Abstract
Thyroid tumors of uncertain malignant potential (TT-UMP) comprise an accepted subgroup of follicular-patterned thyroid tumors for which benignancy or malignancy cannot be precisely assessed. We aimed to evaluate the demographic characteristics, ultrasound (US) findings, and cytological results of patients with TT-UMP and compare these findings to a classical variant of papillary thyroid carcinoma (CV-PTC) and non-encapsulated follicular variant of PTC (NEFV-PTC) patients; we also evaluated the immunohistochemical characteristics of patients with TT-UMP. Twenty-four patients with TT-UMP, 672 with CV-PTC, and 132 with NEFV-PTC were included in the study. Mean longitudinal nodule size and median nodule volume were higher in the TT-UMP group than in the CV-PTC and NEFV-PTC groups (p < 0.001 and p < 0.001 for CV-PTC; p < 0.001 and p = 0.008 for NEFV-PTC). The presence of halo and peripheral vascularization was observed more frequently in the TT-UMP group than in the CV-PTC group (p = 0.002 and p = 0.024). Benign and follicular neoplasm/suspicious for follicular neoplasm cytological results were higher in the TT-UMP group than in the CV-PTC group (p = 0.030 and p = 0.001). US findings were similar between TT-UMP and NEFV-PTC groups (all, p > 0.05). However, none of the patients with TT-UMP were called malignant; 105 patients (31.2 %) of CV-PTC and 11 patients (9.5 %) of NEFV-PTC (infiltrative FV) were classified as malignant cytologically. Tumor size was higher in the TT-UMP group than in the CV-PTC and NEFV-PTC groups (p < 0.001 and p = 0.006). In the TT-UMP group, positive expression of HBME-1, CK-19, and Gal-3 was found in 50, 33.3, and 25 % of patients, respectively. This study demonstrated that none of the TT-UMP patients were evaluated as malignant in preoperative cytology. However, patients with TT-UMP had higher nodule and tumor sizes than CV-PTC and NEFV-PTC patients; US features were similar between NEFV-PTC and TT-UMP patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is the most common type of thyroid cancer and constitutes approximately 70–90 % of well-differentiated thyroid malignancies [1–3]. Nuclear changes consistent with PTC, which include nuclear enlargement, nuclear overlapping, nuclear clearing, nuclear grooves, and cytoplasmic pseudoinclusions, are the most reliable morphological features in the diagnosis of PTC; however, these changes can be also found in benign lesions, such as hyalinizing trabecular adenoma and Hashimoto thyroiditis [4, 5].
For decades, conventional histological evaluation has failed to categorize some encapsulated follicular thyroid tumors as benign or malignant because of their overlapping histological features [6–8]. Thyroid tumors of uncertain malignant potential (TT-UMP) are neoplasms that have been generally accepted as a group of borderline, encapsulated, follicular-patterned lesions with suspicious architectural and/or cytological features but do not fulfill the criteria for malignancy. In 2000, Williams proposed a diagnostic terminology that would better classify these lesions in thyroid pathology: well-differentiated and follicular tumors of UMP (WDT/FT-UMP), which refers to the presence of incompletely developed PTC nuclear changes or questionable capsular/vascular invasion [9].
Ultrasound (US) plays an important role in thyroid nodule evaluation. Many authors have reported ultrasonographic criteria to differentiate benign and malignant thyroid lesions, and the specific findings of PTC are well defined [10–13]. Findings that suggest PTC are as follows: a hypoechoic nodule, microcalcifications, increased central vascularity, infiltrative margins, and lesions that are higher than they are wide in the transverse plane [14].
There have been plenty of studies concerning the US features of patients with PTC [15–18]. According to our knowledge, no reports have been published to date that evaluate the preoperative US features of patients with TT-UMP. Moreover, the clinicopathological and immunohistochemical features of these patients have been evaluated in only a few studies [19–24]. In the present study, we aimed to evaluate the demographic features, preoperative thyroid functions, US findings, and fine-needle aspiration biopsy (FNAB) results of patients with TT-UMP and compare the characteristics of these patients with classical variant of PTC (CV-PTC) and non-encapsulated follicular variant of PTC (NEFV-PTC) patients. Lastly, we also aimed to determine the clinicopathological and immunohistochemical features of patients with TT-UMP.
Materials and Methods
A total of 2870 thyroidectomies were performed from January 2007 to December 2014 in our hospital. The data of 1014 patients with malignant histopathology were evaluated retrospectively. In total, 894 patients were diagnosed with PTC by histopathology. Of these PTC patients, 672 were evaluated as CV-PTC, 132 as NEFV-PTC, 38 as encapsulated FV-PTC (EFV-PTC), 17 as oncocytic PTC, 14 as tall cell PTC, 2 as diffuse sclerosing PTC, and 19 as other variants of PTC. TT-UMP was reported in 24 patients. Patients with CV-PTC, NEFV-PTC, and TT-UMP histopathology were included in the study. Patients with other variants of PTC, follicular thyroid carcinoma, medullary thyroid carcinoma, and poorly differentiated thyroid carcinoma were excluded from the study. Moreover, a prior history of head-neck radiotherapy or insufficient clinical data or histopathological reports were determined as exclusion criteria.
