Abstract
Background and aim
A close relationship between adiposity and increased cortisol levels is well established in patients with endogenous hypercortisolism. Nevertheless, hypothalamic-pituitary-adrenal (HPA) axis regulation in overweight subjects is still a matter of concern. We studied free cortisol (urinary free cortisol, UFC and late night salivary cortisol, LNSC), pituitary feedback (serum cortisol after 1 mg dexamethasone suppression test, 1 mg DST) and peripheral cortisol metabolism (urinary cortisol to cortisone ratio, F/Eratio) in a large series of overweight subjects without Cushing’s Syndrome.
Materials and methods
We considered 234 patients divided in 5 BMI classes, matched for age and gender (BMI ≤ 25 kg/m2n = 38; 25–30 n = 58; 30–35 n = 52; 35–40 n = 52; >40 n = 34). UFC, LNSC and urinary F/Eratio were assessed with LC-MS.
Results
We collected 183 LNSC, 176 UFC, 152 1 mg DST and 64 F/Eratio tests. UFC levels were higher in lean subjects, and they decreased according to the BMI classes (p = 0.022). Non-suppressed cortisol levels (>50 nmol/L) after 1 mg DST were observed especially in patients with normal weight or mild obesity. Patients with BMI ≥ 35 kg/m2 revealed a reduced F/Eratio (0.39 vs. 0.61, p = 0.006). The specificity of tests (false positive results) was higher considering 1 mg DST or UFC in obese patients, on the contrary impaired cortisol rhythm (LNSC above normality) was observed in 47 subjects, irrespective of weight.
Conclusions
Overweight and obese subjects are characterised by an original regulation of HPA axis (reduced UFC levels, increased suppression after 1 mg DST) and peripheral cortisol metabolism (reduced F/Eratio), suggesting an effort to counteract hypercortisolism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been clearly demonstrated that cortisol excess leads to anabolic effects regarding accumulation of fat in adipocytes and weight gain in animal models [1]. Impaired cortisol rhythm (increased levels in the second part of the day) contribute to metabolic consequences such as impaired glucose metabolism [2]: the human model of cortisol excess (Cushing’s Syndrome, CS) presents abdominal obesity as one of its peculiar clinical features [3]. In such patients, the recovery of hypothalamic-pituitary-adrenal (HPA) axis is able to restore a normal fat distribution [4]. Contrariwise, literature data are inconsistent in terms of how HPA axis is dysregulated in overweight or obese patients.
Total daily cortisol secretion could be used to assess the integrity of HPA axis: the 24 h urinary free cortisol (UFC) excretion represents the amount of free cortisol, unbound to proteins [5]. Elevated UFC levels are one of the hallmarks of CS [6, 7], nevertheless contradictory data are reported in literature regarding UFC levels in obese subjects. Some authors described an elevation of UFC as well as an increased excretion of steroid metabolites [8,9,10]; on the contrary, other papers reported that UFC is reduced in patients with abdominal fat distribution [11].
Dexamethasone Suppression Test (DST) is used as a screening test in patients with suspected hypercortisolism or adrenal incidentaloma [12, 13]. It explores the negative HPA axis feedback after the administration of a potent synthetic glucocorticoid drug, as dexamethasone: serum cortisol <50 nmol/L is considered an adequate suppression, sufficient to confirm a preserved cortisol feedback. Therefore, a sub-optimal cortisol suppression indicates a reduced feedback sensitivity to glucocorticoids. Contradictory data are reported: some authors described a reduced inhibition of the HPA axis after DST in obese subjects [14], and others reported that serum cortisol after DST did not differ among normal and overweight patients [8], especially in males [15].
Salivary cortisol is increasingly used tool to asses adrenal-related disorders [16]. The impairment of circadian cortisol rhythm is a peculiar marker of CS, and salivary sampling is non-invasive, stress-free and easy-to-collect for outpatients [6, 17, 18]. When considering obese subjects without CS, several authors have previously reported the abnormal increase of late night salivary cortisol (LNSC) [19,20,21].
