Abstract
The aim of this study is to evaluate the feasibility of percutaneous needle biopsy of mediastinal masses under conebeam computed tomography (CBCT) and “XperGuide” navigation guidance. From September 2013 to April 2016, 40 patients (25 men and 15 women; mean age 52.5 years; range 18.7–86.4 years) with 40 mediastinal masses underwent CBCT-/”XperGuide”-guided percutaneous needle biopsies. Technical success, sensibility, specificity, positive predictive value (ppv), negative predictive value (npv) and complications rate were evaluated. Technical success evaluated as the correct positioning of the needle inside the lesion was 100%. Based on histopathological diagnosis, 2 of 40 biopsies (5%) resulted a false negative. Diagnostic accuracy was 95%, sensitivity was 95%, specificity was 100%, ppv was 100%, and npv was 33%. The mean total procedure time was 32 min (range 15–60 min) revealing a reduction in time comparing the first group of 20 patients (mean time 45 min) with the last group of 20 patients (mean time 17 min). No major complications were recorded. Only three patients (7.5%) had mild pneumothorax as demonstrated by post-procedural CBCT, resolved spontaneously. CBCT/“XperGuide” navigation system is a new, safe and accurate technique that can be used as guidance for mediastinal mass biopsies. It also permits the use of CT machines for diagnostic examinations relieving them from interventional procedures burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mediastinal tumors are uncommon and represent 3% of tumors within the chest [1]. Mediastinal lesions mostly occur in the anterior mediastinum rather than medium or posterior mediastinum [2]. Multimodality imaging plays an important role in determining the nature of the lesions [3, 4].
Different techniques could be used to perform percutaneous mediastinal biopsies. Percutaneous mediastinal biopsies are most commonly performed with computed tomography (CT) and ultrasonography (US) guidance as these modalities allow precise localization of the needle and of the target lesion [5]. CT guidance does not allow the visualization of the puncture in real time [6, 7], unless it is carried out using CT fluoroscopy (fluoro-CT) which, at the present moment, does not permit to reconstruct 3D images in real time.
Interventional magnetic resonance (MR) imaging provides appealing features for the visualization and biopsy of mediastinal masses [8].
Conebeam CT (CBCT) is a new emerging technology that allows 3D image acquisition via a C-arm fluoroscopy system to perform imaging-guided needle interventions. The system produces images similar to those of CT providing the operator with the possibility of real-time fluoroscopy with greater flexibility in the orientation of the detector around the patient compared to the closed CT gantry. A newly developed real-time 3D fluoroscopy guidance system for needle interventions merges conebeam CT with dedicated planning and navigation software (XperGuide, Philips Healthcare, Best, The Netherlands). This software allows the operator to direct needle in real time with fluoroscopy, once the trajectory has been established by the images acquired in 3D CBCT [9–12].
The purpose of this study was to determine the diagnostic performance and safety of conebeam CT-guided percutaneous needle biopsy using XperGuide navigation software in patients with mediastinal lesions.
Materials and methods
Patients
We retrospectively evaluated the hospital records of the 40 patients (25 men and 15 women; mean age 52.5 years; range 18.7–86.4 years) with 40 mediastinal lesions (median diameter 9.5 cm; range 2.5–16.5 cm) who underwent CBCT-/XperGuide-guided percutaneous needle biopsies from September 2013 to April 2016.
Our internal review board approved each procedure, and informed consent was obtained from all individual participants the day before the procedure.
Patients with contraindications for percutaneous intervention (e.g., blood coagulation disorder) were excluded from the study. A chest CT, in our institution or elsewhere, was obtained in all cases and interpreted by a board-certified radiologist with 5 years of experience in thoracic imaging. The images were evaluated by the operator before the procedures, to determine the feasibility of the biopsy.
The procedures were performed by a team of four radiologists with experience in the new C-arm CBCT technology, in our hospital since 2009.
Procedure workflow
Transthoracic needle biopsy: technical procedure
Mediastinal biopsies were performed in the angiography suite equipped with C-arm CBCT system (Philips Allura Xper FD20 system, Philips, Best NL) and with dedicated “XperGuide” software (Philips Healthcare, Best, NL).
The patient was positioned prone or supine, depending on the lesion location and on the access considered optimal. During the procedure, each patient received continuous monitoring of heart rate, oxygen saturation, respiratory rate and blood pressure.
