Abstract
Statins have proven their effectiveness in the treatment of cardiovascular disease. This class of drugs has also attracted attention as a potential treatment for dissimilar diseases such as certain types of cancers and neurodegenerative diseases. What appears to be a contradiction is that, in the case of cancer, it has been suggested that statins increase apoptosis and alter levels of Bcl-2 family members (e.g., reduce Bcl-2 and increase Bax), whereas studies mainly using noncancerous cells report opposite effects. This review examined studies reporting on the effects of statins on Bcl-2 family members, apoptosis, cell death, and cell protection. Much, but not all, of the evidence supporting the pro-apoptotic effects of statins is based on data in cancer cell lines and the use of relatively high drug concentrations. Studies indicating an anti-apoptotic effect of statins are fewer in number and generally used much lower drug concentrations and normal cells. Those conclusions are not definitive, and certainly, there is a need for additional research to determine if statin repositioning is justified for noncardiovascular diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
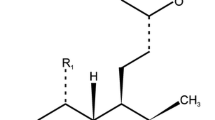
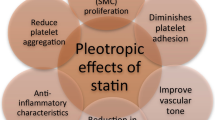
Statins are well-recognized for their efficacy in the prevention/treatment of cardiovascular disease, a topic which has been extensively reviewed [1]. Statins reduce cholesterol synthesis and increase the uptake of low-density lipoproteins (LDL). Within the mevalonate pathway, these drugs also have cholesterol-independent effects, namely, the reduction of the two isoprenoids farnesyl pyrophosphate (FPP) and geranylgeranyl pyrophosphate (GGPP). Reducing FPP and GGPP decreases the prenylation of small GTPases, and it is thought that such a mechanism may contribute to the reduction in morbidity and mortality occurring in cardiovascular disease [2, 3]. In addition to the use of statins in the prevention/treatment of cardiovascular disease, it has been suggested, albeit with some controversy, that these drugs may have efficacy in treating diseases such as various cancers, ischemic stroke, inflammatory diseases, and certain neurodegenerative diseases [4–8]. One of the proposed mechanisms for the effects of statins in noncardiovascular diseases involves changes in expression levels of the pro-apoptotic and anti-apoptotic Bcl-2 family of proteins. Several reports found that statins reduced the levels of the anti-apoptotic protein Bcl-2 and increased apoptosis and cell death. Some of those studies are summarized in Table 1. In contrast, there is evidence that statins increase Bcl-2 abundance which would favor and, in some instances, reduce apoptosis and cell death, and these are listed in Table 2. The purpose of this mini-review will be to focus on studies within the context of what appears to be contradictory findings regarding the effects of statins on Bcl-2 expression levels, apoptosis, cell death, and cell protection.
Statins, Bcl-2 Family Members, and Cell Death
One of the earliest studies associating statins with apoptosis and cell death reported on the effects of lovastatin (0.1 μM) on growth in two cell lines, dexamethasone-resistant and dexamethasone-sensitive lines derived from human acute T cell leukemia patients [9]. Cell death was induced by both lovastatin and dexamethasone, and the observation was made that the cells had “characteristics of apoptosis” but markers of apoptosis were not reported. Since that study, there have been additional [10–14] reports on statin-induced apoptosis and cell death (Table 1). Statin-induced apoptosis and/or cell death occurs in cancer cell lines (e.g., human acute leukemia lines, human promyelocytic HL-60 cells, malignant glioma cells, Barrett’s esophageal adenocarcinoma cells) and noncancer cells (e.g., mouse fibroblasts, rat brain neuroblasts). There is some evidence suggesting that different types of cancer are more susceptible to statins as compared with others [4]. A common feature of many of those studies is that high statin concentrations (from micromolar to millimolar amounts) were required to cause apoptosis and cell death, although there are exceptions [9], including a study showing that lovastatin beginning at 0.1 μM induced DNA degradation in human glioma cells [11]. Although in that study, the effects of lovastatin on DNA degradation in another cell line, anaplastic astrocytoma, was not apparent until a drug concentration of 1 μM.
