Abstract
Obesity is considered a serious global health issue. Patients have been predisposed to comorbidities such as dyslipidemia, cardiovascular diseases, diabetes, cancers, and osteoarthritis. Certain fats in the diet have been linked with an increase in obesity, such as saturated and trans-fats. Meanwhile, some dietary fats such as conjugated linoleic acids (CLAs) and medium-chain triglycerides (MCTs) could potentially reduce energy intake. Various mechanisms for reducing weight by CLAs and MCTs, such as increased lipolysis, improved intestinal microbiota, up-regulating peroxisome proliferator-activated receptors (PPARs), increased the expression of uncoupling protein of respiratory chain-1 (UCP-1), and affected satiety hormones are included. These bioactive compounds, CLAs and MCTs, should be used in moderate concentrations to prevent harmful effects such as insulin resistance for CLAs and hypercholesterolemia for MCTs. However, several studies have proposed CLAs or MCTs as adjuvants to the protocol used to minimize bodyweight. Our objective is to summarize the different causes of obesity and to discuss the effects of CLAs or MCTs on body weight and fat deposition in obese animals or humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Obesity is a state of increase in the mass of adipose tissue with concomitant elevation of body weight greater than the levels of physical requirements. Accumulation of triacylglycerols is believed to be the only manner in which body weight has become excessive. However, obesity cannot be simply defined in terms of body weight solely. In that concept, short individuals are supposed to be lighter than tall ones. There is also a need to standardize body weight against height, which is the body mass index (BMI) (equals a person’s weight in kilograms (kg) divided by their height in meters squared (m2)). The World Health Organization (WHO 1985) defined obesity as BMI > 30 for men and BMI > 28.6 for women.
Obesity is seen as a significant global health concern. More than 2 billion people who are equivalent to 30 percent of the global population are obese or overweight (BMI is greater than or equal to 25 kg/m2) (Ng et al. 2014). It is a major health concern because it predisposes subjects to a variety of comorbidities. Accumulation of excess body fat produces an elevated risk for cardiovascular diseases, multiple forms of cancer, increased mortality, type 2 diabetes, stroke, and osteoarthritis (Björntorp 1993; Guh et al. 2009). Recently, there has been tremendous evidence that obesity has a detrimental impact on the brain. Visceral obesity, in particular, is associated with severe metabolic changes in the central nervous system even in younger populations (Kaur et al. 2015). Obesity has also been involved in cognitive deficits in dementia patients (Whitmer et al. 2007).
Obesity etiology is multi-factorial, both genes and environmental factors may be involved. In particular, increased caloric intake and decreased physical activity are the main causes of weight gain (Pereira et al. 2005; Castro et al. 2020). However, there are also secondary reasons for obesity including endocrine disorders and medications (Karam and McFarLane 2007). Also, a deficiency of vitamin D can be a risk factor for obesity (Kaddam et al. 2017).
Currently, the available therapies for obesity have not been able to reduce its prevalence. Diet therapy with increased physical activity does not achieve significant short-term weight reduction (Frood et al. 2013). Besides, current anorexic drugs and surgical procedures have several harmful side effects that may exceed their benefits (Yanovski and Yanovski 2014). The use of adjuvants in current treatments is therefore a novel, safe, and effective strategy.
These ingredients can help to increase the effectiveness of hypocaloric diets by reducing the side effects associated with low energy intake and avoiding the feeling of hunger (Chambers et al. 2014). Many obese individuals tend to eat more foods containing certain functional elements that help to reduce their weight. From these elements, conjugated linoleic acids (CLAs) are known to be antiobesogenic agents in both animals and humans. A variety of studies researched the treatment of CLAs on obesity (den Hartigh et al. 2017; van Baak and Mariman 2019; Namazi et al. 2019).
Medium-chain triglycerides (MCTs) are triglycerides with saturated fatty acids that have a chain length of 6–12 carbons. Beyond their recognized nutritional values, they substantially minimize bodyweight relative to long-chain triglycerides in mice (Zhang et al. 2015; Sung et al. 2018). Clinical research also demonstrated that for obese women, MCTs succeeded in lowering body fat and weight (Krotkiewski 2001). CLAs and MCTs also increased satiety and decreased energy consumption, suggesting a possible role in helping to maintain energy balance (Coleman et al. 2016; Maher et al. 2020).
However, the study of CLAs and MCTs data, concerning their antiobesity effects, is still inconclusive. Hence, the purpose of this article is to summarize the various kinds of literature discussing the effects of CLAs or MCTs on body weight and fat deposition in obese animals or humans. Also, the authors have tried to explore and compare the potential pathways involved in reducing adiposity by both fats. Moreover, the safety of these fat supplements was considered.
2 Adipose tissue and obesity
Fats are stored in adipose tissue, which is classified into anabolic white adipose tissue (WAT) and catabolic brown adipose tissue (BAT). Their roles are different; WAT stores energy as triacylglycerols (TAGs), while the BAT oxidizes lipids to produce energy (Lee et al. 2014). The balance between WAT and BAT is necessary to maintain homeostasis energy. Notably, WAT is considered an endocrine organ that secretes many adipokines with autocrine, endocrine, and paracrine functions. It has a functional diversity that can affect most of the body’s systems. WAT is also primarily produced by adipocytes but there are different types of cells in this tissue, such as stem cells, lymphocytes, macrophages, preadipocytes, and endothelial cells. Therefore, it has the heterogeneity of cells (Ràfols 2014). WAT secretes various lipid substances mainly fatty acids (released under energy deprivation conditions such as in fasting), prostanoids, cholesterol, and vitamin A (Trayhurn 2005). Besides, sex hormones and glucocorticoids are developed by WAT, as it secretes a large number of protein-grade adipokines that have been classified as adipokines such as leptin, resistin, adiponectin, inflammatory, and anti-inflammatory cytokines (Wozniak et al. 2009). However, WAT is distributed across human bodies; Fat deposits are present in the abdomen around the omentum, bowel, and peripheral areas. Subcutaneous fats are also considered to be from the main fat deposits. The locations of WAT determine its metabolic and endocrine properties (Tchkonia et al. 2002). WAT is sensitive to glucocorticoids in the neck and the upper back, meanwhile; it is extremely affected by estrogen in the breasts. Intra-abdominal fat secretes adipokines, which are closely linked to inflammation and type 2 diabetes. Under conditions of excess energy or sedentary life, these deposits are increasing and the production of proinflammatory adipokines has increased with the consequent promotion of atherosclerosis (Yudkin et al. 2005). Obesity is therefore defined as excess body fat associated with a risk of type 2 diabetes and cardiovascular disease depending on the location of excess fat.
3 Causes of obesity
The main causes of weight gain are strongly linked to high-calorie intake and a sedentary lifestyle. Obesity can also be secondary to adverse changes in the neuroendocrine system or genes. Such changes can affect the energy imbalance, appetite, fat distribution, and metabolism of lipids and glucose (Karam and McFarlane 2007). Various secondary factors were included.
3.1 Endocrine disorders
Obesity is associated with many endocrine disorders such as hypothyroidism (Santini et al. 2014), leptin resistance (Sáinz et al. 2015), polycystic ovarian syndrome (Lo et al. 2006), Cushing’s syndrome (Wajchenberg et al. 1995), hypothalamic disorders (Srinivasan et al. 2004), growth hormone deficiency (Rosen et al. 1993), and hypogonadism (Bhasin et al. 2003).
3.2 Vitamin D deficiency
Vitamin D deficiency is documented in obese patients (Kaddam et al. 2017). Vitamin D can contribute to overweight or even obesity through its effects on glucose and fat homeostasis by acting on the pancreas (Delvin et al. 2010). Cell culture and animal studies have shown that adipose tissue has a vitamin D receptor (VDR) and also can synthesize vitamin D in its bioactive metabolite (1,25 dihydroxy vitamin D3).
