Abstract
Background
We performed a meta-analysis to evaluate the outcomes of acute ischemic stroke (AIS) in patients treated with mechanical thrombectomy (MT), according to diabetes mellitus and admission glucose level (AGL).
Methods
We systematically reviewed previous studies in PubMed that reported outcomes of MT in AIS patients and their relationships with diabetes mellitus or AGL. We used functional independence (modified Rankin score ≤ 2 at 3 months) as the primary end point.
Results
Data from 12,653 patients in 47 articles that evaluated the effect of diabetes mellitus or AGL on outcomes after MT were included. Compared with patients without a history of diabetes mellitus, patients with a diabetes mellitus history had significantly lower odds of functional independence in both the unadjusted meta-analysis (odds ratio [OR] 0.64; 95% confidence interval [CI] 0.54–0.75) and the multivariable analysis (OR 0.48; 95% CI 0.33–0.71). Similarly, higher AGL was associated with an unfavorable functional outcome in the unadjusted meta-analysis (pooled effect size − 0.38; 95% CI − 0.45 to − 0.31), and the adjusted OR (95% CI) per 1 mmol/L increase in AGL was 0.87 (0.83–0.92) for functional independence according to the combined multivariable results. Recanalization rate and symptomatic intracranial hemorrhage were neither related to AGL nor different in patients with or without diabetes mellitus.
Conclusions
The present study confirms that a history of diabetes mellitus and high AGL are associated with unfavorable functional outcomes at 3 months after MT in AIS patients. However, the causal relationship between hyperglycemia and poor prognosis remains undetermined, and further investigations are required to ascertain whether AIS patients receiving MT could benefit from intensive glucose control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, accumulating evidence has demonstrated the safety and efficiency of mechanical thrombectomy (MT) in the management of acute ischemic stroke (AIS) caused by large-vessel occlusion [1,2,3,4,5,6]. Despite the substantial improvements demonstrated by recently published trials, a large number of patients do not experience good neurological outcomes even though successful timely recanalization is achieved. Previous studies [7,8,9,10,11] reveal that hyperglycemia is associated with worse functional outcomes, hemorrhagic transformation, and mortality in AIS patients treated with intravenous or intra-arterial thrombolysis. It is reasonable to speculate that the glucose value is also related to the treatment efficacy of MT.
Possible mechanisms explaining the association between hyperglycemia and poor outcomes in AIS patients include altered blood–brain barrier permeability [12, 13], increased lactic acid production in ischemic tissue [14], impairment of cerebrovascular reactivity in the microvasculature [15], and increased vulnerability to reperfusion injury [16]. A post hoc analysis [17] of the SWIFT (Solitaire Flow Restoration with the Intention for Thrombectomy) trial indicated that in patients treated with MT, hyperglycemia was independently associated with a worse outcome at 3 months. Another analysis [18], using data from the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) study, showed no significant interaction between increased admission serum glucose and clinical outcomes in AIS patients administered intra-arterial treatment. Available evidence shows conflicting results with regard to a potential detrimental effect of glucose level on clinical outcomes.
We therefore sought to investigate whether diabetes mellitus history or admission glucose level (AGL), in patients with AIS treated by MT, was associated with worse outcomes by conducting a systematic review of previous observational studies.
Materials and Methods
Search Strategy
We attempted to identify all published observational and interventional studies reporting the influence of diabetes mellitus or AGL on efficacy or safety outcomes in AIS patients treated with MT by searching PubMed (from January 2007 to October 2017), without language restriction. The following search terms were used: (intra-arterial OR endovascular OR mechanical OR thrombectomy OR embolectomy OR recanalization OR clot removal OR clot disruption) AND stroke. We also searched the reference lists of the retrieved articles and published review articles for additional studies.
Study Selection and Data Extraction
Potentially relevant articles were independently evaluated by two investigators (GD Lu and ZQ Ren) based on the title and abstract. After primary selection, the full text of closely related studies was then obtained for further review, and the prespecified inclusion criteria were as follows: (1) the age of included AIS patients was ≥ 18 years, and the sample size was ≥ 90; (2) ≥ 70% of the included patients were treated with MT with or without thrombolysis; and (3) a statistical analysis of the association of outcomes (efficacy or safety) with a history of diabetes mellitus or AGL was reported. We did not include reviews, meta-analyses, case reports, studies focusing on posterior circulation occlusion, or studies with a treatment time > 24 h after stroke onset. For records with overlapping data, the most updated or most inclusive data were chosen for the analysis. When multiple end points were reported in separate articles or when impacts of diabetes mellitus and AGL were reported in separate articles, duplicate articles were included. We did not assess the quality of studies included, for most of them were not primarily designed to investigate the effects of diabetes mellitus history or AGL on efficacy or safety outcomes in AIS patients treated with MT.
