Abstract
Enhancement of vascular remodeling in affected brain tissue is a novel therapy for acute ischemic stroke (AIS). However, conclusions regarding angiogenesis after AIS remain ambiguous. Vascular endothelial growth factor A (VEGFA) and VEGF receptor 2 (VEGFR2) are potent regulators of angiogenesis and vascular permeability. We aimed to investigate the association between VEGFA/VEGFR2 expression in the acute stage of stroke and prognosis of patients with AIS. We enrolled 120 patients with AIS within 24 h of stroke onset and 26 healthy controls. Plasma levels of VEGFA and VEGFR2 were measured by enzyme-linked immunosorbent assay (ELISA). The primary endpoint was an unfavorable outcome defined as a modified Rankin Scale (mRS) score > 2 at 3 months after AIS. Univariate and multivariate logistic regression analyses were used to identify risk factors affecting prognosis. Plasma VEGFA and VEGFR2 were significantly higher in patients with AIS than in health controls, and also significantly higher in patients with unfavorable than those with favorable outcomes. Moreover, both VEGFA and VEGFR2 showed a significantly positive correlation with mRS at 3 months. Univariate and multivariate analyses showed VEGFA and VEGFR2 remained associated with unfavorable outcomes, and adding VEGFA and VEGFR2 to the clinical model significantly improved risk reclassification (continuous net reclassification improvement, 105.71%; integrated discrimination improvement, 23.45%). The new risk model curve exhibited a good fit with an area under the receiver operating characteristic curve (ROC) curve of 0.9166 (0.8658–0.9674). Plasma VEGFA and VEGFR2 are potential markers for predicting prognosis; thus these two plasma biomarkers may improve risk stratification in patients with AIS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a leading cause of physical disability and a major disease burden worldwide, with limited therapies available. Identifying effective biomarkers to improve the prognosis and treatment of stroke is a major challenge. Vascular endothelial growth factor (VEGFA) and its receptor, VEGF receptor 2 (VEGFR2) are potent angiogenic factors that regulate vascular endothelial migration and permeability [1].Angiogenesis is a natural defense mechanism that restores the oxygen and nutrients supplied to the peri-infarct brain tissue after ischemic stroke [2]. However, increasing evidence has shown that new vessels formed in peri-infarct areas have higher permeability than normal after stroke [3]. Therefore, the association between VEGFA/VEGFR2 levels and acute ischemic stroke (AIS) requires further investigation.
Neuroprotective treatment of ischemic stroke has mainly focused on reducing cerebral infarction volume without considering brain edema [4]. Brain edema leads to blood brain barrier (BBB) leakage, hemorrhagic transformation, inflammation and increased mortality during the acute phase of ischemic stroke [5]. Brain edema is typically followed by vasogenic edema, which increases vascular permeability and angiogenesis [6]. The interaction between VEGFA and VEGFR2 has been implicated in vasogenic brain edema [7]. These mechanisms include the trans-endothelial transport of small solutes via cytoplasmic fenestrations and plasmalemmal caveolae, leakage of fluid and plasma proteins, and extravasation of blood cells through inter-endothelial tight junctions [8]. Tyrosine kinase inhibitor targeting VEGFR which blocks VEGF/VEGFR signaling, have been shown to be effective therapies for patients with intractable vasogenic brain edema [9]. Furthermore, preclinical studies have indicated that increased brain edema is linked to VEGFA/VEGFR2 signaling in the presence of comorbid conditions [4, 10]. Ergul et al. has also demonstrated that excessive angiogenesis in patients with diabetes after AIS is associated with poor prognosis and is related to the interaction between VEGFA and VEGFR2 [11].
The BBB is instrumental in establishing and maintaining microenvironmental homeostasis in the central nervous system (CNS) [12]. Preserving the BBB integrity is beneficial for preventing neuronal apoptosis and further brain injury after AIS [13]. A preclinical study indicated that new vessels in peri-infarct areas have high BBB permeability after stroke because of a lack of tight junction proteins (TJP), including claudin-5, occludin and zonula-occludens-1 (ZO-1) [3]. Several studies have shown that decreased TJP levels are associated with increased expression of VEGFA and VEGFR2 [14,15,16]. The inhibition of VEGFA and VEGFR2 expression restores occludin and ZO-1 expression after neuronal protective treatment [13]. Downregulation of VEGFA can protect the BBB, and claudin-5 and occludin may be the main target of VEGFA [17]. Moreover, activation of the matrix metalloproteinase expression is correlated with the disruption of the interaction between VEGFA and VEGFR2, which leads to the degradation of claudin-5, occludin and ZO-1 [18].
Multiple clinical studies have confirmed that circulating VEGF levels increase after ischemic stroke, but the prognostic value of VEGF for ischemic stroke has varied between studies. Two studies have shown that VEGF is associated with a favorable outcome at 1 month after stroke [19] and 3–12 months after stroke [20] respectively. However, one study showed that elevated levels of combined circulating C-reactive protein and VEGF were associated with unfavorable outcomes 2 years after stroke[21]. In addition, another study showed that elevated blood VEGF levels were associated with moderate to severe disability 6 months after stroke [22]. The difference in these conclusions might be due to the dual role of VEGF in ischemic stroke [23, 24], in which VEGFA plays a critical role. In addition, the complexity of the VEGF family may also contribute to the difference of the conclusions. Furthermore, few studies have conducted to clarify the association between the members of the VEGF family or their receptors and stroke outcomes to date. Therefore, the prognostic value of VEGF on stroke remains unclear. VEGFA and its receptor VEGFR2 are potent factors in regulating angiogenesis and vascular permeability. It has been reported that circulating VEGFR2 and VEGFA levels are elevated in patients with ischemic stroke [25]. However, the association between blood VEGFA/VEGFR2 levels and ischemic stroke outcomes has not yet been investigated. Therefore, we conducted this study to explore the clinical significance of the plasma levels of VEGFA and VEGFR2 in patients in the acute phage of AIS to provide new insights into the risk stratification and treatment of these patients.
