Abstract
Background
The optimal interval of colonoscopy (CS) surveillance in cases with Lynch syndrome (LS), and stratification according to the causative mismatch repair gene mutation, has received much attention. To verify a feasible and effective CS surveillance strategy, we investigated the colorectal cancer (CRC) incidence at different intervals and the characteristics of precancerous colorectal lesions of LS cases.
Methods
This retrospective multicenter study was conducted in Japan. CRCs and advanced adenomas (AAs) in 316 LS cases with germline pathogenic variants (path_) were analyzed according to the data of 1,756 registered CS.
Results
The mean time interval for advanced CRCs (ACs) detected via CS surveillance was 28.7 months (95% confidence interval: 13.8–43.5). The rate of AC detection within (2.1%) and beyond 2 years (8.7%) differed significantly (p = 0.0003). AAs accounted for 43%, 46%, and 41% of lesions < 10 mm in size in the MLH1-, MSH2-, and MSH6-groups, respectively. The lifetime incidence of metachronous CRCs requiring intestinal resection for path_MLH1, path_MSH2, and path_MSH6 cases was 34%, 23%, and 14% in these cases, respectively. The cumulative CRC incidence showed a trend towards a 10-year delay for path_MSH6 cases as compared with that for path_MLH1 and path_MSH2 cases.
Conclusions
In cases with path_MLH1, path_MSH2, and path_MSH6, maintaining an appropriate CS surveillance interval of within 2 years is advisable to detect of the colorectal lesion amenable to endoscopic treatment. path_MSH6 cases could be stratified with path_MLH1 and MSH2 cases in terms of risk of metachronous CRC and age of onset.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lynch syndrome (LS) is an autosomal dominant disease caused by a germline pathogenic variant (path_) in a mismatch repair (MMR) gene [1]. The causative genes include MSH2, MLH1, MSH6, PMS2, and EPCAM [2, 3]. When DNA MMR function is impaired, the microsatellite instability (MSI) is typically high, and various types of tumors appear at a young age [4]. The rate of colorectal cancer (CRC) is very high among patients with LS, at 25–70% [5]. Therefore, colonoscopy (CS) surveillance intervals of 1–2 years are recommended. While this interval is better than an interval of 2–3 years, 1-year intervals are optimal [6, 7]. The guidelines of various medical associations have been revised based on evidence from Western countries. Efforts to validate optimal CS surveillance further are ongoing. Recently, CS surveillance protocols have become nonuniform across the causative MMR genes, and surveillance is recommended to be stratified according to the causative MMR gene [8]. In Europe and in the United States, the cumulative risk of developing CRC by age has been investigated, and stratification of CS surveillance protocols based on the patient’s age and causative MMR gene has been considered [9,10,11].
Moreover, a European validation study of optimal CS surveillance has shown no significant difference in the incidence of CRC at different intervals in three European countries [12], and the staging of CRC at detection was not different, regardless of the examination intervals used [13]. However, these reports from European countries did not include details of endoscopically treated lesions, such as precancerous lesions. The rationale for preventive CS treatment is supported by a report showing that a 1.0% increase in the adenoma detection rate was associated with a 3.0% decrease in the risk of cancer [14] and that the majority of the CRC carcinogenic processes are associated with an adenoma–carcinoma sequence, not only in sporadic cases, but also in cases of LS. Therefore, especially in LS, the particular LS-specific precancerous colorectal lesion should be considered, in addition to CRC.
Thus, in this study, we advanced adenoma (AA) and CRC associated with each causative MMR gene according to the CS registry of a multicenter study conducted in Japan under the recommended CS surveillance interval of 1–2 years.
Methods
Ethics statements
The Ethics Committees of the Japanese Society for Cancer of the Colon and Rectum (JSCCR) (No. 90–7) and Cancer Institute Hospital of the Japanese Foundation for Cancer Research (2019–1100) approved this study. This study was conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. This concept of observational study was disclosed on the conference website, at http://www.jsccr.jp/.
