Abstract
Cyclooxygenase (COX) enzymes are pivotal in inflammation and cancer development. COX-2, in particular, has been implicated in tumor growth, angiogenesis, and immune evasion. Recently, COX-2 inhibitors have arisen as potential therapeutic agents in cancer treatment. In addition, combining COX inhibitors with other treatment modalities has demonstrated the potential to improve therapeutic efficacy. This review aims to investigate the effects of COX inhibition, both alone and in combination with other methods, on signaling pathways and carcinogenesis in various cancers. In this study, a literature search of all major academic databases was conducted (PubMed, Scholar google), including the leading research on the mechanisms of COX-2, COX-2 inhibitors, monotherapy with COX-2 inhibitors, and combining COX-2-inhibitors with chemotherapeutic agents in tumors. The study encompasses preclinical and clinical evidence, highlighting the positive findings and the potential implications for clinical practice. According to preclinical studies, multiple signaling pathways implicated in tumor cell proliferation, survival, invasion, and metastasis can be suppressed by inhibiting COX. In addition, combining COX inhibitors with chemotherapy drugs, targeted therapies, immunotherapies, and miRNA-based approaches has enhanced anti-tumor activity. These results suggest that combination therapy has the potential to overcome resistance mechanisms and improve treatment outcomes. However, caution must be exercised when selecting and administering combination regimens. Not all combinations of COX-2 inhibitors with other drugs result in synergistic effects; some may even have unfavorable interactions. Therefore, personalized approaches that consider the specific characteristics of the cancer and the medications involved are crucial for optimizing therapeutic strategies. In conclusion, as monotherapy or combined with other methods, COX inhibition bears promise in modulating signaling pathways and inhibiting carcinogenesis in various cancers. Additional studies and well-designed clinical trials are required to completely elucidate the efficacy of COX inhibition and combination therapy in enhancing cancer treatment outcomes. This narrative review study provides a detailed summary of COX-2 monotherapy and combination targeted therapy in cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The growing prevalence of cancer across the world poses a risk to human health and well-being and is the second leading cause of death among humans [1]. Cancer can be treated with a variety of medical modalities, including surgery (if the tumors can be removed surgically), chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Combining many therapeutic modalities into a single treatment plan is standard practice. For instance, the most typical form of combination treatment consists of surgery, local radiation, and systemic and local chemotherapy. However, due to chemoresistance, reduced radiation sensitivity, and other tumor molecular adaptations, the results of therapy are frequently poor and troublesome, which can result in a high risk of recurrence of cancer [2].
Prostaglandins are produced from arachidonic acid, and cyclooxygenases (COX) are the rate-limiting enzymes in this process. There are now two isozymes, namely COX-1 and COX-2 [3]. While COX-1 expression is constant in most healthy tissues, COX-2 expression can be induced and is frequently elevated in inflammatory and many neoplastic tissues [4]. Since COX-2 appears to be involved in multiple steps of the carcinogenesis process, blocking its activity has been shown to have anti-tumor and anti-angiogenic effects in a wide range of human malignancies [3].
Since COX-2 signaling pathways exist, using COX-2 inhibitors as a therapeutic method for treating human malignancies appears appealing. This new information might make it much easier to combine COX-2 inhibitor therapy with other types of cancer treatment in future research [5]. A medication combination like this one can simultaneously target several molecular targets. This study analyzed and detailed recent advancements in COX-2 inhibitors in combination with other anti-cancer medications because it has been discovered that COX-2 inhibitors produce anti-tumor activity and have extensive effects on human malignancies.
COX-2 inhibition was previously thought to target tumors primarily by inhibiting the COX-2 pathway. However, the anti-tumor effects of Celecoxib may also occur through mechanisms unrelated to COX-2. For example, studies have shown that COX-2 inhibitors can promote apoptosis and reduce cell proliferation and angiogenesis in cancer cells by regulating various signaling pathways in cancer. In addition, studies have shown that COX-2 inhibitors increase the sensitivity of cancer cells to chemotherapy and radiation therapy [6]. However, they are treated with antibiotics, traditional medicine, etc. It was recently established. Therefore, this review describes investigations into the mechanisms by which COX-2 inhibitors intervene in cancer through different signaling pathways and examines in vitro and in vivo studies to investigate how COX-2 inhibition enhances COX-2-independent mechanisms. in the clinical treatment of cancer [5, 7]. This study provides a detailed summary of COX-2 monotherapy and combination therapy with targeted therapy in cancer treatment.
COX-2 role in tumors
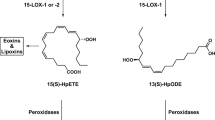
Carcinogen activation
Prostaglandin H synthase metabolizes numerous compounds when metabolizing arachidonic acid. Chemical metabolism often produces reactive metabolites with mutagenic and carcinogenic properties. COX peroxidase converts procarcinogens to carcinogens and causes tumors. COX peroxidase activity co-oxidizes several xenobiotics into mutagens. Cytochrome P-450s in the liver catalyze these oxidative processes, preventing mutagens. However, the colon contains low numbers of P-450s and other monooxygenases; thus, COX peroxidase activity co-oxidizes many xenobiotics to mutagens [8, 9]. This activity may also affect tobacco-exposed organs like the lung, oral cavity, and bladder. COX’s peroxidase activity activates procarcinogens like benzo[a]pyrene to intracellular electrophiles. Arachidonic acid metabolism generates mutagens. Malondialdehyde, a highly reactive byproduct of arachidonic acid oxidation, forms DNA adducts [10].
COX enzymes can activate a variety of environmental and dietary carcinogens, suggesting a role in the activation pathway of aromatic and heterocyclic amines and polycyclic hydrocarbons at extra-hepatic sites during early or late carcinogenesis.
Cancer development and progression
Liu et al. [11] initially reported COX-2 overexpression-induced cancer. They placed the murine COX-2 gene, Prostaglandin-endoperoxide synthase 2 (Ptgs2), downstream of a murine mammary tumor virus promoter. Thus, mammary gland hyperplasia and cancer were linked to significant COX-2 expression in epithelial cells and elevated Prostaglandin E2 (PGE2). Only this study has shown that COX-2 initiates tumors. However, mice models of skin carcinogenesis have been created employing the Ptgs2 gene downstream of the K5 or K14 promoters. Depending on COX-2 expression and prostaglandin accumulation, transgenic mice lines with keratin 5 promoter-driven COX-2 overexpression in basal epidermal cells have preneoplastic skin. Transgenics developed skin cancers after one treatment with 7,12-dimethylbenz[a]anthracene (DMBA). Transgenic mice did not need long-term treatment with the tumor promoter phorbol 12-myristate 13-acetate (PMA, a protein kinase C activator). COX-2 overexpression does not induce tumors but sensitizes the epidermis to genotoxic chemicals. Thus, COX-2 promotes tumor growth, not initiation [12].
In colorectal tumor models, COX-2 promotes tumors. In APCΔ716 mice crossed with mice with an inactivated Ptgs2 gene, Oshima et al. [40] found a reduction in colonic polyps. The number of large polyps was significantly reduced. Homozygous mice were more affected. Oshima et al. [13] tested COX-2 gene (Ptgs2) knockouts and a new COX-2 inhibitor on APCΔ716 knockout mice, a model of human familial adenomatous polyposis, to establish COX-2’s role in colorectal carcinogenesis. Ptgs2 null mutations significantly reduced intestinal polyps. Selective COX-2 inhibitors reduced polyp number in APCΔ716 mice more than sulindac, inhibiting COX-1 and COX-2. These findings suggest that COX-2-selective inhibitors may effectively treat colorectal polyposis and cancer. Downstream pathways also implicate COX-2 in carcinogenesis. Cells that overexpress COX-2 have higher concentrations of PGE2, which is thought to be the most significant COX-2 downstream effector. Homozygous deletion of EP2, a cell-surface receptor of PGE2, reduces intestinal polyps in APCΔ716 mice. Homozygous gene deletion for additional PGE2 receptors, Prostaglandin E2 receptor 1 (EP1) or EP3, did not impact intestinal polyp growth in APCΔ716 mice [14]. PGE2 promotes tumor angiogenesis, invasion, and metastasis. PGE2 expression causes several COX-2 actions. Only COX-2-expressing colon cancer cells establish colonies after PGE2 exposure [15].
Since EGFR is regarded as a therapeutic target for cancer treatment and several Epidermal growth factor receptor (EGFR) inhibitors have been discovered, activation of EGFR via PGE2 is of great interest [16]. Therefore, their interaction with COX-2 inhibitors may represent a novel development in cancer treatment. PGE2 and EGFR pathways frequently cooperate to cause or accelerate tumor development and block apoptosis. For instance, by activating the PI3kinase/Akt pathway, PGE2 prevents apoptosis. The exact biochemical mechanism is stimulated by EGFR receptor activation [17]. The EGFR and COX-2 pathways interact with one another. PGE2 directly causes EGFR transactivation by inducing the Src pathway and stimulating EGFR signaling by shedding active EGFR ligands from the plasma membrane [18, 19]. On the other hand, EGFR transactivation promotes COX-2 expression and, consequently, PGE2 expression via AP-1-mediated induction, creating a feedback loop of stimulation [17].
Invasion and Metastasis
The sneakiest and most lethal features of cancer are invasion and metastasis. Cell mobility and matrix breakdown are crucial to this process. An enzyme family that breaks down the matrix includes matrix metalloproteinases (MMPs) [20]. Their expression is linked to blood vessel penetration, metastasis, and tumor cell invasion of the basement membrane and stroma. Human colon cancer cells (Caco-2) were irreversibly transfected with either a COX-2 expression vector or a vector without the COX-2 insert in research to assess the impact of COX-2 on metastasis. Compared to the original Caco-2 cells or the control cells that had been transfected with a vector, the Caco-2 cells that constitutively produced COX-2 gained greater invasiveness. Metalloproteinase-2 activation was one of the biochemical modifications connected to this phenotypic shift [21].
