Abstract
Background and purpose
Clinical outcome after endovascular thrombectomy in patients with acute ischemic stroke still varies significantly. Higher blood glucose levels (BGL) have been associated with worse clinical outcome, but the pathophysiological causes are not yet understood. We hypothesized that higher levels of BGL are associated with more pronounced ischemic brain edema and worse clinical outcome mediated by cerebral collateral circulation.
Methods
178 acute ischemic stroke patients who underwent mechanical thrombectomy were included. Early ischemic brain edema was determined using quantitative lesion water uptake on initial computed tomography (CT) and collateral status was assessed with an established 5-point scoring system in CT-angiography. Good clinical outcome was defined as functional independence (modified Rankin Scale [mRS] score 0–2). Multivariable logistic regression analysis was performed to predict functional independence and linear regression analyses to investigate the impact of BGL and collateral status on water uptake.
Results
The mean BGL at admission was significantly lower in patients with good outcome at 90 days (116.5 versus 138.5 mg/dl; p < 0.001) and early water uptake was lower (6.3% versus 9.6%; p < 0.001). The likelihood for good outcome declined with increasing BGL (odds ratio [OR] per 100 mg/dl BGL increase: 0.15; 95% CI 0.02–0.86; p = 0.039). Worse collaterals (1% water uptake per point, 95% CI 0.4–1.7%) and higher BGL (0.6% per 10 mg/dl BGL, 95% CI 0.3–0.8%) were significantly associated with increased water uptake.
Conclusion
Elevated admission BGL were associated with increased early brain edema and poor clinical outcome mediated by collateral status. Patients with higher BGL might be targeted by adjuvant anti-edematous treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endovascular thrombectomy is of benefit to patients with acute ischemic stroke caused by a large vessel occlusion in the anterior circulation [9]. Despite substantial improvements in clinical outcomes as demonstrated by the recent prospective trials, there is still a relevant number of patients who do not experience good functional outcome even after successful vessel recanalization [40]. Therefore, the early identification of factors associated with poor outcome is of importance for treatment selection, but especially for further potential targets of adjuvant treatment options [11, 17, 32,33,34].
Elevated levels of blood glucose are well known to be linked with poor clinical outcome [16, 25,26,27, 41]. In a recently published meta-analysis, higher admission blood glucose levels were associated with unfavorable functional outcome [16]. Animal studies suggested that hyperglycemia accelerates the transformation of ischemic penumbra into infarction and leads to larger infarcts [18, 19]. Yet, the pathophysiological mechanisms for this association remain to be determined. Altered blood–brain barrier permeability or increased lactic acid production in the ischemic tissue have been discussed as pathophysiological causes [16]. Recently, higher blood glucose has been described as a baseline predictor for early cerebral edema; however, in this study, edema was only estimated using a visual three-step approach, which primarily rated infarct size [41]. Nevertheless, this study introduced elevated early brain edema as one explanatory factor, whose pathophysiology is not yet entirely understood and matter of the current debate [5]. As edema can lead to severe complications within the first days after stroke onset, with mortality up to 80%, identifying possible risk factors or mediators for early edema formation could lead to important clinical implications and might be targeted by advanced treatment strategies [10].
The purpose of this study was to investigate the relationship of BGL and early brain edema using lesion water uptake as quantitative imaging biomarker. Elevated levels of water uptake using this biomarker have been reported to predict malignant infarctions [3]. As the impact of blood glucose levels on clinical outcome might be mediated by the collateral profile as recently observed, we analyzed this parameter as a important covariable and possible link between brain edema and clinical outcome.
Methods
Patients
We retrospectively analyzed acute ischemic stroke patients with large vessel occlusion of the middle cerebral artery territory admitted between February 2015 and May 2018 at the local university high-volume tertiary stroke center. Anonymized data were recorded in accordance with ethical review board approval and institutional review board waived informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request. The a priori defined inclusion criteria were: (1) acute ischemic stroke with large vessel occlusion of the distal internal carotid artery or middle cerebral artery (MCA) confirmed by multimodal CT on admission (non-enhanced CT [NECT], CT angiography [CTA], and CT perfusions [CTP]) within 6 h from symptom onset; (2) visually evident early infarct lesion as indicated by ischemic hypoattenuation in admission NECT and/or perfusion lesion with reduced cerebral blood volume [CBV] in CTP; (3) subsequently performed endovascular procedure with documented Thrombolysis In Cerebral Infarctions (TICI) score; (4) documented time from symptom onset to imaging and National Institute of Health Stroke Scale (NIHSS) score; (5) absence of intracranial hemorrhage and preexisting infarctions in admission NECT. Baseline clinical characteristics and demographic information were deducted from the medical records, including time from onset to admission and blood glucose at admission, as well as anti-diabetic medication including insulin. A history of diabetes mellitus was retrieved from clinical documentation. Functional outcome was extracted from the registry using modified Rankin Scale (mRS) scores after 90 days.
