Abstract
Purpose
Earlier we reported 3-month graft patency and clinical outcomes of prospective randomized comparison of off-pump and on-pump multivessel coronary artery bypass surgery to evaluate outcomes and graft patency (PROMOTE patency) trial. We now report major adverse cardiac and cerebrovascular events (MACCE) at 1 year of patients who underwent coronary artery bypass grafting (CABG) using either off-pump technique or on-pump technique.
Methods
The PROMOTE patency trial is a two-arm, prospective, randomized, multicentre trial, and enrolled 320 patients with multivessel coronary artery disease from March 2016 through March 2017 at 6 centres and were randomly assigned to undergo either off-pump CABG (OPCAB) (n = 158 patients) or on-pump CABG (n = 162 patients). The outcomes at 1 year were assessed.
Results
One mortality (0.64%) occurred in off-pump group (at 30 days) and 4 (2.48%) in on-pump group (1 at 30 days, 2 at 3 months, and 1 at 1 year) (p = 0.37). There was no difference between off-pump and on-pump groups in the outcomes of nonfatal myocardial infarction (1 in off-pump and 2 in on-pump group, p = 1.00) and cerebrovascular accident (none in off-pump and 2 in on-pump group, p = 0.49). Repeat revascularization was done in one patient in each group (p = 1.00).
Conclusion
There was no significant difference in the incidence of MACCE between off-pump and on-pump CABG group at 1 year.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The PROMOTE patency study results at 3 months reported on graft patency and clinical outcomes [1]. The early outcomes of PROMOTE patency trial are in concurrence with the results of Diegeler et al. [2] in GOPCABE trial, Lamy et al. [3] in CORONARY trial, and Taggart et al. [4] in Arterial Revascularization Trial (ART) and ROOBY trial [5] which showed no significant difference in the rate of composite outcome of death at 30 days.
However, 1-year outcomes of off-pump and on-pump CABG are conflicting. ROOBY trial [6] reported higher rates of primary composite outcome at 1 year (death from any cause, repeat revascularization, or nonfatal myocardial infarction) with off-pump when compared with on-pump CABG. But CORONARY trial [7] reported no significant difference between off-pump and on-pump CABG with respect to the primary composite outcome and the rate of repeat revascularization. In institutions with experience in off-pump CABG, the rates of major adverse events and of complete revascularization and graft patency have been similar to those with on-pump CABG [8]. We performed extended study of PROMOTE patency trial to compare the 1-year outcomes with the two strategies of coronary revascularization.
Patients and methods
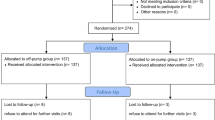
This prospective randomized comparison of off-pump and on-pump multivessel coronary artery bypass surgery to evaluate outcomes and graft patency (PROMOTE patency) was conducted between March 2016 and March 2017. It was a two-arm multicentre study and enrolled a total of 320 patients to either on-pump (n = 162) or off-pump (n = 158) CABG. MACCE were recorded at 1 month (318 patients) and 3 months (316 patients) after surgery. In this study, the 1-year outcomes were analysed (flowchart: Fig. 1).
The PROMOTE patency trial was registered in the Clinical Trials Registry of India (CTRI/2017/10/010030). This trial complies with the principles of the Declaration of Helsinki and was approved by the institutional ethics committees of participating institutions, and all patients signed an informed consent.
Surgical technique
Premedication, anaesthetic protocols, and surgical access to the heart were via a standard median sternotomy in all patients, and conduit harvesting techniques and distal and proximal anastomotic techniques were similar between the groups as previously reported [9]. Off-pump and on-pump techniques and the method of exposure and stabilization of heart to perform distal coronary anastomoses were previously described [9].
Definitions
The occurrence of MACCE was defined as death, myocardial infarction (MI), or stroke at 1 year after CABG. Cerebrovascular (CV) death: all deaths are considered cardiovascular unless a specific non-cardiovascular cause is evident (e.g. malignancy). Stroke: new acute focal neurological deficit (except for subarachnoid haemorrhage which may not be focal) thought to be of vascular origin with signs or symptoms lasting greater than 24 h. MI perioperative (within 24 h of surgery): new pathologic Q waves with documented new wall motion abnormalities other than septal or cardiac markers = 10 × Unique Learner Number (ULN). MI non-perioperative (later than 24 h after surgery): electrocardiogram (ECG) changes consistent with infarction (new significant Q waves in two contiguous leads in the absence of previous left ventricular hypertrophy (LVH) or conduction abnormalities) or evolving ST segment to T wave changes in two contiguous leads or new left bundle branch block or ST segment elevation requiring thrombolysis or percutaneous coronary intervention (PCI) and cardiac markers (troponins or creatinine kinase myocardial band (CK-MB)) in the necrosis range. Carotid artery stenosis: significant carotid artery stenosis is defined as stenosis > 60% of internal carotid artery if it is bilateral and more than 80% if it is unilateral and evaluated by duplex ultrasound [10]. Repeat coronary revascularization: new CABG procedure or PCI associated with documented ischemia by stress testing (ECG, Echo, or nuclear) and graft failure or new culprit lesion = 70% luminal stenosis.