Furthermore, Fernandez et al. reported that COX-2 inhibition reduced MMP-2 and MMP-9 release in the human prostate carcinoma cell line DU-145 [22]. Rat intestinal epithelial (RIE) cells permanently transfected with a COX-2 expression vector orientated in the sense (RIE-S) or antisense (RIE-AS) direction were utilized to determine a correlation between changes in the adhesion characteristics of cancer cells and COX-2 over-expression. The extracellular matrix (ECM) proteins were more readily adhered to by the RIE-S cells, which also produced more significant amounts of COX-2 protein. However, RIE-AS cells had higher levels of E-cadherin than RIE-S cells did. Increased Bcl2 expression, decreased Transforming growth factor 2 (TGF2) receptor levels, and resistance to butyrate-induced apoptosis were all seen in RIE-S cells [23]. These results show intestinal epithelial cells overexpressing COX-2 undergo phenotypic alterations that may increase their tumorigenic potential. Cancer cells are more likely to adhere to endothelial cells when COX-2 is expressed [24]. Selective COX-2 inhibitors have been used to stop animal metastasis, consistent with these in vitro results [25, 26]. For instance, COX-2-specific drugs block the ability of the highly metastatic NCI-H460-LNM35 cell line to spread when it is transplanted into SCID mice (severe combined immunodeficiency) [27].
COX-2 signaling
COX-2 signaling refers to the molecular pathways and processes that involve the COX-2 enzyme. COX-2 is an inducible enzyme that plays a significant role in inflammation and pain by catalyzing the conversion of arachidonic acid to prostaglandins and other bioactive lipids (26). While COX-2 is expressed at low levels constitutively in some tissues, its expression is rapidly up-regulated in response to inflammatory stimuli, growth factors, and cytokines (27).
Multiple cell types, including immune, endothelial, and tumor cells, exhibit tightly regulated activation of COX-2 signaling. PGE2, a byproduct of COX-2 activity, contributes to inflammation, angiogenesis, immune modulation, cell proliferation, and survival (26). Abnormal COX-2 signaling has been linked to tumor development, progression, and metastasis in the context of cancer (26). Numerous cancer varieties, including colorectal, breast, lung, prostate, and gastric cancers, have been observed to exhibit elevated COX-2 expression. Overexpression of COX-2 is linked to increased tumor growth, apoptosis resistance, enhanced angiogenesis, and immune evasion (27).
COX-2 signaling intersects with several crucial cancer biological pathways. For instance, prostaglandins derived from COX-2 can activate the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT) pathway, promoting cell survival and proliferation [28]. Additionally, they can modulate the Wnt/-catenin pathway, resulting in increased tumor growth and invasion [29]. In addition, COX-2 signaling can affect the tumor microenvironment by modulating the secretion of cytokines, chemokines, and growth factors, which can promote immune suppression, tumor-associated angiogenesis, and extracellular matrix remodeling [30]. Given the function of COX-2 signaling in cancer, targeting this pathway has emerged as a potential therapeutic strategy. COX-2 inhibitors, such as non-steroidal anti-inflammatory medications (NSAIDs) and selective COX-2 inhibitors, have been developed and extensively investigated. These inhibitors block the enzymatic activity of COX-2, reducing the production of prostaglandins and modulating downstream signaling events [31].
Multiple anti-cancer effects have been linked to the inhibition of COX-2 signaling, including the suppression of tumor cell proliferation, induction of apoptosis, inhibition of angiogenesis, and modulation of the immune system(28). COX-2 inhibitors have demonstrated efficacy as monotherapy or combined with other cancer therapies. In the prevention and treatment of colorectal cancer, their use has been linked to reduced polyp formation and enhanced survival rates [32]. COX-2 inhibitors can modulate the tumor microenvironment in addition to their direct effects on tumor cells. These inhibitors create a less favorable environment for tumor growth and metastasis by diminishing inflammation, angiogenesis, and immunosuppression. In addition, the combination of COX-2 inhibitors with other therapeutic agents, such as chemotherapy, targeted therapies, immunotherapies, and small RNA-based approaches, has shown synergistic effects and improved treatment outcomes [33, 34].
Overall, COX-2 signaling is essential to cancer biology, and targeting this pathway with COX-2 inhibitors is a promising therapeutic strategy. There is a need for additional research to elucidate the precise mechanisms of COX-2 signaling in various cancer types, identify predictive biomarkers of response, and optimize the use of COX-2 inhibitors in combination therapies. Understanding COX-2 signaling and its role in cancer can create more effective and individualized treatment methods to improve patient outcomes and quality of life [35].
Types of COX-2 inhibitors
COX-2 inhibitors, particularly selective ones, represent a promising class of drugs with the potential to revolutionize cancer treatment. These inhibitors offer a new generation of medications that can be used as adjunct therapies for cancer, providing higher efficacy and fewer side effects compared to traditional treatments. The development of selective COX-2 inhibitors has captivated the interest of scientists due to their remarkable attributes [3, 36].
However, drug resistance poses a significant challenge in cancer therapy, and overcoming it is crucial for successful treatment. Various factors contribute to drug resistance, including the activity of p-glycoprotein (p-gp) and other mechanisms. Therefore, it is imperative to develop newer drugs that exhibit a reduced incidence of drug resistance [3].
Specific selective COX-2 inhibitors, like Celecoxib and Caldecoxib, contain a primary sulfonamide moiety in their chemical structures. This sulfonamide, located in the para position of the phenyl ring attached to the central scaffold of these molecules, not only exerts a COX-2 inhibitory effect but also possesses carbonic anhydrase (CA, EC 4.2.1.1) inhibitory activity. The primary sulfonamide binds to a zinc ion at the active site of the CA enzyme, leading to the inhibition of cancer-related human CA IX isoform at nanomolar concentrations. The anti-cancer effects of these compounds may be attributed to the inhibition of carbonic anhydrase, specifically targeting isoforms IX and XII, in addition to the selective inhibition of COX-2 [37,38,39].
Acetazolamide, a primary sulfonamide compound, is a classic CA inhibitor used to treat conditions such as glaucoma and elevated intracranial pressure (ICP) [40]. Studies have indicated that acetazolamide could impede the growth of intestinal polyps in mice, suggesting the involvement of CA in the intestinal carcinogenesis process [41].
Carbonic anhydrase, a well-known zinc metalloprotein, catalyzes the reaction between carbon dioxide and water to produce bicarbonate anion (HCO3−). Solid tumors often exhibit a hypoxic environment with acidic cytoplasmic pH. Cancer cells employ specific compensatory mechanisms, including the overexpression of CA isoform IX, to survive under such unfavorable conditions. CA activity helps maintain favorable physiological conditions within tumor cells by alkalizing the acidic pH. Overexpression of CA also promotes tumor cell invasion and metastasis [42].
CA inhibition can be considered a novel anti-cancer treatment strategy since unbuffered acidic conditions in the cell cytoplasm ultimately lead to cell death. Additionally, it has been discovered that COX-1 inhibition may play a role in preventing tumorigenesis, indicating that it is not solely COX-2 involved in this process. Thus, non-selective COX inhibitors also exhibit potential as candidates for cancer prevention [43].
Despite the therapeutic benefits of selective COX-2 inhibitors in cancer and inflammation, their widespread use has been associated with adverse effects on various tissues, including the liver, kidney, and cardiovascular system. These inhibitors have been linked to myocardial infarction, hypertension, and diminished renal blood flow [44]. The exact origin of cardiac side effects, such as those observed with rofecoxib, resulting from COX-2 selectivity remains unclear [45]. It is postulated that the cardiovascular adverse effects of selective COX-2 inhibitors arise from an imbalance between thromboxane A2 (TXA2) derived from COX-1, acting as a thrombotic agent, and prostacyclin (PGI2), a vasoprotective factor derived from COX-2. The dosage and duration of treatment may influence the cardiovascular toxicity of these drugs [31].
Moreover, the unique chemical structure, pharmacokinetic profile, and production of toxic metabolites from rofecoxib may contribute to its cardiac toxicity [45]. Research suggests that both NSAIDs and COX-2 inhibitors are associated with an increased risk of gastrointestinal, renal, and cardiovascular adverse reactions [46]. Furthermore, COX-2 inhibitors have been found to induce mitochondrial toxicity by inhibiting oxidative phosphorylation in rat liver tissue mitochondria [47].
However, the potential for these side effects can be mitigated by utilizing novel drug delivery systems such as nanospheres, nanogels, microemulsions, microparticles, liposomes, monoclonal antibodies, and other advanced drug administration approaches. These innovative methods offer a way to enhance drug targeting, reduce systemic toxicity, and improve the overall safety profile of COX-2 inhibitors [48].
In conclusion, selective COX-2 inhibitors hold great promise as a new generation of drugs for cancer therapy. Their ability to inhibit COX-2 and carbonic anhydrase, particularly isoforms IX and XII, makes them potential candidates for effective anti-cancer treatment. However, drug resistance and the adverse effects of COX-2 inhibitors emphasize the need for continued research and development to enhance their efficacy, reduce side effects, and explore novel drug delivery systems.
Monotherapy with COX-2 inhibitors
In the treatment of cancer, monotherapy with COX-2 inhibitors has attracted considerable interest as a potential therapeutic approach. COX-2 inhibitors are a class of drugs that selectively inhibit the enzyme COX-2, which is implicated in inflammation and tumorigenesis. By targeting COX-2, these inhibitors provide a unique opportunity to modulate pathways associated with cancer progression, making them potential candidates for use as stand-alone therapies [49]. COX-2 inhibitors’ mechanisms of action involve their ability to inhibit COX-2, resulting in decreased prostaglandin production selectively. Prostaglandins perform crucial roles in tumor development, angiogenesis, and immune regulation. In addition, it has been demonstrated that COX-2 inhibitors induce apoptosis in cancer cells, inhibit cell proliferation, and modulate the signaling pathways involved in inflammation and cell survival [50].
