Abstract
The aim of the study is to present the diagnostic feasibility, usefulness, and safety of a novel technique for coaxial CT-guided fine-needle aspiration biopsy of small (≤20 mm in diameter) lung nodules. A 18-gauge (G) (1.2 × 40 mm) needle is inserted through the skin in the depth of the thoracic wall tissues remaining outside the pleura. Its positioning is planned and adjusted using multiplanar reconstruction (MPR) images along the 18-G guide needle axis tracing a reference outline extended from the needle tip to the target nodule. When the insertion of the 18-G extra-pleuric needle (EPN) proves to be precise, a 22-G Chiba needle is then passed through the outer 18-G EPN until it reaches the thoracic lesion for the sampling procedure. Patient population included 153 males and 94 females, with a mean age of 61.3 ± 21.6 years. Mean nodule diameter was 14.1 ± 2.2 mm. The lesion depth from pleural plane ranged from 0 mm to 127 mm. An average of 1.29 aspirates were performed per lesion. The most common complication was pneumothorax in 27 cases; there were no cases of PNX requiring chest tube insertion. Intrapulmonary bleeding along the needle track was observed in 32 patients. Exploiting the advantage of MPR images, our novel technique of extra-pleuric coaxial system with a 18-G EPN allows the operator to multiple samplings of small (≤20 mm) target lesions in various locations with a thinner (22-G Chiba) needle, thus reducing the degree of pleural, parenchymal, or adjacent organs damage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pathological verification of pulmonary nodules suspicious for malignancy is a necessary requirement to plan the most adequate treatment [1–4]. The diagnostic options available include computed tomography (CT)-guided biopsy, bronchoscopy with transbronchial biopsy, or diagnostic surgical removal of the lesion [5, 6].
CT-guided fine-needle aspiration biopsy (FNAB) with percutaneous transthoracic access has become a well-established procedure for characterization of pulmonary lesions thanks to its recognized minimal invasiveness, great safety, effectiveness, and tolerability [1, 2, 7–9]. Multidetector CT (MDCT) provides good-quality multiplanar reconstructions (MPR) images revealed to be a very useful tool for guiding percutaneous lung FNAB procedures [7, 10]. Although peripheral lesions are particularly suitable for CT-guided biopsy, central lesions can also be diagnosed, and this option represent an essential diagnostic tool when transbronchial biopsies are not feasible or have failed [1, 5]. For both the single-needle and coaxial system technique, the biopsy needle is advanced in one motion through the pleura to the prescribed depth [6]. It is reported that multiple punctures of the pleura and larger puncture needles are associated with a higher risk of pneumothorax (PNX) [5]. To reduce the complication rate, the coaxial technique can be employed obtaining multiple biopsies by means of a single puncture of the visceral pleura [5]. The precise insertion of the coaxial needle into the target lesion represents a crucial step for avoiding complications during CT-guided FNAB [2]. However, the correct insertion of the coaxial needle may require many attempts also for skillful operator, especially when the nodule is central or small (≤20 mm), increasing the risk of PNX or injuries to adjacent organs [2].
In this novel coaxial technique, a 18-gauge (G) (1.2 × 40 mm) needle is inserted through the skin in the depth of the thoracic wall tissues, and its positioning is planned and adjusted remaining outside the pleura using MPR images. MPR images traced along the guide needle axis are employed to trace a reference outline from the tip of the extra-pleuric needle (EPN) to the target nodule. When the insertion of the 18-G EPN proves to be precise, a 22-G Chiba needle is then passed through the outer 18-G EPN until it reaches the thoracic lesion for the sampling procedure. The aim of this study is to present the diagnostic feasibility, usefulness and safety of this novel technique for coaxial CT-guided FNAB of small (≤20 mm in diameter) lung nodules.
Materials and methods
Study population
Imaging records of all patients who had undergone CT-guided lung biopsies at our institution from January 2007 and December 2015 were retrospectively reviewed. At our institution, retrospective review of the patients’ radiologic images and clinical records does not require institutional review board approval. Patients were referred for diagnosis of primary, metastatic, and inflammatory lung lesions. All examinations were strictly performed for clinical indications only if approved by a fellowship-trained interventional radiologist to ensure feasibility and patient safety. Among all 1283 procedures, small (≤20 mm) nodules were retrospectively identified in 273 (21.3%) cases. Our novel technique was employed in 247/273 (89%) patients (153 males and 94 females; mean age 61.3 ± 21.6 years) with small (≤20 mm) nodules. The diameters of all nodules were measured along the maximum long-axis diameter using lung window settings. All patients had undergone diagnostic chest CT, either in our hospital or at another institution, before the biopsy.
