Abstract
Background
Preclinical results showing therapeutic effect and low toxicity of metronomic chemotherapy with cyclophosphamide (Cy) + celecoxib (Cel) for mammary tumors encouraged its translation to the clinic for treating advanced breast cancer patients (ABCP).
Patients and methods
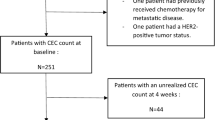
A single-arm, mono-institutional, non-randomized, phase II, two-step clinical trial (approved by Bioethics Committee and Argentine Regulatory Authority) was designed. Patients received Cy (50 mg po.d) + Cel (200 mg p.o.bid). Patient eligibility criteria included: ABCP who progressed to anthracyclines, taxanes and capecitabine, ≤4 chemotherapy schemes, with good performance status. Several pro- and anti-angiogenic molecules and cells were determined as biomarkers. Informed consent was signed by all patients. Primary endpoint was clinical benefit (CB).
Results
Twenty patients were enrolled. Main clinical outcomes were prolonged disease stabilization and partial remission in 10/20 and 1/20 patients, respectively. CB was 55 %, and time to progression (TTP) was 21.1 weeks. Median TTP in patients who achieved CB was 35.6 weeks, and mean overall survival was 44.20 weeks. There were no grade 3/4 toxicities associated with treatment. Circulating endothelial cells (CECs) increased at the time of progression in patients who showed CB (P = 0.014). Baseline CECs and circulating endothelial progenitor cells showed marginal associations with TTP. Serum VEGF decreased (P = 0.050), sVEGFR-2 increased (P = 0.005) and VEGF/sVEGFR-2 ratio decreased during treatment (P = 0.041); baseline VEGF and VEGF/sVEGFR-2 were associated with TTP (P = 0.035 and P = 0.030, respectively), while sVEGFR-2 did not.
Conclusions
Treatment was effective, showing low toxicity profile and excellent tolerability. The combination had anti-angiogenic effect. Increased levels of CEC could be useful for detecting progression. Baseline VEGF and VEGF/sVEGFR-2 values could be useful as early predictors of response.
Trial registration
ANMAT#4596/09.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In advanced breast cancer (ABC), once the first line of treatment has failed, either the response rates or the clinical benefits decrease with the subsequent treatments [1]. Moreover, even after all the advances made in new treatments, the prognosis of this kind of patients continues to be poor [2].
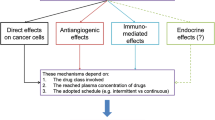
Metronomic chemotherapy (MCT) poses a new paradigm in cancer therapy: “Less is more when administered chronically” [3]. The anti-tumor effect is achieved through an antiangiogenic mechanism demonstrated in preclinical and clinical studies, which showed a decrease in serum vascular endothelial growth factor (VEGF) [4, 5], an increase in serum thrombospondin-1 (TSP-1) [6] and serum soluble VEGF receptor 2 (sVEGFR-2) [7], or the inhibition of both, local and circulating endothelial cells (CECs) and circulating endothelial progenitor cells (CEPs) [8]. Also, other mechanisms of action were described such as restoration of the immune response [9, 10], disruption of cancer stem cells niche [11] or abolishment of host pro-tumorigenic and pro-metastatic effects found on standard chemotherapy [12]. Cyclophosphamide (Cy) is one of the most used drugs in cancer treatment and is one of the earliest cytotoxic drugs used in MCT [13]. Celecoxib (Cel), a selective cyclooxygenase-2 inhibitor, has shown antitumor activity for breast cancer cell lines, not only in vitro but also in vivo [14], and its use has been translated to the clinic [15].
This study evaluates the toxicity, tolerability and clinical effect of MCT with Cy and Cel in ABC patients, who progressed after standard chemotherapy, and the potential role as predictors of response of several pro- and anti-angiogenic molecules and cells.