Numerous cancer varieties, including colorectal, breast, lung, and prostate cancer, have been the subject of clinical studies examining the efficacy of COX-2 inhibitors as monotherapy [51,52,53,54]. While some studies have demonstrated promising results regarding decreased tumor growth, enhanced survival rates, and improved patient outcomes, the findings have not been consistent across all studies [55]. Variations in response to COX-2 inhibitor monotherapy have been observed across patient populations, highlighting the need for additional research to identify specific subgroups of patients most likely to benefit from this treatment strategy [56].
Monotherapy with COX-2 inhibitors presents several obstacles. These include determining the optimal dose and duration of treatment, managing potential adverse effects, and devising predictive biomarkers to identify patients who will respond positively to treatment. Ongoing research focuses on addressing these obstacles and optimizing the effectiveness of COX-2 inhibitor monotherapy. Combining COX-2 inhibitors with other targeted therapies or chemotherapy is being investigated to improve treatment outcomes [57].
Regarding the monotherapy with COX-2 inhibitors, Celecoxib monotherapy enhanced apoptosis in hepatocellular carcinoma by inducing the expression of CD95, tumor necrosis factor-related apoptosis-inducing ligands 1 and 2 (TRAILR1 and R2). It also promotes the expression of myeloid leukemia-1, an anti-apoptotic member of the Bcl-2 family, leading to increased tumor cell apoptosis [58]. Breast cancer experiments have shown that COX-2 inhibition with Celecoxib can significantly reduce Indoleamine 2,3-dioxygenase (IDO) levels in breast cancer, and PGE2 regulation downstream of COX-2 can also inhibit the tryptophan-consuming process of IDO [59]. Valdecoxib is a U.S.-approved non-steroidal anti-inflammatory drug. Food and Drug Administration (FDA) for the treatment of inflammatory diseases. However, it was recently reported that the anti-tumor effect of Valdecoxib induces cell proliferation and apoptosis in nasopharyngeal cancer cells and lung cancer cells. A recent study has shown that Valdecoxib monotherapy significantly reduces cell migration and proliferation and induces apoptosis in hypopharyngeal squamous cell carcinoma cells by regulating the PI3K signaling pathway [60]. Nanoparticle-loaded Etoricoxib exhibited significant cytotoxicity against lung cancer cells by inducing apoptosis/necrosis and cell cycle arrest in lung cancer cells in vitro [61].
In conclusion, monotherapy with COX-2 inhibitors is an effective cancer treatment option. The selective targeting of COX-2 and its associated pathways has potential as a stand-alone treatment for certain types of cancer despite the heterogeneity of the clinical evidence and the need for additional research. Understanding the mechanisms of action, refining treatment strategies, and undertaking well-designed clinical trials will help realize the full potential of COX-2 inhibitors as cancer monotherapy.
COX-2 inhibitors plus conventional chemotherapy
Combining COX-2 inhibitors with chemotherapy medications has been investigated as a potential method for enhancing the efficacy of cancer treatment. Chemotherapy employs a variety of medicines with distinct mechanisms of action to target and eliminate cancer cells. However, standard chemotherapy frequently results in the enrichment or induction of cancer stem cells, which can cause chemoresistance and cancer recurrence [62].
Chemotherapy is associated with severe side effects. To address these issues, researchers have investigated the combination of COX-2 inhibitors with various chemotherapy drugs, such as biological alkylating agents, anti-tumor antibiotics, and anti-tumor plant-derived medicines. The objective is to increase the efficacy of chemotherapy while decreasing its adverse effects [63].
Combination with biological alkylating agents: In chemotherapy, biological alkylating agents such as Cyclophosphamide, Temozolomide, Cisplatin, Oxaliplatin, and so on are frequently employed [64]. However, they can produce toxicity in healthy tissues. Researchers have coupled COX-2 inhibitors, such as Celecoxib, with alkylating agents to mitigate these side effects. Studies have revealed encouraging results, such as decreased toxicity, enhanced anti-tumor activity, and patient tolerability [5]. For instance, a combination of Cyclophosphamide and Celecoxib demonstrated efficacy and low toxicity in metastatic breast cancer patients [65]. Similarly, combining Celecoxib and Temozolomide improved survival rates and quality of life in malignant glioma patients [66]. The combination of Celecoxib with Cisplatin and Gefitinib increased the lethal effect of chemotherapy drugs on cancer cells. It reduced the multidrug resistance response by inhibiting COX-2 and anti-apoptotic B-cell lymphoma 2 (Bcl-2) gene expression [67]. Tolfenamic acid is a non-steroidal anti-inflammatory drug and selective COX-2 inhibitor; its combination with Cisplatin has recently been shown to enhance apoptosis in breast cancer by increasing P-53 levels [68].
Combination with antimetabolites: 5-FU combination with Celecoxib reduced Squamous cell carcinoma proliferation by alleviating the AKT pathway [69]. 5-FU combination with Celecoxib has been shown to be associated with decreased progression-free survival (PFS) and overall survival (OS) of HCC [70]. Capecitabine, an Oxaliplatin combination with Celecoxib, reduced renal cancer through inducing apoptosis and alleviating neovascularization [71].
Combination with anti-tumor antibiotics: Anti-tumor antibiotics such as doxorubicin and epirubicin are frequently used in chemotherapy for cancer [72]. They can, however, have dose-dependent adverse effects on the heart. Combining COX-2 inhibitors, such as Celecoxib, with these antibiotics has demonstrated promise in inhibiting the progression of hepatocellular carcinoma (HCC) and enhancing cytotoxic activity [73]. It has also been discovered that combination therapy suppresses hepatic cancer stem cells, inhibits tumor cell proliferation and angiogenesis, and stimulates anti-tumor immunity. Significantly, the combination therapy did not exacerbate the myelotoxicity induced by antibiotics [73]. Combining Doxorubicin and Celecoxib reduced cell proliferation in non-small lung cancer [74] and induced apoptosis in human skin cancer [75] and breast cancer [26, 33].
Combination with plant anti-tumor drugs: Anti-tumor pharmaceuticals derived from plants, such as Curcumin, Vinblastine, Vincristine, and Paclitaxel, have been studied with COX-2 inhibitors. These combinations have demonstrated synergistic anti-cancer effects in numerous cancer types. For instance, Curcumin and Celecoxib have synergistic effects against colon, pancreatic, and hepatocellular carcinomas [76,77,78]. The combinations have inhibited tumor proliferation, angiogenesis, and inflammatory factors [78]. Combining Plumbagin and Celecoxib reduced cell proliferation in melanoma by modulating the signal transducers and activators of transcription 3 (STAT3) signaling pathway [79]. Combining Tetrahydrocurcumin and Celecoxib inhibited cell angiogenesis by down-regulating the vascular endothelial growth factor (VEGF) and decreased tumor growth by alleviating EGFR in cervical cancer [80]. Utilizing nanotechnology-based delivery systems has improved the delivery and release of these medications to tumor tissues, thereby increasing their effectiveness. It is worth noting that not all combinations of COX-2 inhibitors with chemotherapy drugs result in increased anti-tumor activity. Some varieties may not show synergistic effects or may even have unfavorable interactions. Therefore, caution is required when selecting and administering these combination regimens, considering the specific characteristics of the cancer and the drugs involved [81].
Overall, combining COX-2 inhibitors with chemotherapy drugs can improve cancer treatment outcomes by increasing efficacy, minimizing side effects, and overcoming chemoresistance. Additional research and clinical trials are necessary to completely comprehend the optimal combinations, dosages, and treatment protocols for particular types of cancer.
COX-2 inhibitors plus radiotherapy
In the context of radiotherapy, COX-2 inhibitors have demonstrated promise for improving the efficacy of radiation treatment in multiple ways:
Overcoming radioresistance: Radioresistance is the capacity of cancer cells to sustain radiation exposure and continue to increase. It can reduce the effectiveness of radiotherapy. By targeting specific signaling pathways implicated in radioresistance, COX-2 inhibitors have been found to sensitize cancer cells to radiation therapy (61). For instance, they can inhibit the Janus Kinase 2 (JAK-2)/STAT3 signaling pathway, which promotes cell survival and radiation resistance. COX-2 inhibitors can make cancer cells more susceptible to the detrimental effects of radiation by interfering with these pathways [82].
Enhancing tumor response: It has been demonstrated that COX-2 inhibitors strengthen the response of tumors to radiation therapy. They can inhibit tumor growth by inhibiting cell proliferation and fostering apoptosis in cancer cells [83]. In addition, COX-2 inhibitors can reduce the expression of aggressive tumor-associated markers, such as VEGF and MMPs. These effects improve the therapeutic efficacy of radiation treatment [84].
Protecting normal tissues: One of the difficulties of radiation therapy is the potential for harm to healthy adjacent tissues. It has been discovered that COX-2 inhibitors have a protective effect on normal cells by reducing radiation-induced inflammation and toxicity. They can aid in preserving the integrity and function of normal tissues, thereby minimizing treatment-related adverse effects and enhancing patient outcomes overall [85].
In various varieties of cancer, including lung cancer, head and neck cancer, colorectal cancer, and prostate cancer, the combination of COX-2 inhibitors with radiotherapy is currently being investigated. COX-2 inhibitors combined with radiotherapy have shown promising results in preclinical models and early-phase clinical trials, demonstrating enhanced tumor control and better treatment outcomes [86,87,88,89].
However, it is essential to be aware that COX-2 inhibitors can have adverse effects, including hazards to the cardiovascular system and issues with the digestive system, mainly when used for an extended period or in specific patient populations. Because of this, these products’ usage should be considered cautiously, and medical specialists should properly supervise patients [90].
In conclusion, COX-2 inhibitors have emerged as potentially useful adjuvant therapies in cancer treatment. They are intriguing candidates for combination therapy strategies because they can circumvent radioresistance, boost tumor response, and protect normal tissues. However, additional research is required to maximize their use, identify the patient populations that would benefit the most from the treatment, discover the most effective dosage and treatment regimens, and address potential adverse effects. COX-2 inhibitors play an important part in cancer treatment; therefore, discussing this topic with a medical expert is essential for making individualized and well-informed decisions on how best to use them.