The demographic characteristics, preoperative thyroid functions, thyroid autoantibodies, US findings, and FNAB results of patients were recorded. All of these data were compared between TT-UMP patients and CV-PTC and NEFV-PTC patients.
Histopathological specimens of patients with TT-UMP were re-evaluated by a different experienced pathologist in a second time. All of the specimens with initial TT-UMP histopathology were classified as same finally. Accordingly, overall 24 TT-UMP patients were included to the study. The nuclear features, such as nuclei size, nuclear clearing, nuclear groove, and immunohistochemical staining patterns by using Hector Battifora Mesothelial Cell-1 (HBME-1), Cytokeratin-19 (CK-19), and Galectin-3 (Gal-3); of these, patients were examined. Local ethical committee approval was obtained in accordance with the ethical standards of the Declaration of Helsinki.
Histopathology
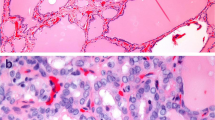
The histopathological diagnosis of PTC was based on nuclear features, such as enlarged and elongated nuclei with irregular contour, chromatin clearing with peripheral margination of chromatin, nuclear grooves, and intranuclear cytoplasmic pseudoinclusions. FV-PTC diagnosis was based on a composition entirely or almost entirely of follicules, which are lined by cells that have the nuclear features of PTC. Tumors showing questionable capsular invasion were diagnosed as FT-UMP if PTC-type nuclear changes were absent and as WDT-UMP if those nuclear changes were questionable (“incomplete”).
Immunohistochemistry
HBME-1 (1: 20, clone mouse anti-mesothelioma, Diagnostic BioSystems), CK-19 (1: 100, clone A-53B/A2.26; Thermo Scientific), and Gal-3 (1:100, mouse anti-Galectin 3 antibody; Diagnostic BioSystemsDako) antibodies were used in protein immunohistochemistry (IHC) applied to 4-μm-thick tumor sections obtained from formalin-fixed paraffin embedded blocks of resection specimens.
IHC was applied using the Benchmark GX Automated stainer (Ventana medical systems, Tuscon, AZ, US). Antigen retrieval was standardized at 37 °C for 16 min on the stainer. Positive and negative controls were used for each antibody. The following staining patterns were considered positive: HBME-1 membraneous staining along the lateral and abluminal surfaces ± cytoplasm and cytoplasm and/or membrane expression of CK-19 and Gal-3. Immunoreactivity was considered positive when at least 10 % of the tumor cells stained positively for these antibodies. The intensity of staining was further evaluated via a scoring system, as follows: “−,” “+,” “++,” or “+++” when 0–10 %, 11–40 % (patchy), 41–70 % (focal) or 71–100 % (diffuse) of the tumor cells showed positive expression, respectively.
Laboratory
Serum thyrotropin (TSH), free triiodothyronine (fT3), and free thyroxine (fT4) levels were measured within at least 3 months prior to surgery in all patients. Chemiluminescence methods (Immulite 2000, Diagnostic Products Corp., Los Angeles, CA, USA and UniCel DXI 800, Beckman Coulter, Brea, CA) were used for the measurement of serum TSH, fT3, fT4, anti-thyroid peroxidase antibody (anti-TPOAb), and anti-thyroglobulin antibody (anti-TgAb) levels. The normal ranges for TSH, fT3, fT4, anti-TPOAb, and anti-TgAb are 0.4–4 μIU/mL, 1.57–4.71 pg/mL, 0.61–1.12 ng/dl, <10 U/mL, and <30 U/mL, respectively. Thyroid antibody levels over the upper range were accepted as positive.
Ultrasonography
Esaote color Doppler US (Model 796FDII; MAG Technology Co. Ltd., Yung-Ho City, Taipei, Taiwan) and a superficial probe (Model LA523 13–4, 5.5–12.5 MHz) were used for US evaluation. Ultrasonographic evaluations were performed by an experienced endocrinologist. The parenchyma of the thyroid gland were determined to be homogenous or heterogeneous. Localization, diameter, volume, echogenicity, texture, marginal regularity, micro- and macrocalcifications, the presence of a peripheral halo, and the vascularization of nodules were recorded.
