Abstract
Objective
The Japanese Off-Pump Coronary Revascularization Investigation (JOCRI) study reported a non-significant difference in early outcomes and graft patency between off-pump coronary artery bypass grafting and on-pump coronary artery bypass grafting in 2005. The JOCRIED study aimed to review the long-term outcomes of the JOCRI study participants.
Method and results
The JOCRIED study enrolled 123 of the JOCRI study participants completing the clinical follow-up between August 2018 and August 2020; 61 patients in the off-pump group and 62 patients in the on-pump group. The follow-up period was 13.8 ± 2.8 years. The groups were compared regarding mortality, the incidence of major adverse cardiac and cerebrovascular events and repeat revascularisation. The 15-year cumulative survival rate (off-pump vs on-pump, respectively; 77.7% vs 75.3%; p = 0.85), major adverse events-free survival rate (62.5% vs 55.6%; p = 0.27) and repeat revascularisation-free rate (84.8% vs 78.0%; p = 0.16) were not significantly different between the two groups. Revascularisation was the most common major adverse events in the JOCRIED participants. Although percutaneous coronary intervention was performed in 8 patients (13%) in the off-pump group and in 14 patients (23%) in the on-pump group (p = 0.23), no patients underwent redo coronary artery bypass grafting.
Conclusions
Off-pump coronary artery bypass grafting provides comparable 15-year outcomes to on-pump coronary artery bypass grafting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Off-pump coronary artery bypass (OPCAB) was developed to address the hypothesis that avoiding cardiopulmonary bypass in OPCAB contributes to decreased perioperative mortality and morbidity, including stroke, compared with on-pump coronary artery bypass (ONCAB). However, several studies failed to show that OPCAB had benefits regarding early outcomes compared with ONCAB [1]. In addition, the long-term outcomes of OPCAB versus ONCAB are still under debate, as reported in two large randomised controlled trials. The coronary artery bypass grafting (CABG) Off or On Pump Revascularization study (CORONARY) showed comparable 5-year results between the two techniques [2], whereas the Randomised On/Off Bypass (ROOBY) trial reported increased 5-year mortality with OPCAB [3]. Therefore, the benefits of avoiding cardiopulmonary bypass may be overwhelmed by the increased technical complexity of OPCAB regarding early and long-term outcomes. In contrast, the Japanese Off-Pump Coronary Revascularization Investigation (JOCRI) study, which was a two-armed randomised multicentre trial, reported a non-significant difference in early outcomes and graft patency between OPCAB and ONCAB [4]. Surgery by expert surgeons and using multiple arterial conduits in the JOCRI study might have contributed to overcoming technical complexity in OPCAB. However, the long-term outcomes of the JOCRI study are unclear. The current study, the JOCRIED study, aimed to review the long-term outcomes of the JOCRI study participants and to verify the rationale for OPCAB using multiple arterial conduits.
Methods
Study cohort and data collection
The JOCRI study was a two-armed randomised multicentre trial conducted at five institutions (National Cerebral and Cardiovascular Center, Fukuoka University, Kanazawa University, Kyoto Prefectural Med University and Nippon Med School) in Japan between 2002 and 2004, with patients randomised equally to an OPCAB or ONCAB group [4]. The protocol and results of the JOCRI study have been published. Briefly, the inclusion criteria in the JOCRI study were isolated, double- or triple-vessel disease and first-time CABG. All CABG procedures were performed by a single experienced surgeon who had performed more than 200 OPCABs before the JOCRI study, in each hospital. The study’s exclusion criteria were age > 70 years, severe ascending aortic calcification on computed tomography, carotid arterial stenosis > 75%, acute Q-wave myocardial infarction necessitating emergency operation, left ventricular ejection fraction < 30%, serum creatinine level > 2.0 mg/dL, liver cirrhosis, chronic obstructive pulmonary disease requiring a bronchodilator or steroid, pulmonary hypertension with a mean pulmonary artery pressure > 25 mmHg or another comorbidity that is not appropriate for cardiopulmonary bypass (CPB), such as anomalous coagulation, cancer or an inability to provide written informed consent. All cases underwent surgery via a median sternotomy. OPCAB was performed using a stabiliser device under systemic heparinisation. ONCAB was performed under full cardiopulmonary bypass with mild hypothermia and under direct cross clamping of the ascending aorta and induced cardiac arrest. Postoperatively, aspirin 100 mg daily was prescribed for life unless the drug was not indicated. Baseline characteristics, surgical data and the early clinical outcomes of the enrolled 167 patients in the JOCRI study were stored as a preserved data sheet in an outside data centre.