COX-2 inhibitors plus kinase inhibitors
To date, tyrosine kinase inhibitor (TKI) therapy has successfully controlled several human cancers, including estrogen receptor, progesterone receptor, and/or human epidermal growth factor receptor 2 (HER2)-positive breast cancer and non-small-cell lung cancer (NSCLC). Therefore, combination therapy may help improve drug sensitivity, and previous studies have shown that combining COX-2 inhibitors with EGFR TKIs can prevent colonic adenoma in mice due to their effects on these two signaling pathways [91].
COX-2-dependent signaling represents a potential mechanism of clinical resistance to EGFR-TKI treatment. A phase 2 clinical trial confirmed the toxicity of Erlotinib and Celecoxib for treating patients with advanced NSCLC [92]. The efficacy of Erlotinib plus Celecoxib was assessed in patients with advanced NSCLC with wild-type EGFR and determined the improved efficacy and toxicity of the therapy [93]. Another study conducted by Sun et al. showed that the combination of erlotinib and Celecoxib increased radiosensitivity after radiotherapy by blocking EGFR- and COX-2-related pathways and inducing apoptosis through the PI3K/AKT signaling pathway [94]. Another study found that Gefitinib (EGFR-TKI) and celecoxib induced apoptosis in EGFR-mutant NSCLC cell lines [94]. In this regard, Lin et al. revealed the efficacy of combining Gefitinib and Celecoxib in prostate cancer by improving tumor cell death and overcoming docetaxel resistance [95].
Vandetanib is a potent VEGFR-2 inhibitor that inhibits tumor growth and prolongs survival. Vandetanib and Celecoxib combination therapy was first reported to have a powerful anti-tumor effect on osteosarcoma in vivo and in vitro by inducing ERK phosphorylation [96]. Kaya et al. demonstrated that combining Motesanib and DuP-697 (selective COX-2 inhibitor) significantly induced apoptosis and attenuated angiogenesis in CRC cells [97]. Celecoxib and Imatinib enhanced anti-tumor activity through caspase-3 activation in CML [98]. Zhao et al. reported that the combination of Sunitinib and Celecoxib exhibited potent anti-tumor activity in renal cell carcinoma cells by significantly reducing the expression of GM-CSF and STAT3 and attenuating the levels of myeloid-derived suppressor cells (MDSCs) [99]. The combination of Sorafenib and Meloxicam (selective COX-2 inhibitor) induced apoptosis by activating endoplasmic reticulum (ER) stress in hepatocellular carcinoma (HCC) [100]. Combination therapy of Celecoxib with Sorafenib and/or sildenafil has been shown to potentently induce apoptosis by significantly reducing the expression of multiple chaperone proteins in ovarian cancer. Their combination sensitized ovarian cancer cells to platinum therapy [101].
COX-2 inhibitors plus angiogenesis inhibitors
Drugs known as angiogenesis inhibitors can thwart the angiogenesis process, also known as developing new blood vessels. This process is essential for the growth and spread of tumors because it forms new blood vessels, which provide cancer cells with nutrition and oxygen. These medications try to reduce the blood supply to tumors by preventing angiogenesis; this will starve the tumors and lead to slow down or even hinder tumor growth [102]. When COX-2 inhibitors and angiogenesis inhibitors are combined, several synergistic effects are possible:
-
A)
Anti-inflammatory and anti-angiogenic effects: Inflammation promotes angiogenesis, and COX-2 inhibitors reduce inflammation. These drugs can reduce the production of inflammatory molecules that contribute to angiogenesis by inhibiting COX-2. When combined with angiogenesis inhibitors, COX-2 inhibitors reduce inflammation and angiogenesis, thereby potentially enhancing the suppression of tumor growth and metastasis [26].
-
B)
Complementary mechanisms of action: COX-2 and angiogenesis inhibitors inhibit cancer progression via distinct mechanisms. Angiogenesis inhibitors target specific molecules implicated in angiogenesis, such as VEGF and its receptors, whereas COX-2 inhibitors primarily target the COX-2 enzyme and associated signaling pathways. The purpose of combining these medications is to attain additive or synergistic effects; this means they can simultaneously target multiple ways, addressing various aspects of tumor development and potentially resulting in improved therapeutic outcomes [103].
-
C)
Overcoming resistance: Over time, tumors can develop resistance to single-agent therapies, diminishing treatment efficacy; this resistance can be circumvented by combining COX-2 and angiogenesis inhibitors. COX-2 inhibitors can sensitize resistant tumor cells to angiogenesis inhibitors’ effects, thereby enhancing angiogenesis inhibitors’ efficacy in resistant tumors. This strategy aims to attack the cancer from numerous angles, increasing the likelihood of a successful treatment response [104].
-
D)
Improved treatment response: COX-2 inhibitors have improved the efficacy of radiation therapy, a standard cancer treatment modality. COX-2 inhibitors may augment the effectiveness of radiation treatment with angiogenesis inhibitors since COX-2 inhibitors can target both tumor cells and tumor vasculature, potentially enhancing tumor control and overall treatment efficacy [105].
Notably, the clinical benefits of combining COX-2 and angiogenesis inhibitors are still being evaluated, and additional research is necessary. The optimal scheduling, dosage, and sequencing of these medications and criteria for patient selection are being investigated. Additionally, it is essential to consider potential adverse effects and drug interactions that may arise when using combination therapies, as they may differ from those of individual drugs [106].
Ongoing clinical trials investigate the combination of COX-2 inhibitors and angiogenesis inhibitors in various cancer types, including colorectal cancer, lung cancer, and breast cancer. These studies aim to determine this combination therapy’s efficacy, safety, and optimal application. Patients can receive the most up-to-date information and treatment options regarding COX-2 and angiogenesis inhibitors for cancer by consulting with a healthcare professional and contemplating participation in clinical trials [107, 108].
COX-2 inhibitors plus other small inhibitors
miRNAs (microRNAs) and non-coding RNAs (ncRNAs) are small RNA molecules that significantly regulate genes. They regulate gene expression, and their dysregulation has been linked to numerous diseases, including malignancy. Certain microRNAs and non-coding RNAs can function as oncogenes or tumor suppressors in cancer [109].
Combining COX-2 inhibitors with miRNA or ncRNA inhibitors can have several potential benefits:
-
A)
Synergistic effects on cancer pathways: microRNAs and non-coding RNAs regulate diverse cancer-related routes, including cell proliferation, apoptosis, angiogenesis, and metastasis. By targeting these molecules, it may be possible to improve the effectiveness of COX-2 inhibitors on these pathways. The combination therapy aims to produce a synergistic effect, resulting in enhanced inhibition of tumor growth and dissemination [110].
-
B)
Overcoming treatment resistance: Resistance to single-agent cancer treatments can be a significant obstacle. Combining COX-2 inhibitors with inhibitors of microRNA or non-coding RNA may assist in overcoming this resistance. Combining therapy can potentially enhance the therapeutic response by simultaneously targeting multiple molecular pathways by addressing various mechanisms contributing to treatment resistance [111].
-
C)
Modulation of immune response: microRNAs and non-coding RNAs affect the immune response in the tumor microenvironment. Some microRNAs have been related to immune evasion by tumors [112], whereas others have been linked to immune activation and anti-tumor immune responses [113]. Targeting specific miRNAs or ncRNAs may be possible to modulate the immune response and boost the efficacy of immune-based therapies, such as immunotherapy or checkpoint inhibitors, when administered with COX-2 inhibitors [114].
-
D)
Personalized medicine approach: As potential biomarkers for cancer diagnosis, prognosis, and treatment response prediction, miRNAs and ncRNAs have demonstrated promise [115]. Integrating the analysis of these molecules with COX-2 inhibitors can facilitate the customization of patient-specific treatment strategies. Identifying specific miRNAs or ncRNAs that are dysregulated in a patient’s cancer makes it possible to devise personalized therapies that target these particular molecules and pathways [116].
Notably, the miRNA and ncRNA research field is still evolving, and the therapeutic potential of these molecules is still being investigated. In clinical trials, the combination of COX-2 inhibitors with miRNA or ncRNA inhibitors for the treatment of colorectal cancer, breast cancer, and lung cancer, among others, is being investigated. These studies aim to determine these combination therapies’ efficacy, safety, and optimal application [117,118,119].
In conclusion, combining COX-2 inhibitors with miRNA or ncRNA inhibitors bears promise as a cancer treatment strategy for enhancing the therapeutic effects of COX-2 inhibition. By simultaneously targeting multiple molecular pathways and overcoming treatment resistance, this strategy seeks to improve patient outcomes. However, additional research is necessary to comprehend these combinations’ mechanisms and clinical benefits thoroughly. Patients can obtain the most up-to-date information and personalized treatment options by consulting with healthcare professionals and contemplating participation in clinical trials (Fig. 1).
Discussion and conclusion
Combination therapy with COX-2 inhibitors is a promising strategy to improve the efficacy of cancer treatment. Extensive preclinical and clinical evidence supports the hypothesis that combining COX-2 inhibitors with other drugs can induce synergistic effects, overcome drug resistance, modulate the tumor microenvironment, and revolutionize personalized medicine. Combining COX-2 inhibitors with miRNAs, ncRNAs, angiogenesis inhibitors, immunotherapy, and conventional chemotherapy agents improved anti-tumor activity compared with monotherapy. This combination enhances treatment response and extends disease control by targeting pathways involved in tumor growth, angiogenesis, immune evasion, and drug resistance. Combination therapies have the potential to address the complexity and heterogeneity of cancer by capitalizing on the unique mechanisms of action of COX-2 inhibitors and their ability to modulate diverse molecular and cellular processes [120, 121].