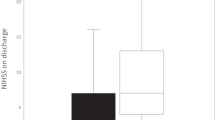
Data extraction from eligible studies was independently performed by two authors (GD Lu and ZQ Ren), and disagreements were resolved through discussion with another author (QQ Zu). The following relevant information was collected: report features (first author, year of publication, journal); study design (country included, study period, study type); subjects included (number, age, sex, occlusion sites, admission National Institutes of Health Stroke Scale [NIHSS]); mechanical technologies used (Merci retriever, Penumbra system, clot disruption, angioplasty, stent placement, manual aspiration, or stent retriever); definition and incidence of outcomes (recanalization, mortality, functional outcomes, intracranial hemorrhage); associations with diabetes mellitus (or AGL); and outcomes in univariate or multivariate analyses. We did not contact the authors of the studies to obtain incomplete data.
Outcome Variables and Statistical Analysis
The primary end point of the present study was functional independence, defined as a modified Rankin Scale score of ≤ 2 at 90 days after endovascular treatment. Other end points included successful recanalization/angiographic outcomes (Thrombolysis in Myocardial Infarction ≥ 2 or Thrombolysis in Cerebral Infarction 2b/3) and symptomatic intracranial hemorrhage (sICH, defined according to definitions in the original studies).
In the present study, AGLs were reported with the conventional unit (mg/dL), and the standard unit (mmol/L) was converted to the conventional unit by multiplying by 18 when necessary. Using patients without a diabetes mellitus history as the reference group, the unadjusted effect size for diabetes mellitus according to the ORs and associated 95% CIs was calculated by the Mantel–Haenszel method. The unadjusted effect size for AGL was reported as the standardized mean difference (SMD) and 95% CIs based on the inverse variance method between patients with and without end points. When AGL means (± SD) were not available, the effect size was approximated by medians (interquartile range) or converted based on the OR associated with the glucose cutoff level [19]. A random-effects model was used for all syntheses. Statistical heterogeneity was assessed with Cochran’s Q via a Chi-square test. We performed sensitivity analyses to investigate the end points, including only studies that used modern mechanical thrombectomy technologies (i.e., stent retrievers and direct aspiration) and studies that relied heavily on the Merci device or Penumbra or did not specify the type of mechanical thrombectomy technology used. Sensitivity analyses restricted to the studies in which the effect size was not approximated were also reported. Funnel plots and the Egger test (for the primary end point only) were used to assess publication bias [20]. Finally, we collected and combined the available multivariate results, and for AGL, we calculated the adjusted OR per 18 mg/dL (= 1 mmol/L) increase in glucose values. All statistical analyses were performed using Stata 14.0 (Stata Corp, College Station, TX). A probability value of < 0.05 was considered significant, except for heterogeneity testing, for which significance was accepted at a probability value of 0.10.
Results
Study Selection and Characteristics
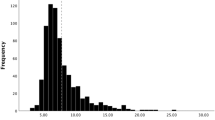
A total of 5975 potentially eligible records were identified from PubMed. During the selection process, 5582 records were eliminated after reading the titles and abstracts alone: 1301 reviews; 2913 studies not related to our study; 932 case reports, comments, errata, or study protocols; and 436 studies in which the number of patients was < 90. Of the 393 remaining articles, the full text was reviewed, and study exclusion was as follows: 240 were excluded due to missing required information, 8 were excluded because of overlapping patient populations, 5 were excluded because they only included patients with posterior circulation occlusion, 88 were excluded because they only included patients with simple intravenous thrombolysis or > 30% of the included patients underwent intra-arterial thrombolysis only, and 5 were excluded because they only included patients with successful recanalization. No additional studies were found by hand-searching the review and relevant articles. Finally, 47 articles from 42 studies including a total of 12,653 patients were included in the meta-analysis (Fig. 1).