Procedure
Pre-procedural preparation
Prior to the procedure, previously performed diagnostic CT scans were reviewed to provisionally decide the patient position (supine, prone, or lateral) and the most appropriate route on the basis of the location of the target lesion in relation to the pleural fissures, large bronchi, vascular structures, and bones and distance from the chest wall. Any anticoagulation or antiaggregant therapy was promptly discontinued when possible. The patients were instructed to take a reproducible breath and to abstain from talking, moving, coughing, or breathing deeply during the procedure. An intravenous 20-G cannula was inserted to have a venous access ready in the event of complications.
MDCT
All procedures were performed under MDCT guidance after obtaining the patient’s informed consent. After proper positioning of the patient, a spiral 6-row CT (Somatom Emotion 6, Siemens, Erlangen, Germany) was performed in the region of interest. Technical parameters were 120 mAs, 90 kV, 10.26 mGv, 6 × 2-mm collimation, 2.5-mm slice thickness, and 1-mm reconstruction increment. Image post-processing was performed on a Leonardo workstation (Siemens).
Biopsy
The biopsy procedure was standardized. Preliminary unenhanced MDCT images were obtained through the thoracic lesion when the patients held their breath at the end of a normal inhalation. A metallic centimeter grid was placed on the body surface corresponding to the target lesion to identify the skin landmark around which to prepare the sterile field (Fig. 1a). Three-dimensional CT images were reconstructed using 1-mm-thick MPR in axial, coronal, and sagittal planes, as appropriate. The most appropriate skin entry site and route were determined. The biopsy route was planned so that the needle trajectory would reach highly attenuating areas of non-calcified tissue within the nodule avoiding emphysematous lung, traversing large vessels, main and lobar bronchi, pleural fissures, or bony structures. The puncture angle and the distance from the skin entry site and pleura were measured in order to verify the feasibility of the EPN positioning. The distance of pleural plane from the skin surface should not be <4 cm along the bioptic route.
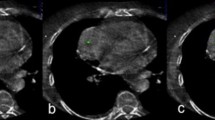
CT images of a 67-year-old male smoker with cytological diagnosis of non-small-cell lung cancer. a The CT axial section shows a 18-mm solid non-calcified pulmonary nodule (arrow) close to the pericardium. See the metallic grid used to mark the skin entry region. b MPR oblique sagittal image along the needle axis shows the 18-G extra-pleuric needle; an outline (dotted line) traced from the tip of the needle toward the target lesion and parallel to needle axis, indicates the correct needle path toward the nodule. c MPR oblique axial image shows the tip (arrowhead) of the 22-G Chiba needle inserted in the target lesion through the extra-pleuric guide. d Post-procedural CT axial image reveals no pneumothrax and the presence of low-grade parenchymal bleeding along the needle track; notice the extra-pleuric needle remained fixed
The patient was advanced into the gantry again and stopped at the skin entry site. The selected skin entry site was marked using a skin marker and the integrated laser beam. The skin entry site was then prepared and draped in a sterile manner. A local anesthetic (lidocaine 1%) was injected through the skin entry site into the level of the parietal pleura. The anesthetic needle was kept in an extra-pleuric position, and then a CT scan was performed to verify if the position of the skin entry site was correct. In between breaths held by the patient at the end of a normal inhalation phase, the 18-G EPN was gradually advanced toward the predefined sampling position without penetrating the pleura. The needle position was checked several times during the procedure by using intermittent CT guidance. MPR images along the needle axis were employed to evaluate the needle path and its inclination in the three spatial planes. On these MPR images, an outline was extended along the EPN axis from EPN tip to the predefined sampling position of the target nodule (Fig. 1b) to verify the alignment of the EPN direction with the most appropriate route and to assess the projective overlapping of the predefined sampling position with the distal extremity of the extended MPR outlines. If the position of the EPN tip was confirmed to be incorrect even after manipulation, the EPN was withdrawn from the thoracic wall and then inserted again without penetrating the pleura toward the same predefined sampling position. If the nodule was on the MPR extended line of the needle path, the biopsy procedure was continued introducing a 22-G Chiba needle with centimeter markings and appropriate length passing inside EPN and penetrating the pleura to reach the nodule for the sampling (Fig. 1c). If control CT images confirmed the position of the 22-G needle tip into the target lesion (Fig. 2a, b), then the Chiba needle was connected to a 20-mL syringe for aspiration, and suction was applied while rotating and moving the needle to and from within the lesion. The plunger was then released and the needle withdrawn, while the EPN remained fixed (Fig. 1d) for any eventual further sampling.