Vitamin D may increase adipose tissue lipogenesis and adipogenesis (Earthman et al. 2012) which leads to obesity. Cases of vitamin D deficiency have reported higher levels of parathyroid hormone (PTH) (Stein et al. 2009). Hyperparathyroidism has a potential role in obesity by promoting lipogenesis thus encourages weight gain (Snijder et al. 2005). Wakayo et al. (2016) have shown that for a unit elevation in the vitamin D serum level of school children, overweight or obesity risk is reduced by 5.8%. Also, weight loss and decrease in blood androgen levels and blood pressure were fulfilled in obese women who had a significant decrease of vitamin D with polycystic ovarian syndrome after three months of vitamin D supplementation (Pal et al. 2012). It was found that circulatory vitamin D repletion in extremely obese subjects was achieved by the use of prescribed forms of ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3) but the latter is preferable (Stein et al. 2009).
3.3 Genetics
Obesity is a form of polygenic disease. It is the product of the cumulative action of genetic, epigenetic, and environmental influences (Herrera et al. 2011). Several genes have been actively involved in signaling between the hypothalamic satiety and hunger centers and the peripheral leptin, convertase 1, and melanocortin 4 receptors. Mutation of these genes leads to extreme early obesity (Clément et al. 1998).
In particular, insulin and leptin stimulate certain neurons in the hypothalamus to produce alpha-melanocyte-stimulating hormone (alpha-MSH), a neurotransmitter that acts on hypothalamus melanocortin receptors (MCR) to reduce food intake. Mutations of genes responsible for alpha-MSH or MCR contribute to obesity (Girardet and Butler 2014). Moreover, another mutation of genes encoding leptin, leptin receptor, or proopiomelanocortin is associated with weight gain. Human obesity may result from polygenic mutations (Comuzzie and Allison 1998).
3.4 Medications
Side effects of many drugs may develop obesity among susceptible subjects. Antidiabetic medications such as insulin, thiazolidinediones, and sulfonylurea have been shown to increase body weight gain in diabetic patients (Cheng and Kashyap 2011). Also, several therapies that function centrally as antidepressants (Patten et al. 2011), antiepileptics, and antipsychotics may increase body weight gain by operating on brain monoamines (Newcomer and Lieberman 2007).
Besides, the withdrawal of nicotine during smoking cessation was associated with weight gain (Bush et al. 2016). Possible mechanisms include declining metabolic resting rate, decreased physical activity, reduced-calorie burn, and increased appetite.
3.5 Environmental chemicals
Substances such as endocrine-disrupting chemicals (EDCs) may be related to the obesity epidemic (Baillie-Hamilton 2002). Exposure to EDCs takes place at home, in the workplace, on the farm, in the air we breathe, the food we consume, and the water we drink. Early-life exposure to atmospheric particles increases susceptibility to dietary weight gain, insulin resistance, adiposity, and inflammation (Wei et al. 2016). Obesogens are a group of EDCs that may interact with the endocrine system and may contribute to obesity (Janesick and Blumberg 2016).
Bisphenol A (BPA), is used in plastic containers for food and beverage. The composition of BPA is identical to estradiol. Consequently, it binds to estrogen receptors in the body (Do et al. 2017). Phthalates can promote obesity through anti-androgenic effects, anti-thyroid activity, and/or activation of peroxisome proliferator-activated receptors (PPARs) (Kim and Park 2014). Atrazine is an herbicide that is widely used. It has been shown to destroy mitochondria in rats, decrease the metabolic rate, and increase abdominal obesity (Lim et al. 2009). Organotin polluting tributyltin (TBT) contributes to obesity in humans by increasing the number of fat cells (Grün 2014).
3.6 Disruption of energy homeostasis
Continuous disturbance of energy homeostasis contributes to adiposity. The central nervous system (CNS) regulates the feeding activity and thus influences the energy balance. Disturbances in the feeding activity lead to a high incidence of obesity. Energy expenditure includes the basic metabolic rate (BMR), thermogenesis, and physical activity.
BMR is equivalent to about 60–70 percent of the total energy expenditure and it increases with an increase in body weight. However, BMR is centrally regulated (Galgani and Ravussin 2011) that, when dysregulated results in weight gain. It is worth mentioning that physical activity is responsible for 20–30% of overall energy expenditure, except for athletes. A sedentary lifestyle is responsible for major obesity (Bhurosy and Jeewon 2014).
3.7 Saturated and trans-fats
Fats and oils in the diet are the main sources of energy as compared to the other macronutrients. High intake of such fats increases the proportion of calories that would be closely associated with overweight or, in some instances, with obesity (Raatz et al. 2017). It is well documented that a high intake of saturated fatty acids (SFA) is associated with obesity, especially in obesity-prone carriers of the obesity gene (Phillips et al. 2012). Hu et al. (2018) exposed mice to 29 types of diets varying in the proportions of fat, carbohydrates, and protein. They found that increased energy intake and adiposity were caused only by elevated dietary fat content. Astrup (2005) findings are consistent with those of Hu et al. (2018) since they suggested a low-fat diet to avoid weight gain, obesity, type 2 diabetes, and cardiovascular disease. It was found that the degree of saturation of fatty acids affects their β oxidation (Kien et al. 2005). Therefore, SFA increases the deposition of fats in adipose tissue (Piers et al. 2003). In addition to classic monoamine systems and leptin in controlling energy balance, there are two opposing systems, one orexigenic and one anorexigenic, which are part of the energy balance regulation. Neuropeptide Y (NPY) and agouti-related protein (AgRP) are orexigenic, increase food consumption, and enhance obesity. Diets with high saturated fats content significantly increased NPY protein expression with concomitant body weight, elevation (Piggott et al. 2002).
Trans-fats (TFs) are prepared by the hardening of both vegetable and marine oils by industry. Also, trans-fatty acids are naturally constituted a small content in ruminants, meat, and milk. Koh-Banerjee et al. (2003) documented that a high intake of TFs elevated the risk of weight gain and abdominal fat. This could be explained by the role of TFs as ligands for the peroxisome proliferator-activated receptors gamma (PPARγ) system (Mozaffarian et al. 2006) and by induction of insulin resistance (Kavanagh et al. 2007).
4 Dietary supplements and obesity
Lifestyle modifications by changes in diet and physical activity are expected to be the cornerstone of the management of obesity (Strasser and Fuchs 2016). However, people are failing to reach their weight-reduction goals. Therefore, the provision of dietary supplements could be helpful for weight reduction. Many animal studies have shown that high consumption of oleuropein (Lepore et al. 2015) or oleoresin (Lombardo et al. 2018) (olive oil products) is significantly correlated with weight reduction. Merola et al. (2017) also proved that citrolive, a commercial extract from the combination of citrus fruit and olive leaf extracts, could ameliorate the metabolic disorders associated with obesity in rats. In humans, consumption of extra virgin olive oil showed a decline in body weight in obese women (Galvão et al. 2018). Moreover, weight reduction by enhancing lipid metabolism through activation of AMP-activated protein kinase (AMPK) by tea polyphenols has been reported (Rothenberg et al. 2018). Since AMPK can modulate energy homeostasis and lipid metabolism. The results of Yang et al. (2018) are consistent with those of Rothenberg et al. and added that consumption of 600–900 mg tea catechins substantially reduces weight gain. Furthermore, apple polyphenols have anti-obesity effects through a variety of pathways, including free radical scavenging, regulation of gene expression, and altering signal transduction in fat tissues (Asgary et al. 2018). A combination of hibiscus and lemon verbena polyphenolic extracts was consumed by overweight subjects. It exerted an anthropometric measurement improvement, increased anorexigenic hormone (glucagon-like peptide-1), and reduced orexigenic hormone (Ghrelin) through AMPK (Boix-Castejón et al. 2018).
Recently the health benefits of fats may vary according to their fatty acid compositions (Schwab et al. 2014). Fatty acids that consumed in relatively large amounts are linoleic, oleic, and palmitic, meanwhile, others such as α-linolenic acid (ALA), median chain triacyleglycerols, and omega 3 fatty acids are consumed in smaller quantities, but they have clear health benefits (Oliveira-de-Lira et al. 2018) and may be used as dietary supplements (Ludwig et al. 2013).