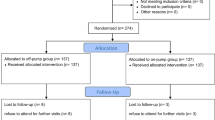
The JOCRIED study enrolled 123 of the JOCRI study participants completing the clinical follow-up between August 2018 and August 2020. Data were collected from the medical records at the five participating institutions and from referral letters, which were further supplemented by telephone interviews with patients under the care of distant physicians. There were 61 patients in the OPCAB group and 62 patients in the ONCAB group. The follow-up period was 13.8 ± 2.8 years. The remaining 44 patients in the JOCRI trial were those who were not contactable between August 2018 and August 2020 by telephone or at the contact address or those who were not recorded as deceased by August 2020. Backgrounds, characteristics, operative procedure, early outcomes and the study institutes of these 44 patients were not significantly different from those of the JOCRIED study participants. Preoperatively, all patients or their legal representatives provided written informed consent for surgery and the use of their data for diagnostic and research purposes. This study was approved by National Cerebral and Cardiovascular Center review board (Approval Number: M30-024).
Study outcomes
The two groups were compared regarding mortality and the incidence of major adverse cardiac and cerebrovascular events (MACCE), namely all-cause mortality, myocardial infarction (MI), cerebrovascular accidents and repeat revascularisation. Cerebrovascular accident was defined as a new neurological deficiency evidenced by clinical signs lasting more than 24 h or evidence on computed tomography or magnetic resonance imaging of a recent brain infarct. Repeat revascularisation was defined as coronary bypass surgery or percutaneous coronary intervention (PCI) performed after the JOCRI trial.
Indications for coronary intervention post-OPCAB or -ONCAB bypass grafting
The indications and procedures for coronary intervention post-OPCAB or -ONCAB were determined by heart team discussions at each institute. Coronary intervention was indicated in cases having (1) acute coronary syndrome with significant stenosis or occlusion of the culprit arteries and/or the bypassed conduits, or (2) angina symptoms and/or evidence of myocardial ischaemia with significant stenosis or occlusion of the major branches of the native coronary artery or the grafted conduits. Myocardial ischaemia was diagnosed by stress myocardial scintigraphy and/or by fractional flow reserve under coronary angiography. CABG was selected in cases with multiple complex lesions; otherwise, PCI was selected for coronary intervention post-OPCAB or -ONCAB. The procedural details of the PCI were determined by the interventional cardiology team at each institute.
Statistical analyses
Continuous variables were summarised as medians and interquartile ranges. Between-group differences were assessed using the Wilcoxon rank sum test. Categorical and ordinal variables were summarised as numbers and percentages (%), and between-group differences were assessed using the chi-square test. The cumulative probability of freedom from death was computed using the Kaplan–Meier method. A Cox proportional hazards model was used to assess the hazard of freedom from mortality, MACCE and repeat revascularisation in patients undergoing OPCAB versus ONCAB grafting. In the Cox proportional analysis, missing data were imputed with the multiple imputation method using the “aregImpute” function in the rms package in R (The R Foundation for Statistical Computing, Vienna, Austria). All statistical analyses were performed with a two-sided significance level of 5% using R 3.6.0.
Results
Patients’ characteristics and operative data
The patients’ backgrounds and characteristics were not significantly different between the OPCAB and the ONCAB groups (Table 1). The majority of cases had triple-vessel disease, and half of the cases had diabetes mellitus in both groups. Operation time was significantly shorter in the OPCAB group than that in the ONCAB group (Table 2), and no cases required intraoperative conversion from OPCAB to ONCAB or from ONCAB to OPCAB. Bypass grafting was performed in all major branches with proximal significant stenosis to achieve complete revascularisation in all cases. Direct anastomosis of the conduit to the ascending aorta was avoided in 52 (85%) cases in the OPCAB group and in 51 (84%) cases in the ONCAB group.
There was no significant difference in the conduit selection or the graft design between the two groups. Complete myocardial revascularisation was achieved in 56 patients (95%) in the OPCAB group and in 54 (96%) patients in the ONCAB group. The left internal thoracic artery (LITA) was used in all cases apart from one case whose LITA was dissected, while bilateral ITAs were used in 83 cases (72%). The radial artery was used in 89 cases (72%), the right gastroepiploic artery was used in 25 cases (20.3%) and a saphenous vein graft was used in 17 cases (13.8%).
