Abstract
Summary
After a single cholecalciferol load, peak serum 25-hydroxycholecalciferol (25OHD) is lower in individuals with a higher body mass index (BMI), probably due to it being distributed in a greater volume. Its subsequent disappearance from the serum is slower the higher the individual’s BMI, probably due to the combination of a larger body volume and a slower release into the circulation of vitamin D stored in adipose tissue.
Introduction
The aim of the study is to examine 25-hydroxycholecalciferol (25OHD) response to a single oral load of cholecalciferol in the normal weight, overweight, and obese.
Methods
We considered 55 healthy women aged from 25 to 67 years (mean ± SD, 50.8 ± 9.5) with a BMI ranging from 18.7 to 42 kg/m2 (mean ± SD, 27.1 ± 6.0). The sample was divided into three groups by BMI: 20 were normal weight (BMI ≤ 25 kg/m2), 21 overweight (25.1 ≤ BMI ≤ 29.9 kg/ m2), and 14 obese (BMI ≥ 30 kg/m2). Each subject was given 300,000 IU of cholecalciferol orally during lunch. A fasting blood test was obtained before cholecalciferol loading and then 7, 30, and 90 days afterwards to measure serum 25OHD, 1,25 dihydroxyvitamin D [1,25 (OH)2D], parathyroid hormone (PTH), calcium (Ca), and phosphorus (P). Participants’ absolute fat mass was measured using dual energy X-ray absorptiometry (DEXA).
Results
The fat mass of the normal weight subjects was significantly lower than that of the overweight, which in turn was lower than that of the obese participants. Serum 25OHD levels increased significantly in all groups, peaking 1 week after the cholecalciferol load. Peak serum 25OHD levels were lower the higher the individuals’ BMI. After peaking, the 25OHD levels gradually decreased, following a significantly different trend in the three groups. The slope was similar for the overweight and obese, declining significantly more slowly than in the normal weight group. In the sample as a whole, there was a weakly significant negative correlation between fat mass and baseline 25OHD level, while this correlation became strongly significant at all time points after cholecalciferol loading.
Conclusions
The lower peak 25OHD levels seen in the obese and overweight is probably due to the cholecalciferol load being distributed in a larger body volume. The longer persistence of 25OHD in their serum could be due to both their larger body volume and a slower release into the circulation of the vitamin D stored in their adipose tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D is essential to ensure an adequate intestinal absorption of calcium. It is also involved in many other physiological and pathological processes, including the immune system [1, 2], cardiovascular diseases [3], endocrine gland function [4, 5], and oncological diseases [6, 7]. Cholecalciferol (vitamin D3) of animal origin (produced by irradiation of the skin with UVB) and plant-derived ergocalciferol (vitamin D2) are hydroxylated in the liver in position 25. The resulting 25-hydroxyvitamin D (25OHD) provides the substrate for subsequent hydroxylation in position 1-alpha (which occurs mainly in the kidney) to synthesize 1,25 dihydroxyvitamin D [1,25(OH)2D], which has systemic effects. Serum 25OHD concentration is considered the most reliable indicator of vitamin D status, but what constitutes a normal serum 25OHD level is still not clear. Several studies have shown an inverse relationship between parathyroid hormone (PTH) and 25OHD levels, higher serum 25OHD levels being associated with lower PTH levels. The 25OHD levels at which PTH reaches a plateau range from 12 to 50 ng/ml (30–125 nmol/L), but this generally occurs at less than 30 ng/ml (75 nmol/L) [8]. Other studies that considered other effects of 25OHD, such as its influence in reducing the incidence of juvenile diabetes, colon cancer, and other diseases, have reported that 25OHD levels higher than 30 ng/ml are required to be effective [9].
The adipose tissue plays a part in the distribution of vitamin D, though its importance has yet to be clearly established. There is increasing evidence of serum 25OHD levels being inversely associated with obesity [10–17]. Whether vitamin D in the adipose tissue serves as a reserve that can be released into the circulation to meet the body’s needs or whether its deposition in fat is definitive, and this vitamin D is no longer able to return to the circulation is still object of debate. The aim of this study was to examine serum 25OHD levels in response to oral loading with a single, high dose of cholecalciferol in normal weight, overweight, and obese individuals.