Methods
Study Participants
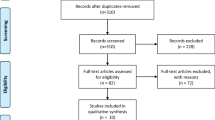
This cohort study recruited 210 patients who underwent thrombolytic evaluation at the Department of Emergency at Xuanwu Hospital of Capital Medical University between September and November 2022. The inclusion criteria were as follows: (1) diagnosis of AIS confirmed by brain magnetic resonance imaging (MRI) or computed tomography (CT); (2) clear neurological deficits; (3) age ≥ 18 years; (4) presentation within 24 h after symptoms onset; (5) complete case and follow-up data; and (6) willingness to participate and provide informed consent. The exclusion criteria were as follows: (1) cerebral hemorrhage diagnosed by CT or MRI; (2) transient ischemic attack; (3) cancer; (4) blood disease; (5) severe infection; (6) epilepsy; (7) livers/kidney dysfunction; and (8) immune diseases. Finally, the study included 120 patients with AIS (Fig. 1). A total of 26 age and sex-matched healthy participants were included in the control group. This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University. The experiment was conducted with the understanding and written consent of all patients or their immediate family members.
Collection of Clinical Data and Blood Samples
The baseline variables included demographic characteristics, risk factors, stroke characteristics and treatment, stroke classification, and general evaluation on admission collected from clinical interviews and neurological examinations by board-certified neurologists. Stroke severity was assessed using the National Institutes of Health Stroke Score (NIHSS) on admission in all enrolled patients. Clinical outcomes were evaluated using the modified Rankin Score (mRS) by trained neurologists via telephone interviews 3 months after stroke. We defined a favorable outcome as an mRS score of 0–2, and an unfavorable outcome as an mRS score of 3–6.
Plasma Levels of VEGFA and VEGFR2
Blood samples were collected in EDTA tubes from patients with AIS and the healthy controls before treatment. The blood samples of patients were collected within 24 h after the AIS onset. The separated plasma was stored at -80 ℃. Plasma levels of VEGFA and VEGFR2 were detected using Human VEGFA ELISA kits (F9809-A; FANKEW) and Human VEGFR2 ELISA kits (F0109-A; FANKEW), respectively. All samples were tested by board-certified laboratory technicians blinded to the clinical data according to the manufacturer’s protocols.
Statistical Analysis
GraphPad Prism 9.4.0 (GraphPad Software, La Jolla, CA, United States) and R software (version 4.3.0) were used for statistical analyses. A p value < 0.05 was considered of statistical significance. The Kolmogorov–Smirnov test was used to assess normal distribution of data. Continuous variables conforming to a normal distribution are reported as the mean ± standard deviation. Variables not conforming to a normal distribution are represented as the median with 25th and 75th percentiles (Q1-Q3). Comparison between two groups was tested using the unpaired t test or Mann–Whitney test. Comparison between multiple groups was performed using analysis of variance on ranks. Correlations were analyzed using Spearman’s rank correlation coefficient. The chi-squared tests were used to compare the categorical variables and are reported as frequency (%).
Univariate and multivariate logistic regression analyses were used to analyze the relationship between VEGFA and VEGFR2 and functional outcomes in patients with AIS after 3 months. The predictive values of plasma VEGFA and VEGFR2 for stroke outcomes were evaluated using the receiver operating characteristic (ROC) curves. VEGFA and VEGFR2 were cut off into dichotomous variables using the Youden index [26]. We, then assessed the association of dichotomous VEGFA and VEGFR2 expression with stroke outcomes using multivariate logistic regression analysis. Least absolute shrinkage and selection operator (LASSO) regression using a penalized regression approach was used to screen variables based on lambda. min and lambda.1se [27]. A risk prediction-model was established by integrating variables with non-zero coefficients. A nomogram was constructed based on the risk-prediction model. The area under ROC curve (AUC) was used to evaluate the discriminative ability and accuracy of the risk model. A calibration diagram was used to evaluate the fitting performance. The net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were calculated to quantify the improvement in correct reclassification and discrimination in the risk-prediction model. The clinical value of the risk model was evaluated using the decision curve analysis (DCA).
Results
Patient Characteristics and Clinical Variables
The baseline clinical characteristics of the 120 patients with AIS are listed in Table 1. The median age was 67.50 (58.25–75.75) years, and 73 of the patients (60.83%) were male. The median NIHSS score was 8.0 (3.0–15.0) on admission, median time from stroke onset to treatment was 2.675 (1.385–4.160) hours, and 67 of the patients (55.83%) presented with large-artery atherosclerosis stroke. Among the 120 patients, 69 (57.5%) presented with favorable outcomes and 51 (42.5%) presented with unfavorable outcomes. Atrial fibrillation, higher NIHSS scores on admission, higher mRS scores on admission, recombinant tissue plasminogen activator treatment, higher plasma VEGFA levels and higher plasma VEGFR2 levels were more common in patients with unfavorable outcomes than in those with favorable outcomes (Table 1).
