Abstract
Hydatid disease is a parasitic infestation that is caused by the larvae of the tapeworm Echinococcus granulosus. Clinical manifestations are extremely variable and related to the location and the size of the cysts. Syncope as the first clinical presentation of hydatid cyst is a very rare condition. Herein, we report two cases of patients with cardiac and pleural hydatid cysts who had syncope as the initial symptom.
Zusammenfassung
Die Echinokokkose stellte einen Parasitenbefall dar, der durch Larven des Bandwurms Echinococcus granulosus verursacht wird. Die klinische Manifestation kann sehr stark variieren und ist abhängig von der Lokalisation und der Zystengröße. Eine Synkope als erstes klinisches Symptom einer Echinokokkuszyste ist äußerst selten. Im vorliegenden Beitrag werden 2 Fälle mit einer kardialen bzw. einer pleuralen Echinokokkuszyste dargestellt, in denen die Vorstellung beim Arzt wegen einer Synkope als Erstsymptom erfolgt war.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hydatid disease (HD) is a zoonosis resulting from parasitic infestation in which the larvae of various nematodes develop into cysts [1]. The disease seems to be under control in many countries; however, because of the importation of animals, traveling, and immigration from endemic regions, a number of sporadic cases can still be encountered even in the countries where control measures are effective [2, 3]. Clinical manifestations are highly variable and symptoms are often related to the location and the size of the cysts [1, 4]. HD generally progresses silently and can have dangerous complications [1, 4]. Syncope as the primary manifestation of HD is a very rare condition. Herein, we describe two patients with cardiac and pleural HD who were admitted to hospital with syncope.
Case 1
A 51-year-old man complaining of recurrent syncope was referred to our institute. Physical examination, blood tests, electrocardiography, head-up tilt table test, and 24-h Holter monitoring did not show any pathological finding. A comprehensive neurological examination was nonspecific. Cranial computed tomography (CT) revealed no abnormality. Transthoracic echocardiography depicted a multilocular cystic lesion in the apex of the left ventricle; cysts were round and had a well-defined, double-layered wall (Fig. 1 a, Video 1). These echocardiographic findings were compatible with active cardiac echinococcosis [1]; however, serologic tests for Echinococcus granulosus were found to be negative, and thoracic and abdominal imaging did not reveal any extracardiac hydatid involvement. Dynamic cardiac CT confirmed the diagnosis of multilocular hydatid cyst in the left ventricular apex, obstructing almost one half of the true ventricular cavity (Fig. 1 b). Oral albendazole therapy was initiated before surgery in an attempt to lessen the risk of secondary dissemination through cyst rupture or spillage of cyst fluid, and to reduce the likelihood of postoperative recurrence. Surgical and parasitological findings confirmed the diagnosis of cardiac echinococcosis. With an uneventful postoperative period, the patient was discharged from hospital without any symptoms. Moreover, the outpatient follow-up over 18 months revealed no new syncopal attack.
a Transthoracic echocardiography showing a huge cystic lesion significantly obliterating the left ventricular cavity. LV left ventricle, LA left atrium, RA right atrium. See also Video 1 online. b Cardiac computed tomography demonstrates the cystic lesion obstructing nearly one half of the left ventricular cavity. LV left ventricle
Case 2
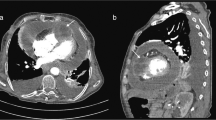
A 46-year-old woman was admitted to our hospital following a syncopal episode. The accompanying persons disclosed that the patient had experienced three syncopal attacks in the previous 1 month. She had history of surgery for hepatic and pulmonary HD. Physical examination, electrocardiography, routine laboratory tests, head-up tilt table test, and 24-h Holter monitoring revealed no abnormality. The patient’s comprehensive neurological examination results and cranial CT scans were normal. Transthoracic echocardiography revealed an echo-free cystic structure behind the right atrium on apical four-chamber view (Fig. 2 a). Thoracic CT depicted a large multiseptated, thick-walled cystic lesion (7 × 7 cm) located in the right cardiophrenic pleural space (Fig. 2 b) compressing the right atrium (Fig. 2 c). Liver involvement was also documented on the abdominal CT slices. Serologic tests for Echinococcus granulosus were found to be negative. An albendazole regimen was initiated and continued for a 7-day period before the planned surgical intervention. Macroscopic and histopathological evaluation of the cystic material confirmed the diagnosis of HD. Furthermore, the patient was free of any new syncopal attack during the 16-month follow-up period.
