Abstract
Metabolic reprogramming is an important hallmark of cancer cells, including the alterations of activity and expression in tricarboxylic acid (TCA) cycle key enzymes. Previous studies have reported the associations between tumor formation and three core enzymes involved in the TCA cycle. However, the association between functional single nucleotide polymorphisms (SNPs) in one of TCA cycle key gene isocitrate dehydrogenase (IDH) and the overall survival of hepatocellular carcinoma (HCC) patients treated with transcatheter arterial chemoembolization (TACE) has never been investigated. Five functional SNPs in IDH1 and IDH2 genes were genotyped using the Sequenom iPLEX genotyping system in a cohort of 419 unresectable Chinese HCC patients treated with TACE. Multivariate Cox proportional hazards model and Kaplan–Meier curve were used for the prognosis analysis. We found that SNPs rs12478635 in IDH1 and rs11632348 in IDH2 gene exhibited significant associations with death risk in HCC patients in the dominant model (HR 1.33; 95 % CI 1.02–1.73; P = 0.037) and in recessive model (HR 1.87; 95 % CI 1.27–2.75; P = 0.001), respectively. Moreover, we observed a cumulative effect of these two SNPs on HCC overall survival, indicating a significant trend of death risk increase with increasing number of unfavorable genotypes (P for trend = 0.001). Additionally, our data suggest that unfavorable genotypes of two SNPs may be used as an independent prognostic marker in those with advanced stage and patients with serum AFP <200 μg/L. Our results for the first time suggest that IDH gene polymorphisms may serve as an independent prognostic marker for HCC patients treated with TACE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common cancers and third leading cause of cancer-related death worldwide. Almost half of these cases and deaths were estimated to occur in China [1]. According to the data from the National Central Cancer Registry of China, the crude incidence of HCC was 27.29/100,000, and the crude mortality was 23.76/100,000 in 2010 [2]. The prognosis of post-operational HCC patients is still poor due to the high recurrence rate, and most HCC patients, diagnosed with advanced tumors, have to receive palliative or conservative therapy only [3]. Transcatheter arterial chemoembolization (TACE) is one of the therapies recommended as first-line therapy for patients with intermediate-stage HCC [4]. It has been demonstrated that TACE significantly improves the overall survival of unresectable HCC patients [5]. But there is still a lack of effective and specific biomarkers for prediction of TACE treatment responses.
The tricarboxylic acid (TCA) cycle, which occurs in mitochondria, is a core pathway for the metabolism of sugars, lipids, and amino acids [6]. The fundamental role of TCA cycle is usually described as a cyclic pathway constantly oxidizing the acetyl moiety of acetyl-CoA to CO2 and generating NADH and FADH2 that feed electrons to the respiratory chain for ATP generation [7]. Recently, the roles of mitochondrial alterations in cancer come to general attention with the discovery of mutations in mitochondrial TCA cycle core genes, which mainly include succinate isocitrate dehydrogenase 1 (IDH1) and 2 (IDH2), succinate dehydrogenase (SDH), and fumarate hydratase (FH) [8]. The recent identification of cancer-associated mutations in three metabolic enzymes suggests that altered cellular metabolism can indeed be a cause of some cancers [6, 9, 10].
Isocitrate dehydrogenase is a member of the β-decarboxylating dehydrogenase family with activity of catalyzing the oxidative decarboxylation of isocitrate to produce α-ketoglutarate (α-KG) and CO2 in the TCA cycle. There are three isoforms for IDH. IDH1 and IDH2 are the cytoplasmic and mitochondrial NADP+-dependent isocitrate dehydrogenases, respectively, and are homologs. IDH3, which is unrelated to IDH1 and IDH2, is a NAD+-dependent isocitrate dehydrogenase and has not been found to be mutated in cancer. IDH1 catalyzes this reaction in the cytosol and peroxisome to mediate a variety of cellular housekeeping functions, whereas IDH2 and IDH3 catalyze a step in the tricarboxylic acid (TCA) cycle [11]. Recently, loss-of-function mutations in IDH1 and IDH2 have been identified in a diverse array of cancers, including gliomas, acute myelogenous leukemia (AML), and cancers of thyroid, colon, and prostate [12–14].
