Abstract
Glioblastoma multiform (GBM) is a primary malignant brain tumor with a few therapeutic targets available for it. The interaction between the immune system and glioma is an important factor that could lead to novel therapeutic approaches to fight glioma. In this study, we investigated in vitro anti-inflammatory and apoptotic activity of atorvastatin in different concentrations 1, 5, and 10 μM on glioma spheroid cells cultured in a three-dimensional model in fibrin gel that indicate the complex in vivo microenvironment better than a simple two-dimensional cell culture. A mechanistic insight into the role of IL-17RA, TRAF3IP2, and apoptotic genes in progression of glioma could provide an important way for therapy of malignant tumors with manipulation of this inflammatory axis. To reach for these aims, after 24 and 48 h exposure with different concentrations of atorvastatin, caspase-8, caspase-3, Bcl-2, TRAF3IP2, and IL-17RA gene expression were assayed. Terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling assay and cell cycle assay were used for evaluating the cell apoptosis and proliferation. The results showed that atorvastatin has anti-inflammatory and apoptotic effects against glioma spheroids. Atorvastatin induced the expression of caspase-3 and caspase-8 and downregulated the expression of Bcl-2, TRAF3IP2, and IL-17RA especially at 10 μM concentration. These effects are dose dependent. The most likely mechanisms are the inhibition of inflammation by IL-17RA interaction with TRAF3IP2 and NF-κB signaling pathway. Finally, these results suggest that atorvastatin could be used as an anti-cancer agent for glioblastoma treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiform (GBM), a highly malignant astrocytic tumor, is one of the most common primary malignant tumors of the central nervous system [1]. Despite many efforts to get over this aggressive disease with the use of surgery, radiation, and conventional chemotherapy, the median overall survival of patients with GBM is still just more than 1 year, mostly because of resistance to therapy [2]. Interferences that can prevent the development or slow the growth of these tumors are necessary. There are a few therapeutic targets for GBM, so the understanding of the molecular mechanisms of GBM progression is more important. The inflammatory microenvironment generally promotes malignant progression [3]. Studies have suggested a connection between inflammation and glioma. Absolutely, the survival, growth, and invasion of GBM cells are promoted by various inflammatory cytokines [4–6]. Understanding how the immune system and glioma interact with each other could lead to novel therapeutic approaches to fight glioma [7]. The microenvironment of glioblastoma is another factor that recently received more attention as a possible target for the development of a new and more efficient therapy [8, 9]. Numerous studies have evaluated the potentially preventive activity of anti-inflammatory drugs against tumors [10]. Statins, the 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase (HMGR) inhibitors, are increasingly known as anti-inflammatory agents [11]. Experimental evidences suggest that these agents have potent anti-inflammatory properties in vitro and in animal models. Also, recent clinical studies independent of the magnitude of lipid lowering provide evidence that in human, statin-mediated inhibition of inflammation affects clinical outcomes [12]. Clinical trials have shown a noticeable reduction in cardiovascular mortality in patients treated with statins [13–15]. Statins have been reported to have properties of suppression of the proinflammatory mediators such as TNF-α, IFN-γ, and iNOS [16]. Statins have also been shown to activate caspase proteases involved in programmed cell death. Studies show that statins cause cell death in tumor cells by activating caspase-3, caspase-8, and caspase-9 [17]. To survey the signal transduction mechanisms induced by statins in U87 glioma cells, we have chosen a lipid soluble statin, atorvastatin, because it has been shown that cell death were not able to induce by hydrophilic statins, whereas all hydrophobic ones were associated with apoptosis in endothelial cells [15]. Statins, such as atorvastatin, are known to exert lipid-lowering but also anti-inflammatory effects. Growth of solid tumors results in most cases in a hypoxic microenvironment and the release of various cytokines and growth factors, which together increase inflammation, angiogenesis in tumor stroma, and triggering signaling cascades that activate NF-kappa B and STAT3 that produces predominantly by a specific subset of T helper cells (Th cells), namely Th17 cells [18–20]. IL-17R (renamed IL-17RA), a first receptor for IL-17, was described with the discovery of IL-17 [21]. Among IL-17 receptors, IL-17RA is the cognate receptor for IL-17. IL-17RA by the binding of IL-17 is activated after that IL-17 signaling has been shown to induce various downstream pathways such as mitogen-activated protein kinase (MAPK) and nuclear factor-κB (NF-κB) pathways [22]. Recent studies have demonstrated that the adaptor protein NF-κB activator 1 (Act-1) plays an essential role in IL-17-dependent signaling [23, 24]. TRAF3IP2 (TRAF3 interacting protein 2) also known as (ACT1; CIKS; C6orf2; C6orf4; C6orf5; C6orf6; CANDF8; PSORS13) is a redox-sensitive cytoplasmic adapter protein and an upstream regulator of IKK/NF-κB and JNK/AP-1 and a mediator of various autoimmune and inflammatory diseases [25]. This gene product communicates with TRAF proteins (tumor necrosis factor receptor-associated factors) and either I-kappaB kinase or MAPK to activate either NF-κB or Jun kinase. Multiple members of the TNF-receptor-associated factor (TRAF) family including TRAF2, TRAF3, and TRAF5 have been implicated in TNF signaling; however, clarifying their functional roles has been complicated because of diverse heterotypic and homotypic interactions that can occur between members of this family [7, 23–25].