a Transthoracic echocardiography showing an echo-free cystic structure behind the right atrium. LA left atrium, RA right atrium. b Thoracic CT showing a large multiseptated cystic lesion located in the right cardiophrenic pleural space. RA right atrium. c Thoracic CT showing significantly compressed right atrium by the cystic lesion. RA right atrium
Discussion
Cystic echinococcosis is a human parasitic infestation that is caused by the larvae of the cestode Echinococcus granulosus [1]. Hydatid cysts preferentially involve the liver; however, any organ may be affected via the portal or systemic circulation [5, 6]. Cardiac or pleural involvement is very rare even in endemic countries [1, 4]. Cardiac echinococcosis represents only 0.5–2 % of all HD cases even in the regions where the disease risk is particularly high and the prognosis is grave [1, 7]. The parasites reach the heart by way of the coronary circulation and settle most commonly in the left ventricle, moving subsequently into the interventricular septum, right ventricle, atrium, and the pericardium [7, 6]. Clinical signs of cardiac echinococcosis depend on the location and the size of the cyst [8]. Chest discomfort, palpitations, and dyspnea are the most common presentations, and may be associated with a number of serious life-threatening complications [1, 9]. Pleural involvement usually develops secondary to rupture of the pulmonary or hepatic cysts into the pleural space, thus leading to secondary pleural hydatidosis [10]. Three types of secondary pleural hydatidosis have been defined: pleural hydatid graft, pleural granulomatosis, and hydatidothorax [10, 11]. Our case represents the first type, and this type mostly remains asymptomatic or is associated with atypical symptoms, such as dyspnea and cough [11]; however, cardiac symptoms in this type are extremely uncommon.
Syncope as the first clinical manifestation of HD is a very rare clinical condition. As such, the literature contains only a scarce number of case reports. The majority of these cases presenting with syncope were patients with cardiac echinococcosis in whom the syncopal episodes had been triggered by various mechanisms, such as complete atrioventricular block [12], several rhythm disturbances [8, 13], severe mitral insufficiency [14] and obstruction of the left ventricular outflow tract [15]. Our first patient presented with syncope because of a voluminous cyst significantly obliterating the left ventricular cavity. The second patient, the case with pleural hydatidosis, presented with syncope due to significant right atrial impingement that ultimately led to insufficient right atrial and hence right ventricular fillings. To the best of our knowledge, this localization of a hydatid cyst has not been reported to date as a cause of syncope.
Hydatid cyst should be considered in the differential diagnosis of a mass lesion within or around the cardiac chambers. A voluminous cyst can produce cardiac symptoms and signs by impinging on the structures in the vicinity or by obliterating the cardiac chambers. Early diagnosis is of paramount importance, since the risk of rupture of the cyst is high, and an imminent rupture may result in potentially life-threatening complications [6, 15]. Therefore, bedside echocardiographic examination is a useful imaging method for the rare differential diagnoses of syncope where quick decision is mandatory for a surgical intervention. Surgical resection followed by an appropriate medical therapy is the best treatment with favorable results [6, 15]. In patients with HD, positive hydatid serology test result has a diagnostic value, whereas a negative serology result is deemed insufficient to exclude the diagnosis [16]. The serum samples from our two patients were negative for anti-echinococcus granulosus antibody by ELISA test and echinococcus hemagglutination test. Therefore, this disease should be included in the differential diagnosis of every patient with syncopal attack who has come from relevant endemic areas and in whom imaging modalities have documented cyst-like mass lesions around the cardiac chambers, even in the absence of a positive parasitic serology result.