Patients and methods
Eligibility
Patients were required to have histopathologically confirmed ABC progressing after no more than four lines of chemotherapy. Other inclusion criteria were: acceptable bone marrow, renal and liver function, normal calcemia, at least one lesion according to RECIST criteria and more than 3 months of life expectancy. Also all patients must be recovered from any prior cancer treatment before their inclusion. Signed informed consent was obtained from all patients. The complete inclusion and exclusion criteria are given in supplementary material 1. The protocol was approved by institutional bioethics committee and by A.N.M.A.T. (Argentine Regulatory Agency, #4596/09).
Treatment plan and follow-up
All patients received Cy 50 mg p.o. daily plus Cel 400 mg (200 mg p.o. bid).
Baseline evaluation includes history taking, physical examination, chest X-ray, abdominal and pelvic ultrasound or CT scan and complete biochemical and hematological tests. Patients’ follow-up was performed every 14 days during the first 6 months, and every 28 days thereafter, and consisted of physical examination and hematologic tests. Toxicity and response were evaluated every 2 months or earlier, if it was necessary. Patients were followed until progression or death. All the adverse events (AE) were recorded, assessed according to Common Terminology Criteria for Adverse Events (CTCAE) version 4.03 and followed until their resolution.
Study design and endpoints
For this prospective, mono-institutional, single-arm, non-randomized, phase II clinical trial, sample size calculation was based on an optimal two-stage minimax design [16]. Assuming an alpha error of 0.05 and beta error of 0.20, it was required to recruit a total of 20 patients, 15 in the first stage and five in the second.
The primary endpoint was clinical benefit (CB), which was defined as complete response (CR) + partial response (PR) + prolonged stable disease (pSD) ≥24 weeks. Response was assessed every 2 months by RECIST. Time to progression (TTP) was defined as the time from the beginning of treatment to time of disease progression (PD). Progression-free survival (PFS), response rate (RR) and overall survival (OS) were also calculated.
Biomarker assessments
Samples were collected at baseline, at the first three visits and every 2 months thereafter.
Cellular biomarkers
Quantification of CECs and CEPs by flow cytometry was carried out on peripheral blood collected in tubes with EDTA and separated by Ficoll–Hypaque gradient. Anti-CD45-FITC (BD Pharmingen, USA) was used to exclude hematopoietic cells, and anti-CD31-ALEXA Fluor® 488 (BD Pharmingen) and anti-CD133-PE (Miltenyi Biotec, Germany) were used to determine the percentages of CECs and CEPs, respectively. Samples were evaluated using a Coulter Epics XL flow cytometer.
Serological biomarkers
Serum levels of VEGF, fraction C of VEGF (VEGF-C), sVEGFR-2, sVEGFR-3 and TSP-1 were evaluated by ELISA (Quantikine© ELISA kit, R & D Systems Inc, Minneapolis, MN, USA) according to manufacturer’s instructions. Blood samples were allowed to clot for 2 h. After centrifugation, serum was collected and stored at −20 °C until used.
Statistical analyses
Variations in cellular and serological biomarkers were analyzed with ANOVA for repeated measurements. The association between baseline values of VEGF, sVEGFR-2, sVEGFR-3 and VEGF/TSP-1, VEGF/sVEGFR-2, VEGF-C/sVEGFR-2 and VEGF-C/sVEGFR-3 ratios with TTP was evaluated using Spearman’s correlation coefficients. A multiple regression analysis was used to evaluate the goodness of prediction. To confirm the prediction, the 50th percentile of the baseline value was set as a cutoff value and PFS curves were calculated. Group-specific survival curves were calculated by Kaplan–Meier test. Also, a multivariate logistic regression analysis was carried out to evaluate association of response with hormonal receptor status and baseline ECOG status. All statistical tests were one-sided with significance defined as a P value <0.05. STATA was used for the analysis (StataCorp: Stata Statistical Software: Release 6.0, College Station, TX, USA, 1999), and GraphPad Prism® version 3.0 (GraphPad Software, San Diego, CA, USA) was used for the graphics.
Results
Demographic characteristics
During the period 2008–2013, 20 female patients were included. The median age at diagnosis was 45.5 years (range = 36–72). All patients had advanced disease, three of them since diagnosis, and were heavily pretreated. All patients that were positive for hormone receptors or Her2/neu had previously received hormonal therapy and trastuzumab. Demographic characteristics of patients and tumors are summarized in Table 1.