Imaging
Patients received a comprehensive stroke imaging protocol by multimodal CT at admission with NECT and CTA and additional CTP in equal order on an iCT 256™ scanner (Philips Healthcare, Best, The Netherlands). NECT: collimation 64 × 0.625, pitch 0.297, rotation time 0.4 s, field of view (FOV) 270 mm, tube voltage 120 kV, tube current 300 mA, 4.0 mm slice reconstruction. CTA: collimation 64 × 0.625, pitch 0.985, rotation time 0.4 s, FOV 220 mm, tube voltage 120 kV, 300 mAs, 2.0 mm slice reconstruction, 5 mm maximum intensity projection (MIP) reconstruction with 1 mm increment. CTP: collimation 64 × 1.25, rotation time 0.5 s, FOV 220 mm, tube current 80 kV, tube current 140 mAs, 5 mm slice reconstruction, slice sampling rate 1.8 s, scan time 72 s, biphasic injection with 40 ml of highly iodinated contrast medium with 400 mM/ml injected with 6 ml/s followed by 40 ml NaCl chaser bolus. Perfusion datasets were inspected for quality and excluded in case of severe motion artifacts.
Image analysis
All CT imaging material was anonymized at an external imaging core lab for blinded analysis. We used a standardized procedure to quantify early net lesion water uptake (NWU) in the ischemic core lesion at the time of admission imaging as reported elsewhere [2, 3, 22, 23] using commercially available software (Analyze 11.0, Biomedical Imaging Resource, Mayo Clinic, Rochester, MN). This method of determining the volume of water uptake due to ischemic brain edema has initially been described as biomarker to estimate lesion age and has subsequently been validated extensively in further in vitro and in vivo studies [1, 2, 22]. It has specifically been demonstrated how hypoattenuation in CT is directly related to the volume of water uptake, and how this imaging biomarker may be used to precisely quantify ischemic edema [2, 3, 23].
Collateral status was assessed using an established 5-point scoring system by Souza et al. [39]. The rating was performed by an experienced neuroradiologist (GB; > 3 years) and verified by a second experienced neuroradiologist (UH; > 8 years). Intracranial CTA maximum intensity projections (MIPs) were used for grading: 0 = absent collaterals in > 50% of an MCA-M2 branch (superior or inferior division) territory; 1 = diminished collaterals in > 50% of an MCA-M2 branch territory; 3 = collaterals equal to the contralateral hemisphere; and 4 = increased collaterals [39]. Poor collaterals were defined as grade 0–2 and good collaterals as 3–4 according to Kim et al. [12]. Alberta Stroke Program Early CT Scores (ASPECTS) were deducted from the clinical documentations. In this context, the rating is regularly performed by an experienced neuroradiologist and verified by a second attending neuroradiologist. These scores were finally controlled for accuracy in a consensus reading (GB and UH). Image analysis was performed blinded to clinical data.
Statistical analysis
Continuous variables are presented as means or confidence intervals (CI) of means, standard deviations (SD) or medians and interquartile ranges (IQR). Kolmogorov–Smirnov tests were used to determine if the data sets were well-modeled by a normal distribution. Patients with good clinical outcome (mRS 0–2) were compared to patients with worse outcome (mRS 3–6) in Table 1 using Student t tests (normal distribution) or Mann–Whitney U tests (non-normal distribution). Moreover, patients below or above 140 mg/dl BGL were compared according to recent references [12, 20, 38].
The relationship of BGL on early edema (NWU in admission CT) was analyzed using multivariable linear regression adjusted for collateral status as important covariable, as well as ASPECTS, age, and NIHSS. Collateral status was examined as continuous variable and dichotomized into “poor” and “good” collaterals. The association of BGL on clinical outcome was analyzed using univariable and multivariable logistic regression analysis with backward selection adjusted for collateral score, age, NIHSS, ASPECTS, NWU, and recanalization status (Table 2). The dependent variable was functional independence (mRS 0–2). A three-dimension surface plot was created displaying the probability for functional independence for BGL and NWU separately for patients with poor (0–2) and good collaterals (3–4) based on multivariate logistic regression.
