Abstract
Objective
Colorectal cancer is the leading cause of cancer death in Puerto Rico and third among Hispanics in the USA. Up to 2–4% of colorectal cancer cases are a result of Lynch syndrome (LS), a hereditary cancer syndrome caused by a germline mutation in at least one of the DNA mismatch repair genes. The objective of this study was to determine the prevalence of LS in colorectal tumors during the first 15-months after the implementation of universal tumor-based screening for LS in Puerto Rico.
Methods
A total of 317 colorectal tumors were evaluated in a large private pathology laboratory from September 2014 to December 2015. Clinical characteristics were obtained from the pathology reports. Unadjusted and adjusted logistic regression models were used to estimate the magnitude of association (odds ratio [OR] with 95% confidence intervals [CI]) between absent MMR protein expression and patient characteristics.
Results
Most cases (93.4%) were analyzed by immunohistochemistry; 11.8% (35 of 296) had deficient mismatch repair protein expression. While 29 of the 317 cases were subjected to PCR-based microsatellite instability analysis of which 10.3% (3 of 317) had microsatellite instability. In total, 11.0% of the tumors were reported MMR deficient. These tumors were more likely from females and more likely localized in the proximal colon compared to those with proficient MMR expression.
Conclusions
Our data is consistent with the results from other studies including US Hispanics, where approximately 10% of Hispanic individuals with colorectal cancer have microsatellite instability. Our results support universal tumor-based screening for LS among Hispanics in accordance with National Comprehensive Cancer Network guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2020, colorectal cancer (CRC) is estimated to account for 8.2% of all newly diagnosed cancer cases in the USA [1]. In Puerto Rico (PR), a US territory, CRC is one of the most commonly diagnosed cancers and the leading cause of cancer death [2]. Approximately 5–6% of all CRC cases worldwide are due to hereditary cancer syndromes [3]. Lynch syndrome (LS) is the most common hereditary form of CRC, responsible for 2–4% of all CRC cases [4,5,6,7]. Individuals diagnosed with LS may present with family history of CRC and other cancers (e.g., endometrial, stomach, among others) [8], CRC diagnosis at a younger age, predominance of proximal location of tumors in the colon, and multiple primary tumors [9,10,11]. Patients with LS have up to 70% risk of developing CRC (depending on the gene mutated) in their lifetime, with a mean age of diagnosis from 44 to 61 years [3, 10,11,12,13].
LS is caused by loss in proficiency in at least one of the four DNA mismatch repair (MMR) proteins due to a germline mutation in the MMR genes (MLH1, MSH2, MSH6, and/or PMS2) or EpCAm [4]. The MMR pathway repairs DNA base mismatches as well as insertion/deletions loops that occur during DNA replication [14]. Tumors from LS patients exhibit an increase in the frequency of small insertions or deletions in microsatellites [15], tracts of intergenic repetitive DNA regions. This increased frequency of microsatellite insertions or deletions is called microsatellite instability (MSI), and is a hallmark of CRC tumors associated with LS [15]. Tumors with MSI have distinct features that include being more likely to arise at the proximal colon, be mucinous, have signet-ring type cell morphology, be poorly differentiated, and being more likely to be diagnosed at earlier stages when compared with microsatellite stable (MSS) tumors [16, 17].
Screening and diagnosis of LS have been driven by a set of clinical and pathological guidelines: the Amsterdam Criteria [5] and the Bethesda Guidelines [18]. These guidelines are informed by clinicopathological characteristics and family history of the patient, and primarily recommend germline genetic testing for the MMR genes. However, sensitivity for LS diagnosis using these clinical guidelines remains low, detecting 50–60% of all LS patients [18]. An alternative to this clinical-based approach was developed using tumor-based screening methods for all patients with CRC, regardless if LS guidelines were met. Universal tumor-based screening for LS for all newly diagnosed CRC patients was recommended in 2014 by the National Comprehensive Cancer Network (NCCN) and US Multi-Society Task Force on Colorectal Cancer using tumor immunohistochemistry (IHC) and/or microsatellite instability (MSI) testing [12, 19]. This approach would identify most LS cases and help identify patients at high-risk of secondary LS-associated cancers [20,21,22]. Once a LS patient has been diagnosed, cascade testing of family members may be completed allowing for early diagnosis of mutation carriers and establishment of personalized cancer surveillance and prevention algorithms. However, there have been conflicting reports regarding adherence to the universal tumor-based screening for LS guidelines. In a study evaluating the utilization of MMR deficiency testing in adults with CRC using a large, contemporary, national data set during a period of increasing endorsement of universal testing (2016–2017), only 28% of patients had tumor testing and African Americans were tested less frequently [23]. In a statewide population-based study, MSI and/or IHC was only performed in 23% of colorectal tumors [24]. However, in another study that evaluated universal tumor testing in four academic centers, 92% of colorectal tumors were analyzed for mismatch repair deficiency without significant differences among races/ethnicities, but minority patients were significantly less likely to be referred for genetic evaluation compared to non-Hispanic Whites [25].