The pivotal roles that Bcl-2 family members play in apoptosis and cell death are well-recognized, and that large body of work has been extensively reviewed [15–20]. There have been several studies showing that statins alter the expression levels of Bcl-2 family members. This section will examine reports indicating that statins alter levels of proteins such as Bcl-2, Bcl-xL, and Bax. Reductions in Bcl-2 and Bcl-xL and an increase in Bax favor a pro-apoptotic cell environment. An early study reported that serum from normal human subjects receiving fluvastatin (92 μM/day for 6 days) added to human smooth muscle cells in vitro reduced Bcl-2 protein levels and increased apoptosis [21]. Similar findings were seen in T cells of patients with acute coronary syndromes who received rosuvastatin (20 μM/day for 6 weeks) [22]. There have been several in vitro studies using different statins (lovastatin, atorvastatin, simvastatin, pravastatin, and cerivastatin) and different noncancer and cancer cell lines demonstrating that, generally, statins at high concentrations reduced Bcl-2 protein levels (Table 1). A notable exception to the observation that high statin concentrations are needed to act on Bcl-2 was a study that found that Bcl-2 protein and mRNA levels were reduced by lovastatin at concentrations of 2.4 and 6.2 nM/ml [23], although in that study, a Western blot showed that the lower lovastatin concentration had a larger reducing effect on Bcl-2 as compared with the higher concentration. The data did not appear to be semi-quantified (scanned); only a single experiment was shown, and so, it is not clear if differences were significant. Protein levels of another anti-apoptotic member of the Bcl-2 family, Bcl-xL were also reduced by statins (lovastatin and simvastatin) in different cell types (rat brain neuroblasts, mouse tubular cells, human myeloid KBM-5 cells, human colon cancer cells, and human prostate cancer cells PC3) [24–28]. While most studies using relatively high concentrations of statins have found that Bcl-2 levels were reduced, a recent study found opposite results [29]. Simvastatin (5 μM) significantly increased Bcl-2 protein levels in primary human skeletal myotubes, which was associated with decreased cell viability and enhanced oxidative stress [29]. A conclusion reached in that study was that the simvastatin-induced increase in Bcl-2 protein expression might have been a protective response to drug-induced cell death. In the same study, levels of the pro-apoptotic protein Bax were also significantly increased. Several studies have reported that statins did not alter Bax levels [25, 30–37].
Generally, at high statin concentrations, apoptosis is increased and Bcl-2 expression levels and cell viability are reduced. The mechanisms for the statin-induced reduction of Bcl-2 protein levels have not been forthcoming. Statins reduce cholesterol, FPP, GGPP, and protein prenylation, but how those reductions trigger an attenuation of the anti-apoptotic protein Bcl-2 and increase the abundance of pro-apoptotic proteins such as Bax and Bim is not understood. There is evidence that statins can act outside of the mevalonate pathway. Statins, for example, bind to the lymphocyte function-associated antigen-1, which is a heterodimeric glycoprotein and is a member of the β2 integrin family [38, 39]. Directly related to the issue of statins and Bcl-2 is work discussed later in this review on Bcl-2 and cell protection showing that statins stimulate Bcl-2 gene expression and protein levels, which do not involve the mevalonate pathway.
Statins, Bcl-2 Family Members, and Cell Protection
In the previous section, studies that found that statins reduced Bcl-2 protein levels were reviewed. This section will examine in vivo and in vitro studies which found that statins increase Bcl-2 levels, and some of those studies are listed in Table 2. In 2005, our laboratory was the first to report that a statin, simvastatin, significantly increased Bcl-2 gene expression in brain tissue of mice receiving the drug orally (120 μmol/kg for 21 days) [40]. Separate groups of mice treated with lovastatin and pravastatin also showed increased Bcl-2 gene expression, but those differences were not significant. Simvastatin induction of Bcl-2 gene expression was detected using the Affymetrix DNA array and confirmed using RT-PCR. Bcl-2 protein levels were also significantly increased in simvastatin-treated mice. There were several other genes whose expression levels were also altered by statins (e.g., Igfbp3, Hk1, c-fos, c-myc, Npy1r, MCT2, Sdc4). In a subsequent study in collaboration with Walter Muller and Gunter Eckert, we replicated our findings on simvastatin induction of brain Bcl-2 protein levels but this time in the guinea pig, demonstrating that the drug increased Bcl-2 protein levels in another species [41]. In the same study, Bax protein levels were significantly reduced. Dissociated brain cells from the guinea pigs administered simvastatin in vivo exhibited neuroprotection when challenged ex vitro with sodium nitroprusside and the Bcl-2 protein inhibitor HA14-1. In an in vivo rat quinolinic acid model of Huntington’s disease, simvastatin (2.4 μmol/kg i.p./day, 2 or 8 weeks) was neuroprotective [42]. Bcl-2 protein levels were increased, whereas levels of the pro-apoptotic protein Bax were reduced, results which are similar to what we observed in the brain tissue of simvastatin-treated guinea pigs [41]. Other in vivo studies [43–45] reported that statins increased Bcl-2 abundance and reduced apoptosis, and they are summarized in Table 2. An exception to those findings is a study showing that the administration of atorvastatin (41 μmol/kg for 3 weeks) did not significantly alter levels of Bcl-2 and Bax in aortic smooth muscle cells from spontaneously hypertensive rats [46]. Markers of apoptosis were not affected by atorvastatin treatment in those animals.