Patient data
We retrospectively extracted the information and data of all registered CS for LS cases with an identified germline variant, who underwent CS surveillance from January 2009 to December 2018 at any of the 13 participating institutes. To achieve uniformity between institutions, CS findings were recorded by each participating staff member according to the following definitions. Histopathological classifications included hyperplastic polyp (HP), sessile serrated adenoma/polyp (SSA/P), low-grade adenoma (LGA), high-grade adenoma (HGA), intramucosal carcinoma (pTis), slightly sub-mucosal invasive carcinoma (pT1a), and massive sub-mucosal invasive carcinoma (pT1b), according to the definition of the JSCCR [15]. Tumors were classified according to the International Cancer Union staging system (TNM) [16]. In this study, AA included HGA, regardless of size, in addition to pTis, which are defined as intramucosal carcinomas by the JSCCR. CRC referred to cancer in pT1, T2, T3, and T4 stages, while advanced CRC (AC) referred to cancers in pT2, T3, and T4 stages. Metachronous CRCs requiring surgery (r-CRCs) were those requiring surgical intervention, such as pT1b and AC. The morphologically classified polypoid lesions included 0-Is, 0-Isp, and 0-Ip; non-polypoid lesions included 0-IIa, laterally spreading tumors, 0-IIc, and 0-IIa + IIc (depressed lesions: 0-IIc and 0-IIa + IIc).
For the analysis by causative MMR genes, since the number of cases with path_PMS2 and path_EPCAM (spilt from MSH2, as in the original registry) were small and might not reflect the actual trend, this study focused on cases with path_MLH1, path_MSH2, and path_MSH6.
Colorectal cancers and advanced adenomas by causative MMR genes
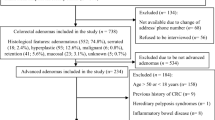
In the 316 included LS cases, 1756 CS sessions were tabulated according to the causative MMR gene (Fig. 1). In the participating institutions, regardless of the presence or absence of previous CRC, patients were instructed to undergo testing every 1–2 years, in accordance with the Japanese guidelines. Table 1 shows the follow-up period for each causative MMR gene and the number of colonoscopies performed during the study period. When examination indicated the need for an endoscopic treatment session, overlapping colorectal lesions were excluded from the analysis. To investigate the possibility of AA, even if the lesions were small in size, we examined the tumor diameters of colorectal polyps in cases with path_MLH1, path_MSH2, and path_MSH6. Lesion results of cases with path_MLH1, path_MSH2, and path_MSH6 are presented for the MLH1-group, MSH2-group, and MSH6-group, respectively.
During the enrolment period, 316 Lynch syndrome cases and 1756 colonoscopies were analyzed. Among these, we analyzed the characteristics of 1261 lesions by causative MMR genes. We focused on three groups of lesions in cases with germline pathogenic variants in MLH1, MSH2, and MSH6. In the analysis of incident CRCs, we excluded lesions diagnosed colonoscopically at 0–3 months as pre-existing lesions. MMR: mismatch repair; GPV: germline pathogenic variant; CRC: pT1, T2, T3, and T4; non-CRC: low-grade adenoma, high-grade adenoma, and pTis; AC: advanced colorectal cancer (pT2, T3, and T4) Non-AC: non-CRC and pT1
The time interval was calculated in months between the examination date on which each lesion (LGA, HGA, pTis, and pT1–4) was identified and the latest examination date. Since this was retrospective study, endoscopically resectable lesions, including precancerous lesions, were treated in a timely manner. Therefore, instead of cumulative incidence, we tabulated the proportion of each lesion detected within 1, 2, and 3-years, as well as beyond 1, 2, and 3-years. We excluded the first CS conducted within 3 months of the initial visit at a previous hospital, which would have been the prompt for undergoing genetic testing (Fig. 1).
In addition, any endoscopic findings (i.e., lesion detection and therapeutic intervention) and these endoscopically treated lesions were counted according to patient age. When an endoscopic finding was present, these CS were represented as “event present”.
Metachronous CRC rates and intestinal preservation rates in each case
The cumulative incidence of CRC in cases with path_MLH1, path_MSH2, and path_MSH6 was calculated from the age at which the first CRC was diagnosed, based on medical history information. Analysis of metachronous CRC during a patient’s lifetime was based on the surgical CRC resection dates, with intervals determined in months. In terms of the probability of intestinal preservation, we calculated the duration of intestinal preservation from the first surgery for CRC to the second CRC-related surgery.
Statistical analysis
The aggregation of lesion frequencies for each causative MMR gene is presented using descriptive statistics. The rate of detected CRC per CS interval was evaluated using the chi-squared test for the expected and observational frequencies. The occurrence of CS events by age for each causative MMR gene was calculated using R version 4.2.0 (R Project for Statistical Computing, Vienna, Austria; http://www.r-project.org/). The cumulative incidence of the first CRC and duration of intestinal preservation for each causative MMR gene, were calculated using the Kaplan–Meier method.