4.1 Conjugated linoleic acid supplement
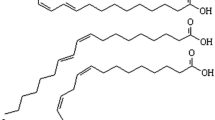
Conjugated linoleic acids (CLAs, 18:2n-6) are natural fatty acids found in meat and dairy products. CLAs are isomers of linoleic acid (LA) but with a double-bond conjugated system. Ruminants have an enzyme that converts omega 6 fatty acids in green plants to CLAs that are stored in animals’ meat and milk. They are also present to a lesser degree, in turkeys, chickens, and pigs.
Synthesized CLAs can be also produced by the action of fermentative bacteria in LA (Kishino et al. 2002). CLAs have a variety of beneficial effects on cancer, atherosclerosis, and obesity (Koba and Yanagita 2014; den Hartigh 2019; Basak and Duttaroy 2020; O’Reilly et al. 2020). The most beneficial effect associated with the intake of trans-10, cis-12 CLAs (t10-c12- CLAs) isomer is the reduction of obesity in both animals and humans (den Hartigh et al. 2018; Mądry et al. 2016 respectively). CLAs consumption by obese patients with non-alcoholic fatty liver disease often significantly improves their lipid profile, glycemic response, and markedly ameliorates oxidative stress (Ebrahimi-Mameghani et al. 2016). On the other hand, for overweight type 2 diabetics, the administration of CLAs for eight weeks does not affect anthropometric measurements and body composition (Shadman et al. 2013; Namazi et al. 2019). In the meantime, CLAs supplementation for obese postmenopausal women with type 2 diabetes significantly improves both body weight and glycemic parameters (Norris et al. 2009; den Hartigh 2019). López-Plaza et al. (2013) reported that skimmed milk fortified with 3g of 1:1 mixture of CLAs isomers (c9-t11 and t10-c12) to overweight healthy subjects for 24 weeks significantly decreased both body weight and total fat mass. Also, Kamphuis et al. (2003) documented that a mixture of CLAs isomers increased the feeling of fullness and increased satiety after thirteen weeks of supplementation. A reduced weight gain was achieved after six months of intake of mixed isomer CLAs (Watras et al. 2007). Both t10-c12 CLAs supplementation and diet restriction in mice exerted equal weight reduction with more fat loss by CLAs followed by increased fat oxidation and energy consumption (den Hartigh et al. 2017).
4.1.1 Mechanisms of CLAs
Many studies demonstrated that CLAs exert their effects by influencing lipid metabolism, modifying enzyme activity, and hormonal profile (Kennedy et al. 2010; Lehnen et al. 2015). CLAs isomers significantly increase lipolysis in human adipocytes and diminish fatty acids synthesis (Martins et al. 2015). They also inhibit the expression of genes that are involved in the differentiation of the pre-adipocytes to mature adipocytes thus reducing lipogenesis (Reardon et al. 2012). The peroxisome proliferator-activated receptors (PPARs) are transcription factors in the nucleus that play an important role in the catabolism and the storage of fatty acids. PPARα and β isomers are involved in the expression of proteins responsible for fatty acid oxidation and, PPARγ isomer is associated with adipocytes differentiation (Tavares et al. 2007). CLAs inhibits PPARγ leading to the reduction of body fat by altering the gene expression that inhibits cell differentiation and modulates the activity of proteins involved in lipogenesis and lipolysis (Boschini and Garcia Júnior 2005) (figure 1).
PPARγ in the adipocytes regulates the expression of genes of acyl-CoA synthetase, lipoprotein- lipase (LPL), and fatty acid transport protein that is involved in the uptake of fatty acids into the adipocytes (Tavares et al. 2007). As a result, the activation of PPARγ increases acyl-CoA synthetase which activates fatty acids, forming an activated complex with carnitine palmitoyl-transferase-1 (CPT-1). This complex enters the mitochondria where it is oxidized to produce adenosine triphosphate (ATP) (Yamashita et al. 2008).
CLAs increase the activity of CPT-1consequently and collectively reduce the accumulation of fatty acids in the adipose tissue. Increased β oxidation of mitochondrial fatty acids induced by CLAs also significantly decreases triacylglycerols synthesis with concomitant reduction of adipocyte size (Botelho et al. 2005). The reduction of body fat occurred due to a decrease in adipocyte size, not the number.
It is noticed that CLAs significantly elevated the expression of the uncoupling protein of the respiratory chain-1 (UCP-1) that leads to weight loss (Busiello et al. 2015). Where, β oxidation of fatty acids results in energy, part of this energy is used for the production of ATP, the rest of the energy is released as heat. UCP-1 also is known as thermogenin, it accelerates the loss of energy as heat. Thus, CLAs increases energy metabolism and expenditure via increasing basal metabolic rate (BMR) or thermogenesis. Consistent with this theory, Shen et al. (2013) proved that the CLAs increase the browning of white adipose tissue with a concomitant increase in energy expenditure. The increased brown fat is significantly associated with lower obesity risk in both mice (Almind et al. 2007) and humans (Cypess et al. 2009). It has been documented that t10-c12 CLA noticeably elevates cyclooxygenase (Cox-2) expression and production of prostaglandin (PG) in the human adipocytes associated with the induction of browning of WAT (Madsen et al. 2010).
Coelho et al. (2019) demonstrated that dietary fat can regulate obesity through its effects on gut microbiota. Diets supplemented with 0.5 percent t10c12 CLA for eight weeks resulted in enhanced cecum fermentation with the concomitant rise in short-chain fatty acids (SCFAs). The intake of CLAs regulates dysbiosis-induced obesity by gut microbiota modulation (Marques et al. 2015). SCFAs induce satiety through the elevation of circulating anorexogenous hormones (Nilsson et al. 2013) and the reduction of ghrelin in the blood (Parnell and Reimer 2009).
4.1.2 Adverse effects of CLAs
It is noteworthy that some animal and human studies have shown that CLAs administration can increase inflammation and insulin resistance (Risérus et al. 2004; Hamilton et al. 2015; Shen and McIntosh 2016), where cultured adipocytes treated with t10 C12CLA display inflammatory reactions (den Hartigh et al. 2013). Besides, CLAs consumption has been related to reduced insulin signaling in mice (Poirier et al. 2006) which is indicative of insulin resistance. Den Hartigh et al. (2017) confirmed that CLAs supplementation significantly enhances weight loss associated with insulin resistance. These drawbacks in the consumption of CLAs are significantly related to the dose. High levels of t10-c12CLA might increase inflammatory markers (LaRosa et al. 2006). In addition to inflammation, such high doses of CLAs cause an increase in hepatic steatosis that is characterized by an overt appearance of fats in the liver, increased liver weight and triacylglycerol content which may be attributed to insulin resistance (Shen et al. 2013). Therefore, controlling the supplemented level or dose of CLAs is a must.
4.2 Medium-chain triglycerides supplement
Medium-chain triglycerides (MCTs) are esters formed of glycerol and three fatty acids with a chain length of 6–12 carbon atoms. Dietary medium-chain fatty acids (MCFAs) include caproic acid or hexanoic acid (C6:0), caprylic acid, or octanoic acid (C8:0), capric acid, or decanoic acid (C10:0), and lauric acid (C12:0). Natural sources of MCFAs in the form of MCTs are coconut and palm kernel oils. MCTs differ from long-chain triglycerides (LCTs) by their smaller molecular size. Besides, MCTs are hydrolyzed faster and more extensively during digestion. MCFAs also undergo limited re-esterification as they have a low affinity for anabolic enzymes such as diglyceride acyltransferase. Furthermore, after digestion, both MCFAs and MCTs are directly reached into the liver via the portal system for rapid oxidation (Babayan 1987). MCFAs and MCTs efficiently enter the mitochondria without carnitine esterification (Hoppel, 1982) through the CPT-1 transport system. Unlike long-chain fatty acids (LCFAs) which are packed into chylomicrons for their tissue distribution through the lymphatic system, allowing maximum uptake by adipose tissue for storage as fat. Collectively, MCTs are extremely less likely to be stored, don’t produce ectopic fat metabolites which promote insulin resistance and also inflammation (McCarty and DiNicolantonio 2016). MCTs were documented to reduce the accumulation of body fat in both clinical trials and animal studies (Liu et al. 2009; Liu et al. 2012). Also, St-onge and Jones (2002) have shown that MCTs have important potential in the prevention of obesity.