There is a body of data from in vitro studies showing that statins increase Bcl-2 and reduce apoptosis (Table 2), which is in agreement with the majority of in vivo studies discussed in this section. We reported that simvastatin (0.1 μM) significantly increased Bcl-2 mRNA and protein levels and provided neuroprotection in mouse primary neurons when challenged with oligomeric amyloid β-protein(42) [47]. When Bcl-2 expression was inhibited by the antisense oligonucleotide G3139, simvastatin neuroprotection was abolished in cells. The finding that inhibition of Bcl-2 eliminates the protective effects of simvastatin was replicated using another statin, fluvastatin (0.01–0.1 μM), and a different cell type, human vascular endothelial cells, which were challenged with H2O2 [48]. In that study, it was also observed that fluvastatin increased Bcl-2 mRNA expression and protein levels, which is consistent with the earlier study using simvastatin and mouse primary neurons [47]. Treatment of different cell types (mesenchymal stem cells, human osteosarcoma cells, and human atrial trabeculae) with statins (atorvastatin, simvastatin, and pravastatin) increased Bcl-2 protein levels and reduced markers of apoptosis [49–51], and those studies are summarized in Table 2.
Biphasic Effects of Statins on Bcl-2 Family Members
Statins reduce Bcl-2 mRNA and protein levels and increase apoptosis and cell death (Table 1). In stark contrast, Table 2 lists the studies reporting that statins increase Bcl-2 mRNA and protein levels, reduce apoptosis, and are protective. Many of the in vitro studies supporting a detrimental effect of statins used cancer cell lines, suggesting that cancer cells may respond differently to statins as compared to normal cells. It was recently reported that simvastatin (20 μM) reduced Bcl-2 mRNA and increased apoptosis in different cancer cell lines (MCF7 human breast cancer cells, HepG2 human hepatocellular carcinoma cells, NCI-N87 human gastric cancer NCI gastric cells, and NCiH12299 human non-small cell lung carcinoma NCH lung cells), but normal cells (SAEC human normal small airway epithelial cells) were unaffected [52]. However, in view of the fact that a high concentration of simvastatin was employed, the absence of an effect in the epithelial cells may be a unique property of those cells. The majority of studies showing that statins increase Bcl-2 mRNA and proteins levels and reduce apoptosis have used normal cells (Table 2). Exceptions have been studies using human neuroblastoma cells (SH-SY5Y cells) [47] and human osteosarcoma cells (MG63 cells) [50].
The two studies using cancer cell lines cited previously [47, 50] used low statin concentrations to stimulate Bcl-2 expression. The study with SH-SY5Y cells used a simvastatin concentration of 0.1 μM and the study with osteosarcoma cells used simvastatin at concentrations ranging from 0.001 to 0.1 μM. The question is raised if statin concentration is a determining factor in whether Bcl-2 levels are increased or reduced. Figure 1 plots in vitro studies showing statins reducing or increasing Bcl-2 mRNA and protein levels as a function of statin concentration. There are more studies showing that Bcl-2 levels are reduced by statins as compared with those studies showing an increase. The majority of studies showing that statins reduce Bcl-2 levels used statin concentrations of 5 μM or greater. Studies showing that statins increase Bcl-2 levels used concentrations of 1 μM or less. Certainly, there were exceptions, but a guarded conclusion is that, whether statins increase or decrease Bcl-2, such effects are dependent on statin concentrations.