Elevated Plasma VEGFA and VEGFR2 Levels Were Correlated With Unfavorable Outcome in AIS
Plasma VEGFA and VEGFR2 levels were significantly higher in patients with AIS than in healthy controls (VEGFA, p = 0.023; VEGFR2, p < 0.001; Fig. 2A, 2D). A subgroup analysis of patients with AIS based on mRS score at 3 months revealed that plasma VEGFA and VEGFR2 levels were significantly higher in patients with unfavorable outcome (mRS > 2) than those with favorable outcome (mRS ≤ 2) (VEGFA, p < 0.0001; VEGFR2, p < 0.0001; Fig. 2B, 2E, Table 1) or healthy controls (VEGFA, p < 0.001; VEGFR2, p < 0.0001; Fig. 2B, 2E). Furthermore, correlation analysis showed that both VEGFA and VEGFR2 levels were significantly positively correlated with mRS scores at 3 months after AIS (VEGFA, r2 = 0.097, p < 0.001; VEGFR2, r2 = 0.086, p < 0.01; Fig. 2C, 2F). In addition, plasma VEGFR2 levels were significantly higher in AIS patients with diabetes than in those without diabetes (p = 0.048, Fig. 3A), and were significantly positively correlated with blood glucose levels (r2 = 0.053, p = 0.012, Fig. 3B), which are risk factors and treatment target associated with ischemic stroke. However, plasma VEGFA levels in AIS patients with and without diabetes showed no significant difference (p = 0.443, Fig. 3C), and there was not a prominent positive correlation with blood glucose levels (r2 = 0.022, p = 0.105, Fig. 3D).
Plasma levels of VEGFR2 and VEGFA in patients with AIS and healthy controls and their correlation with mRS at 3 months. Plasma levels of VEGFR2 in patients with AIS and healthy controls (A). Plasma levels of VEGFR2 in patients with favorable outcomes (mRS ≤ 2) and unfavorable outcomes (mRS > 2) (B). Correlation of plasma levels of VEGFR2 with mRS at 3 months (C). Plasma levels of VEGFA in patients with AIS and healthy controls (D). Plasma levels of VEGFA in patients with favorable outcomes (mRS ≤ 2) and unfavorable outcomes (mRS > 2) (E). Correlation of plasma levels of VEGFA with mRS at 3 months (F). Patients with AIS, n = 120 (favorable outcome, n = 69; unfavorable outcome, n = 51); healthy controls, n = 26. ****p < 0.0001, ***p < 0.001, *p < 0.05. AIS, acute ischemic stroke; VEGFR2, vascular endothelial growth factor receptor 2; VEGFA, vascular endothelial growth factor A; mRS, modified Rankin scale
Plasma levels of VEGFR2 and VEGFA in AIS patients with or without diabetes and their correlation with blood glucose. Plasma levels of VEGFR2 in AIS patients with or without diabetes (A). Correlation of plasma levels of VEGFR2 with blood glucose in patients with AIS. (B).Plasma levels of VEGFA in AIS patients with or without diabetes (C). Correlation of plasma levels of VEGFA with blood glucose in patients with AIS. (D). Patients with AIS, n = 120 (with diabetes, n = 41; without diabetes, n = 79); *p < 0.05. AIS, acute ischemic stroke; VEGFR2, vascular endothelial growth factor receptor 2; VEGFA, vascular endothelial growth factor A
Variable Selection Based on LASSO Regression
Twenty-seven variables were selected as candidate risk-prediction factors. We found NIHSS score on admission, diabetes, platelet, and higher VEGFR2 level were associated with unfavorable outcomes in multivariate logistic regression after adjusting all potential confounding factors (Fig. 4A). The LASSO regression yielded five variables based on lambda.1se that were most concise and strongly correlated with unfavorable outcomes in AIS, including the mRS score on admission, NIHSS score on admission, atrial fibrillation, VEGFA, and VEGFR2. The predictive model was established by adding the variables and relative coefficient of each variable in the LASSO regression as follows: risk score = 0.028156526 * amRS + 0.060542902 * aNIHSS + 0.189654221 * AF + 0.001254513 * VEGFR2 + 0.001477991 * VEGFA. Models with different variable configurations were tested and fitted using fivefold cross validation. The λ value was used to determine the number of variables, and when λ = lambda. min, 23 variables were screened; and when λ = lambda.1se, five variables were selected. The model with the best performance and fewest independent variables corresponded to the λ of lambda.1se (Fig. 4B, 4C).
Characteristic variables screened by LASSO regression and forest map of variables influencing mRS at 3 months determined using logistic regression. Forest map of variables influencing mRS at 3 months after adjusting potential confounding factors (A). The number of characteristic variables screened based on LASSO regression. When λ = lambda.1se, five variables are selected (B). The change trajectory of variable coefficients (C). Forest map of variables influencing mRS at 3 months based on LASSO regression model (D). (Note: mRS > 2 at 3 months is the dependent variable. The independent variables include mRS score at admission, NIHSS score at admission, atrial fibrillation, VEGFR2 and VEGFA (screened using LASSO regression). mRS, modified Rankin scale; NIHSS, national institutes health stroke scale; LASSO, least absolute shrinkage and selection operator; amRS, mRS score on admission; aNIHSS, NIHSS score on admission; AF, atrial fibrillation; PLT, platelet
Plasma VEGFA and VEGFR2 Represented Independent Predictors for Unfavorable Outcomes in AIS
We examined the predictive value of plasma VEGFA and VEGFR2 levels for unfavorable outcomes and found that high plasma level were associated with an increased risk of unfavorable outcomes in the univariate analysis (VEGFA, odds ratio (OR) = 1.015 (1.005–1.026), p = 0.005; VEGFR2, OR = 1.005 (1.002–1.008), p < 0.01; Table 2).
After adjusting for mRS score on admission, NIHSS score on admission, and atrial fibrillation in multivariate logistic regression, VEGFA and VEGFR2 levels remained prominent for the prediction of unfavorable outcomes in AIS (VEGFA, OR = 1.020 (1.007–1.036), p = 0.006; VEGFR2, OR = 1.005 (1.002–1.010), p = 0.006; Table 2). A cutoff point for VEGFA of 208.9 pg/ml had 55.00% sensitivity and 76.92% specificity (Youden index = 0.346) for the prediction value of unfavorable outcome at 3 months, and a cut off point for VEGFR2 of 694.9 pg/ml had 72.50% sensitivity and 65.38% specificity (Youden index = 0.379) for the prediction value of unfavorable outcome at 3 months. Plasma VEGFA and VEGFR2 levels were dichotomized using these cut-off points. Logistic regression analysis was conducted and showed that plasma VEGFA > 208.9 pg/ml (OR = 6.123 (2.031–20.850), p = 0.002) and VEGFR2 > 694.9 pg/ml (OR = 39.750 (5.856–637.300), p = 0.02) were associated with increasing risk of unfavorable outcome at 3 months in AIS (Table 2).