In this study, we investigated the in vitro anti-inflammatory and apoptotic activities of atorvastatin on glioma spheroid cells in a three-dimensional model in fibrin gel.
Materials and Methods
Reagents
Atorvastatin ([R-(R*, R*)-2-(4-fluorophenyl)-ß, δ-dihydroxy-5-(1-methylethyl)-3-phenyl-4-(phenylamino)-carbonyl]-1-h-pyrrole-1-heptanoic acid) was purchased from Sigma Aldrich and dissolved in sterile DMSO (Beyotime, Shanghai, China). The stock solution was 10 mM and diluted to 1, 5, and 10 μM concentrations with cell culture medium immediately before use. The final concentration of DMSO in any media did not exceed 0.1%.
Cell Culture
The human U87 human primary glioblastoma cell line (U87MG) was obtained from the Cell Bank of the Pasteur Institute, Iran. This cell line was cultured in DEMEM/F12 media (Gibco BRL-Life Technologies, Rockville, MD), supplemented with 10% fetal bovine serum (FBS) (Invitrogen), 100 U/ml penicillin and 100 μg/ml streptomycin (Sigma), and incubated in a humidified atmosphere containing 37 °C with 5% CO2. U87 glioma cells were used in the first five passages.
Glioma Spheroids in 3D Culture Medium
The U87 cell line was cultured in a non-adherent plate. Briefly, the cells were washed with PBS, added cell dissociation enzyme, and incubated at 37 °C for 2–5 min after that cell suspension was centrifuged and removed supernatant and cell pellet resuspended in 1 ml of complete growth medium. The cell suspension was transferred to a sterile non-adherent 8-well plate and incubated at 37 °C, 5% CO2, 95% humidity. Tumor spheroid formation was confirmed visually 4 days later, and after that glioma spheroids encapsulated in fibrin gel. To prepare the fibrin gel, 3 mg of fibrinogen (Sigma, USA) was dissolved in 1 ml M199 solution (Sigma, USA) and along with spheroids transferred to a 24-well culture dish. Afterward, 15 μl of a thrombin solution (120 U/ml in 1 M sodium buffer; Sigma, USA) and 50 μl of FBS were added to each well. The culture plates were placed at 37 °C for 1 h to form a 3D network structure. To investigate the effect of atorvastatin on inflammation, spheroids were then stimulated with 1, 5, and 10 μM concentrations of atorvastatin for 48 h.
Cell Proliferation Assay
Glioma spheroids were encapsulated in fibrin gel in 12-well culture plates. After 2 days that the spheroids were exposed to different concentrations of atorvastatin (1, 5, and 10 μM), they were resuspended in 1–2 ml of medium and counted using a hemocytometer.
Cell Death Detection
To detect apoptosis of treated tumor spheroid cells, terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling (TUNEL) assay was performed by using an in situ cell death detection kit (Roche, Mannheim, Germany) according to the manufacturer instructions at 48 h post treatment. Glioma spheroids were encapsulated in fibrin gel in 96-well flat-bottom microtiter plate and treated with atorvastatin at three concentrations of 1, 5, and 10 μM. Briefly, spheroids were washed and fixed in 4% (w/v) paraformaldehyde and were then washed in PBS, and stored in 70% ethanol at 4 °C overnight. After being washed with 10 mM Tris–HCl (pH 7.6), the spheroids were incubated in methanol containing 0.3% H2O2 for 10 min to quench endogenous peroxidase activity. These cells were then treated with proteinase K (Roche, 20 μg/ml in Tris buffer) at 37 °C for 30 min. The spheroids were then incubated in the TUNEL reaction mixture (450 μl of label solution and 50 μl of enzyme solution) at 37 °C for 60 min and then in horseradish peroxidase (Santa Cruz, Germany) solution for 30 min. The color reaction was developed in 3,30-diaminobenzidine (DAB, Roche; 0.5 μl DAB and 1.5 μl peroxide buffer) for 5–10 min. A set of cells was incubated in the absence of TUNEL as a negative control. With this procedure, apoptotic cell nuclei will be dark brown. The stained cells were observed under a light microscope (Olympus, Tokyo, Japan). Apoptotic cells were counted in each four groups.
MTT Assay
Cell viability was assessed by a microplate-based 3-(4,5-dimethylthia-zol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) cell viability assay. Glioma spheroids were encapsulated in fibrin gel in 96-multiwell culture plate and incubated for 24 h at 37 °C. Then, they were treated with different concentrations of atorvastatin (1, 5, and 10 μM) for 24 h. After incubation, MTT reagents (0.5 mg/ml) were added to the each well and the plates were in the dark at 37 °C for 4 h. At the end of the incubation, the medium was removed, the resulting formazan was dissolved in DMSO, and the optical density was measured at 570 nm using an ELISA plate reader.