Outside secretion of HPA axis, peripheral cortisol metabolism in adipocyte cells plays a crucial role too. The balance of cortisol (F, active metabolite) and cortisone (E, inactive steroid) regulates the glucocorticoid receptor activity in fat cells [1]. The enzymes involved are the two forms of 11β-hydroxysteroid-dehydrogenase (11β-HSD) types 1 and 2 :11β-HSD-1 catalyses the intracellular regeneration of F from E, and 11β-HSD2 inactivate F to E [22, 23]. Several animal and human studies suggest that an imbalance between 11β-HSDs in adipose tissue can lead to a local hypercortisolism, thus promoting visceral obesity and metabolic syndrome [1, 24].
We studied free cortisol levels (with UFC and LNSC), glucocorticoid sensitivity of HPA axis (with serum cortisol after 1 mg DST) and cortisol metabolism (with urinary F/Eratio) in a large series of overweigh and obese subjects.
Materials and methods
Patients
We enroled 260 consecutive patients, evaluated in the Endocrine Unit of Padova for weight gain (at least 10% compared with the weight referred in the previous 6 months) or increased Body Mass Index (BMI ≥ 25 kg/m2). Inclusion criteria were suppressed serum cortisol (<50 nmol/L) after 1 mg DST, normal UFC or LNSC levels. In case of cortisol after 1 mg DST 50–138 nmol/L and UFC or LNSC below 2 times Upper Limit of Normality (ULN), pseudo-CS and overt CS were ruled out by repeating screening tests or considering dynamic HPA axis evaluation (with dexamethasone-CRH or desmopressin test), as well as with dedicated imaging, according to Endocrine Society’s Guidelines for CS [12] or Expert Opinion for pseudo-CS [25, 26]. Exclusion criteria were overt hypercortisolism (serum cortisol >138 nmol/L after 1 mg DST, UFC or LNSC > 2 ULN in two consecutive collections) irrespective of being it overt-CS or pseudo-CS; use of glucocorticoid, antiepileptic or estro-progestinic drugs; pregnancy; active malignancy; positive history for adrenal incidentaloma, liver or renal failure. Finally, we considered 234 patients.
Wearing light clothing and no shoes, participants were weighed and measured using a balanced beam scale and a vertical ruler. Weight was recorded to the nearest 0.5 kg and height to the nearest 0.5 cm. BMI was calculated in all subjects (weight divided by height squared, kg/m2). Waist circumference was measured at the end of natural breaths, at the midpoint between the top of the iliac crest and the lower margin of the last palpable rib. We considered five groups according to BMI classes proposed by the World Health Organization [27]:
-
Group 1: BMI ≤ 25 kg/m2, 38 cases, 29 female;
-
Group 2: 25 < BMI ≤ 30 kg/m2, 58 cases, 40 female;
-
Group 3: 30 < BMI ≤ 35 kg/m2, 52 cases, 44 female;
-
Group 4: 35 < BMI ≤ 40 kg/m2, 52 cases, 49 female;
-
Group 5: BMI ≥ 40 kg/m2, 34 cases, 28 female;
One of the major issue concerning first-line screening tests for suspected CS is their adequate home collection (for urine and saliva), as well as proper dexamethasone intake, therefore all the protocols were described to the patients in a written step-by-step instruction form, to ensure a correct home sampling. For 24 h urine collections, patients were instructed to discard the first morning urine void and to collect all urine for the next 24 h, so that the morning urine void on the second day was the final collection. Appropriate urinary volume was carefully recorded (collection was discarded in case of incomplete collection or large urinary volume), then a sample was collected and kept refrigerated until UFC measurement with a liquid chromatography tandem-mass spectrometry (LC-MS/MS) method previously described [28], considering ULN of 168 nmol/24 h. The same method was used to measure urinary free cortisone (to calculate F/Eratio). Salivary cortisol, to measure LNSC, was collected before sleeping: patients were advised to soak for two or three minutes the absorbent cotton of a Salivette® device (Sarstedt, Numbrecht, Germany). To avoid any contamination, saliva samples were collected at least 2 h after taking a meal/drink, all participants brushed their teeth after saliva collection, moreover they did not smoke or eat licorice in the day of saliva collections [29]. Salivary cortisol was measured with the LC-MS/MS method previously reported, considering ULN of 2.6 nmol/L for LNSC [18]. The 1 mg DST was performed as recommended in the Endocrine Society guidelines [12]: 1 mg of dexamethasone was assumed per os at late night (between 23.00 and 24.00), a blood sample for serum cortisol was collected the next morning before 9.00. Serum cortisol was measured with a commercial chemiluminescence immunoassay (Immulite 2000; Diagnostic Products Co), a sufficient serum dexamethasone was achieved in all cases [30].