Mechanisms of Statin-Induced Changes in Bcl-2
Statins reduce cholesterol by reducing the production of mevalonate and upregulate the LDL receptor, producing an increase in the removal of LDL from the blood. Mevalonate is not only the precursor of cholesterol but it is the precursor of the two isoprenoids, FPP and GGPP. FPP is a midpoint precursor of cholesterol and the direct precursor of GGPP. Both FPP and GGPP prenylate small GTPases such as the Rho, Ras, and Rab family of proteins whose coordinated activity is critical for cell structure/function. Simvastatin reduces FPP and GGPP levels [53] and it has been proposed that the beneficial effects of statins may be due to a reduction in prenylation of specific proteins [3, 8, 54–56]. How such changes in the mevalonate pathway would cause changes in Bcl-2 levels is unclear. Bcl-2 gene expression has been found to be activated by the transcription factor NF-κB [57]. Simvastatin at a high concentration (50 μM) inhibited TNF-α-induced NF-κB activation which was associated with a reduction in Bcl-2 protein levels in human myeloid KBM-5 cells [26]. In the same study, however, it was noted that simvastatin alone had no effect on NF-κB activation.
There is evidence that endothelin-1 (ET-1) can increase Bcl-2 abundance via the transcription factor nuclear factor of activated thymocytes (NFATc) [58]. We found that simvastatin increased ET-1 gene expression whose product is the precursor of the ET-1 protein [40]. The hypothesis that simvastatin stimulation of Bcl-2 involves the upregulation of ET-1 and binding of NFATc to Bcl-2 promoter sites in SH-SY5Y human neuroblastoma cells was tested [59]. Simvastatin increased both intracellular and secreted ET-1 protein levels. Exogenous ET-1 increased Bcl-2 protein abundance, which was inhibited by ET-1 receptor antagonists. Simvastatin increased the translocation of NFATc3 to the nucleus while reducing nuclear NFATc1 and having no effect on NFATc4. The Bcl-2 promoter has multiple NFAT binding sites [58], and we found that treatment of cells with simvastatin stimulated the binding of NFATc3 to the Bcl-2 promoter. This study was the first to directly identify a transcriptional mechanism for the regulation of statin-induced changes in Bcl-2 protein levels. These results do not preclude other mechanisms, and the role of protein prenylation in Bcl-2 regulation remains unknown. Also, further study is needed on how statins alter levels of other Bcl-2 family members.
Summary
There is evidence that statins may be efficacious in treating certain types of cancers by acting on Bcl-2 family members and increasing apoptosis and cell death. Equally compelling are studies showing that statins reduce apoptosis and increase Bcl-2. Much, but not all, of the evidence supporting a pro-apoptotic effect of statins is based on data in cancer cell lines and the use of relatively high drug concentrations. Studies indicating an anti-apoptotic effect of statins are fewer in number and generally used low drug concentrations and normal cells. Several questions remain unanswered regarding statin effects on apoptosis, cell death/protection, and Bcl-2 family members. There has not been a comprehensive examination of differences in cell types, malignant versus nonmalignant in response to statins, or for that matter, comparisons across different normal cells types (e.g., neurons, astrocytes, endothelial cells, etc.). The clinical use of statins for the treatment of cardiovascular disease began in the 1970s. Much more work is needed to determine if statins have efficacy in noncardiovascular diseases such as different cancers and neurodegenerative diseases.