A two-way ANOVA analysis was performed with early ischemic brain edema as dependent variable and blood glucose (<140 mg/dl versus > 140 mg/dl) and collaterals (good versus poor collaterals) as dependent variables.
A statistically significant difference was accepted at a p-value of less than 0.05. Analyses were performed using MedCalc (version 11.5.1.0; Mariakerke, Belgium) and R (R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria, 2017).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Results
178 patients fulfilled all inclusion criteria and were analyzed. The median age was 76 (IQR 65–82) and 75 patients (43%) were women. In 34 patients, a known history of diabetes mellitus type 2 was deducted from medical documentation (19%). In these patients, the mean BGL at admission was significantly higher (164 mg/dl versus 126 mg/dl; p < 0.0001). 9 patients had subcutaneous insulin in their medication list, 6 patients with metformin, 5 patients with gliptins, and 1 patient with sulfonylurea. 136 patients (77%) received successful endovascular recanalization with TICI 2b/3. The main characteristics of patients are summarized in Table 1. Comparing patients with poor collaterals versus good collaterals, NWU was significantly higher in patients with poor collaterals (9.2% versus 6.8%; p = 0.02) and mRS was significantly higher in these patients (median 5 [IQR 2–6] versus 1.5 [IQR 1–4]; p < 0.001).
Impact of blood glucose on early ischemic brain edema
Patients with a history of diabetes had no significant difference in early formation of ischemic edema than patients without (Mean NWU 10.2% versus 8.3%; p = 0.08). When using BGL of 140 mg/dl as to differentiate two patient groups we found significant differences. The mean (SD) NWU for patients with BGL < 140 mg/dl was significantly lower than NWU in patients with BGL > 140 mg/dl (7.6% versus 11.3%; p < 0.001). Furthermore, patients with BGL < 140 mg/dl exhibited better collateral scores by trend: the median collateral score was 2 (IQR 1–3), which was higher than the collateral score in patients with BGL > 140 mg/dl: 1; IQR 1–3; p = 0.06). In multivariate linear regression analysis, the association of BGL on NWU was assessed adjusted for ASPECTS, collaterals, NIHSS, and age. For every 10 mg/dl increase in BGL, NWU significantly increased by 0.43% (95% CI 0.21–0.65; p < 0.001). An increase in collateral score by 1 point was significantly associated with a lowered NWU of 1% (95% CI 0.3–1.7%; p = 0.03), adjusted for BGL and age (Fig. 2).
After dichotomization into patients with poor versus good collaterals, a 10 mg/dl increase in BGL in patients with good collaterals was significantly associated with a NWU increase of 4.7% (95% CI 1.7–8.2; p = 0.01). The same BGL increase in patients with poor collaterals resulted in a 3.9% increase in NWU, 95% CI 1.1–6.8%; p = 0.007). In the two-way ANOVA, patients with good collaterals did not offer significant group differences when comparing low and high blood glucose (cut off 140 mg/dl). In patients with good collaterals and low blood glucose, the mean NWU was 5.7% (95% CI 3.9–7.5%) versus 9.6% in patients with good collaterals and high blood glucose (95% CI 6.8–12.4%). In patients with poor collaterals, however, there was a significant difference in NWU according to blood glucose. The mean NWU was 11.4% (95% CI 9.7–13.1%) in patients with poor collaterals and high blood glucose and 7.8% (95% CI 6.6–9.1%) in patients with poor collaterals and low blood glucose.
Prediction of clinical outcome
The median mRS after 90 days was 4 (IQR 2–5) both for patients with or without history of diabetes (p = 0.8). 52 patients (30%) exhibited functional independence (mRS 0–2). Comparing patients with functional independence and patients with mRS 3–6, the mean BGL was lower in patients with functional independence (118 mg/dl versus 141 mg/dl; p < 0.001).
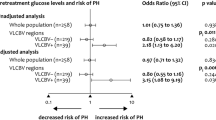
(Fig. 1), early NWU was lower (6.1% versus 9.7%; p < 0.001), and the median collateral score was higher (2, IQR 2–3 versus 2, IQR 1–2; p < 0.001).