Even though CRC is one of the leading causes of cancer deaths among Hispanics, mortality rates due to Lynch syndrome remain unknown. No significant differences in MSI and mismatch repair deficiency have been reported according to ethnicity or race, approximately 12–13% of CRC tumors among Hispanics are mismatch repair deficient [26,27,28]. Ricker et al. reports that 5.7% of Hispanics harbored mutations in the MMR genes [28]. The objective of this study was to determine the prevalence of positive LS-screening tests in CRC tumors from Puerto Rican Hispanics (PRH), determined by IHC and/or MSI testing in CRC tumors, since the implementation of the universal tumor-based LS screening guidelines [12].
Methods
Study Design and Population
A cross-sectional study aimed to estimate the prevalence of LS-positive screening tests (IHC and/or MSI analysis) using pathology reports from all CRC cases analyzed at Hato Rey Pathology Laboratories, Inc. (HRP), a high-volume private pathology laboratory in Puerto Rico, between September 2014 and December 2015. HRP serves 11 private community hospitals in PR and handles approximately 120,000 biopsies/year. The hospitals currently being serviced by HRP represent community-based practices along the San Juan Metropolitan Area, and the Southern, Northwestern, and Southeastern coasts of the island (Fig. 1). The study period selected coinciding with the first 15-month period after the NCCN and US Multi-Society Task Force on Colorectal Cancer guidelines recommended tumor universal screening for LS in all colorectal tumors, regardless of age at diagnosis [12, 19]. The pathology obtained from HRP did not have personal identifiers other than age, gender, date reported, and tumor characteristics, including tumor location and stage.
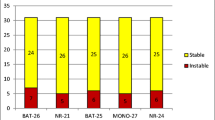
Colorectal tumors diagnosed between September 2014 and December 2015 with either DNA-based MSI testing and/or MMR protein IHC analysis in the pathology report were included in this study. A total of 317 cases were included in the study (n = 296 had IHC testing, n = 21 had MSI analysis, and n = 8 had both tests performed). Tumors were classified as MMR deficient if they had absence of any of the MMR proteins in the IHC. Tumors were classified as MSI-high if they had the presence of two or more markers or microsatellite stable (MSS) if none of the markers showed instability [29] when comparing tumor DNA with that of normal mucosa. Other tumor information, such as BRAF and KRAS oncogene mutational status, was not available from the pathology reports collected.
Data Analysis
The clinical characteristics obtained from the pathology reports were gender, age at diagnosis, and tumor location; variables were described using frequency distribution. Unadjusted and adjusted logistic regression models were used to estimate the magnitude of association (odds ratio [OR] with 95% confidence intervals [CI]) between absent MMR protein expression and patient characteristics. Statistical analyses were performed using STATA 14 (Stata Corp 2011, STATA Statistical Software: Release 12; College Station, TX: Stata Corp LP). No significant interaction terms were found in the multivariable logistic regression models evaluated (p > 0.05).
Results
Immunohistochemistry (IHC) and Microsatellite Instability (MSI) Tests
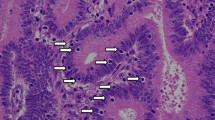
The main goal of our study was to examine the results of the implementation of universal tumor-based screening for LS in a community practice setting from September 2014 through December 2015. A total of 317 CRC cases were evaluated. The median age of the reported cases was 65.8 ± 12.1 years and the majority of tumors were localized in the distal colon/rectum (51.7%). Out of the 317 cases, 296 (93.4%) had IHC testing and 29 (9.1%) had MSI testing performed. Eight individuals had both tests performed and the results were concordant. Of the 296 cases with IHC testing, 35 (11.8%) were MMR deficient with the absence of at least one MMR protein. The majority of MMR deficient tumors (77.1%) lacked MLH1/PMS2 expression, followed by loss of both MSH2 and MSH6 proteins (14.3%). Of the 29 samples with MSI testing, 3 (10.3%) were reported to be microsatellite unstable (MSI-high). In all the tumors tested (with IHC and/or MSI), 11.0% of the tumors were reported MMR deficient (Table 1).