Follow-up
Follow-up was done at 1 year at the hospitals and by telephonic contacts.
Statistical analysis
Primary analysis of the data was performed according to the principle of “intention to treat”. Statistical analysis was performed by the trial coordinating centre using software SAS version 9.2. Continuous variables are expressed as median and mean ± standard deviation. Categorical variables are expressed as raw numbers and percentages. The differences were analysed with a chi-square, Fisher exact test (if cell frequency is less than 5), and two sample t tests. The statistical significance for all the tests was accepted at a probability level < 0.05. The odds ratios (ORs) and risk ratio (RRs) with 95% confidence intervals (CIs) are reported for each group. Cumulative event rates were estimated using Kaplan-Meier analysis.
Study end points and power calculation
The primary objective of this study was to ascertain the non-inferiority of off-pump CABG when compared with on-pump CABG in terms of angiographically assessed graft patency at 3 months. The short-term primary endpoint was graft patency at 3 months. Hence, the required primary sample size of 310 patients (155 patients in each arm) was determined based on graft patency rates in order to detect a difference of 10% in patency rates between off-pump and on-pump CABG, with a power of 90%. The short-term secondary end points were death, nonfatal cerebrovascular stroke/accident (CVS/CVA), MI, and repeat revascularisation at 30 days and 3 months postoperatively. At 3 months, cumulative combined MACCE in off-pump group (0.63%) was significantly lower than on-pump group (5.55%), p = 0.01, with rates of 0.006 in off-pump group and 0.055 in on-pump group [1].
The primary long-term end point was a composite of all-cause mortality, cerebrovascular accident, or a nonfatal myocardial infarction (MACCE) at 1 year. Assuming the rates of cumulative MACCE of 3 months as 0.006 in off-pump group and 0.055 in on-pump with a 5% significance level, the power was detected for the samples (156 in off-pump and161 in on-pump) at 1 year. The study is adequately powered for the sample in both the groups with a power of more than 80% to detect the difference in the incidence of MACCE between the two groups at 1 year.
Testing comparison p = baseline p (versus <)
Calculating power for baseline p = 0.055
Comparison p | Sample size | Power |
|---|---|---|
0.006 | 156 | 0.810777 |
0.006 | 161 | 0.821524 |
Results
A total of 320 patients were enrolled and were randomly assigned to undergo either off-pump CABG (n = 158 patients) or on-pump CABG (n = 162 patients). Of 320 patients, 318 patients (at 1 month) and 316 patients (at 3 months) survived and were analysed for MACCE. Among the survivors, 239 (75.6%) patients (120 in off-pump group and 119 in on-pump group) returned to graft evaluation and underwent graft imaging [multidetector computed tomography (MDCT) in 190 patients and catheter conventional catheter coronary angiography (CAG) in 49 patients] at 3 months.
Baseline demographic and clinical characteristics of both groups did not significantly differ between both treatment groups (Table 1). Using carotid duplex ultrasound, 245 (76.5%) patients underwent carotid artery evaluation. At 2 of the centres, a total of 75 (23.43%) patients did not undergo preoperative carotid artery screening as the centres do not subject the patients for carotid evaluation routinely prior to CABG. Of 245 patients, 123 (50.20%) patients underwent off-pump technique, and 122 (49.79%) underwent on-pump CABG. Carotid artery stenosis was observed in 1 (0.81%) in off-pump group and 1 (0.82%) in on-pump group (Table 1). Of 320 patients, 3 patients lost to follow up at 1 year. Cumulative analysis was performed on 317 patients (156 patients in off-pump CABG and 161 patients in on-pump CABG) to asses MACCE including mortality (5 patients), nonfatal MI (3 patients), and cerebrovascular accident (2 patients) at 1 year. At 1 year, the adverse events occurred in 10 patients [1.28% (2 patients) in off-pump CABG and 4.97% (8 patients) in on-pump CABG), odds ratio 0.24, 95% CI, 0.005–1.18, p = 1.00 (Table 2)]. The rates of individual components of MACCE did not differ significantly between the groups.