References
Taylor F, Ward K, Moore THM, Burke M, Smith GD, Casas JP, Ebrahim S (2012) Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 1:2–8
Werner N, Nickenig G, Laufs U (2002) Pleiotropic effects of HMG-CoA reductase inhibitors. Basic Res Cardiol 97:105–116
Liao JK, Laufs U (2004) Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol 45:89–118
Wong WWL, Dimitroulakos J, Minden MD, Penn LZ (2002) HMG-CoA reductase inhibitors and the malignant cell: the statin family of drugs as triggers of tumor-specific apoptosis. Leukemia 16:508–519
Hindler K, Cleeland CS, Rivera E, Collard CD (2006) The role of statins in cancer therapy. Oncologist 11:306–315
Elewa HF, El-Remessy AB, Somanath PR, Fagan SC (2010) Pharmacotherapy 30:169–176
Eckert GP, Muller WE, Wood WG (2007) Cholesterol-lowering drugs and Alzheimer’s disease. Future Lipidol 2:423–432
Wood WG, Eckert GP, Igbavboa U, Muller WE (2010) Statins and neuroprotection: a prescription to move the field forward. Ann NY Acad Sci 1197:1–8
Bansal N, Houle AG, Melnykovych G (1989) Comparison of dexamethasone and lovastatin (mevinolin) as growth inhibitors in cultures of T-cell derived human acute leukemia lines (CEM). Leuk Res 13:875–882
Pérez-Sala D, Mollinedo F (1994) Inhibition of isoprenoid biosynthesis induces apoptosis in human promyelocytic HL-60 cells. Biochem Biophys Res Commun 199:1209–1215
Jones KD, Couldwell WT, Hinton DR, Su Y, He S, Anker L, Law RE (1994) Lovastatin induces growth inhibition and apoptosis in human malignant glioma cells. Biochem Biophys Res Commun 205:1681–1687
Chang MY, Jan MS, Won SJ, Liu HS (1998) Ha-rasVal12 oncogene increases susceptibility of NIH/3T3 cells to lovastatin. Biochem Biophys Res Commun 248:62–68
Cerezo-Guisado MI, Alvarez-Barrientos A, Argent R, Garcìa-Marín LJ, Bragado MJ, Lorenzo MJ (2007) c-Jun N-terminal protein kinase signaling pathway mediates lovastatin-induced rat brain neuroblast apoptosis. Biochim Biophys Acta 1771:164–176
Ogunwobi OO, Beales IL (2008) Statins inhibit proliferation and induce apoptosis in Barett’s esophageal adenocarcinoma cells. Am J Gastroenterol 103:825–837
Chao DT, Korsmeyer SJ (1998) Bcl-2 family: regulators of cell death. Annu Rev Immunol 16:395–419
Akhtar RS, Ness JM, Roth KA (2004) Bcl-2 family regulation of neuronal development and neurodegeneration. Biochim Biophys Acta 1644:189–203
Breckenridge DG, Xue D (2004) Regulation of mitochondrial membrane permeabilization by Bcl-2 family proteins and caspases. Curr Opin Cell Biol 16:647–652
Walensky LD (2006) Bcl-2 in the crosshairs: tipping the balance of life and death. Cell Death Differ 13:1339–1350
Willis SN, Fletcher JI, Kaufmann T, van Delft MF, Chen L, Czabotar PE, Ierino H, Lee EF, Fairlie WD, Bouillet P, Strasser A, Kluck RM, Adams JM, Huang DCS (2007) Apoptosis initiated when BH3 ligands engage multiple Bcl-2 homologs, not Bax or Bak. Science 315:856–859
Youle RJ (2007) Cellular demolition and the rules of engagement. Science 315:776–778
Buemi M, Allegra A, Senatore M, Marino D, Medici MA, Aloisi C, DiPasquale G, Corica F (1999) Pro-apoptotic effect of fluvastatin on human smooth muscle cells. Eur J Pharmacol 370:201–203
Link A, Selejan S, Hewera L, Walter F, Nickenig G, Böhm M (2011) Rosuvastatin induces apoptosis in CD4(+)CD28(null) T cells in patients with acute coronary syndromes. Clin Res Cardiol 100:147–158
Jánosi J, Sebestyén A, Bocsi J, Barna G, Nagy K, Vályi-Nagy I, Kopper L (2004) Mevastatin-induced apoptosis and growth suppression in U266 myeloma cells. Anticancer Res 24:1817–1822