Single nucleotide polymorphisms (SNPs) are easily detectable genetic variants as they can be analyzed from blood samples [15]. Thus, SNPs are attractive molecular markers for translational studies. Our previous studies have found that several SNPs are capable of predicting survival of HCC [16, 17]. Considering that the important role of TCA pathway core genes IDH1 and IDH2 in cancer progression [18], we hypothesize that SNPs in these genes may alter gene expression and/or protein activity and have an effect on the prognosis of HCC. To test this hypothesis, we selected five functional SNPs in the IDH1 and IDH2 genes and evaluated their associations with the survival in a cohort of 419 unresectable Chinese HCC patients treated with TACE.
Materials and methods
Study population
A total of 448 Han Chinese patients who had unresectable HCC were recruited from an undergoing study at the Departments of Pain Treatment, Tangdu Hospital affiliated to the Fourth Military Medical University in Xi’an and Eastern Hepatobiliary Surgery Hospital affiliated to the Secondary Military Medical University in Shanghai, China. These patients were recruited between January 2008 and November 2011. All cases had no previous history of other cancers or cancer-related treatments. There were no recruitment restrictions on age, gender, and tumor stage. After recruitment, all patients received TACE as the first-line treatment within a week after diagnosis. In the present study, 29 cases with incomplete clinical information or follow-up data or poor DNA quality were excluded. Finally, a total of 419 patients were included in the primary cohort and successfully genotype-assayed. Written informed consent was obtained from each participant before enrollment. Our study was approved by Hospital’s Ethics Committees both in Shanghai and Xi’an.
Demographic and clinical data
Demographic variables, including age, gender, ethnicity, residential region, and family history of cancer, were collected by well-trained interviewers. Detailed clinical information was collected through medical chart review or consulting with treating physicians, including the date of diagnosis, history of hepatitis virus infection, tumor number, tumor size, lymph node invasiveness and/or distant metastases, portal vein tumor thrombosis (PVTT), Child–Pugh score, serum alpha-fetoprotein (AFP), treatment protocols, and response. Clinical staging was determined according to tumor-node-metastasis (TNM) classification system. The follow-up information was updated every 3-month interval through onsite interview, direct calling, or medical chart review by a trained clinical specialist. The latest follow-up data in this analysis were obtained in July 2013. For each patient, 5 mL of venous blood was collected for genomic DNA extraction using the E.Z.N.A. Blood DNA Midi Kit (Omega Bio-Tek, Norcross, GA, USA) in the laboratory.
SNP selection and genotyping
Functional SNPs in the IDH1 and IDH2 genes were selected by an approach combining SNPs that were predicted in a web-based tool (available at http://snpinfo.niehs.nih.gov/snpinfo/snpfunc.htm) and SNPs that have been reported in related diseases. Only validated SNPs were selected, and SNPs with minor allele frequency <5 % in Han Chinese population (CHB) were excluded. Potential functional SNPs were identified to meet the following criteria: (a) SNPs located in miRNA binding sites of 3′ untranslated region (UTR), SNPs in the transcription factor binding site of the 5′ flanking region (2,000 bp upstream from the transcript start site), SNPs in splice sites or non-synonymous SNPs in exons. (b) SNPs were shown to be associated with disease according to the literature review [19]. If there were multiple potential functional SNPs within the same haplotype block (defined by the linkage coefficient r 2 >0.8), only 1 SNP was included. Finally, we identified five SNPs including one in IDH1 gene (rs12478635, TFBS), and four in IDH2 gene (rs11540478, splicing site; rs11632348, rs4283211, rs4932158, TFBS). All selected SNPs were genotyped by iPLEX genotyping system (Sequenom, San Diego, CA, USA). Laboratory persons who conducted the genotyping assay were blinded to patient information. Internal quality controls and negative controls were used to ensure genotyping accuracy, and strict quality control measures were implemented during genotyping with over 99.0 % concordance with the main genotyping results. Call rate for genotyping ranged from 98.6 to 99.8 %.
Statistical analysis
The SPSS Statistics19.0 software (IBM) was used for all statistical analyses in this study. The survival time was defined as the period from the date of first treatment to the date of death or last follow-up. The association between single SNP and OS was estimated as hazard ratios (HRs) by Cox proportional hazards regression model, with adjusting for gender, age, serum HBsAg, serum AFP, TNM stage, and treatment. The main analyses were performed under three genetic models, including dominant (homozygous variant + heterozygous genotypes vs. homozygous wild-type), recessive (homozygous variant vs. heterozygous + homozygous wild-type genotypes), and additive (homozygous variant vs. heterozygous vs. homozygous wild-type, showing as P for trend) models. The Kaplan–Meier survival curve and log-rank test were used to assess the differences in OS time. Cumulative effect was evaluated by the combination of unfavorable genotypes identified from the main effects analysis of individual SNPs. All statistical tests were two-sided and P ≤ 0.05 was considered to be statistically significant.