Results
In this study, 316 cases were genetically diagnosed with LS, as follows: path_MLH1, 124 cases; path_MSH2, 139 cases; path_MSH6, 37 cases; path_PMS2, 11 cases, and path_EPCAM, 5 cases (Table 1).
Colorectal cancers and advanced adenomas by causative MMR genes
In the MLH1-, MSH2-, and MSH6-groups, more than 80% of the lesions (84%, 88%, and 84%, respectively) were treated with curative endoscopic resection. In the MLH1-, MSH2-, and MSH6-group, AAs were present in 22%, 22%, and 16%, respectively, and non-polypoid lesions of early-stage cancer, such as pTis and pT1 stage accounted for 46%, 58%, and 44%, respectively (Table 1). AAs accounted for 43%, 46%, and 41% of lesions < 10 mm in size in the MLH1-, MSH2-, and MSH6-groups, respectively (Table 2). In the analysis of the incidence of CRC, 90 CRCs diagnosed at 0–3 months were excluded as pre-existing lesions (Fig. 1). Twenty-four ACs were detected in the MLH1-, MSH2-, and MSH6-groups overall, with a mean interval of 28.7 months (95% confidence interval, 13.8–43.5 months). The rates of AC detection during the 3-year surveillance period were 2.8% and 3.3% for detection within and beyond 1 year, respectively, whereas the rates of detection within and beyond 2 and 3 years were significantly different, at 2.1% and 8.7% (p = 0.0003), and at 2.5% and 8.5% (p = 0.0047), respectively (Table 3). In the MLH1-, MSH2-, and MSH6-groups, the rates of CRC detection within 2 years were 4.8%, 4.2%, and 5.2%, respectively, with more than half (11 of 17 lesions) of the CRCs in the MSH2-group being pT1 lesions (Fig. 2a). The 18 AC lesions detected within the 3-year surveillance interval are summarized in Fig. 2b: one lesion (pT4, mucinous) was detected beyond 1 year but within 2 years, and three lesions were detected beyond 2 years but within 3 years. Fourteen lesions in 10 cases, were detected within 1 year. These included six pT3 lesions, all in path_MLH1 cases (Fig. 2b).
a Colorectal cancers (CRCs) were detected within 2 years in some cases with germline pathogenic variants (path-) in MLH1, MSH2, and MSH6 (4.8%, 4.2%, and 5.1%, respectively). b Overview of advanced CRCs detected within 3 years. Nine lesions (seven cases) were found among the path_MLH1, eight lesions (six cases) among the path_MSH2, and one lesion among the path_MSH6 cases. Advanced CRCs of 300 cases in the three groups, 3.3% (10 cases) were detected in ≤ 1 year; 3.7% (11 cases) were detected in ≤ 2 years, and 4.7% (14 cases) were detected in ≤ 3 years. CRC; pT1, T2, T3, and T4; non-CRC: low-grade adenoma, high-grade adenoma, and pTis; OP: Surgical operation for CRC
When the occurrence of events was calculated according to age, the incidence of events was high at ages 50 and 65 years among those with path_MLH1, at ages 45 and 70 years for those with path_MSH2, and peaked at age 70 years for path_MSH6. Those events included endoscopic treatment for early-stage colorectal polyps (Online Resource 1: Figure).
Metachronous CRC rates and intestinal preservation rates in each case
The cumulative incidence of the first CRC and rates of intestinal preservation for path_MLH1, path_MSH2, and path_MSH6 cases are shown in Fig. 3. The median age at diagnosis of the first CRCs in path_MLH1, path_MSH2, and path_MSH6 were 43 (range: 25–83 years), 46 (range: 14–76 years), and 55 years (range: 24–80 years), respectively. The lifetime incidence of metachronous CRCs requiring intestinal resection was 34%, 23%, and 14% for path_MLH1, path_MSH2, and path_MSH6 cases, respectively, and the median ages for any detected metachronous CRC were 61 years (range: 24–84 years), 64 years (range: 36–84 years), and 67 years (range: 53–78 years), respectively. The median time elapsed to the detection of CRC requiring a second surgery was 120 months (range: 11–528 months), 59 months (range; 7–324 months), and 143 months (range: 23–241 months) for path_MLH1, path_MSH2, and path_MSH6 cases, respectively (Table 4).