Materials and methods
We examined 55 healthy women from 25 to 67 years of age (mean ± SD, 50.8 ± 9.5) with a body mass index (BMI, kg/m2) ranging from 18.7 to 42.1 (mean ± SD, 27.1 ± 6.0).
Our inclusion criteria were age >20 years, no intestinal or endocrine diseases, and no use of drugs that could interfere with calcium or vitamin D metabolism. Our exclusion criteria were intestinal malabsorption, current intake of vitamin D in any form, renal or hepatic insufficiency, and prior bariatric surgery.
All the women volunteered for the study and were recruited from among the students, technical and medical staff at our institution, or their relatives and friends. All procedures performed in this study were in accordance with the ethical standards of our institutional research committee and with the 1964 Helsinki Declaration and its subsequent amendments. All participants gave their informed consent to the study and to the use of their personal data. The local ethical committee was informed of the study design.
At the baseline, data on daily calcium intake were collected using the self-report questionnaire proposed by Montomoli et al. [18], which is based on 15 questions concerning food and beverage commonly ingested over the course of 1 week. Subjects were classified as having a daily calcium intake of less or more than 1 g a day. Exposure to sunlight was calculated from a self-report questionnaire using a simplified version of the one proposed by Glanz et al. [19] for adults, based on the average time (hours/day) spent outside on weekdays (Monday-Friday) and at weekends (Saturday and Sunday) between 10 am and 4 pm from March to September, without using sunscreens. Subjects were grouped into three categories: group 1, an hour a day or less; group 2, 1 to 3 h; and group 3, more than 3 h.
The sample was divided into three groups by BMI: 20 women were normal weight (BMI ≤ 25 kg/m2), 21 were overweight (25.1 ≤ BMI ≤ 29.9 kg/m2), and 14 were obese (BMI ≥ 30 kg/m2).
Between October and December 2013, each participant was given a single oral dose of 300,000 IU of cholecalciferol in an oily solution on a slice of bread during lunch. All subjects underwent venous blood sampling to measure their serum levels of 25OHD, 1,25(OH)2D, parathyroid hormone (PTH), calcium (Ca), and phosphorus (P). Fasting blood samples were collected from 7.00 to 9.00 am before cholecalciferol loading, then 7, 30, and 90 days afterwards. No vitamin D or 25OHD supplements were added to the participants’ diet. Serum Ca was measured using a colorimetric assay with the chromophore 5-nitro-5′-methyl-1,2-bis(o-aminophenoxy)ethan-N,N,N′,N′-tetraacetic acid (NM-BAPTA). Serum P was measured using a colorimetric assay with ammonium molybdate. Both methods were automated on a Cobas 8000 instrument (Roche Diagnostics). Serum PTH was measured with the LIAISON® N-tactTMPTH kit that relies on chemiluminescence (CLIA) technology in an immunoassay for quantifying intact human parathyroid hormone in the serum (detection limit [DL], 10 pg/ml; inter- and intra-assay coefficient of variation [CV], 4 and 3.5 %, respectively). Serum 25OHD concentrations were measured with the direct competitive method using a chemiluminescence immunoassay (DiaSorin, Italy) automated on the LIAISON XL instrument (DL, 1.5 nmol/L; inter- and intra-assay CV, 9 %). The method was linear from 1.5 to 375 nmol/L. The assay demonstrates a 100 % analytical specificity towards 25OHD, and a cross-reactivity of <2 % towards vitamin D2 and vitamin D3, and from 2 to 9 % for other vitamin D metabolites. During the study, the method’s analytical performance was monitored using internal quality control as well as an external quality assurance scheme. Serum 1,25(OH)2D was measured with the 1,25 dihydroxyvitamin D IDS RIA® kit (DL, 5 pmol/L; inter- and intra-assay CV, 8.6–16.6 and 11.9–20 %, respectively). Body composition, and fat mass in particular, was measured by DXA using a Hologic Delphi device (Hologic Inc., Bedford, MA, USA).