Based on the five variables screened using LASSO regression, an additional logistic regression analysis was performed. The analysis showed that NIHSS score on admission, atrial fibrillation, and higher plasma VEGFA and VEGFR2 levels were associated with an unfavorable outcome. The results are presented in a forest map (p < 0.05, Fig. 4D).
Enhancive Prediction Value of Plasma VEGFA and VEGFR2 Levels in AIS
We investigated whether the addition of VEGFA and VEGFR2 to the clinical model improved its predictive power. Logistic regression confirmed that VEGFA > 208.9 pg/ml (OR = 6.123 (2.031–20.850), p = 0.002) and VEGFR2 > 694.9 pg/ml (OR = 39.750 (5.856–637.300), p = 0.002) were predictors of poor outcome at 3 months, together with mRS score on admission (OR = 0.937 (0.590–1.054), p = 0.780), NIHSS score on admission (OR = 1.211 (1.103–1.357), p < 0.001) and atrial fibrillation (OR = 7.644 (1.477–56.980), p = 0.026) (Table 3). The incremental benefits of plasma VEGFA and VEGFR2 levels were investigated by calculating the AUC, and IDI and NRI indexes. The results indicated that the addition of plasma VEGFA and VEGFR2 into the clinical model significantly improved the AUC from 81.36% to 91.66% (p < 0.0001). Furthermore, the addition of VEGFA and VEGFR2 to the clinical model also improved the integrated discriminatory ability of the new risk-prediction model (total IDI% = 23.450% (16.100–30.810%), p < 0.0001) and net classification (categorical NRI = 28.820% (6.020–51.610%), p = 0.013; continuous NRI = 105.710% (75.390–136.030%), p < 0.0001; Table 3). In addition, the R2 (Cox & Snell) in the new risk-prediction model (R2 (Cox & Snell) = 0.465) was greater than that in the clinical model (R2 (Cox & Snell) = 0.276), and the Akaike information criterion (AIC) in the new risk-prediction model (AIC = 101.2) was smaller than that in the clinical model (AIC = 167.5). These results indicate that the new risk-prediction model has a greater goodness of fit.
Prognostic Nomogram and Clinical Application
The risk-prediction model was converted into a nomogram to intuitively predict unfavorable outcomes (Fig. 5A). The predictive values of the nomogram were in good agreement with the actual values, indicating that the risk-prediction model had a better fit (Fig. 5B). The AUC of the nomogram was 0.917 (0.866–0.967) with 84.3% sensitivity and 82.6% specificity, indicating that the new risk-prediction model had good discriminative ability and accuracy (Fig. 5C). The DCA integrate patient or decision-makers preferences into the analysis and quantifies the net benefit of different threshold probabilities in a dataset to evaluate the clinical value of the nomogram. The results indicated that the new risk-prediction model exhibited a greater ability to predict unfavorable outcomes in patients with AIS (Fig. 5D). These results suggest that the new risk-prediction model has great clinical value.
Nomogram based on the risk model for predicting prognosis and evaluation of the risk model. Nomogram for predict the poor prognosis probability in patients with AIS at 3 months (A). Calibration curve of the relationship between predicted and actual probabilities of the poor prognosis. The solid line represents the ideal predictive model, and the dotted line represents the observed model (B). ROC curve was used to evaluate the accuracy of the nomogram. The red solid line represents the risk model including amRS, aNIHSS, AF, VEGFR2 and VEGFA (C). DCA curves evaluate nomogram from the perspective of clinical benefit and scope of clinical benefits. The y-axis represents the net benefit. The x-axis represents the predicted poor prognosis probability. The gray solid line represents the condition that all patients were classified as high risk and the intervention had been implemented ahead of time, while the black solid line represents the condition that none of the patients were classified as high risk, did not intervene in advance, and had a net benefit of 0. The red solid line represents the risk model including amRS, aNIHSS, AF, VEGFR2 and VEGFA (D). ROC, receiver operating characteristic; DCA, decision curve analysis. mRS, modified Rankin scale; NIHSS, national institutes health stroke scale; amRS, modified Rankin scale on admission; aNIHSS, national institutes of health stroke scale on admission; AF, atrial fibrillation; AIS, acute ischemic stroke; VEGFR2, vascular endothelial growth factor receptor 2; VEGFA, vascular endothelial growth factor A
Discussion
In the present study, we demonstrated that plasma VEGFA and VEGFR2 levels were associated with unfavorable outcomes at 3 months after AIS. Patients with higher plasma VEGFA and VEGFR2 levels were more likely to have poor outcomes, and plasma VEGFA and VEGFR2 levels positively correlated with the mRS score at 3 months. Furthermore, the addition of plasma VEGFA and VEGFR2 levels to the clinical model significantly improved risk stratification for unfavorable outcomes. For the first time, we founded that plasma VEGFA and VEGFR2 levels in the acute phase of stroke might be predictors for the prognosis of AIS.