All patients included in the present study underwent CBCT in modality “XperCT 5s” integrated with XperGuide navigation software (Philips Healthcare). With this modality, the motorized C-arm covered a 240° clockwise arc at a rotation speed of up to 55°/s, 312 projection images (60 frames/s) acquired in 5.2 s. The C-arm gantry followed an open trajectory from +55° to −185°, and the acquisition parameters were set to 120 kV tube voltage, 0.4 Cu filtration, 5- to 6-ms exposure time and 250 mA tube current, the latter being modulated automatically during the acquisition to adjust for patient size. The two-dimensional projections were automatically transferred to the reconstruction workstation where they were reconstructed into 3D volumetric images with an isotropic resolution of 0.6 mm, a FOV of 250 × 250 × 194 mm and a matrix size of 384 × 384 × 296.
CBCT- guided biopsy
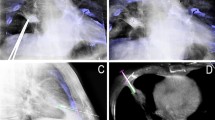
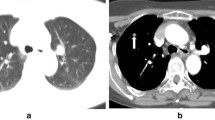
The first step was a CBCT scan for adequate planning of the biopsy. Briefly, using the XperGuide software, the operator or the assistant in training at the workstation monitor established the target in the context of the lesion (“target point”) and decided the needle entry point at the skin surface. In all cases, we used a 20-gauge cutting needle with a coaxial system (Biopsy Bell, Medical Device, Modena, Italy). The virtual segment connecting the entry and target points marked the needle path (Fig. 1). Based on this planning, the XperGuide software automatically calculated the C-arm correct position, to display the needle “entry point” on the patient’s skin. This phase of the procedure, followed by C-arm positioning, was called “entry point position.” After skin disinfection at the access area and under local anesthesia (10 cc of 2% mepivacaine, Angelini, Rome, Italy), via fluoroscopy the operator positioned the needle tip at the cutaneous “entry point,” based on the CBCT image appearing on the monitor as a fusion of the 3D volume previously acquired using CBCT and the real-time fluoroscopy bi-dimensional plane. At this time, the C-arm was rotated in the “progression view” position, perpendicular to the previous one. Then, the needle was advanced into the chest to reach the target point, following the virtual path previously determined and displayed on the monitor in real-time fluoroscopy. Thereafter, a second CBCT scan was performed to verify the needle correct placement (Fig. 2), and the biopsy was taken. A third and final scan was acquired to assess any biopsy-related complications (Fig. 3). The biopsy material was macroscopically assessed by the interventional radiologist, and another satisfactory specimen was obtained when necessary. Rapid on-site cytopathology examination was not available at our unit.
After every biopsy, the patient was monitored for at least 4 h in the recovery room, and before discharge, a chest X-ray exam was done in a single PA projection in maximum expiration, to highlight possible pneumothorax or hemorrhage.
Biopsy tissue samples were formalin-fixed and paraffin-embedded for pathologic examination. The biopsy material was considered inadequate if sampled tissue was insufficient for pathologic diagnosis of the pulmonary lesion (no specimen, necrotic tissue, normal lung/chest wall tissue).
Data collection and analysis
Data were assessed for technical success, diagnostic performance, procedure time and complications. Technical success was defined as the correct placement of the needle within the lesion.
Diagnostic performance was evaluated by calculating sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy. The final diagnosis was confirmed by a pathological examination of surgical specimens; in cases where no surgical resection was performed, the final diagnosis was confirmed by clinical and radiological follow-up. True positive (TP) was biopsies result of malignant lesion that agreed with the definitive histological findings or with the results of the follow-up. True negative (TN) was biopsies result of benign disease which resolved or remained unchanged during the follow-up. False negative (FN) was patients in which the histological results of the biopsy sample were negative for malignancy and thus were discordant with the examination of the surgical specimen, which instead documented malignancy.
Mean total procedure time was recorded. Mean total procedure time was considered from the first acquired CBCT until the end of the procedure including the time needed to plan the needle pathway using the XperGuide navigation system.
Complications were classified into major and minor according to the SIR classification (Society of Interventional Radiology) [13].
Results
Technical success was obtained in 100% of the patients.
Based on histopathological diagnosis, 2 of 40 biopsies (5%) resulted as false negative (Table 1).
Diagnostic accuracy was 95%, sensitivity was 95%, specificity was 100%, positive predictive value was 100%, and negative predictive value was 33%.
The collected data revealed a reduction in the mean total procedure time to procedure comparing a first from the first 20 patients (group A: between September 2013 December 2014) to the 20 patients (group B: between January and April 2016). In group A, the mean total procedure time was 45 min (range 30–60 min); in group B, the mean total procedure time was 17.6 min (range 15–20 min).
No major complications were recorded. Only three patients (7.5%) had mild pneumothorax as demonstrated by post-procedural CBCT. In these patients, pneumothorax resolved spontaneously a few hours after procedure.
Discussion
XperGuide/CBCT is considered as an innovative technique for interventional procedures as thoracic and abdominal percutaneous needle biopsy or ablative treatments [9–12, 14–19].