Statistical analysis
The results are summarized as counts and percentages for categorical variables and as means and standard deviations for quantitative variables. Participants’ baseline characteristics were compared using the chi-square or Fisher’s exact test in the case of categorical variables and ANOVA in the case of quantitative variables, followed by Bonferroni’s multiple comparisons, when the previous tests were statistically significant. Correlations between baseline fat mass and 25OHD at each time point, baseline PTH, baseline 1,25(OH)2D, and individual slopes for 25OHD trends beyond the peak were estimated using Pearson’s correlation coefficient and calculating the p value to establish their statistical significance. The trends of the 25OHD, 1,25(OH)2D, and PTH levels after cholecalciferol loading were compared in the three BMI groups using a mixed model analysis of covariance for repeated measures with an unstructured variance-covariance matrix, and considering the baseline value as the covariate and the effects of group and time, and the group by time interactions. Our results are presented as p values, unadjusted means and standard deviations, least squares means with 95 % confidence intervals (CI) for each group 7, 30, and 90 days after cholecalciferol loading, and pairwise least squares means comparing the groups at 7, 30, and 90 days with 95 % CI after Bonferroni’s adjustment for multiple comparisons. Statistical significance was set at the 5 % level. The statistical analysis was conducted with SAS 9.4 (SAS Institute Inc., Cary, NC, USA) for Windows and GraphPad Prism (GraphPad Software, Inc., La Jolla, CA, USA).
Results
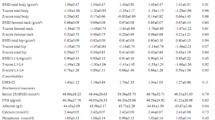
Table 1 shows participants’ baseline characteristics. In the sample as a whole, total fat mass ranged from 11.8 to 54.6 kg. When subjects were grouped by BMI, the body fat mass of the normal weight group was significantly lower than that of the overweight individuals, which was in turn lower than that of the obese women.
At the baseline, all the women had detectable 25OHD serum levels, but 96.4 % of them had 25OHD levels below 75 nmol/L, which is considered the minimum threshold of the normal range in the Italian guidelines [20]; only two women (3.6 %), both in the overweight group, had baseline 25OHD higher than 75 nmol/L. The obese group had lower serum 25OHD levels than the normal weight or overweight groups, but the difference was only statistically significant vis-à-vis the overweight group. The obese also had significantly lower 1,25(OH)2D levels than the normal weight group, but higher PTH levels. Daily calcium intake and exposure to sunlight did not differ statistically among the three groups. At the baseline, there was a weakly significant negative correlation between fat mass and 25OHD, which became strongly significant at all time points after cholecalciferol loading (Fig. 1). Baseline fat mass correlated positively with PTH and negatively with 1,25(OH)2D (Fig. 2).
Table 2 and Fig. 3 show the trends of 25OHD, PTH, and 1,25(OH)2D levels after cholecalciferol loading. The participants’ 25OHD levels increased significantly after cholecalciferol loading and were found highest on day 7, but they remained higher than at the baseline in all groups until the end of the study. The increase in 25OHD levels persisting 7 and 30 days after cholecalciferol loading was significantly greater in the normal weight than that in the overweight or obese women, while the difference between the latter two groups was not significant. After peaking, the 25OHD levels dropped significantly over time, but at a significantly different rate in the three BMI groups. A week after cholecalciferol loading, PTH levels were found significantly lower than baseline only in the normal weight (p = 0.028), not in the overweight or obese subjects, with no difference among the three groups. Participants’ 1,25(OH)2D levels were found significantly higher than baseline in all groups on days 7 and 30, but by day 90, they only remained high in the overweight group, with no differences among the three groups (for p values, see Table 2). In the sample as a whole, individual slopes correlated positively with total fat mass, while the absolute delta values of the 25OHD levels from the baseline to the peak at 7 days correlated negatively with total fat mass (Fig. 4).
a Least squares means of serum 25OHD levels in the three BMI groups 7, 30, and 90 days after cholecalciferol loading. Following the peak, 25OHD values dropped significantly over time, but at different rates in the three groups. b Least squares means of PTH levels after cholecalciferol loading in the three BMI groups: the obese reached a higher peak PTH than the other two groups (which did not differ from one another), then the levels remained stable in all three groups. c Least squares means of 1,25(OH)2D in the three BMI groups after cholecalciferol loading. Calcitriol levels reached a lower peak in the obese than in the other two groups, but the rate of decline afterwards did not differ between the three groups
There was a positive correlation between 25OHD and 1,25(OH)2D at all time points in the study except for day 30 (Fig. 5), and there was a negative correlation between 25OHD and PTH at all time points in the study except for day 90 (Fig. 6). There was a trend towards a negative correlation between PTH and 1,25(OH)2D, which was only statistically significant 7 days after cholecalciferol loading (Fig. 7).