A comparison between MMR proficient and MMR deficient tumors is shown in Table 2. Women were more likely to have MMR deficient tumors in both the adjusted and unadjusted models (Table 2). MMR deficient tumors were also more likely to be located in the proximal colon (OR = 6.16; 95% CI 2.56–14.81) compared with MMR proficient colorectal tumors. Tumor differentiation and staging were also analyzed, but limited tumor stage information precluded completion of this analysis (data not shown).
Discussion
The identification of Lynch syndrome (LS) patients using only clinical criteria guidelines (Amsterdam I and II, and Bethesda) is suboptimal and misses a significant number of LS cases who do not fulfill those criteria [20, 21]. Thus, the NCCN, Evaluation of Genomic Applications in Practice and Prevention (EGAPP) working group, US Multi-Society Task Force (USMSTF), and the American Gastroenterology Association (AGA) have recommended that CRC cases be universally screened for LS [19, 30,31,32]. The current study reports the prevalence of LS-positive screening tests (determined by IHC and/or MSI testing in CRC tumors) since the implementation of universal tumor-based screening for LS in the largest Hispanic community-based pathology laboratory in Puerto Rico.
The prevalence of MMR deficient tumors in our Hispanic cohort was 11.0% (95% CI = 8.02–15.02%), using the combination of IHC and/or MSI testing. Previous studies have investigated the prevalence of LS-positive screening tests in a variety of populations, using IHC and/or MSI analysis [4, 5, 20, 21, 33,34,35]. In two studies by Hampel et al. evaluating 500 population-based CRC cases, the prevalence of MSI in the two cohorts studied was 19.5% and 12.8%, respectively [4, 5]. In a study comparing the LS-positive screening tests when using Bethesda Guidelines vs. universal screening (8.5% vs. 20.6%), IHC and MSI testing was shown to be a better strategy to detect possible LS cases [20]. In France, in 9.8% of 214 CRC cases, the prevalence of LS-positive screening tests using MSI analysis in a cohort of 214 CRC cases [33]. In three additional studies examining the prevalence of LS-positive universal screening tests in larger study populations, the prevalence of LS-positive screening tests ranged from 8.6 to 17% [21, 34, 35]. All of the aforementioned studies were performed in populations that are predominantly non-Hispanic Whites. Recent studies have shown that the prevalence of LS-positive screening tests in Hispanic populations is similar to non-Hispanic White populations, ranging from 12.0–13.0% [27, 28, 36]. Although not all of the abovementioned studies identify possible Lynch syndrome using both IHC and MSI, all of them support that universal tumor-based screening for LS can identify more at-risk individuals than the current clinical guidelines of Amsterdam (I and II) and Bethesda Criteria. Moreover, 11.0% of CRC cases in our study population had a positive LS screening test, which is comparable with previous studies evaluating non-hereditary CRC cohorts for LS. Thus, our data supports that the utilization of universal tumor-based screening for LS among a Hispanic population is feasible in a community-based setting, and will be helpful in the identification of patients and their at-risk family members who could benefit from genetic counseling and/or testing.
Positive LS tumor-based testing prompts further evaluation with genetic testing, as the possibility of harboring a germline mutation in one of the MMR genes is suspected. Previous studies by our group reported the prevalence of MMR protein expression loss among samples of Hispanic CRC patients in the Caribbean [37], showing that MSH2 was the most commonly lost protein among Hispanics with CRC. However, in the present study, most CRC tumors presented a combined loss of MLH1/PMS2, protein suggesting a loss of MLH1 protein. For the study by De Jesus-Monge et al. [37], cases were ascertained from a referral Academic Medical Center, while in the current investigation, cases represent a community-based cohort from an island-wide population. Thus, the observed differences in the prevalence of MMR-proteins could be due to differences in case ascertainment.