Cell Cycle
Cell cycle analysis was executed using Propidium Iodide Flow Cytometry Kit (Abcam). Glioma spheroids in fibrin gel were cultured in the presence of 1, 5, and 10 μM atorvastatin at 37 °C and 5% CO2 for 2 days. Prepared spheroids were suspended in buffer (e.g., PBS + 2% FBS; PBS + 0.1% BSA) then washed and spun cells at 300×g for 5 min X2 resuspend at 3–6 × 106 cells/ml. Aliquot 500 ul cells were in a 15 ml polypropylene, V-bottomed tube and added 5 ml cold 70% ethanol dropwise while gently vortexing. If cells are not vortexed on addition to the ethanol, they will be fixed to each other in clumps. After that, fix cells for at least 1 h at 4 °C. Add 1 ml of propidium iodide (PI) staining solution (3.8 mM sodium citrate, 50μg/ml PI [Sigma, P 4170] in PBS) to cell pellet and mix well. Add 50 ul of RNase A stock solution (final concentration 0.5 μg/ml (Worthington Biochemicals, RASE LS005649, LS005650)) and incubate overnight (or at least 4 h) at 4 °C. Store samples at 4 °C until analyzed by flow cytometry.
Real-Time Polymerase Chain Reaction (PCR)
Total RNA from glioma spheroids was extracted using the RNeasy Mini Kit (Qiagen, Valencia, CA, USA), and reverse transcription was carried out with a Sensiscript Reverse Transcriptase Kit (Qiagen). Primers used for qPCR were as follows: sequences of the IL-17RA primer were used: forward primer, 5′-AATTTCCTTGTGCCTGACTGTGAG-3′; reverse primer, 5′-TCCACAGGGTGAAGCTCACAC-3′. Sequences of TRAF3IP2 primer were used: forward primer, 5′-CTTAGGGATACCGTGATGATAATCG-3′; reverse primer, 5′-GAACTCAATCTGCATCATTCGATG-3′, Sequences of Bcl2 primer were used: forward primer, 5′-AAAATACAACATCACAGAGGAAGTAGACTG-3′, reverse primer, 5′-TCAATCACGCGGAACACTTG-3′, Sequences of caspase-3 primer were used: forward primer, 5′-AAAAGCACTGGAATGACATCTCG-3′, reverse primer, 5′-GAAACATCACGCATCAATTCCAC-3′, Sequences of caspase-8 primer were used: forward primer, 5′-ACTGGATGATGACATGAACCTGC-3′, reverse primer, 5′-CCTCCCCTTTGCTGAATTCTTC-3′ and sequences of GAPDH primer were used: forward primer, 5′-TCGCCAGCCGAGCCA-3′, reverse primer, 5′-CCTTGACGGTGCCATGGAAT-3′. PCR was carried out in an 7300 real-time PCR System (Applied Biosystems, Carlsbad, CA, USA) based on specific cytokine primers and general SYBR green fluorescence detection for 10 min at 94 °C followed by 45 cycles of 15 s at 95 °C, 30 s at 60 °C, and 30 s at 72 °C. Total RNA was isolated from glioma spheroids and treated cells by using the RNeasy Mini Kit (Qiagen, Valencia, CA, USA) and was reverse transcribed to cDNA by using the ExScript RT Reagent Kit (Takara Bio Inc., Otsu, Japan), according to the manufacturers’ protocols. All PCR reactions were performed via the LightCycler System (Roche Diagnostics, Basel, Switzerland) with SYBR Premix DimerEraser (Takara Bio Inc.).
Statistical Analysis
Data was presented as means ± standard deviation (SD), one-way analysis of variance (ANOVA) was used to analyze differences between the treatments and control groups and a p value <0.05 was considered significant.
Results
Atorvastatin Suppresses the Growth of U87 Cells
After seeding, U87 cells were adherent within 3–5 h. In the 2D monolayer system, U87 cells formed 70–80% confluent cell after 2–3 days after plating in 25-cm2 tissue flasks (Fig. 1a), also gloma spheroids in fibrin gel were observed by using an inverted light microscope (Nikon Eclipse TE2000-S, Germany) (Fig. 1b, c).
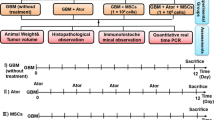
The effects of atorvastatin on cell growth were measured by cell proliferation assay in glioma spheroids; we performed dose-response studies in glioma spheroid form of U87 encapsulated in fibrin gel and the spheroids were treated with increasing concentrations of atorvastatin (1, 5, and 10 μM) for 48 h. Atorvastatin markedly inhibited proliferation of glioblastoma cells in a dose-dependent manner. As shown in Fig. 2a, atorvastatin significantly inhibited glioma spheroids proliferation in a dose-dependent manner (1, 5, and 10 μM) after 48 h of treatment (proliferation assay) proliferation was greatly reduced for glioma spheroids exposed to 10 μM concentration (Fig. 2). We found that atorvastatin obviously reduced spheroid size and pseudopodia following 48 h incubation. These results indicated the potential proliferation reducing effect of atorvastatin in glioblastoma for further analysis.