Discussion
In our sample, 25OHD deficiency was more severe in individuals with a higher BMI. This finding is consistent with previous reports of 25OHD levels correlating inversely with BMI [21]. Several hypotheses have been advanced to explain this relationship, including limited exposure to sunlight [22], a greater vitamin D uptake in adipose tissue [23], and a greater volume dilution [24]. All of these hypotheses may contribute in various ways to lowering 25OHD levels in the obese. In a large population cohort receiving no vitamin D supplements, Drincic et al. [24] found body weight and body fat inversely related to 25OHD levels, and a hyperbolic model (the mathematical expression of dilution) best explained the lower 25OHD levels in obesity. The same authors investigated the response to three different doses of vitamin D in a group of obese subjects, demonstrating a direct relationship between the administered dose and body size. Given the parallelism of the dose-response curves in their obese and non-obese subjects, the authors suggested that the dilution of vitamin D in fat tissue and extracellular fluid—rather than its sequestration in the fat tissue—could account for the different response [25].
In our study, the increase in serum 25OHD levels after cholecalciferol loading was greater in normal weight women than that in the overweight or obese. This finding is perfectly consistent with a different dilution of vitamin D in the body tissues. After peaking, the 25OHD levels dropped more slowly in the obese women. Judging from the positive relationship between fat mass and the rate of decline in 25OHD levels after peaking, combined with the negative relationship between fat mass and the delta of the 25OHD levels between the baseline and the peak, a greater fat mass coincides with a smaller increase in 25OHD levels after loading, and the body compartment where vitamin D is distributed consists mainly of fat, which seems to have an important role in the distribution of 25OHD within the body. This assumption is supported by direct cholecalciferol measurements in the subcutaneous fat tissue obtained by needle biopsy in 29 subjects with impaired glucose intolerance: Didriksen et al. showed that subcutaneous adipose tissue can store large amounts of cholecalciferol after long-term oral supplementation [26]. The slower drop in our obese women’s 25OHD levels may derive from an increased peripheral metabolism or from the increased cholecalciferol deposition in the adipose tissue. There is some evidence to suggest that cholecalciferol itself is stored in fat, whereas its 25OHD is absorbed in the muscle, and its serum concentrations would correlate mainly with muscle-related parameters, such as lean body mass and exercise [27, 28]. There are reports of differentiated muscle cells being able to uptake 25OHD in a megalin-dependent process [29, 30]. On the other hand, pre-adipocytes (but not differentiated adipocytes) are capable of accumulating 25OHD in a time-dependent manner [31]. Because adipose tissue consists mainly of differentiated adipocytes, it is only marginally involved in supplying the extracellular pool of circulating 25OHD. Unlike 25OHD, its precursor cholecalciferol has been found to accumulate mainly in adipose tissue, especially when taken orally [26]. This is explained mainly by the fact that oral cholecalciferol is carried in the blood by chylomicrons, and it binds only minimally to vitamin D binding protein (DBP), towards which it has a low affinity. The cholecalciferol circulating in chylomicrons is then absorbed by the adipose tissue, due to the action of lipoprotein lipase. The liver collects any cholecalciferol that has not been taken up in the adipose tissue, promptly removing it from the blood [32]. If cholecalciferol was sequestered permanently in the adipose tissue, then we should see a lower peak and a rapid removal of cholecalciferol from the blood in the obese because, for a given dose administered, their adipose tissue would accumulate more cholecalciferol than normal weight subjects, so the blood would contain less 25OHD (of which cholecalciferol is the precursor). In other words, obese people would have a smaller proportion of substrate from which to form 25OHD. Therefore, whatever the amount of cholecalciferol deposited in the adipose tissue, once 25OHD has been synthetized by the liver, it should follow the same metabolic pathway, irrespective of an individual’s BMI, and the slope of the declining levels of 25OHD in the blood would be the same for normal weight, overweight, or obese individuals. Instead, the slopes differed in our sample, with the obese showing a slower drop in serum 25OHD levels than individuals with a lower fat mass. The differences in slopes could be due both to the difference in concentration—due to a larger body size and distribution—and to a gradual, slow release of cholecalciferol from body fat, which would increase the amount of substrate available to the liver for 25OHD synthesis.
