Abstract
Obesity leads to several chronic morbidities including type 2 diabetes, dyslipidemia, atherosclerosis, and hypertension, which are major components of the metabolic syndrome (MetS). Low-grade inflammation has been identified as a key factor in the development of MetS features affecting obese subjects. Several studies have proposed beneficial effects of the omega-3 polyunsaturated fatty acids (n-3 PUFAs) for the prevention and amelioration of MetS features. In this chapter, we will focus on reviewing randomized, controlled trials that evaluate the effects of supplementation with marine-derived EPA and DHA on weight loss, insulin sensitivity, lipid metabolism, blood pressure, and inflammation in overweight/obese subjects with MetS characteristics. Supplementation with n-3 PUFAs may be an interesting therapy to reduce hypertriglyceridemia and hypertension, while the ability of n-3 PUFAs to promote weight loss, insulin sensitivity, and changes in cholesterol metabolism in patients with MetS remains controversial. The role of n-3 PUFAs-derived proresolving lipid mediators such as resolvins, protectins, and maresins in MetS is also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Omega-3 fatty acids
- Obesity
- Metabolic syndrome
- Insulin resistance
- Lipid metabolism
- Blood pressure
- Inflammation
Obesity and Metabolic Syndrome
The incidence of the metabolic syndrome (MetS) is increasing at an alarming rate, becoming a major public and clinical problem worldwide. MetS is defined as a cluster of pathophysiological conditions, which include abnormalities in blood pressure, low high density lipoprotein-cholesterol (HDL-ch), high triglycerides (TG), altered glucose tolerance, and increased waist circumference, raising the risk of cardiovascular disease (CVD) and diabetes [1, 2]. Different international organizations have attempted to determine the cutoff for the MetS criteria in adult population, and although there is a consensus in almost all parameters, discrepancies on the cutoff for waist circumference continue [3]. Despite the genetic variations between populations, it is widely accepted that the appearance of MetS is closely related to obesity, inappropriate dietary behaviors, and sedentary lifestyle [1].
The imbalance in the carbohydrate and lipid metabolism in MetS patients is characterized by impaired insulin response, high plasma-free fatty acids (FFA) concentration, hypertriglyceridemia, low levels of HDL-ch, and changes in the composition of both lipoproteins and apolipoproteins; all these alterations work together to deteriorate cardiovascular health and to increase the risk of cardiovascular disease [4].
Initially, in an attempt to restore glucose metabolism, the hyperinsulinemia is the first stage that precedes insulin resistance, and when the insulin signaling is not enough to promote glucose uptake in peripheral tissues, the increment in the glucose production triggers type 2 diabetes mellitus [5]. In a normal state, the insulin secreted by the β-cells of pancreas is able to suppress the release of fatty acids by adipose tissue and to decrease the concentration of lipoprotein lipase in peripheral tissues [4]; however, in an insulin resistance condition, this mechanism fails, promoting an abnormal release of FFA into circulation which in turn favors their flux and accumulation in key energetic organs as the liver [5]. The increment of lipids in the liver may raise the production of TG and the release of triglyceride-rich lipoproteins (TRLs) such as very low density lipoprotein (VLDL), favoring an atherogenic state. Thus, hypertriglyceridemia is associated with the predominance of the atherogenic small-density low density lipoprotein (sdLDL) versus the highly buoyant less atherogenic LDL, as well as with low HDL-ch levels and high levels of LDL-ch [4, 5]. Furthermore, there is a disproportion between the TG synthesis and TG clearance, which favors the increment in VLDL proportion, leading to the augmentation of the apolipoprotein B (apoB) production and of the remnant lipoprotein particle concentration [6].
Additionally, in MetS, there are other factors that are implicated in lipid metabolism disorders as the increment in the synthesis of apolipoprotein C-III (apo C-III) and the cholesteryl ester transfer protein (CETP). The apo C-III is carried through VLDL particles and could disrupt the action of lipoprotein lipase and inhibit the uptake of VLDL remnants by liver receptors [7]. Also, the increased activity of CETP promotes the transfer of TG from VLDL to LDL, resulting in triglyceride-rich LDL, which are the favorite substrate of hepatic lipase, leading to the formation of sdLDL particles [6], which are more likely to be filter into the arterial wall and are more susceptible to oxidation that the highly buoyant LDL particles [4, 7]. Increased levels of VLDL can also promote alterations in the composition of HDL, leading to the formation of sdLDL and increased catabolism of these particles [6].
The metabolic disturbances characterizing the MetS condition perturb the normal endothelial function, increasing the risk of cardiovascular diseases and promoting a vicious cycle in which the high blood pressure, hyperglycemia, hyperinsulinemia, oxidative stress, and inflammation are implicated [8, 9]. Taking into account the fact that endothelium is the major regulator of vascular homeostasis, the endothelial dysfunction is an important factor in the appearance of circulatory pathologies. The alterations in the renin–angiotensin–aldosterone system and the increment of the oxidative stress during hypertension are associated with the impairments of important vasodilator pathways in the endothelium leading to endothelial dysfunction, including alterations in the nitric oxide (NO) cycle [8–10]. Moreover, the increment in the arterial stiffness either in general population and in type 2 diabetic patients is a predictor factor to cardiovascular risk and mortality [11].
In summary, insulin resistance seems to be a major underlying mechanism responsible for the development of MetS, and a number of studies have also suggested that the low-grade chronic inflammatory state associated with obesity and MetS plays a key role in the development of insulin resistance and other metabolic complications [12].
n-3 PUFAs in Obesity and Metabolic Syndrome
The long-chain omega-3 polyunsaturated fatty acids (n-3 PUFAs) are essential nutrients which can be divided according to their natural food source in plant-derived (alpha-linolenic acid, C18:3) and marine-derived (eicosapentaenoic acid (EPA), C20:5 and docosahexaenoic acid (DHA), C22:6). The principal sources of alpha-linolenic acid are the vegetable oil (flaxseeds, canola, soybean), while EPA and DHA are found in fatty fish (salmon, herring, mackerel, and sardines) [13]. Although it has been suggested that alpha-linolenic acid is converted to EPA and DHA, the conversion rate is controversial and apparently modest [14, 15], and the beneficial effects of n-3 PUFAs in cardiovascular health have been principally attributed to the marine-derived EPA and DHA.