CT images of a 52-year-old female smoker (prone position) with cytological diagnosis of adenocarcinoma. a CT axial image shows the tip (arrowhead) of the 22-G Chiba needle inserted in the target lesion. b MPR oblique axial image shows the 22-G Chiba needle inserted in the target lesion through the extra-pleuric guide
The cytological sample adequacy was assessed immediately by the onsite cytopathologist after being smeared on a glass slide, immersed in 95% alcohol and stained with Giemsa. The bioptic sampling through the same EPN guide was repeated whenever real-time cytology proved non-diagnostic.
Post-biopsy evaluation
After obtaining adequate sampling, the EPN was removed and unenhanced MDCT scan was performed on the whole thorax to check for immediate PNX and hemorrhage. Patients were observed in a monitored recovery unit for a minimum of 4 h after the procedure, and upright chest radiography was performed prior to discharge.
The degree of PNX detected by CT was graded as mild when lung surface retraction was <2 cm, moderate when lung surface retraction measured between 2 and 4 cm, and severe when lung surface retraction was more than 4 cm from the chest wall [8]. If a small, asymptomatic, immediate PNX developed, the patient was conservatively treated by the administration of supplemental oxygen and serial inspiratory chest radiographs were obtained to monitor the PNX.
Symptomatic PNXs were treated with manual immediate aspiration, while patients with rapidly expanding PNX or decreased oxygen saturation received chest tube insertions and were managed as inpatients. Inpatients were then followed up regularly to ensure resolution of the PNX and improvement in patient symptoms. The discharged patients were instructed to return to the nearest emergency department if symptoms, including substantial pain and shortness of breath, developed following dismissal.
Bleeding complications were graded as mild (intrapulmonary bleeding along the needle track or around the target lesion presenting as air spaces haziness) moderate (<5 episodes of hemoptysis, estimated at <30 ml blood or minimal hemothorax), and severe (hemoptysis or hemothorax associated with hemodynamic instability) [8, 11]. For patients with severe hemoptysis, lung hemorrhage, and hemothorax, hemostasis was provided.
Statistical analysis
Data were analyzed with SPSS software version 22.0 (SPSS Inc., Chicago, IL) and are presented as the mean and standard deviation (SD) for continuous variables and as frequency and percentage for categorical variables. A P value <0.05 was considered significant. Chi-squared tests and t tests were performed to compare the presence of PNX according to categorical and continuous variables, respectively.
Results
From January 2007 through December 2015, 247 patients underwent CT-guided FNAB of small (≤20 mm) lung nodules with extra-pleuric coaxial system.
The characteristics of 247 patients, lung lesions and biopsy procedures are reported in Table 1. Of 247 nodules, 49 were covered by ribs (Figs. 3, 5) by pleural fissures; in these cases, MPR images proved essential for needle guidance.
CT images of a 65-year-old male smoker (prone position) with cytological diagnosis of adenocarcinoma. a CT axial image shows a solid pulmonary nodule (20 mm) of the left upper lobe totally covered by a rib (see Fig. 4); the tip (arrowhead) of the 22-G Chiba needle is within the nodule. b MPR oblique sagittal image shows the 18-G extra-pleuric needle and the outlines traced (dotted line) from the tip to the nodule in order to verify the precision of the needle path. c MPR oblique sagital image shows the tip of the 22-G Chiba needle inserted in the target lesion through the extra-pleuric guide
The overall diagnostic yield of extra-pleuric coaxial technique was 89.9% among all confirmed cases (Fig. 6). The sensitivity, specificity, and negative and positive predicted values for malignancy were 88.7, 97.1, 59.6, and 99.4%, respectively.