Univariate and multivariate logistic regression analysis was performed to predict good outcome (mRS 0–2) using BGL, collateral score, NIHSS, age, NWU, recanalization status and ASPECTS as independent variables (see Table 2). The remaining independent variables in multivariate model were age, NIHSS, collateral score, and BGL (Figs. 2, 3). Higher BGL significantly reduced the likelihood of good outcome (odds ratio (OR) 0.15 for 100 mg/dl increase in BGL; 95% CI 0.02–0.80; p = 0.039), and a higher collateral score increased the likelihood for good outcome (per 1-point increase; OR 1.6; 95% CI 1.0–2.5; p = 0.04). Both increasing age (per 1 year; OR 0.95; 95% CI 0.91–0.99; p < 0.01) and increasing NIHSS (per 1-point increase; OR 0.87; 95% CI 0.78–0.96; p < 0.01) reduced the likelihood for good outcome.
Impact of blood glucose levels on early ischemic edema and clinical outcome. a Multivariate linear regression analysis to display the impact of blood glucose (x-axis) on ischemic brain edema (NWU, y-axis) depending on collateral score (good collateral status 3–4 versus poor collateral status 0–2), adjusted for age. B: Impact of blood glucose (x-axis) on functional outcome (probability for modified Rankin scale score 0–2 after 90 days, y-axis) based on multivariate logistic regression analysis adjusted for collateral status, ASPECTS, age, NIHSS, and early water uptake
3D-Surface plot illustrating the impact of early brain edema and blood glucose on clinical outcome. Impact of blood glucose (x-axis) and early ischemic brain edema (z-axis) on probability for good clinical outcome based on modified Rankin scale scores 0–2 after 90 days, separated by collateral score (good collaterals on the left side, poor collaterals on the right side)
Discussion
The aim of this study was to investigate the relationship of blood glucose and early ischemic brain edema at admission and its impact on clinical outcome in ischemic stroke patients. The main finding of this study was that increasing blood glucose was significantly associated with higher early brain edema, assessed using quantitative lesion water uptake and worse functional outcome with collateral status as important covariable.
Our findings are in accordance with a recently published study describing the impact of higher BGL on outcome [12]. The authors concluded that the effect of BGL on outcome depended on collateral status and was less significant for patients with poor collaterals [26]. However, the reasons for this phenomenon remained unknown. In the present study, we observed an interrelation between higher BGL, poor collaterals, and pronounced early ischemic edema that may result in poor clinical outcome even despite successful vessel recanalization. While patients with poor collaterals showed higher degree of early brain edema, the impact of increasing BGL on early brain edema was by trend higher in patients with good collaterals. The development of brain edema caused by hyperglycemia might, therefore, be more alterable in patients with good collaterals and this might be a strategy for adjuvant treatment with anti-edematous drugs [8, 33, 35].
The potential interaction between blood glucose, collateral status, and brain edema still requires further investigation. These factors are known independent predictors of poor outcome, but its relationship has not been described yet. Metabolic factors have been observed to be associated with collateral status [21]. Hyperglycemia could potentially reduce the recruitment of new collateral channels after acute arterial occlusion [21]. Poor collaterals, however, relate to an increased degree of ischemic edema and elevated edema might again increase interstitial pressure, which increases the resistance of collateral arterioles and downstream perforating arterioles [8, 29]. This vicious cycle may significantly contribute to aggravated clinical outcome. Therefore, the incorporation of these factors in diagnosis might improve the acute triage of stroke patients, could be used as criteria to select patients with uncertain indication for endovascular thrombectomy (e.g. low ASPECTS, or very elderly patients), and be tested as target of adjuvant treatment [4, 24]. Patients presenting with good collaterals and manifest elevated BGL might particularly profit from lowering blood sugar. Patients with poor collaterals, however, might rather profit from anti-edematous drugs such as glyburide [13, 32, 33]. Glyburide is an inhibitor of the sulfonylurea receptor 1 and transient receptor potential melastatin 4 (SUR1-TRPM4). This receptor exists for instance in pancreatic beta cells and brain tissue [15, 28, 31]. The application of glyburide has been reported to be safe and feasible and was introduced as a novel therapy for preventing edematous brain swelling [33, 34, 37]. The inhibition of SUR1-TRPM4 leads to depolarization of cell membranes opening voltage-depending calcium channels. An increased intracellular calcium in pancreatic beta cells then stimulates insulin release [31]. In ischemic brain during acute stroke, a setting of ATP depletion results in SUR1 upregulation and subsequent tissue swelling as well as the formation of brain edema [14]. In preclinical studies using rodent models with malignant cerebral edema, selective inhibition of SUR1 resulted in decreased infarct volume, reduced mortality, and better neurological function [34, 37]. Supporting these preclinical data, retrospective analyses involving patients with diabetes mellitus and acute ischemic stroke concluded that patients who took sulfonylurea drugs have shown significantly improved clinical outcomes with less hemorrhagic transformation [14, 35]. In our patients cohort only one patient had glyburide in his medication list. This patient exhibited a low NWU of only 1.3% (mean NWU of all patients: 9.0%; 95% CI 8.1–9.8%) measured after a time from onset to imaging of 3.8 h despite poor collateral score (1) and higher BGL (231 mg/dl).