Combination therapy has the potential to overcome drug resistance, which is a significant advantage. Combination therapies can bypass the adaptive mechanisms used by cancer cells, thereby avoiding treatments that target multiple signaling pathways and cellular processes. This strategy represents a significant change in cancer treatment and offers a new treatment option for patients resistant to existing treatments. In addition, combination therapy with COX-2 inhibitors could modify the tumor microenvironment, thereby improving the immune environment. By reducing immunosuppression and increasing anti-tumor immune responses, these combinations may enhance the efficacy of immunotherapy and pave the way for new immunomodulatory approaches. The tumor microenvironment plays a critical role in tumor progression and treatment response, and combination therapies target this dynamic ecosystem, providing a comprehensive approach to cancer treatment [122, 123].
Clinicians can tailor treatment regimens to individual patients by identifying specific molecular targets, biomarkers, and patient characteristics, maximizing treatment efficacy and minimizing side effects. Identifying patients most likely to benefit from combination therapy will improve treatment outcomes, optimize resource allocation, and reduce treatment-related toxicities. However, it must be recognized that the safety and tolerability of combination therapy must be carefully evaluated. However, the safety profile of COX-2 inhibitors is well established, and their combination with other drugs was generally well tolerated in early clinical trials. Monitoring and managing potential side effects and drug interactions is essential to ensure patient safety and optimize treatment outcomes. Combination therapy with COX-2 inhibitors has the potential to improve cancer outcomes significantly. Multifaceted strategies involving microRNAs, noncoding RNAs, angiogenesis inhibitors, immunotherapy, and conventional chemotherapy agents provide a comprehensive blueprint to address the complex biology of cancer. Potential impacts of combination therapy include increased anti-tumor activity, elimination of drug resistance, modification of the tumor microenvironment, personalized drug delivery approaches, and favorable safety profile [124, 125].
In conclusion, although preclinical and early clinical trial results are promising, further studies are needed to confirm these findings and determine the functionality of COX-2 inhibitor combination therapies in routine clinical practice. Large-scale clinical trials, comprehensive biomarker studies, and in-depth mechanistic studies are needed to fully understand the therapeutic potential and optimize the use of COX-2 inhibitors in combination with other modalities. By harnessing the power of combination therapies, we can improve patient outcomes, extend survival, and ultimately move closer to a future where cancer is easier to manage and treat; however, further studies are needed to determine the exact role of COX as well as its corresponding pathways and its hindering in cancer (Table 1).
Data availability
Data sharing does not apply to this article as no new data were created or analyzed in this review study.
Abbreviations
- COX:
-
Cyclooxygenases
- Ptgs2:
-
Prostaglandin-endoperoxide synthase 2
- PGE2:
-
Prostaglandin E2
- DMBA:
-
7,12-dimethylbenz[a]anthracene
- EP1:
-
Prostaglandin E2 receptor 1
- EGFR:
-
Epidermal growth factor receptor
- MMPs:
-
Matrix metalloproteinases
- TGF2:
-
Transforming growth factor 2
- PI3K:
-
Phosphatidylinositol 3-kinase
- AKT:
-
protein kinase B
- NSAIDs:
-
Non-steroidal anti-inflammatory medications
- ICP:
-
Intracranial pressure
- TXA2:
-
Thromboxane A2
- TRAILR:
-
Tumor necrosis factor-related apoptosis-inducing ligand Receptor
- IDO:
-
Indoleamine 2,3-dioxygenase
- BCL-2:
-
B-cell lymphoma 2
- OS:
-
Overall survival
- STAT3:
-
Signal transducers and activators of transcription 3
- VEGF:
-
vascular endothelial growth factor
- JAK-2:
-
Janus Kinase 2
- TKI:
-
Tyrosine kinase inhibitor
- HER2:
-
Human epidermal growth factor receptor 2
- NSCLC:
-
Non-small-cell lung cancer
- MDSCs:
-
Myeloid-derived suppressor cells
- ER:
-
Endoplasmic reticulum
- HCC:
-
Hepatocellular carcinoma
- miRNA:
-
MicroRNA
- ncRNAs:
-
Non-coding RNAs
- MDR:
-
Multidrug resistance protein 1
- NF-κB:
-
Nuclear factor kappa B
- LRP:
-
low-density lipoprotein receptor-related protein-1
- mTOR:
-
Mammalian target of rapamycin
- ABCB1:
-
Adenosine triphosphate–binding cassette subfamily B member 1
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F, Global Cancer Statistics 2020. GLOBOCAN estimates of incidence and mortality Worldwide for 36 cancers in 185 Countries. CA: Canc J Clin. 2021;71:209–49.
Fodale V, Pierobon M, Liotta L, Petricoin E. Mechanism of cell adaptation: when and how do cancer cells develop chemoresistance? Cancer J (Sudbury Mass). 2011;17:89–95.
Xu XC. COX-2 inhibitors in cancer treatment and prevention, a recent development. Anticancer Drugs. 2002;13:127–37.
Wang D, Guo XZ, Li HY, Zhao JJ, Shao XD, Wu CY. Prognostic significance of cyclooxygenase-2 protein in Pancreatic cancer: a meta-analysis. Tumour Biol. 2014;35:10301–7.
Li S, Jiang M, Wang L, Yu S. Combined chemotherapy with cyclooxygenase-2 (COX-2) inhibitors in treating human cancers: recent advancement. Biomed Pharmacother. 2020;129:110389.
Mahboubi Rabbani SMI, Zarghi A. Selective COX-2 inhibitors as anti-cancer agents: a patent review (2014–2018). Exp Opinion Ther Pat. 2019;29:407–27.
El-Malah AA, Gineinah MM, Deb PK, Khayyat AN, Bansal M, Venugopala KN, Aljahdali AS. Selective COX-2 inhibitors: road from success to controversy and the quest for repurposing. Pharmaceuticals. 2022;15(7):827.
Dannenberg AJ, Zakim D. Chemoprevention of Colorectal cancer through inhibition of cyclooxygenase-2. Semin Oncol. 1999;26:499–504.
Eling TE, Thompson DC, Foureman GL, Curtis JF, Hughes MF. Prostaglandin H synthase and xenobiotic oxidation. Annu Rev Pharmacol Toxicol. 1990;30:1–45.
Wiese FW, Thompson PA, Kadlubar FF. Carcinogen substrate specificity of human COX-1 and COX-2. Carcinogenesis. 2001;22:5–10.
Liu CH, Chang SH, Narko K, Trifan OC, Wu MT, Smith E, Haudenschild C, Lane TF, Hla T. Overexpression of cyclooxygenase-2 is sufficient to induce tumorigenesis in transgenic mice. J Biol Chem. 2001;276:18563–9.
Muller-Decker K, Neufang G, Berger I, Neumann M, Marks F, Furstenberger G. Transgenic cyclooxygenase-2 overexpression sensitizes mouse skin for carcinogenesis. Proc Natl Acad Sci USA. 2002;99:12483–8.
Oshima M, Dinchuk JE, Kargman SL, Oshima H, Hancock B, Kwong E, Trzaskos JM, Evans JF, Taketo MM. Suppression of intestinal polyposis in apc delta716 knockout mice by inhibition of cyclooxygenase 2 (COX-2). Cell. 1996;87:803–9.
Sonoshita M, Takaku K, Sasaki N, Sugimoto Y, Ushikubi F, Narumiya S, Oshima M, Taketo MM. Acceleration of intestinal polyposis through prostaglandin receptor EP2 in apc(Delta 716) knockout mice. Nat Med. 2001;7:1048–51.
Sheng H, Shao J, Morrow JD, Beauchamp RD, DuBois RN. Modulation of apoptosis and Bcl-2 expression by prostaglandin E2 in human colon Cancer cells. Cancer Res. 1998;58:362–6.
Pai R, Soreghan B, Szabo IL, Pavelka M, Baatar D, Tarnawski AS. Prostaglandin E2 transactivates EGF receptor: a novel mechanism for promoting colon Cancer growth and gastrointestinal hypertrophy. Nat Med. 2002;8:289–93.
Dannenberg AJ, Lippman SM, Mann JR, Subbaramaiah K, DuBois RN. Cyclooxygenase-2 and epidermal growth factor receptor: pharmacologic targets for chemoprevention. J Clin Oncology: Official J Am Soc Clin Oncol. 2005;23:254–66.
Buchanan FG, Wang D, Bargiacchi F, DuBois RN. Prostaglandin E2 regulates cell migration via the intracellular activation of the epidermal growth factor receptor. J Biol Chem. 2003;278:35451–7.
Shao J, Lee SB, Guo H, Evers BM, Sheng H. Prostaglandin E2 stimulates the growth of colon Cancer cells via induction of amphiregulin. Cancer Res. 2003;63:5218–23.
Laronha H, Caldeira J. Structure and function of human matrix metalloproteinases. Cells. 2020;9(5):1076.
Tsujii M, Kawano S, DuBois RN. Cyclooxygenase-2 expression in human colon Cancer cells increases metastatic potential. Proc Natl Acad Sci USA. 1997;94:3336–40.
Attiga FA, Fernandez PM, Weeraratna AT, Manyak MJ, Patierno SR. Inhibitors of prostaglandin synthesis inhibit human prostate Tumor cell invasiveness and reduce the release of matrix metalloproteinases. Cancer Res. 2000;60:4629–37.
Tsujii M, DuBois RN. Alterations in cellular adhesion and apoptosis in epithelial cells overexpressing prostaglandin endoperoxide synthase 2. Cell. 1995;83:493–501.
Kakiuchi Y, Tsuji S, Tsujii M, Murata H, Kawai N, Yasumaru M, Kimura A, Komori M, Irie T, Miyoshi E, Sasaki Y, Hayashi N, Kawano S, Hori M. Cyclooxygenase-2 activity altered the cell-surface carbohydrate antigens on colon cancer cells and enhanced liver metastasis. Cancer Res. 2002;62:1567–72.
Tian J, Wang V, Wang N, Khadang B, Boudreault J, Bakdounes K, Ali S, Lebrun JJ. Identification of MFGE8 and KLK5/7 as mediators of breast tumorigenesis and resistance to COX-2 inhibition. Breast Cancer Res. 2021;23(1):1–8.