The main features of the included articles are shown in Table I in Supplemental Material. Thirty-eight studies reported the number of diabetes mellitus patients, and the proportion of diabetes mellitus patients was 21.3% (2586/12,138). Of the 41 studies that reported occlusion location, 28 included anterior circulation strokes only, and the remaining 13 studies included both anterior and posterior circulation strokes. Of the 36 studies that reported the type of mechanical thrombectomy technology used, modern mechanical thrombectomy technologies (i.e., stent retrievers and direct aspiration) were used in 21 of them.
Diabetes Mellitus and Outcomes
The available unadjusted results of the effect of diabetes mellitus on functional outcomes were reported in 23 studies (n = 6515). Compared with those without, patients with a history of diabetes mellitus were associated with significantly lower odds of functional independence (Fig. 2). We found similar results in a sensitivity analysis that only included studies that utilized modern mechanical thrombectomy technologies (Fig. 2) and in a pooled analysis of available multivariate ORs (Fig. 4a). There was no significant difference in recanalization rates (OR 1.00; 95% CI 0.85–1.18; I2 = 0.0%) between the patients with and without a history of diabetes mellitus (13 studies; n = 4234). A similar result was found in the sensitivity analysis that only included studies utilizing modern mechanical thrombectomy technologies (6 studies, n = 1254; OR 0.99; 95% CI 0.72–1.36; I2 = 0.0%). We also found no difference in the combined available unadjusted results for sICH (OR 0.97; 95% CI 0.71–1.31; I2 = 0.0%) between patients with and without a history of diabetes mellitus (6 studies; n = 2729). Additionally, the sensitivity analysis that only included studies utilizing modern mechanical thrombectomy technologies showed a similar result (2 studies, n = 778; OR 0.89; 95% CI 0.53–1.48; I2 = 0.0%).
Forest plots of unadjusted odds ratios (ORs) for functional independence associated with diabetes mellitus history. EDM/DM = number of patients with both functional independence and diabetes mellitus/number of patients with diabetes mellitus; ENDM/NDM = number of patients without diabetes mellitus but with functional independence/number of patients without diabetes mellitus. Ellipses denote not available. References to the studies listed are provided in Supplemental Material
Admission Blood Glucose Levels and Outcomes
The available unadjusted effect sizes of the effect of AGL on functional outcomes were reported in 13 studies (n = 3199), and patients with functional independence had a significantly lower AGL than patients without functional independence (Fig. 3). A similar result was found in a sensitivity analysis that only included studies with modern mechanical thrombectomy technologies (Fig. 4) or excluded studies with approximate effect sizes (7 studies; n = 2007; pooled effect size − 0.37; 95% CI − 0.46 to − 0.28; I2 = 0.0%). A higher AGL remained associated with poor functional outcomes when the available multivariable results were combined (calculated as ORs per 18 mg/dL of glucose, Fig. 4b). There was no difference in AGL (pooled effect size − 0.04; 95% CI − 0.18 to 0.09; I2 = 0.0%) between the patients with and without successful recanalization (6 studies; n = 1070). Moreover, a similar result was found in a sensitivity analysis that only included studies with modern mechanical thrombectomy technologies (4 studies; n = 793; pooled effect size − 0.03; 95% CI − 0.19 to 0.13; I2 = 0.0%) or excluded studies with approximate effect sizes (3 studies; n = 436; pooled effect size − 0.03; 95% CI − 0.24 to 0.18; I2 = 0.0%). A nonsignificant difference in available unadjusted effect sizes of AGL (pooled effect size 0.28; 95% CI − 0.01 to 0.58; I2 = 57.4%) was found between patients with and without sICH (5 studies; n = 1230). Additionally, the sensitivity analysis that only included studies utilizing modern mechanical thrombectomy technologies (3 studies; n = 921; pooled effect size 0.26; 95% CI − 0.05 to 0.57; I2 = 47.8%) and excluded studies with approximate effect sizes (3 studies; n = 452; pooled effect size 0.22; 95% CI − 0.41 to 0.85; I2 = 73.3%) showed a similar result.
Forest plots of unadjusted SMDs in admission glucose level between patients with and without functional independence. G-mean (SD) = the mean admission glucose level in patients with functional independence and the standard deviation; P-mean (SD) = the mean admission glucose level in patients without functional independence and the standard deviation. References to the studies listed are provided in Supplemental Material
Publication Bias
The funnel plot did not suggest publication bias for both a history of diabetes mellitus and AGL with respect to functional independence (Fig. 5). The P value for publication bias was 0.404 for the relationship between diabetes mellitus and functional outcomes and 0.665 for the relationship between AGL and functional outcomes.