In order to avoid selection bias, none of the subjects enroled were used as controls in previous published study.
The study was performed in accordance with the guidelines in the Declaration of Helsinki, it was approved by the Ethics Committee of Padova University-Hospital, and all patients gave informed consent.
Data are presented as mean and standard deviation. Groups were compared by chi-square test for categorical variables and by the Student’s T test test for quantitative variables; Bonferroni correction was used to adjust multiple comparisons. Linear regression and one-way multivariate analysis of variance (one-way MANOVA) were used to study the relationship between quantitative variables. The database was managed and statistical analysis performed by SPSS 24 software package for Windows (2016, IBM-SPSS, Armonk, New York, USA). The significance level was set at a p value < 0.05 for all the tests.
Results
The five groups are similar for age (all p between 0.139 and 0.998); gender distribution is similar according to BMI classification (as reported in Table 1), however female patients are prevalent in each different BMI category (from 69 to 94%, p = 0.014).
We collect 176 UFC, 183 LNSC and 152 1 mg DST tests (97 patients performed all 3 tests). Mean UFC and F/Eratio levels are lower in female: respectively 72 ± 51 nmol/24 h vs. 95 ± 66 nmol/24 h (p = 0.039) and 0.49 ± 0.29 vs. 0.76 ± 0.69 (p = 0.045). The other clinical data, biochemical parameters of HPA axis and cortisol metabolism are similar considering gender.
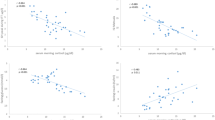
As reported in Table 1, serum cortisol levels after 1 mg DST are more suppressed in patients with severe obesity (BMI ≥ 40 kg/m2) than in lean subjects (BMI ≤ 25 kg/m2, 23 vs. 32 nmol/L, p = 0.038). Considering serum cortisol after 1 mg DST inadequately suppressed if >50 nmol/L, 24% of lean subjects do not present a preserved pituitary feedback to dexamethasone. On the other hand, an adequate suppression is observed especially in obese patients (p = 0.016, as reported in Fig. 1). Considering 35 kg/m2 as a cut-off of morbid obesity, serum cortisol levels after 1 mg DST are lower in obese patients (24 ± 1 vs. 29 ± 17 nmol/L, p = 0.048).
UFC levels in patients with severe obesity are lower than in overweight and lean subjects (56 nmol/24 vs. respectively 94 and 92 nmol/24 h, p = 0.026 and p = 0.038). We observe a trend to decrease in UFC levels according to the BMI class, especially among lean and obese subjects (ANOVA p = 0.018). As depicted in Fig. 2, UFC values decrease with increasing BMI (y = −1.2632x + 118.02; R = 0.173; p = 0.022) in the whole cohort, especially in male (R = 0.323, p = 0.046) with a non-significant trend in female (R = 0.112, p = 0.182). UFC levels are higher in patients with BMI < 35 kg/m2 (108 vs. 68 nmol/24 h, p = 0.039), on the contrary F/Eratio is lower in patients with BMI ≥ 35 kg/m2 (0.39 ± 0.16 vs. 0.61 ± 0.45, p = 0.006, as indicated in Fig. 3). F/Eratio reduces with increasing waist circumference (R = 0.338, p = 0.049). Considering gender, UFC levels are lower in male patients with BMI ≥ 35 kg/m2 (60 ± 35 vs. 105 ± 69 nmol/24 h, p = 0.033). Other parameters (LNSC, DST and ACTH levels), are similar.
