Abstract
Cardiac echinococcosis is a rare manifestation of Echinococcus infection, affecting 0.5–2% of the patients. Since it may be a life-threatening condition, surgical treatment should be always considered. Herein, here we present a case of a 66-year-old male with chest pain. Subsequent exams confirmed the diagnosis of multiple cardiac hydatic cysts. The patient initiated treatment with albendazole and was submitted to a surgical resection with cardiopulmonary bypass. A complete surgical resection was achieved, and patient remains asymptomatic without disease signs of recurrence on imaging exams. We highlight the necessity of cardiac screening in echinococcosis cases and the surgical management in this case.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac hydatidosis is a rare manifestation of Echinococcus infection. Although the liver is the most affected organ, 0.5–2% of the patients show cardiac involvement [1, 2]. Symptoms depend on the location of the cysts and their growth rate, and include cardiac symptoms, such as chest pain, dyspnea, syncope, palpitations, and newly detected heart murmurs. Patients can also present fatigue and weight loss. Up to 10% of the patients have symptoms upon the diagnosis, but almost all patients with cardiac involvement will eventually develop symptoms with the progression of the cardiac dissemination [2, 3].
Considering the heart, the left ventricle is the most infected structure (55–60%), followed by the right ventricle (15%), the left atrium (8%), the interventricular septum (5–9%), the pericardium (8%) and the pulmonary arteries (7%) [4].
Troponin levels can be elevated due to the coronary malperfusion and subsequent myocardial ischemia caused by the hydatic cysts [4]. Cardiac imaging (echocardiography, magnetic resonance or computed tomography) is highly sensitive and specific for the diagnosis [5], and can be sufficient to justify a surgical approach.
We present a case of a primary cardiac hydatic cyst with multiple locations involvement, and its cardiothoracic surgical management. Approval by the Institutional Review Board was waived due to the anonymized case report, and informed consent was obtained from the patient.
Case presentation
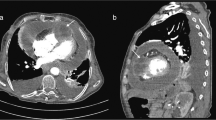
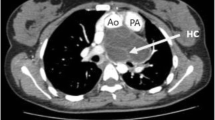
A 66-year-old man presented with occasional episodes of chest pain. Patient had a previous history of coronary artery disease, with an acute myocardial infarction 5 years before. A subsequent coronary angiography at the time demonstrated significant disease of the left circumflex artery, and this lesion was appropriately treated by percutaneous coronary intervention. When the patient currently presented to the consultation, a 12-lead electrocardiograph showed ischemia of the anterior, lateral and inferior walls. The echocardiogram showed normal left ventricular function, without motion abnormalities or valve disease. The patient underwent a nuclear stress test that revealed ischemia and necrosis of the inferior and inferolateral walls. Consequent coronary angiography showed no restenosis of the stent, and non-significant disease of the remaining coronary arteries. To better clarify the symptoms, the patient underwent a thoracic computed tomography (CT), revealing multiple and multifocal pericardial cysts (Fig. 1). Further examinations with thoracic magnetic resonance imaging (MRI) confirmed the multiple and multifocal pericardial cysts, located in the right ventricle and apex (7 × 4 cm), compressing the left ventricle (Fig. 1). A serological test for cystic echinococcosis antibody detection was requested, which was positive (> 1/1280).
Since the patient had no history of echinococcosis and no treatment was previously completed, we have initiated treatment with albendazole 400 mg (mg) twice a day for 21 days before the surgery. Due to the anatomical locations of the cysts and patient’s symptoms, surgical removal with cardiopulmonary bypass (CPB) was planned. After median sternotomy, three clustered cysts were found: (1) on the right ventricle and apex (Figs. 2a, b); (2) on the left atrium and superior vena cava (Fig. 2c); and (3) on the right ventricular outflow tract (Fig. 2d). CPB was established with arterial cannulation on the ascending aorta and venous return provided by bicaval cannulation. The surgery was performed on pump with non-beating heart, with blood cardioplegia. The patient was kept in normothermia. The cysts on the left atrium and right ventricular outflow tract were promptly removed, and the site closed with a continuous suture. The cyst on the right ventricle and apex was firmly adherent and a careful and thorough removal was necessary. The cysts were regularly washed with 3% saline solution and were removed with the germinal membrane. Reconstruction of the right ventricle and apex with a ventriculoplasty was necessary due to the weakening of the myocardial walls and the existence of continuity solutions in the myocardial tissue. We used interrupted U-shaped polypropylene mattress stitches on Teflon pledgets on the border between normal and evolved myocardial tissue, and sutured the Dacron patch to preserve the ventricle morphophysiology (Fig. 3). None of the cysts ruptured during the procedure (Fig. 4).