It is important to realize that the application of antidiabetic drugs or insulin in prior clinical trials did not improve functional outcome [30, 36], although previous animal studies often showed promising results [36]. In contrast to clinical trials, > 80% of preclinical studies examined the specific drug in rodent models in combination with complete reperfusion. Acknowledging the low recanalization rates in patients with large vessel occlusion and intravenous lysis (10-33%), the disappointing results of several clinical trials testing adjuvant treatment options are comprehensible [6, 36]. Therefore, future clinical trials might combine reperfusion with further adjuvant treatment in patients with hyperglycemia. Nevertheless, future research is needed to affirm these findings using blood sugar analyses over time with multiple BGL tests.
Yet, there is no established method to monitor potential effects on ischemic brain edema after application of anti-edema drugs such as glyburide. Quantitative NWU might serve as imaging biomarker to measure effects of these drugs in prospective trials. This method is based on prior theoretical, in vitro, and clinical in vivo studies that demonstrated the linear relationship between hypoattenuation of an infarct lesion to its relative volume increase due to edema [1, 2, 22, 23]. Moreover, there is prior independent data that show how the method of calculating water uptake by CT density can be universally applied to histopathological gold standard measurement of volume of water uptake. Dzialowski et al. measured changes in density after onset of vessel occlusion in rats and correlated these measurements with histological determination of %-water content change (wet–dry method). Their findings are in line with the lately published studies on CT water uptake measurements [7].
To our knowledge, the present study is the first study that investigated the relationship of BGL, collaterals status, and early ischemic edema using a quantitative imaging biomarker. The results are in accordance with a recent exploratory pilot study discussing blood glucose as potential cause of early ischemic brain edema [5]. A lately published paper involving 42,187 patients observed that elevated BGL was an important predictor for early ischemic edema, but these findings were only based on visual rating primarily describing infarct size [41].
Limitations of our study include the relatively small number of patients due to strict inclusion and exclusion criteria. Second, this was a retrospective analysis and requires further prospective validation. Furthermore, poststroke hyperglycemia is a dynamic process, and one isolated blood glucose value may not be sufficient to capture the whole complexity of ischemic brain. Hb1Ac values were not available in the present study, as they are not part of the routine laboratory. Future studies could investigate the relationship of brain edema with Hb1Ac levels to more precisely distinguish between manifest diabetes and temporary BGL increase. The different time interval from last ingestion was unknown which might affect comparability of patient individual BGL. Nevertheless, using admission BGL is well established in literature and used in prior studies [12, 16].
Conclusion
Our study confirmed that higher levels of blood glucose reduced the likelihood for functional independence adjusted for baseline clinical parameter and treatment. Early cerebral brain edema may be the link between elevated BGL and poor outcome with collateral status as important covariable. Quantification of early ischemic edema might be used to monitor treatment effects of adjuvant anti-edematous treatment, such as glyburide.