Conclusion
Although HD seems be under control in Europe, changes in the economic and politic sphere in the last decade have resulted in uneventful progress in public health policies in many countries [2, 3]. Europe is a region with continuous growth in immigration, especially from more endemic areas [2, 3]. Therefore, patients with atypical cardiac symptoms coming from highly endemic areas must also be evaluated for HD.
References
Tufekcioglu O, Birincioglu CL, Arda K et al (2007) Echocardiography findings in 16 cases of cardiac echinococcosis: proposal for a new classification system. J Am Soc Echocardiogr 20:895–904
Rojo-Vazquez FA, Pardo-Lledias J, Francos-Von Hunefeld M et al (2011) Cystic echinococcosis in spain: current situation and relevance for other endemic areas in Europe. PLoS Negl Trop Dis 5:e893
Richter J, Orhun A, Gruner B et al (2009) Autochthonous cystic echinococcosis in patients who grew up in Germany. Euro Surveill 14(22). pii:19229
Gursoy S, Ucvet A, Tozum H et al (2009) Primary intrathoracic extrapulmonary hydatid cysts: analysis of 14 patients with a rare clinical entity. Tex Heart Inst J 36:230–233
Ozer T, Gundogdu S, Ozer Y et al (2004) Echinococcosis involving the liver, retrovesical and seminal vesicle presented with syncope. Int J Urol 11:922–924
Brecker SJ, Mandal K, Harrison T et al (2005) Hydatid disease of the heart. Ann R Coll Surg Engl 87:W1–W4
Kammoun S, Frikha I, Fourati K et al (2000) Hydatid cyst of the heart located in the interventricular septum. Can J Cardiol 16:921–924
Fabijanic D, Bulat C, Letica D et al (2011) Echocardiographic appearance of a hydatid cyst of the papillary muscle and chordae tendineae. J Clin Ultrasound 39:431–433
Iltumur K, Karabulut A, Toprak N (2005) Recurrent multiple cardiac hydatidosis. Eur J Echocardiogr 6:294–296
Aguilar X, Fernandez-Muixi J, Magarolas R et al (1998) An unusual presentation of secondary pleural hydatidosis. Eur Respir J 11:243–245
Ozyurtkan MO, Kocyigit S, Cakmak M et al (2009) Case report: secondary pleural hydatidosis. Turkiye Parazitol Derg 33:177–178
Ben-Ismail M, Fourati M, Bousnina A, Kafsi N (1978) Complete syncopal auriculoventricular block by a hydatid cyst of the intraventricular septum. Ann Med Interne 129:539–542
Niarchos C, Kounis GN, Frangides CR et al (2007) Large hydatic cyst of the left ventricle associated with syncopal attacks. Int J Cardiol 118:e24–e26
Journet M, Gay J, Benoit P et al (1982) Syncope with a rare etiology, cardiac hydatidosis. Ann Med Interne 33:478–482
Rekik S, Krichene S, Sahnoun M et al (2009) Unusual cause of syncope in a 17 year-old young woman: left ventricular hydatid cyst. Int J Cardiol 136:e21–e23
Salehi M, Soleimani A (2009) Cardiac echinococcosis with negative serologies: a report of two cases. Heart Lung Circ 18:59–61
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article includes an additional video. You will find this supplemental at dx.doi.org/10.1007/s00059-013-3827-x.
Electronic supplementary material
Video Transthoracic echocardiography showing a huge cystic lesion that significantly obliterates the left ventricular cavity (avi 8MB)
Rights and permissions
About this article
Cite this article
Turak, O., Özcan, F., Sökmen, E. et al. Syncope as the primary manifestation of hydatid cyst. Herz 39, 287–290 (2014). https://doi.org/10.1007/s00059-013-3827-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-013-3827-x