Adverse events and toxicity
The hematologic AE associated with treatment were mild: anemia G2 (N = 9/20), leukopenia G1 (N = 2/20) and G2 (N = 2/20), neutropenia G1 (N = 1/20) and G2 (N = 2/20) and thrombocytopenia G2 (N = 1/20). Those events were easily overcome with transitory reduction of Cy doses. Minimal gastrointestinal toxicity (dyspepsia) G1 was seen in 4/20 patients, without affecting compliance, and was easily reversed by administration of daily omeprazole 20 mg v.o. There was no evidence of hepatic, renal or cardiac toxicities associated with therapy. All the AE, whether related or not to the therapy, are summarized in Table 2.
Therapeutic response
The main responses were PR and pSD. PR was observed in one patient (RR = 5 %), while no complete responses (CR) were seen. Stable disease was observed in 14/20 patients (70 %) and pSD in 10/20 patients (50 %). Five patients showed progressive disease (PD). The RR was 5 % (CR + PR = 1/20) and the CB 55 % (11/20). The therapeutic response is summarized in Table 3.
Mean TTP was 21.1 weeks (median = 15.5; range = 3–81) and among patients with pSD was 35.6 weeks (median = 27; range = 24–81). PFS at 24 weeks was 30 %. The OS rate, 1 year after enrollment in the trial, was 25 % and the mean OS 44.20 weeks (median = 36; range = 5–153). Significant longer OS (P = 0.0134) was seen in patients with CB (Fig. 1).
Progression-free survival and overall survival. a PFS progression-free survival (N = 20); mean 21.1 weeks (median 15.5, range 3–81). b OS overall survival (N = 20); mean 44.20 weeks (median 36, range 5.14–232.14). c Overall survival stratified by clinical benefit; with CB: median, 45 weeks; without CB: 21 weeks, P = 0.0134 (log-rank, Mantel–Cox)
Cellular biomarkers
The percentages of CECs and CEPs did not show a defined trend during treatment. However, CECs showed a significant increase (P = 0.010) in patients with CB by the time of PD (Supplementary material 2).
Serum biomarkers
Serum concentration of VEGF decreased (P = 0.050) and sVEGFR-2 increased (P = 0.005) during treatment, whereas non-significant variations were detected for VEGF-C, sVEGFR-3 and TSP-1. The VEGF/sVEGFR-2 ratio decreased significantly during treatment (P = 0.041). On the other hand, non-significant variations for VEGF/TSP-1, VEGF-C/sVEGFR-2 and VEGF-C/sVEGFR-3 ratios were observed (Fig. 2).
Variations of serum markers and constructed ratios during treatment. a VEGF (N = 20): P = 0.050; b VEGF-C (N = 15*): P = 0.128; c sVEGFR-2 (N = 20): P = 0.005; d sVEGFR-3 (N = 15*): P = 0.128; e TSP-1 (N = 15*): P = 0.369. f VEGF/sVEGFR-2 (N = 20): P = 0.041; g VEGF/TSP-1 (N = 15*): P = 0.803; h VEGF-C/sVEGFR-2 (N = 15*): P = 0.293. i VEGF-C/sVEGFR-3 (N = 15*): P = 0.177 (ANOVA for repeated measurements). *Patients included in the first stage
Predictors of response and survival analysis
Each marker that showed significant variation during treatment was correlated with TTP. A significant association between baseline VEGF (P = 0.011; Fig. 3a), baseline VEGF/sVEGFR-2 (P = 0.029; Fig. 3c) and TTP was found. That was not the case for sVEGFR-2 (Fig. 3b). Association between baseline CECs and TTP was marginally significant (P = 0.075; Fig. 3d). When considering VEGF and VEGF/sVEGFR-2 in a multiple regression analysis, the goodness of the prediction was not improved (data not shown).