Fine Needle Aspiration Biopsy
FNAB was performed with a 27-gauge needle and a 20-ml syringe under US guidance (Logic Pro 200 GE and 7.5 MHz probe; Kyunggigo, Korea) for all nodules >1 cm and nodules ≤1 cm in diameter with at least one of the suspicious US findings. All patients gave informed consent prior to procedure. FNAB results were classified according to the Bethesda classification system and grouped as nondiagnostic, benign, atypia of undetermined significance/follicular lesion of undetermined significance (AUS/FLUS), follicular neoplasm/suspicious for follicular neoplasm (FN/SFN), suspicious for malignancy, and malignant [25, 26]. A nodule was accepted as nondiagnostic when the result was unsatisfactory in three repeated biopsies performed at different times.
Statistical Analysis
All statistical analyses were performed via the SPSS 15.0 software package (SPSS Inc., Chicago, IL, USA). Descriptive statistics for the constant variables were expressed as mean ± standard deviation or median (range), and categorical variables were noted as numerics and percent. The Chi-square test was used to investigate the difference between the groups regarding the categorical variables. The groups were compared by Student’s t test and one-way ANOVA for the parametric variables and the Mann-Whitney U test for non-parametric variables. A p value less than 0.05 was considered statistically significant.
Results
Twenty-four patients (16 females, 8 males) with TT-UMP, 672 patients (528 females, 144 males) with CV-PTC, and 132 patients (111 females, 21 males) with NEFV-PTC were enrolled in our study.
Distribution of patients according to sex and age was similar between goups (p = 0.114 and p = 0.080, respectively). There was no significant difference between the thyroid function tests of TT-UMP group and the CV-PTC and NEFV-PTC groups (p = 0.335 and p = 0.146, respectively). Hyperthyroidism was observed with a higher frequency in the CV-PTC group than the NEFV-PTC group (p = 0.002). Serum TSH, fT3, and fT4 levels were similar in the three groups (p = 0.138, p = 0.737, and p = 0.763, respectively) and there were no significant differences in anti-TPOAb and anti-TgAb positivity between the groups (p = 0.687 and p = 0.506, respectively) (Table 1).
Ultrasonographic Features
The preoperative US findings of 347 nodules with a histopathological diagnosis of CV-PTC, 119 nodules with a histopathological diagnosis of NEFV-PTC, and 24 nodules with a histopathological diagnosis of TT-UMP were recorded.
Patents in the TT-UMP group had higher mean longitudinal nodule size and median nodule volume than patients in the CV-PTC group (p < 0.001 and p < 0.001, respectively). Nodule localization, texture, echogenicity, the presence of microcalcification, and the presence of macrocalcification were similar in the TT-UMP and CV-PTC groups. The presence of halo and peripheral vascularization were observed more frequently in the TT-UMP group than the CV-PTC group (p = 0.002 and p = 0.024, respectively). The presence of an irregular margin was observed less frequently in the TT-UMP group than the CV-PTC group (p = 0.045) (Table 2).
The TT-UMP group had higher mean longitudinal nodule size and median nodule volume than the NEFV-PTC group (p < 0.001 and p = 0.008, respectively). Nodule localization, texture, echogenicity, the presence of microcalcification and macrocalcification, the presence of peripheral halo, marginal regularity, and peripheral vascularization were all similar between the TT-UMP and NEFV-PTC groups (p > 0.05, for all parameters) (Table 3).
Fine Needle Aspiration Biopsy Results
Preoperative FNAB results were present in 337 patients of the CV-PTC group, 116 patients of the NEFV-PTC group, and 23 patients of the TT-UMP group. There were no significant differences between the TT-UMP and CV-PTC groups concerning nondiagnostic, AUS/FLUS, and suspicious for malignancy cytological results (p = 1.000, p = 0.147, and p = 0.219, respectively). Benign cytology and FN/SFN were higher in the TT-UMP group than the CV-PTC group (p = 0.030 and p = 0.001, respectively); however, while malignant cytology was not present in any of the TT-UMP patients, 31.2 % patients in the CV-PTC group had malignant cytology (p = 0.003) (Table 2). The distribution of cytological results was similar in the TT-UMP and NEFV-PTC groups (p = 0.327). However, none of the patients with TT-UMP were called malignant, 11 (9.5 %) patients of NEFV-PTC (infiltrative FV) were classified as malignant in preoperative cytology (Table 3).
Clinicopathological and Immunohistochemical Characteristics of TT-UMP
Twenty-four patients with TT-UMP (21 WDT-UMP, 3 FT-UMP) were present in this study. The patients’ ages ranged from 31 to 76 years (53.62 ± 12.28 years). Females predominated, with a female to male ratio of 2/1 (16 females and 8 males). Twenty-three patients had preoperative FNAB results. The cytological results of these 23 patients were as follows: nondiagnostic in 3 patients, benign in 7 patients, AUS/FLUS in 7 patients, FN/FNS in 3 patients, and suspicious for malignancy in 3 patients. None of the patients had preoperative malignant cytology. The median tumor size was 25.0 mm (minimum 5.0 mm, maximum 80.0 mm) in the TT-UMP group and evaluated as significantly higher than that of the CV-PTC and NEFV-PTC groups (p < 0.001 and p = 0.006, respectively). However, tumor size was < 10 mm in only 3 patients (13.0 %); 20 patients (87 %) had a tumor size ≥10 mm. Tumor size was not recorded in 1 patient.