Discussion
Evidence from currently available data suggests that diabetes mellitus and high AGL are associated with lower odds of functional independence at 3 months after MT in AIS patients. Recanalization rates and sICH were not related to AGL and were not different between patients with and without diabetes mellitus.
Animal studies have shown that hyperglycemia is associated with larger infarct sizes in permanent MCA occlusion models that have large penumbral areas in collaterally perfused regions, such as cats or monkeys [21, 22]. A pioneering magnetic resonance imaging study in patients with AIS also reported that hyperglycemia reduced salvage of perfusion–diffusion mismatch tissue from infarction and resulted in greater infarct sizes, as glucose levels < 7.0 mmol/L were associated with > 80% penumbra salvage and levels > 8.0 mmol/L were associated with < 50% salvage [23]. A prospective study indicates that hyperglycemia correlates with a markedly larger increase in the infarction volume in patients receiving intravenous thrombolysis [24]. Hyperglycemia may accelerate the transformation of ischemic penumbra into infarction, as a result of lactate accumulation and acidosis, which can be directly toxic or trigger different mechanisms that eventually leading to infarction. Furthermore, hyperglycemia is also associated with increased reperfusion injury, which aggravates the impairment of brain tissue after recanalization [14, 16, 25]. Despite all these supporting data, a Cochrane review including 11 randomized controlled trials showed that treatment with intravenous insulin to maintain normal glucose levels did not provide a benefit in terms of functional outcomes, death, or improvement in final neurological deficits, but it significantly increased the number of hypoglycemic episodes [26]. A randomized controlled trial even reported that compared with control treatment in patients with vessel occlusion, greater infarct growth was observed in patients treated with glucose–potassium–insulin [27]. Currently available evidence suggests that hyperglycemia may only be a transient stress response, which reflects the severity of the stroke, rather than a causal factor, explaining why interventional studies on hyperglycemia were all inconclusive.
However, all the relevant randomized controlled trials regarding glucose control enrolled patients within 12 h [28, 29] or 24 h [27, 30,31,32,33] of ischemic stroke onset, and the recanalization condition of the included patients was not taken into account. The benefits of intensive glucose control in cases of stroke with hyperglycemia may therefore be masked by the time delay after stroke or the low recanalization rate in the experimental groups, as arterial recanalization grade and speed have been reported to be one of the strongest predictors of favorable outcomes after thrombolysis. An experiment in rats with reversible middle cerebral artery (MCA) occlusion showed that large infarcts occurred after 15–45 min of MCA occlusion in hyperglycemic rats, whereas they only appeared after 60–90 min in normoglycemic rats, and the final infarct sizes were fivefold to tenfold larger in hyperglycemic compared with normoglycemic rats [34]. Ribo et al. found that the time before arterial recanalization that was associated with poor outcomes was only 3.5 h in AIS patients with hyperglycemia, whereas it was 7.5 h in patients with adequate glucose control [35]. Accumulating evidence has shown the success of endovascular treatment, especially MT using stent retrievers, in improving the recanalization rate in patients with AIS caused by large-vessel occlusion. Moreover, in most cases, MT was performed within 8 h of ischemic stroke onset. Since the time delay and the low recanalization rate have been overcome by MT, it is reasonable to assume that the effect of intensive glucose control would become visible in AIS patients.
Although our results show that high AGL is related to unfavorable functional outcomes, the precise association between serum glucose levels and functional outcomes in AIS patients needs to be further studied. Ntaios et al. [36] reported that functional outcomes and glucose values are best modeled as a J-shaped curve with worse outcomes at both low and high glucose values. A retrospective study with 58,265 patients also showed that the relationship between hyperglycemia and clinical outcomes in AIS patients treated with tPA was nonlinear. A similar association may also be present in AIS patients treated with MT [11].