Discussion
This study revealed the characteristics of early-stage colorectal lesions, such as AAs and pT1, for each causative MMR gene in Japan, which, to the best of our knowledge, had not been reported previously. Although many early-stage colorectal lesions could be analyzed, for comparison with previous reports, if we excluded lesions that occurred within 1 year of the initial visit, only 22 CRCs were available for analysis, which was too few to analyze for interval CRC (Online Resource 2: Table). When excluding CRCs occurring within 3 months of the initial visit, we assessed 50 lesions, approximately half of which were pT1, which could be removed endoscopically. In this study, the rates of AC detection within or beyond 2 years differed significantly.
In discussions about post-colonoscopy CRC, the latest consensus statements advocate an examination interval of ≤ 4 years [17]. However, in this study, the interval range was considered as CRCs occurring in 1–3 years, targeting LS-specific incident CRCs occurring during the CS surveillance period. The high frequency of MSI-high or MMR-deficiency among adenomas in cases with LS and the previous reports of small AAs [18,19,20], we believe that cancerous transformation of untreated AAs may also lead to interval CRCs. In this study, the frequency of AAs < 10 mm in the MLH1-, MSH2-, and MSH6-groups, treated in patients with LS, was higher than that previously reported in the general population [21]. However, no obvious morphological trends were found in patients with LS.
In terms of why a certain proportion of interval CRCs occur in LS despite strict CS surveillance, Ahadova et al. investigated MMR-deficient crypt foci and CTNNB1-mutation in detail and hypothesized that the LS-specific immediate invasive carcinogenic pathways, which are involved in the phenotype of non-polypoid lesions, are responsible, and that these cannot be detected by CS. This also supports European reports that intervals shorter than 3 years between examinations do not lead to a reduction in cancer incidence [12, 13] and points to the limitations of CS polypectomy in preventing carcinogenesis [22, 23]. In our analysis of ACs detected during the 3-year surveillance period in this study, although the number of relevant cases was small, we noted that short-interval AC progression was specific to path_MLH1 cases. Engel et al. noted variant-specific differences in the pathway of CRC development: the incidence of AAs and proportion of somatic APC mutations were lower in those with path_MLH1, although path_MLH1 and path_MSH2 were associated with similar risks of developing CRC [24]. In this study, immunohistochemistry was not performed for each lesion. In future, LS-specific lesions associated with each causative MMR gene should be investigated based on phenotype and somatic mutations. In addition, quality indicators (QI) for LS regarding easily missed non-polypoid lesions, and lesions with unclear margins in the proximal colon, have been reported [25,26,27,28,29]. The feasibility of preventive CS treatment needs to be studied prospectively using effective QI for LS-specific lesions, with the goal of reducing the incidence of AC.
In terms of stratification of surveillance by causative MMR gene, CS is recommended to commence at the age of 25 years for path_MLH1 and path_MSH2 cases, and at 35–40 years for path_MSH6 and path_PMS2 cases [30, 31]. The cumulative incidence of CRC in this study was similar to that in previous reports, with a trend towards a 10-year delay for path_MSH6 cases as compared to that for path_MLH1 and path_MSH2 cases. The high CRC penetrance rate in the present study may be related to our enrollment of many cases of pre-existing CRC, which had been the trigger for genetic examination for LS. There might be few unaffected LSs with blood relative diagnosis. Interestingly, the interval between the peaks of events by CS was 15 years for path_MLH1 and 25 years for path_MSH2 (Online Resource 1: Figure), which should be kept in mind by endoscopists. The prevalence of adenomas also increases with age, as previously reported, and enhanced surveillance tailored to the age at onset needs to be discussed [32, 33].
As more cases of LS are analyzed, stratified CS surveillance attempts should also focus on factors other than causative MMR genes, as the penetrance of these LS-causative MMR genes, in terms of CRC development, is variable [34]. Lifetime metachronous CRC is not uncommon in path_MLH1 and path_MSH2 cases, who develop cancer at a relatively young age. These individuals should be aware of the increased risk of second events at middle-age and older age, when cancer is more likely to develop. Therefore, pre-existing CRC would be another important factor for stratification. In path_MLH1and path_MSH2 cases, metachronous CRC in the residual intestine has been shown to be present in 34% and 23% of cases, and the intervals between lesion occurrence are not always short. In terms of specific locations of CRC in LS, our group reported that, when the first CRC was present in the left-side of the colon, more metachronous CRC tended to occur in the residual intestine [35]. The need for intestinal reconstruction or extended intestinal resection to facilitate CS surveillance of the residual intestine should be discussed in future. The CS surveillance period required for patients with LS diagnosed at a young age is very long; therefore, tailor-made options that consider daily life and mental quality of life should be considered during decision-making and stratification.