Complications were observed in 71 of the 247 (28.7%) patients. Overall, the most common complication observed in 27 cases was mild (21/27) and moderate (6/27) PNX—23/27 pneumothoraces (85.1%) resolved spontaneously, 4/27 (14.8%) by immediate aspiration. There were no cases of PNX requiring chest tube insertion. Intrapulmonary bleeding along the needle track was observed in 32 (12.9%) patients, pulmonary hemorrhage around the target lesion was found in 9 (3.6%) cases, while hemoptysis (<5 episodes) presented in 3 (1.2%) patients without clinical significance.
In univariate analysis, the lesion–pleural distance (P = 0.031) was a significant factor related to the risk of PNX. No significance was found in the rate of PNX in relation to patient sex, age, lesion size, lesion location, patient position, number of pleural passes, and emphysema on CT.
Discussion
The traditional general procedure of coaxial CT-guided FNAB is as follows: with CT guidance, a coaxial needle (consisting of an outer cannula and an introducer stylet used for positioning the outer cannula) is inserted through the skin until it reaches the thoracic lesion. The introducer stylet is then removed while keeping the outer cannula in position. A biopsy needle is then passed through the outer cannula for the sampling procedure [2, 12]. Our extra-pleuric coaxial technique introduces a modification of the traditional coaxial one since a large entry (18-G) needle remains in extra-pleuric position while it is used as guidance cannula to pass through the subcutaneous tissues to target the lesion. According to our experience, this variation represents a safe and accurate technique for performing CT-guided FNAB of small (≤20 mm) lung nodules.
Using MPR images oriented along the EPN axis, an outline is traced extending from the tip of the EPN (placed within the thoracic wall soft tissue) toward the target nodule. The MPR line is used to verify the alignment of the EPN direction with the most appropriate route and to check whether the distal extremity of the extended MPR outline projectively matches the predefined sampling position. Moreover, MPR images are employed to determine the best needle path for lesions difficult to reach on the basis of the native axial images alone because of overlying bony structures (ribs, sternum, and scapulae) (Fig. 4) or critical location (pulmonary hilum, proximity to the heart or large mediastinal vessels) or simply for the small size (≤20 mm) [13]. MPR needle guidance makes it possible to avoid crossing pleural fissures during the procedure and to select a plane parallel to the needle path without crossing bullous emphysema or pleural fissures in order to reduce the rate of PNX. Furthermore, MPR images allow a precise depiction of the needle tip inside the lesion and a clear visualization of necrotic areas to be avoided in order to reduce the risk of false-negative results [7]. The wrong placement of the needle tip not appreciated in the native axial images is reported to be the most common negative predictive factor of CT-guided FNAB [14].
Serial CT axial images of the same case described in Fig. 3; the needle penetrates the chest wall at C7 level in oblique caudal direction toward the nodule below the rib
In the depth of soft tissue, craniocaudal, and/or mediolateral inclination of the extra-pleuric (18-G) guide can be easily and safely adjusted more times with painless manipulations, and even if the needle is withdrawn from the thoracic wall and then inserted again there is no risk of pleural injury. This is not possible with traditional coaxial technique procedure in which repeated attempts to angle the introducer needle toward the lesion often follow the previous trajectory and cause pleural/parenchymal damage [6]. Clearly, our novel coaxial technique is not feasible when subcutaneous tissue of any possible appropriate entry sites is not enough thick to include the entire length (40 mm) of the EPN (18-G) along its planned orientation avoiding pleural puncture. In our study, 9.5% of patients with small (≤20 mm) nodules were not suitable for extra-pleuric coaxial technique. These nodules were mainly (76.9%) located in anterior segments of upper lobes, where soft tissue are generally less represented. However, lesion location in the upper lobes has been described as predictive of traditional coaxial FNAB success, likely due to minimal respiratory lung motion and ease of access relative to other lobes. Superior lesions frequently have pleural bases and exhibit close-fitting surfaces or chest wall infiltration; thus, the biopsy needle can be introduced without transposing the pleural space [15]. Instead, it has been reported that injurious effect to the lung tissues and pleura due to traditional coaxial technique are more frequent for basal lesions because of the effect of the diaphragmatic movement than the upper lung zone [16].