Results
Distribution of patients’ characteristics and prognosis analysis
A total of 419 eligible patients were included in this study. As shown in Table 1, the patients included 366 males (87.4 %) and 53 female (12.6 %) with a median age of 53 years (range 20–80). Three hundred and fifty-nine (85.7 %) patients were HBsAg positive. The percentage of patients with tumor stage I and II was 48.0 %. Two hundred and thirty (54.9 %) patients had significantly increased serum alpha-fetoprotein (≥200 μg/L). Among all patients, 341 (81.4 %) received only TACE treatment, whereas the remaining 78 (18.6 %) received TACE and other non-surgical treatments, such as radio frequency ablation (RFA), percutaneous ethanol injection (PEI), gamma knife radiosurgery, and/or immunoradiotherapy. During the median follow-up of 12.1 months (ranging from 2 to 57.0), a total of 326 (77.8 %) patients died and 8.7 % patients were lost during follow-up. The median survival time for all patients was 9.9 months. Furthermore, multivariate analysis indicated significant poor overall survival in HCC patients’ advanced tumor stage III and IV (HR 1.87; 95 % CI 1.48–2.35) and higher serum AFP (HR 1.40; 95 % CI 1.11–1.77). But patients who received TACE and other non-surgical treatments showed a significantly decreased risk of death (HR = 0.40; 95 % CI 0.29–0.56) compared with those treated by TACE alone. There was no association between HCC outcome and gender (P = 0.499), age (P = 0.956), as well as HBV infection status (P = 0.220).
Association of SNPs with clinical outcome in HCC patients
We assessed the association of each individual SNP with clinical outcome using multivariate Cox proportional hazards model with adjustment for gender, age, HBV infection, TNM stage, serum AFP, and treatment. We found that rs12478635 was significantly associated with HCC overall survival (Table 2). Compared to the homozygous wild-type (WW) of rs12478635, heterozygous variant (WV) and the homozygous variant (VV) conferred a significant increased risk of death (HR 1.33; 95 % CI 1.02–1.73; P = 0.037) in HCC patients. Another two SNPs rs11632348 and rs4283211 in IDH2 gene were significantly associated with increased death risk in HCC patients with HR of 1.87 (95 % CI 1.27–2.75; P = 0.001) and 1.88 (95 % CI 1.28–2.77; P = 0.001), respectively, under recessive model. Because of the similar risk ratio of these two SNPs, we evaluated the linkage disequilibrium (LD) of them in our data and the r 2 was over 0.8 between these SNPs. So we only choose one (rs11632348) of them for further analysis.
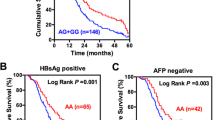
Cumulative effect of unfavorable genotypes on HCC overall survival
To further assess the cumulative effect of genetic variants on HCC overall survival, we conducted a combination analysis by including the two SNPs with a significant association in single SNP analysis. The unfavorable genotypes were defined as WV + VV for rs12478635 and VV for rs11632348. When we combined these unfavorable genotypes, there was a significant trend of increasing death risk with increasing number of unfavorable genotypes. Compared with the reference (group 1 without any unfavorable genotypes), the HRs for patients with 1 (group 2) and 2 (group 3) unfavorable genotypes were 1.33 (95 % CI 1.01–1.75; P = 0.044) and 2.45 (95 % CI 1.52–3.97, P < 0.001), respectively. A significant dose–response trend was observed as well (P = 0.001) (Table 3). Kaplan–Meier analysis showed that there was a significant trend for decreased overall survival with the increasing number of unfavorable genotypes (Log rank P = 0.031, Fig. 1).