Atorvastatin inhibited proliferation. a Dose-dependent effect of atorvastatin on proliferation of glioma spheroids. Encapsulated glioma spheroids in fibrin were treated with 1, 5, and 10 μM concentrations of atorvastatin over a period of 48 h. At the indicated time point, spheroids were observed with inverted microscope. b The proliferation rate was inhibited by all concentrations, especially at 10 μM. Presenting data are mean ± SD of three identical experiments made in three replicates. (*p < 0.05; **p < 0.01; ***p < 0.001)
Atorvastatin Induces Cell Death in Human Glioma Spheroids
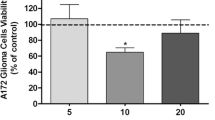
Previous studies have reported that statins can trigger a subset of tumor cells to undergo apoptosis [17]. Apoptosis in glioblastoma was detected by in situ end-labeling of nuclear DNA fragments (TUNEL) staining. To determine the apoptotic effect of atorvastatin, spheroids of glioblastoma cells in fibrin gel were treated with 1, 5, and 10 μM of atorvastatin for 72 h. TUNEL assay analysis of treated glioma spheroids confirmed the increased apoptosis in the treated group, especially at 10 μM of atorvastatin than in the other treated groups (Fig. 3a, b). The viability of glioma spheroids was measured by MTT assay in increasing doses of atorvastatin (1, 5, and 10 μM) after 48 h. We found that atorvastatin significantly reduced the viability of U87 cells in a dose-dependent manner (Fig. 3c).
Atorvastatin induced apoptosis. a Apoptotic index. The TUNEL technique revealed the specific apoptosis-induced DNA strand breaks and provided the percentages of positive cells. Cells were treated with different concentrations of atorvastatin for 48 h. Apoptotic nuclei and fragmented DNA appeared dark brown after staining. b Results are expressed as mean ± SEM (n = 3). ***p < 0.001 compared with control, error bars indicate SE. c Effect of atorvastatin on glioma spheroids viability. Glioma spheroids were treated with 1, 5, and 10 μM concentrations of atorvastatin for 48 h. The cell viabilities were determined by MTT assay. MTT assay showed that 10 μM atorvastatin inhibited proliferation more than other concentrations. Experiments were performed three times in triplicate. Data are presented as mean ± SD, scale bar:100µm
Effect of Atorvastatin on the Cell Cycle
A recent study analyzed the effects of atorvastatin on cell cycle on encapsulated glioma spheroids in fibrin gel. It was evaluated whether the marked inhibition of proliferation was due to an increase in cellular apoptosis or to a possible interference in the cell cycle in response to atorvastatin. For this purpose, glioma spheroids were treated with atorvastatin (1, 5, and 10 μM) for 48 h and then analyzed for cell cycle stage by flow cytometry. Different concentrations of atorvastatin (1, 5, and 10 μM) were able to interfere the cell cycle progression, arresting cells in the G0/G1 phase (Fig. 4), while leading to a significant decrease in the percentage of cells in G2/M phases. With regard to the group treated with atorvastatin, there was an increase in the percentage of apoptosis compared to the untreated group with atorvastatin (Fig. 4). The results show that atorvastatin significantly reduced proliferation at 48 h in a dose-dependent manner. Optimal concentration for atorvastatin was 10 μM.
Effect of atorvastatin on the cell cycle. Glioma spheroids were treated with atorvastatin (1, 5, and 10 μM) for 48 h and then analyzed for cell cycle stage by flow cytometry. The results show that atorvastatin significantly reduced proliferation at 48 h in a dose-dependent manner. Optimal concentration for atorvastatin was 10 μM. Values are the means ± SEM from three independent determinations. Significance compared with control, ***p < 0.001
Atorvastatin Leads to Expression of Related Apoptotic Genes in Glioma Spheroids
To understand the molecular mechanism by which atorvastatin regulates apoptosis, we examined the expression of apoptotic factors such as caspase-3 and caspase-8 and anti-apoptotic protein expression like Bcl-2 on glioma spheroids that were affected by atorvastatin. Real-time PCR analysis showed that the expression of caspase-3 and caspase-8 at the mRNA level were obviously higher in the treated groups with 10 μM than the levels in the other treated groups and the expression of Bcl-2 in the treated groups with 10 μM was lower than that in the other groups (Fig. 5). These results suggested that atorvastatin-induced cell apoptosis by downregulating the expression of Bcl-2 and upregulating the expression of caspase-3 and caspase-8.
Real-time PCR analysis of the mRNA levels of the proapoptotic genes (caspase-3 and capase-8), anti-apoptotic gen Bcl-2, and proinflammatory gens (IL-17RA and TRAF3IP2) in encapsulated glioma spheroid cells in fibrin gel that treated with atorvastatin in the different concentrations. Presenting data are mean ± SD of three identical experiments made in three replicates followed by normalization with GAPDH protein amount. (a p < 0.05; b p < 0.01; c p < 0.001)
Effect of Atorvastatin on TRAF3IP2 Expression a Regulatory or Proinflammatory Factor
Previously, studies showed TRAF3IP2, as an upstream regulator of the NF-κB and AP-1 pathways, encodes a protein involved in regulation of responses to cytokines by members of the Rel/NF-kappaB transcription factor family. These factors play a central role in innate immunity in response to pathogens, inflammatory signals, and stress. To analyze in detail the reduction of inflammation in giloma spheroids after treatment with atorvastatin, we assessed TRAF3IP2 mRNA expression by real-time PCR. Our results indicated that atorvastatin significantly reduced TRAF3IP2 after 48 h in a dose-dependent manner. Optimal concentration for atorvastatin was 10 μM. To study the possible inhibitory effect of atorvastatin, we cultured glioma spheroid cells that encapsulated in fibrin gel with different concentrations of atorvastatin for 48 h (Fig. 5). The inflammatory gene of treated glioma spheroids was lower than untreated glioma spheroids. Of note, treatment with atorvastatin inhibited the inflammatory response, and 10 μM was more effective than other concentrations. This result showed that atorvastatin is efficient to downregulate Nf-κB signaling of U87 cells in 3D modeling of glioblastoma.