PNX remains the most common complication of CT-guided FNAB despite advanced techniques, occurring in the range of 8–64% of cases (with chest tube insertion rate ranging from 2 to 31%) [6, 11, 17]. In addiction to lesions size ≤20 mm, for both coaxial and non-coaxial techniques, emphysema, basal lung localization, increased distance of lung parenchyma transgressed by biopsy needle, traversing many pulmonary surfaces in the needle path, the frequency of needle passes, the guide needle G, the degree of needle angle, patient’s age, and operator experience are reported as potential significant risk factors responsible for the occurrence of PNX [8, 11, 14, 16–18]. The use of traditional coaxial technique decreases the number of passes through the pleura in an effort to reduce the frequency of PNX [17]. As for traditional coaxial system, in this new technique the EPN provides a temporary guide to the lesion allowing the repetition of multiple sampling whenever real-time cytology proves non-diagnostic, but despite the traditional procedure which reduces the number of pleural punctures, each biopsy specimens to be obtained with our technique requires pleural re-penetration because the guide needle does not penetrate the lung parenchyma [15, 16]. Although it is reassuring that the coaxial technique makes a single pleural pass possible, some studies agreeing with our results have failed to show a relationship between the number of pleural passes and the rate of PNX with this system [17, 19]. Our observed low PNX rate, despite a mean of 1.29 (range 1–4) pleural passage numbers, is in agreement with the statistically insignificant difference in incidence between traditional coaxial and non-coaxial techniques [16, 20]. It has been reported that a moderately longer duration of the coaxial needle in the lung parenchyma in the case of multiple biopsies with onsite pathologic interpretation does not appear to result in a significant increase in the risk of PNX [5]. However, with longer dwell times of the traditional coaxial technique, needle motion during patient respiration could influence PNX rate by widening the pleural puncture site and damaging the lung parenchyma [21].
The risk of PNX is also influenced by other technically modifiable factors such as the guide needle G and the needle angle degree [16]. During the past two decades, there has been a trend toward the use of smaller guide needles (19-G or smaller) to reduce PNX rate and chest tube insertion [17, 19]. The bottom line is that the use of smaller needle sizes which penetrate pleura and lung parenchyma lowers the risk of PNX [5]. Unlike other unavoidable technical risks such as lesion size and depth, the choice of guide needle G is within operator control. In the current study, the null chest tube insertion rate (0%) may be explained by the small G of the needle which penetrated the lung parenchyma (22-G) thanks to the extra-pleuric position of the guide used for repositioning. Our results support the hypothesis that lower needle guide G may determine the reduction of PNX and chest tube insertion rates also for small nodules.
The precise placement of the coaxial needle is a prerequisite for minimizing injuries and complications and its precision increases as the experience of the operator increases [2]. However, experience may help to lower the incidence of PNX during a CT-guided coaxial FNAB until a critical lung lesion size (≤20 mm) is reached [22]. Indeed, during FNAB procedures of small (≤20 mm) lesions, a correct needle–pleura angulation is technically more difficult, resulting in a higher number of needle path modifications and longer procedure times [8]. In particular if in a deeper location, smaller lesions also theoretically require more redirection, causing torque at the pleural surface and expanding the pleural puncture [19]. Our novel technique enables the operator with more or less experience to multiple painless extra-pleuric manipulations in order to correct the bioptic route in a safe way.
As in other studies, our PNX risk correlated significantly with the increasing length of the intrapulmonary puncture track. A longer needle path tends to damage a larger part of the lung parenchyma between the pleura and the target nodule, and it may cause an increase in the amount of air leakage, which in turn may affect the chest tube rate [19]. Increasing target nodule depth is also described to correlate with increased risk of bleeding, due to the greater number of needle crossings of pulmonary vessels in a longer lung parenchyma needle tract [8]. Our overall bleeding rate (12.9%) did not differ from the incidence of pulmonary hemorrhage reported in the literature varying from 3.4 to 43% [8]. Most (91.1%) of intrapulmonary hemorrhages were considered as mild, asymptomatic alveolar bleeding (9/41) or needle tract bleeding (32/41) and none of the patients presented hemothorax or hemodynamic instability. However, parenchymal bleeding seems to results in an advantage protecting against PNX [11]. According to this hypothesis, in the present study PNX was not observed in association to intrapulmonary bleeding along the Chiba needle track (Fig. 5) [11]. Even if small lesions are reported to be associated with decreased diagnostic accuracy of CT-guided FNAB, however, in our study, safety was not at the expense of accuracy; our result (89.9%) was slightly higher than the upper limit of the reported range (64.6–88%) for lesions ≤20 mm [6, 8] (Fig. 6).