References
Broocks G, Faizy TD, Flottmann F, Schon G, Langner S, Fiehler J, Kemmling A, Gellissen S (2018) Subacute infarct volume with edema correction in computed tomography is equivalent to final infarct volume after ischemic stroke: improving the comparability of infarct imaging endpoints in clinical trials. Investig Radiol 53:472–476
Broocks G, Flottmann F, Ernst M, Faizy TD, Minnerup J, Siemonsen S, Fiehler J, Kemmling A (2018) Computed tomography-based imaging of voxel-wise lesion water uptake in ischemic brain: relationship between density and direct volumetry. Investig Radiol 53:207–213
Broocks G, Flottmann F, Scheibel A, Aigner A, Faizy TD, Hanning U, Leischner H, Broocks SI, Fiehler J, Gellissen S, Kemmling A (2018) Quantitative lesion water uptake in acute stroke computed tomography is a predictor of malignant infarction. Stroke 49:1906–1912
Broocks G, Hanning U, Flottmann F, Schoenfeld M, Faizy T, Sporns P, Baumgart M, Leischner H, Schoen G, Minnerup J, Thomalla G, Fiehler J, Kemmling A (2019) Clinical benefit of thrombectomy in stroke patients with low ASPECTS is mediated by edema reduction. Brain 142:1399–1407
Broocks G, Kemmling A, Aberle J, Kniep H, Bechstein M, Flottmann F, Leischner H, Faizy TD, Nawabi J, Schon G, Sporns P, Thomalla G, Fiehler J, Hanning U (2019) Ischemic lesion water uptake in acute stroke: is blood glucose related to cause and effect? J Stroke 21:347–349
Campbell BCV, Mitchell PJ, Churilov L, Yassi N, Kleinig TJ, Dowling RJ, Yan B, Bush SJ, Dewey HM, Thijs V, Scroop R, Simpson M, Brooks M, Asadi H, Wu TY, Shah DG, Wijeratne T, Ang T, Miteff F, Levi CR, Rodrigues E, Zhao H, Salvaris P, Garcia-Esperon C, Bailey P, Rice H, de Villiers L, Brown H, Redmond K, Leggett D, Fink JN, Collecutt W, Wong AA, Muller C, Coulthard A, Mitchell K, Clouston J, Mahady K, Field D, Ma H, Phan TG, Chong W, Chandra RV, Slater LA, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Bladin CF, Sharma G, Desmond PM, Parsons MW, Donnan GA, Davis SM, Investigators E-IT (2018) Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med 378:1573–1582
Dzialowski I, Klotz E, Goericke S, Doerfler A, Forsting M, von Kummer R (2007) Ischemic brain tissue water content: CT monitoring during middle cerebral artery occlusion and reperfusion in rats. Radiology 243:720–726
Galego O, Jesus-Ribeiro J, Baptista M, Sargento-Freitas J, Martins AI, Silva F, Santos GC, Cunha L, Nunes C, Machado E (2018) Collateral pial circulation relates to the degree of brain edema on CT 24 hours after ischemic stroke. Neuroradiol J 31:456–463
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millan M, Davis SM, Roy D, Thornton J, Roman LS, Ribo M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, Collaborators H (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731
Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R (1996) 'Malignant' middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol 53:309–315
Hill MD, Martin RH, Mikulis D, Wong JH, Silver FL, Terbrugge KG, Milot G, Clark WM, Macdonald RL, Kelly ME, Boulton M, Fleetwood I, McDougall C, Gunnarsson T, Chow M, Lum C, Dodd R, Poublanc J, Krings T, Demchuk AM, Goyal M, Anderson R, Bishop J, Garman D, Tymianski M, Investigators Et (2012) Safety and efficacy of NA-1 in patients with iatrogenic stroke after endovascular aneurysm repair (ENACT): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet Neurol 11:942–950
Kim JT, Liebeskind DS, Jahan R, Menon BK, Goyal M, Nogueira RG, Pereira VM, Gralla J, Saver JL (2018) Impact of hyperglycemia according to the collateral status on outcomes in mechanical thrombectomy. Stroke 49:2706–2714
Kimberly WT, Battey TW, Pham L, Wu O, Yoo AJ, Furie KL, Singhal AB, Elm JJ, Stern BJ, Sheth KN (2014) Glyburide is associated with attenuated vasogenic edema in stroke patients. Neurocrit Care 20:193–201