Braak et al. [5] performed mediastinal needle interventions using XperGuide/CBCT guidance in 5 of 145 patients with a technical success of 100% and an accuracy of 93.1%, similar to our results. However, data reported in this study include different anatomic areas (upper and lower thorax, upper and lower abdomen and musculoskeletal) making difficult a direct comparison with our study. Other authors examined XperGuide/CBCT during percutaneous transthoracic needle biopsy of lung nodules [6, 13, 14]. In these studies, accuracy ranged from 91.7 to 97% (mean 93.7%), sensitivity ranged from 90 to 95.7% (mean 92.2%), and specificity was 100% in all reports, with similar results compared to our study. Nevertheless, it is difficult to make a comparison between the two studies, due to different anatomic sectors and other variables (e.g., lesion depth and diameter and patient breathing movements).
Recently Kim et al. [19] reported the larger series of CBCT-guided mediastinal biopsies with high accuracy (97.4%) for the diagnosis of malignant mediastinal lesions in accordance with our results.
They highlighted the utility of XperGuide/CBCT in imaging-guided percutaneous biopsy of mediastinal lesions. Thanks to multiplanar reconstructions, needle pathway can be visualized during the entire procedure with high spatial resolution. CBCT associated with the navigation system guarantees the technical success avoiding important anatomic structures. Co-registering live fluoroscopy with CBCT 3D volume reconstruction allows the operator to reference the fused imaging during fluoroscopy, combining fusion guidance with real-time X-ray guidance [19].
To the best of our knowledge, this is the first study which evaluates the procedure time. It is our opinion that it is important to evaluate the timing in order to understand whether the operator needs a learning curve and whether the procedure is time-consuming compared to CT-guided mediastinal biopsies. We considered the mean total time as the elapsed time between the first acquired CBCT and the end of the procedure, including the time needed for planning the needle pathway with XperGuide navigation system. We compared group A (September 2013–December 2014) and group B (January 2015–April 2016). The mean procedure time in group A was 45 min (range 30–60 min), whereas in group B, it was 17.6 min (range 15–20 min). The mean total procedure time decreased progressively in connection with increasing operator experience and confidence, demonstrating the significant relationship of this technique with the learning curve of the operator. An effective dose reduction could be hypothesized with the decreasing mean total procedure time and thanks to the reduced number of CBCT scans needed during biopsy, related to the greater precision during the approach to lesion sampling with the XperGuide software. However, we decided to focus our study on the technical aspect of the procedure, not considering the dosimetric aspect [20].
Anyway we reported recently, in other study concerning lung biopsies [21], that the mean estimated effective dose through CBCT-guided lung biopsies was slightly lower than that of fluoro-CT-guided biopsies.
Non-fatal complications are taken into account during percutaneous needle interventions. Complications rate is calculated to be 3.85% by Kim et al. [19]. In the literature, studies about lung percutaneous needle biopsy is described a rate of 19–22.6% referring to minor complications and 0–2.4% referring to major complications [10, 17, 18]. In the present study, we reported 8% mild self-limiting pneumothorax (2/25 patients) and no major complications.
There are some limitations in our study. First, no randomized comparison was made between CBCT guidance and CT/fluoro-CT guidance. Second, we have not included DAP and effective dose using CBCT guidance. Finally, the small number of patients is a limit.
However, with this preliminary study we wanted to focus on feasibility, safety and accuracy of the technique.
The results of this study lead us to believe that XperGuide/CBCT guidance during percutaneous mediastinal needle biopsy appears to be a safe and accurate method to biopsy mediastinal lesions, with a technical success of 100% and low rate of minor complications (8%). Furthermore, the possibility of performing biopsies in angiographic suite with XperGuide/CBCT could be an important advantage in order to reduce the workload of the CT service.
The results obtained in our study should be considered preliminary, but they are encouraging and worthy of further study.
References
Aroor AR, Prakasha RS, Seshadri S, Teerthanath S, Raghuraj U. A study of clinical characteristics of mediastinal mass. J Clin Diagn Res. 2014;8(2):77–80.
Ching CO, Lynette LST. Imaging of anterior mediastinal tumours. Cancer Imaging. 2012;12:506–15.
Reginelli A, Rossi C, Capasso R, Urraro F, Cagini L, Di Crescenzo V, et al. Evaluation with multislice CT of the hilar pulmonary nodules for probable infiltration of vascular-bronchial structures. Recenti Prog Med. 2013;104:403–5.
Brunese L, Greco B, Setola FR, Lassandro F, Guarracino MR, De Rimini M, et al. Non-small cell lung cancer evaluated with quantitative contrast-enhanced CT and PET-CT: net enhancement and standardized uptake values are related to tumour size and histology. Med Sci Monit. 2013;7(19):95–101.