We cannot exclude a direct involvement of 25OHD in the exchange between adipose tissue and the blood; however, Piccolo et al. [33] measured the concentration of 25OHD in the subcutaneous white adipose tissue (SWAT) from a group of obese subjects taking part in a clinical weight loss program. They found a positive association between SWAT 25OHD and serum 25OHD, which did not change after 20 weeks of a low-calorie diet achieving an average loss of 5 kg of fat and 6 % of total body weight. The authors concluded that 25OHD in fat does not significantly contribute to serum levels of 25OHD, although they confirmed a balance between 25OHD concentrations in the serum and adipose tissue. It may be that no change in serum 25OHD levels came to light after participants lost weight because of the modest reduction in their fat mass. In fact, another had demonstrated that a loss of >15 % of body weight was associated with a significant increase in serum 25OHD levels, which was not seen in individuals whose weight remained stable or dropped by less than 15 % [34].
In our study, 1,25(OH)2D levels appeared to be lower in the obese and overweight than in normal weight individuals. It is well known that 1,25(OH)2D levels depend not only on PTH-dependent 1-alpha hydroxylation in the kidney but also on the amount of substrate available. We found a positive correlation between 25OHD and 1,25(OH)2D at all time points, except after 30 days, which probably means that an adequate amount of substrate is needed for 1,25(OH)2D synthesis and an inadequate amount of substrate might explain the lower 1,25(OH)2D levels in obese subjects. The negative correlation between PTH and 1,25(OH)2D at all time points (though it was only significant 1 week after cholecalciferol loading) suggests that an increase in serum 1,25(OH)2D levels is responsible for a reduction in PTH, not vice versa. However, factors other than 1,25(OH)2D may influence PTH levels: 25OHD may directly suppress the PTH secretion via binding to the vitamin D receptor [35, 36]; furthermore, the simple increase in weight may explain the higher PTH level in the obese population independently of vitamin D metabolites [37].
Our study has some limitations that need to be acknowledged. For a start, our sample consisted entirely of women, so our results cannot be extended to the male gender. We measured total body fat, without distinguishing between the white and brown types, which might interfere with vitamin D metabolism to a different extent. Although the 2–9 % they account for is not a large proportion per se, the vitamin D metabolites that we did not measure [and 24,25(OH)2D in particular] might have affected our results, given the amount of cholecalciferol administered. Ours was a pharmacological study, since the ingested dose of cholecalciferol was unusual, making the implications of our findings in normal physiology minimal. Finally, serum cholecalciferol was not measured in our study.
In conclusion, 25OHD response to a large, single oral dose of cholecalciferol differed in relation to BMI in obese and normal weight subjects under our experimental conditions. Peak serum 25OHD levels were lower in individuals with a higher BMI, probably due to the cholecalciferol being distributed in a larger body volume in the obese. The subsequent slower decline in the obese subjects’ serum 25OHD levels could again have to do with their larger body size and also derive from a slower release of vitamin D from their body fat. This finding has practical implications for cholecalciferol supplementation: a slower decline in serum 25OHD levels over time means that, once an optimal serum concentration of 25OHD has been reached, the interval between cholecalciferol administrations needed to maintain this concentration could be longer for subjects with a higher BMI.
