Abstract
Background
Lynch syndrome (LS) increases the risk of many types of cancer, mainly colorectal cancer (CRC). The purpose of this study was to assess the prevalence of mismatch repair (MMR) deficiency in patients under the age of 50 with advanced adenomatous polyps, aiming at an early diagnosis of LS.
Methods
This retrospective, cross-sectional study included eligible patients with advanced adenomas diagnosed ≤ 50 years of age registered between April 2014 and February 2017 at three pathology centers in Mashhad. Pathological records were reviewed, and colon tissue specimens were analyzed by immunohistochemistry (IHC) staining to identify proteins which serve as markers for LS as they are related to loss of MMR gene (MLH1, MSH2, MSH6, and PMS2) expression.
Results
Of 862 consecutive patients, a total of 50 adenomas (54% males, 46% females of mean age 41.24 ± 6.5) met the eligibility criteria. Of the adenomas examined, 20 (40%) had a tubulovillous component, 34 (68%) had high-grade dysplasia, and 30 (60%) had were larger than 10 mm protrusions. None of the patients had loss of MMR protein expression.
Conclusion
No individual with MMR genetic disorder was identified by IHC screening of early-onset advanced colorectal adenomas. This strategy is therefore not an effective strategy for detecting MMR mutation carriers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lynch syndrome (LS), which accounts for about 3–5% of all colorectal cancers (CRCs), is an autosomal dominant disorder caused by germline mutations in one or more DNA mismatch repair (MMR) genes (MLH1, MSH2, MSH6, PMS2) or within the EpCAM gene [1,2,3,4,5]. It is characterized by early-age onset of CRC, and patients with LS are at increased risk of malignancies, predominantly LS-associated tumors [6, 7]. One of the most common precancerous lesions of CRC is colorectal adenoma [8], which in LS mutation carriers may precede invasive malignancy at increased rates and/or in younger ages compared with that seen in sporadic cases [3].
Immunohistochemistry (IHC) and tests for microsatellite instability (MSI) are used in screenings to identify individuals at high risk of LS [9]. Adenomas in carriers of mismatch repair (MMR) gene mutations have rates of MMR deficiencies from 50 to 84% [10,11,12]. There are little data on loss of MMR expression among sporadic adenomas. According to the current guidelines, routine screening for LS by IHC and/or MSI analysis is recommended in CRC patients up to 70 years old. Therefore, adenoma patients are not routinely screened for LS. However, screening for LS in patients with adenomatous polyps by IHC and/or MSI analysis, as a tailored-made surveillance strategy, could prevent future malignancy development and would be of clinical value.
There is some controversy about the role of loss of MMR expression with respect to progression of adenoma to cancer in various studies. Although only about 1–2% of early-onset colorectal adenomatous polyps have MMR deficiency [5, 6, 13], evaluating the role of MMR screening in the diagnosis of early-onset adenomatous polyps might still be relevant.
Lynch-associated CRCs almost evolve from adenomas. The adenomas of the carriers tend to be larger and more likely have high-grade dysplasia and/or villous component for early-onset adenomas compared to the sporadic ones [14, 15]. Likewise, the early-onset adenomas with high-grade dysplasia or villous component are most likely to show MMR deficiency [10, 11]. Since adenomas with MMR deficiency progress to adenocarcinoma more rapidly than sporadic ones (35 months versus 10–15 years), an early screening strategy to identify them would be useful [1, 3].
Iranian hereditary colorectal cancer registry is a registry program to detect, register, and follow LS patients and their families in Iran. It was started from Mashhad in 2012 and is spreading throughout the country. Previously, we recommended the identification of CRC cases at high risk of LS [16, 17]. However, no clear strategy is present for LS screening among colorectal adenomas. The current study was conducted to examine the performance of a strategy evaluating loss of MMR expression in the early-onset advanced colorectal adenomas in Iran, aimed to improve the identification of LS.