In patients with MetS, decreased levels of erythrocyte content of EPA and DHA and increased ratio of n-6/n-3 have been observed, being associated with the development of insulin resistance [16]. Additionally, different studies have observed that high consumption of fish, especially fatty fish rich in n-3 PUFAs, is inversely correlated with MetS [17].
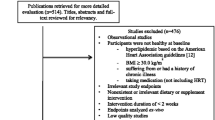
In this context, the consumption and supplementation of n-3 PUFAs for the prevention and amelioration of MetS features have been proposed. In this chapter, we will focus on reviewing randomized, controlled trials that evaluate the effects of supplementation with marine-derived EPA and DHA. We excluded the studies that used functional products enriched with n-3 PUFAs, also trials with population with previous cardiovascular event or heart disease, and studies with subjects under medication that could affect the target metabolic outcomes as lipid-lowering agents, antihypertensive, and hypoglycemic drugs.
Effects of n-3 PUFAs on Weight Loss and Body Composition
Moderate weight loss (5–10 % of body weight) can help to restore insulin sensitivity and greatly reduce MetS features. Several studies have evaluated the effects of n-3 PUFAs supplementation on weight loss, rising to contradictory outcomes (Table 14.1). The majority of trials with n-3 PUFAs supplementation have been performed using a combination of EPA and DHA with or without an energy-restricted regime and with and without exercise.
n-3 PUFAs Trials with Isocaloric Diets
The study by Ebrahimi et al. [18] in Iranian males and females, giving a general dietary advice to both study groups and using a supplementation of 1 g/day of fish oils (containing 180 mg EPA and 120 mg DHA) for 6 months, observed that n-3 PUFAs promoted a reduction in body weight. Moreover, the trials by Kabir et al. [19] providing 1.8 g/day of n-3 PUFAs (1.08 g EPA + 0.72 g DHA) found no changes in body weight but a reduction in fat mass and adipocyte diameter. Similarly, the study by Hill et al. [20] evaluated the effects of n-3 PUFAs (6 g/day of tuna fish oil containing 260 mg DHA and 60 mg EPA per gram) for 12 weeks in combination or in the absence of a regular exercise (3 times/week), finding that supplementation with fish oil promoted a decrease in fat mass independently of the exercise effect.
In contrast, a 90-day short-time study conducted in Brazilians with a supplementation of n-3 PUFAs in a dose of 3 g/day (180 mg EPA plus 120 mg DHA per capsule) found no effects of supplementation in body weight and waist circumference [21, 22]. Similarly, the study by Tousoulis et al. [23] in Caucasic males and females showed that the supplementation of the usual diet with 2 g/day of n-3 PUFAs (46 % EPA and 38 % DHA) during 12 weeks with a washout period of four weeks between treatments did not promote a reduction in body weight.
n-3 PUFAs Trials with Hypocaloric Diets
While some trials have reported that supplementation of hypocaloric diets with n-3 PUFAs may promote additional weight loss, most of the studies have not found body weight-lowering properties for n-3 PUFAs (Table 14.1). Thus, the study by Tapsell et al. [24] found no additional effects on body weight loss in Australian overweight or obese adults consuming fatty fish or fish oil supplementation (180 g fatty fish alone or plus 1 g/day of fish oil capsule containing 420 mg EPA and 210 mg DHA) for 12 months. Additionally, the study by Su et al. [25] in Taiwanese women with a calorie-restricted diet supplemented with 2.13 g/day of n-3 PUFAs showed that the treatment had no additional effects on anthropometry and body composition variables. DeFina et al. [26] using a supplementation of n-3 PUFAs (3 g/day EPA plus DHA at a ratio of 5:1) in conjunction with diet and exercise during 24 weeks observed no effects of supplementation in weight loss and body composition in overweight/obese subjects. Also, the study by Munro and Garg [27] supplementing 6 × 1 g capsules/day containing 70 mg EPA plus 270 mg DHA for 12 weeks in conjunction with an energy-restricted diet found no differences in the body weight and waist circumference losses.
Some trials have addressed the effects of n-3 PUFAs supplementation not only during a weight loss period but also during a weight maintenance phase. Thus, the study by Krebs et al. [28], which lasted 24 weeks and included first five weeks on an energy-restricted diet, followed by a maintenance period in the subsequent weeks, observed no differential effect on weight loss with n-3 PUFAs supplementation (1.3 g/day of EPA plus 2.9 g/day of DHA) in overweight/obese women. In the same way, Munro and Garg [29] reported that supplementation for 14 weeks with n-3 PUFAs (6 × 1 g capsules/day containing 70 mg EPA plus 270 mg DHA) during a very-low-energy-restricted diet (4 weeks), followed by a maintenance period of 10 weeks, did not promote a greater decrease in anthropometric measurements and fat mass in obese subjects.
Interestingly, another trial of the same group reported that a prior supplementation during 4 weeks with n-3 PUFAs (6 × 1 g capsules/day containing 70 mg EPA plus 270 mg DHA) followed by a 4-week very-low-energy-restricted diet promoted a greater reduction in weight than placebo but only in healthy overweight/obese women, suggesting that supplementation with n-3 PUFAs had a time-dependent effect on weight loss, especially in females [30]. Some studies have suggested a sex-based interaction of n-3 PUFAs. In this context, the trial by Thorsdottir et al. [31], performed in overweight or obese adults under a personalized energy-restricted diet during 8 weeks, observed a greater reduction in weight loss and waist circumference only in men, in the groups taking fish (150 g cod or salmon 3 times/week) or fish oil capsules (1.3 g/day EPA plus DHA). The study by Kunesova et al. [32], performed in severely obese women during 3 weeks with a very-low-calorie diet and light-to-moderate physical activity, also showed that the supplementation with n-3 PUFAs (2.98 g/day EPA plus DHA at a ratio of 2:1) promoted a decrease in body weight, body mass index (BMI), and hip circumference.