It is well documented that the consumption of MCTs in ad libitum meals can substantially induce satiety and reduce body weight (Rial et al. 2016; Gunasekaran et al. 2017). It was also found that when MCTs were added to human breakfast, the consumption at the next meal was reduced (Van Wymelbeke et al. 1998). In this context, MCTs supplementation reduces energy intake over the following two days compared to long-chain triglycerides. Decreased energy intake may be mediated by increasing β-hydroxybutyrate concentration and/or delaying gastric emptying (Maher et al. 2020). Furthermore, there was reduced intake at the dinner after lunch with MCTs as compared to LCTs or other fat replacements (Van Wymelbeke et al. 2001). Interestingly, MCTs consumption resulted in a decrease in food intake either in overweight males (St-Ong et al. 2014) or in healthy, non-obese adult males (Van Wymelbeke et al. 1998).On the other hand, it has been stated that there is no impact on food intake by MCTs supplement (Poppitt et al. 2010). This controversy may be explained by the small dose of MCTs (10 g) in this study. In the meantime, the effective doses in other studies were 20g or more of MCTs. Obese women eating coconut oil had a marked reduction in waist circumference as compared to those who consumed soya bean oil (Assunção et al. 2009). McCarty and DiNicolantonio (2016) recommended that lauric acid should be administered instead of LCFAs to manage obesity, as it is less obesogenic and does not intensify obesity. In mice, coconut oil reduced body weight gain and decreased fat deposition after six weeks of treatments (Gunasekaran et al. 2017).
4.2.1 Mechanisms of MCTs
Zhang et al. (2015) fed a high-fat diet with 2% MCTs or LCTs to obese mice for twelve weeks. Their results showed that diet-containing MCTs produced a significant reduction in fat mass. Such a decrease may be partially attributed to the activation of BAT, probably by the norepinephrine (NE) pathway. Since MCTs are significantly irritating to the sympathetic nervous system, an increase in expression of mRNA, and the protein of the beta-3adrenergic receptors (β3-AR) was observed. NE can trigger many biochemical lipolysis reactions such as the up-regulation of adipose lipase and hormone-sensitive lipase (Liu et al. 2012). NE may also induce thermogenesis (Zhao et al. 1994). It was proved that an increase in β3-AR expression could cause elevated UCP-1 expression in BAT and thermogenesis (Lowell and Flier 1997).
Very low-calorie diets (VLCD) enriched with MCTs or LCTs have been administered to obese women for 4 weeks. Both body fat and body weight showed a significant reduction in the MCTs’ diet. Moreover, the feeling of hunger was lower and directly proportional to the levels of the plasma ketone bodies. Also, MCTs diet-induced lower nitrogen excretion in the urine (Krotkiewski 2001) indicating a protein-sparing effect of MCTs with a concomitant transition to anabolic protein metabolism. Recently, some studies indicate that the net protein catabolism is decreased by 32% in the ketone state such as in cases of fasting and VLCD conditions (Ryde et al. 1993). In this case, ketones that are the result of fatty acid oxidation are utilized by the brain and skeletal muscles as an energy source (figure 2). Therefore, they ameliorate the hunger feeling, spare protein conversion to glucose, and increase the synthesis of proteins (Hoffer et al., 1982). MCTs produce ketones even in the presence of a large concentration of glycogen (Foster and McGarry 1982) because they have rapid access to the inner mitochondrial matrix in the hepatocytes. The main ketone formed by MCTs is the β-hydroxybutyrate. It decreases appetite and exerts an anorexic effect (Laeger et al. 2010).
Many obese patients have a variety of metabolic abnormalities with multifactorial causes. Among these factors, the disturbance of gut microbiota is identified as a causative factor for such complications in obese subjects. MCTs supplementation does not only improve this dysbiosis but also improves intestinal permeability, which helps to manage obesity (Rial et al. 2016). Correction of gut microbiota significantly enhances obese well-being and thus increases SCFAs, consequently participates in weight reduction (Parnell and Reimer 2009; Nilsson et al. 2013). Moreover, the influence of MCTs on reduction in satiety and food intake is done by a significant increase of MCFAs in plasma after MCTs consumption such as capric, caprylic, and lauric. These fatty acids affect the acylation mechanism of ghrelin, which modulates the feeling of satiety and appetite (Lemarié et al. 2016). Each of the capric acid and lauric acid promotes fatty acid oxidation with a concomitant increase of satiety (Lemarié et al. 2015). Cholecystokinin (CCK) is the first gut hormone that is found to affect satiety. Ingestion of lipid is linked to the secretion of CCK which depends on the length of the fatty acid chain. It is reported that CCK is considered a mediator of fat-related satiety via delaying gastric emptying (Matzinger et al. 1999). It was noticed that CCK was released after the ingestion of either capric or lauric acids (Mclaughlin et al. 1999). Furthermore, Feltrin et al. (2004) found that C12 and C10 fatty acids increased CCK release, but the magnitude of this elevation was higher with C12.
Dietary administration of MCTs may likely influence mRNA expression of genes capable of altering the lipogenic capacity of animals (Ferreira et al. 2014). MCTs work through PPAR-γ to down-regulate adipogenic genes. Moderate doses of MCTs are required to improve their anti-lipogenic effect otherwise high doses can have lipogenic effects (Marten et al. 2006).
Peptide YY (PYY) is an amino acid peptide that belongs to pancreatic peptides. Its secretion is stimulated by the sense of protein and fats. It has an anorexic effect by inhibiting food intake via increasing the C-fos expression in the arcuate nucleus (ARC). ARC reduces food consumption (Riediger et al. 2004). MCTs containing 56% octanoic and 43% decanoic acid markedly increased PYY secretion (Maas et al. 1998). This finding was supported by Feltrin et al. (2007) since they found that decanoic acid could stimulate the PYY release in a dose-dependent manner. Moreover, in overweight men, MCTs administration significantly elevated the concentrations of leptin and PYY but did not affect ghrelin or GLP-1as compared to LCTs (St-onge et al. 2014).
4.2.2 Adverse effects of MCTs
The MCTs administration as oil may produce a large elevation of plasma ketones which returns to the normal levels within three hours. This can be avoided by the ingestion of intact sources of these MCTs such as coconut oil which causes a less prominent and a delayed rise of ketones (Newport 2013). Also, although MCTs have an important effect on weight loss, they can increase fasting triglycerides and cholesterol levels (Gunasekaran et al. 2017). By contrast, Sung et al. (2018) demonstrated that MCTs have a potential role in lowering the blood lipids in diabetic rats. Also, this hypercholesterolemia can be considered to be benign (McCarty and DiNicolantonio 2016) and can be avoided by administering moderate amounts of such oils (Marten et al.2006). However, it has been shown that MCTs did not have toxicological effects, even with chronic dietary supplementation (Nagao and Yanagita 2010).
5 Conclusion
Obesity is a condition of excessive body weight with an exaggeration of adipose tissue. It plays an important role in several pathophysiological disorders such as atherosclerosis, hypertension, insulin resistance, and diabetes. The etiology of obesity is multifactorial. The primary causes of obesity are higher caloric intake, especially with saturated and/or trans-fats, and a sedentary lifestyle. Meanwhile, secondary factors include several endocrine disorders, vitamin D deficiency, gene mutation, some medications, environmental obesogens, and disruption of energy homeostasis. Many strategies are designed to minimize weight gain; however, each has some adverse effects. Therefore, a trial used a hypocaloric diet with some dietary supplements has shown marked success. Certain dietary fats, besides their role as a source of energy, can be used as nutraceuticals or dietary supplements to enhance weight reduction. In this context, CLAs and MCTs exhibit a promising issue. Several mechanisms are involved to explain their effects such as increasing satiety, energy expenditure, correcting intestinal microbiota, modifying gene expression, reducing food intake, and increasing mitochondrial oxidation. However, their amounts or doses should be carefully adjusted to avoid unpleasant side effects. Further experimental studies and clinical trials are warranted to confirm the use of such fats as complementary medicine with selected a strategy for weight reduction.