In the TT-UMP group, totally 12 (50 %) patients (3 focal, 9 patchy) had HBME-1 expression. Eight (33.3 %) patients (3 focal, 5 patchy) were positive for CK-19. Gal-3 was stained in 6 (25 %) patients (4 patchy, 2 focal).
Six patients showed the coexpression of HBME-1, CK-19, and Gal-3. Additionally, one patient was positive for both HBME-1 and CK-19. Eleven patients had no staining of HBME-1, CK-19 or Gal-3 (Table 4).
Follow-up data were available for 18 patients, with a median duration of 4 years (minimum 2 years, maximum 6 years). None of these patients developed distant metastasis during the follow-up period (Table 4).
Discussion
Thyroid nodules are frequent in the general population and are usually discovered during routine medical care. However, it is estimated that up to 7 % of the general population develops clinically palpable thyroid nodules, the widely used, new, and more sophisticated diagnostic techniques have led to the discovery of infra-clinical thyroid nodules in 20 to 76 % of the general population [27, 28]. Most thyroid nodules are benign; thyroid cancer represents only 5–24 % of thyroid nodules. PTC is by far the most common type of thyroid malignancy and is characterized by distinctive nuclear features [29].
In the great majority of cases, the pathological diagnosis of surgically removed thyroid nodules is possible. Despite all past and recent efforts, conventional pathology has failed to classify some follicular-patterned thyroid lesions as benign or malignant due to the presence of some overlapping histological features [6, 7, 29, 30]. These are considered “controversial” cases, which are generally encapsulated tumors that show no clear signs of invasion and/or have focal or questionable PTC nuclear features; these are also called TT-UMP. For tumors showing questionable capsular and/or vascular invasion, it is recommended to call them “FT-UMP” if papillary carcinoma-type nuclear changes are absent and “WDT-UMP” if these nuclear changes are imprecise [31].
The incidence of WDT-UMP has been reported as 1.1 % (30/2648 cases) in the study of Liu et al., 1.5 % (16/1078 cases) in the study of Hofman et al., and 0.5 % (5/1009 cases) in the study of Piana et al. [19, 24, 32]. In the present study, the incidences of WDT-UMP and TT-UMP were 0.7 % (21/2870 cases) and 0.8 % (24/2870 cases), respectively, similar to the rates in the literature. It has been also reported that there may be interobserver variation in the diagnosis of TT-UMP [24]. In the present study, the pathological specimens of 24 patients were re-evaluated and the diagnosis of TT-UMP was finally made after a second evaluation. Female dominance has been a striking feature in previous studies of patients with WDT-UMP [19, 21, 24, 33]. In the present study, females exceeded males in numbers (F/M = 2/1) similar to those reported in the literature.
US plays an important role in the evaluation of thyroid nodules. Among the US features, hypoechoic pattern, margin irregularity, the presence of microcalcifications, absent halo sign, solid pattern, intranodular vascularization, and shape (taller rather than wide) have been reported to be associated with an increased risk of thyroid cancer [34]. Up to date, the literature lacks data concerning the preoperative ultrasonographic features of patients with TT-UMP. In the present study, the ultrasonographic features of patients with TT-UMP were compared with the features of patients with CV-PTC or NEFV-PTC. The size of the thyroid nodule is not indicative of malignancy. Moreover, it has been reported that small nodules detected incidentally on US were associated with the same 15–25 % risk of cancer as larger nodules [35]. In our study, nodule size and nodule volume were smaller in patients with CV-PTC and NEFV-PTC than in patients with TT-UMP.
PTC shows a predominantly ill-defined, irregular margin, hypoechoic (79–90 %), mostly solid (70 %), multifocal (10–20 %), and specific microcalcifications due to psammoma bodies (40–50 %) [36, 37]. Dense calcification is seen in 10 % of all thyroid nodules [38]. Other studies, however, have also indicated that dense calcification has no diagnostic value or can even serve as an indicator for benign lesions [39]. Mixed thyroid nodules, in which the tumor contains partially solid and cystic components, account for about 15.0–53.8 % of all thyroid nodules detected via US, and 17.6 % of all cystic thyroid nodules are confirmed as malignant after thyroidectomy [40–42]. In our study, halo sign and peripheral vascularization were high and irregular margin was low in patients with TT-UMP, compared to patients with CV-PTC. Other ultrasonographic findings were similar between these two groups. Additionally, in our study, the ultrasonographic findings of patients with TT-UMP were similar to those of patients with NEFV-PTC.