Atorvastatin Decreases the Expression of IL-17RA in Glioma Spheroids
IL-17A exerts its protumorigenic activity through its type A receptor (IL-17RA). IL-17RA engagement activates NF-κB signaling and promotes the proliferation of tumorigenic [26]. To investigate whether atorvastatin modulate IL-17RA in glioblastoma, the human glioma spheroids cells in a three-dimensional model in fibrin gel were used as a model and were stimulated with 1-, 5-, and 10-μM doses of atorvastatin for 48 h. To analyze in detail the reduction of IL-17RA in glioblastoma after treatment, we assessed IL-17RA mRNA expression by qRT-PCR. As shown in Fig. 5, the qRT-PCR assay revealed that 48-h stimulation with different concentrations of atorvastatin make a significant decrease in IL-17RA mRNA expression, whereas the strongest inhibition of IL-17RA was achieved with atorvastatin in 10 μM concentration (Fig. 5).
Discussion
Statin drugs were used for hypercholesterolaemia but recently many studies show that they have more potential for cancer treatments [26]. Recent findings in some cancers such as osteosarcoma and non-small-cell-lung carcinomas (NSCLCs) have shown that atorvastatin has anti-tumor effects [27–30]. Effective anti-glioblastoma therapy should prevent proliferation and inhibit tumor cell growth of cancer cells [31]. In short, atorvastatin is a potential chemopreventive agent for glioblastoma that can induce U87 glioblastoma cell apoptosis and inhibit inflammation, but the molecular mechanisms through which atorvastatin affects glioblastoma cells remain unclear. To survey the mechanisms of apoptosis and anti-inflammatory effects of atorvastatin in U87 glioblastoma cells, we investigated the influence of atorvastatin on the crucial proteins associated with apoptosis and inflammation. Three-dimensional systems have the ability to mimic tumor-like microenvironment and this suggests the potential of engineered tumor models for drug testing [32]. The present study developed a simple in vitro cell model that can also be applied to evaluate the effect of atorvastatin on the glioma cell line. Recent studies have shown that inhibitors of HMG-CoA reductase decrease cell migration and invasiveness in several cancers including glioma [33–36]. The anti-tumor effects may include cytotoxicity [29], induction of apoptosis [37], and inhibitory effects on MMPs [36, 38]. Lastly, there has been considerable interest to develop novel pharmacologic inhibitors of NF-κB and STAT3 for glioma treatment [39, 40]. Our data showed that numbers of TUNEL positive cells are significantly increased in atorvastatin groups. The present study demonstrates the apoptotic potency and anti-inflammatory effect of atorvastatin. We found that atorvastatin induced apoptosis of U87 cells in an increasing trend, but with treatment of atorvastatin, the percentage of total apoptosis increased more significantly compared with that of the untreated group (p > 0.001). In addition, certain studies have previously noticed that atorvastatin induced cell apoptosis in different cancer cell lines [17], which is consistent with the results of our study. According to the results of the present study, atorvastatin downregulated the expression of Bcl-2 and upregulated the expression of caspase-3 and the caspase-8, which indicated that these proteins are involved in the atorvastatin-triggered apoptosis in U87cells. Caspases are key factors in the execution of apoptosis [41]. In this study, atorvastatin significantly increased caspase-3 mRNA expression observed 48 h after exposure. It should be mentioned that the inhibitory effects of atorvastatin were not the result of decreased cell viability, atorvastatin at the 1, 5, and 10 μM concentrations used in the 3D model of glioblastoma. By contrast, the proinflammatory gene expression rates were identified to be significantly different compared with those of the control group (p < 0.05). IL-17RA is expressed in most tissues examined to activate many of the same signaling cascades as innate cytokines such as TNFα and IL-1β [42]. Furthermore, emerging knowledge regarding IL-17A/IL-17RA signaling in numerous tissues suggests an important role in health and disease beyond the immune system [42]. Given this importance of IL-17RA signaling, the understanding of IL17RA signaling roles in the CNS is of particular interest. It has observed significant constitutive expression of the IL-17RA mRNA in both astrocytes and microglia in purified cultures, free of peripheral immune cells [19]. It has demonstrated the infiltration/enhancement of IL-17-producing cells in malignant