The potential differential effects of EPA and DHA on weight loss and body composition have not been clearly addressed. Interestingly, the study by Kunesova et al. [32] found a significant negative correlation between BMI change and phospholipid docosahexaenoic acid change, suggesting that docosahexaenoate (22:6n-3) seems to be the active component. In this context, the study by Vasickova et al. [33] has also suggested a possible beneficial effect of DHA intake on body weight reduction in obese children that consumed an extra 300 mg DHA and 42 mg EPA daily for a period of 3 weeks. Regarding EPA, the Japan Obesity and Metabolic Syndrome Study, a randomized, single-blind, parallel design trial with a supplementation of 1.8 g/day of highly purified (>98 %) EPA in combination with a hypocaloric diet (25 kcal/kg ideal body weight) during 3 months, did not find changes in BMI or waist circumference [34, 35]. In concordance with this, the study by Huerta et al. [36] with a supplementation of 1.3 g EPA-rich capsules (80 %) shows no additional effect of body weight on the energy-restricted diet in the supplemented groups, although EPA promoted a moderate decrease in the waist-to-hip ratio.
n-3 PUFAs and Carbohydrate Metabolism in Metabolic Syndrome
Although some evidence in murine models and in overweight or obese healthy subjects has suggested that the supplementation with n-3 PUFAs could promote an improvement in insulin sensitivity [37], most of the trials in subjects with MetS characteristics have observed that supplementation with n-3 PUFAs, at different ratios of EPA:DHA and at different doses (1–4 g), has no significant effect on decreasing glucose metabolism parameters or improving the insulin sensitivity [23, 25, 26, 28, 38–46]. In contrast, the study by Ramel et al. [47], performed in overweight/obese young adults following an energy-restricted diet, detected that the supplementation with fish oil (EPA + DHA) improved insulin sensitivity independently of changes in body weight, TG, or adiponectin. Table 14.2 summarizes the clinical trials assessing the effects of n-3 PUFAs supplementation on glucose metabolism in subjects with MetS features.
Because some studies have suggested that EPA and DHA have different hemodynamic and metabolic effects, randomized trials evaluating the supplementation of both n-3 PUFAs separately are discussed. In this context, studies using a supplementation of DHA (2–3 g/day) in conjunction with isocaloric diet did not find any effect on glucose parameters in subjects with MetS features [41, 48]. Moreover, the study by Mori et al. [49], which evaluated the differential effect of DHA and EPA (4 g/day) on females and males following their usual diet, revealed that both EPA and DHA promoted an increment in fasting insulin levels without significant changes in fasting glucose. The differential effects observed between trials with DHA supplementation could be due to the different n-3 PUFAs source (ethyl ester capsules or algae source), the isocaloric diet, and the dose of DHA used.
In summary, the evidence suggests that supplementation with n-3 PUFAs has none or marginal effects on glucose homeostasis and insulin sensitivity in subjects with MetS features.
N-3 PUFAs and Lipid Metabolism in Metabolic Syndrome
Effects on Triglycerides and Triglyceride-Rich Lipoproteins
Several trials performed in subjects with MetS features, using either different ratios of EPA:DHA or these marine-derived n-3 PUFAs separately, in combination or not with an energy-restricted diet and with a range duration between 6 weeks and 1 year, have evidenced the ability of n-3 PUFAs to decrease TG levels [23, 28, 39, 40, 42–44, 46, 48–56] along with the reduction in the TRL and remnant lipoprotein particle concentration [38, 45, 48, 53, 55, 57, 58] (see Table 14.2 for further information about these trials). Additionally, based on the present data, the detriment in TG blood concentration could promote a drop in both the production and concentration of some apolipoproteins, principally apo B48 and apo CIII [41, 42, 45]. Moreover, the supplementation with n-3 PUFAs has shown to improve the postprandial TG response characteristic of MetS subjects [45, 55]. However, in some few trials, this hypotriglyceridemic effect was not clearly perceived. Thus, Su et al. [25] observed a greater but non-significant reduction in TG levels with n-3 PUFAs supplementation in MetS females with an energy-restricted diet. Moreover, DeFina et al. [26] reported also a lack of additional effect on TG in females and males with n-3 PUFAs supplementation in conjunction with exercise and dietary counseling. However, it is important to mention that this study was conducted mainly in healthy overweight to obese individuals (<30 % with MetS), which likely masked potential metabolic reduction in triglycerides in those with hypertriglyceridemia [26].
Effects on LDL-ch and Non-HDL-ch Fractions
According to the outcomes of trials summarized in Table 14.2, there is not a consensus about the effects of n-3 PUFAs regarding the LDL-ch fraction. Some studies in dyslipidemic subjects with MetS features have observed that supplementation with n-3 PUFAs could rise LDL-ch concentration [26, 38, 40, 49, 54], while others have found no effect [25, 28, 42–44, 50, 56, 59]. Furthermore, the data suggest that although the overall effect of n-3 PUFAs on LDL-ch remains unclear, the supplementation could decrease the concentration of the proatherogenic sdLDL-ch promoting the formation of the highly buoyant less atherogenic LDL-ch [41, 48, 49, 55]. Moreover, Chan et al. [57] concluded that the decrease in VLDL blood concentration observed in subjects supplemented with n-3 PUFAs was produced by an increase in the conversion rate of VLDL to LDL and intermediate-density lipoprotein (IDL) and by the amelioration in the VLDL production rate. Additionally, it has been proposed that n-3 PUFAs consumption could decrease VLDL particle diameter [48, 55]. The non-HDL-ch fraction was evaluated in one study, observing that in dyslipidemic patients following their usual diet, the supplementation of n-3 PUFAs (EPA + DHA) had no effect on the non-HDL-ch [51, 57].
Effects on HDL-ch
The overall effects of n-3 PUFAs in HDL-ch fraction remain unclear. Thus, some trials have found that the supplementation promoted an increment of HDL-ch [20, 42, 51, 52], while others have observed no relevant effects [23, 25, 26, 28, 38, 40, 43, 44, 49, 50, 54–56, 59]. Additionally, some studies have suggested that there could exist differential effects of n-3 PUFAs on the different HDL-ch subfractions, promoting an increase in HDL2-ch and a decrease in HDL3-ch [49, 52]. Also, Neff et al. [48] observed that n-3 PUFAs are capable of modifying HDL particle concentrations, decreasing medium HDL while increasing large HDL without changes in small HDL (Table 14.2).