Garcia-Román N, Alvarez AM, Toro MJ, Lorenzo MJ (2001) Lovastatin induces apoptosis of spontaneously immortalized rat brain neuroblasts: involvement of nonsterol isoprenoid biosynthesis inhibition. Mol Cell Neurosci 17:329–341
Blanco-Colio LM, Justo P, Daehn I, Lorz C, Ortiz A, Egido J (2003) Bcl-xl overexpression protects from apoptosis induced by HMG-CoA reductase inhibitors in murine tubular cells. Kidney Int 64:181–191
Ahn KS, Sethi G, Aggarwal BB (2007) Simvastatin potentiates TNF-alpha-induced apoptosis through the down-regulation of NF-kappaB-dependent antiapoptotic gene products: role of IkappaBalpha kinase and TGF-beta-activated kinase-1. J Immunol 178:2507–2516
Cho SJ, Kim JS, Kim JM, Lee JY, Jung HC, Song IS (2008) Simvastatin induces apoptosis in human colon cancer cells and in tumor xenografts, and attenuates colitis-associated colon cancer in mice. Int J Cancer 123:951–957
Goc A, Kochuparambil ST, Al-Husein B, Al-Azayzih A, Mohammad S, Somanath PR (2012) Simultaneous modulation of the intrinsic and extrinsic pathways by simvastatin in mediating prostate cancer cell apoptosis. BMC Cancer 12:409
Kwak HB, Thalacker-Mercer A, Anderson EJ, Lin CT, Kane DA, Lee NS, Cortright RN, Bamman MM, Neufer PD (2012) Simvastatin impairs ADP-stimulated respiration and increases mitochondrial oxidative stress in primary human skeletal myotubes. Free Radic Biol Med 52:198–207
Blanco-Colio LM, Villa A, Ortego M, Hernández-Presa MA, Pascual A, Plaza JJ, Egido J (2002) 3-Hydroxy-3-methyl-glutaryl coenzyme A reductase inhibitors, atorvastatin and simvastatin, induce apoptosis of vascular smooth muscle cells by downregulation of Bcl-2 expression and Rho A prenylation. Atherosclerosis 161:17–26
van de Donk NW, Kamphuis MM, Lokhorst HM, Bloem AC (2002) The cholesterol lowering drug lovastatin induces cell death in myeloma plasma cells. Leukemia 16:1362–1371
Jiang Z, Zheng X, Lytle RA, Higashikubo R, Rich KM (2004) Lovastatin-induced up-regulation of the BH3-only protein, Bim, and cell death in glioblastoma cells. J Neurochem 89:168–178
Samson KT, Minoguchi K, Tanaka A, Oda N, Yoke T, Okada S, Yamamoto Y, Watanabe Y, Yamamoto M, Ohta S, Adachi M (2005) Effect of fluvastatin on apoptosis in human CD4+ T cells. Cell Immunol 235:136–144
Fromigué O, Haÿ E, Modrowski D, Bouvet S, Jacquel A, Auberger P, Marie PJ (2006) RhoA GTPase inactivation by statins induces osteosarcoma cell apoptosis by inhibiting p42/p44-MAPKs-Bcl-2 signaling independently of BMP-2 and cell differentiation. Cell Death Differ 13:1845–1856
Demyanets S, Kaun C, Pfaffenberger S, Hohensinner PJ, Rega G, Pammer J, Maurer G, Huber K, Wojta J (2006) Hydroxymethylglutaryl-coenzyme A reductase inhibitors induce apoptosis in human cardiac myocytes in vitro. Biochem Pharmacol 71:1324–1330
Aberg M, Wickström M, Siegbahn A (2008) Simvastatin induces apoptosis in human breast cancer cells in a NKkappaB-dependent manner and abolishes the anti-apoptotic signaling of TF/FVIIa and TF/FVIIa. Thromb Res 122:191–202
Tu YS, Kang XL, Zhou JG, Lv XF, Tang YB, Guan YY (2013) Involvement of Chk1-Cdc25A-cyclin A/CDK2 pathway in simvastatin induced S-phase cell cycle arrest and apoptosis in multiple myeloma cells. Eur J Pharmacol 670:356–364
Kallen J, Welzenbach K, Ramage P, Geyl D, Kriwacki R, Legge G, Cottens S, Weitz-Schmidt G, Hommel U (1999) Structural basis for LFA-1 inhibition upon lovastatin binding to the CD11a I-domain. J Mol Biol 292:1–9