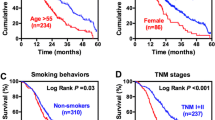
Stratified analysis on association of unfavorable genotypes with outcomes in HCC patients
The associations between unfavorable genotypes and HCC survival were further evaluated by stratified analysis of AFP level and TNM stage. As shown in Table 4, the significant increased death risk conferred by unfavorable genotypes is observed in patients with AFP <200 μg/L (HR 1.90; 95 % CI 1.21–2.99), but not in patients with AFP ≥200 μg/L (HR 1.19; 95 % CI 0.84–1.70). Similar results were also observed in patients with advanced stage (stage III and IV, HR 1.77; 95 %CI 1.21–2.60; P = 0.003), but not in patients with early stage (stage I and II) (HR 0.97; 95 %CI 0.65–1.46; P = 0.896). As indicated in Fig. 2a–d, log-rank test indicates a significant difference in overall survival between patients with unfavorable genotypes in above-mentioned subgroups.
Discussion
In the present study, we examined whether genetic polymorphisms in the IDH1 and IDH2 gene are associated with survival in a cohort of 419 TACE-treated HCC patients. The most important finding is that SNP rs12478635 in 5′UTR region of IDH1 and rs11632348 in 5′UTR region of IDH2 are significantly associated with HCC overall survival and cumulative effect analysis demonstrated that the effects of these SNPs on OS of HCC patients showed a dose-dependent manner. Additionally, our data suggest that unfavorable genotypes of two SNPs may be used as an independent prognostic marker in those with advanced stage and patients with serum AFP <200 μg/L. To the best of our knowledge, this is the first study to report that IDH gene polymorphisms may serve as an independent prognostic marker for HCC patients treated with TACE.
Cellular metabolism has been hypothesized to play a central role in cancer [20]. Mutations in metabolic enzymes, including IDH1 and IDH2, in cancer strongly implicate altered metabolism in tumorigenesis [6, 10]. In eukaryotic cells, IDH1 and IDH2 are homodimeric NADP+-dependent enzymes that catalyze the oxidative decarboxylation of isocitrate to produce a-ketoglutarate, NADPH, and CO2 [21]. Gain-of-functions mutations in IDH1 and IDH2 generate neomorphic enzyme activity to catalyze the production of high levels of a metabolite, (R)-2-hydroxyglutarate [(R)-2HG], which is normally found at very low levels in cells [22, 23]. (R)-2HG promotes cellular transformation, perhaps by altering the redox state of cells or modulating the activity of metabolic and epigenetic tumor suppressor enzymes that use the structurally similar metabolite a-ketoglutarate as a cosubstrate [11, 14, 24]. Another hypotheses suggested that loss of IDH activity from either loss of the wild-type allele or gain of a dominant-negative mutant allele alters normal mitochondrial function and promotes the metabolic switch of cancer cells to glycolysis, the major bioenergic form in cancer cells as suggested by Warburg [20, 25, 26].
Recently, a series of studies have reported the association between mutations in IDH genes and various malignancies. Several sequencing studies of malignant gliomas confirmed that IDH1 Arg132 mutation is very common in specific types of adult brain tumors, occurring in >70 % of adult grade II and grade III gliomas and >80 % of adult secondary glioblastoma multiformes [27, 28]. IDH1 Arg132 mutation was also identified in normal karyotype acute myelogenous leukemia (AML) by whole-genome sequencing [29]. Besides, IDH mutations have been found in 10–20 % of cholangiocarcinomas as well as a few rare cases of paraganglioma, colon cancer, prostate cancer, and lung cancer [13, 28, 30–32]. All these studies strongly support the idea that the mutations in IDH are involved in the development or progression of human cancers.
Since SNPs play an important role in the variation of gene expression level and activity of proteins, it is reasonable to presume that SNPs in IDH genes may affect the intracellular concentration of the metabolites through their impact on the enzyme activity. Variations of these metabolites would activate oncogenic signaling pathways at different levels in tumor cells, leading to different characteristics of tumor and distinctions in patient survival at last. Indeed, it has been reported that variant genotype of rs11554137 in IDH1 is associated with poor prognosis of AML and glioma [33–35]. In addition, genotype of rs11554137 is associated with the expression level of IDH1 [33]. In our study, we for the first time linked the SNPs in IDH genes with clinical outcome of HCC patients. Both the significant SNPs rs12478635 and rs11632348 are located in the predicted transcription factor binding sites in IDH1 and IDH2 genes. It is reasonable to assume that genetic variation of these SNPs might alter the expression level of IDH by affecting the binding capacity of specific transfactors and thus to regulate the translational efficacy of IDH mRNA.