Association between biomarkers baseline values and time to progression and survival analysis. a Baseline VEGF (N = 20): r = −0.5055, P = 0.011; b baseline sVEGFR-2 (N = 20): r = 0.271, P = 0.162; c baseline VEGF/sVEGFR‑2 (N = 20): r = −0.451, P = 0.029; (Spearman’s correlation); d baseline CEC (N = 20): r = 0.364, P = 0.075; e VEGF (N = 20), median survival = 23 and 7 weeks, P = 0.0001; f VEGF/sVEGFR-2 (N = 20), median survival = 26 and 11 weeks, P = 0,014. Kaplan–Meier and log-rank tests. PFS progression-free survival
To confirm baseline VEGF and VEGF/sVEGFR-2 ratio as predictors of response, the 50th percentile of each biomarker was set as a cutoff value to analyze the percentage of PFS. Patients who showed VEGF or VEGF/sVEGFR-2 values equal or lower than the cutoff were those who had longer TTP (P = 0.0001 Fig. 3e; P = 0.014, Fig. 3f).
In the multivariate analysis, the chance of pSD or PR was not associated with hormone receptor, HER-2/neu or baseline performance status ≤2. Finally, when analyzed together the three variables, they were not associated with treatment response.
Discussion
The introduction of MCT in the field of cancer treatment has yielded the valuable outcome of overcoming drug resistance through the activation of several antitumor mechanisms. Moreover, together with the importance of obtaining CB, MCT offers economic benefits related to the reduced costs of low doses of already approved drugs, frequently off patent, and with low toxicity, avoiding the need of additional treatments and hospitalizations [17].
Our preclinical results with mammary tumors, treated metronomically with Cy + Cel or Cy + doxorubicin, showing therapeutic effect and low toxicity [18, 19] suggested its translation to the clinic.
The AE were scarce, mild and, mainly, hematological. They were associated with chronic use of Cy, appeared after several weeks of medication and reverted with dose reduction. These types of AE are also the most frequently observed in MCT schemes using Cy [20, 21]. Dyspepsia was the only non-hematological AE associated with the chronic use of Cel and reversed with symptomatic treatment.
The RR obtained in this study was 5 %, which is low compared with those obtained with schemes combining Cy + methotrexate ± trastuzumab [4, 22]. However, since our patients were metastatic and heavily pretreated, it is not expected to obtain a high RR. Interestingly, CB was close to 60 %, which is similar to those reached with high-dose chemotherapy for metastatic breast cancer [23, 24], but with the advantage of avoiding toxicity. The CB is the most frequent outcome found in MCT schemes [21, 25, 26]. Since disease at this stage is not curable, preserving quality of life remains as one of the main goals.
Mean TTP in this study was 21.1 weeks, and 35.6 weeks for patients who achieved CB. Similar results were found by other authors [4, 22, 27]. Also, the OS was longer in those patients with CB. However, two studies reported longer OS using metronomic capecitabine for advanced disease, both with excellent outcomes [28, 29].
Hematopoietic cells and bone marrow-derived CEPs are required for tumor angiogenesis. Both, CECs and CEPs, were proposed to be direct targets of MCT [8] and have been extensively studied as prognostic and predictive biomarkers in clinical trials using antiangiogenic agents and MCT, but the results have indicated high inconsistency [30, 31]. In our study, variations of CECs and CEPs did not show a clear trend but, interestingly, patients who showed CB evinced an increase in CECs level at the time of PD, suggesting its use as a potential biomarker for follow-up. However, some of the limitations in the use of CECs as biomarkers are their low concentration in blood and the heterogeneity in the methods used to detect them, making their quantification not accurate or comparable. The importance of VEGF and its receptors has been extensively reviewed [32–35]. As expected, MCT with Cy + Cel reduced VEGF and increased sVEGFR-2 levels, demonstrating its antiangiogenic mechanism of action. The decrease in VEGF has also been reported in other MCT studies [4, 5, 36]. However, its usefulness as a predictive biomarker of response has not been proved yet and remains controversial [31].
No significant changes in serum concentrations of VEGF-C and sVEGFR-3 were found during treatment, suggesting that it would not affect lymphangiogenesis.