Our study has several potential limitations. First, the definition of sICH was obtained from the original studies instead of from a standardized definition, which may influence the reliability of the pooled results for this end point. Second, all the studies included in our analysis were observational, and most of them did not control for baseline characteristics. It is reported that patients with hyperglycemia are older, have a higher median stroke severity (as measured by the National Institutes of Health Stroke Scale), have longer median onset to treatment times, and have more frequently documented medical histories of hypertension, carotid stenosis, dyslipidemia, and heart failure [11], which indicates that the pooled unadjusted results of the present study may be influenced by intrinsic biases in the baseline nonrandomized data. However, our combined multivariate results showed similar outcomes with combined unadjusted effect sizes, which partly enhanced the credibility of our results. Third, we did not evaluate the quality of the included studies. Although important differences in inclusion criteria, devices used, and stroke severity between studies may limit the generalization of our conclusions, we have attempted to overcome this issue by performing sensitivity analyses that only included studies that used modern mechanical thrombectomy technologies and studies in which the effect size was not approximated. Finally, we did not evaluate the effects of diabetes mellitus or AGL on clinical outcomes according to reperfusion status and ischemic stroke type. Kim et al. [17] reported that the negative effect of high glucose levels may be exacerbated in patients with incomplete reperfusion after MT and another study [37] suggested that the adverse effects of hyperglycemia in AIS patients receiving thrombolysis were primarily found in the large-vessel occlusive rather than in the cardioembolic stroke subtype.
In conclusion, a history of diabetes mellitus and high AGL are associated with unfavorable functional outcomes at 3 months after MT in AIS patients. However, the causal relationship between hyperglycemia and poor prognosis remains uncertain, and high AGL may just be a transient stress response related to stroke severity rather than a causal factor. Further randomized controlled studies, such as the ongoing Stroke Hyperglycemia Insulin Network Effort (SHINE) trial [38], may provide important novel information regarding the management of AIS patients with hyperglycemia receiving MT.
References
Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20.
Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18.
Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–95.
Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306.
Bracard S, Ducrocq X, Mas JL, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–47.
Desilles JP, Meseguer E, Labreuche J, et al. Diabetes mellitus, admission glucose, and outcomes after stroke thrombolysis: a registry and systematic review. Stroke. 2013;44:1915–23.
Demchuk AM, Morgenstern LB, Krieger DW, et al. Serum glucose level and diabetes predict tissue plasminogen activator-related intracerebral hemorrhage in acute ischemic stroke. Stroke. 1999;30:34–9.
Bruno A, Levine SR, Frankel MR, et al. Admission glucose level and clinical outcomes in the NINDS rt-PA Stroke Trial. Neurology. 2002;59:669–74.
Ribo M, Molina C, Montaner J, et al. Acute hyperglycemia state is associated with lower tPA-induced recanalization rates in stroke patients. Stroke. 2005;36:1705–9.
Masrur S, Cox M, Bhatt DL, et al. Association of acute and chronic hyperglycemia with acute ischemic stroke outcomes post-thrombolysis: findings from get with the guidelines-stroke. J Am Heart Assoc. 2015;4:e002193.
Kamada H, Yu F, Nito C, Chan PH. Influence of hyperglycemia on oxidative stress and matrix metalloproteinase-9 activation after focal cerebral ischemia/reperfusion in rats: relation to blood-brain barrier dysfunction. Stroke. 2007;38:1044–9.
Ennis SR, Keep RF. Effect of sustained-mild and transient-severe hyperglycemia on ischemia-induced blood-brain barrier opening. J Cereb Blood Flow Metab. 2007;27:1573–82.
Suh SW, Shin BS, Ma H, et al. Glucose and NADPH oxidase drive neuronal superoxide formation in stroke. Ann Neurol. 2008;64:654–63.
Kawai N, Keep RF, Betz AL. Hyperglycemia and the vascular effects of cerebral ischemia. Stroke. 1997;28:149–54.
Martini SR, Kent TA. Hyperglycemia in acute ischemic stroke: a vascular perspective. J Cereb Blood Flow Metab. 2007;27:435–51.
Kim JT, Jahan R, Saver JL. Impact of glucose on outcomes in patients treated with mechanical thrombectomy: a post hoc analysis of the solitaire flow restoration with the intention for thrombectomy study. Stroke. 2016;47:120–7.
Osei E, den Hertog HM, Berkhemer OA, et al. Admission glucose and effect of intra-arterial treatment in patients with acute ischemic stroke. Stroke. 2017;48:1299–305.
Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19:3127–31.
Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
de Courten-Myers G, Myers RE, Schoolfield L. Hyperglycemia enlarges infarct size in cerebrovascular occlusion in cats. Stroke. 1988;19:623–30.
de Courten-Myers GM, Kleinholz M, Wagner KR, Myers RE. Normoglycemia (not hypoglycemia) optimizes outcome from middle cerebral artery occlusion. J Cereb Blood Flow Metab. 1994;14:227–36.
Parsons MW, Barber PA, Desmond PM, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52:20–8.
Els T, Klisch J, Orszagh M, et al. Hyperglycemia in patients with focal cerebral ischemia after intravenous thrombolysis: influence on clinical outcome and infarct size. Cerebrovasc Dis. 2002;13:89–94.
Yip PK, He YY, Hsu CY, Garg N, Marangos P, Hogan EL. Effect of plasma glucose on infarct size in focal cerebral ischemia-reperfusion. Neurology. 1991;41:899–905.
Bellolio MF, Gilmore RM, Ganti L. Insulin for glycaemic control in acute ischaemic stroke. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD005346.pub4.
McCormick M, Hadley D, McLean JR, Macfarlane JA, Condon B, Muir KW. Randomized, controlled trial of insulin for acute poststroke hyperglycemia. Ann Neurol. 2010;67:570–8.
Bruno A, Kent TA, Coull BM, et al. Treatment of hyperglycemia in ischemic stroke (THIS): a randomized pilot trial. Stroke. 2008;39:384–9.
Staszewski J, Brodacki B, Kotowicz J, Stepien A. Intravenous insulin therapy in the maintenance of strict glycemic control in nondiabetic acute stroke patients with mild hyperglycemia. J Stroke Cerebrovasc Dis. 2011;20:150–4.
Gray CS, Hildreth AJ, Sandercock PA, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007;6:397–406.
Walters MR, Weir CJ, Lees KR. A randomised, controlled pilot study to investigate the potential benefit of intervention with insulin in hyperglycaemic acute ischaemic stroke patients. Cerebrovasc Dis. 2006;22:116–22.
Kreisel SH, Berschin UM, Hammes HP, et al. Pragmatic management of hyperglycaemia in acute ischaemic stroke: safety and feasibility of intensive intravenous insulin treatment. Cerebrovasc Dis. 2009;27:167–75.
Johnston KC, Hall CE, Kissela BM, Bleck TP, Conaway MR. Glucose Regulation in Acute Stroke Patients (GRASP) trial: a randomized pilot trial. Stroke. 2009;40:3804–9.
Piironen K, Putaala J, Rosso C, Samson Y. Glucose and acute stroke: evidence for an interlude. Stroke. 2012;43:898–902.
Ribo M, Molina CA, Delgado P, et al. Hyperglycemia during ischemia rapidly accelerates brain damage in stroke patients treated with tPA. J Cereb Blood Flow Metab. 2007;27:1616–22.
Ntaios G, Egli M, Faouzi M, Michel P. J-shaped association between serum glucose and functional outcome in acute ischemic stroke. Stroke. 2010;41:2366–70.
Mandava P, Martini SR, Munoz M, et al. Hyperglycemia worsens outcome after rt-PA primarily in the large-vessel occlusive stroke subtype. Transl Stroke Res. 2014;5:519–25.
Bruno A, Durkalski VL, Hall CE, et al. The Stroke Hyperglycemia Insulin Network Effort (SHINE) trial protocol: a randomized, blinded, efficacy trial of standard vs. intensive hyperglycemia management in acute stroke. Int J Stroke. 2014;9:246–51.
Acknowledgements
We would like to thank Jin Xu from Nanjing Medical University for his advices on statistical analysis.
Funding
This research received no specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
GDL was responsible for study design, literature search, data extraction, data analysis and manuscript drafting. ZQR was responsible for literature search, data extraction and manuscript drafting. JXZ was responsible for data analysis and manuscript drafting. QQZ was responsible for manuscript drafting and manuscript revision. HBS was responsible for study design, study supervision, manuscript drafting and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, GD., Ren, ZQ., Zhang, JX. et al. Effects of Diabetes Mellitus and Admission Glucose in Patients Receiving Mechanical Thrombectomy: A Systematic Review and Meta-analysis. Neurocrit Care 29, 426–434 (2018). https://doi.org/10.1007/s12028-018-0562-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0562-4