N-3 PUFAs and Blood Pressure and Endothelial Health
Regarding the effects of n-3 PUFAs on blood pressure, studies using a supplementation between 1 and 2 g/day of n-3 PUFAs at different ratios of EPA:DHA with duration between 8 and 12 weeks have not found any significant effect on blood pressure [20, 25, 40, 60]. Moreover, the fish oil supplementation between 3 and 4 g/day with different ratios of EPA:DHA has reported contradictory outcomes (see Table 14.2). Thus, the trial by Wong et al. [45] found that 16-week supplementation with n-3 PUFAs promoted a significant reduction in systolic blood pressure (SBP) without additional changes to weight loss in diastolic blood pressure (DBP). In contrast, the study by Dewell et al. [40], which lasted 8 weeks, observed that the supplementation with n-3 PUFAs decreased both and mainly DBP. Also, Skulas-Ray et al. [60] concluded that n-3 PUFAs reduced the median blood pressure, but only at the highest dose tested (3.4 g/day). However, other trials have not observed any significant effect of n-3 PUFAs on blood pressure parameters [26, 28]. Although apparently the n-3 PUFAs (EPA + DHA) have no clear effect on blood pressure in the studies reviewed, the evidence suggests that they could improve cardiovascular health by promoting a decrease in arterial stiffness [23, 46] and by recovering endothelial dysfunction [20, 23, 56, 60].
Additionally, several trials have evaluated the effects of EPA and DHA separately. The study by Nestel et al. [56], performed in hyperlipidemic subjects, found an improvement in systemic arterial compliance without changes in blood pressure and no differences between both n-3 PUFAs (~3 g/day of EPA or DHA). In contrast, the study by Mori et al. [49, 61] in hyperlipidemic men with 4 g/day of DHA observed that supplementation decreased blood pressure and induced beneficial changes in ambulatory blood pressure and heart rate, as well as in vasodilator and constrictor responses, with no effect on EPA supplementation. Additionally, Neff et al. [48], using a supplementation of algal DHA at a dose of 2 g/day, showed no effects on either systolic and diastolic ambulatory blood pressures in dyslipidemic subjects.
The effects of n-3 PUFAs on blood pressure are in accordance with the European Food Safety Authority (EFSA) report. According to the evidence, the effects of n-3 PUFAs on blood pressure have been demonstrated with a dose of >3 g/day of EPA + DHA. Moreover, the response to n-3 PUFAs treatment is conditioned to the initial levels of blood pressure [62]. The population of the trials revised for this chapter includes subjects without and with hypertension, as a characteristic of the MetS; in this sense, the different outcomes found in trials with a supplementation between 3 and 4 g/day could be affected by the proportion of hypertensive and non-hypertensive populations and by the hypertension degree. Furthermore, the effects on endothelial health could be affected also by the diet consumed during the study.
n-3 PUFAs and Inflammatory Markers
The increment in the inflammatory factors and the excessive production of oxidants in the organism during obesity and MetS have been proposed as one of the factors that could be implicated in the increment of insulin resistance and cardiovascular risk [8].
Evidence about the role of n-3 PUFAs in inflammatory markers in subjects with MetS is confusing (see Table 14.2). Some studies have observed no effect on the proinflammatory parameters measured [25, 28, 38, 40, 43, 46], while others have described that dietary supplementation with n-3 PUFAs could help to reduce the chronic inflammatory state associated with obesity by increasing anti-inflammatory molecules, such as adiponectin or interleukin (IL) 10 [28, 48], and by decreasing levels of proinflammatory markers and cytokines, such as C reactive protein or IL-6 [23, 50, 63].
Also, it has been suggested that n-3 PUFAs exert its anti-inflammatory effects at the adipose tissue level, decreasing the production of chemoattractant proteins, the infiltration of proinflammatory macrophages, and the endothelial dysfunction markers [30]. In this sense, Spencer et al. [44] showed that supplementation with EPA + DHA decreased plasma concentration and gene expression of macrophage chemoattractant protein-1 (MCP-1) and CD68, decreasing the formation of adipose tissue crown-like structures. Contrariwise, other studies have observed no effect on plasma levels of MCP-1 and other adhesion molecules as ICAM-1, VCAM-1, and E-selectin [50, 57, 63].
Although some studies suggest that n-3 PUFAs supplementation might counteract the systemic inflammatory state in obesity and MetS, the controversial outcomes of the reviewed trials make still unclear to state the efficacy and necessary dose and type of formula of n-3 PUFAs supplementation to decrease the proinflammatory response. However, some trials suggest that n-3 PUFAs supplementation may attenuate inflammation in key metabolic organs, such as adipose or muscle tissues, and perhaps the importance of n-3 PUFAs could be evident at the tissue level. Larger studies examining these issues are needed.
Conclusions and Future Perspectives
The hypotriglyceridemic benefits of n-3 PUFAs supplementation are strongly supported by most of the trials, and intakes of approximately 3 g EPA + DHA per day are able to decrease fasting TG levels by 25–35 % [64]. Based on this available evidence, the American Heart Association and the Panel on Dietetic Products, Nutrition and Allergies (NDA Panel) of the EFSA have recommended intakes of 2–4 g/day as an effective therapy for hypertriglyceridemia [65] and as an alternative to pharmacological approaches. Regarding the blood pressure-lowering properties of marine n-3 PUFAs, a recent meta-analysis of 70 randomized, controlled trials has concluded that the supplementation of ≥2 g/day of EPA + DHA may reduce both SBP and DBP, with the strongest benefits observed among hypertensive individuals who are not on antihypertensive medication [66]. Therefore, oral supplementation with n-3 PUFAs may constitute an interesting therapeutic option to reduce hypertriglyceridemia and hypertension in patients with MetS. However, the ability of n-3 PUFAs to promote weight loss, insulin sensitivity, and changes in cholesterol metabolism in patients with MetS remains controversial. Thus, further larger clinical trials are needed to better elucidate the efficacy of n-3 PUFAs on these features of MetS.
A rising interest is paid on the bioavailability and effects of different formulations of n-3 PUFAs, including re-esterified TG, ethyl ester (EE), carboxylic acids, and phospholipids (PLs) [67, 68]. In the USA and Europe, an EE n-3 PUFAs formulation containing EPA and DHA (Lovaza®/Omacor®) was approved for the treatment of severe hypertriglyceridemia. More recently, an EE formulation (Vascepa®) containing only EPA, as well as a formulation (Epanova®) containing DHA and EPA as free fatty acids, has been also approved in the USA [69]. All prescription n-3 PUFAs products effectively lower TG, but it has been suggested that carboxylic acids have greater bioavailability than EE forms since they do not require pancreatic enzyme activity for absorption [70, 71]. It should be considered that some trials suggest that products that contain DHA can raise levels of LDL-ch, which is of particular concern in patients with atherosclerosis. Krill oil is characterized by a higher amount of EPA compared to DHA (ratio of 2:1), and EPA is mainly in PL and not in TG form. It has been suggested that the delivery of EPA and DHA to tissues in the PL form is higher than that in TG form [72].