gliomas [43, 44] and IL-17 has been linked to cancer progression in many tumor types [45]. Overall, the role of IL-17 in glioma progression remains uncertain and the precise underlying mechanisms remain largely unknown. Results from the analysis of tumor tissues from patients with malignant gliomas have demonstrated preferential expression of IL-17R in glioma cells [44]. Results demonstrate that IL-17R in glioma stem cells is functional and it can play an important role in the maintenance of glioma stem cells by inducing their proliferation or self-renewal. This increasing evidence suggests that IL-17A and Th17 play a main role in autoimmune inflammation, but there are gaps in our understanding of IL-17RA signaling mechanisms [46]. In the current study, results have demonstrated a potential impact of IL-17R in glioma growth and progression. Data showed that atorvastatin downregulates IL-17RA expression in glioblastoma cells especially at 10 μM concentration. Further studies are needed to confirm the same. Further studies are warranted to examine whether any of the mechanisms are associated with IL-17R-mediated stimulation of glioblastoma cell renewal [44, 47]. Scientists identify the adaptor Act1 as a key connection between IL-17 receptor (IL-17R) ligation by IL-17 and “downstream” signaling [48]. TRAF3IP2 is an upstream regulator of IKK and JNK [49, 50]. In fact, TRAF3IP2 has been shown to physically associate with IKK [51]. It has reported that the activation of NF-κB via IKK and AP-1 via JNK, by oxLDL, is inhibited by the knockdown of TRAF3IP2. Studies indicate that targeting TRAF3IP2 can potentially inhibit progression of atherosclerotic vascular diseases [51]. It may provide an opportunity for further studies into targeting IL-17R itself for therapeutic attenuation of glioblastom cells population, and more studies into the mechanism of IL-17R_TRAF3IP2 interaction may show other molecular targets in downstream of IL-17R pathway. Previous studies have shown that silencing TRAF3IP2 by siRNA decreased cardiac fibroblast migration and led to cardiomyocyte death in vitro [49]. We showed that the glioma model could be used in cancer stem cell research. From the results obtained, we can observe some interesting effects caused by atorvastatin on glioma cells by providing some information on the molecular mechanisms of atorvastatin inhibitory effects. In this study, we found that atorvastatin reduced glioma cell inflammation by suppressing the protumorigenic effects on glioma cells at 1, 5, and 10 μM concentrations. Therefore, identifying therapeutic targets in upstream of cytokine secretion factors, especially at the receptor level, seems an efficient clinical therapy against malignant gliomas. The results corroborated with the proliferation and apoptosis data and confirmed that TRAF3IP2 enhance glioblastoma progression. Some studies in this field can provide valuable insight into alternative mechanisms that IL-17R interaction could promote glioma progression. It has been demonstrated Act1 by SEFIR domains binds to IL-17RA and IL-17RC [52]. The studies demonstrated that IL-17R–Act1-mediated signaling is required for local IL-17-dependent production of proinflammatory cytokines by astrocytes and epithelial cells during inflammation in the central nervous system and intestine, respectively [48, 52]. The results of this study indicated the usefulness of atorvastatin in efficient control of glioma, but future studies should investigate the effects of atorvastatin in glioma in vitro and in vivo.
Conclusion
In conclusion, our studies demonstrate that atorvastatin has potent apoptosis and inflammation-inhibiting effects against U87 glioblastoma cells. In the present study, the expression of IL-17RA and TRAF3IP2 in glioblastoma cells were reduced in the 3D model of glioblastoma, possibly suggesting that reduced inflammatory activation in these cells might have resulted in reduced cytokine and these effects are dose dependent. The most likely mechanisms are the inhibition of inflammation by IL-17RA interaction with TRAF3IP2 and NFKB signaling pathway. This study proposes that atorvastatin may be a suitable candidate for glioblastoma treatment [52]. However, the results of this study indicated the usefulness of atorvastatin in efficient control of glioma, but to the best of our knowledge, numerous mechanisms are involved in anti-inflammatory effect and apoptosis induction of atorvastatin that further research in vitro and in vivo is required to elucidate these.
Change history
06 May 2017
An erratum to this article has been published.