This study had some limitations. First, the rates of colorectal lesions and occurrence events were analyzed on a lesion-by-lesion basis and for each examination. Second, the study participants included many with residual intestine after surgical operation, and the exact location of small lesions could not be identified. Third, the QI of CS at each institution was not prospectively standardized or evaluated.
In conclusion, the analysis of Japanese CS surveillance in LS showed that many AAs and some early-stage CRCs had been treated with curative endoscopic resection. Therefore, CS surveillance intervals of at least 2 years should be maintained in cases with path_MLH1, path_MSH2, and path_MSH6, considering the detection of the colorectal lesion amenable to endoscopic treatment. path_MSH6 cases could be stratified with path_MLH1 and MSH2 cases in terms of risk of metachronous CRC and age of onset.
References
Lynch HT, Shaw MW, Magnuson CW, et al. Hereditary factors in cancer. Study of two large midwestern kindreds. Aech Arch Intern Med. 1966;117:206–12.
Idos G MS, Valle l. Lynch syndrome gene reviews. Available via DIALOG. http://www.ncbi.nlm.nih.gov/books/NBK1211/. Accessed 29 Jan 2024.
InSiGHT. Lynch syndrome. Available at https://www.insight-group.org/syndromes/lynch-syndrome/. Accessed 29 Jan 2024.
Tanakaya K. Current clinical topics of Lynch syndrome. Int J Clin Oncol. 2019;24:1013–9.
Vasen HFA, Blanco I, Aktan-Collan K, et al. Revised guidelines for the clinical management of Lynch syndrome (HNPCC): recommendations by a group of European experts. Gut. 2013;62:812–23.
Vasen HF, Abdirahman M, Brohet R, et al. One to 2-year surveillance intervals reduce risk of colorectal cancer in families with Lynch syndrome. Gastroenterology. 2010;138:2300–6.
Engel C, Rahner N, Schulmann K, et al. Efficacy of annual colonoscopic surveillance in individuals with hereditary nonpolyposis colorectal cancer. Clin Gastroenterol Hepatol. 2010;8:174–82.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: genetic/familial high-risk assessment: colorectal. Version 1. 2023. http://www.nccn.org. Accessed 29 Jan 2024.
Bonadona V, Bonaïti B, Olschwang S, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–10.
Ryan NAJ, Morris J, Green K, et al. Association of mismatch repair mutation with age at cancer onset in Lynch syndrome: implications for stratified surveillance strategies. JAMA Oncol. 2017;3:1702–6.
Møller P, Seppälä T, Bernstein I, et al. Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. Gut. 2017;66:464–72.
Engel C, Vasen HF, Seppälä T, et al. No difference in colorectal cancer incidence or stage at detection by colonoscopy among 3 countries with different Lynch syndrome surveillance policies. Gastroenterology. 2018;155:1400-9.e2.
Seppälä TT, Ahadova A, Dominguez-Valentin M, et al. Lack of association between screening interval and cancer stage in Lynch syndrome may be accounted for by over- diagnosis; a prospective Lynch syndrome database report. Hered Cancer Clin Pract. 2019;17:8.
Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298–306.
Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal, appendiceal, and anal carcinoma. J Anus Rectum Colon. 2019;18:175–95.
Brierley JD, Gospodarowicz MK, Wittekind C, et al. UICC TNM classification of malignant tumours. 8th ed. Oxford: Wiley-Blackwell; 2017. p. 272.
Matthew DR, Iisif B, Roland V, et al. World endoscopy organization consensus statements on post-colonoscopy and post-imaging colorectal cancer. Gastroenterology. 2018;155:909–25.
Iino H, Simms L, Young J, et al. DNA microsatellite instability and mismatch repair protein loss in adenomas presenting in hereditary non-polyposis colorectal cancer. Gut. 2000;47:37–42.
Sekine S, Mori T, Ogawa R, et al. Mismatch repair deficiency commonly precedes adenoma formation in Lynch syndrome-associated colorectal tumorigenesis. Mod Pathol. 2017;30:1144–51.
Hatamori H, Chino A, Arai M, et al. Malignant potential of colorectal neoplasms in Lynch syndrome: an analysis of 325 lesions endoscopically treated at a single institute. Jpn J Clin Oncol. 2021;51:737–43.