Another important issue is the evidence about the heterogeneity in response to n-3 PUFAs supplementation within population. In this context, it has been proposed that genetic background may influence this differential responsiveness [64]. For example, polymorphisms in the CD36 gene modulate the ability of fish oil supplements to lower fasting TG and raise HDL-ch [73]. There is also limited but consistent evidence that apoE and tumor necrosis factor-α (TNF-α) genotypes interact with n-3 PUFAs in outcomes relating to both inflammation and blood lipid responses [64]. The rising development of nutrigenetics will allow identifying different genotype-dependent responses to n-3 PUFAs supplementation.
There is a strong evidence that obesity-induced low-grade inflammation plays an important causative link between obesity and its associated diseases such as type 2 diabetes and atherosclerosis. In obesity, the expanding white adipose tissue makes a substantial contribution to the development of obesity-linked inflammation via increased secretion of proinflammatory cytokines, chemokines, and adipokines and the reduction of anti-inflammatory adipokines. The state of chronic low-grade inflammation is powerfully amplified through the infiltration of macrophages into adipose tissue. This dysregulated situation initiated primarily within adipose tissue can affect the function of other metabolic organs, including liver, muscle, and pancreas. Several trials in rodents and some few in humans have suggested that n-3 PUFAs are able to prevent and/or ameliorate inflammation associated with obesity and MetS by reducing adipose tissue inflammation [74]. During the last decade, Serhan and collaborators discovered that n-3 PUFAs are enzymatically converted into bioactive endogenous lipid mediators such as resolvins (Rv), protectins (PD), and maresins with powerful anti-inflammatory and proresolving properties [75]. In a study using a metabolo-lipidomics approach, Claria et al. [76] reported that human subcutaneous adipose tissue has a range of these specialized proresolving mediators including RvD1, RvD2, PD1, lipoxin (LX) A4, and the monohydroxy biosynthetic pathway markers of RvD1 and PD1 (17-HDHA), RvE1 (18-HEPE), and maresin 1 (14-HDHA). Interestingly, the levels of some of these proresolving lipid mediators such as PD1 and 17-HDHA were reduced in fat from patients with peripheral vascular disease [76]. Importantly, the study by Itariu et al. [74] showed that n-3 PUFAs supplementation to severely obese non-diabetic patients significantly increased the production of some of these proresolving lipid mediators, including RvE1, 17-HDHA, PD1, and RvD1 in visceral adipose tissue in parallel with the reduction of adipose tissue and systemic inflammation and the reduction of circulating TG. Several studies in animal models of obesity and MetS have suggested that some of these lipid mediators play a role in governing the local inflammatory tone in obese fat and that the treatments with these n-3 PUFAs-derived proresolving lipid mediators are capable of resolving the inflammation associated with obesity as well as insulin resistance and hepatic steatosis [77–81]. This is an interesting research field that deserves that these observations be further explored to determine the role of these n-3 PUFAs-derived lipid mediators in the prevention of the progression of MetS features in obese humans.
Evolution of “-omics”—transcriptomics, proteomics, metabolomics, and lipidomics—together with the advances in nutrigenomic and nutrigenetic research will greatly contribute to the deciphering of the molecular networks involved in MetS and their regulation by n-3 PUFAs. The major challenge will be in translating these outcomes into personalized recommendations.
Abbreviations
- AUC:
-
Area under curve
- CAVI:
-
Cardio-ankle vascular index
- CETP:
-
Cholesteryl ester transfer protein
- CVD:
-
Cardiovascular disease
- DHA:
-
Docosahexaenoic acid
- DBP:
-
Diastolic blood pressure
- EPA:
-
Eicosapentaenoic acid
- EE:
-
Ethyl ester
- FBI:
-
Fasting blood insulin
- FBG:
-
Fasting blood glucose
- FFA:
-
Free fatty acids
- FMD:
-
Flow-mediated dilatation
- HbA1c:
-
Glycosylated hemoglobin
- HDL:
-
High-density lipoprotein
- ICAM-1:
-
intracellular adhesion molecule 1
- IDL:
-
Intermediate-density lipoprotein
- IL:
-
Interleukin
- LDL:
-
Low-density lipoprotein
- sdLDL:
-
Small-density LDL
- PWV:
-
Pulse wave velocity
- MetS:
-
Metabolic syndrome
- n-3 PUFAs:
-
Long-chain omega-3 polyunsaturated fatty acids
- RLP:
-
Remnant lipoprotein particle
- SBP:
-
Systolic blood pressure
- TG:
-
Triglycerides
- TNF-α:
-
Tumor necrosis factor-α
- TNFR:
-
Tumor necrosis factor receptor
- TRL:
-
Triglyceride rich lipoprotein
- VCAM-1:
-
Vascular cell adhesion molecule 1
- VLDL:
-
Very-low-density lipoprotein
References
Simmons RK, Alberti KGMM, Gale EAM, Colagiuri S, Tuomilehto J, Qiao Q, et al. The metabolic syndrome: useful concept or clinical tool? Report of a WHO expert consultation. Diabetologia. 2010;53(4):600–5.
Torris C, Molin M, Cvancarova Smastuen M. Fish consumption and its possible preventive role on the development and prevalence of metabolic syndrome—a systematic review. Diabetol Metab Syndr. 2014;6(1):112.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–5.
Grundy MDP, Scott M. Hypertriglyceridemia, atherogenic dyslipidemia, and the metabolic syndrome. Am J Cardiol. 1998;81(4 Suppl 1):18B–25B.
Eckel RH, Alberti K, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010;375(9710):181–3.
Adiels M, Olofsson S, Taskinen M, Borén J. Overproduction of very low–density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28(7):1225–36.
Grundy SM. Hypertriglyceridemia, insulin resistance, and the metabolic syndrome. Am J Cardiol. 1999;83(9 Suppl 2):25–9.
Nova Science Publishers. Advances in hypertension research. New York: Ed.Ramon Rodrigo; 2014.
Payne RA, Wilkinson IB, Webb DJ. Arterial stiffness and hypertension emerging concepts. Hypertension. 2010;55(1):9–14.
Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25(5):932–43.