CT images of 49-year-old male smoker with cytological diagnosis of non-small cell lung cancer. a CT axial image shows a solid pulmonary nodule (14 mm) and the 18-G extra-pleuric needle (EPN) inserted in the chest wall tissue. b First sampling; MPR oblique axial section to check the needle progress depicts the 22-G Chiba needle—inserted through the EPN—correctly directed toward the lesion, with the tip (arrow) 5 mm away from the nodule. The Chiba needle was then advanced for the sampling (not shown). c Post-procedural MPR oblique axial CT scan image shows the bleeding along the needle path (arrowheads) up to the nodule without pneumothorax. d Second sampling; MPR oblique axial image depicts the 22-G Chiba needle inserted into another area of the nodule (arrow) through the EPN guide
This study had several limitations because of its retrospective design which impeded the evaluation of any relations between the operator experience and the safety of this new technique, because all procedures were performed by a single operator. The study did not consider other factors that have previously been reported to influence the PNX and chest tube insertion rates such as the proximity to bronchovascular tree or diaphragm, prior chest surgery or the angle of needle entry.
Results of CT-guided FNAB procedures of 247 small nodules. The diagnoses of 239 biopsies were confirmed and included in the analysis. Among malignant cytology, definitive diagnosis confirmed malignancy in 181/182 cases with 1 false-positive case; among benign cytology, definite diagnosis confirmed benignity in 34/65 cases, revealed benignity in 23/65 cases, while 8 cases were not confirmed
Conclusions
For pathological characterization of lesions with difficult approaches, including small (≤20 mm), deep nodules and lesions near large vessels, MDCT-guided percutaneous FNAB represents a safe and useful diagnostic tool, more widely used than cutting-needle biopsy [6, 15]. PNX and missed pathological diagnosis are the main complications of the procedure, and in the attempt to overcome these limitations, we introduced a variant of the traditional coaxial technique. Exploiting the advantage of MPR images, our novel extra-pleuric coaxial technique allows the operator to multiple sampling of target small (≤20 mm) lesions in various locations with a thinner (22-G Chiba) needle thus reducing the degree of pleural, parenchymal or adjacent organs damage.
Abbreviations
- CT:
-
Computed tomography
- EPN:
-
Extra-pleuric needle
- FNAB:
-
Fine-needle aspiration biopsy
- G:
-
Gauge
- MDCT:
-
Multidetector CT
- MPR:
-
Multiplanar reconstruction
- PNX:
-
Pneumothorax
References
Otto S, Mensel B, Friedrich N, Schäfer S, Mahlke C, von Bernstorff W, et al. Predictors of technical success and rate of complications of image-guided percutaneous transthoracic lung needle biopsy of pulmonary tumors. PLoS ONE. 2015;10:e0124947.
Rui H, Nan-Chuan J, Hao-Hao L, Yu-Hui W, Li H, He-Shui S, et al. Precision of coaxial needle placement in computed tomography-guided transthoracic needle biopsy. Exp Ther Med. 2013;6:1307–11.
Ierardi AM, Mangini M, Fontana F, Floridi C, De Marchi G, Petrillo M, et al. Usefulness and safety of biliary percutaneous transluminal forceps biopsy (PTFB): our experience. Minim Invasive Ther Allied Technol. 2014;23:96–101.
Sa YJ, Kim JJ, Du Kim Y, Sim SB, Moon SW. A new protocol for concomitant needle aspiration biopsy and localization of solitary pulmonary nodules. J Cardiothorac Surg. 2015;10:104.
Schulze R, Seebacher G, Enderes B, Kugler G, Fischer JR, Graeter TP. Complications in CT-guided, semi-automatic coaxial core biopsy of potentially malignant pulmonary lesions. RöFo Fortschr auf dem Geb der Röntgenstr und der Nukl. 2015;187:697–702.
Yaffe D, Koslow M, Haskiya H, Shitrit D. A novel technique for CT-guided transthoracic biopsy of lung lesions: improved biopsy accuracy and safety. Eur Radiol. 2015;25(11):3354–60.
De Filippo M, Onniboni M, Rusca M, Carbognani P, Ferrari L, Guazzi A, et al. Advantages of multidetector-row CT with multiplanar reformation in guiding percutaneous lung biopsies. Radiol Med. 2008;113:945–53.
Li Y, Du Y, Yang HF, Yu JH, Xu XX. CT-guided percutaneous core needle biopsy for small (≤20 mm) pulmonary lesions. Clin Radiol. 2013;68:e43–8.