Multiple studies have demonstrated that blood VEGF levels are associated with outcomes in patients with AIS [28,29,30,31]. VEGF is one of the most commonly studied growth factors in ischemic stroke; however, these conclusions are inconsistent with those of other experimental studies [22, 25, 32]. The reasons for the differences in these conclusions may be as follows: 1) differences in the time points to collect blood samples. Previous studies have demonstrated upregulation of endogenous VEGF levels and the use of exogenous VEGF are harmful after acute ischemic stroke [24]. However, the deleterious effects of VEGF on vascular integrity are transient, and both VEGF preconditioning [33] and VEGF treatment after the acute phase [34] have neuroprotective effects. Therefore, the effects of VEGF on AIS are associated with the time points of its expression. 2) limitations in data analysis or sample size, for example, potential clinical confounders associated with AIS were not adjusted in regression analyze. 3) the complexity of VEGF family. There are many uncertainties and contradictions about the role of VEGF family in current research of ischemic stroke. Furthermore, the VEGF receptors and co-receptors have different properties and activate different intracellular signaling pathways [23]. The VEGF family contain several members, including VEGFA, VEGFB, VEGFC, VEGFD and PIGF, which play their roles by combining with three specific receptors, VEGFR1, VEGFR2, and VEGFR3. Several studies have reported that the mRNA and protein expressions of VEGFA, VEGFB and VEGFD are elevated following BBB breakdown in a rat model of cold injury [35, 36]. However, their expression shows temporal and spatial differences during BBB injury and angiogenesis, indicating that they have specific and separate roles in these processes [36]. VEGFB, as a new member of VEGF family, less is known about it. VEGFB binds to its receptor VEGFR1 to exert vascular and neuroprotection effects against a wide arrange of apoptotic stimuli [37,38,39,40]. However, the exact function of VEGFB is still controversial [41]. Another member of the VEGF family, VEGFC, is a secreted glycoproteins that exhibits structural homology with VEGFD. Both VEGFC and VEGFD promote lymph-angiogenesis and angiogenesis by combining with VEGFR2 and VEGFR3 [42,43,44,45]. Elevated VEGFD levels may be an adaptation to the requirement of the lymphatic system to eliminate fluid from the extravascular space off the lungs and peripheral tissues [46]. Serum VEGFC levels are associated with dyslipidemia [47], which is a causative risk factor and treatment target for ischemic stroke. Therefore, the VEGF family and their receptors are complexity. The expression profiles and the effects of the VEGF members after ischemic stroke need to be further studies. These may provide new targets for the treatment of patients with AIS. The VEGF family has been shown to participate in atherosclerosis, cerebral edema, neuroprotection, neurogenesis, angiogenesis and postischemic brain and vessel repair in experimental stroke [2]. However, the above actions mainly involve the interaction between VEGFA and VEGFR2. VEGFA and VEGFR2 have been strongly implicated in regulating angiogenesis and vascular permeability during homeostasis and pathological conditions [4]. Therefore, VEGFA and VEGFR2may function as osmotic factors, damage the vascular endothelial barrier, increase vascular permeability, and exacerbate BBB leakage in patients with AIS. Studies in vitro have indicated that VEGFA expression increases in astrocytes, endothelial cells and neurons, whereas VEGFR2 expression increases in endothelial cells in the peri-infarct area following stroke [48]. In addition, many studies have indicated that VEGFA and VEGFR2 participate in BBB breakdown [13, 35, 49, 50], thus aggravating neurological function injury following ischemic stroke. In our study, plasma VEGFA and VEGFR2 levels were significantly elevated in patients with AIS within 24 h after stroke compared to those in healthy controls, which is consistent with the results of other studies [1, 51]. Furthermore, we found that VEGFA and VEGFR2 levels were significantly higher in patients with unfavorable outcomes than in those with favorable outcomes, and were positively correlated with the mRS score at 3 months. These results indicated that VEGFA and VEGFR2 are correlated with unfavorable outcomes in AIS.
Previous studies have shown that diabetes is a major risk factor for ischemic stroke [52, 53] and a strong predictor of poor prognosis [54,55,56,57]. An in vitro study had demonstrated an abnormal and persistent increase in VEGFR2 expression in the peri-infarct vascular network following ischemic stroke in mouse model of type 1 diabetes [55]. A clinical study showed that higher blood glucose levels are associated with aggravated brain edema [58], which exacerbates BBB breakdown. Blood VEGF are concentrations were correlated with glycosylated hemoglobin [22]. Similarly, we found that plasma VEGFR2 levels were significantly higher in AIS patients with diabetes than in those without diabetes and were positively correlated with blood glucose concentration on admission in our study. Therefore, it is important to consider comorbidities when determining the appropriate treatment for ischemic stroke.
Brain edema is a potentially fatal pathological state and is one of the most devastating consequences of ischemic stroke. VEGF1/VEGFR2 has been shown to be associated with brain edema in animal models of cerebral ischemia. It is of great clinical significance to explore the association between VEGFA/VEGFR2 and brain edema in patients with AIS. When collecting patient data, we also paid attention to collecting information on brain edema. However, only 16 of the enrolled patients showed significant brain edema on imaging, which is relatively small and we cannot statistically analyze them. Research on brain edema after AIS may be more appropriate for severe cerebral infarction [59].
Univariate analysis demonstrated that elevated plasma VEGFA and VEGFR2 levels were associated with an increased risk of unfavorable outcomes at 3 months. After adjusting for potential contributing factors in multivariate logistic regression, we found that plasma VEGFA and VEGFR2 levels were independent biomarkers for predicting poor prognosis in patients with AIS. Furthermore, the addition the VEGFA and VEGFR2 to the clinical risk-prediction model significantly improved prediction efficiency. In this study, a nomogram based on LASSO regression was constructed to visualize the risk-prediction model. The AUC and calibration curve were used to determine the discrimination and consistency of the prediction model. The NRI and IDI indexes were used to evaluate the accuracy of the prediction model. Therefore, the new risk-prediction model integrating VEGFA and VEGFR2 levels is more discriminative, consistent and accurate than the conditional clinical model. Furthermore, DCA revealed that the new risk-prediction model had greater clinical value than the conventional clinical model. This is the first study to report that plasma VEGFA and VEGFR2 levels may predict the prognosis of patients with AIS, indicating their novel value as biomarkers for risk stratification. Improved stratification may help identify patients with unfavorable outcomes, which may facilitate early diagnosis and treatment to improve prognosis.