In the present study, the tumor size of patients with TT-UMP ranged from 5.0 to 80 mm, and 87 % of patients had tumor size ≥10 mm. Moreover, tumor size was higher in patients with TT-UMP than patients with CV-PTC and NEFV-PTC. The tumor size of patients with TT-UMP is present in a wide range in other studies. Mean tumor size was reported as 3.1 ± 1.5 cm (range 0.8 to 7.5 cm) for TT-UMP in the study of Nechifor-Boila et al. [21]. Another study reported a mean tumor size of 3.2 cm (range 1.0 to 8.0 cm) for WDT-UMP [24].
FNAB is considered the gold standard in the diagnosis of thyroid nodules, showing a high sensitivity of 83–98 % [39, 43, 44]. However, the cytological diagnosis of thyroid lesions often results in overdiagnosis or underdiagnosis because of the overlapping features between benign and malignant thyroid lesions; diagnoses of indeterminate are common and comprise up to 20 % of all FNAB samples [45–47]. Preoperatively, most of the TT-UMP patients had benign (30.4 %) or AUS/FLUS (30.4 %) cytology and none of the patients had malignant cytology in the present study. In addition, benign and FN/SFN cytology in TT-UMP group were higher than CV-PTC group.
Although no single morphological feature is diagnostic for malignancy in thyroid lesions, a group of features has to be considered, especially the nuclear features of PTC. Nishigami et al. reported the incidence of nuclear grooves in different thyroid lesions [23]; although they did not find nuclear grooves in adenomatous goiter or follicular adenoma, they reported that the incidence of nuclear groove increased gradually from WDT-UMP (4.5 %) to PTC (6.5 %) [23]. Yassin Fel-Z found that 16 out of 18 cases (89 %) with WDT-UMP showed a characteristic incomplete thin groove with irregular distribution [20]. In the same study, the author reported that 100 % of WDT-UMP lesions had nuclear clearing [20]. Liu et al. demonstrated that the nuclear size of WDT-UMP lesions was 2–4 times that of normal thyroid follicular cells [19]. In the present study, nuclear clearing was found in 95.2 % (20/21 cases) of the WDT-UMP patients, similar to the literature, and the nuclei size was approximately 2.08 ± 0.65 times that of normal thyroid follicular cells.
Several studies demonstrated that immunohistochemistry may provide additional support in the evaluation and diagnosis of thyroid lesions. HBME-1, Gal-3, and CK-19 have been the most frequently used antibodies in thyroid pathology, although a wide range of sensibility and specificity values of these markers has been reported by different studies [48–51]. Literature data are scarce and controversial regarding the expression and possible diagnostic role of various immunohistochemical markers in TT-UMP cases [24, 33, 50]. Hofman et al. evaluated 31 cases with TT-UMP and they did not find any specific immunohistochemical and molecular genetics profiling that could be useful for detecting a low- or high-risk population of patients among the different TT-UMP subgroups [24]. Another study demonstrated a very heterogeneous immunohistochemical profile for WDT-UMP lesions [21]. Liu et al. reported that the positive frequencies of Gal-3, CK-19, and HBME-1 were 36.7, 33.3, and 40.0 %, respectively [19]; this heterogeneous immunohistochemical profile of WDT-UMP had already been stated by Papotti et al., who demonstrated positive HBME-1 expression in 9/13 WDT-UMP cases and some degree of positivity with either HBME-1 or Gal-3 in all of the cases except one [33]. In our study, positive expression of HBME-1, CK-19 and Gal-3 was found in 50, 33.3, and 25 % of our samples, respectively. However, we could not evaluate these immunohistochemical markers in PTC patients in our study.
To date, firmly established management protocols for TT-UMP do not exist due to their unknown biologic behavior; however, most of the authors recommend a conservative approach, such as lobectomy or lobectomy plus isthmectomy and clinical surveillance, for the treatment of these tumors, since they seem to have a rather benign course [32, 33, 52, 53]. Liu et al. confirmed that none of the 20 cases of WDT-UMP with follow-up data developed tumor recurrence during follow-up of, on average, 8 years [19]. Piana et al. reviewed 67 cases that died of thyroid carcinoma in a cohort of 1009 consecutive cases of thyroid carcinoma treated at a single institute in Italy with an average follow-up of 11.9 years. They found 11 TT-UMP cases in the 1009 cases, and no cancer deaths occurred among the 11 patients [32]. In another study, follow-up information was available for 21 of 29 cases with TT-UMP, with a median follow-up of 4 years, and authors reported that none of these patients had persistent disease or developed distant metastasis during the follow-up period [21]. In our study, 18 TT-UMP patients with follow-up information were evaluated, and we found that none of the patients had distant metastasis during the follow-up period. Nevertheless, further studies with more prolonged follow-up periods are needed in order to evaluate the clinical course and possible occurrence of distant metastasis.