Zhang T, Liu H, Li Y, Li C, Wan G, Chen B, Li C, Wang Y. A pH-sensitive nanotherapeutic system based on a marine sulfated polysaccharide for the treatment of metastatic Breast cancer through combining chemotherapy and COX-2 inhibition. Acta Biomater. 2019;99:412–25.
Takahashi T, Kozaki K, Yatabe Y, Achiwa H, Hida T. Increased expression of COX-2 in the development of human lung cancers. J Environ Pathol Toxicol Oncol. 2002;21:177–81.
Jin K, Qian C, Lin J, Liu B. Cyclooxygenase-2-Prostaglandin E2 pathway: a key player in tumor-associated immune cells. Front Oncol. 2023;13:1099811.
Zhao H, Ming T, Tang S, Ren S, Yang H, Liu M, Tao Q, Xu H. Wnt signaling in Colorectal cancer: pathogenic role and therapeutic target. Mol Cancer. 2022;21:144.
Geindreau M, Bruchard M, Vegran F. Role of cytokines and chemokines in angiogenesis in a tumor context. Cancers. 2022;14(10):2446.
Zarghi A, Arfaei S. Selective COX-2 inhibitors: a review of their structure-activity relationships. Iran J Pharm Res: IJPR. 2011;10:655–83.
Zhang Z, Ghosh A, Connolly PJ, King P, Wilde T, Wang J, Dong Y, Li X, Liao D, Chen H, Tian G, Suarez J, Bonnette WG, Pande V, Diloreto KA, Shi Y, Patel S, Pietrak B, Szewczuk L, Sensenhauser C, Dallas S, Edwards JP, Bachman KE, Evans DC. Gut-restricted selective Cyclooxygenase-2 (COX-2) inhibitors for chemoprevention of colorectal cancer. J Med Chem. 2021;64:11570–96.
Zhang S, Guo N, Wan G, Zhang T, Li C, Wang Y, Wang Y, Liu Y. pH and redox dual-responsive nanoparticles based on disulfide-containing poly(β-amino ester) for combining chemotherapy and COX-2 inhibitor to overcome drug resistance in breast cancer. J Nanobiotechnol. 2019;17:109.
Amit A, Yadav S, Singh RP, Kumar C. Development of RNA-Based medicine for colorectal cancer: current scenario. In: Colon cancer diagnosis and therapy. 3rd ed. Heidelberg: Springer; 2022. p. 339–60.
Jara-Gutiérrez A, Baladrón V. The role of prostaglandins in different types of cancer. Cells. 2021;10(6):1487.
Lee Y, Rodriguez C, Dionne RA. The role of COX-2 in acute pain and the use of selective COX-2 inhibitors for acute pain relief. Curr Pharm Des. 2005;11:1737–55.
De Monte C, Carradori S, Gentili A, Mollica A, Trisciuoglio D, Supuran CT. Dual cyclooxygenase and carbonic anhydrase inhibition by non-steroidal anti-inflammatory drugs for the treatment of cancer. Curr Med Chem. 2015;22:2812–8.
Supuran CT, Casini A, Mastrolorenzo A, Scozzafava A. COX-2 selective inhibitors, carbonic anhydrase inhibition and anti-cancer properties of sulfonamides belonging to this class of pharmacological agents. Mini Rev Med Chem. 2004;4:625–32.
Dogné JM, Thiry A, Pratico D, Masereel B, Supuran CT. Dual carbonic anhydrase–cyclooxygenase-2 inhibitors. Curr Top Med Chem. 2007;7:885–91.
Temperini C, Cecchi A, Scozzafava A, Supuran CT. Carbonic anhydrase inhibitors. Sulfonamide diuretics revisited–old leads for new applications? Org Biomol Chem. 2008;6(14):2499–506.
Noma N, Fujii G, Miyamoto S, Komiya M, Nakanishi R, Shimura M, Tanuma SI, Mutoh M. Impact of acetazolamide, a carbonic anhydrase inhibitor, on the development of intestinal polyps in min mice. Int J Mol Sci. 2017;18(4):851.
Singh S, Lomelino CL, Mboge MY, Frost SC, McKenna R. Cancer drug development of carbonic anhydrase inhibitors beyond the active site. Molecules (Basel). 2018;23(5):1045.
Pannunzio A, Coluccia M. Cyclooxygenase-1 (COX-1) and COX-1 inhibitors in cancer: a review of oncology and medicinal chemistry literature. Pharmaceuticals (Basel). 2018;11(4):101.
Mattia C, Coluzzi F. COX-2 inhibitors: pharmacological data and adverse effects. Minerva Anestesiol. 2005;71:461–70.
Davies NM, Jamali F. COX-2 selective inhibitors cardiac toxicity: getting to the heart of the matter. J Pharm Pharm Sci. 2004;7:332–6.
Mathew ST, Devi SG, Prasanth VV, Vinod B. Efficacy and safety of COX-2 Inhibitors in the clinical management of arthritis: Mini review. ISRN Pharmacol. 2011;2011:480291.
Syed M, Skonberg C, Hansen SH. Mitochondrial toxicity of selective COX-2 inhibitors via inhibition of oxidative phosphorylation (ATP synthesis) in rat liver mitochondria. Toxicol Vitro. 2016;32:26–40.
Bansal SS, Joshi A, Bansal AK. New dosage formulations for targeted delivery of cyclo-oxygenase-2 inhibitors: focus on use in the elderly. Drugs Aging. 2007;24:441–51.
Moon H, White AC, Borowsky AD. New insights into the functions of Cox-2 in skin and esophageal malignancies. Exp Mol Med. 2020;52:538–47.
Zhang P, He D, Song E, Jiang M, Song Y. Celecoxib enhances the sensitivity of non-small-cell lung cancer cells to radiation-induced apoptosis through downregulation of the Akt/mTOR signaling pathway and COX-2 expression. PLoS ONE. 2019;14:e0223760.
Fournier DB, Gordon GB. COX-2 and colon cancer: potential targets for chemoprevention. J Cell Biochem Suppl. 2000;34:97–102.
Arun B, Goss P. The role of COX-2 inhibition in Breast cancer treatment and prevention. Semin Oncol. 2004;31:22–9.
Klenke FM, Abdollahi A, Bischof M, Gebhard M-M, Ewerbeck V, Huber PE, Sckell A. Celecoxib enhances radiation response of secondary bone tumors of a human non-small cell Lung cancer via antiangiogenesis in vivo. Strahlenther Onkol. 2011;187:45–51.
Garg R, Blando JM, Perez CJ, Lal P, Feldman MD, Smyth EM, Ricciotti E, Grosser T, Benavides F, Kazanietz MG. COX-2 mediates pro-tumorigenic effects of PKCε in Prostate cancer. Oncogene. 2018;37:4735–49.
Ghosh N, Chaki R, Mandal V, Mandal SC. COX-2 as a target for cancer chemotherapy. Pharmacol Rep. 2010;62:233–44.
El-Malah AA, Gineinah MM, Deb PK, Khayyat AN, Bansal M, Venugopala KN, Aljahdali AS. Selective COX-2 Inhibitors: road from success to controversy and the quest for repurposing. Pharmaceuticals (Basel). 2022;15(7):827.
Pu D, Yin L, Huang L, Qin C, Zhou Y, Wu Q, Li Y, Zhou Q, Li L. Cyclooxygenase-2 inhibitor: a potential combination strategy with immunotherapy in cancer. Front Oncol. 2021;11:637504.
Wen B, Wei YT, Mu LL, Wen GR, Zhao K. The molecular mechanisms of celecoxib in tumor development. Medicine. 2020;99:e22544.
Curry JM, Besmer DM, Erick TK, Steuerwald N, Das Roy L, Grover P, Rao S, Nath S, Ferrier JW, Reid RW, Mukherjee P. Indomethacin enhances anti-tumor efficacy of a MUC1 peptide vaccine against Breast cancer in MUC1 transgenic mice. PLoS ONE. 2019;14:e0224309.
Trang NTK, Yoo H. Anti-tumor effects of Valdecoxib on hypopharyngeal squamous carcinoma cells. Korean J Physiol Pharmacol: Offl J Korean Physiol Soc Korean Soc Pharmacol. 2022;26:439–46.
Md S, Alhakamy NA, Alharbi WS, Ahmad J, Shaik RA, Ibrahim IM, Ali J. Development and evaluation of repurposed etoricoxib loaded nanoemulsion for improving anti-cancer activities against lung cancer cells. Int J Mol Sci. 2021;22(24):13284.
Das M, Law S. Role of tumor microenvironment in cancer stem cell chemoresistance and recurrence. Int J Biochem Cell Biol. 2018;103:115–24.
Rehman FU, Al-Waeel M, Naz SS, Shah KU. Anti-cancer therapeutics: a brief account on wide refinements. Am J cancer Res. 2020;10:3599–621.
Scott WW, Johnson DE, Schmidt JE, Gibbons RP, Prout GR, Joiner JR, Saroff J, Murphy GP. Chemotherapy of advanced prostatic carcinoma with cyclophosphamide or 5-fluorouracil: results of first national randomized study. J Urol. 1975;114:909–11.
Perroud HA, Alasino CM, Rico MJ, Mainetti LE, Queralt F, Pezzotto SM, Rozados VR. Graciela Scharovsky, metastatic Breast cancer patients treated with low-dose metronomic chemotherapy with cyclophosphamide and celecoxib: clinical outcomes and biomarkers of response. Cancer Chemother Pharmacol. 2016;77:365–74.
Stockhammer F, Misch M, Koch A, Czabanka M, Plotkin M, Blechschmidt C, Tuettenberg J, Vajkoczy P. Continuous low-dose temozolomide and Celecoxib in recurrent glioblastoma. J Neurooncol. 2010;100:407–15.
Lin XM, Li S, Zhou C, Li RZ, Wang H, Luo W, Huang YS, Chen LK, Cai JL, Wang TX, Zhang QH, Cao H, Wu XP. Cisplatin induces chemoresistance through the PTGS2-mediated anti-apoptosis in gastric cancer. Int J Biochem Cell Biol. 2019;116:105610.