Gupta S, Seaberg K, Wallace M. Imaging-guided percutaneous biopsy of mediastinal lesions: different approaches and anatomic consideration. Radiographics. 2005;25(3):763–86.
De Filippo M, Saba L, Silva M, Zagaria R, Concari G, Nizzoli R, et al. CT-guided biopsy of pulmonary nodules: is pulmonary hemorrhage a complication or an advantage? Diagn Interv Radiol. 2014;20(5):421–5.
De Filippo M, Saba L, Concari G, Nizzoli R, Ferrari L, et al. Predictive factors of diagnostic accuracy of CT-guided transthoracic fine-needle aspiration for solid noncalcified, subsolid and mixed pulmonary nodules. Radiol Med. 2013;118(7):1071–81.
Lu Y, Fritz J, Li C, Liu M, Lee P, Wu L, Carrino JA. Magnetic resonance imaging-guided percutaneous biopsy of mediastinal masses. Diagnostic performance and safety. Invest Radiol. 2013;48(6):452–7.
Braak SJ, Van Strjen MJL, Van Leersum M, Van Es HW, Van Heesewijk JPM. Real-time 3D fluoroscopy guidance during needle interventions: technique, accuracy and feasibility. AJR Am J Roentgenol. 2010;194(5):W445–51.
Floridi C, Muollo A, Fontana F, et al. C-arm cone-beam computed tomography needle path overlay for percutaneous biopsy of pulmonary nodules. Radiol Med. 2014;119(11):820–7.
Carrafiello G, Fontana F, Mangini M, Ierardi AM, Cotta E, Floridi C, Piacentino F, Fugazzola C. Initial experience with percutaneous biopsies of bone lesions using XperGuide cone-beam CT (CBCT): technical note. Radiol Med. 2012;117:1386–97.
Busser WMH, Hoogeveen YL, Veth RPH, Schreuder HWB, Balguid A, Renema WK, Schultzekool LJ. Percutaneous radiofrequency ablation of osteoid osteomas with use of real-time needle guidance for accurate needle placement: a pilot study. Cardiovasc Intervent Radiol. 2011;34:180–3.
Cardella JF, Kundu S, Miller DL. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2009;20(7 Suppl):S189–91.
Racadio JM, Babic D, Homan R, Rampton JW, Patel MN, Racadio JM, Johnson ND. Live 3D guidance in the interventional radiology suite. AJR. 2007;189:W357–64.
Braak SJ, Van Melick HHE, Onaca MG, Van Heesewijk JPM, Van Strijen MJL. 3D cone-beam CT guidance, a novel technique in renal biopsy-results in 41 patients with suspected renal masses. Eur Radiol. 2012;22:2547–52.
Floridi C, Radaelli A, Abi-Jaoudeh N, Grass M, De Lin M, Chiaradia M, Geschwind JF, Kobeiter H, Squillaci E, Maleux G, Giovagnoni A, Brunese L, Wood B, Carrafiello G, Rotondo A. C-arm cone-beam computed tomography in interventional oncology: technical aspects and clinical applications. Radiol Med. 2014;119:521–32.
Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology. 2014;271(1):291–300.
Braak SJ, Herder GJM, Van Heesewijk JPM, Van Strijen MJL. Pulmonary masses: initial results of cone-beam CT guidance with needle planning software for percutaneous lung biopsy. Cardiovasc Intervent Radiol. 2012;35:1414–21.
Kim H, Park CM, Lee SM, Goo JM. C-arm cone-beam CT virtual navigation-guided percutaneous mediastinal mass biopsy: diagnostic accuracy and complications. Eur Radiol. 2015;25(12):3508–17.
Abi-Jaoudeh N, Kruecker J, Kadoury S, Kobeiter H, Venkatesan A, Levy E, Wood BJ. Multimodality image fusion guided procedures: technique, accuracy, and applications. Cardiovasc Intervent Radiol. 2012;35(5):986–98.
Rotolo N, Floridi C, Imperatori A, Fontana F, Ierardi AM, Mangini M, Arlant V, De Marchi G, Novario R, Dominioni L, Fugazzola C, Carrafiello G. Comparison of cone-beam CT-guided and CT fluoroscopy-guided transthoracic needle biopsy of lung nodules. Eur Radiol. 2016;26(2):381–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Floridi, C., Reginelli, A., Capasso, R. et al. Percutaneous needle biopsy of mediastinal masses under C-arm conebeam CT guidance: diagnostic performance and safety. Med Oncol 34, 67 (2017). https://doi.org/10.1007/s12032-017-0911-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-017-0911-8