Stehouwer CDA, Henry RMA, Ferreira I. Arterial stiffness in diabetes and the metabolic syndrome: a pathway to cardiovascular disease. Diabetologia. 2008;51(4):527–39.
Fernandez-Garcia JC, Cardona F, Tinahones FJ. Inflammation, oxidative stress and metabolic syndrome: dietary modulation. Curr Vasc Pharmacol. 2013;11(6):906–19.
Lorente-Cebrian S, Costa AG, Navas-Carretero S, Zabala M, Martinez JA, Moreno-Aliaga MJ. Role of omega-3 fatty acids in obesity, metabolic syndrome, and cardiovascular diseases: a review of the evidence. J Physiol Biochem. 2013;69(3):633–51.
Emken EA, Adlof RO, Gulley RM. Dietary linoleic acid influences desaturation and acylation of deuterium-labeled linoleic and linolenic acids in young adult males. Biochim Biophys Acta. 1994;1213(3):277–88.
Pawlosky RJ, Hibbeln JR, Novotny JA, Salem N. Physiological compartmental analysis of alpha-linolenic acid metabolism in adult humans. J Lipid Res. 2001;42(8):1257–65.
Nigam A, Frasure-Smith N, Lespérance F, Julien P. Relationship between n-3 and n-6 plasma fatty acid levels and insulin resistance in coronary patients with and without metabolic syndrome. Nutr Metab Cardiovasc Dis. 2009;19(4):264–70.
Zaribaf F, Falahi E, Barak F, Heidari M, Keshteli AH, Yazdannik A, et al. Fish consumption is inversely associated with the metabolic syndrome. Eur J Clin Nutr. 2014;68(4):474–80.
Ebrahimi M, Ghayour-Mobarhan M, Rezaiean S, Hoseini M, Parizade SMR, Farhoudi F, et al. Omega-3 fatty acid supplements improve the cardiovascular risk profile of subjects with metabolic syndrome, including markers of inflammation and auto-immunity. Acta Cardiol. 2009;64(3):321–7.
Kabir M, Skurnik G, Naour N, Pechtner V, Meugnier E, Rome S, et al. Treatment for 2 mo with n 3 polyunsaturated fatty acids reduces adiposity and some atherogenic factors but does not improve insulin sensitivity in women with type 2 diabetes: a randomized controlled study. Am J Clin Nutr. 2007;86(6):1670–9.
Hill AM, Buckley JD, Murphy KJ, Howe PR. Combining fish-oil supplements with regular aerobic exercise improves body composition and cardiovascular disease risk factors. Am J Clin Nutr. 2007;85(5):1267–74.
Simão ANC, Lozovoy MAB, Bahls LD, Morimoto HK, Simão TNC, Matsuo T, et al. Blood pressure decrease with ingestion of a soya product (kinako) or fish oil in women with the metabolic syndrome: role of adiponectin and nitric oxide. Br J Nutr. 2012;108(8):1435–42.
Simão ANC, Lozovoy MAB, Dichi I. Effect of soy product kinako and fish oil on serum lipids and glucose metabolism in women with metabolic syndrome. Nutrition. 2014;30(1):112–5.
Tousoulis D, Plastiras A, Siasos G, Oikonomou E, Verveniotis A, Kokkou E, et al. Omega-3 PUFAs improved endothelial function and arterial stiffness with a parallel anti inflammatory effect in adults with metabolic syndrome. Atherosclerosis. 2014;232(1):10–6.
Tapsell LC, Batterham MJ, Charlton KE, Neale EP, Probst YC, O’Shea JE, et al. Foods, nutrients or whole diets: effects of targeting fish and LCn3PUFA consumption in a 12mo weight loss trial. BMC Public Health. 2013;13:1231.
Su H, Lee H, Cheng W, Huang S. A calorie-restriction diet supplemented with fish oil and high-protein powder is associated with reduced severity of metabolic syndrome in obese women. Eur J Clin Nutr. 2014;69(3):322–8.
DeFina LF, Marcoux LG, Devers SM, Cleaver JP, Willis BL. Effects of omega-3 supplementation in combination with diet and exercise on weight loss and body composition. Am J Clin Nutr. 2011;93(2):455–62.
Munro IA, Garg ML. Dietary supplementation with long chain omega-3 polyunsaturated fatty acids and weight loss in obese adults. Obes Res Clin Pract. 2013;7(3):73–81.
Krebs JD, Browning LM, McLean NK, Rothwell JL, Mishra GD, Moore CS, et al. Additive benefits of long-chain n-3 polyunsaturated fatty acids and weight-loss in the management of cardiovascular disease risk in overweight hyperinsulinaemic women. Obes Res Clin Pract. 2006;30(10):1535–44.
Munro IA, Garg ML. Dietary supplementation with n-3 PUFA does not promote weight loss when combined with a very-low-energy diet. Br J Nutr. 2012;108(8):1466–74.
Munro IA, Garg ML. Prior supplementation with long chain omega-3 polyunsaturated fatty acids promotes weight loss in obese adults: a double-blinded randomised controlled trial. Food Funct. 2013;4(4):650–8.
Thorsdottir I, Tomasson H, Gunnarsdottir I, Gisladottir E, Kiely M, Parra MD, et al. Randomized trial of weight-loss-diets for young adults varying in fish and fish oil content. Food Funct. 2007;31(10):1560–6.
Kunesova M, Braunerova R, Hlavaty P, Tvrzicka E, Stankova B, Skrha J, et al. The influence of n-3 polyunsaturated fatty acids and very low calorie diet during a short-term weight reducing regimen on weight loss and serum fatty acid composition in severely obese women. Physiol Res. 2006;55(1):63–72.
Vasickova L, Stavek P, Suchanek P. Possible effect of DHA intake on body weight reduction and lipid metabolism in obese children. Neuro Endocrinol Lett. 2011;32(Suppl 2):64–7.
Itoh M, Suganami T, Satoh N, Tanimoto-Koyama K, Yuan X, Tanaka M, et al. Increased adiponectin secretion by highly purified eicosapentaenoic acid in rodent models of obesity and human obese subjects. Arterioscler Thromb Vasc Biol. 2007;27(9):1918–25.
Yamada H, Yoshida M, Nakano Y, Suganami T, Satoh N, Mita T, et al. In vivo and in vitro inhibition of monocyte adhesion to endothelial cells and endothelial adhesion molecules by eicosapentaenoic acid. Arterioscler Thromb Vasc Biol. 2008;28(12):2173–9.