In multivariate analyses, first-line screening tests (cortisol after 1 mg DST, LNSC and UFC) are different in obese patients (Wilk’s Λ = 0.791, partial η2 = 0.075, p = 0.043). Including age, it was close to a significant result (Wilk’s Λ = 0.763, partial η2 = 0.065, p = 0.074), however considering gender and BMI category the difference was preserved for cortisol after 1 mg DST (partial η2 = 0.15, p = 0.035).
False positive results are reassumed in Table 2. Overall, 11 patients present with unsuppressed serum cortisol levels (50–138 nmol/L) after 1 mg DST: UFC or LNSC levels are <ULN in 9 out of 11 cases, in one we observe impaired LNSC (4.6 nmol/L, not confirmed in a repeated saliva collection) and increased UFC in another one (177 nmol/24 h, resulted normal in 2 further urine collections). Increased UFC levels are observed in 13 cases: 10 presented adequate cortisol suppression after 1 mg DST and 9 normal LNSC levels. Impaired cortisol rhythm is the more prevalent false positive results in the whole cohort of subjects (23%: cortisol suppression after DST or UFC were normal in all patients, respectively in 35 and in 30 subjects).
Discussion
Weight gain is a common clinical feature in overt hypercortisolism [3, 12]; however, the impairment of HPA axis in obese subjects has yet to be defined. The aims of our study are to assess the HPA axis regulation in obese subjects during basal (free cortisol secretion and rhythm, respectively with UFC and LNSC) and dynamic conditions (the cortisol response to 1 mg DST), considering also peripheral metabolism in adipose tissue (assessed with F/Eratio).
We observe a reduced cortisol suppression after 1 mg DST in normal weight or overweight patients; on the contrary, an increased suppression in obese patients is confirmed with multivariate analyses, also considering BMI and gender. The specificity of 1 mg DST to diagnose CS in high-risk population, as obese patients, is well established [31, 32]; however, at the best of our knowledge this is the first study that report different cortisol feedback throughout the weight spectrum. Assuming that there are no reasons for a different absorption of the drug in the distinct weight groups, it is reasonable to speculate a reduced clearance of dexamethasone. It has been reported a different distribution of vitamin D (a lipophilic steroid-like compound) in obesity, suggesting a dilution of vitamin D3 in body tissues (in fat cell mass as well as in extracellular fluid), explaining the different response after its supplementation [33]. Dexamethasone, a lipophilic steroid drug characterised by a high distribution volume in fat tissue, could present different pharmacokinetic in patients with a larger body volume, as described with vitamin D [34]. In obesity, we could therefore speculate an increased serum half-life leading to the great HPA axis suppression observed in patients with abdominal adiposity. Another possible explanation can be an increased central (in the hypothalamus or in the pituitary) glucocorticoid sensitivity in obese subjects. This option can be due to the up-regulation of glucocorticoid receptors in a setting of chronic mild increase of local cortisol levels in visceral obesity. On the contrary, it has been recently described that higher unsuppressed serum cortisol level after 1 mg DST may be predictive for cortisol-related comorbidities (as diabetes mellitus and hypertension) in the obese population [35]. To conclude, contrasting data are reported in literature [1, 8, 10, 15, 19], therefore further studies, ideally longitudinal, are needed.
In our cohort, UFC levels decreased as the BMI category increased. As per inclusion criteria, only patients with normal or only mild excessive cortisol secretion were recruited, after excluding an overt hypercortisolism. Data in literature are scarce and discordant: in 2007 Pecori Giraldi et al. reported a weak inverse relationship between BMI and UFC levels [31], although the population included all patients with suspected hypercortisolism (with hypertension, diabetes, osteoporosis, depression and so on), however we select only subjects referred for weight gain. Reduced UFC levels observed in our cohort of obese subjects could be justified by the larger volume of distribution or by an increased clearance of cortisol [10], which has already been observed also with isotope tracers [36]. Moreover, a longitudinal study reported a weak decrease of serum cortisol levels according to BMI, describing also an increase in BMI following a rise in cortisol after 6 years [37].