A strength in our study is that the universal tumor-based screening for LS was implemented in a community-based pathology laboratory that captures approximately 20% of all CRC patients diagnosed in PR. This pathology laboratory receives CRC tumors from eleven hospitals across the island and uses standardized pathology methods to determine MMR protein expression (IHC) and perform DNA-based MSI testing. The findings from the present study confirm previous observations reported by other groups demonstrating that universal screening for LS is feasible and that approximately 1 out of 10 CRC patients will have a positive screening test requiring referral for genetic counseling. A limitation to consider is that covariates in our study, such as family history, use of medications, and germline genetic testing, were not available, thus limiting additional analysis. In addition, cases without MMR IHC and/or MSI results were not included in this study thereby limiting comparisons with tumors that were not screened for LS. There was also limited information regarding tumor characteristics, such as tumor differentiation and staging. An important point to consider is that loss of MLH1/PMS2 protein expression is the result of either germline mutations in the MLH1 gene or PMS2 gene, or can be caused by methylation of the MLH1 gene promoter [5, 38,39,40]. Testing for BRAF gene mutations or MLH1 gene methylation should be used to confirm a possible LS diagnosis following IHC and/or MSI analysis. In our clinical setting, reflex testing for methylation or BRAF gene mutation is not done by the laboratory, and requires a medical order after clinical evaluation and counseling. Thus, the percentage of patients who have mutation-confirmed LS cannot be estimated in the present study. In addition, caution must be exercised in interpreting these results as generalizable to the CRC population of Puerto Rico, given that our study was limited to the CRC samples analyzed in one private community-based pathology laboratory in Puerto Rico and the reduced number of samples analyzed may contribute to a greater imprecision in the OR estimation.
There are conflicting reports regarding adherence to the universal colorectal tumor screening guidelines. In a large, contemporary, national data set during a period of increasing endorsement of universal testing (2016–2017), only 28% of patients had tumor testing and African Americans were tested less frequently [23]. In a statewide population-based study, MSI and/or IHC was only performed in 23% of colorectal tumors [24]. However, in another study that evaluated universal tumor testing in four academic centers, 92% of colorectal tumors were analyzed for mismatch repair deficiency without significant differences among races/ethnicities [25]. Future studies aimed at determining universal tumor-based LS screening utilization rates in Puerto Rico are warranted in order to evaluate if underutilization may be a factor that contributes to the disparities in CRC mortality observed in this Hispanic subpopulation.
Conclusions
In conclusion, our results showed that universal tumor-based screening for LS is feasible in a community-based setting, and may help identify individuals who may benefit from genetic counseling and testing. Using the algorithm presented, we can evaluate if a patient with CRC should undergo genetic counseling and testing (Fig. 2) [19]. Cases with a normal IHC test result should be considered sporadic CRC, while those with abnormal IHC or MSI results need to be tested for BRAF mutations and/or MLH1 methylation. From these cases, those without a mutation in BRAF, would then be tested for germline mutations in the MMR genes. Expanding the implementation of universal tumor-based LS testing to include additional pathology laboratories and hospitals has the potential to improve identification of LS-positive individuals in PR. However, studies examining the utilization of genetic testing for LS in PR are limited [41]. An improvement of genetic testing uptake in PR has been observed recently, in part due to educational efforts made by our group and others [42]. Universal tumor-based LS screening is a useful tool for identification of LS in CRC cases and should be incorporated as standard of care in the evaluation of all CRC patients, regardless of race/ethnicity, as recommended by national professional groups [12, 30, 43]. Implementation of health policies including coverage for universal LS screening for all CRC patients will support efforts in decreasing disparities among Hispanic minorities.
Algorithm for the classification of colorectal cancer patients after universal screening for Lynch Syndrome [19]
Availability of Data and Materials
The data obtained and analyzed on the current study is available from the corresponding author on reasonable request.
References
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Data Source: Incidence case file from the Puerto Rico Central Cancer Registry (August 21,2019).
Stoffel EM, Mangu PB, Gruber SB, Hamilton SR, Kalady MF, Lau MW, et al. Hereditary colorectal cancer syndromes: American Society of Clinical Oncology Clinical Practice Guideline endorsement of the familial risk-colorectal cancer: European Society for Medical Oncology Clinical Practice Guidelines. J Clin Oncol. 2015;33(2):209–17.
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, et al. Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J Clin Oncol. 2008;26(35):5783–8.
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, et al. Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N Engl J Med. 2005;352(18):1851–60.
Salovaara R, Loukola A, Kristo P, Kääriäinen H, Ahtola H, Eskelinen M, et al. Population-based molecular detection of hereditary nonpolyposis colorectal cancer. J Clin Oncol. 2000;18(11):2193–200.