Sakamoto T, Matsuda T, Nakajima Y, et al. clinicopathological features of colorectal polyps: evaluation of the ‘predict, resect and discard’ strategies. Colorectal Dis. 2013;15:295–300.
Ahadova A, von Knebel Doeberitz MK, Bläker H, et al. CTNNB1-mutant colorectal carcinomas with immediate invasive growth: A model of interval cancers in Lynch syndrome. Fam Cancer. 2016;15:579–86.
Ahadova A, Gallon R, Gebert J, et al. Three molecular pathways model colorectal carcinogenesis in Lynch syndrome. Int J Cancer. 2018;143:139–50.
Engel C, Ahadova A, Seppälä TT, et al. Associations of pathogenic variants in MLH1, MSH2, and MSH6 with risk of colorectal adenomas and tumors and with somatic mutations in patients with Lynch syndrome. Gastroenterology. 2020;158:1326–33.
Rondagh EJA, Gulikers S, Gómez-García EB, et al. Nonpolypoid colorectal neoplasms: a challenge in endoscopic surveillance of patients with Lynch syndrome. Endoscopy. 2013;45:257–64.
Rivero-Sánchez L, Arnau-Collell C, Herrero J, et al. White-Light endoscopy is adequate for Lynch syndrome surveillance in a randomized and noninferiority study. Gastroenterology. 2020;158:895-904.e1.
Perrod G, Samaha E, Rahmi G, et al. Impact of an optimized colonoscopic screening program for patients with Lynch syndrome: 6-Year results of a specialized French network. Therap Adv Gastroenterol. 2018;11:1756284818775058.
Ahadova A, Seppälä TT, Engel C, et al. The “unnatural” history of colorectal cancer in Lynch syndrome: lessons from colonoscopy surveillance. Int J Cancer. 2021;148:800–11.
Perrod G, Rahmi G, Cellier C. Colorectal cancer screening in Lynch syndrome: indication, techniques and future perspectives. Dig Endosc. 2021;33:520–8.
Møller P, Seppälä TT, Bernstein I, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective lynch syndrome database. Gut. 2018;67:1306–16.
Møller P, Seppälä T, Bernstein I, et al. Incidence of and survival after subsequent cancers in carriers of pathogenic MMR variants with previous cancer: a report from the prospective Lynch syndrome database. Gut. 2017;66:1657–64.
Liljegren A, Barker G, Elliott F, et al. Prevalence of adenomas and hyperplastic polyps in mismatch repair mutation carriers among CAPP2 participants: report by the colorectal adenoma/carcinoma prevention program 2. J Clin Oncol. 2008;26:3434–9.
Staffa L, Echterdiek F, Nelius N, et al. Mismatch repair-deficient crypt foci in Lynch syndrome—molecular alterations and association with clinical parameters. PLoS ONE. 2015;10: e0121980.
International Mismatch Repair Consortium. Variation in the risk of colorectal cancer in families with Lynch syndrome: a retrospective cohort study. Lancet Oncol. 2021;22:1014–22.
Chikatani K, Ishida H, Mori Y, et al. Risk of metachronous colorectal cancer after colectomy for first colon cancer in Lynch syndrome: multicenter retrospective study in Japan. Int J Clinical Oncol. 2023;28:1633–40.
Acknowledgements
The authors thank Doctor Koichi Koizumi for suggesting the initiation of this multicenter study. This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
Akiko Chino, Kohji Tanakaya, Tatsuro Yamaguchi, and Naohiro Tomita contributed significantly to the conception and design of the study. Akiko Chino, Takeshi Nakajima, Kiwamu Akagi, Akinari Takao, Masayoshi Yamada, Kohji Tanakaya, Hideyuki Ishida, Koji Komori, Kazuhito Sasaki, Masashi Miguchi, Keiji Hirata, Tomoya Sudo, Yasuyuki Miyakura, and Toshiaki Ishikawa contributed to the acquisition of the clinical data and critical revision of the manuscript. Akiko Chino, Takeshi Nakajima, Kohji Tanakaya, Tatsuro Yamaguchi, and Naohiro Tomita analyzed the data. Akiko Chino interpreted the data and drafted the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest or financial ties.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chino, A., Tanakaya, K., Nakajima, T. et al. Colorectal cancer and advanced adenoma characteristics according to causative mismatch repair gene variant in Japanese colorectal surveillance for Lynch syndrome. J Gastroenterol 59, 699–708 (2024). https://doi.org/10.1007/s00535-024-02128-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-024-02128-5