In humans, several studies have been performed to check the 11β-HSDs activity in visceral adiposity, leading to controversial conclusions [38]. Our experience agrees with some previously reported results [8, 10], assuming that in obese patients there is a dysregulation of the 11β-HSD type 1 and type 2, with a new set point of F–E interconversion, leading to reduced F levels. This observation could be due to a reduced E activation to F or to an increased conversion of F to inactive E. We observe not only a reduced F (UFC) levels in obesity, but also a lower F/Eratio, secondary therefore to increased E levels, in patients with visceral adiposity. The reason for a change in set point could be due to a paracrine self-regulation of adipose tissue with the involvement of the 11β-HSD type 1 (expressed in the liver and in fat tissue) and type 2 (expressed in the kidney) activity in cross-talk with the glucocorticoid receptor. In adipose cells, 11β-HSD type 1 activity is impaired, leading to increase local F levels [10], raising new questions regarding its role in the pathogenesis of insulin resistance and increased waist [8]. Data from other studies do not confirm a different F/Eratio and therefore a direct involvement of the 11β-HSD type 2, nevertheless they can be limited by the smaller sample compared with our population (Stewart: 36 subjects, 24 obese [8], Woods: 21 obese cases [39]). Recently, Chiodini et al. reported, in a large series of postmenopausal women with normal cortisol secretion, the progressive increase of the number of possible cortisol-related consequences with F/Eratio; nevertheless, they did considered severe obesity as an exclusion criteria [40]. As previously described, the study of HPA axis in obesity could also be influenced by different functional glucocorticoid receptors with distinct sensitivity of the feedback regulation [14].
We observe the higher number of false positive results with LNSC. A meta-analyses study described similar diagnostic accuracy among screening tests for CS [6]; however, it has already been proposed a subtle impaired cortisol rhythm in obese subjects, thus limiting its final specificity in this peculiar clinical setting [21, 41, 42]. An abnormal cortisol rhythm could be related to a real cortisol excess, but also to the collection of saliva. It is reasonable to suggest that LNSC sampling must be repeated at least twice, with the attempt to reduce the collection biases and the false positives. Further studies are needed to establish if an impaired cortisol rhythm could explain the continuum among cortisol-related symptoms and overt CS. On the other hand, an adequate suppression of serum cortisol or a normal urinary cortisol excretion (in an obese subject) suggests a low likelihood of being an endogenous hypercortisolism.
Besides strengths, our work presents several limitations. First, its cross-sectional design, without a follow-up according to weight loss. Second, HPA axis was not assessed in a schematic study, therefore all tests were not performed in all subjects. Furthermore, we did not routinely measure urinary creatinine, considering that an appropriate urine collection according to our selection criteria is reliable for UFC measurement. Finally, other cortisol-related comorbidities (as hypertension, diabetes mellitus, depression, osteoporosis or vertebral fractures) were not systematically considered in our cohort.
To conclude, a new regulation of HPA axis is observed in obese subjects. We could speculate that the lower UFC levels, combined with reduced F/Eratio, reflect an attempt to counteract the detrimental effects of increased cortisol levels in the adipose tissue. In such scenario, also the increased feedback to glucocorticoids in obese subjects (the suppressed cortisol levels after DST) could confirm this hypothesis.
Data availability
Data are available on request due to local (academic) restrictions.