Rotolo N, Floridi C, Imperatori A, Fontana F, Ierardi AM, Mangini M, et al. Comparison of cone-beam CT-guided and CT fluoroscopy-guided transthoracic needle biopsy of lung nodules. Eur Radiol. 2016;26:381–9.
De Filippo M, Saba L, Rossi E, Nizzoli R, Tiseo M, Pedrazzi G, et al. Curved needles in CT-guided fine needle biopsies of abdominal and retroperitoneal small lesions. Cardiovasc Intervent Radiol. 2015;38:1611–6.
De FilippoM, Saba L, Silva M, Zagaria R, Concari G, Nizzoli R, et al. CT-guided biopsy of pulmonary nodules: is pulmonary hemorrhage a complication or an advantage? Diagn Interv Radiol. 2014;20:421–5.
De Filippo M, Saba L, Azzali E, Milanese G, Mostardi M, Borgia D, et al. CT-guided fine-needle aspiration of abdominal and retroperitoneal small lesions with the coaxial technique using MPR images. Acta Biomed. 2016;87(Suppl 3):57–62.
Reginelli A, Rossi C, Capasso R, Urraro F, Cagini L, Di Crescenzo V, et al. Evaluation with multislice CT of the hilar pulmonary nodules for probable infiltration of vascular-bronchial structures. Recenti Prog Med. 2013;104:403–5.
De Filippo M, Saba L, Concari G, Nizzoli R, Ferrari L, Tiseo M, et al. Predictive factors of diagnostic accuracy of CT-guided transthoracic fine-needle aspiration for solid noncalcified, subsolid and mixed pulmonary nodules. Radiol Med. 2013;118:1071–81.
Guimaraes M, Marchiori E, Hochhegger B, Chojniak R, Gross J. CT-guided biopsy of lung lesions: defining the best needle option for a specific diagnosis. Clinics. 2014;69:335–40.
Nour-Eldin N-EA, Alsubhi M, Emam A, Lehnert T, Beeres M, Jacobi V, et al. Pneumothorax complicating coaxial and non-coaxial CT-guided lung biopsy: comparative analysis of determining risk factors and management of pneumothorax in a retrospective review of 650 patients. Cardiovasc Intervent Radiol. 2016;39(2):261–70.
Geraghty PR, Kee ST, McFarlane G, Razavi MK, Sze DY, Dake MD. CT-guided transthoracic needle aspiration biopsy of pulmonary nodules: needle size and pneumothorax rate. Radiology. 2003;229:475–81.
Carrafiello G, Mangini M, Fontana F, Di Massa A, Ierardi AM, Cotta E, et al. Complications of microwave and radiofrequency lung ablation: personal experience and review of the literature. Radiol Med. 2012;117(2):201–13.
Kuban JD, Tam AL, Huang SY, Ensor JE, Philip AS, Chen GJ, et al. The effect of needle gauge on the risk of pneumothorax and chest tube placement after percutaneous computed tomographic (CT)-guided lung biopsy. Cardiovasc Intervent Radiol. 2015;38:1595–602.
Priola AM, Priola SM, Cataldi A, Di Franco M, Pazè F, Marci V, et al. Diagnostic accuracy and complication rate of CT-guided fine needle aspiration biopsy of lung lesions: a study based on the experience of the cytopathologist. Acta Radiol. 2010;51:527–33.
Ko JP, Shepard JO, Drucker EA, Aquino SL, Sharma A, Sabloff B, et al. Factors influencing pneumothorax rate at lung biopsy: are dwell time and angle of pleural puncture contributing factors? Radiology. 2001;218:491–6.
Yeow KM, Su IH, Pan KT, Tsay PK, Lui KW, Cheung YC, et al. Risk factors of pneumothorax and bleeding: Multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126:748–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Patient consent
Informed consent was obtained from all patients before diagnostic examination.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Rights and permissions
About this article
Cite this article
Capasso, R., Nizzoli, R., Tiseo, M. et al. Extra-pleuric coaxial system for CT-guided percutaneous fine-needle aspiration biopsy (FNAB) of small (≤20 mm) lung nodules: a novel technique using multiplanar reconstruction (MPR) images. Med Oncol 34, 17 (2017). https://doi.org/10.1007/s12032-016-0871-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-016-0871-4