TSP-1 inhibits proliferation, growth, motility and adhesion of tumor endothelial cells, and its expression may be involved in the regulation of tumor angiogenesis [6]. Our results showed that serum TSP-1 was not related to response or PD. Indeed, other clinical MCT trials evaluated TSP-1 levels without finding a consistent behavior. Hence, it does not seem to be a useful biomarker, at least for MCT treatments [37–40].
The association of baseline VEGF and VEGF/sVEGFR-2 ratio with TTP was significant, and patients with values below both 50th percentiles showed higher TTP, suggesting them as potential candidates for predictor biomarkers of response to MCT. Interestingly, baseline serum VEGF was a better predictor than VEGF/sVEGFR-2 ratio. However, larger studies are needed for establishing their utility. As previously proposed [7], it would be interesting that those groups that have worked, or are presently working, in MCT trials determine baseline VEGF and sVEGFR-2, calculate the ratio and analyze its association with therapeutic response.
In summary, MCT combining Cy + Cel showed low toxicity and CB as main outcome. The decrease of VEGF and the increase of sVEGFR-2 confirmed the anti-angiogenic effect of the scheme. Also, potential predictive biomarkers of response (baseline VEGF and VEGF/sVEGFR-2) and follow-up (CECs) were identified. The need for finding noninvasive biomarkers to predict response to cancer therapies has not yet been fulfilled. Hence, we believe that the results herein described may help to achieve such a goal.
References
Palumbo R, Sottotetti F, Riccardi A, Teragni C, Pozzi E, Quaquarini E, Tagliaferri B, Bernardo A (2013) Which patients with metastatic breast cancer benefit from subsequent lines of treatment? An update for clinicians. Ther Adv Med Oncol 5(6):334–350. doi:10.1177/1758834013508197
Nelson R (2013) Targeted therapies offer promise, but are they affordable? Medscape. http://www.medscape.com/viewarticle/810147#vp_2. Accessed March 13 2015
Hanahan D, Bergers G, Bergsland E (2000) Less is more, regularly: metronomic dosing of cytotoxic drugs can target tumor angiogenesis in mice. J Clin Invest 105(8):1045–1047. doi:10.1172/JCI9872
Colleoni M, Rocca A, Sandri MT, Zorzino L, Masci G, Nole F, Peruzzotti G, Robertson C, Orlando L, Cinieri S, de Braud F, Viale G, Goldhirsch A (2002) Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: antitumor activity and correlation with vascular endothelial growth factor levels. Ann Oncol 13(1):73–80
Perroud HA, Rico MJ, Alasino CM, Queralt F, Mainetti LE, Pezzotto SM, Rozados VR, Scharovsky OG (2013) Safety and therapeutic effect of metronomic chemotherapy with cyclophosphamide and celecoxib in advanced breast cancer patients. Future Oncol 9(3):451–462. doi:10.2217/fon.12.196
Lansiaux A, Salingue S, Dewitte A, Clisant S, Penel N (2012) Circulating thrombospondin 1 level as a surrogate marker in patients receiving cyclophosphamide-based metronomic chemotherapy. Invest New Drugs 30(1):403–404. doi:10.1007/s10637-010-9443-1
Perroud HA, Rico MJ, Alasino CM, Pezzotto SM, Rozados VR, Scharovsky OG (2013) Association between baseline VEGF/sVEGFR-2 and VEGF/TSP-1 ratios and response to metronomic chemotherapy using cyclophosphamide and celecoxib in patients with advanced breast cancer. Indian J Cancer 50(2):115–121. doi:10.4103/0019-509X.117031