References
Almind K, Manieri M, Sivitz WI, Cinti S and Kahn CR 2007 Ectopic brown adipose tissue in .muscle provides a mechanism for differences in risk of metabolic syndrome in mice. Proc. Natl. Acad. Sci. USA 104 2366–2371
Asgary S, Rastqar A and Keshvari M 2018 Weight loss associated with consumption of apples: a review. J. Am. Coll. Nutr. 37 627–639
Assunção ML, Ferreira HS, dos Santos AF, Cabral CR Jr and Florêncio TM 2009 Effects of dietary coconut oil on the biochemical and anthropometric profiles of women presenting abdominal obesity. Lipids 44 593–601
Astrup A 2005 The role of dietary fat in obesity. Semin. Vasc. Med. 5 40–47
Babayan VK 1987 Medium chain triglycerides and structured lipids. Lipids 22 417–720.
Baillie-Hamilton PF 2002 Chemical toxins: a hypothesis to explain the global obesity epidemic. J. Altern. Complement. Med. 8 185–192
Basak S and Duttaroy AK 2020 Conjugated linoleic acid and its beneficial effects in obesity, cardiovascular disease, and cancer. Nutrients 12 1913
Bhasin S, Woodhouse L and Storer TW 2003. Androgen effects on body composition. Growth Hormone IGF Res. 13 S63–S71
Bhurosy T and Jeewon R 2014 Overweight and obesity epidemic in developing countries: a problem with diet, physical activity, or socioeconomic status? Sci. World J. 2014 964236
Björntorp P 1993 Visceral obesity: a “civilization syndrome”. Obes. Rev. 1 206–222
Boix-Castejón M, Herranz-López M, Pérez Gago A, Olivares-Vicente M, Caturla N, Roche E and Micol V 2018 Hibiscus and lemon verbena polyphenols modulate appetite-related biomarkers in overweight subjects: a randomized controlled trial. Food Funct. 9 3173–3184
Boschini RP and Garcia Júnior JR 2005 UCP2 and UCP3 genic expression: regulation by food restriction, fasting and physical exercise. Braz. J. Nutr. 18 753–764
Botelho AP, Santos-Zago LF, Reis SMPM and Oliveira AC 2005 Conjugated linoleic acid suplementation decreased the body fat in Wistar rats. Braz. J. Nutr. 18 561–565
Bush T, Lovejoy JC, Deprey M and Carpenter KM 2016 The effect of tobacco cessation on weight gain, obesity and diabetes risk. Obesity 24 1834–1841
Busiello RA, Savarese S and Lombardi A 2015 Mitochondrial uncoupling proteins and energy metabolism. Front. Physiol. 6 36
Castro EA, Carraça EV, Cupeiro R, López-Plaza B, Teixeira PJ, González-Lamuño D and Peinado AB 2020 The effects of the type of exercise and physical activity on eating behavior and body composition in overweight and obese subjects. Nutrients 12 557
Chambers L, McCrickerd K and Yeomans MR 2014 Optimising foods for satiety. Trends Food Sci. Technol. 41 149–160
Cheng V and Kashyap SR 2011 Weight considerations in pharmacotherapy for type 2 diabetes. J. Obes. 2011 984245
Clément K, Vaisse C, Lahlou N, et al. 1998 A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature 392 398–401
Coelho OGL, Cândido FG, Alfenas RCG 2019 Dietary fat and gut microbiota: mechanisms involved in obesity control. Crit. Rev. Food Sci. Nutr. 59 3045–3053
Comuzzie AG and Allison DB 1998 The search for human obesity genes. Science 280 1374–7
Coleman H, Quinn P and Clegg ME 2016 Medium-chain triglycerides and conjugated linoleic acids in beverage form increase satiety and reduce food intake in humans. Nutr. Res. 36 526- 533
Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, Kuo FC, Palmer EL, Tseng YH, Doria A, Kolodny GM and Kahn CR 2009 Identification and importance of brown adipose tissue in adult humans. N. Engl. J. Med. 360 1509–1517
Delvin EE, Lambert M, Levy E, O’Loughlin J, Mark S, Gray-Donald K and Paradis G 2010 Vitamin D status is modestly associated with glycemia and indicators of lipid metabolism in French-Canadian children and adolescents. J. Nutr. 140 987–991
den Hartigh LJ 2019 Conjugated linoleic acid effects on cancer, obesity, and atherosclerosis: a review of pre-clinical and human trials with current perspectives. Nutrients 11 370
den Hartigh LJ, Gao Z, Goodspeed L, Wang S, Das AK, Burant CF, Chait A and Blaser MJ 2018 Obese Mice Losing Weight Due to trans-10,cis-12 Conjugated linoleic acid supplementation or food restriction harbor distinct gut microbiota. J. Nutr. 148 562–572
den Hartigh LJ, Han CY, Wang S, Omer M and Chait A 2013 10E,12 Z-conjugated linoleic acid impairs adipocyte triglyceride storage by enhancing fatty acid oxidation, lipolysis, and mitochondrial reactive oxygen species. J. Lipid Res. 54 2964–2978.
den Hartigh LJ, Wang S, Goodspeed L, et al. 2017 Metabolically distinct weight loss by 10,12 CLA and caloric restriction highlight the importance of subcutaneous white adipose tissue for glucose homeostasis in mice. PLoS One 12 e0172912
Do MT, Chang VC, Mendez MA and de Groh M 2017 Urinary bisphenol A and obesity in adults: results from the Canadian Health Measures Survey. Health Promot. Chronic Dis. Prev. Can. 37 403–412
Earthman CP, Beckman LM, Masodkar K and Sibley SD 2012 The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. Int. J. Obes. 36 387–396
Ebrahimi-Mameghani M, Jamali H, Mahdavi R, Kakaei F, Abedi R and Kabir-Mamdooh B 2016 Conjugated linoleic acid improves glycemic response, lipid profile, and oxidative stress in obese patients with non-alcoholic fatty liver disease: a randomized controlled clinical trial. Croat. Med. J. 57 331–342
Feltrin KL, Little TJ, Meyer JH, Horowitz M, Smout AJ, Wishart J, Pilichiewicz AN, Rades T, Chapman IM and Feinle-Bisset C 2004 Effects of intraduodenal fatty acids on appetite, antropyloroduodenal motility, and plasma CCK and GLP-1 in humans vary with their chain length. Am. J. Physiol. Regul. Integr. Comp. Physiol. 287 R524–33
Feltrin KL, Little TJ, Meyer JH, Horowitz M, Rades T, Wishart J and Feinle-Bisset C 2007 Effects of lauric acid on upper gut motility, plasma cholecystokinin and peptide YY, and energy intake are load, but not concentration, dependent in humans. J. Physiol. 581 767–777
Ferreira L, Lisenko K, Barros B, Zangeronimo M, Pereira L and Sousa R 2014 Influence of medium-chain triglycerides on consumption and weight gain in rats: a systematic review. J. Animal Physiol. Animal Nutr. 98 1–8
Foster DW and McGarry JD 1982 The regulation of ketogenesis. Ciba Found. Symp. 87 120–131
Frood S, Johnston LM, Matteson CL and Finegood DT 2013 Obesity, Complexity, and the Role of the Health System. Curr. Obes. Rep. 2 320–326
Galgani J and Ravussin E 2011 Principles of Human Energy Metabolism. In: Ahoma RS (ed). Metabolic Basis of Obesity. Spriger: New York, pp 1–23. https://springerlink.bibliotecabuap.elogim.com/book/10.1007/978-1-4419-1607-5
Galvão CF, Xavier VF, da Silva LE, Gonçalves LCO, Gouveia PMDC and Gonçalves ARC 2018 Consumption of extra virgin olive oil improves body composition and blood pressure in women with excess body fat: a randomized, double-blinded, placebo-controlled clinical trial. Eur. J. Nutr. 57 2445–2455
Girardet C and Butler AA 2014 Neural melanocortin receptors in obesity and related metabolic disorders. Biochim Biophys Acta. 1842 482–494
Grün F 2014 The obesogen tributyltin. Vitam. Horm. 94 277–325
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL and Anis AH 2009 The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9 88
Gunasekaran R, Shaker MR, Mohd-Zin SW, Abdullah A, Ahmad-Annuar A and Abdul-Aziz NM 2017 Maternal intake of dietary virgin coconut oil modifies essential fatty acids and causes low body weight and spiky fur in mice. BMC Complement. Altern. Med. 17 79
Hamilton M, Hopkins LE, AlZahal O, MacDonald TL, Cervone DT, Wright DC, McBride BW and Dyck DJ 2015.Feeding butter with elevated content of trans-10, cis-12 conjugated linoleic acid to obese-prone rats impairs glucose and insulin tolerance. Lipids Health Dis. 14 119
Herrera BM, Keildson S and Lindgren CM 2011 Genetics and epigenetics of obesity. Maturitas 69 41–49
Hoffer LJ, Bistrian BR, Young VR, Blackburn GL and Matthews DE 1982 Metabolic effects of very low calorie weight reduction diets. J. Clin. Invest. 73 750–758
Hoppel CL 1982 Carnitine and carnitine palmitoyltransferase in fatty acid oxidation and ketosis. Fed. Proc. 41 2853–2857
Hu S, Wang L, Yang D, et al. 2018 Dietary fat, but not protein or carbohydrate, regulates energy intake and causes adiposity in mice. Cell Metab. 8 415–431.