Long-term outcomes
Death (all-cause mortality) occurred in 13 cases (21%) in the OPCAB group and in 14 cases (23%) in the ONCAB group (Table 3). Of these cases, there were four cardiac mortalities, which resulted from congestive heart failure in two cases in the OPCAB group and in one case in the ONCAB group, and acute MI-related multiorgan failure in one case in the ONCAB group. The 5-year cumulative survival rate was 98.4% in the OPCAB group and 93.5% in the ONCAB group, while the 15-year cumulative survival rate was 77.7% in the OPCAB group and 75.3% in the ONCAB group (Fig. 1a). In addition, the 5-year MACCE-free survival rate was 96.7% in the OPCAB group and 83.9% in the ONCAB group, while the 15-year MACCE-free survival rate was 62.5% in the OPCAB group and 55.6% in the ONCAB group (Fig. 1b). The long-term outcomes for mortality (hazard ratio, 0.793; 95% confidence interval (CI), 0.394–1.595; p = 0.516), MACCE risk (hazard ratio, 0.751; 95% CI 0.457–1.235; p = 0.259) and revascularisation rate (hazard ratio, 0.723; 95% CI 0.436–1.200; p = 0.21) were not significantly different between the two groups (Table 4).
Coronary intervention post-CABG
Revascularisation was the most common MACCE in the JOCRIED participants. The evaluation of graft patency by coronary angiography or coronary computed tomography was performed in 28 (48%) of the OPCAB patients and in 28 (49%) of the ONCAB patients. Complete graft patency was confirmed in 18 (64%) of the OPCAB patients and in 19 (68%) of the ONCAB patients. While PCI was performed in 8 cases (13%) in the OPCAB group and in 14 cases (23%) in the ONCAB group (p = 0.23), no cases underwent redo CABG. PCI was performed for acute coronary syndrome in four cases (7%) in the OPCAB group and in seven cases (11%) in the ONCAB group (p = 0.53). The remaining four cases in the OPCAB group and seven cases in the ONCAB group underwent PCI for angina symptoms and/or evidence of myocardial ischaemia. The 15-year revascularisation-free rate was 84.8% in the OPCAB group and 78.0% in the ONCAB group (Fig. 1c).
Eight cases in the OPCAB group underwent PCI for 10 regions, namely two regions in the left circumflex territory, five regions in the right coronary artery territory and three unrecorded regions. Fourteen cases in the ONCAB group underwent PCI for 16 regions, namely 1 region in the left main, 1 region in the left anterior descending territory, 6 regions in the left circumflex territory, 5 regions in the right coronary artery territory and 3 unrecorded regions. Revascularisation was successfully achieved in all cases, with improvement in symptoms and/or myocardial ischaemia. No cases experienced major adverse events or underwent repeat PCI after the primary PCI post-OPCAB or -ONCAB.
Discussion
The JOCRIED study revealed the very long-term outcomes of OPCAB versus ONCAB; participant enrolment in the JOCRI study was complete in 2004. There was no significant difference in long-term outcomes between the OPCAB group and the ONCAB group in the JOCRIED study. This core outcome was consistent with previous reports that included a larger number of participants with a shorter follow-up than that in the JOCRIED study. In contrast, several reports showed that OPCAB lead to inferior long-term outcomes compared with ONCAB [5, 6]. Success following OPCAB in the JOCRI study and the JOCRIED study may be attributed to surgery performed by expert surgeons and using multiple arterial conduits.
Technical complexity in OPCAB is represented by anastomotic site deployment, conduit length adjustment and by anastomosis itself [7]. However, these aspects can be appropriately addressed by expert surgeons [8]. Several previous studies reported that a less-experienced surgeon, incomplete revascularisation and conversion to ONCAB were associated with higher mortality than mortality after procedures without these factors [3, 6]. In addition, using arterial conduits makes conduit length adjustment easy compared with using venous grafts, and arterial conduits are less likely to kink than venous grafts. Moreover, instability in the anastomosis may result in fewer technical errors with arterial conduits than those with venous grafts early and long term.
In addition to the core outcomes, the JOCRIED study provides several important implications in the contemporary performance of CABG. First, survival rates and MACCE-free survival rates post-CABG using multiple arterial conduits were revealed in this study. The 15-year survival and the 15-year MACCE-free survival were > 75% and > 60%, respectively, in the JOCRIED study, which were comparable or even better to those in other studies reporting > 15 year outcomes post-CABG [9,10,11,12]. Second, no cases with multiple regional ischaemia required redo CABG in the JOCRIED study. Additionally, only two cases required PCI for the left main or left anterior descending territory in this study. More importantly, only one case died because of acute MI. Again, using multiple arterial conduits possibly contributed to avoiding severe or lethal ischaemic regions [11, 12].