References
Höck AD (2014) Vitamin D3 deficiency results in dysfunctions of immunity with severe fatigue and depression in a variety of diseases. In Vivo 28(1):133–145
Lucas RM, Gorman S, Geldenhuys S, Hart PH (2014) Vitamin D and immunity. F1000 Prime Rep. 1;6:118
Zittermann A (2014) Vitamin D and cardiovascular disease. Anticancer Res 34(9):4641–4648
Romagnoli E, Pepe J, Piemonte S, Cipriani C, Minisola S (2013) Management of endocrine disease: value and limitations of assessing vitamin D nutritional status and advised levels of vitamin D supplementation. Eur J Endocrinol 169(4):R59–R69
Muscogiuri G, Mitri J, Mathieu C, Badenhoop K, Tamer G, Orio F, Mezza T, Vieth R, Colao A, Pittas A (2014) Mechanisms in endocrinology: vitamin D as a potential contributor in endocrine health and disease. Eur J Endocrinol 171(3):R101–R110
Shui I, Giovannucci E (2014) Vitamin D status and cancer incidence and mortality. Adv Exp Med Biol 810:33–51
Ordóñez Mena JM, Brenner H (2014) Vitamin D and cancer: an overview on epidemiological studies. Adv Exp Med Biol 810:17–32
Sai AJ, Walters RW, Fang X, Gallagher JC (2011) Relationship between vitamin D, parathyroid hormone, and bone health. J Clin Endocrinol Metab 96(3):E436–E446
Gandini S, Boniol M, Haukka J, Byrnes G, Cox B, Sneyd MJ, Mullie P, Autier P (2011) Meta-analysis of observational studies of serum 25-hydroxyvitamin D levels and colorectal, breast and prostate cancer and colorectal adenoma. Int J Cancer 128(6):1414–1424
Peterson CA, Tosh AK, Belenchia AM (2014) Vitamin D insufficiency and insulin resistance in obese adolescents. Ther Adv Endocrinol Metab 5(6):166–189
Cipriani C, Pepe J, Piemonte S, Colangelo L, Cilli M, Minisola S (2014) Vitamin D and its relationship with obesity and muscle. Int J Endocrinol 2014:841248. doi:10.1155/2014/841248
Gulseth HL, Gjelstad IM, Birkeland KI, Drevon CA (2013) Vitamin D and the metabolic syndrome. Curr Vasc Pharmacol 11(6):968–984
Vanlint S (2013) Vitamin D and obesity. Nutrients 5(3):949–956
Blum M, Dallal GE, Dawson-Hughes B (2008) Body size and serum 25 hydroxy vitamin D response to oral supplements in healthy older adults. J Am Coll Nutr 27(2):274–279
Lee P, Greenfield JR, Seibel MJ, Eisman JA, Center JR (2009) Adequacy of vitamin D replacement in severe deficiency is dependent on body mass index. Am J Med 122(11):1056–1060
Tepper S, Shahar DR, Geva D, Ish-Shalom S (2014) Predictors of serum 25(OH)D increase following bimonthly supplementation with 100,000 IU vitamin D in healthy, men aged 25-65 years. J Steroid Biochem Mol Biol 144 Pt A:163–166
Ekwaru JP, Zwicker JD, Holick MF, Giovannucci E, Veugelers PJ (2014) The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One 9(11):e111265
Montomoli M, Gonnelli S, Giacchi M, Mattei R, Cuda C, Rossi S, Gennari C (2002) Validation of a food frequency questionnaire for nutritional calcium intake assessment in Italian women. Eur J Clin Nutr 56(1):21–30
Glanz K, Yaroch AL, Dancel M, Saraiya M, Crane LA, Buller DB, Manne S, O’Riordan DL, Heckman CJ, Hay J, Robinson JK (2008) Measures of sun exposure and sun protection practices for behavioral and epidemiologic research. Arch Dermatol 144(2):217–222
Società Italiana dell’Osteoporosi, del Metabolismo Minerale e delle Malattie dello Scheletro (2013) Guidelines for the diagnosis, prevention and treatment of osteoporosis. Italian Osteoporosis, Mineral Metabolism, and Skeletal Diseases Society. Minerva Endocrinol 38(1 Suppl 1):1–30
Saneei P, Salehi-Abargouei A, Esmaillzadeh A (2013) Serum 25-hydroxyvitamin D levels in relation to body mass index: a systematic review and meta-analysis. Obes Rev 14(5):393–404
Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80(6 Suppl):1678S–1688S
Foo LH, Teo PS, Abdullah NF, Aziz ME, Hills AP (2013) Relationship between anthropometric and dual energy X-ray absorptiometry measures to assess total and regional adiposity in Malaysian adolescents. Asia Pac J Clin Nutr 22(3):348–356
Drincic AT, Armas LA, Van Diest EE, Heaney RP (2012) Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity 20(7):1444–1448
Drincic A, Fuller E, Heaney RP, Armas LA (2013) 25-Hydroxyvitamin D response to graded vitamin D3 supplementation among obese adults. J Clin Endocrinol Metab 98(12):4845–4851
Didriksen A, Burild A, Jakobsen J, Fuskevåg OM, Jorde R (2015) Vitamin D3 increases in abdominal subcutaneous fat tissue after supplementation with vitamin D3. Eur J Endocrinol 172(3):235–241
Brock K, Cant R, Clemson L, Mason RS, Fraser DR (2007) Effects of diet and exercise on plasma vitamin D (25OHD) levels in Vietnamese immigrant elderly in Sydney, Australia. J Steroid Biochem Mol Biol 103(3-5):786–792
Abboud M, Puglisi DA, Davies BN, Rybchyn M, Whitehead NP, Brock KE, Cole L, Gordon-Thomson C, Fraser DR, Mason RS (2013) Evidence for a specific uptake and retention mechanism for 25-hydroxyvitamin D (25OHD) in skeletal muscle cells. Endocrinology 154(9):3022–3030
Rowling MJ, Kemmis CM, Taffany DA, Welsh J (2006) Megalin-mediated endocytosis of vitamin D binding protein correlates with 25-hydroxycholecalciferol actions in human mammary cells. J Nutr 136(11):2754–2759
Abboud M, Gordon-Thomson C, Hoy AJ, Balaban S, Rybchyn MS, Cole L, Su Y, Brennan-Speranza TC, Fraser DR, Mason RS (2014) Uptake of 25-hydroxyvitamin D by muscle and fat cells. J Steroid Biochem Mol Biol 144 Pt A:232–236
Haddad JG, Matsuoka LY, Hollis BW, Hu YZ, Wortsman J (1993) Human plasma transport of vitamin D after its endogenous synthesis. J Clin Invest 91(6):2552–2555
Jones G (2008) Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr 88(2):582S–586S
Piccolo BD, Dolnikowski G, Seyoum E, Thomas AP, Gertz ER, Souza EC, Woodhouse LR, Newman JW, Keim NL, Adams SH, Van Loan MD (2013) Association between subcutaneous white adipose tissue and serum 25-hydroxyvitamin D in overweight and obese adults. Nutrients 5(9):3352–3366
Mason C, Xiao L, Imayama I, Duggan CR, Bain C, Foster-Schubert KE, Kong A, Campbell KL, Wang CY, Neuhouser ML, Jeffery RW, Robien K, Alfano CM, Blackburn GL, McTiernan A (2011) Effects of weight loss on serum vitamin D in postmenopausal women. Am J Clin Nutr 94(1):95–103
Ritter CS, Armbrecht HJ, Slatopolsky E, Brown AJ (2011) 25-Hydroxyvitamin D(3) suppresses PTH synthesis and secretion by bovine parathyroid cells. Kidney Int 70(4):654–659
Ritter CS, Brown AJ (2011) Direct suppression of PTH gene expression by the vitamin D prohormones doxercalciferol and calcidiol requires the vitamin D receptor. J Mol Endocrinol 46(2):63–66
Grethen E, McClintock R, Gupta CE, Jones R, Cacucci BM, Diaz D, Fulford AD, Perkins SM, Considine RV, Peacock M (2011) Vitamin D and hyperparathyroidism in obesity. J Clin Endocrinol Metab 96(5):1320–1326
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Valentina Camozzi, Francesca Sanguin, Anna Chiara Frigo, Martina Zaninotto, Mario Plebani, Marco Boscaro, Lisa Schiavon, and Giovanni Luisetto have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Camozzi, V., Frigo, A.C., Zaninotto, M. et al. 25-Hydroxycholecalciferol response to single oral cholecalciferol loading in the normal weight, overweight, and obese. Osteoporos Int 27, 2593–2602 (2016). https://doi.org/10.1007/s00198-016-3574-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3574-y