Lynch HT, de la Chapelle A. Hereditary colorectal cancer. N Engl J Med. 2003;348(10):919–32.
Umar A, Boland CR, Terdiman JP, Syngal S, Chapelle A, Ruschoff J, et al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96(4):261–8.
Aaltonen LA, Salovaara R, Kristo P, Canzian F, Hemminki A, Peltomäki P, et al. Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med. 1998;338(21):1481–7.
Aarnio M, Mecklin JP, Aaltonen LA, Nyström-Lahti M, Järvinen HJ. Life-time risk of different cancers in hereditary non-polyposis colorectal cancer (HNPCC) syndrome. Int J Cancer. 1995;64(6):430–3.
Win AK, Young JP, Lindor NM, Tucker KM, Ahnen DJ, Young GP, et al. Colorectal and other cancer risks for carriers and noncarriers from families with a DNA mismatch repair gene mutation: a prospective cohort study. J Clin Oncol. 2012;30(9):958–64.
National Comprehensive Cancer Network. Genetics/familial high-risk assessment: colorectal. 2017 [cited 2017 08/21/17]; V2.2017:[Available from: www.nccn.org.
Stoffel E, Mukherjee B, Raymond VM, Tayob N, Kastrinos F, Sparr J, et al. Calculation of risk of colorectal and endometrial cancer among patients with Lynch syndrome. Gastroenterology. 2009;137(5):1621–7.
Hsieh P, Yamane K. DNA mismatch repair: molecular mechanism, cancer, and ageing. Mech Ageing Dev. 2008;129(7–8):391–407.
Aaltonen LA, et al. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260(5109):812–6.
Sameer AS, Nissar S, Fatima K. Mismatch repair pathway: molecules, functions, and role in colorectal carcinogenesis. Eur J Cancer Prev. 2014;23(4):246–57.
Michailidi C, Papavassiliou AG, Troungos C. DNA repair mechanisms in colorectal carcinogenesis. Curr Mol Med. 2012;12(3):237–46.
Vasen HF, Blanco I, Aktan-Collan K. Revised guidelines for the clinical management of Lynch syndrome (HNPCC): recommendations by a group of European experts. Gut. 2013.
Giardiello FM, Allen JI, Axilbund JE, Boland RC, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-society Task Force on colorectal cancer. Am J Gastroenterol. 2014;109(8):1159–79.
Morrison J, Bronner M, Leach BH, Downs-Kelly E, Goldblum JR, Liu X. Lynch syndrome screening in newly diagnosed colorectal cancer in general pathology practice: from the revised Bethesda guidelines to a universal approach. Scand J Gastroenterol. 2011;46(11):1340–8.
Perez-Carbonell L, et al. Comparison between universal molecular screening for Lynch syndrome and revised Bethesda guidelines in a large population-based cohort of patients with colorectal cancer. Gut. 2012;61(6):865–72.
Sierra I, et al. Implementation of Universal Colorectal Cancer Screening for Lynch Syndrome: A Population-Based Study. in AACR Science of Health Disparities. Fort Lauderdale: AACR; 2016.
Shaikh T, Handorf EA, Meyer JE, Hall MJ, Esnaola NF. Mismatch repair deficiency testing in patients with colorectal cancer and nonadherence to testing guidelines in young adults. JAMA Oncol. 2018;4(2):e173580.
Karlitz JJ, Hsieh MC, Liu Y, Blanton C, Schmidt B, Jessup MJ, et al. Population-based Lynch syndrome screening by microsatellite instability in patients </=50: prevalence, testing determinants, and result availability prior to colon surgery. Am J Gastroenterol. 2015;110(7):948–55.
Muller C, Lee SM, Barge W, Siddique SM, Berera S, Wideroff G, et al. Low referral rate for genetic testing in racially and ethnically diverse patients despite universal colorectal cancer screening. Clin Gastroenterol Hepatol. 2018;16(12):1911–1918.e2.
Ashktorab H, Ahuja S, Kannan L, Llor X, Ellis NA, Xicola RM, et al. A meta-analysis of MSI frequency and race in colorectal cancer. Oncotarget. 2016;7(23):34546–57.
Berera S, Koru-Sengul T, Miao F, Carrasquillo O, Nadji M, Zhang Y, et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14(8):1163–71.
Ricker CN, Hanna DL, Peng C, Nguyen NT, Stern MC, Schmit SL, et al. DNA mismatch repair deficiency and hereditary syndromes in Latino patients with colorectal cancer. Cancer. 2017;123(19):3732–43.