References
A.C. Incollingo Rodriguez, E.S. Epel, M.L. White, E.C. Standen, J.R. Seckl, A.J. Tomiyama, Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: a systematic review. Psychoneuroendocrinology. 62, 301–318 (2015). https://doi.org/10.1016/j.psyneuen.2015.08.014
L. Plat, R. Leproult, M. L’Hermite-Baleriaux et al. Metabolic effects of short-term elevations of plasma cortisol are more pronounced in the evening than in the morning 1. J. Clin. Endocrino.l Metab. 84(9), 3082–3092 (1999). https://doi.org/10.1210/jcem.84.9.5978
M. Boscaro, G. Arnaldi, Approach to the patient with possible cushing’s syndrome. J. Clin. Endocrinol. Metab. 94(9), 3121–3131 (2009). https://doi.org/10.1210/jc.2009-0612
F. Ceccato, M. Boccato, M. Zilio et al. Body composition is different after surgical or pharmacological remission of cushing’s syndrome: a prospective DXA study. Horm. Metab. Res. 49(9) (2017). https://doi.org/10.1055/s-0043-115008
K.I. Alexandraki, A.B. Grossman, Is urinary free cortisol of value in the diagnosis of Cushing’s syndrome? Curr. Opin. Endocrinol. Diabetes Obes. 18(4), 259–263 (2011). https://doi.org/10.1097/MED.0b013e3283487193
M.B. Elamin, M.H. Murad, R. Mullan et al. Accuracy of diagnostic tests for cushing’s syndrome: a systematic review and metaanalyses. J. Clin. Endocrinol. Metab. 93(5), 1553–1562 (2008). https://doi.org/10.1210/jc.2008-0139
F. Ceccato, M. Barbot, M. Zilio et al. Screening tests for cushing’s syndrome: urinary free cortisol role measured by LC-MS/MS. J. Clin. Endocrinol. Metab. 100(10) (2015). https://doi.org/10.1210/jc.2015-2507
P.M. Stewart, A. Boulton, S. Kumar, P.M.S. Clark, C.H.L. Shackleton, Cortisol metabolism in human obesity: impaired cortisone→cortisol conversion in subjects with central adiposity 1. J. Clin. Endocrinol. Metab. 84(3), 1022–1027 (1999). https://doi.org/10.1210/jcem.84.3.5538
E. Rask, T. Olsson, S. Söderberg et al. Tissue-specific dysregulation of cortisol metabolism in human obesity. J. Clin. Endocrinol. Metab. 86(3), 1418–1421 (2001). https://doi.org/10.1210/jcem.86.3.7453
E. Rask, B.R. Walker, S. Söderberg et al. Tissue-specific changes in peripheral cortisol metabolism in obese women: increased adipose 11beta-hydroxysteroid dehydrogenase type 1 activity. J. Clin. Endocrinol. Metab. 87(7), 3330–3336 (2002). https://doi.org/10.1210/jcem.87.7.8661
V. Vicennati, R. Pasquali, Abnormalities of the hypothalamic-pituitary-adrenal axis in nondepressed women with abdominal obesity and relations with insulin resistance: evidence for a central and a peripheral alteration. J. Clin. Endocrinol. Metab. 85(11), 4093–4098 (2000). https://doi.org/10.1210/jcem.85.11.6946
L.K. Nieman, B.M.K. Biller, J.W. Findling et al. The diagnosis of cushing’s syndrome: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 93(5), 1526–1540 (2008). https://doi.org/10.1210/jc.2008-0125
M. Fassnacht, W. Arlt, I. Bancos et al. Management of adrenal incidentalomas: european society of endocrinology clinical practice guideline in collaboration with the european network for the study of adrenal tumors. Eur. J. Endocrinol. 175(2), G34 (2016). https://doi.org/10.1530/EJE-16-0467
T. Ljung, M. Ottosson, A.C. Ahlberg et al. Central and peripheral glucocorticoid receptor function in abdominal obesity. J Endocrinol. Investig. 25(3), 229–235 (2002). https://doi.org/10.1007/BF03343995
R. Pasquali, B. Ambrosi, D. Armanini et al. Cortisol and ACTH response to oral dexamethasone in obesity and effects of sex, body fat distribution, and dexamethasone concentrations: a dose-response study. J. Clin. Endocrinol. Metab. 87(1), 166–175 (2002). https://doi.org/10.1210/jcem.87.1.8158