References
Galvão RP, Zong H (2013) Inflammation and gliomagenesis: bi-directional communication at early and late stages of tumor progression. Curr Pathobiology Reports 1(1):19–28
Furnari FB, Fenton T, Bachoo RM, Mukasa A, Stommel JM, Stegh A, Hahn WC, Ligon KL et al (2007) Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev 21(21):2683–2710
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30(7):1073–1081
Sciume G, Santoni A and Bernardini G (2010) Chemokines and glioma: invasion and more. J Neuroimmunol 224(1–2):8–12
Yeung YT, McDonald KL, Grewal T, Munoz L (2013) Interleukins in glioblastoma pathophysiology: implications for therapy. Br J Pharmacol 168(3):591–606
Bhat KP, Balasubramaniyan V, Vaillant B, Ezhilarasan R, Hummelink K, Hollingsworth F, Wani K, Heathcock L et al (2013) Mesenchymal differentiation mediated by NF-kappaB promotes radiation resistance in glioblastoma. Cancer Cell 24(3):331–346
Guo J, Shinriki S, Su Y, Nakamura T, Hayashi M, Tsuda Y, Murakami Y, Tasaki M et al (2014) Hypoxia suppresses cylindromatosis (CYLD) expression to promote inflammation in glioblastoma: possible link to acquired resistance to anti-VEGF therapy. Oncotarget 5(15):6353–6364
Barcellos-Hoff MH, Newcomb EW, Zagzag D, Narayana A (2009) Therapeutic targets in malignant glioblastoma microenvironment. Semin Radiat Oncol 19(3):163–170
Anderson JC, McFarland BC, Gladson CL (2008) New molecular targets in angiogenic vessels of glioblastoma tumours. Expert Rev Mol Med 10:e23
Daugherty SE, Moore SC, Pfeiffer RM, Inskip PD, Park Y, Hollenbeck A, Rajaraman P (2011) Nonsteroidal anti-inflammatory drugs and glioma in the NIH-AARP Diet and Health Study cohort. Cancer Prev Res 4(12):2027–2034
Riad A, Du J, Stiehl S, Westermann D, Mohr Z, Sobirey M, Doehner W, Adams V et al (2007) Low-dose treatment with atorvastatin leads to anti-oxidative and anti-inflammatory effects in diabetes mellitus. Eur J Pharmacol 569(3):204–211
Jain MK, Ridker PM (2005) Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov 4(12):977–987
Blanco-Colio LM, Tuñón J, Martín-Ventura JL, Egido J (2003) Anti-inflammatory and immunomodulatory effects of statins. Kidney Int 63(1):12–23
Gómez-Gerique JA, Ros E, Oliván J, Mostaza JM, Vilardell M, Pintó X, Civeira F, Hernández A et al (2002) Effect of atorvastatin and bezafibrate on plasma levels of C-reactive protein in combined (mixed) hyperlipidemia. Atherosclerosis 162(2):245–251
Ferro D, Parrotto S, Basili S, Alessandri C, Violi F (2000) Simvastatin inhibits the monocyte expression of proinflammatory cytokines in patients with hypercholesterolemia. J Am Coll Cardiol 36(2):427–431
Stanislaus R, Gilg AG, Singh AK, Singh I (2002) Immunomodulation of experimental autoimmune encephalomyelitis in the Lewis rats by Lovastatin. Neurosci Lett 333(3):167–170
Antonopoulos AS, Margaritis M, Lee R, Channon K, Antoniades C (2012) Statins as anti-inflammatory agents in atherogenesis: molecular mechanisms and lessons from the recent clinical trials. Curr Pharm Des 18(11):1519–1530
Onishi RM, Gaffen SL (2010) Interleukin-17 and its target genes: mechanisms of interleukin-17 function in disease. Immunology 129(3):311–321
Miossec P (2009) IL-17 and Th17 cells in human inflammatory diseases. Microbes Infect 11(5):625–630
Weaver CT, Hatton RD, Mangan PR, Harrington LE (2007) IL-17 family cytokines and the expanding diversity of effector T cell lineages. Annu Rev Immunol 25:821–852
Hwang SY, Kim JY, Kim KW, Park MK, Moon Y, Kim WU, Kim HY (2004) IL-17 induces production of IL-6 and IL-8 in rheumatoid arthritis synovial fibroblasts via NF-κB-and PI3-kinase/Akt-dependent pathways. Arthritis Res Ther 6(2):1
Gu C, Wu L, Li X (2013) IL-17 family: cytokines, receptors and signaling. Cytokine 64(2):477–485
Li X, Commane M, Nie H, Hua X, Chatterjee-Kishore M, Wald D, Haag M, Stark GR (2000) Act1, an NF-κB-activating protein. Proc Natl Acad Sci 97(19):10489–10493
Ellinghaus E, Ellinghaus D, Stuart PE, Nair RP, Debrus S, Raelson JV, Belouchi M, Fournier H et al (2010) Genome-wide association study identifies a psoriasis susceptibility locus at TRAF3IP2. Nat Genet 42(11):991–995
Jiang P, Mukthavaram R, Chao Y, Nomura N, Bharati IS, Fogal V, Pastorino S, Teng D et al (2014) In vitro and in vivo anticancer effects of mevalonate pathway modulation on human cancer cells. Br J Cancer 111(8):1562–1571
Altwairgi AK (2015) Statins are potential anticancerous agents (review). Oncol Rep 33(3):1019–1039
Wu XD, Zeng K, Xue FQ, Chen JH, Chen YQ (2013) Statins are associated with reduced risk of gastric cancer: a meta-analysis. Eur J Clin Pharmacol 69(10):1855–1860
Tapia-Pérez JH, Kirches E, Mawrin C, Firsching R, Schneider T (2011) Cytotoxic effect of different statins and thiazolidinediones on malignant glioma cells. Cancer Chemother Pharmacol 67(5):1193–1201