Materials and Methods
Setting and Participants
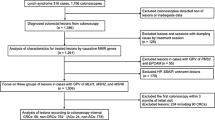
This retrospective cross-sectional study of a local population-based cohort of consecutive patients was conducted between April 2014 and February 2017 in Mashhad, north-eastern Iran. Initially, 862 patients with colorectal adenoma/polyps registered in the databases of three referral centers were included to review their pathology and colonoscopy reports. Of these, 68 cases were unavailable due to changes in address/phone number, and 56 refused to be interviewed. Of the remaining 738 cases, 688 were excluded due to the following exclusion criteria: < 18 years and > 50 years of age, previous history of CRC, hereditary polyposis syndrome, inflammatory bowel disease (IBD), incomplete colonoscopy, incomplete polypectomy, incomplete records, and non-advanced adenomas. The latter symptom was defined by the presence of one or more of the following histological and endoscopic findings: 10 mm or more in size, exhibited high-grade dysplasia, or consisting of ≥ 25% villous components. The most advanced lesion was evaluated for all cases. Finally, 50 early-onset advanced cases underwent IHC screening for the MMR proteins. The work followed the flowchart outlined in Fig. 1.
Family History of Cancer
The following data were collected for all patients: age at diagnosis, sex, family history for CRC in first- and second-degree relatives, colonoscopy including histological findings such as the number of adenomas, size and type of polyp and dysplasia grade through archive data, and pathology reports and interviews. Nonetheless, due to lacking CRC registry in the setting, several variables remained missing. Informed consent was obtained from all participants before interviewing and/or testing.
IHC Investigation of Adenomas
To confirm an adenoma diagnosis, all polyps were histologically assessed by two pathologists. IHC staining was performed for four proteins related to loss of expression of MMR genes (MLH1, MSH2, MSH6, and PMS2) and considered abnormal if IHC staining was absent for any of them. In the case of MHL1/PMS2 paired loss, BRAF testing [17, 18] for the V600E mutation would be performed to exclude sporadic adenomas; however, there were no cases with this characteristic in the IHC screening. Thus, the germline mutations of the MMR genes were not assessed in these cases.
Statistical Analysis
Chi-square and Fisher’s exact tests were used to perform intergroup and categorical comparisons. The Lilliefors and Shapiro–Wilk tests were used to examine normality of data [19]. Two-tailed Student’s t and Mann–Whitney U tests were used to compare grouped continuous variable data where appropriate. Reported p values of less than 0.05 were considered statistically significant. SPSS software version 16 (SPSS Inc., Chicago, IL, USA) was used to analyze the data.
Results
Of 862 eligible patients with colorectal adenoma/polyps, 738 cases with a mean age of 54.61 ± 14.53 were included in the study to describe their polyp’s characteristics. A total of 234 out of the 738 cases (31.70%) had an advanced adenoma, of which 50 met all selection criteria and were therefore included in the IHC staining for MMR proteins. The analysis showed no dMMR for any adenomas (see Fig. 1 for details).
Early-onset advanced adenoma characteristics. Of 50 early-onset advanced adenomas with a mean age of 41.24 ± 6.5 years included in the IHC analysis, 27 (54%) were from male patients (Table 1). The pathological features of these 50 cases are summarized in Table 2. The site of the early-onset advanced adenomas was distributed as follows: 44 cases (88%) were from the distal colon and 6 (12%) from the proximal colon. Of the 23 early-onset advanced adenomas that had sufficient information for evaluation of the family history of CRC, mostly had low-grade dysplasia (n = 15; 65.22%) and the mean age of these cases with family history of CRC was significantly higher than of that without a family history (46.86 ± 5.43 years vs. 40.94 ± 4.61, p value = 0.01).
Polyp characteristics. The location of adenomas in both males and females was mostly in the distal part of the colon (Table 3). The age of the patients with adenomas was mostly > 50, and there was no statistically significant difference between mean ages of the patients with advanced and non-advanced adenomas (Table 3). Statistically, there was a significant association between location of adenomas and their histological features, and the adenomas with each histological feature were mostly located at the distal site (Table 4).
Discussion
The results of IHC staining of MMR protein expression in an Iranian setting revealed MMR deficiency in none of the early-onset advanced adenomas. Our findings, in consistent with other literature [5, 13, 20, 21], suggest that screening early-onset advanced adenomas for early diagnosis of LS is likely not an effective strategy.