H. Raff, Cushing’s syndrome: diagnosis and surveillance using salivary cortisol. Pituitary. 15(1), 64–70 (2012). https://doi.org/10.1007/s11102-011-0333-0
T. Deutschbein, M. Broecker-Preuss, J. Flitsch et al. Salivary cortisol as a diagnostic tool for Cushing’s syndrome and adrenal insufficiency: improved screening by an automatic immunoassay. Eur. J. Endocrinol. 166(4), 613 (2012). https://doi.org/10.1530/EJE-11-0945
G. Antonelli, F. Ceccato, C. Artusi, M. Marinova, M. Plebani, Salivary cortisol and cortisone by LC-MS/MS: validation, reference intervals and diagnostic accuracy in Cushing’s syndrome. Clin. Chim. Acta. 451 (2015). https://doi.org/10.1016/j.cca.2015.10.004
S.B. Abraham, D. Rubino, N. Sinaii, S. Ramsey, L.K. Nieman, Cortisol, obesity, and the metabolic syndrome: a cross-sectional study of obese subjects and review of the literature. Obesity. 21(1), E105–E117 (2013). https://doi.org/10.1002/oby.20083
F. Ceccato, M. Barbot, M. Zilio et al. Age and the metabolic syndrome affect salivary cortisol rhythm: data from a community sample. Hormones. 14(3) (2015). https://doi.org/10.14310/horm.2002.1591
F. Ceccato, G. Marcelli, M. Martino et al. The diagnostic accuracy of increased late night salivary cortisol for Cushing’s syndrome: a real-life prospective study. J. Endocrinol. Investig. 1–9 (2018). https://doi.org/10.1007/s40618-018-0921-1
B. MARINIELLO, V. RONCONI, C. SARDU et al. Analysis of the 11β-Hydroxysteroid Dehydrogenase Type 2 Gene (HSD11B2) in human essential hypertension. Am. J. Hypertens. 18(8), 1091–1098 (2005). https://doi.org/10.1016/j.amjhyper.2005.02.020
P. Limumpornpetch, P. M. Stewart. Apparent Mineralocorticoid Excess. In: I Huhtaniemi, (ed.) Encyclopedia of Endocrine Diseases. 3, Academic Press, Elsevier; 638–643 (2018). https://doi.org/10.1016/B978-0-12-801238-3.64338-6. https://www.elsevier.com/books/encyclopedia-of-endocrine-diseases/huhtaniemi/978-0-12-812199-3
R. Pasquali, V. Vicennati, M. Cacciari, U. Pagotto, The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Ann. N. Y. Acad. Sci. 1083, 111–128 (2006). https://doi.org/10.1196/annals.1367.009
J.W. Findling, H. Raff, O.F. DIAGNOSIS, Endocrine disease: differentiation of pathologic/neoplastic hypercortisolism (Cushing’s syndrome) from physiologic/non-neoplastic hypercortisolism (formerly known as pseudo-Cushing’s syndrome). Eur. J. Endocrinol. 176(5), R205–R216 (2017). https://doi.org/10.1530/EJE-16-0946
C. Scaroni, N.M. Albiger, S. Palmieri et al. Approach to patients with pseudo-Cushing’s states. Endocr. Connect. 9(1), R1–R13 (2020). https://doi.org/10.1530/EC-19-0435
World Health Organization. Obesity: preventing and managing the global epidemic report of a WHO consultation (WHO Technical Report Series 894). Geneva, 2000. https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
F. Ceccato, G. Antonelli, M. Barbot et al. The diagnostic performance of urinary free cortisol is better than the cortisol: cortisone ratio in detecting de novo Cushing’s Syndrome: The use of a LC-MS/MS method in routine clinical practice. Eur. J. Endocrinol. 171(1) (2014). https://doi.org/10.1530/EJE-14-0061
F. Ceccato, M. Barbot, N. Albiger et al. Daily salivary cortisol and cortisone rhythm in patients with adrenal incidentaloma. Endocrine. 2017. https://doi.org/10.1007/s12020-017-1421-3