Nielsen SF, Nordestgaard BG, Bojesen SE (2012) Statin use and reduced cancer-related mortality. N Engl J Med 367(19):1792–1802
Zhang Z, Li C, Shang L, Zhang Y, Zou R, Zhan Y, Bi B (2016) Sulforaphane induces apoptosis and inhibits invasion in U251MG glioblastoma cells. Springerplus 5(235):016–1910
Xu X, Farach-Carson MC, Jia X (2014) Three-dimensional in vitro tumor models for cancer research and drug evaluation. Biotechnol Adv 32(7):1256–1268
Kula M, Tanriverdi G, Oksuz E, Bilir A, Shahzadi A, Yazici Z (2014) Simvastatin and dexamethasone potentiate antitumor activity of fotemustine. Int J Pharmacol 10(5):267–274
Obara S, Nakata M, Takeshima H, Kuratsu JI, Maruyama I, Kitajima I (2002) Inhibition of migration of human glioblastoma cells by cerivastatin in association with focal adhesion kinase (FAK). Cancer Lett 185(2):153–161
Takahashi HK, Nishibori M (2007) The antitumour activities of statins. Curr Oncol 14(6):246
Hindler K, Cleeland CS, Rivera E, Collard CD (2006) The role of statins in cancer therapy. Oncologist 11(3):306–315
Wang G, Dinkins M, He Q, Zhu G, Poirier C, Campbell A, Mayer-Proschel M, Bieberich E (2012) Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4) potential mechanism of apoptosis induction in Alzheimer disease (AD). J Biol Chem 287(25):21384–21395
Fromigué O, Hamidouche Z, Marie PJ (2008) Blockade of the RhoA-JNK-c-Jun-MMP2 cascade by atorvastatin reduces osteosarcoma cell invasion. J Biol Chem 283(45):30549–30556
Gray GK, McFarland BC, Nozell SE, Benveniste EN (2014) NF-kappaB and STAT3 in glioblastoma: therapeutic targets coming of age. Expert Rev Neurother 14(11):1293–1306
McFarland BC, Gray GK, Nozell SE, Hong SW, Benveniste EN (2013) Activation of the NF-kappaB pathway by the STAT3 inhibitor JSI-124 in human glioblastoma cells. Mol Cancer Res 11(5):494–505
Wood WG, Igbavboa U, Muller WE, Eckert GP (2013) Statins, Bcl-2, and apoptosis: cell death or cell protection? Mol Neurobiol 48(2):308–314
Fan TJ, Han LH, Cong RS, Liang J (2005) Caspase family proteases and apoptosis. Acta Biochim Biophys Sin 37(11):719–727
Sarma JD, Ciric B, Marek R, Sadhukhan S, Caruso ML et al (2009) Functional interleukin-17 receptor A is expressed in central nervous system glia and upregulated in experimental autoimmune encephalomyelitis. J Neuroinflammation 6:14
Parajuli P, Mittal S (2013) Role of IL-17 in glioma progression. J Spine Neurosurg 1:1–4
Parajuli P, Anand R, Mandalaparty C, Suryadevara R, Sriranga PU et al (2016) Preferential expression of functional IL-17R in glioma stem cells: potential role in self-renewal. Oncotarget 7(5):6121
Yang B, Kang H, Fung A, Zhao H, Wang T, Ma D (2014) The role of interleukin 17 in tumour proliferation, angiogenesis, and metastasis. Mediat Inflamm 1:1–12
Tabarkiewicz J, Pogoda K, Karczmarczyk A, Pozarowski P, Giannopoulos K (2015) The role of IL-17 and Th17 lymphocytes in autoimmune diseases. Arch Immunol Ther Exp 63(6):435–449
Wang K, Kim MK, Di Caro G, Wong J, Shalapour S, Wan J, Zhang W, Zhong Z et al (2014) Interleukin-17 receptor a signaling in transformed enterocytes promotes early colorectal tumorigenesis. Immunity 41(6):1052–1063
Hunter CA (2007) Act1-ivating IL-17 inflammation. Nat Immunol 8(3):232–234
Valente AJ, Sakamuri SS, Siddesha JM, Yoshida T, Gardner JD, Prabhu R, Siebenlist U, Chandrasekar B (2013) TRAF3IP2 mediates interleukin-18-induced cardiac fibroblast migration and differentiation. Cell Signal 25(11):2176–2184
Venkatesan B, Valente AJ, Das NA, Carpenter AJ, Yoshida T, Delafontaine JL, Siebenlist U, Chandrasekar B (2013) CIKS (Act1 or TRAF3IP2) mediates high glucose-induced endothelial dysfunction. Cell Signal 25(1):359–371
Valente AJ, Irimpen AM, Siebenlist U, Chandrasekar B (2014) OxLDL induces endothelial dysfunction and death via TRAF3IP2: inhibition by HDL3 and AMPK activators. Free Radic Biol Med 70:117–128
Gaffen SL (2009) Structure and signaling in the IL-17 receptor superfamily. Nat Rev Immunol 9(8):556–567
Acknowledgments
We thank the Iran National Science Foundation (INSF) for the financial support (grant number 93051217) and Tehran University of Medical Sciences for this research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Dr. Jafar Ai is the first corresponding author.
An erratum to this article is available at https://doi.org/10.1007/s12035-017-0577-4.
Rights and permissions
About this article
Cite this article
Bayat, N., Ebrahimi-Barough, S., Norouzi-Javidan, A. et al. Anti-inflammatory Effects of Atorvastatin by Suppressing TRAF3IP2 and IL-17RA in Human Glioblastoma Spheroids Cultured in a Three-dimensional Model: Possible Relevance to Glioblastoma Treatment. Mol Neurobiol 55, 2102–2110 (2018). https://doi.org/10.1007/s12035-017-0445-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0445-2