Weitz-Schmidt G, Welzenbach K, Brinkmann V, Kamata T, Kallen J, Bruns C, Cottens S, Takada Y, Hommel U (2001) Statins selectively inhibit leukocyte function antigen-1 by binding to a novel regulatory integrin site. Nat Med 7:687–692
Johnson-Anuna LN, Eckert GP, Keller JH, Igbavboa U, Franke C, Fechner T, Schubert-Zsilavecz M, Karas M, Muller WE, Wood WG (2005) Chronic administration of statins alters multiple gene expression patterns in mouse cerebral cortex. J Pharmacol Exp Ther 312:786–793
Franke C, Nöldner M, Abdel-Kader R, Johnson-Anuna LN, Wood WG, Muller WE, Eckert GP (2007) Bcl-2 upregulation and neuroprotection in guinea pig brain following chronic simvastatin treatment. Neurobiol Dis 25:438–445
Patassini S, Giampà C, Martorana A, Bernardi G, Fusco FR (2008) Effects of simvastatin on neuroprotection and modulation of Bcl-2 and BAX in the rat quinolinic acid model of Huntington’s disease. Neurosci Res 448:166–169
Malik S, Sharma AK, Bharti S, Nepal S, Bhatia J, Nag TC, Narang R, Arya DS (2011) In vivo cardioprotection by pitavastatin from ischemic-reperfusion injury through suppression of IKK/NF-κB and upregulation of pAkt-e-NOS. J Cardiovasc Pharmacol 58:199–206
Rajtík T, Carnická S, Szobi A, Mesárošová L, Mát'uš M, Svec P, Ravingerová T, Adameová A (2012) Pleiotropic effects of simvastatin are associated with mitigation of apoptotic component of cell death upon lethal myocardial reperfusion-induced injury. Physiol Res 61(S2):S33–S41
Qin W, Lu Y, Zhan C, Shen T, Dou L, Man Y, Wang S, Xiao C, Bian Y, Li J (2012) Simvastatin suppresses apoptosis in vulnerable atherosclerotic plaques through regulating the expression of p(53), Bcl-2 and Bcl-xL. Cardiovasc Drugs Ther 26:23–30
Doyon M, Hale TM, Huot-Marchand JE, Wu R, de Champlain J, DeBlois D (2011) Does atorvastatin induce aortic smooth muscle cell apoptosis in vivo? Vascul Pharmacol 54:5–12
Johnson-Anuna LN, Eckert GP, Franke C, Igbavboa U, Muller WE, Wood WG (2007) Simvastatin protects neurons from cytotoxicity by up-regulating Bcl-2 mRNA and protein. J Neurochem 101:77–86
Xu SZ, Zhong W, Watson NM, Dickerson E, Wake JD, Lindow SW, Newton CJ, Atkin SL (2008) Fluvastatin reduces oxidative damage in human vascular endothelial cells by upregulating Bcl-2. J Thromb Haemost 6:692–700
Dong Q, Yang Y, Song L, Qian H, Xu Z (2011) Atorvastatin prevents mesenchymal stem cells from hypoxia and serum-free injury through activating AMP-activated protein kinase. Int J Cardiol 153:311–316
Zhao XH, Xu ZR, Zhang Q, Yang YM (2012) Simvastatin protects human osteosarcoma cells from oxidative stress-induced apoptosis through mitochondrial-mediated signaling. Mol Med Report 5:483–488
Lemoine S, Allouche S, Coulbault L, Cornet V, Massetti M, Galera P, Géard J-L, Hanouz J-L (2012) Mechanisms involved in cardioprotective effects of pravastatin administered during reoxygenation in human myocardium in vitro. Anesthesiology 116:824–833
Spampanato C, De Maria S, Sarnataro M, Giordano E, Zanfardino M, Baiano S, Carteni M, Morelli F (2012) Simvastatin inhibits cancer cell growth by inducing apoptosis correlated to activation of Bax and down-regulation of Bcl-2 gene expression. Int J Oncol 40:935–941
Eckert GP, Hooff GP, Strandjord DM, Igbavboa U, Volmer DA, Muller WE, Wood WG (2009) Regulation of the brain isoprenoids farnesyl- and geranylgeranylpyrophosphate is altered in male Alzheimer patients. Neurobiol Dis 35:251–257