However, this study had several limitations. First, although we adjusted for multiple potential confounders in the entire cohort, the effects of possible residual confounding factors could not be excluded. Second, VEGFA and VEGFR2 levels may be dynamic, and temporal changes in plasma VEGFA and VEGFR2 levels in AIS deserve further investigation. Finally, this study is only conducted in a single center, and further validation is required through multi-center, large-scale clinical trials.
Conclusion
The present study demonstrates that the addition of plasma VEGFA and VEGFR2 levels to the clinical risk-prediction model may aid in improving the risk stratification of patients with AIS within 24 h of the stroke. Therefore, the combination of plasma VEGFA and VEGFR2 levels determination in conjunction with clinical and imaging examinations will yield greater accuracy for predicting 3-month prognosis in patients with AIS. However, large-scale, multi-center studies are required to validate the association between plasma VEGFA and VEGFR2 levels on admission and the prognosis of AIS. VEGFA and VEGFR2 are likely important mediators of stroke and comorbidities, which warrants further studies.
Data Availability
The data and materials support the findings of this study are available from the corresponding authors.
References
Babkina AS, Yadgarov MY, Ostrova IV et al (2022) Serum levels of vegf-a and its receptors in patients in different phases of hemorrhagic and ischemic strokes. Curr Issues Mol Biol 44(10):4888–4901. https://doi.org/10.3390/cimb44100332
Greenberg DA, Jin K (2013) Vascular endothelial growth factors (vegfs) and stroke. Cell Mol Life Sci 70(10):1753–1761. https://doi.org/10.1007/s00018-013-1282-8
Yang Y, Torbey MT (2020) Angiogenesis and blood-brain barrier permeability in vascular remodeling after stroke. Curr Neuropharmacol 18(12):1250–1265. https://doi.org/10.2174/1570159X18666200720173316
Kim ID, Cave JW, Cho S (2021) Aflibercept, a vegf (vascular endothelial growth factor)-trap, reduces vascular permeability and stroke-induced brain swelling in obese mice. Stroke 52(8):2637–2648. https://doi.org/10.1161/STROKEAHA.121.034362
Stokum JA, Gerzanich V, Simard JM (2016) Molecular pathophysiology of cerebral edema. J Cereb Blood Flow Metab 36(3):513–538. https://doi.org/10.1177/0271678X15617172
Rosenberg GA (1999) Ischemic brain edema. Prog Cardiovasc Dis 42(3):209–216. https://doi.org/10.1016/s0033-0620(99)70003-4
Roth P, Regli L, Tonder M et al (2013) Tumor-associated edema in brain cancer patients: Pathogenesis and management. Expert Rev Anticancer Ther 13(11):1319–1325. https://doi.org/10.1586/14737140.2013.852473
Weis SM, Cheresh DA (2005) Pathophysiological consequences of vegf-induced vascular permeability. Nature 437(7058):497–504. https://doi.org/10.1038/nature03987
Song Y, Liu B, Guan M et al (2018) Successful treatment using apatinib in intractable brain edema: a case report and literatures review. Cancer Biol Ther 19(12):1093–1096. https://doi.org/10.1080/15384047.2018.1491502
Kim E, Yang J, Park KW et al (2018) Inhibition of vegf signaling reduces diabetes-exacerbated brain swelling, but not infarct size, in large cerebral infarction in mice. Transl Stroke Res 9(5):540–548. https://doi.org/10.1007/s12975-017-0601-z
Ergul A, Abdelsaid M, Fouda AY et al (2014) Cerebral neovascularization in diabetes: Implications for stroke recovery and beyond. J Cereb Blood Flow Metab 34(4):553–563. https://doi.org/10.1038/jcbfm.2014.18
Huang Y, Chen S, Luo Y et al (2020) Crosstalk between inflammation and the bbb in stroke. Curr Neuropharmacol 18(12):1227–1236. https://doi.org/10.2174/1570159X18666200620230321
Liu J, Chen L, Zhang X et al (2020) The protective effects of juglanin in cerebral ischemia reduce blood-brain barrier permeability via inhibition of vegf/vegfr2 signaling. Drug Des Devel Ther 14:3165–3175. https://doi.org/10.2147/DDDT.S250904
Lee B, Shin H, Oh JE et al (2021) An autophagic deficit in the uterine vessel microenvironment provokes hyperpermeability through deregulated vegfa, nos1, and ctnnb1. Autophagy 17(7):1649–1666. https://doi.org/10.1080/15548627.2020.1778292
Castaneda-Cabral JL, Colunga-Duran A, Urena-Guerrero ME et al (2020) Expression of vegf- and tight junction-related proteins in the neocortical microvasculature of patients with drug-resistant temporal lobe epilepsy. Microvasc Res 132:104059. https://doi.org/10.1016/j.mvr.2020.104059
Annese T, Ruggieri S, De Giorgis M et al (2019) Alpha-methyl-prednisolone normalizes the pkc mediated brain angiogenesis in dystrophic mdx mice. Brain Res Bull 147:69–77. https://doi.org/10.1016/j.brainresbull.2019.01.023
Lv B, Zheng K, Sun Y et al (2022) Network pharmacology experiments show that emodin can exert a protective effect on mcao rats by regulating hif-1alpha/vegf-a signaling. ACS Omega 7(26):22577–22593. https://doi.org/10.1021/acsomega.2c01897
Abdul Muneer PM, Alikunju S, Szlachetka AM et al (2012) The mechanisms of cerebral vascular dysfunction and neuroinflammation by mmp-mediated degradation of vegfr-2 in alcohol ingestion. Arterioscler Thromb Vasc Biol 32(5):1167–1177. https://doi.org/10.1161/ATVBAHA.112.247668