Kunte H, Schmidt S, Eliasziw M, del Zoppo GJ, Simard JM, Masuhr F, Weih M, Dirnagl U (2007) Sulfonylureas improve outcome in patients with type 2 diabetes and acute ischemic stroke. Stroke 38:2526–2530
Liu R, Wang H, Xu B, Chen W, Turlova E, Dong N, Sun CL, Lu Y, Fu H, Shi R, Barszczyk A, Yang D, Jin T, Mannucci E, Feng ZP, Sun HS (2016) Cerebrovascular safety of sulfonylureas: the role of KATP channels in neuroprotection and the risk of stroke in patients with type 2 diabetes. Diabetes 65:2795–2809
Lu GD, Ren ZQ, Zhang JX, Zu QQ, Shi HB (2018) Effects of diabetes mellitus and admission glucose in patients receiving mechanical thrombectomy: a systematic review and meta-analysis. Neurocrit Care 29:426–434
Malhotra K, Ahmed N, Filippatou A, Katsanos AH, Goyal N, Tsioufis K, Manios E, Pikilidou M, Schellinger PD, Alexandrov AW, Alexandrov AV, Tsivgoulis G (2019) Association of elevated blood pressure levels with outcomes in acute ischemic stroke patients treated with intravenous thrombolysis: a systematic review and meta-analysis. J Stroke 21:78–90
Mandava P, Martini SR, Munoz M, Dalmeida W, Sarma AK, Anderson JA, Fabian RH, Kent TA (2014) Hyperglycemia worsens outcome after rt-PA primarily in the large-vessel occlusive stroke subtype. Transl Stroke Res 5:519–525
Martini SR, Kent TA (2007) Hyperglycemia in acute ischemic stroke: a vascular perspective. J Cereb Blood Flow Metab 27:435–451
Mayfield J (1998) Diagnosis and classification of diabetes mellitus: new criteria. Am Fam Physician 58(1355–1362):1369–1370
Menon BK, Smith EE, Coutts SB, Welsh DG, Faber JE, Goyal M, Hill MD, Demchuk AM, Damani Z, Cho KH, Chang HW, Hong JH, Sohn SI (2013) Leptomeningeal collaterals are associated with modifiable metabolic risk factors. Ann Neurol 74:241–248
Minnerup J, Broocks G, Kalkoffen J, Langner S, Knauth M, Psychogios MN, Wersching H, Teuber A, Heindel W, Eckert B, Wiendl H, Schramm P, Fiehler J, Kemmling A (2016) Computed tomography-based quantification of lesion water uptake identifies patients within 4.5 hours of stroke onset: A multicenter observational study. Ann Neurol 80:924–934
Nawabi J, Flottmann F, Hanning U, Bechstein M, Schoen G, Kemmling A, Fiehler J, Broocks G (2018) Futile recanalization with poor clinical outcome is associated with increased edema volume after ischemic stroke. Invest Radiol 54:282–287
Nikneshan D, Raptis R, Pongmoragot J, Zhou L, Johnston SC, Saposnik G, Investigators of the Registry of the Canadian Stroke N, Stroke Outcomes Research Canada Working G (2013) Predicting clinical outcomes and response to thrombolysis in acute stroke patients with diabetes. Diabetes Care 36:2041–2047
Ntaios G, Egli M, Faouzi M, Michel P (2010) J-shaped association between serum glucose and functional outcome in acute ischemic stroke. Stroke 41:2366–2370
Osei E, den Hertog HM, Berkhemer OA, Fransen PS, Roos YB, Beumer D, van Oostenbrugge RJ, Schonewille WJ, Boiten J, Zandbergen AA, Koudstaal PJ, Dippel DW, Investigators MCp (2016) Increased admission and fasting glucose are associated with unfavorable short-term outcome after intra-arterial treatment of ischemic stroke in the MR CLEAN pretrial cohort. J Neurol Sci 371:1–5
Osei E, Fonville S, Zandbergen AAM, Koudstaal PJ, Dippel DWJ, den Hertog HM (2018) Impaired fasting glucose is associated with unfavorable outcome in ischemic stroke patients treated with intravenous alteplase. J Neurol 265:1426–1431
Parkinson FE, Hatch GM (2016) Is there enhanced risk of cerebral ischemic stroke by sulfonylureas in type 2 diabetes? Diabetes 65:2479–2481
Rocha M, Jovin TG (2017) Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke 48:2621–2627
Rosso C, Corvol JC, Pires C, Crozier S, Attal Y, Jacqueminet S, Deltour S, Multlu G, Leger A, Meresse I, Payan C, Dormont D, Samson Y (2012) Intensive versus subcutaneous insulin in patients with hyperacute stroke: results from the randomized INSULINFARCT trial. Stroke 43:2343–2349