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58(22):5248–57.
Evaluation of Genomic Applications in, P. and G. Prevention Working, Recommendations from the EGAPP Working Group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med. 2009;11(1):35–41.
Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, et al. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110(2):223–62 quiz 263.
Rubenstein JH, et al. American Gastroenterological Association Institute Guideline on the Diagnosis and Management of Lynch Syndrome. Gastroenterology. 2015;149(3):777–82 quiz e16–7.
Julie C, et al. Identification in daily practice of patients with Lynch syndrome (hereditary non-polyposis colorectal cancer): revised Bethesda guidelines-based approach versus molecular screening. Am J Gastroenterol. 2008;103:2825–35.
Moreira L, Balaguer F, Lindor N, de la Chapelle A, Hampel H, Aaltonen LA, et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA. 2012;308(15):1555–65.
Brennan B, Hemmings CT, Clark I, Yip D, Fadia M, Taupin DR. Universal molecular screening does not effectively detect Lynch syndrome in clinical practice. Ther Adv Gastroenterol. 2017;10(4):361–71.
Gupta S, Ashfaq R, Kapur P, Afonso BB, Nguyen TPT, Ansari F, et al. Microsatellite instability among individuals of Hispanic origin with colorectal cancer. Cancer. 2010;116(21):4965–72.
De Jesus-Monge WE, et al. Mismatch repair protein expression and colorectal cancer in Hispanics from Puerto Rico. Familial Cancer. 2010;9(2):155–66.
Iacopetta B, Grieu F, Amanuel B. Microsatellite instability in colorectal cancer. Asia Pac J Clin Oncol. 2010;6(4):260–9.
Kane MF, Loda M, Gaida GM, Lipman J, Mishra R, Goldman H, et al. Methylation of the hMLH1 promoter correlates with lack of expression of hMLH1 in sporadic colon tumors and mismatch repair-defective human tumor cell lines. Cancer Res. 1997;57(5):808–11.
Lochhead P, Kuchiba A, Imamura Y, Liao X, Yamauchi M, Nishihara R, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst. 2013;105(15):1151–6.
Cruz-Correa M, Diaz-Algorri Y, Pérez-Mayoral J, Suleiman-Suleiman W, del Mar Gonzalez-Pons M, Bertrán C, et al. Clinical characterization and mutation spectrum in Caribbean Hispanic families with Lynch syndrome. Familial Cancer. 2015;14(3):415–25.
Cruz-Correa M, et al. Clinical Cancer genetics disparities among Latinos. J Genet Couns. 2017;26(3):379–86.
Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, et al. NCCN clinical practice guidelines in oncology: colon cancer. J Natl Compr Cancer Netw. 2009;7(8):778–831.
Acknowledgments
The authors would like to thank the University of Puerto Rico/MD Anderson Cancer Center Partnership’s Data and Omics Sciences Core for their support and critical reading of the manuscript.
Funding
The research reported in this publication was partially supported by the Biostatistics, Epidemiology and Bioinformatics Core (BEBiC), now Data and Omics Sciences Core (DATAOmics), of the University of Puerto Rico/MD Anderson Cancer Center Partnership for Excellence in Cancer Research under Award Grant Number CA096297/CA096300 from the National Cancer Institute (NCI), by the National Institute on Minority Health and Health Disparities (NIMHD) and the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health under Award Number U54MD007587, and by the Comprehensive Cancer Center of the UPR (a public corporation of the Government of Puerto Rico created in virtue of Law 230 of August 26, 2004 as amended). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
IS, MCC, YDA, and KR conceived the study and participated in its design. IS, JPM, KAZ, and MCC participated in the design of the study and drafted the manuscript. VA, JSP, MT, LT, MLA, VICC, and SRQ participated in the coordination of data gathering. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report. MCC is in an advisory board for EXACT Sciences and BeiGene Pharmaceutical.
Ethics Approval and Consent to Participate
The study was approved by the University of Puerto Rico Medical Sciences Campus Institutional Review Board.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sierra, I., Pérez-Mayoral, J., Rosado, K. et al. Implementation of Universal Colorectal Cancer Screening for Lynch Syndrome in Hispanics Living in Puerto Rico. J. Racial and Ethnic Health Disparities 8, 1185–1191 (2021). https://doi.org/10.1007/s40615-020-00876-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00876-7