As early detection of LS patients could decrease the incidence of CRC [22,23,24], screening for MMR deficiency for all early-onset adenomas has been previously recommended by clinical criteria [25]. Although a study detected 6 (1.6%) of 378 adenomas by the MSI test and suggested MSI analysis of colorectal adenomas as a prescreening method of LS [26], another study, evaluating 40 early-onset adenomas using MSI and IHC testing for loss of MSH2 or MLH1 expression, did not find any positive results [21]. Our study confirmed the later study findings. However, there are differences between two study designs. While the former study included low-risk adenomas (< 5 mm in size with no dysplasia or villous histology), our research extended those findings to high-risk early-onset adenomas and reinforced their findings and conclusions. Furthermore, our study findings are in line with those of Kushnir et al. [13] that previously assessed 64 early-onset advanced adenomas and detected only one potential case of LS in a 19-year-old patient with a family history of CRC. Although our study and that of Kushnir et al. have the same study designs, they both evaluated small sample size of adenomas in limited centers that decrease the generalizability of those findings. On the other hand, our findings are consistent with those of Goverde et al. [20] that previously assessed 456 late-onset (55 to 75 years) advanced adenomas and reported no cases with this genetic disorder. In 508 patients with colorectal adenomas, MMR deficiency was detected in 6 samples, two of them with a family history of cancer [27]. Moreover, our findings confirmed those studies that found LS was infrequent in young patients with nonfamilial CRC [13, 28].
Nevertheless, to our knowledge, there is only one study on MMR deficiency among Iranian patients, i.e., Molaie et al. who investigated sporadic colorectal polyps in 400 patients without age restriction and irrespective of family history of CRC [6]. They detected loss of expression of MLH1 and PMS2 in serrated polyps more than in other adenomatous polyps and suggested MMR deficiency may cause sporadic colorectal polyps in younger age patients. The differences in results may be attributed to differences in sample size, the eligibility criteria, and the participants’ mean age. The strength of our study was inclusion of early-onset advanced adenomas, which are the highest risk of MMR deficiency [29, 30]. However, our results revealed no MMR deficiency when addressing early-onset advanced adenomas by IHC screening.
The findings of the large sample size screening of polyps in Iran are in line with the study by Conway et al. [31], and both the adenoma and advanced adenoma did not differ significantly between age and location groups, although both were less frequent in the younger and proximal site groups. Conway et al. suggested CRC screening should begin at age 40 years in their setting, while our MMR deficiency evaluation following this polyp screening did not confirm this strategy for Iran.
To the best of our knowledge, this is the first study evaluating MMR deficiency in early-onset advanced adenomas in Iranian patients. However, our study has some limitations; firstly, although all consecutive adenomas were screened, however, a small sample size and single center experience may fail to detect MMR deficiencies, and the results need to be confirmed in more extensive studies. Secondly, our screening for LS in tumor tissue may indeed have missed a few cases due to the lack of investigation on MMR deficiency non-polypous, which is another important precursor in LS. Finally, IHC screening strategy for the patient with LS may also miss a few cases.
Accordingly, routine universal IHC screening of early-onset (≤ 50 years) advanced colorectal adenomas for LS is not an effective strategy to identifying mutation carriers, and screening of newly diagnosed CRC cases should be more effective.
Availability of Data and Material
Data will be available upon request.
References
Giardiello FM, Allen JI, Axilbund JE, Boland CR, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US multi-society task force on colorectal cancer. Gastroenterology. 2014;147(2):502–26. https://doi.org/10.1053/j.gastro.2014.04.001.
Giardiello FM, Brensinger JD, Petersen GM. AGA technical review on hereditary colorectal cancer and genetic testing. Gastroenterology. 2001;121(1):198–213. https://doi.org/10.1053/gast.2001.25581.
Jass JR, Stewart SM, Stewart J, Lane MR. Hereditary non-polyposis colorectal cancer--morphologies, genes and mutations. Mutat Res. 1994;310(1):125–33. https://doi.org/10.1016/0027-5107(94)90016-7.
Lynch HT, Smyrk TC, Watson P, Lanspa SJ, Lynch JF, Lynch PM, et al. Genetics, natural history, tumor spectrum, and pathology of hereditary nonpolyposis colorectal cancer: an updated review. Gastroenterology. 1993;104(5):1535–49. https://doi.org/10.1016/0016-5085(93)90368-m.
Mendelsohn RB, Herzog K, Shia J, Rahaman N, Stadler ZK, Shike M. Molecular screening for Lynch syndrome in young patients with colorectal adenomas. Clin Colorectal Cancer. 2017;16(3):173–7. https://doi.org/10.1016/j.clcc.2017.01.002.