F. Ceccato, C. Artusi, M. Barbot et al. Dexamethasone measurement during low-dose suppression test for suspected hypercortisolism: threshold development with and validation. J. Endocrinol. Investig. 2020. https://doi.org/10.1007/s40618-020-01197-6
F. Pecori Giraldi, A.G. Ambrogio, M. De Martin, L.M. Fatti, M. Scacchi, F. Cavagnini, Specificity of first-line tests for the diagnosis of cushing’s syndrome: assessment in a large series. J. Clin. Endocrinol. Metab. 92(11), 4123–4129 (2007). https://doi.org/10.1210/jc.2007-0596
S.K. Baid, D. Rubino, N. Sinaii, S. Ramsey, A. Frank, L.K. Nieman, Specificity of screening tests for cushing’s syndrome in an overweight and obese population. J. Clin. Endocrinol. Metab. 94(10), 3857–3864 (2009). https://doi.org/10.1210/jc.2008-2766
A. Drincic, E. Fuller, R.P. Heaney, L.A.G. Armas, 25-Hydroxyvitamin D response to graded vitamin D3 supplementation among obese adults. J. Clin. Endocrinol. Metab. 98(12), 4845–4851 (2013). https://doi.org/10.1210/jc.2012-4103
V. Camozzi, A.C. Frigo, M. Zaninotto et al. 25-Hydroxycholecalciferol response to single oral cholecalciferol loading in the normal weight, overweight, and obese. Osteoporos Int. 27(8), 2593–2602 (2016). https://doi.org/10.1007/s00198-016-3574-y
S. Hepsen, E. Sencar, D. Sakiz et al. Serum cortisol level after low dose dexamethasone suppression test may be predictive for diabetes mellitus and hypertension presence in obese patients: a retrospective study. Diabetes Res. Clin. Pract. 161, 108081 (2020). https://doi.org/10.1016/j.diabres.2020.108081
G.W. Strain, B. Zumoff, J.J. Strain, J. Levin, D.K. Fukushima, Cortisol production in obesity. Metabolism. 29(10), 980–985 (1980). http://www.ncbi.nlm.nih.gov/pubmed/6999293
T.G. Travison, A.B. O’Donnell, A.B. Araujo, A.M. Matsumoto, J.B. McKinlay, Cortisol levels and measures of body composition in middle-aged and older men. Clin. Endocrinol (Oxf). 67(1), 71–77 (2007). https://doi.org/10.1111/j.1365-2265.2007.02837.x
V. Vicennati, S. Garelli, E. Rinaldi, G. Di Dalmazi, U. Pagotto, R. Pasquali, Cross-talk between adipose tissue and the HPA axis in obesity and overt hypercortisolemic states. Horm. Mol. Biol. Clin. Investig. 17(2), 63–77 (2014). https://doi.org/10.1515/hmbci-2013-0068
C.P. Woods, M. Corrigan, L. Gathercole et al. Tissue specific regulation of glucocorticoids in severe obesity and the response to significant weight loss following bariatric surgery (BARICORT). J. Clin. Endocrinol. Metab. 100(4), 1434–1444 (2015). https://doi.org/10.1210/jc.2014-4120
I. Chiodini, A. Gaudio, C. Eller-Vainicher et al. Cortisol secretion, sensitivity, and activity are associated with hypertension in postmenopausal eucortisolemic women. J. Clin. Endocrinol. Metab. 104(10), 4441–4448 (2019). https://doi.org/10.1210/jc.2019-00037
S. Champaneri, X. Xu, M.R. Carnethon et al. Diurnal salivary cortisol is associated with body mass index and waist circumference: the multiethnic study of atherosclerosis. Obesity. 21(1), E56–E63 (2013). https://doi.org/10.1002/oby.20047
S. Coelli, C.B. Farias, A.A. Soares et al. Influence of age, gender and body mass index on late-night salivary cortisol in healthy adults. Clin. Chem. Lab. Med. 55(12), 1954–1961 (2017). https://doi.org/10.1515/cclm-2016-1100
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ceccato, F., Lizzul, L., Barbot, M. et al. Pituitary-adrenal axis and peripheral cortisol metabolism in obese patients. Endocrine 69, 386–392 (2020). https://doi.org/10.1007/s12020-020-02392-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02392-4