The major limitation of our study is that we analyzed the clinical records, US findings, and cytological data of the patients retrospectively. In the literature, there have been studies of TT-UMP patients with limited numbers of cases. Similarly, only 24 patients with TT-UMP were enrolled in our study. Thereby, the other limitations of present study are the small sample size and that it did not evaluate HBME-1, CK-19, and Gal-3 expression in patients with CV-PTC and NEFV-PTC. Moreover, only 18 patients with TT-UMP had follow-up data; 6 patients with TT-UMP had no follow-up, and neither did the CV-PTC or NEFV-PTC patients. This can be accepted as the other limitation of our study.
In conclusion, the present study is the first to evaluate the preoperative US findings and FNAB results of patients with TT-UMP and compare these findings with CV-PTC and NEFV-PTC patients. This study demonstrated that both nodule and tumor size were higher in TT-UMP patients than in CV-PTC and NEFV-PTC patients. None of the TT-UMP patients had malignant cytology versus 9.5 % of NEFV-PTC and 31.2 % of CV-PTC had malignant cytology preoperatively. US findings were similar in TT-UMP and NEFV-PTC groups.
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295: 2164–2167
Rego-Iraeta A, Perez-Mendez LF, Mantinan B, Garcia-Mayor RV (2009)Time trends for thyroid cancer in northwestern Spain: true rise in the incidence of micro and larger forms of papillary thyroid carcinoma. Thyroid 19:333–340
Zhu C, Zheng T, Kilfoy BA, Han X, Ma S, Ba Y, Bai Y, Wang R, Zhu Y, Zhang Y (2009) A birth cohort analysis of the incidence of papillary thyroid cancer in the United States, 1973–2004. Thyroid 19:1061–1066
Asioli S, Erickson LA, Lloyd RV (2009) Solid cell nests in Hashimoto’s thyroiditis sharing features with papillary thyroid microcarcinoma. Endocr Pathol 20:197–203
Carney JA, Hirokawa M, Lloyd RV, Papotti M, Sebo TJ (2008) Hyalinizing trabecular tumors of the thyroid gland are almost all benign. Am J Surg Pathol 32:1877–1889
Fonseca E, Soares P, Cardoso-Oliveira M, Sobrinho-Simões M (2006) Diagnostic criteria in well-differentiated thyroid carcinomas. Endocr Pathol 17:109–117
Rosai J (2005) Handling of thyroid follicular patterned lesions. Endocr Pathol 16:279–283
Rosai J, Kuhn E, Cargangiu ML (2006) Pitfalls in thyroid tumour pathology. Histopathology 49:107–120
Williams ED (2000) Guest Editorial: Two proposals regarding the terminology of thyroid tumors. Int J Surg Pathol 8:181–183
Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, Kim J, Kim HS, Byun JS, Lee DH; Thyroid Study Group, Korean Society of Neuro- and Head and Neck Radiology (2008) Benign and malignant thyroid nodules: US differentiation-multicenter retrospective study. Radiology 247:762–770
Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, Panunzi C, Rinaldi R, Toscano V, Pacella CM (2002) Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab 87:1941– 1946
Shimura H, Haraguchi K, Hiejima Y, Fukunari N, Fujimoto Y, Katagiri M, Koyanagi N, Kurita T, Miyakawa M, Miyamoto Y, Suzuki N, Suzuki S, Kanbe M, Kato Y, Murakami T, Tohno E, Tsunoda-Shimizu H, Yamada K, Ueno E, Kobayashi K, Kobayashi T, Yokozawa T, Kitaoka M (2005) Distinct diagnostic criteria for ultrasonographic examination of papillary thyroid carcinoma: a multicenter study. Thyroid 15:251–258
Tae HJ, Lim DJ, Baek KH, Park WC, Lee YS, Choi JE, Lee JM, Kang MI, Cha BY, Son HY, Lee KW, Kang SK (2007) Diagnostic value of ultrasonography to distinguish between benign and malignant lesions in the management of thyroid nodules. Thyroid 17:461–466
NCCN.ORG. NCCN clinical practice guidelines in oncology (NCCN guidelinesTM) thyroid carcinoma version 1; 2011.