Molaei M, Yadollahzadeh M, Almasi S, Shivarani S, Fatemi SR, Zali MR. Sporadic colorectal polyps and mismatch repair proteins. Indian J Pathol Microbiol. 2011;54(4):725–9. https://doi.org/10.4103/0377-4929.91505.
Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Ruschoff J, et al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96(4):261–8. https://doi.org/10.1093/jnci/djh034.
Conteduca V, Sansonno D, Russi S, Dammacco F. Precancerous colorectal lesions (review). Int J Oncol. 2013;43(4):973–84. https://doi.org/10.3892/ijo.2013.2041.
Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017;3(4):464–71. https://doi.org/10.1001/jamaoncol.2016.5194.
Pino MS, Mino-Kenudson M, Wildemore BM, Ganguly A, Batten J, Sperduti I, et al. Deficient DNA mismatch repair is common in Lynch syndrome-associated colorectal adenomas. J Mol Diagn. 2009;11(3):238–47. https://doi.org/10.2353/jmoldx.2009.080142.
Tanaka M, Nakajima T, Sugano K, Yoshida T, Taniguchi H, Kanemitsu Y, et al. Mismatch repair deficiency in Lynch syndrome-associated colorectal adenomas is more prevalent in older patients. Histopathology. 2016;69(2):322–8. https://doi.org/10.1111/his.12941.
Walsh MD, Buchanan DD, Pearson SA, Clendenning M, Jenkins MA, Win AK, et al. Immunohistochemical testing of conventional adenomas for loss of expression of mismatch repair proteins in Lynch syndrome mutation carriers: a case series from the Australasian site of the colon cancer family registry. Mod Pathol. 2012;25(5):722–30. https://doi.org/10.1038/modpathol.2011.209.
Kushnir VM, Nalbantoglu I, Watson R, Goodwin J, Safar E, Chokshi RV, et al. Advanced colorectal adenomas in patients under 45 years of age are mostly sporadic. Dig Dis Sci. 2014;59(11):2757–64. https://doi.org/10.1007/s10620-014-3245-9.
De Jong AE, Morreau H, Van Puijenbroek M, Eilers PH, Wijnen J, Nagengast FM, et al. The role of mismatch repair gene defects in the development of adenomas in patients with HNPCC. Gastroenterology. 2004;126(1):42–8. https://doi.org/10.1053/j.gastro.2003.10.043.
Vasen HF, Taal BG, Nagengast FM, Griffioen G, Menko FH, Kleibeuker JH, et al. Hereditary nonpolyposis colorectal cancer: results of long-term surveillance in 50 families. Eur J Cancer. 1995;31a(7-8):1145–8.
Goshayeshi L, Ghaffarzadegan K, Khooei A, Esmaeilzadeh A, Rahmani Khorram M, Mosannen Mozaffari H, et al. Prevalence and clinicopathological characteristics of mismatch repair-deficient colorectal carcinoma in early onset cases as compared with late-onset cases: a retrospective cross-sectional study in northeastern Iran. BMJ Open. 2018;8(8):e023102. https://doi.org/10.1136/bmjopen-2018-023102.
Goshayeshi L, Khooiee A, Ghaffarzadegan K, Rahmani Khorram M, Bishehsari F, Hoseini B, Akhavan Rezayat K, Esmaeilzadeh A, Mosannen Mozaffari H, Ghanayee O, Lari S, Bahari A, Allahyari A, Bari A, Ganji A, Goshayeshi L, Rajabzadeh F, Esmaeili J (2017) Screening for Lynch syndrome in cases with colorectal carcinoma from Mashhad. Arch Iran Med 20 (6):332-337. 0172006/AIM.003.
Lee EJ, Park CK, Kim JW, Chang DK, Kim KM. Deletion mutation of BRAF in a serrated adenoma from a patient with familial adenomatous polyposis. APMIS. 2007;115(8):982–6. https://doi.org/10.1111/j.1600-0463.2007.apm_670.x.
Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012;10(2):486–9. https://doi.org/10.5812/ijem.3505.
Goverde A, Wagner A, Bruno MJ, Hofstra RMW, Doukas M, van der Weiden MM, et al. Routine molecular analysis for Lynch syndrome among adenomas or colorectal cancer within a National Screening Program. Gastroenterology. 2018;155(5):1410–5. https://doi.org/10.1053/j.gastro.2018.07.029.