The limitation of this study is the small size of the study cohort, which resulted from incomplete follow-up of the JOCRI participants. The original JOCRI trial was the oldest randomised clinical trial of OPCAB versus ONCABG, and the study was completed in September 2004. However, the backgrounds, characteristics and surgical procedures of the cases who were not enrolled in the JOCRIED study were not significantly different from those of the JOCRIED study participants. Moreover, because we performed an analysis that complemented the missing values, the effect of incomplete follow-up was minimal. Additionally, the study limitations of the JOCRIED study are similar to those of the JOCRI study, in which cases ≥ 70 years of age and cases with left ventricular ejection fraction < 30% were excluded.
The clinical goals of OPCAB are (1) quick recovery from surgery for low-risk CABG candidates, (2) avoiding postoperative complications for high-risk CABG candidates and (3) minimising medical costs. Previously published randomised clinical studies of OPCAB versus ONCAB, including the JOCRI and JOCRIED studies, enrolled low-risk CABG candidates. As a result, early- and long-term outcomes were comparable between OPCAB and ONCAB. Thus, high-risk CABG candidates would benefit more from OPCAB, which has been shown to reduce postoperative complications in high-risk cases, such as those with chronic kidney disease or cerebral infarction [7, 13, 14].
In conclusion, OPCAB provided comparable 15-year outcomes to those with ONCAB in low-risk patients. Surgery by expert surgeons and using multiple arterial conduits are keys to success in OPCAB. OPCAB is warranted for high-risk CABG candidates.
References
Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med. 2013;368:1179–88.
Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2016;375:2359–68.
Shroyer AL, Hattler B, Wagner TH, Collins JF, Baltz JH, Quin JA, et al. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med. 2017;377:623–32.
Kobayashi J, Tashiro T, Ochi M, Yaku H, Watanabe G, Satoh T, et al. Early outcome of a randomized comparison of off-pump and on-pump multiple arterial coronary revascularization. Circulation. 2005;112:I338–43.
Takagi H, Umemoto T. Worse long-term survival after off-pump than on-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2014;148:1820–9.
Chikwe J, Lee T, Itagaki S, Adams DH, Egorova NN. Long-term outcomes after off-pump versus on-pump coronary artery bypass grafting by experienced surgeons. J Am Coll Cardiol. 2018;72:1478–86.
Benedetto U, Caputo M, Patel NN, Fiorentino F, Bryan A, Angelini GD. Long-term survival after off-pump versus on-pump coronary artery bypass graft surgery. Does completeness of revascularization play a role? Int J Cardiol. 2017;246:32–6.
Benedetto U, Lau C, Caputo M, Kim L, Feldman DN, Ohmes LB, et al. Comparison of outcomes for off-pump versus on-pump coronary artery bypass grafting in low-volume and high-volume centers and by low-volume and high-volume surgeons. Am J Cardiol. 2018;121:552–7.
Benedetto U, Caputo M, Mariscalco G, Gaudino M, Chivasso P, Bryan A, et al. Impact of multiple arterial grafts in off-pump and on-pump coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2017;153:300-9.e306.
Kirmani BH, Guo H, Ahmadyur O, Bittar MN. Long-term survival following on-pump and off-pump coronary artery bypass graft surgery: a propensity score-matched analysis. Eur J Cardiothorac Surg. 2019;56:1147–53.
Gaudino M, Benedetto U, Fremes S, Biondi-Zoccai G, Sedrakyan A, Puskas JD, et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378:2069–77.
Ruttmann E, Dietl M, Feuchtner GM, Metzler B, Bonaros N, Taggart DP, et al. Long-term clinical outcome and graft patency of radial artery and saphenous vein grafts in multiple arterial revascularization. J Thorac Cardiovasc Surg. 2019;158:442–50.
Kowalewski M, Pawliszak W, Malvindi PG, Bokszanski MP, Perlinski D, Raffa GM, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: meta-analysis. J Thorac Cardiovasc Surg. 2016;151:60-77 e61-58.
Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, et al. Coronary artery bypass grafting with and without manipulation of the ascending aorta: a network meta-analysis. J Am Coll Cardiol. 2017;69:924–36.
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Disclosures
This work was not supported by a specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the content of the article by designing this work; participating in data collection, analysis and interpretation; drafting and revising the manuscript and approving the final version of the manuscript. All authors agree to submission of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
IRB information
This study was approved by the National Cerebral and Cardiovascular Center review board (Approval Number: M30-024).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tadokoro, N., Fukushima, S., Minami, K. et al. 15-year outcomes of the JOCRI study (JOCRIED study): a randomised comparison of off-pump and on-pump multiple arterial coronary revascularisation. Gen Thorac Cardiovasc Surg 71, 151–157 (2023). https://doi.org/10.1007/s11748-022-01854-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01854-y