Abstract
Metastatic hydatid disease of the lung may happen when a hydatid cyst (HC) anywhere in the body ruptures into a systemic vein, a right heart chamber or a pulmonary artery (PA), resulting in the embolisation of the cyst’s contents into the lungs. We submit herewith, the images of embolised hydatids within the PA, in a patient who had surgery for HC involving the right ventricular (RV) wall in 2014. Despite adequate surgical and medical management, investigations in 2017 revealed multiple embolised cysts within PA branches. Further continued medical therapy resulted only in partial resolution of the disease, indicating probably the inadequacy of the currently available treatment strategies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The lung is the second most commonly affected organ in the zoonosis caused by the cestode echinococcus. In humans, pulmonary hydatids manifest themselves as cysts, when the oncospheres hatching out of ingested eggs in the bowel find their way into the lungs. Rarely, these eggs may be inhaled. The lungs may also get secondarily infested when a cyst in an adjacent organ erodes into it, or when a pulmonary cyst ruptures into a bronchus [1]. Besides these usual ways of lung involvement, metastatic infestation of the lung may also happen when a hydatid cyst (HC) anywhere in the body ruptures into a systemic vein, right heart chambers or a pulmonary artery (PA), embolising the lungs with its contents—the scolices and the daughter cysts [1]. This embolisation may happen spontaneously, or as a complication of trauma or surgery on a hydatid.
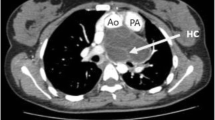
A 22-year-old man was diagnosed in 2014 to have a right ventricular (RV) wall hydatid and an emptied left upper lobe of lung (LUL) hydatid, when he presented with complaints of chest pain, breathlessness, cough, salty expectorations and syncope (Figs. 1 and 2a). He had a history of sternal compressions initiated on him during an episode of syncope, by a bystander. When the cardiac cyst was excised, some punctate openings in the base of the pericyst were also closed meticulously [2]. The RV lumen was not opened. Perioperatively, he was treated with four interrupted cycles of albendazole and praziquantel over 6 months. His follow-up investigations over the next two years were normal. In 2017, he complained of mild breathlessness, and investigations revealed metastatic hydatids within some segmental PA, and a recurrence in the LUL (Figs. 2b and 3). The D-dimer levels were normal. Echocardiogram showed no cardiac lesions or evidence of pulmonary hypertension. Imaging in 2018 showed infarction of a portion of the left lower lobe of lung (LLL), corresponding to the emboli (Figs. 2c and 4). In 2019, the x-ray showed resolution of the LLL lesion only (Fig. 2d). From 2017 till date, he has been on repeated cycles of both drugs. His liver function tests and blood cell counts have always been normal.
Serial chest x-rays: a Preoperatively in 2014, showing an empty cyst in the LUL. b In 2017, showing recurrence in LUL and LLL. c In 2018, showing a persistent LUL cyst (single arrow) and areas of pulmonary infarction in LLL (double arrows). d In 2019, showing persisting LUL lesion and resolution of the LLL lesion
Cardiac hydatidosis is known to cause syncope, besides other symptoms [3]. The trauma caused by the sternal compressions, the surgery or the disease process by itself may have resulted in the embolisation. Another possible cause is the LUL cyst rupturing into an adjacent PA branch. However, pulmonary hydatids are more likely to rupture into a bronchus or the pleural cavity, than into a PA [1]. These emboli may produce the conventional signs and symptoms of pulmonary embolism [4, 5]. Surgery, complemented by chemotherapy, is the recommended treatment for pulmonary hydatids [6,7,8]. Patients unfit for surgery, complex diseases, recurrences and embolisation are best treated medically [4, 9]. Enucleation or embolectomy may be considered to treat the emboli, but could lead to major complications [4, 5]. Opinions differ regarding the appropriate drug regimen and follow-up strategies. There are many reports of partial responses and recurrences with the currently available treatment protocols [6,7,8,9,10,11,12].
We wish to publish these images highlighting this uncommon complication of hydatidosis and stress upon the need for further research into this orphaned disease.
References
Sarkar M, Pathania R, Jhobta A, Thakur BR, Chopra R. Cystic pulmonary hydatidosis. Lung India. 2016;33:179–91.
Shankar R, Thankachen R, Choudhary LK, Rao VM. Right ventricular hydatid cyst excision without the use of cardiopulmonary bypass. Indian J Thorac Cardiovasc Surg. 2016;32:163–4.
Turak O, Özcan F, Sökmen E, et al. Syncope as the primary manifestation of hydatid cyst. Report of two cases with different etiologies. Herz. 2014;39:287–90.
Namn Y, Maldjian PD. Hydatid cyst embolization to the pulmonary artery: CT and MR features. Emerg Radiol. 2013;20:565–8.
Akgun V, Battal B, Karaman B, Ors F, Deniz O, Daku A. Pulmonary artery embolism due to a ruptured hepatic hydatid cyst: clinical and radiologic imaging findings. Emerg Radiol. 2011;18:437–9.
Nabi MS, Waseem T. Pulmonary hydatid disease: what is the optimal surgical strategy? Int J Surg. 2010;8:612–6.
Shehatha J, Alizzi A, Alward M, Konstantinov I. Thoracic hydatid disease; a review of 763 cases. Heart Lung Circ. 2008;17:502–4.
Alvela-Suárez L, Velasco-Tirado V, Belhassen-Garcia M, et al. Safety of the combined use of praziquantel and albendazole in the treatment of human hydatid disease. Am J Trop Med Hyg. 2014;90:819–22.
Vuitton DA. Benzimidazoles for the treatment of cystic and alveolar echinococcosis: what is the consensus? Expert Rev Anti-Infect Ther. 2009;7:145–9.
Rawat S, Kumar R, Raja J, Singh RS, Thingnam SKR. Pulmonary hydatid cyst: review of literature. J Family Med Prim Care. 2019;8:2774–8.
Jamshidi M, Mohraz M, Zangeneh M, Jamshidi A. The effect of combination therapy with albendazole and praziquantel on hydatid cyst treatment. Parasitol Res. 2008;103:195–9.
Horton R. Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Acta Trop. 1997;64:79–93.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design, material preparation discussions and image selection. The drafts and the final manuscript were written by Prof. Birla Roy Gnanamuthu and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
The approval of the institutional review board has been obtained.
Informed consent
Written informed consent for research and publication has been taken from patients before surgery.
Research involving human and animal rights
This article does not contain any studies with animals performed by any of the authors. The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohammad, A., Sameer, M., Vimala, L.R. et al. Pulmonary embolism from cardiac hydatids. Indian J Thorac Cardiovasc Surg 37, 205–208 (2021). https://doi.org/10.1007/s12055-020-01070-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-020-01070-4