Mancuso P, Colleoni M, Calleri A, Orlando L, Maisonneuve P, Pruneri G, Agliano A, Goldhirsch A, Shaked Y, Kerbel RS, Bertolini F (2006) Circulating endothelial-cell kinetics and viability predict survival in breast cancer patients receiving metronomic chemotherapy. Blood 108(2):452–459. doi:10.1182/blood-2005-11-4570
Rozados VR, Mainetti LE, Rico MJ, Zacarias Fluck MF, Matar P, Scharovsky OG (2010) The immune response and the therapeutic effect of metronomic chemotherapy with cyclophosphamide. Oncol Res 18(11–12):601–605
Ghiringhelli F, Menard C, Puig PE, Ladoire S, Roux S, Martin F, Solary E, Le Cesne A, Zitvogel L, Chauffert B (2007) Metronomic cyclophosphamide regimen selectively depletes CD4+ CD25+ regulatory T cells and restores T and NK effector functions in end stage cancer patients. Cancer Immunol Immunother 56(5):641–648. doi:10.1007/s00262-006-0225-8
Martin-Padura I, Marighetti P, Agliano A, Colombo F, Larzabal L, Redrado M, Bleau AM, Prior C, Bertolini F, Calvo A (2012) Residual dormant cancer stem-cell foci are responsible for tumor relapse after antiangiogenic metronomic therapy in hepatocellular carcinoma xenografts. Lab Invest 92(7):952–966. doi:10.1038/labinvest.2012.65
Vives M, Ginesta MM, Gracova K, Graupera M, Casanovas O, Capella G, Serrano T, Laquente B, Vinals F (2013) Metronomic chemotherapy following the maximum tolerated dose is an effective anti-tumour therapy affecting angiogenesis, tumour dissemination and cancer stem cells. Int J Cancer 133(10):2464–2472. doi:10.1002/ijc.28259
Browder T, Butterfield CE, Kraling BM, Shi B, Marshall B, O’Reilly MS, Folkman J (2000) Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 60(7):1878–1886
Dai ZJ, Ma XB, Kang HF, Gao J, Min WL, Guan HT, Diao Y, Lu WF, Wang XJ (2012) Antitumor activity of the selective cyclooxygenase-2 inhibitor, celecoxib, on breast cancer in vitro and in vivo. Cancer Cell Int 12(1):53. doi:10.1186/1475-2867-12-53
Young SD, Lafrenie RM, Clemons MJ (2012) Phase ii trial of a metronomic schedule of docetaxel and capecitabine with concurrent celecoxib in patients with prior anthracycline exposure for metastatic breast cancer. Curr Oncol 19(2):e75–e83. doi:10.3747/co.19.879
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10(1):1–10
Bouche G, Andre N, Banavali S, Berthold F, Berruti A, Bocci G, Brandi G, Cavallaro U, Cinieri S, Colleoni M, Curigliano G, Di Desidero T, Eniu A, Fazio N, Kerbel R, Hutchinson L, Ledzewicz U, Munzone E, Pasquier E, Graciela Scharovsky O, Shaked Y, Sterba J, Villalba M, Bertolini F (2014) Lessons from the fourth metronomic and anti-angiogenic therapy meeting, 24–25 June 2014, Milan. Ecancermedicalscience 8:463. doi:10.3332/ecancer.2014.463
Mainetti LE, Rozados VR, Rossa A, Bonfil RD, Scharovsky OG (2011) Antitumoral and antimetastatic effects of metronomic chemotherapy with cyclophosphamide combined with celecoxib on murine mammary adenocarcinomas. J Cancer Res Clin Oncol 137(1):151–163. doi:10.1007/s00432-010-0869-9
Mainetti LE, Rico MJ, Fernandez-Zenobi MV, Perroud HA, Roggero EA, Rozados VR, Scharovsky OG (2013) Therapeutic efficacy of metronomic chemotherapy with cyclophosphamide and doxorubicin on murine mammary adenocarcinomas. Ann Oncol 24(9):2310–2316. doi:10.1093/annonc/mdt164
Colleoni M, Orlando L, Sanna G, Rocca A, Maisonneuve P, Peruzzotti G, Ghisini R, Sandri MT, Zorzino L, Nole F, Viale G, Goldhirsch A (2006) Metronomic low-dose oral cyclophosphamide and methotrexate plus or minus thalidomide in metastatic breast cancer: antitumor activity and biological effects. Ann Oncol 17(2):232–238. doi:10.1093/annonc/mdj066