Velayos FS, Allen BA, Conrad PG, Gum J Jr, Kakar S, Chung DC, et al. Low rate of microsatellite instability in young patients with adenomas: reassessing the Bethesda guidelines. Am J Gastroenterol. 2005;100(5):1143–9. https://doi.org/10.1111/j.1572-0241.2005.40862.x.
Jarvinen HJ, Aarnio M, Mustonen H, Aktan-Collan K, Aaltonen LA, Peltomaki P, et al. Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology. 2000;118(5):829–34. https://doi.org/10.1016/s0016-5085(00)70168-5.
Jarvinen HJ, Renkonen-Sinisalo L, Aktan-Collan K, Peltomaki P, Aaltonen LA, Mecklin JP. Ten years after mutation testing for Lynch syndrome: cancer incidence and outcome in mutation-positive and mutation-negative family members. J Clin Oncol. 2009;27(28):4793–7. https://doi.org/10.1200/jco.2009.23.7784.
Stupart DA, Goldberg PA, Algar U, Ramesar R. Surveillance colonoscopy improves survival in a cohort of subjects with a single mismatch repair gene mutation. Colorectal Dis. 2009;11(2):126–30. https://doi.org/10.1111/j.1463-1318.2008.01702.x.
Rodriguez-Bigas MA, Boland CR, Hamilton SR, Henson DE, Jass JR, Khan PM, et al. A National Cancer Institute Workshop on hereditary nonpolyposis colorectal cancer syndrome: meeting highlights and Bethesda guidelines. J Natl Cancer Inst. 1997;89(23):1758–62. https://doi.org/10.1093/jnci/89.23.1758.
Loukola A, Salovaara R, Kristo P, Moisio AL, Kaariainen H, Ahtola H, et al. Microsatellite instability in adenomas as a marker for hereditary nonpolyposis colorectal cancer. Am J Pathol. 1999;155(6):1849–53. https://doi.org/10.1016/s0002-9440(10)65503-4.
Zhu F, Pan D, Zhang H, Ye Q, Xu P, Pan J. Single-center study of Lynch syndrome screening in colorectal polyps. Hered Cancer Clin Pract. 2019;17:9. https://doi.org/10.1186/s13053-019-0108-6.
Goel A, Nagasaka T, Spiegel J, Meyer R, Lichliter WE, Boland CR. Low frequency of Lynch syndrome among young patients with non-familial colorectal cancer. Clin Gastroenterol Hepatol. 2010;8(11):966–71. https://doi.org/10.1016/j.cgh.2010.06.030.
Halvarsson B, Lindblom A, Johansson L, Lagerstedt K, Nilbert M. Loss of mismatch repair protein immunostaining in colorectal adenomas from patients with hereditary nonpolyposis colorectal cancer. Mod Pathol. 2005;18(8):1095–101. https://doi.org/10.1038/modpathol.3800392.
Shia J, Klimstra DS, Nafa K, Offit K, Guillem JG, Markowitz AJ, et al. Value of immunohistochemical detection of DNA mismatch repair proteins in predicting germline mutation in hereditary colorectal neoplasms. Am J Surg Pathol. 2005;29(1):96–104.
Conway AA, Gerry JM, Sacco F, Wren SM. High prevalence of adenomatous polyps in Alaska native people aged 40-49 years. J Surg Res. 2019;243:524–30. https://doi.org/10.1016/j.jss.2019.07.004.
Acknowledgements
The authors would like to thank all study participants.
Funding
This study was funded by Mashhad University of Medical Sciences (Grant number 951047).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Benyamin Hoseini, Ladan Goshayeshi, and Mahla Rahmani Khorram.
The first draft of the manuscript was written by Mahla Rahmani Khorram and Fatemeh Maghool and then edited by Benyamin Hoseini. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval and Consent to Participate
Ethical approval was obtained from the ethics committee of Mashhad University of Medical Sciences (IR.MUMS.fm.REC.1396.240), and the study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all participants before interviewing and/or testing.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khorram, M.R., Goshayeshi, L., Maghool, F. et al. Prevalence of Mismatch Repair-Deficient Colorectal Adenoma/Polyp in Early-Onset, Advanced Cases: a Cross-Sectional Study Based on Iranian Hereditary Colorectal Cancer Registry. J Gastrointest Canc 52, 263–268 (2021). https://doi.org/10.1007/s12029-020-00395-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-020-00395-y