One mortality occurred in off-pump group (at 30 days) and 4 in on-pump group (1 at 30 days, 2 at 3 months, and 1 at 1 year). There is no significant difference in mortality at 1 year between off-pump and on-pump groups (off-pump 1; on-pump 4; odds ratio 0.25, CI 0.02–2.29, p = 0.37). There was no significant difference between the groups in the outcome of nonfatal myocardial infarction [0.64% (1patient) in off-pump and 1.24% (2 patients) in on-pump group, odds ratio 0.512, CI 0.04–5.71, p = 1.00] and cerebrovascular accident [0.00% in off-pump and 1.24% (2 patients) in on-pump group (p = 0.49) (Table 2)]. Repeat revascularization was done in one patient in each group (p = 1.00). The survival curves show no significant difference between the off-pump and on-pump groups (Fig. 2).
Discussion
PROMOTE patency trial is a unique randomized controlled trial that studied the graft patency at 3 months as the primary end point of off-pump and on-pump coronary artery bypass graft surgery [1]. One-year outcomes of this study showed no significant difference in the outcomes between the off-pump and on-pump CABG surgery. The study enrolled low-risk population with EuroSCORE II less than 1, and the mean age of the patient was 58 years with preserved left ventricular function. We are in concurrence with the clinical outcomes of numerous prospective randomized trials [11,12,13] comparing on-pump vs off-pump CABG which showed no differences between the groups in low-risk populations.
This study showed no significant difference in mortality between off-pump (0.64) and on-pump groups (3.48) (p = 0.37) and aligned with the results of Angelini et al. [11] and Nathoe et al. [12]. Angelini et al. conducted beating heart against cardioplegic arrest studies (BHACAS 1 and 2) and two single-centre prospective trials, with 400 patients randomized to on-pump or off-pump CABG. No significant difference in mortality was observed (0% for off-pump and 1% for on-pump). At 2 years of follow-up for BHACAS 1 and over 1 year for BHACAS 2, mortality was 2% and 3%, respectively [11]. Nathoe et al. also showed no significant difference in mortality (1.4% on-pump and 1.4% in off-pump surgery, p = 0.98) [12].
The Octopus Study [13] is a multicentre randomized controlled trial conducted in the Netherlands, which enrolled 281 low-risk CABG patients between 1998 and 2000. No statistically significant differences were observed between the on-pump and off-pump groups in quality of life, stroke rate, or all-cause mortality at 3 and 12 months. In the Octopus Study, they found a trend toward better cognitive outcome 3 months after off-pump surgery, but this difference disappeared at 12 months. Nathoe et al. [12] reported no difference in the stroke rates between off-pump (0.7%) and on-pump CABG (1.4%), p = 0.55. In concurrence with these studies, the present study also observed no significant difference in stroke rate between off-pump (0.00%) and on-pump (1.24%) CABG, p = 0.49.
Okano et al. [14] analysed the National Health Insurance Research Database, using data for patients between 18 and 45 years of age who had undergone isolated coronary artery bypass between 2001 and 2011. A total of 344 patients received off-pump surgery, and 741 patients received on-pump surgery. One-year MACCE outcomes in terms of death, myocardial infarction, and stroke were not different between the groups. There is no significant difference in mortality between off-pump (2.03%) and on-pump (1.62%). Nathoe et al. [12], in a multicentre randomized study, concluded that in low-risk patients, there was no difference in cardiac outcome at 1 year between on-pump bypass and off-pump surgery. At 1 year, the rate of freedom from death, stroke, myocardial infarction, and coronary re-intervention was 90.6% after on-pump surgery and 88.0% after off-pump surgery. In the present, the freedom from death, stroke, and MI was 98.72% in off-pump surgery and 95.03% in on-pump surgery. The low MACCE rates in our study could be inclusion of very low-risk patients as evidenced by low EuroSCORES.
ROOBY trial [6] showed long-term (1 year) composite of death, repeat revascularization, and nonfatal myocardial infraction and was higher (9.9% vs. 7.4%, P = 0.04) for the off-pump group with no significant differences between the individual composite components. The coronary artery bypass grafting off- or on-Pump revascularization study [7] at 1 year reported no difference in primary composite outcome of death, myocardial infarction, stroke, or new renal failure requiring dialysis. The primary outcome event had occurred in 288 participants (12.1%) in the off-pump group and 316 participants (13.3%) in the on-pump group [hazard ratio (HR) with the off-pump procedure, 0.91; 95% CI 0.77–1.07; p = 0.24] [4]. Even though composite outcomes of present study were in concurrence with the results of ROOBY and CORONARY trials in terms of difference between the groups, they reported higher MACCE rates compared with our study (4.97% in the on-pump group and 1.28% in the off-pump group).