Nam SY, Shin JH, Han BK, Ko EY, Ko ES, Hahn SY, Chung JH (2013) Preoperative ultrasonographic features of papillary thyroid carcinoma predict biological behavior. J Clin Endocrinol Metab 98:1476–1482
Yoon JH, Kwon HJ, Kim EK, Moon HJ, Kwak JY (2015) The follicular variant of papillary thyroid carcinoma: characteristics of preoperative ultrasonography and cytology. Ultrasonography doi: 10.14366/usg.15037
Kim JY, Kim EK, Lee HS, Kwak JK (2014) Conventional papillary thyroid carcinoma: effects of cystic changes visible on ultrasonography on disease prognosis. Ultrasonography 33:291–297
Ohmori N, Miyakawa M, Ohmori K, Takano K (2007) Ultrasonographic findings of papillary thyroid carcinoma with Hashimoto's thyroiditis. Intern Med 46:547–550
Liu Z, Zhou G, Nakamura M, Koike E, Li Y, Ozaki T, Mori I, Tanuguchi E, Kakudo K (2011) Encapsulated follicular thyroid tumor with equivocal nuclear changes, so-called well-differentiated tumor of uncertain malignant potential: a morphological, immunohistochemical, and molecular appraisal. Cancer Sci 102:288–294
Yassin Fel-Z (2015) Diagnostic criteria of well differentiated thyroid tumor of uncertain malignant potential; a histomorphological and immunohistochemical appraisal. J Egypt Natl Canc Inst 27:59–67
Nechifor-Boila A, Borda A, Sassolas G, Hafdi-Nejjari Z, Cătană R, Borson-Chazot F, Berger N, Decaussin-Petrucci M (2015) Thyroid tumors of uncertain malignant potential: morphologic and imunohistochemical analysis of 29 cases. Pathol Res Pract 211:320–325
Nechifor-Boila A, Cătană R, Loghin A, Radu TG, Borda A (2014) Diagnostic value of HBME-1, CD56, Galectin-3 and Cytokeratin-19 in papillary thyroid carcinomas and thyroid tumors of uncertain malignant potential. Rom J Morphol Embryol 55:49–56
Nighigami K, Liu Z, Taniguchi E, Koike E, Ozaki T, Mori I, Kakudo K (2012) Cytological - features of well-differentiated tumors of uncertain malignant potential: Indeterminate cytology and WDT-UMP. Endocr J 59:483–487
Hofman V, Lassalle S, Bonnetaud C, Butori C, Loubatier C, Ilie M, Bordone O, Brest P, Guevara N, Santini J, Franc B, Hofman P (2009) Thyroid tumours of uncertain malignant potential: frequency and diagnostic reproducibility. Virchows Arch 455: 21–33
Jo VY, Stelow EB, Dustin SM, Hanley KZ (2010) Malignancy risk for fine-needle aspiration of thyroid lesions according to the Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol 134:450–456
Cibas ES, Ali SZ (2009) The Bethesda System for Reporting Thyroid Cytopathology. Thyroid 19:1159–1165
Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, Vitti P; AACE/AME/ETA Task Force on Thyroid Nodules (2010) American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract 16:1–43
Rosen JE, Stone MD (2006) Contemporary diagnostic approach to the thyroid nodule. J Surg Oncol 94:649–661
DeLellis RA, Williams ED (2004) Pathology of the thyroid and parathyroid. In: DeLellis RA, Lloyd RV, Heitz PU, Eng C (Eds), Pathology and genetics of tumours of endocrine organs, World Health Organization Classification of Tumours, IARC Press, Lyon, pp. 57–66
Kakudo K, Bai Y, Liu Z, Li Y, Ito Y, Ozaki T (2012) Classification of thyroid follicular cell tumors: with special reference to borderline lesions. Endocr J 59:1–12
De Lellis RA, Lloyd RV, Heitz PU (2004) Pathology and genetics: tumours and endocrine organs, 3rd edn. WHO, Geneva
Piana S, Frasoldai A, Di Felice E, Gardini G, Tallini G, Rosai J (2010) Encapsulated well-differentiated follicular-patterned thyroid carcinoma do not play a significant role in the fatality rate from thyroid carcinoma. Am J Surg Pathol 34:868–872
Papotti M, Rodriguez J, De Pompa R, Bartolazzi A, Rosai J (2005) Galectin-3 and HBME-1 expression in well-differentiated thyroid tumors with follicular architecture of uncertain malignant potential. Mod Pathol 18:541–546
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN (2006) Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Ultrasound Q 22:231–238
Nam-Goong IS, Kim HY, Gong G, Lee HK, Hong SJ, Kim WB, Shong YK (2004) Ultrasonography-guided fine-needleaspiration of thyroid incidentaloma: correlation with pathological findings. Clinical Endocrinology (Oxf) 60:21–28