The present study had some limitations. Firstly, only 419 patients were included for statistical analysis, so our findings need to be confirmed by additional studies with large sample size. Second, the exact biological significance of these SNPs need further clarification by functional studies. Moreover, our results should be validated among different ethnic populations in future.
In conclusion, our study reported the first epidemiological evidence supporting a role of rs12478635 and rs11632348 in the prognosis prediction of Chinese HCC patients treated with TACE. Further functional studies are warranted to understand the underlying mechanism implied in our findings.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Wei KR, Yu X, Zheng RS, Peng XB, Zhang SW, Ji MF, et al. Incidence and mortality of liver cancer in China, 2010. Chin J cancer. 2014;33(8):388–94. doi:10.5732/cjc.014.10088.
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245–55. doi:10.1016/S0140-6736(11)61347-0.
Murata S, Mine T, Ueda T, Nakazawa K, Onozawa S, Yasui D, et al. Transcatheter arterial chemoembolization based on hepatic hemodynamics for hepatocellular carcinoma. Sci World J. 2013;2013:479805. doi:10.1155/2013/479805.
Bruix J, Sherman M. Practice guidelines committee AAftSoLD. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–36. doi:10.1002/hep.20933.
Raimundo N, Baysal BE, Shadel GS. Revisiting the TCA cycle: signaling to tumor formation. Trends Mol Med. 2011;17(11):641–9. doi:10.1016/j.molmed.2011.06.001.
Cardaci S, Ciriolo MR. TCA cycle defects and cancer: When metabolism tunes redox state. Int J Cell Biol. 2012;2012:161837. doi:10.1155/2012/161837.
Wallace DC. Mitochondria and cancer. Nat Rev Cancer. 2012;12(10):685–98. doi:10.1038/nrc3365.
King A, Selak MA, Gottlieb E. Succinate dehydrogenase and fumarate hydratase: linking mitochondrial dysfunction and cancer. Oncogene. 2006;25(34):4675–82. doi:10.1038/sj.onc.1209594.
Pollard PJ, Wortham NC, Tomlinson IP. The TCA cycle and tumorigenesis: the examples of fumarate hydratase and succinate dehydrogenase. Ann Med. 2003;35(8):632–9.
Reitman ZJ, Yan H. Isocitrate dehydrogenase 1 and 2 mutations in cancer: alterations at a crossroads of cellular metabolism. J Natl Cancer Inst. 2010;102(13):932–41. doi:10.1093/jnci/djq187.
Dang L, Jin S, Su SM. IDH mutations in glioma and acute myeloid leukemia. Trends Mol Med. 2010;16(9):387–97. doi:10.1016/j.molmed.2010.07.002.
Kang MR, Kim MS, Oh JE, Kim YR, Song SY, Seo SI, et al. Mutational analysis of IDH1 codon 132 in glioblastomas and other common cancers. Int J Cancer J Int du cancer. 2009;125(2):353–5. doi:10.1002/ijc.24379.
Yen KE, Bittinger MA, Su SM, Fantin VR. Cancer-associated IDH mutations: biomarker and therapeutic opportunities. Oncogene. 2010;29(49):6409–17. doi:10.1038/onc.2010.444.
Di Paolo A, Danesi R, Del Tacca M. Pharmacogenetics of neoplastic diseases: new trends. Pharmacol Res. 2004;49(4):331–42.
Zhao B, Lu J, Yin J, Liu H, Guo X, Yang Y, et al. A functional polymorphism in PER3 gene is associated with prognosis in hepatocellular carcinoma. Liver Int. 2012;32(9):1451–9. doi:10.1111/j.1478-3231.2012.02849.x.
Yuan P, Wang S, Zhou F, Wan S, Yang Y, Huang X, et al. Functional polymorphisms in the NPAS2 gene are associated with overall survival in transcatheter arterial chemoembolization-treated hepatocellular carcinoma patients. Cancer Sci. 2014;105(7):825–32. doi:10.1111/cas.12428.
Fu Y, Zheng S, Zheng Y, Huang R, An N, Liang A, et al. Glioma derived isocitrate dehydrogenase-2 mutations induced up-regulation of HIF-1alpha and beta-catenin signaling: possible impact on glioma cell metastasis and chemo-resistance. Int J Biochem Cell Biol. 2012;44(5):770–5. doi:10.1016/j.biocel.2012.01.017.