Lasek-Bal A, Jedrzejowska-Szypulka H, Student S et al (2019) The importance of selected markers of inflammation and blood-brain barrier damage for short-term ischemic stroke prognosis. J Physiol Pharmacol 70(2). https://doi.org/10.26402/jpp.2019.2.04
Sobrino T, Rodriguez-Yanez M, Campos F et al (2020) Association of high serum levels of growth factors with good outcome in ischemic stroke: a multicenter study. Transl Stroke Res 11(4):653–663. https://doi.org/10.1007/s12975-019-00747-2
Aberg ND, Wall A, Anger O et al (2020) Circulating levels of vascular endothelial growth factor and post-stroke long-term functional outcome. Acta Neurol Scand 141(5):405–414. https://doi.org/10.1111/ane.13219
Escudero C, Acurio J, Lopez E et al (2021) Vascular endothelial growth factor and poor prognosis after ischaemic stroke. Eur J Neurol 28(5):1759–1764. https://doi.org/10.1111/ene.14641
Geiseler SJ,Morland C (2018) The janus face of vegf in stroke. Int J Mol Sci 19(5). https://doi.org/10.3390/ijms19051362
Hu Y, Zheng Y, Wang T et al (2022) Vegf, a key factor for blood brain barrier injury after cerebral ischemic stroke. Aging Dis 13(3):647–654. https://doi.org/10.14336/AD.2021.1121
Alrafiah A, Alofi E, Almohaya Y et al (2021) Angiogenesis biomarkers in ischemic stroke patients. J Inflamm Res 14:4893–4900. https://doi.org/10.2147/JIR.S331868
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35. https://doi.org/10.1002/1097-0142(1950)3:1%3c32::aid-cncr2820030106%3e3.0.co;2-3
Burke Quinlan E, Dodakian L, See J et al (2015) Neural function, injury, and stroke subtype predict treatment gains after stroke. Ann Neurol 77(1):132–145. https://doi.org/10.1002/ana.24309
Prodjohardjono A, Vidyanti AN, Susianti NA et al (2020) Higher level of acute serum vegf and larger infarct volume are more frequently associated with post-stroke cognitive impairment. PLoS One 15(10):e0239370. https://doi.org/10.1371/journal.pone.0239370
Bhasin A, Srivastava MVP, Vivekanandhan S et al (2019) Vascular endothelial growth factor as predictive biomarker for stroke severity and outcome; an evaluation of a new clinical module in acute ischemic stroke. Neurol India 67(5):1280–1285. https://doi.org/10.4103/0028-3886.271241
Navarro-Sobrino M, Rosell A, Hernandez-Guillamon M et al (2011) A large screening of angiogenesis biomarkers and their association with neurological outcome after ischemic stroke. Atherosclerosis 216(1):205–211. https://doi.org/10.1016/j.atherosclerosis.2011.01.030
Kwon HS, Kim YS, Park HH et al (2015) Increased vegf and decreased sdf-1alpha in patients with silent brain infarction are associated with better prognosis after first-ever acute lacunar stroke. J Stroke Cerebrovasc Dis 24(3):704–710. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.11.021
Muller S, Kufner A, Dell’Orco A et al (2021) Evolution of blood-brain barrier permeability in subacute ischemic stroke and associations with serum biomarkers and functional outcome. Front Neurol 12:730923. https://doi.org/10.3389/fneur.2021.730923
Wang J, Fu X, Yu L et al (2020) Correction to: Preconditioning with vegf enhances angiogenic and neuroprotective effects of bone marrow mononuclear cell transplantation in a rat model of chronic cerebral hypoperfusion. Mol Neurobiol 57(9):3989–3990. https://doi.org/10.1007/s12035-020-01898-2
Rite I, Machado A, Cano J et al (2008) Intracerebral vegf injection highly upregulates aqp4 mrna and protein in the perivascular space and glia limitans externa. Neurochem Int 52(4–5):897–903. https://doi.org/10.1016/j.neuint.2007.10.004
Nag S, Eskandarian MR, Davis J et al (2002) Differential expression of vascular endothelial growth factor-a (vegf-a) and vegf-b after brain injury. J Neuropathol Exp Neurol 61(9):778–788. https://doi.org/10.1093/jnen/61.9.778
Nag S, Manias J, Eubanks JH et al (2019) Increased expression of vascular endothelial growth factor-d following brain injury. Int J Mol Sci 20(7). https://doi.org/10.3390/ijms20071594
Zhang F, Tang ZS, Hou X et al (2009) Vegf-b is dispensable for blood vessel growth but critical for their survival, and vegf-b targeting inhibits pathological angiogenesis. P Natl Acad Sci USA 106(15):6152–6157. https://doi.org/10.1073/pnas.0813061106
Sun YJ, Jin KL, Childs JT et al (2006) Vascular endothelial growth factor-b (vegfb) stimulates neurogenesis: evidence from knockout mice and growth factor administration. Dev Biol 289(2):329–335. https://doi.org/10.1016/j.ydbio.2005.10.016
Ishrat T, Soliman S, Eldahshan W et al (2018) Silencing vegf-b diminishes the neuroprotective effect of candesartan treatment after experimental focal cerebral ischemia. Neurochem Res 43(10):1869–1878. https://doi.org/10.1007/s11064-018-2604-x
Jean LeBlanc N, Guruswamy R, ElAli A (2018) Vascular endothelial growth factor isoform-b stimulates neurovascular repair after ischemic stroke by promoting the function of pericytes via vascular endothelial growth factor receptor-1. Mol Neurobiol 55(5):3611–3626. https://doi.org/10.1007/s12035-017-0478-6
Soliman S, Ishrat T, Pillai A et al (2014) Candesartan induces a prolonged proangiogenic effect and augments endothelium-mediated neuroprotection after oxygen and glucose deprivation: role of vascular endothelial growth factors a and b. J Pharmacol Exp Ther 349(3):444–457. https://doi.org/10.1124/jpet.113.212613