Yousem DM, Scheff AM (1996) Thyroid and parathyroid. In: Head and Neck Imaging, Som DM, Curtin HD, Eds. 3rd ed. Mosby, St Louis, 952–975
LiVolsi VA (1997) Pathology of thryroid disease. In: Thyroid Disease: Endocrinology, Surgery, Nuclear Medicine and Radiology, Falk SA, Eds. Lippincott-Raven, Philadelphia, 65–104
Takashima S, Fukuda H, Nomura N, Kishimoto H, Kim T, Kobayashi T (1995) Thyroid nodules: re-evaluation with ultrasound. J Clin Ultrasoud 23:179–184
Kim EK, Parl CS, Chung WY, Oh KK, Kim DI, Lee JT, Yoo HS (2002) New sonographic criteria for recommends fine-needle aspiration biopsy of nonpalpable solid nodule of the thyroid. A JR Am J Roentgenol 178:617–691
de los Santos ET, Keyhani-Rofagha S, Cunningham JJ, Mazzaferri EL (1990) Cystic thyroid nodules. The dilemma of malignant lesions. Arch Intern Med 150:1422–1427
Frates MC, Benson CB, Doubilet PM, Kunreuther E, Contreras M, Cibas ES, Orcut J, Jr Moore FD, Larsen PR, Marqusee E, Alexander EK (2006) Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 91:3411–3417
Bellantone R, Lombardi CP, Raffaelli M, Traini E, De Crea C, Rossi ED, Fadda G (2004) Management of cystic or predominantly cystic thyroid nodules: the role of ultrasound-guided fine-needle aspiration biopsy. Thyroid 14:43–47
Lin HW, Bhattacharyya N (2010) Clinical behavior of follicular variant of papillary thyroid carcinoma: presentation and survival. Laryngoscope 120:712–716
Rivera M, Ricarte-Filho J, Knauf J, Shaha A, Tuttle M, Fagin JA, Ghossein RA (2010) Molecular genotyping of papillary thyroid carcinoma follicular variant according to its histological subtypes (encapsulated vs infiltrative) reveals distinct BRAF and RAS mutation patterns. Mod Pathol 23:1191–1200
Ylagan LR, Farkas T, Dehner LP (2004) Fine needle aspiration of the thyroid: a cytohistologic correlation and study of discrepant cases. Thyroid 14:35–41
Baloch ZW, Gupta PK, Yu GH, Sack MJ, LiVolsi VA (1999) Follicular variant of papillary carcinoma. Cytologic and histologic correlation. Am J Clin Pathol 111:216–222
Wu HH, Jones JN, Grzybicki DM, Elsheikh TM (2003) Sensitive cytologic criteria for the identification of follicular variant of papillary thyroid carcinoma in fine needle aspiration biopsy. Diagn Cytopathol 29:262–266
Barroeta JE, Baloch ZW, Lal P, Pasha TL, Zhang PJ, LiVolsi VA (2006) Diagnostic value of differential expression of CK19, Galectin-3, HBME-1, ERK, RET, and p16 in benign and malignant follicular-derived lesions of the thyroid: an immunohistochemical tissue microarray analysis. Endocr Pathol 17: 225–234
Barut F, Onak Kandemir N, Bektas S, Bahadir B, Keser S, Ozdamar SO (2010) Universal markers of thyroid malignancies: galectin-3, HBME-1, and cytokeratin-19. Endocr Pathol 21: 80–89
Scognamiglio T, Hyjek E, Kao J, Chen YT (2006) Diagnostic usefulness of HBME1, galectin-3, CK19, and CITED1 and evaluation of their expression in encapsulated lesions with questionable features of papillary thyroid carcinoma. Am J Clin Pathol 126:700–708
Nechifor-Boila A, Borda A, Sassolas G, Hafdi-Nejjari Z, Borson-Chazot F, Lifante JC, Sturm N, Lavérriere MH, Berger N, Decaussin-Petrucci M (2013) Immunohistochemical markers in the diagnosis of papillary thyroid carcinomas: The promising role of combined immunostaining using HBME-1 and CD56. Pathol Res Pract 209:585–592
Sobrinho-Simões M, Eloy C, Magalhães J, Lobo C, Amaro T (2011) Follicular thyroidcarcinoma. Mod Pathol 24:S10–S18
Widder S, Guggisberg K, Khalil M, Pasieka JL (2008) A pathologic re-review of follicular thyroid neoplasms: the impact of changing the threshold for the diagnosis of the follicular variant of papillary thyroid carcinoma, Surgery 144:80–85
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Local ethical committee approval was obtained in accordance with the ethical standards of the Declaration of Helsinki.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Baser, H., Topaloglu, O., Tam, A.A. et al. Comparing Clinicopathologic and Radiographic Findings Between TT-UMP, Classical, and Non-Encapsulated Follicular Variants of Papillary Thyroid Carcinomas. Endocr Pathol 27, 233–242 (2016). https://doi.org/10.1007/s12022-016-9437-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-016-9437-4