Xu Z, Taylor JA. SNPinfo: integrating GWAS and candidate gene information into functional SNP selection for genetic association studies. Nucleic Acids Res. 2009;37:W600–5. doi:10.1093/nar/gkp290 (Web Server issue).
Warburg O. On the origin of cancer cells. Science. 1956;123(3191):309–14.
Dalziel K. Isocitrate dehydrogenase and related oxidative decarboxylases. FEBS Lett. 1980;117(Suppl):K45–55.
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–44. doi:10.1038/nature08617.
Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA, et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell. 2010;17(3):225–34. doi:10.1016/j.ccr.2010.01.020.
Kaelin WG Jr. Cancer and altered metabolism: potential importance of hypoxia-inducible factor and 2-oxoglutarate-dependent dioxygenases. Cold Spring Harb Symp Quant Biol. 2011;76:335–45. doi:10.1101/sqb.2011.76.010975.
Leonardi R, Subramanian C, Jackowski S, Rock CO. Cancer-associated isocitrate dehydrogenase mutations inactivate NADPH-dependent reductive carboxylation. J Biol Chem. 2012;287(18):14615–20. doi:10.1074/jbc.C112.353946.
Oermann EK, Wu J, Guan KL, Xiong Y. Alterations of metabolic genes and metabolites in cancer. Semin Cell Dev Biol. 2012;23(4):370–80. doi:10.1016/j.semcdb.2012.01.013.
Balss J, Meyer J, Mueller W, Korshunov A, Hartmann C, von Deimling A. Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol. 2008;116(6):597–602. doi:10.1007/s00401-008-0455-2.
Bleeker FE, Lamba S, Leenstra S, Troost D, Hulsebos T, Vandertop WP, et al. IDH1 mutations at residue p. R132 (IDH1(R132)) occur frequently in high-grade gliomas but not in other solid tumors. Hum Mutat. 2009;30(1):7–11. doi:10.1002/humu.20937.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. New Engl J Med. 2009;361(11):1058–66. doi:10.1056/NEJMoa0903840.
Sjoblom T, Jones S, Wood LD, Parsons DW, Lin J, Barber TD, et al. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314(5797):268–74. doi:10.1126/science.1133427.
Gaal J, Burnichon N, Korpershoek E, Roncelin I, Bertherat J, Plouin PF, et al. Isocitrate dehydrogenase mutations are rare in pheochromocytomas and paragangliomas. J Clin Endocrinol Metab. 2010;95(3):1274–8. doi:10.1210/jc.2009-2170.
Sequist LV, Heist RS, Shaw AT, Fidias P, Rosovsky R, Temel JS, et al. Implementing multiplexed genotyping of non-small-cell lung cancers into routine clinical practice. Ann Oncol. 2011;22(12):2616–24. doi:10.1093/annonc/mdr489.
Wagner K, Damm F, Gohring G, Gorlich K, Heuser M, Schafer I, et al. Impact of IDH1 R132 mutations and an IDH1 single nucleotide polymorphism in cytogenetically normal acute myeloid leukemia: SNP rs11554137 is an adverse prognostic factor. J Clin Oncol. 2010;28(14):2356–64. doi:10.1200/JCO.2009.27.6899.
Ho PA, Kopecky KJ, Alonzo TA, Gerbing RB, Miller KL, Kuhn J, et al. Prognostic implications of the IDH1 synonymous SNP rs11554137 in pediatric and adult AML: a report from the children’s oncology group and SWOG. Blood. 2011;118(17):4561–6. doi:10.1182/blood-2011-04-348888.
Wang XW, Boisselier B, Rossetto M, Marie Y, Idbaih A, Mokhtari K, et al. Prognostic impact of the isocitrate dehydrogenase 1 single-nucleotide polymorphism rs11554137 in malignant gliomas. Cancer. 2013;119(4):806–13. doi:10.1002/cncr.27798.
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 81302054, No. 81272522 and No. 81270505) and grants2011gr0239 from the International S & T Cooperation Program of China.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Huiqing Zhang and Xu Guo have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, H., Guo, X., Dai, J. et al. Genetic variations in IDH gene as prognosis predictors in TACE-treated hepatocellular carcinoma patients. Med Oncol 31, 278 (2014). https://doi.org/10.1007/s12032-014-0278-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0278-z