Achen MG, Jeltsch M, Kukk E et al (1998) Vascular endothelial growth factor d (vegf-d) is a ligand for the tyrosine kinases vegf receptor 2 (flk1) and vegf receptor 3 (flt4). Proc Natl Acad Sci U S A 95(2):548–553. https://doi.org/10.1073/pnas.95.2.548
Stacker SA, Williams SP, Karnezis T et al (2014) Lymphangiogenesis and lymphatic vessel remodelling in cancer. Nat Rev Cancer 14(3):159–172. https://doi.org/10.1038/nrc3677
Zheng W, Aspelund A, Alitalo K (2014) Lymphangiogenic factors, mechanisms, and applications. J Clin Invest 124(3):878–887. https://doi.org/10.1172/JCI71603
Ober EA, Olofsson B, Makinen T et al (2004) Vegfc is required for vascular development and endoderm morphogenesis in zebrafish. EMBO Rep 5(1):78–84. https://doi.org/10.1038/sj.embor.7400047
Borne Y, Gransbo K, Nilsson J et al (2018) Vascular endothelial growth factor d, pulmonary congestion, and incidence of heart failure. J Am Coll Cardiol 71(5):580–582. https://doi.org/10.1016/j.jacc.2017.11.058
Wada H, Ura S, Kitaoka S et al (2011) Distinct characteristics of circulating vascular endothelial growth factor-a and c levels in human subjects. PLoS One 6(12):e29351. https://doi.org/10.1371/journal.pone.0029351
Margaritescu O, Pirici D, Margaritescu C (2011) Vegf expression in human brain tissue after acute ischemic stroke. Rom J Morphol Embryol 52(4):1283–1292
Nag S, Takahashi JL, Kilty DW (1997) Role of vascular endothelial growth factor in blood-brain barrier breakdown and angiogenesis in brain trauma. J Neuropathol Exp Neurol 56(8):912–921. https://doi.org/10.1097/00005072-199708000-00009
Kim Y, Lee S, Zhang H et al (2020) Clec14a deficiency exacerbates neuronal loss by increasing blood-brain barrier permeability and inflammation. J Neuroinflammation 17(1):48. https://doi.org/10.1186/s12974-020-1727-6
Nielsen HH, Soares CB, Hogedal SS et al (2020) Acute neurofilament light chain plasma levels correlate with stroke severity and clinical outcome in ischemic stroke patients. Front Neurol 11:448. https://doi.org/10.3389/fneur.2020.00448
Wei JW, Heeley EL, Wang JG et al (2010) Comparison of recovery patterns and prognostic indicators for ischemic and hemorrhagic stroke in china: the chinaquest (quality evaluation of stroke care and treatment) registry study. Stroke 41(9):1877–1883. https://doi.org/10.1161/STROKEAHA.110.586909
Iemolo F, Beghi E, Cavestro C et al (2002) Incidence, risk factors and short-term mortality of stroke in vittoria, southern italy. Neurol Sci 23(1):15–21. https://doi.org/10.1007/s100720200018
Kruyt ND, Nys GM, van der Worp HB et al (2008) Hyperglycemia and cognitive outcome after ischemic stroke. J Neurol Sci 270(1–2):141–147. https://doi.org/10.1016/j.jns.2008.02.020
Reeson P, Tennant KA, Gerrow K et al (2015) Delayed inhibition of vegf signaling after stroke attenuates blood-brain barrier breakdown and improves functional recovery in a comorbidity-dependent manner. J Neurosci 35(13):5128–5143. https://doi.org/10.1523/JNEUROSCI.2810-14.2015
Lu GD, Ren ZQ, Zhang JX et al (2018) Effects of diabetes mellitus and admission glucose in patients receiving mechanical thrombectomy: a systematic review and meta-analysis. Neurocrit Care 29(3):426–434. https://doi.org/10.1007/s12028-018-0562-4
Ntaios G, Egli M, Faouzi M et al (2010) J-shaped association between serum glucose and functional outcome in acute ischemic stroke. Stroke 41(10):2366–2370. https://doi.org/10.1161/STROKEAHA.110.592170
Broocks G, Kemmling A, Aberle J et al (2020) Elevated blood glucose is associated with aggravated brain edema in acute stroke. J Neurol 267(2):440–448. https://doi.org/10.1007/s00415-019-09601-9
Vorasayan P, Bevers MB, Beslow LA et al (2019) Intravenous glibenclamide reduces lesional water uptake in large hemispheric infarction. Stroke 50(11):3021–3027. https://doi.org/10.1161/strokeaha.119.026036
Acknowledgements
We would appreciate that all the authors participate in this study, and the nurses in stroke center of Xuanwu hospital for the collection of the samples.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82171301), the Beijing Natural Science Foundation (7222083), and Capital Funds for Health Improvement and Research (2020–2-1032).
Author information
Authors and Affiliations
Contributions
Yue Hu and Yumin Luo conceived the study. Shuangfeng Huang, Tong Shen, Meng Geng, Rongliang Wang, Yilin Wang collected samples and processed samples. Yue Hu performed the experiments, analyzed the data and wrote the first draft of the manuscript. All authors commented on previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Xuanwu Hospital of Capital Medical University.
Consent to Participate
The experiment was undertaken with the understanding and informed consent was obtained from all individual participants or their immediate family members.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, Y., Huang, S., Shen, T. et al. Prognostic Significance of Plasma VEGFA and VEGFR2 in Acute Ischemic Stroke-a Prospective Cohort Study. Mol Neurobiol 61, 6341–6353 (2024). https://doi.org/10.1007/s12035-024-03973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-024-03973-4