Janesick AS and Blumberg, B 2016 Obesogens: an emerging threat to public health. Am. J. Obstet. Gynecol. 9214 559–565
Kaddam IM, Al-Shaikh AM, Abaalkhail BA, Asseri KS, Al-Saleh YM, Al-Qarni AA, Al-Shuaibi AM, Tamimi WG and Mukhtar AM 2017 Prevalence of vitamin D deficiency and its associated factors in three regions of Saudi Arabia. Saudi Med. J. 38 381–390
Kamphuis MM, Lejeune MP, Saris WH and Westerterp-Plantenga MS 2003 Effect of conjugated linoleic acid supplementation after weight loss on appetite and food intake in overweight subjects. Eur. J. Clin. Nutr. 57 1268–1274
Karam JG and McFarlane SI 2007 Secondary causes of obesity. Therapy 4 641–650
Kaur S, Gonzales MM, Strasser B, Pasha E, McNeely J, Tanaka H and Haley AP 2015 Central adiposity and cortical thickness in midlife. Psychosom. Med. 77 671–678
Kavanagh K, Jones KL, Sawyer J, Kelley K, Carr JJ, Wagner JD and Rudel LL 2007 Trans-fat Diet Induces Abdominal Obesity and Changes in Insulin Sensitivity in Monkeys. Obesity 15 1675–1684
Kennedy A, Martinez K, Schmidt S, Mandrup S, LaPoint K and McIntosh M 2010 Antiobesity mechanisms of action of conjugated linoleic acid. J. Nutr. Biochem. 21 171–179
Kien CL, Bunn JY and Ugrasbul F 2005 Increasing dietary palmitic acid decreases fat oxidation and daily energy expenditure. Am. J. Clin. Nutr. 82 320–326
Kim SH and Park MJ 2014 Phthalate exposure and childhood obesity. Ann. Pediatr. Endocrinol. Metab. 19 69–75
Kishino S, Ogawa J, Omura Y, Matsumura K and Shimizu S 2002 Conjugated linoleic acid production from linoleic acid by lactic acid bacteria. J. Am. Oil Chem. Soc. 79 159–163
Koba K and Yanagita T 2014 Health benefits of conjugated linoleic acid (CLA). Obes. Res. Clin. Pract. 8 e525–e532
Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W and Rimm E 2003 Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am. J. Clin. Nutr. 78 719–727
Krotkiewski M 2001 Value of VLCD supplementation with medium chain triglycerides. Int. J. Obes. Relat. Metab. Disord. 25 1393–1400
Laeger T, Metges CC and Kuhla B 2010 Role of beta-hydroxybutyric acid in the central regulation of energy balance. Appetite 54 450–455
LaRosa PC, Miner J, Xia Y, Zhou Y, Kachman S and Fromm ME 2006 Trans-10, cis-12 conjugated linoleic acid causes inflammation and delipidation of white adipose tissue in mice: a microarray and histological analysis. Physiol. Genomics 27 282–294
Lee Y, Mottillo EP and Granneman JG 2014 Adipose tissue plasticity from WAT to BAT and in between. Biochim. Biophys. Acta 1842 358–369
Lehnen TE, da Silva MR, Camacho A, Marcadenti A and Lehnen AM 2015 A review on effects of conjugated linoleic fatty acid (CLA) upon body composition and energetic metabolism. J. Int. Soc. Sports Nutr. 12 36
Lemarié F, Beauchamp E, Dayot S, Duby C, Legrand P and Rioux V 2015 Dietary caprylic acid (C8:0) does not increase plasma acylated ghrelin but decreases plasma unacylated ghrelin in the rat. PLoS One 10 e0133600
Lemarié F, Beauchamp E, Legrand P and Rioux V 2016 Revisiting the metabolism and physiological functions of caprylic acid (C8:0) with special focus on ghrelin octanoylation. Biochimie 120 40–48
Lepore SM, Morittu VM, Celano M, Trimboli F, Oliverio M, Procopio A, Di Loreto C, Damante G, Britti D, Bulotta S and Russo D 2015 Oral administration of oleuropein and its semisynthetic peracetylated derivative prevents hepatic steatosis, hyperinsulinemia, and weight gain in mice fed with high fat cafeteria diet. Int.J. Endocrinol. 2015 431453
Lim S, Ahn SY, Song IC, Chung MH, Jang HC, Park KS, Lee KU, Pak YK and Lee HK 2009. Chronic Exposure to the Herbicide, Atrazine, Causes Mitochondrial Dysfunction and Insulin Resistance. PLoS ONE 4 e5186
Liu Y, Wang J, Zhang R, et al. 2009 A good response to oil with medium- and long-chain fatty acids in body fat and blood lipid profiles of male hypertriglyceridemic subjects. Asia Pac. J. Clin. Nutr. 18 351–358
Liu YH, Zhang Y, Xu Q, Yu XM, Zhang XS, Wang J, Xue C, Yang XY, Zhang RX and Xue CY 2012 Increased norepinephrine by medium-chain triglyceride attributable to lipolysis in white and brown adipose tissue of C57BL/6J mice. Biosci. Biotechnol. Biochem. 76 1213–1218
Lo JC, Feigenbaum SL, Yang J, Pressman AR, Selby JV and Go AS 2006 Epidemiology and adverse cardiovascular risk profile of diagnosed polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 91 1357–63
Lombardo GE, Lepore SM, Morittu VM, et al. 2018 Effects of Oleacein on High-Fat Diet-Dependent Steatosis, Weight Gain, and Insulin Resistance in Mice. Front. Endocrinol. 9 116
López-Plaza B, Bermejo LM, Koester Weber T, Parra P, Serra F, Hernández M, Palma Milla S and Gómez-Candela C 2013 Effects of milk supplementation with conjugated linoleic acid on weight control and body composition in healthy overweight people. Nutr. Hosp. 28 2090–2098
Lowell BB and Flier JS 1997 Brown adipose tissue, beta 3-adrenergic receptors, and obesity. Annu. Rev. Med. 48 307–316
Ludwig T, Worsch S, Heikenwalder M, Daniel H, Hauner H and Bader BL 2013 Metabolic and immunomodulatory effects of n-3 fatty acids are different in mesenteric and epididymal adipose tissue of diet-induced obese mice. Am. J. Physiol. Endocrinol. Metab. 304 E1140–E1156
Maas MIM, Hopman WPM, Katan MB and Jansen JBMJ 1998 Release of peptide YY and inhibition of gastric acid secretion by long-chain and medium-chain triglycerides but not by sucrose polyester in men. Eur. J. Clin. Investig. 28 123–130
Mądry E, Chudzicka-Strugała I, Grabańska-Martyńska K, Malikowska K, Grebowiec P, Lisowska A, Bogdański P and Walkowiak J 2016 Twelve weeks CLA supplementation decreases the hip circumference in overweight and obese women. A double-blind, randomized, placebo-controlled trial. Acta Sci. Pol. Technol. Aliment.15 107–113
Madsen L, Pedersen LM, Lillefosse HH, et al. 2010 UCP1 induction during recruitment of brown adipocytes in white adipose tissue is dependent on cyclooxygenase activity. PLoS One 5 e11391
Maher T, Deleuse M, Thondre S, Shafat A and Clegg ME 2020 A comparison of the satiating properties of medium-chain triglycerides and conjugated linoleic acid in participants with healthy weight and overweight or obesity. Eur. J. Nutr. https://doi.org/10.1007/s00394-020-02235-y
Marques TM, Wall R, O’Sullivan O, Fitzgerald GF, Shanahan F, Quigley EM, Cotter PD, Cryan JF, Dinan TG, Ross RP and Stanton C 2015 Dietary trans-10, cis-12-conjugated linoleic acid alters fatty acid metabolism and microbiota composition in mice. Br. J. Nutr. 113 728–738
Marten B, Pfeuffer M and Schrezenmeir J 2006 Medium-chain triglycerides. Int. Dairy J. 16 1374–1382