Yang CX, Xing L, Chang X, Zhou TJ, Bi YY, Yu ZQ, Zhang ZQ, Jiang HL. Synergistic Platinum(II) prodrug nanoparticles for enhanced breast cancer therapy. Mol Pharm. 2020;17:1300–9.
Sung MW, Lee DY, Park SW, Oh SM, Choi JJ, Shin ES, Kwon SK, Ahn SH, Kim YH. Celecoxib enhances the inhibitory effect of 5-FU on human squamous cell carcinoma proliferation by ROS production. Laryngoscope. 2017;127:E117–e123.
Guo Q, Li Q, Wang J, Liu M, Wang Y, Chen Z, Ye Y, Guan Q, Zhou Y. A comprehensive evaluation of clinical efficacy and safety of Celecoxib in combination with chemotherapy in metastatic or postoperative recurrent gastric cancer patients: a preliminary, three-center, clinical trial study. Medicine. 2019;98:e16234.
Araujo-Mino EP, Patt YZ, Murray-Krezan C, Hanson JA, Bansal P, Liem BJ, Rajput A, Fekrazad MH, Heywood G, Lee FC. Phase II trial using a combination of oxaliplatin, capecitabine, and celecoxib with concurrent radiation for newly diagnosed resectable rectal cancer. Oncologist. 2018;23:2-e5.
Khasraw M, Bell R, Dang C. Epirubicin: is it like doxorubicin in Breast cancer? A clinical review. Breast. 2012;21:142–9.
Cox J, Weinman S. Mechanisms of doxorubicin resistance in hepatocellular carcinoma. Hepatic Oncol. 2016;3:57–9.
Shi L, Xu L, Wu C, Xue B, Jin X, Yang J, Zhu X. Celecoxib-induced self-assembly of smart albumin-doxorubicin conjugate for enhanced cancer therapy. ACS Appl Mater Interfaces. 2018;10(10):8555–65.
Singh S. Liposome encapsulation of doxorubicin and celecoxib in combination inhibits progression of human skin cancer cells. Int J Nanomed. 2018;13:11–3.
Abdallah FM, Helmy MW, Katary MA, Ghoneim AI. Synergistic antiproliferative effects of Curcumin and Celecoxib in hepatocellular carcinoma HepG2 cells. Naunyn-Schmiedeberg’s Arch Pharmacol. 2018;391:1399–410.
Lev-Ari S, Zinger H, Kazanov D, Yona D, Ben-Yosef R, Starr A, Figer A, Arber N. Curcumin synergistically potentiates the growth inhibitory and pro-apoptotic effects of celecoxib in pancreatic adenocarcinoma cells. Biomed Pharmacother. 2005;59:276-S280.
Lev-Ari S, Strier L, Kazanov D, Madar-Shapiro L, Dvory-Sobol H, Pinchuk I, Marian B, Lichtenberg D, Arber N. Celecoxib and curcumin synergistically inhibit the growth of colorectal cancer cells. Clin Cancer Res. 2005;11:6738–44.
Gowda R, Kardos G, Sharma A, Singh S, Robertson GP. Nanoparticle-based celecoxib and plumbagin for the synergistic treatment of melanoma. Mol Cancer Ther. 2017;16:440–52.
Yoysungnoen B, Bhattarakosol O, Changtam C, Patumraj S. Combinational treatment effect of tetrahydrocurcumin and celecoxib on cervical cancer cell-induced tumor growth and tumor angiogenesis in nude mice. J Med Association Thailand = Chotmaihet Thangphaet. 2016;99(4):23–31.
Chehelgerdi M, Chehelgerdi M, Allela OQB, Pecho RDC, Jayasankar N, Rao DP, Thamaraikani T, Vasanthan M, Viktor P, Lakshmaiya N, Saadh MJ, Amajd A, Abo-Zaid MA, Castillo-Acobo RY, Ismail AH, Amin AH. Akhavan-Sigari, progressing nanotechnology to improve targeted cancer treatment: overcoming hurdles in its clinical implementation. Mol Cancer. 2023;22:169.
Kim W, Son B, Lee S, Do H, Youn B. Targeting the enzymes involved in arachidonic acid metabolism to improve radiotherapy. Cancer Metastasis Rev. 2018;37:213–25.
Nakata E, Mason KA, Hunter N, Husain A, Raju U, Liao Z, Ang KK, Milas L. Potentiation of Tumor response to radiation or chemoradiation by selective cyclooxygenase-2 enzyme inhibitors. Int J Radiation Oncology* Biology* Phys. 2004;58:369–75.
Amano H, Ito Y, Suzuki T, Kato S, Matsui Y, Ogawa F, Murata T, Sugimoto Y, Senior R, Kitasato H. Roles of a prostaglandin E-type receptor, EP3, in upregulation of matrix metalloproteinase‐9 and vascular endothelial growth factor during enhancement of tumor Metastasis. Cancer Sci. 2009;100:2318–24.
Salehifar E, Hosseinimehr SJ. The use of cyclooxygenase-2 inhibitors for improvement of efficacy of radiotherapy in cancers. Drug Discovery Today. 2016;21:654–62.
Sandler AB, Dubinett SM. COX-2 inhibition and lung cancer. In: Seminars in oncology. Amsterdam: Elsevier; 2004. p. 45–52.
Halamka M, Cvek J, Kubes J, Zavadova E, Kominek P, Horacek J, Dusek L, Feltl D. Plasma levels of vascular endothelial growth factor during and after radiotherapy in combination with Celecoxib in patients with advanced Head and Neck cancer. Oral Oncol. 2011;47:763–7.
Kefayat A, Ghahremani F, Safavi A, Hajiaghababa A. Moshtaghian, c-phycocyanin: a natural product with radiosensitizing property for enhancement of colon Cancer radiation therapy efficacy through inhibition of COX-2 expression. Sci Rep. 2019;9:19161.
King L, Christie D, Arora D, Anoopkumar-Dukie S. Cyclooxygenase-2 inhibitors delay relapse and reduce prostate specific Antigen (PSA) velocity in patients treated with radiotherapy for nonmetastatic Prostate cancer: a pilot study. Prostate Int. 2020;8:34–40.
Walker C. Are All Oral COX-2 Selective Inhibitors the Same? A Consideration of Celecoxib, Etoricoxib, and Diclofenac. International journal of rheumatology. 2018;2018:1302835. https://doi.org/10.1155/2018/1302835.
Liu H, Ruan S, Larsen ME, Tan C, Liu B, Lyu H. Trastuzumab-resistant Breast cancer cells-derived Tumor xenograft models exhibit distinct sensitivity to lapatinib treatment in vivo. Biol Procedures Online. 2023;25:19.
Reckamp KL, Koczywas M, Cristea MC, Dowell JE, Wang HJ, Gardner BK, Milne GL, Figlin RA, Fishbein MC, Elashoff RM, Dubinett SM. Randomized phase 2 trial of erlotinib in combination with high-dose celecoxib or placebo in patients with advanced non-small cell Lung cancer. Cancer. 2015;121:3298–306.
Jin YH, Li WH, Bai Y, Ni L. Efficacy of erlotinib and celecoxib for patients with advanced non-small cell Lung cancer: a retrospective study. Medicine. 2019;98:e14785.
Sun J, Liu NB, Zhuang HQ, Zhao LJ, Yuan ZY, Wang P. Celecoxib-erlotinib combination treatment enhances radiosensitivity in A549 human lung cancer cell. Cancer biomarkers. 2017;19(1):45–50.
Li N, Li H, Su F, Li J, Ma X, Gong P. Relationship between epidermal growth factor receptor (EGFR) mutation and serum cyclooxygenase-2 level, and the synergistic effect of Celecoxib and Gefitinib on EGFR expression in non-small cell Lung cancer cells. Int J Clin Exp Pathol. 2015;8:9010–20.
Liu J, Wu J, Zhou L, Pan C, Zhou Y, Du W, Chen JM, Zhu X, Shen J, Chen S, Liu RY, Huang W. ZD6474, a new treatment strategy for human osteosarcoma, and its potential synergistic effect with Celecoxib. Oncotarget. 2015;6(25):21341–52.
Kaya TT, Altun A, Turgut NH, Ataseven H, Koyluoglu G. Effects of a multikinase inhibitor Motesanib (AMG 706) alone and combined with the selective DuP-697 COX-2 inhibitor on Colorectal Cancer cells. Asian Pac J cancer Prevention: APJCP. 2016;17:1103–10.
Atari-Hajipirloo S, Nikanfar S, Heydari A, Noori F, Kheradmand F. The effect of Celecoxib and its combination with Imatinib on human HT-29 Colorectal cancer cells: involvement of COX-2, Caspase-3, VEGF and NF-κB genes expression. Cellular Mol Biol. 2016;62:68–74.
Zhao Q, Guo J, Wang G, Chu Y, Hu X. Suppression of immune regulatory cells with combined therapy of Celecoxib and sunitinib in renal cell carcinoma. Oncotarget. 2017;8:1668–77.
Zhong J, Xiu P, Dong X, Wang F, Wei H, Wang X, Xu Z, Liu F, Li T, Wang Y, Li J. Meloxicam combined with sorafenib synergistically inhibits Tumor growth of human hepatocellular carcinoma cells via ER stress-related apoptosis. Oncol Rep. 2015;34:2142–50.
Webb T, Carter J, Roberts JL, Poklepovic A, McGuire WP, Booth L, Dent P. Celecoxib enhances [sorafenib + sildenafil] lethality in cancer cells and reverts platinum chemotherapy resistance. Cancer Biol Ther. 2015;16:1660–70.
Dudley AC, Griffioen AW. Pathological angiogenesis: mechanisms and therapeutic strategies. Angiogenesis. 2023;26:313–47.
Sui W, Zhang Y, Wang Z, Wang Z, Jia Q, Wu L, Zhang W. Anti-tumor effect of a selective COX-2 inhibitor, Celecoxib, may be attributed to angiogenesis inhibition through modulating the PTEN/PI3K/Akt/HIF-1 pathway in an H22 murine hepatocarcinoma model. Oncol Rep. 2014;31:2252–60.