Dellapasqua S, Bertolini F, Bagnardi V, Campagnoli E, Scarano E, Torrisi R, Shaked Y, Mancuso P, Goldhirsch A, Rocca A, Pietri E, Colleoni M (2008) Metronomic cyclophosphamide and capecitabine combined with bevacizumab in advanced breast cancer. J Clin Oncol 26(30):4899–4905. doi:10.1200/JCO.2008.17.4789
Orlando L, Cardillo A, Ghisini R, Rocca A, Balduzzi A, Torrisi R, Peruzzotti G, Goldhirsch A, Pietri E, Colleoni M (2006) Trastuzumab in combination with metronomic cyclophosphamide and methotrexate in patients with HER-2 positive metastatic breast cancer. BMC Cancer 6:225. doi:10.1186/1471-2407-6-225
Gampenrieder SP, Bartsch R, Matzneller P, Pluschnig U, Dubsky P, Gnant MX, Zielinski CC, Steger GG (2010) Capecitabine and vinorelbine as an all-oral chemotherapy in HER2-negative locally advanced and metastatic breast cancer. Breast Care (Basel) 5(3):158–162. doi:10.1159/000314214
Rau KM, Li SH, Chen SM, Tang Y, Huang CH, Wu SC, Chen YY (2011) Weekly paclitaxel combining with gemcitabine is an effective and safe treatment for advanced breast cancer patients. Jpn J Clin Oncol 41(4):455–461. doi:10.1093/jjco/hyq232
Bottini A, Generali D, Brizzi MP, Fox SB, Bersiga A, Bonardi S, Allevi G, Aguggini S, Bodini G, Milani M, Dionisio R, Bernardi C, Montruccoli A, Bruzzi P, Harris AL, Dogliotti L, Berruti A (2006) Randomized phase II trial of letrozole and letrozole plus low-dose metronomic oral cyclophosphamide as primary systemic treatment in elderly breast cancer patients. J Clin Oncol 24(22):3623–3628. doi:10.1200/JCO.2005.04.5773
Montagna E, Cancello G, Bagnardi V, Pastrello D, Dellapasqua S, Perri G, Viale G, Veronesi P, Luini A, Intra M, Calleri A, Rampinelli C, Goldhirsch A, Bertolini F, Colleoni M (2012) Metronomic chemotherapy combined with bevacizumab and erlotinib in patients with metastatic HER2-negative breast cancer: clinical and biological activity. Clin Breast Cancer 12(3):207–214. doi:10.1016/j.clbc.2012.03.008
Gebbia V, Boussen H, Valerio MR (2012) Oral metronomic cyclophosphamide with and without methotrexate as palliative treatment for patients with metastatic breast carcinoma. Anticancer Res 32(2):529–536
Taguchi T, Nakayama T, Masuda N, Yoshidome K, Akagi K, Nishida Y, Yoshikawa Y, Ogino N, Abe C, Sakamoto J, Noguchi S (2010) Study of low-dose capecitabine monotherapy for metastatic breast cancer. Chemotherapy 56(2):166–170. doi:10.1159/000313531
Fedele P, Marino A, Orlando L, Schiavone P, Nacci A, Sponziello F, Rizzo P, Calvani N, Mazzoni E, Cinefra M, Cinieri S (2012) Efficacy and safety of low-dose metronomic chemotherapy with capecitabine in heavily pretreated patients with metastatic breast cancer. Eur J Cancer 48(1):24–29. doi:10.1016/j.ejca.2011.06.040
Kraan J, Sleijfer S, Foekens JA, Gratama JW (2012) Clinical value of circulating endothelial cell detection in oncology. Drug Discov Today 17(13–14):710–717. doi:10.1016/j.drudis.2012.01.011
Cramarossa G, Lee EK, Sivanathan L, Georgsdottir S, Lien K, Santos KD, Chan K, Emmenegger U (2014) A systematic literature analysis of correlative studies in low-dose metronomic chemotherapy trials. Biomark Med 8(6):893–911. doi:10.2217/bmm.14.14
Ferrara N, Hillan KJ, Gerber HP, Novotny W (2004) Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov 3(5):391–400. doi:10.1038/nrd1381
Kerbel RS, Kamen BA (2004) The anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer 4(6):423–436. doi:10.1038/nrc1369