Martins SV, Madeira A, Lopes PA, Pires VM, Alfaia CM, Prates JA, Moura T and Soveral G 2015 Adipocyte membrane glycerol permeability is involved in the anti-adipogenic effect of conjugated linoleic acid. Biochem. Biophys. Res. Commun. 458 356–361
Matzinger D, Gutzwiller JP, Drewe J, Orban A, Engel R, D’Amato M, Rovati L and Beglinger C 1999 Inhibition of food intake in response to intestinal lipid is mediated by cholecystokinin in humans. Am. J. Physiol. 277 R1718–1724
McCarty MF and DiNicolantonio JJ 2016 Lauric acid-rich medium-chain triglycerides can substitute for other oils in cooking applications and may have limited pathogenicity. Open Heart 3 e000467
McLaughlin J, Grazia Lucà M, Jones MN, D’Amato M, Dockray GJ and Thompson DG 1999 Fatty acid chain length determines cholecystokinin secretion and effect on human gastric motility. Gastroenterology 116 46–53
Merola N, Castillo J, Benavente-García O, Ros G and Nieto G 2017 The effect of consumption of citrus fruit and olive leaf extract on lipid metabolism. Nutrients 9 E1062
Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ and Willett WC 2006 Trans-fatty acids and cardiovascular disease. N. Engl. J. Med. 354 1601–1613
Nagao K and Yanagita T 2010 Medium-chain fatty acids: functional lipids for the prevention and treatment of the metabolic syndrome. Pharmacol. Res. 61 208–212
Namazi N, Irandoost P, Larijani B and Azadbakht L 2019 The effects of supplementation with conjugated linoleic acid on anthropometric indices and body composition in overweight and obese subjects: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 59 2720–2733
Newcomer JW and Lieberman JA 2007 Comparing safety and tolerability of antipsychotic treatment. J. Clin. Psychiatry 68 e07
Newport MT 2013 Alzheimer’s disease - what if there were a cure? 2nd edn. Laguna Beach: Basic Health Publications
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany E C, Biryukov S, Abbafati C, Stapelberg N and et al 2014 Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384 766–781
Nilsson A, Johansson E, Ekström L, and Björck I 2013 Effects of a brown beans evening meal on metabolic risk markers and appetite regulating hormones at a subsequent standardized breakfast: a randomized cross-over study. PLoS One 8 e59985
Norris LE, Collene AL, Asp ML, Hsu JC, Liu LF, Richardson JR, Li D, Bell D, Osei K, Jackson RD and Belury MA 2009 Comparison of dietary conjugated linoleic acid with safflower oil on body composition in obese postmenopausal women with type 2 diabetes mellitus. Am. J. Clin. Nutr. 90 468–476
Oliveira-de-Lira L, Santos EMC, de Souza RF, Matos RJB, Silva MCD, Oliveira LDS, Nascimento TGD, Schemly PALS and Souza SL 2018 Supplementation-dependent effects of vegetable oils with varying fatty acid compositions on anthropometric and biochemical parameters in obese women. Nutrients 10 E932
O’Reilly ME, Lenighan YM, Dillon E, Kajani S, Curley S, Bruen R, Byrne R, Heslin AM, Moloney AP, Roche HM and McGillicuddy FC 2020 Conjugated linoleic acid and alpha linolenic acid improve cholesterol homeostasis in obesity by modulating distinct hepatic protein pathways. Mol. Nutr. Food Res. 64 e1900599
Pal L, Berry A, Coraluzzi L, Kustan E, Danton C, Shaw J and Taylor H 2012 Therapeutic implications of vitamin D and calcium in overweight women with polycystic ovary syndrome. Gynecol. Endocrinol. 28 965–968
Parnell JA and Reimer RA 2009 Weight loss during oligofructose supplementation is associated with decreased ghrelin and increased peptide YY in overweight and obese adults. Am. J. Clin. Nutr. 89 1751–1759
Patten SB, Williams JV, Lavorato DH, Khaled S and Bulloch AG 2011 Weight gain in relation to major depression and antidepressant medication use. J. Affect. Disord. 134 288–293
Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr, Ludwig DS 2005 Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 365 36–42
Phillips CM, Kesse-Guyot E, McManus R, Hercberg S, Lairon D, Planells R, Roche HM 2012 High dietary saturated fat intake accentuates obesity risk associated with the fat mass and obesity-associated gene in adults. J. Nutr. 142 824–831
Piers LS, Walker KZ, Stoney RM, Soares MJ and O’Dea K 2003 Substitution of saturated with monounsaturated fat in a 4-week diet affects body weight and composition of overweight and obese men. Br. J.Nutr. 90 717–727
Piggott M, Owens J, O’Brien J, Paling S, Wyper D, Fenwick J, Johnson M, Perry R and Perry, E 2002 Comparative distribution of binding of the muscarinic receptor ligands pirenzepine, AF-DX 384, (R,R)-I-QNB and (R,S)-I-QNB to human brain. J. Chem. Neuroanat. 24 211–223.
Poirier H, Shapiro JS, Kim RJ and Lazar MA 2006 Nutritional supplementation with trans-10, cis-12-conjugated linoleic acid induces inflammation of white adipose tissue. Diabetes 55 1634–41
Poppitt SD, Strik CM, MacGibbon AK, McArdle BH, Budgett SC and McGill AT 2010 Fatty acid chain length, postprandial satiety and food intake in lean men. Physiol. Behav. 101 161–167
Raatz SK, Conrad Z, Johnson LK, Picklo MJ, Jahns L 2017 Relationship of the reported intakes of fat and fatty acids to body weight in US adults. Nutrients 9 E438
Ràfols ME 2014 Adipose tissue: Cell heterogeneity and functional diversityTejido adiposo: heterogeneidad celulary diversidad functional. Endocrinol. Nut. 61 100–112
Reardon M, Gobern S, Martinez K, Shen W, Reid T and McIntosh M 2012 Oleic acid attenuates trans-10, cis-12 conjugated linoleic acid-mediated inflammatory gene expression in human adipocytes. Lipids 47 1043–1051
Rial SA, Karelis AD, Bergeron KF and Mounier C 2016 Gut Microbiota and Metabolic Health: The Potential Beneficial Effects of a Medium Chain Triglyceride Diet in Obese Individuals. Nutrients 8 E281
Riediger T, Bothe C, Becskei C, Lutz TA 2004 Peptide YY directly inhibits ghrelin-activated neurons of the arcuate nucleus and reverses fasting-induced c-Fos expression. Neuroendocrinol 79 317–326
Risérus U, Vessby B, Arner P and Zethelius B 2004 Supplementation with trans10cis12-conjugated linoleic acid induces hyperproinsulinaemia in obese men: close association with impaired insulin sensitivity. Diabetologia 47 1016–1019
Rosen T, Bosaeus I, TöIli J, Lindstedt G and Bengtsson B 1993 Increased body fat mass and decreased extracellular fluid volume in adults with growth hormone deficiency. Clin. Endocrinol. 38 63–71
Rothenberg DO, Zhou C and Zhang L 2018 A Review on the Weight-Loss Effects of Oxidized Tea Polyphenols. Molecules. 23 E1176
Ryde SIS, Saunders NH, Birks JL, Ali PA, Thomas DW, Morgan VD, Evans CJ, Al-Zeibak A, Dutton J and Sivyer A 1993 The effects of VLCD on body composition. In: Krietzman SN, Howard AN (eds). The Swansea trial. Smith Gordon: London, pp 31 – 54.