Huerta AE, Navas-Carretero S, Prieto-Hontoria PL, Martínez JA, Moreno-Aliaga MJ. Effects of alpha-lipoic acid and eicosapentaenoic acid in overweight and obese women during weigh loss. Obesity. 2014;23(2):313–21.
Flachs P, Rossmeisl M, Kopecky J. The effect of n-3 fatty acids on glucose homeostasis and insulin sensitivity. Physiol Res. 2014;63(Suppl 1):93–118.
Bragt MCE, Mensink RP. Comparison of the effects of n-3 long chain polyunsaturated fatty acids and fenofibrate on markers of inflammation and vascular function, and on the serum lipoprotein profile in overweight and obese subjects. Nutr Metab Cardiovasc Dis. 2012;22(11):966–73.
Chan DC, Nguyen MN, Watts GF, Ooi EM, Barrett PH. Effects of atorvastatin and n-3 fatty acid supplementation on VLDL apolipoprotein C-III kinetics in men with abdominal obesity. Am J Clin Nutr. 2010;91(4):900–6.
Dewell A, Marvasti FF, Harris WS, Tsao P, Gardner CD. Low- and high-dose plant and marine (n-3) fatty acids do not affect plasma inflammatory markers in adults with metabolic syndrome. J Nutr. 2011;141(12):2166–71.
Kelley DS, Adkins Y, Woodhouse LR, Swislocki A, Mackey BE, Siegel D. Docosahexaenoic acid supplementation improved lipocentric but not glucocentric markers of insulin sensitivity in hypertriglyceridemic men. Metab Syndr Relat Disord. 2012;10(1):32–8.
Lovegrove JA, Lovegrove SS, Lesauvage SV, Brady LM, Saini N, Minihane AM, et al. Moderate fish-oil supplementation reverses low-platelet, long-chain n-3 polyunsaturated fatty acid status and reduces plasma triacylglycerol concentrations in British Indo-Asians. Am J Clin Nutr. 2004;79(6):974–82.
Skulas-Ray AC, Kris-Etherton PM, Harris WS, Heuvel JPV, Wagner PR, West SG. Dose-response effects of omega-3 fatty acids on triglycerides, inflammation, and endothelial function in healthy persons with moderate hypertriglyceridemia. Am J Clin Nutr. 2011;93(2):243–52.
Spencer M, Finlin BS, Unal R, Zhu B, Morris AJ, Shipp LR, et al. Omega-3 fatty acids reduce adipose tissue macrophages in human subjects with insulin resistance. Diabetes. 2013;62(5):1709–17.
Wong ATY, Chan DC, Barrett PHR, Adams LA, Watts GF. Effect of ω-3 Fatty acid ethyl esters on apolipoprotein b-48 kinetics in obese subjects on a weight-loss diet: a new tracer kinetic study in the postprandial state. J Clin Endocrinol Metab. 2014;99(8):E1427–35.
Wong AT, Chan DC, Barrett PH, Adams LA, Watts GF. Supplementation with n3 fatty acid ethyl esters increases large and small artery elasticity in obese adults on a weight loss diet. J Nutr. 2013;143(4):437–41.
Ramel A, Martinez A, Kiely M, Morais G, Bandarra NM, Thorsdottir I. Beneficial effects of long-chain n-3 fatty acids included in an energy-restricted diet on insulin resistance in overweight and obese European young adults. Diabetologia. 2008;51(7):1261–8.
Neff LM, Culiner J, Cunningham-Rundles S, Seidman C, Meehan D, Maturi J, et al. Algal docosahexaenoic acid affects plasma lipoprotein particle size distribution in overweight and obese adults. J Nutr. 2011;141(2):207–13.
Mori TA, Watts GF, Burke V, Hilme E, Puddey IB, Beilin LJ. Differential effects of eicosapentaenoic acid and docosahexaenoic acid on vascular reactivity of the forearm microcirculation in hyperlipidemic, overweight men. Circulation. 2000;102(11):1264–9.
Browning LM, Krebs JD, Moore CS, Mishra GD, O’Connell MA, Jebb SA. The impact of long chain n-3 polyunsaturated fatty acid supplementation on inflammation, insulin sensitivity and CVD risk in a group of overweight women with an inflammatory phenotype. Diabetes Obes Metab. 2007;9(1):70–80.
Chan DC, Watts GF, Mori TA, Barrett PHR, Beilin LJ, Redgrave TG. Factorial study of the effects of atorvastatin and fish oil on dyslipidemia in visceral obesity. Eur J Clin Invest. 2002;32(6):429–36.
Chan DC, Watts GF, Nguyen MN, Barrett PHR. Factorial study of the effect of n–3 fatty acid supplementation and atorvastatin on the kinetics of HDL apolipoproteins A-I and A-II in men with abdominal obesity. Am J Clin Nutr. 2006;84(1):37–43.
Chan DC, Watts GF, Mori TA, Barrett PHR, Redgrave TG, Beilin LJ. Randomized controlled trial of the effect of n–3 fatty acid supplementation on the metabolism of apolipoprotein B-100 and chylomicron remnants in men with visceral obesity. Am J Clin Nutr. 2003;77(2):300–7.
Davidson MH, Maki KC, Kalkowski J, Schaefer EJ, Torri SA, Drennan KB. Effects of docosahexaenoic acid on serum lipoproteins in patients with combined hyperlipidemia: a randomized, double-blind, placebo-controlled trial. J Am Coll Nutr. 1997;16(3):236–43.
Kelley DS, Siegel D, Vemuri M, Mackey BE. Docosahexaenoic acid supplementation improves fasting and postprandial lipid profiles in hypertriglyceridemic men. Am J Clin Nutr. 2007;86(2):324–33.
Nestel P, Shige H, Pomeroy S, Cehun M, Abbey M, Raederstorff D. The n−3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr. 2002;76(2):326–30.
Chan DC, Watts GF, Barrett PHR, Beilin LJ, Redgrave TG, Mori TA. Regulatory effects of HMG CoA reductase inhibitor and fish oils on apolipoprotein B-100 kinetics in insulin-resistant obese male subjects with dyslipidemia. Diabetes. 2002;51(8):2377–86.
