1):17–22
Kim CS, Jung HW, Yoo KY (1993) Prevalence and risk factors of chronic otitis media in Korea: results of nation-wide survey. Acta Otolaryngol (Stockh) 113:369–375
Koç A, Ekinci G, Bilgili AM, Akpinar IN, Yakut H, Han T (2003) Evaluation of the mastoid air cell system by high resolution computed tomography: three-dimensional multiplanar volume rendering technique. J Laryngol Otol 117(8):595–598
Min HJ, Kim SG, Jung JH, Jeong JH, Lee SH, Park CW (2011) Epitympanic development and mastoid pneumatization in chronic otitis media with and without cholesteatoma. Korean J Audol 15:25–31
Olszewska E, Wanger M, Bernal-Sprekelsen M et al (2004) Etiopathogenesis of cholesteatoma. Eur Arch Otorhinolaryngol 261:6–24
Paparella MM, Schachern PA, Yoon TH et al (1990) Otopathologic correlates of the continuum of otitis media. Ann Otol Rhinol Laryngol 99:17–22
Sade J, Avraham S, Brown M (2008) Atelectasis, retraction pocket and cholesteatoma. Acta Otolaryngol 72:1419–1423
Sade J (1992) The correlation of middle ear aeration with mastoid pneumatization. The mastoid as a pressure buffer. Eur Arch Otorhinolaryngol 249:301–304
Saggese D, Pirodda A, Palma S, Nola G, Rinaldi Ceroni A (1997) The contralateral ear in acquired cholesteatoma in children and adults. Acta Otorhinolaryngol Ital 17(6):414–418
Selaimen da Costa S, Rosito LP, Dornelles C, Sperling N (2008) The contralateral ear in chronic otitis media: a series of 500 patient. Arch Otolaryngol Head Neck Surg 134(3):290–293
Sirikci A, Bayazit YA, Bayram M, Kanlikama M (2001) Significance of the auditory tube angle and mastoid size in chronic ear disease. Surg Radiol Anat 23(3):91–95
Takahashi H, Honjo I, Naito Y (1997) Gas exchange function through the mastoid mucosa in ears after surgery. Laryngoscope 107:1117–1121
Tos M, Stangerup SE (1985) The causes of asymmetry of the mastoid air cell system. Acta Otolaryngol 99:564–570
Tsuji T, Yamaguchi N, Aoki K, Mitani Y, Moriyama H (2000) Mastoid pneumatization of the patulous Eustachian tube. Ann Otol Rhinol Laryngol 109(11):1028–1032
Conflict of interest
The authors report no conflicts of interest. They alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, J.H., Lee, S.H., Min, H.J. et al. The clinical and radiological status of contralateral ears in unilateral cholesteatoma patients. Surg Radiol Anat 36, 439–445 (2014). https://doi.org/10.1007/s00276-013-1204-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-013-1204-3