The patient developed a post-operative low cardiac output syndrome at the Intensive Care Unit (ICU), with the necessity of inotropic and vasopressor support. The patient was discharged from the ICU on the fifth post-operative day, and discharged home on the seventh post-operative day. No significant events were observed during the in-hospital course. Medications at discharged included aspirin (100 mg/daily) and albendazole (400 mg/twice a day).
The pathology report confirmed the cyst as a hydatic cyst (Fig. 5) and the parasitological culture of the removed cysts identified Echinococcus granulosus.
The patient was observed on a post-operative consultation 4 weeks after the surgery, remaining asymptomatic. A cardiac MRI was repeated 9 months later, without any signs of the disease (Fig. 6). The patient was continued on therapeutic with albendazole, remaining asymptomatic one year after the surgery.
Discussion and conclusion
Cardiac echinococcosis is a rare entity that can be associated with significant morbidity. Since it might be a life-threatening situation, screening of cardiac lesions should be part of echinococcosis diagnostic workup. In seronegative patients, the verification of cardiac hydatic cysts using imaging methods is sufficient to justify a surgical treatment [4]. Hydatic cysts should always be surgically removed, even in asymptomatic patients, due to the high risk of a spontaneous rupture [2].
In cases when there is exclusively cardiac involvement, surgery may be curative [3] and the associated mortality arises from the surgical procedure itself (infective endocarditis, ventricular rupture, intramyocardial fistulas, arrhythmias, embolisms or massive cyst rupture with anaphylaxis) [3].
Surgery usually is combined with a short course of pre-procedure treatment to prevent the spread of the cyst and sterilize the cysts, improving surgical manipulation by reducing cyst integrity and turgidity [6]. However, its use may not be recommended because the pericyst membrane may become more friable and may rupture during surgical manipulation [3].
Concluding, cardiac hydatidosis is a rare manifestation of Echinococcus infection, with a high risk of life-threatening complications. Screening for cardiac lesions should be performed in all patients with the diagnosis of hydatic cysts. Long-term treatment with albendazole and an annual follow-up consultation with an imaging exam should be maintained after surgical resection. Patients with exclusive heart dissemination can have good prognosis with a low rate of recurrence after surgical treatment.
References
Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. ClinMicrobiol Rev. 2004;17(1):107–35.
Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114(1):1–16.
Díaz-Menéndez M, Perez-Molina J, Norman F, Pérez-Ayala A, Monge M, Pilar B, Fuertes Z, et al. Management and outcome of cardiac and endovascular cystic echinococcosis. PLoSNegl Trop Dis. 2012;6:1-e1437.
Kahlfuß S, Flieger R, Roepke TK, Yilmaz K. Diagnosis and treatment of cardiac echinococcosis. Heart. 2016;102(17):1348–53.
Joseph AG, Lahiri R, Joseph A, Sengupta G. Giant hydatid cyst of interventricular septum of heart. Indian J ThoracCardiovascSurg. 2020;36(1):81–4.
Smego RA, Sebanego P. Treatment options for hepatic cystic echinococcosis. Int J Infect Dis. 2005;9(2):69–76.
Funding
This research did not receive any specific funding from commercial or public agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The data that support this case report is on the clinical record of the patient, available from the corresponding author, upon reasonable request.
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Velho, T.R., Gonçalves, J.M., Pereira, R.M. et al. Primary cardiac hydatic cyst with multiple locations: an unusual case of chest pain. Gen Thorac Cardiovasc Surg 69, 1147–1150 (2021). https://doi.org/10.1007/s11748-021-01631-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01631-3