Kelley DS, Siegel D, Vemuri M, Chung GH, Mackey BE. Docosahexaenoic acid supplementation decreases remnant-like particle-cholesterol and increases the (n-3) index in hypertriglyceridemic men. J Nutr. 2008;138(1):30–5.
Bitzur R, Cohen H, Cohen T, Dror TW, Herzog Y, Lifshitz Y, et al. The metabolic effects of omega-3 plant sterol esters in mixed hyperlipidemic subjects. Cardiovasc Drugs Ther. 2010;24(5–6):429–37.
Skulas-Ray AC, Kris-Etherton PM, Harris WS, West SG. Effects of marine-derived omega-3 fatty acids on systemic hemodynamics at rest and during stress: a dose–response study. Ann Behav Med. 2012;44(3):301–8.
Mori TA, Bao DQ, Burke V, Puddey IB, Beilin LJ. Docosahexaenoic acid but not eicosapentaenoic acid lowers ambulatory blood pressure and heart rate in humans. Hypertension. 1999;34(2):253–60.
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on the substantiation of health claims related to EPA, DHA, DPA and maintenance of normal blood pressure (ID 502), maintenance of normal HDL-cholesterol concentrations (ID 515), maintenance of normal (fasting) blood concentrations of triglycerides (ID 517), maintenance of normal LDL-cholesterol concentrations (ID 528, 698) and maintenance of joints (ID 503, 505, 507, 511, 518, 524, 526, 535, 537) pursuant to Article 13(1) of Regulation (EC) No 1924/2006 on request from the European Commission. EFSA J 2009;7(9):1263[26-pp].
Kelley DS, Siegel D, Fedor DM, Adkins Y, Mackey BE. DHA supplementation decreases serum C-reactive protein and other markers of inflammation in hypertriglyceridemic men. J Nutr. 2009;139(3):495–501.
Madden J, Williams CM, Calder PC, Lietz G, Miles EA, Cordell H, et al. The impact of common gene variants on the response of biomarkers of cardiovascular disease (CVD) risk to increased fish oil fatty acids intakes. Annu Rev Nutr. 2011;31:203–34.
Kris-Etherton PM, Harris WS, Appel LJ, AHA Nutrition Committee, American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151–2.
Miller PE, Van Elswyk M, Alexander DD. Long-chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and blood pressure: a meta-analysis of randomized controlled trials. Am J Hypertens. 2014;27(7):885–96.
Dyerberg J, Madsen P, Moller JM, Aardestrup I, Schmidt EB. Bioavailability of marine n-3 fatty acid formulations. Prostaglandins Leukot Essent Fatty Acids. 2010;83(3):137–41.
Weintraub H. Update on marine omega-3 fatty acids: management of dyslipidemia and current omega-3 treatment options. Atherosclerosis. 2013;230(2):381–9.
Hedengran A, Szecsi PB, Dyerberg J, Harris WS, Stender S. n-3 PUFA esterified to glycerol or as ethyl esters reduce non-fasting plasma triacylglycerol in subjects with hypertriglyceridemia: a randomized trial. Lipids. 2014;50(2):165–75.
Blair HA, Dhillon S. Omega-3 carboxylic acids (Epanova): a review of its use in patients with severe hypertriglyceridemia. Am J Cardiovasc Drugs. 2014;14(5):393–400.
Roth EM. Omega-3 carboxylic acids for hypertriglyceridemia. Expert Opin Pharmacother. 2015;16(1):123–33.
Berge K, Musa-Veloso K, Harwood M, Hoem N, Burri L. Krill oil supplementation lowers serum triglycerides without increasing low-density lipoprotein cholesterol in adults with borderline high or high triglyceride levels. Nutr Res. 2014;34(2):126–33.
Madden J, Carrero JJ, Brunner A, Dastur N, Shearman CP, Calder PC, et al. Polymorphisms in the CD36 gene modulate the ability of fish oil supplements to lower fasting plasma triacyl glycerol and raise HDL cholesterol concentrations in healthy middle-aged men. Prostaglandins Leukot Essent Fatty Acids. 2008;78(6):327–35.
Itariu BK, Zeyda M, Hochbrugger EE, Neuhofer A, Prager G, Schindler K, et al. Long-chain n-3 PUFAs reduce adipose tissue and systemic inflammation in severely obese nondiabetic patients: a randomized controlled trial. Am J Clin Nutr. 2012;96(5):1137–49.
Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014;510(7503):92–101.
Claria J, Nguyen BT, Madenci AL, Ozaki CK, Serhan CN. Diversity of lipid mediators in human adipose tissue depots. Am J Physiol Cell Physiol. 2013;304(12):C1141–9.
Gonzalez-Periz A, Horrillo R, Ferre N, Gronert K, Dong B, Moran-Salvador E, et al. Obesity-induced insulin resistance and hepatic steatosis are alleviated by omega-3 fatty acids: a role for resolvins and protectins. FASEB J. 2009;23(6):1946–57.
Hellmann J, Tang Y, Kosuri M, Bhatnagar A, Spite M. Resolvin D1 decreases adipose tissue macrophage accumulation and improves insulin sensitivity in obese-diabetic mice. FASEB J. 2011;25(7):2399–407.
Titos E, Rius B, Gonzalez-Periz A, Lopez-Vicario C, Moran-Salvador E, Martinez-Clemente M, et al. Resolvin D1 and its precursor docosahexaenoic acid promote resolution of adipose tissue inflammation by eliciting macrophage polarization toward an M2-like phenotype. J Immunol. 2011;187(10):5408–18.
Claria J, Dalli J, Yacoubian S, Gao F, Serhan CN. Resolvin D1 and resolvin D2 govern local inflammatory tone in obese fat. J Immunol. 2012;189(5):2597–605.
Spite M, Claria J, Serhan CN. Resolvins, specialized proresolving lipid mediators, and their potential roles in metabolic diseases. Cell Metab. 2014;19(1):21–36.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Huerta, A.E., Laiglesia, L.M., Martínez-Fernández, L., Moreno-Aliaga, M.J. (2016). Role of Omega-3 Fatty Acids in Metabolic Syndrome. In: Hegde, M., Zanwar, A., Adekar, S. (eds) Omega-3 Fatty Acids. Springer, Cham. https://doi.org/10.1007/978-3-319-40458-5_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-40458-5_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40456-1
Online ISBN: 978-3-319-40458-5
eBook Packages: MedicineMedicine (R0)