Mcfarlane SI, Muniyappa R, Francisco R, Sowers JR (2002) Pleiotropic effects of statins: lipid reduction and beyond. J Clin Endocrinol Metab 87:1451–1458
Eckert GP, Wood WG, Muller WE (2005) Statins: drugs for Alzheimer’s disease? J Neural Transm 112:1057–1071
Li L, Zhang W, Cheng S, Cao D (2012) Isoprenoids and related pharmacological interventions: potential application in Alzheimer’s disease. Mol Neurobiol 46:64–77
Viatour P, Bentires-Alj M, Chariot A, Deregowski V, de Leval L, Merville M-P, Bours V (2003) NF-κB2/p100 induces Bcl-2 expression. Leukemia 17:1349–1356
Kawamura T, Ono K, Morimoto T, Akao M, Iwai-Kanai E, Wada H, Sowa N, Kita T, Hasegawa K (2004) Endothelin-1-dependent nuclear factor of activated T lymphocyte signaling associates with transcriptional coactivator p300 in the activation of the B cell leukemia-2 promoter in cardiac myocytes. Circ Res 94:1492–1499
Butterick TA, Igbavboa U, Eckert GP, Sun GY, Weisman GA, Muller WE, Wood WG (2010) Simvastatin stimulates production of the antiapoptotic protein Bcl-2 via endothelin-1 and NFATc3 in SH-SY5Y cells. Mol Neurobiol 41:384–391
Park WH, Lee YY, Kim ES, Seol JG, Jung CW, Lee CC, Kim BK (1999) Lovastatin-induced inhibition of HL-60 cell proliferation via cell cycle arrest and apoptosis. Anticancer Res 19:3133–3140
Igarashi M, Yamaguchi H, Hirata A, Tsuchiya H, Ohnuma H, Tominaga M, Daimon M, Kato T (2002) Mechanisms of inhibitory effects of cerivastatin on rat vascular smooth muscle cell growth. J Cardiovasc Pharmacol 40:277–287
Mück AO, Seeger H, Wallwiener D (2004) Class-specific pro-apoptotic effects of statins on human vascular endothelial cells. Z Kardiol 93:398–402
Kubota T, Fujisaki K, Itoh Y, Yano T, Sendo T, Oishi R (2004) Apoptotic injury in cultured human hepatocytes induced by HMG-CoA reductase inhibitors. Biochem Pharmacol 67:2175–2186
Mück AO, Seeger H, Wallwiener D (2004) Inhibitory effect of statins on the proliferation of human breast cancer cells. Int J Clin Pharmacol Ther 42:695–700
Konturek PC, Burnat G, Hahn EG (2007) Inhibition of Barret’s adenocarcinoma cell growth by simvastatin: involvement of COX-2 and apoptosis-related proteins. J Physiol Pharmacol 58:141–148
Kaneko R, Tsuji N, Asanuma K, Tanabe H, Kobayashi D, Watanabe N (2007) Survivin down-regulation plays a crucial role in 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor-induced apoptosis in cancer. J Biol Chem 282:19273–19281
Gauthaman K, Manasi N, Bongso A (2009) Statins inhibit the growth of variant human embryonic stem cells and cancer cells in vitro but not normal human embryonic stem cells. Br J Pharmacol 157:962–973
Lee SK, Kim YC, Song SB, Kim YS (2010) Stabilization and translocation of p53 to mitochondria is linked to Bax translocation to mitochondria in simvastatin-induced apoptosis. Biochem Biophys Res Commun 391:1592–1597
Zhang W, Wu J, Zhou L, Xie HY, Zheng SS (2010) Fluvastatin, a lipophilic statin, induces apoptosis in human hepatocellular carcinoma cells through mitochondria-operated pathway. Indian J Exp Biol 48:1167–1174
Acknowledgments
This work was supported in part by grants from the National Institutes of Health (AG-23524 and AG-18357) and the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wood, W.G., Igbavboa, U., Muller, W.E. et al. Statins, Bcl-2, and Apoptosis: Cell Death or Cell Protection?. Mol Neurobiol 48, 308–314 (2013). https://doi.org/10.1007/s12035-013-8496-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-013-8496-5