Serrano-Martin X, Payares G, Mendoza-Leon A (2006) Glibenclamide, a blocker of K+(ATP) channels, shows antileishmanial activity in experimental murine cutaneous leishmaniasis. Antimicrob Agents Chemother 50:4214–4216
Sheth KN, Elm JJ, Beslow LA, Sze GK, Kimberly WT (2016) Glyburide advantage in malignant edema and stroke (GAMES-RP) trial: rationale and design. Neurocrit Care 24:132–139
Sheth KN, Elm JJ, Molyneaux BJ, Hinson H, Beslow LA, Sze GK, Ostwaldt AC, Del Zoppo GJ, Simard JM, Jacobson S, Kimberly WT (2016) Safety and efficacy of intravenous glyburide on brain swelling after large hemispheric infarction (GAMES-RP): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol 15:1160–1169
Sheth KN, Kimberly WT, Elm JJ, Kent TA, Mandava P, Yoo AJ, Thomalla G, Campbell B, Donnan GA, Davis SM, Albers GW, Jacobson S, Simard JM, Stern BJ (2014) Pilot study of intravenous glyburide in patients with a large ischemic stroke. Stroke 45:281–283
Sheth KN, Kimberly WT, Elm JJ, Kent TA, Yoo AJ, Thomalla G, Campbell B, Donnan GA, Davis SM, Albers GW, Jacobson S, del Zoppo G, Simard JM, Stern BJ, Mandava P (2014) Exploratory analysis of glyburide as a novel therapy for preventing brain swelling. Neurocrit Care 21:43–51
Shi L, Rocha M, Leak RK, Zhao J, Bhatia TN, Mu H, Wei Z, Yu F, Weiner SL, Ma F, Jovin TG, Chen J (2018) A new era for stroke therapy: Integrating neurovascular protection with optimal reperfusion. J Cereb Blood Flow Metab. https://doi.org/10.1177/0271678X18798162
Simard JM, Chen M, Tarasov KV, Bhatta S, Ivanova S, Melnitchenko L, Tsymbalyuk N, West GA, Gerzanich V (2006) Newly expressed SUR1-regulated NC(Ca-ATP) channel mediates cerebral edema after ischemic stroke. Nat Med 12:433–440
Somannavar S, Ganesan A, Deepa M, Datta M, Mohan V (2009) Random capillary blood glucose cut points for diabetes and pre-diabetes derived from community-based opportunistic screening in India. Diabetes Care 32:641–643
Souza LC, Yoo AJ, Chaudhry ZA, Payabvash S, Kemmling A, Schaefer PW, Hirsch JA, Furie KL, Gonzalez RG, Nogueira RG, Lev MH (2012) Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol 33:1331–1336
Sporns PB, Minnerup J, Warneke N, Dziewas R, Hanning U, Berkemeyer S, Zoubi T, Heindel W, Schwindt W, Niederstadt T (2017) Impact of the implementation of thrombectomy with stent retrievers on the frequency of hemicraniectomy in patients with acute ischemic stroke. Clin Neuroradiol 27:193–197
Thoren M, Azevedo E, Dawson J, Egido JA, Falcou A, Ford GA, Holmin S, Mikulik R, Ollikainen J, Wahlgren N, Ahmed N (2017) Predictors for cerebral edema in acute ischemic stroke treated with intravenous thrombolysis. Stroke 48:2464–2471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Prof. Fiehler: Research support: German Ministry of Science and Education (BMBF and BMWi), German Research Foundation (DFG), European Union (EU), Hamburgische Investitions- und Förderbank (IFB), Medtronic, Microvention, Philips, Stryker, Consultant for: Acandis, Boehringer Ingelheim, Cerenovus, Covidien, Evasc Neurovascular, MD Clinicals, Medtronic, Medina, Microvention, Penumbra, Route92, Stryker, Transverse Medical. Prof. Thomalla: Consultant for Acandis, Bayer Healthcare, Boehringer Ingelheim, BristolMyersSquibb/Pfizer, Covidien, Glaxo Smith Kline; lead investigator of the WAKE-UP study; Principal Investigator of the THRILL study; Grants by the European Union (Grant No. 278276 und 634809) and Deutsche Forschungsgemeinschaft (SFB 936, Projekt C2). All author authors report no disclosures.
Ethical approval
Anonymized data were recorded in accordance with ethical review board approval and institutional review board waived informed consent. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Rights and permissions
About this article
Cite this article
Broocks, G., Kemmling, A., Aberle, J. et al. Elevated blood glucose is associated with aggravated brain edema in acute stroke. J Neurol 267, 440–448 (2020). https://doi.org/10.1007/s00415-019-09601-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09601-9