In this trial, the need for repeat revascularization up to 1 year is low as the index of completeness of revascularization is 1. This study showed no significant difference in MACCE between off-pump and on-pump technique at 1 year. The cohort of the patients will be followed up yearly for MAACE, and angiographic graft evaluation at 5 years is contemplated.
Limitations
The sample size was primarily calculated for the graft patency at 3 months, and data were collected prospectively. This extended study is observational in nature, and hence, a risk of bias but the power is adequate to find the differences in MACCE at 1 year. One-year follow-up was done at the hospitals and by telephonic contacts. The telephonic follow-up and low-risk population may result in lower rates of MACCE. Therefore, the results cannot be extrapolated to high-risk population.
Conclusions
There was no significant difference in the incidence of MACCE (death, nonfatal MI, stroke, repeat revascularization) at 1 year between the off-pump and on-pump groups.
References
Sajja LR, Sarkar K, Mannam G, et al. Graft patency at 3 months after off- and on-pump coronary bypass surgery: a randomized trial. Indian J Thorac Cardiovasc Surg. 2020;36:93–104.
Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med. 2013;368:1189–98.
Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary artery bypass grafting at 30 days. N Engl J Med. 2012;366:1489–97.
Taggart DP, Altman DG, Gray AM, et al. Effects of on-pump and off-pump surgery in the arterial revascularization trial. Eur J Cardiothorac Surg. 2015;47:1059–65.
Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary artery bypass surgery. N Engl J Med. 2009;361:1827–37.
Hattler B, Messenger JC, Shroyer AL, et al. Off-pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: results from the veterans affairs randomized on/off bypass (ROOBY) trial. Circulation. 2012;125:2827–35.
Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med. 2013;368:1179–88.
Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs. conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA. 2004;291:1841–9.
Sajja LR, Mannam G, Sompali S, et al. Does multi- vessel off-pump coronary artery bypass grafting reduce post-operative morbidity compared to on-pump CABG? Ind J Thorac Cardiovasc Surg. 2004;20:173–7.
Biller J, Feinberg W, Castaldo JE, et al. Guidelines for carotid endarterectomy. A statement for healthcare professionals from a special writing group of the stroke council, American Heart Association. Stroke. 1998;29:554–62.
Angelini GD, Taylor FC, Reeves BC, Ascione R. Early and midterm outcome after off-pump and on-pump surgery in beating heart against cardioplegic arrest studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet. 2002;359:1194–9.
Nathoe HM, van Dijk D, Jansen EW, et al. A comparison of on-pump and off-pump coronary bypass surgery in low-risk patients. N Engl J Med. 2003;348:394–402.
van Dijk D, Nierich AP, Jansen EW, et al. Early outcome after off-pump versus on-pump coronary bypass surgery: results from a randomized study. Circulation. 2001;104:1761–6.
Okano R, Liou YJ, Yu HY, et al. Coronary artery bypass in young patients—on or off-pump? J Clin Med. 2019;8:128. https://doi.org/10.3390/jcm8020128.
Acknowledgements
We thank Mr. A. Nadamuni Naidu, M. Sc (Stat), Head, Department of Statistics (Retired), National Institute of Nutrition, ICMR, Hyderabad, India and Trustee, Sajja Heart Foundation, Hyderabad, India for statistical advice and analysis for this study, and we thank all the coordinators of the study from various institutions in coordinating the study: Mr. Mamidala Parusharamulu of Star Hospitals, Hyderabad; Mr. Arnab Naik of Medica Superspeciality, Kolkata; MS. Shashirekha of Krishna Institute of Medical Sciences, Hyderabad; MS. Mahalakshmi Shanmugam of G Kuppuswamy Naidu Memorial Hospital, Coimbatore; Dr. Reenali Bariya of DDMM Heart Institute, Gujarat; and Dr. Neeraj of Fortis Hospital, Mumbai.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This trial complies with the principles of The Declaration of Helsinki and was approved by the institutional ethics committees of participating institutions.
Informed consent
All patients signed an informed consent.
Research involving human participants and/or animals
This study complies with the principles of The Declaration of Helsinki and was approved by the institutional ethics committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sajja, L.R., Sarkar, K., Mannam, G. et al. One-year outcomes of off- and on-pump coronary artery bypass grafting: PROMOTE patency trial. Indian J Thorac Cardiovasc Surg 36, 469–475 (2020). https://doi.org/10.1007/s12055-020-00940-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-020-00940-1