Guo S, Colbert LS, Fuller M, Zhang Y, Gonzalez-Perez RR (2010) Vascular endothelial growth factor receptor-2 in breast cancer. Biochim Biophys Acta 1806(1):108–121. doi:10.1016/j.bbcan.2010.04.004
Ebos JM, Lee CR, Bogdanovic E, Alami J, Van Slyke P, Francia G, Xu P, Mutsaers AJ, Dumont DJ, Kerbel RS (2008) Vascular endothelial growth factor-mediated decrease in plasma soluble vascular endothelial growth factor receptor-2 levels as a surrogate biomarker for tumor growth. Cancer Res 68(2):521–529. doi:10.1158/0008-5472.CAN-07-3217
El-Arab LR, Swellam M, El Mahdy MM (2012) Metronomic chemotherapy in metastatic breast cancer: impact on VEGF. J Egypt Natl Cancer Inst 24(1):15–22. doi:10.1016/j.jnci.2011.12.002
Allegrini G, Di Desidero T, Barletta MT, Fioravanti A, Orlandi P, Canu B, Chericoni S, Loupakis F, Di Paolo A, Masi G, Fontana A, Lucchesi S, Arrighi G, Giusiani M, Ciarlo A, Brandi G, Danesi R, Kerbel RS, Falcone A, Bocci G (2012) Clinical, pharmacokinetic and pharmacodynamic evaluations of metronomic UFT and cyclophosphamide plus celecoxib in patients with advanced refractory gastrointestinal cancers. Angiogenesis 15(2):275–286. doi:10.1007/s10456-012-9260-6
Bhatt RS, Merchan J, Parker R, Wu HK, Zhang L, Seery V, Heymach JV, Atkins MB, McDermott D, Sukhatme VP (2010) A phase 2 pilot trial of low-dose, continuous infusion, or “metronomic” paclitaxel and oral celecoxib in patients with metastatic melanoma. Cancer 116(7):1751–1756. doi:10.1002/cncr.24902
Fontana A, Galli L, Fioravanti A, Orlandi P, Galli C, Landi L, Bursi S, Allegrini G, Fontana E, Di Marsico R, Antonuzzo A, D’Arcangelo M, Danesi R, Del Tacca M, Falcone A, Bocci G (2009) Clinical and pharmacodynamic evaluation of metronomic cyclophosphamide, celecoxib, and dexamethasone in advanced hormone-refractory prostate cancer. Clin Cancer Res 15(15):4954–4962. doi:10.1158/1078-0432.CCR-08-3317
Khan OA, Blann AD, Payne MJ, Middleton MR, Protheroe AS, Talbot DC, Taylor M, Kirichek O, Han C, Patil M, Harris AL (2011) Continuous low-dose cyclophosphamide and methotrexate combined with celecoxib for patients with advanced cancer. Br J Cancer 104(12):1822–1827. doi:10.1038/bjc.2011.154
Acknowledgments
We would like to thank NCI “National Cancer Institute of Argentina” and the National Scientific and Technical Research Council (CONICET) for their support in this study, as well as Cibic S.A. and especially to Dr. Ricardo Giordano, for their help in flow cytometry studies.
Funding
This work was supported by Agencia Nacional de Promoción Científica y Tecnológica (ANPCyT) [Grant Number: PICT 2006/1908 to OGS, VRR, SMP and CMA]. The National Cancer Institute at the National Institutes of Health grants for doctoral fellows to HAP. HAP is a fellow of Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest.
Ethical standard
The authors declare that the protocol herein described complies with the current laws of Argentina. The protocol was authorized by the School of Medicine Bioethics Committee and by A.N.M.A.T. (Argentine Regulatory Agency).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Perroud, H.A., Alasino, C.M., Rico, M.J. et al. Metastatic breast cancer patients treated with low-dose metronomic chemotherapy with cyclophosphamide and celecoxib: clinical outcomes and biomarkers of response. Cancer Chemother Pharmacol 77, 365–374 (2016). https://doi.org/10.1007/s00280-015-2947-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2947-9