Sáinz N, Barrenetxe J, Moreno-Aliaga MJ and Martínez JA 2015 Leptin resistance and diet-induced obesity: central and peripheral actions of leptin. Metabolism 64 35–46
Santini F, Marzullo P, Rotondi M, Ceccarini G, Pagano L and Ippolito S 2014 Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease. Eur. J. Endocrinol. 171 R137–R152
Schwab U, Lauritzen L, Tholstrup T, Haldorssoni T, Riserus U, Uusitupa M and Becker W 2014 Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food Nutr. Res. 10 58
Shadman Z, Taleban FA, Saadat N and Hedayati M 2013 Effect of conjugated linoleic acid and vitamin E on glycemic control, body composition, and inflammatory markers in overweight type2 diabetics. J. Diabetes Metab. Disord. 12 42.
Shen W, Chuang CC, Martinez K, Reid T, Brown JM, Xi L, Hixson L, Hopkins R, Starnes J and McIntosh M 2013 Conjugated linoleic acid reduces adiposity and increases markers of browning and inflammation in white adipose tissue of mice. J. Lipid Res. 54 909–922
Shen W and McIntosh MK 2016 Nutrient Regulation: Conjugated Linoleic Acid’s Inflammatory and Browning Properties in Adipose Tissue. Annu. Rev. Nutr. 36 183–210
Snijder MB, van Dam RM, Visser M, Deeg DJ, Dekker JM, Bouter LM, Seidell JC and Lips P 2005 Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J. Clin Endocrinol. Metab. 90 4119–23
Srinivasan S, Ogle GD, Garnett SP, Briody JN, Lee JW and Cowell CT 2004 Features of the metabolic syndrome after childhood Craniopharyngioma. J. Clin. Endocrinol. Metab. 89 81–6
Stein EM, Strain G, Sinha N, Ortiz D, Pomp A, Dakin G, McMahon DJ, Bockman R and Silverberg SJ 2009 Vitamin D insufficiency prior to bariatric surgery: risk factors and a pilot treatment study. Clin. Endocrinol. 71 176–183
St-Onge MP and Jones PJH 2002 Medium chain triglyceride consumption increases energy expenditure relative to long chain triglyceride in overweight men. Am. J. Clin. Nutr. 75 340S
St-Onge MP, Mayrsohn B, O’Keeffe M, Kissileff HR, Choudhury AR and Laferrère B 2014 Impact of medium and long chain triglycerides consumption on appetite and food intake in overweight men. Eur. J. Clin. Nutr. 68 1134–1140
Strasser B and Fuchs D 2016 Diet Versus Exercise in Weight Loss and Maintenance: Focus on Tryptophan. Int. J. Tryptophan Res. 9 9–16
Sung MH, Liao FH and Chien YW 2018 Medium-Chain Triglycerides Lower Blood Lipids and Body Weight in Streptozotocin-Induced Type 2 Diabetes Rats. Nutrients 10 pii: E963
Tavares V, Hirata MH and Hirata RDC 2007 Peroxisome proliferator-activated receptor gamma (PPARgamma): molecular study in glucose homeostasis, lipid metabolism and therapeutic approach. Arch. Endocrinol. Metabol. 51 526–533
Tchkonia T, Giorgadze N, Pirtskhalava T, Tchoukalova Y, Karagiannides I, Forse RA, DePonte M, Stevenson M, Guo W, Han J, Waloga G, Lash TL, Jensen MD and Kirkland JL 2002 Fat depot origin affects adipogenesis in primary cultured and cloned human preadipocytes. Am. J. Physiol. Regul. Integr. Comp. Physiol. 282 R1286–R1296
Trayhurn P 2005 Endocrine and signalling role of adipose tissue: new perspectives on fat. Acta Physiol. Scand. 184 285–293
van Baak MA and Mariman ECM 2019 Dietary strategies for weight loss maintenance. Nutrients. 11 1916
Van Wymelbeke V, Himaya A, Louis-Sylvestre J and Fantino M 1998 Influence of medium-chain and long-chain triacylglycerols on the control of food intake in men. Am. J. Clin. Nutr. 68 226–234
Van Wymelbeke V, Louis-Sylvestre J and Fantino M 2001 Substrate oxidation and control of food intake in men after a fat-substitute meal compared with meals supplemented with an isoenergetic load of carbohydrate, long-chain triacylglycerols, or medium-chain triacylglycerols. J.Clin. Nutr. 74 620–630
Whitmer RA, Gunderson EP, Quesenberry Jr CP, Zhou J and Yaffe K 2007 Body mass index in midlife and risk of Alzheimer disease and vascular dementia. Curr. Alzheimer Res. 4 103–9
Wajchenberg BL, Bosco A, Marone MM, Levin S, Rocha M, Lerário AC, Nery M, Goldman J and Liberman B 1995 Estimation of body fat and lean tissue distribution by dual energy X-ray absorptiometry and abdominal body fat evaluation by computed tomography in Cushing’s disease. J. Clin. Endocrinol. Metab. 80 2791–2794
Wakayo T, Whiting SJ and Belachew T 2016 Vitamin D deficiency is associated with overweight and/or obesity among school children in central ethiopia: a cross-sectional study. Nutrients 8 190
Watras AC, Buchholz AC, Close RN, Zhang Z and Schoeller DA 2007 The role of conjugated linoleic acid in reducing body fat and preventing holiday weight gain. Int. J. Obes. 31 481–487
Wei Y, Zhang JJ, Li Z, Gow A, Chung KF, Hu M, Sun Z, Zeng L, Zhu T, Jia G, Li X, Duarte M and Tang X 2016 Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: findings from a natural experiment in Beijing. FASEB J. 30 2115–2122
World Health Organization (WHO) 1985 Energy and protein requirements : report of a Joint FAO/WHO/UNU Expert Consultation – Geneva, Switzeland Technical Report Series no. 724
Wozniak SE, Gee LL, Wachtel MS and Frezza EE 2009 Adipose tissue: the new endocrine organ? A review article. Dig. Dis. Sci. 54 1847–1856
Yamashita AS, Lira FS, Lima WP, Carnevali LC, Gonçalves DC, Tavares FL and et al 2008 Influence of aerobic physical training in the motochondrial transport of long chain fatty acids in the skeletal muscle: role of the carnitine palmitoil transferase. Rev. Bras. Med. Esporte. 14 150–154
Yang CS, Wang H and Sheridan ZP 2018 Studies on prevention of obesity, metabolic syndrome, diabetes, cardiovascular diseases and cancer by tea. J. Food Drug Anal. 26 1–13
Yanovski SZ and Yanovski JA 2014 Drugs for the treatment of obesity–reply. JAMA 311 1807
Yudkin JS, Eringa E and Stehouwer CD. 2005 “Vasocrine” signalling from perivascular fat: a mechanism linking insulin resistance to vascular disease. Lancet 365 1817–1820
Zhang Y, Xu Q, Liu YH, Zhang XS, Wang J, Yu XM, Zhang RX, Xue C, Yang XY and Xue CY 2015 Medium-Chain Triglyceride Activated Brown Adipose Tissue and Induced Reduction of Fat Mass in C57BL/6J Mice Fed High-fat Diet. Biomed. Environ. Sci. 28 97–104
Zhao J, Unelius L, Bengtsson T, Cannon B and Nedergaard J 1994 Coexisting beta-adrenoceptor subtypes: significance for thermogenic process in brown fat cells. Am. J. Physiol. 267 C969–C979
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Ullas Kolthur-Seetharam.
Corresponding editor: Ullas Kolthur-Seetharam
Rights and permissions
About this article
Cite this article
Ibrahim, K.S., El-Sayed, E.M. Dietary conjugated linoleic acid and medium-chain triglycerides for obesity management. J Biosci 46, 12 (2021). https://doi.org/10.1007/s12038-020-00133-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12038-020-00133-3