Hwang J-T, Ha J, Park OJ. Combination of 5-fluorouracil and genistein induces apoptosis synergistically in chemo-resistant cancer cells through the modulation of AMPK and COX-2 signaling pathways. Biochem Biophys Res Commun. 2005;332:433–40.
Sminia P, Kuipers G, Geldof A, Lafleur V, Slotman B. COX-2 inhibitors act as radiosensitizer in tumor treatment. Biomed Pharmacother. 2005;59:272-S275.
Albini A, Pennesi G, Donatelli F, Cammarota R, De Flora S, Noonan DM. Cardiotoxicity of anti-cancer Drugs: the need for cardio-oncology and cardio-oncological prevention. J Natl Cancer Inst. 2010;102:14–25.
Ioakeim-Skoufa I, Tobajas-Ramos N, Menditto E, Aza-Pascual-Salcedo M, Gimeno-Miguel A, Orlando V, González-Rubio F, Fanlo-Villacampa A, Lasala-Aza C, Ostasz E. Drug repurposing in oncology: a systematic review of randomized controlled clinical trials. Cancers. 2023;15(11):2972.
Jaaks P, Coker EA, Vis DJ, Edwards O, Carpenter EF, Leto SM, Dwane L, Sassi F, Lightfoot H, Barthorpe S, van der Meer D, Yang W, Beck A, Mironenko T, Hall C, Hall J, Mali I, Richardson L, Tolley C, Morris J, Thomas F, Lleshi E, Aben N, Benes CH, Bertotti A, Trusolino L, Wessels L, Garnett MJ. Effective drug combinations in breast, colon and pancreatic cancer cells. Nature. 2022;603:166–73.
Oliveto S, Mancino M, Manfrini N, Biffo S. Role of microRNAs in translation regulation and cancer. World J Biol Chem. 2017;8:45–56.
Mishan MA, Tabari MAK, Zargari M, Bagheri A. MicroRNAs in the anti-cancer effects of Celecoxib: a systematic review. Eur J Pharmacol. 2020;882:173325.
Fanale D, Castiglia M, Bazan V, Russo A. Involvement of non-coding RNAs in chemo-and radioresistance of colorectal cancer. Non-coding RNAs Colorectal Cancer. 2016;937:207–28.
Yi M, Xu L, Jiao Y, Luo S, Li A, Wu K. The role of cancer-derived microRNAs in cancer immune escape. J Hematol Oncol. 2020;13:1–14.
Rezaei R, Baghaei K, Hashemi SM, Zali MR, Ghanbarian H, Amani D. Tumor-derived exosomes enriched by miRNA-124 promote anti-tumor immune response in CT-26 tumor-bearing mice. Front Med. 2021;8:619939.
Gong Z, Huang W, Wang B, Liang N, Long S, Li W, Zhou Q. Interplay between cyclooxygenase–2 and microRNAs in cancer. Mol Med Rep. 2021;23:1–10.
Pucci P. Combination therapy and noncoding RNAs: A new era of cancer personalized medicine. Epigenomics. 2022;14(3):117–20.
Uramova S, Kubatka P, Dankova Z, Kapinova A, Zolakova B, Samec M, Zubor P, Zulli A, Valentova V, Kwon TK. Plant natural modulators in Breast cancer prevention: status quo and future perspectives reinforced by predictive, preventive, and personalized medical approach. EPMA J. 2018;9:403–19.
Sun P, Quan J-C, Wang S, Zhuang M, Liu Z, Guan X, Wang G-Y, Wang H-Y, Wang X-S. lncRNA-PACER up-regulates COX-2 and PGE2 through the NF-κB pathway to promote the proliferation and invasion of Colorectal-cancer cells. Gastroenterol Rep. 2021;9:257–68.
Harati R, Mabondzo A, Tlili A, Khoder G, Mahfood M, Hamoudi R. Combinatorial targeting of microRNA-26b and microRNA-101 exerts a synergistic inhibition on cyclooxygenase-2 in brain metastatic triple-negative breast cancer cells. Breast Cancer Res Treat. 2021;187:695–713.
Desind SZ, Iacona JR, Christina YY, Mitrofanova A, Lutz CS. PACER lncRNA regulates COX-2 expression in Lung cancer cells. Oncotarget. 2022;13:291.
Tudor DV, Bâldea I, Lupu M, Kacso T, Kutasi E, Hopârtean A, Stretea R, Gabriela Filip A. COX-2 as a potential biomarker and therapeutic target in Melanoma. Cancer Biol Med. 2020;17:20–31.
Silva JPN, Pinto B, Monteiro L, Silva PMA, Bousbaa H. Combination therapy as a promising way to fight oral cancer. Pharmaceutics. 2023;15(6):1653.
Bayat Mokhtari R, Homayouni TS, Baluch N, Morgatskaya E, Kumar S, Das B, Yeger H. Combination therapy in combating cancer. Oncotarget. 2017;8:38022–43.
Ahronian LG, Corcoran RB. Strategies for monitoring and combating resistance to combination kinase inhibitors for cancer therapy. Genome Med. 2017;9:1–12.
Wang RC, Wang Z. Precision medicine: Disease subtyping and tailored treatment. Cancers. 2023;15(15):3837.
Goetz LH, Schork NJ. Personalized medicine: motivation, challenges, and progress. Fertil Steril. 2018;109:952–63.
Perroud HA, Alasino CM, Rico MJ, Mainetti LE, Queralt F, Pezzotto SM, Rozados VR, Scharovsky OG. Metastatic Breast cancer patients treated with low-dose metronomic chemotherapy with cyclophosphamide and celecoxib: clinical outcomes and biomarkers of response. Cancer Chemother Pharmacol. 2016;77:365–74.
Chu TH, Chan HH, Hu TH, Wang EM, Ma YL, Huang SC, Wu JC, Chang YC, Weng WT, Wen ZH, Wu DC, Chen YA, Tai MH. Celecoxib enhances the therapeutic efficacy of epirubicin for Novikoff hepatoma in rats. Cancer Med. 2018;7:2567–80.
Cao Y, Qu J, Li C, Yang D, Hou K, Zheng H, Liu Y, Qu X. Celecoxib sensitizes gastric cancer to rapamycin via inhibition of the Cbl-b-regulated PI3K/Akt pathway, tumour biology. J Int Soc Oncodeve Biol Med. 2015;36:5607–15.
Abdallah FM, Helmy MW, Katary MA, Ghoneim AI. Synergistic antiproliferative effects of curcumin and celecoxib in hepatocellular carcinoma HepG2 cells. Naunyn Schmiedebergs Arch Pharmacol. 2018;391:1399–410.
Chen J, Liu S, Li Q, Peng J. [Combined application of Cisplatin and Celecoxib inhibits the proliferation and promotes apoptosis of nasopharyngeal carcinoma cells resistant to cisplatin], Xi bao Yu Fen Zi Mian Yi Xue Za Zhi = Chinese. J Cell Mol Immunol. 2015;31:203–6.
Li N, Li H, Su F, Li J, Ma X, Gong P. Relationship between epidermal growth factor receptor (EGFR) mutation and serum cyclooxygenase-2 level, and the synergistic effect of Celecoxib and Gefitinib on EGFR expression in non-small cell Lung cancer cells. Int J Clin Exp Pathol. 2015;8:9010.
Lin JZ, Hameed I, Xu Z, Yu Y, Ren ZY, Zhu JG. Efficacy of gefitinib–celecoxib combination therapy in docetaxel–resistant prostate cancer. Oncol Rep. 2018;40:2242–50.
Riva B, De Dominici M, Gnemmi I, Mariani SA, Minassi A, Minieri V, Salomoni P, Canonico PL, Genazzani AA, Calabretta B, Condorelli F. Celecoxib inhibits proliferation and survival of chronic myelogeous leukemia (CML) cells via AMPK-dependent regulation of β-catenin and mTORC1/2. Oncotarget. 2016;7:81555–70.
Zhao Q, Guo J, Wang G, Chu Y, Hu X. Suppression of immune regulatory cells with combined therapy of Celecoxib and sunitinib in renal cell carcinoma. Oncotarget. 2017;8:1668.
Zhong J, Xiu P, Dong X, Wang F, Wei H, Wang X, Xu Z, Liu F, Li T, Wang Y. Meloxicam combined with sorafenib synergistically inhibits Tumor growth of human hepatocellular carcinoma cells via ER stress-related apoptosis. Oncol Rep. 2015;34:2142–50.
Sung MW, Lee DY, Park SW, Oh SM, Choi JJ, Shin ES, Kwon SK, Ahn SH, Kim YH. Celecoxib enhances the inhibitory effect of 5-FU on human squamous cell carcinoma proliferation by ROS production. Laryngoscope. 2017;127:E117–23.
Araujo-Mino EP, Patt YZ, Murray‐Krezan C, Hanson JA, Bansal P, Liem BJ, Rajput A, Fekrazad MH, Heywood G, Lee FC. Phase II trial using a combination of oxaliplatin, capecitabine, and Celecoxib with concurrent radiation for newly diagnosed resectable rectal cancer. Oncologist. 2018;23:2–e5.
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research at King Khalid University for funding this work through a large group Research Project under grant number RGP2/420/44.
Funding
This study was supported by the deanship of Scientific Research at King Khalid University for funding this work through a large group Research Project under grant number RGP2/420/44.
Author information
Authors and Affiliations
Contributions
PR, HB, YFM, HRAKA-H, ATA: Conceptualization, Writing—original draft preparation. MMD, MMA-T, RSZ, AA: Conceptualization, Writing—review and editing, Visualization. AH: Conceptualization, Supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodrigues, P., Bangali, H., Hammoud, A. et al. COX 2-inhibitors; a thorough and updated survey into combinational therapies in cancers. Med Oncol 41, 41 (2024). https://doi.org/10.1007/s12032-023-02256-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02256-7