Abstract
Summary
Discontinuation of denosumab (Dmab) therapy is associated with lower serum CTX levels in osteoporotic patients previously exposed to bisphosphonates compared to those who were not.
Introduction
Discontinuation of Dmab therapy is followed by a transient increase of bone turnover markers (BTMs) above pretreatment values, together with accelerated bone loss, and potentially an increased risk of multiple vertebral fractures. Since a substantial proportion of patients discontinuing Dmab have previously been exposed to bisphosphonates (BPs), we hypothesized that previous BP therapy could attenuate this increase in bone turnover because of the prolonged biological effects of BPs on bone.
Methods
In a retrospective observation, we assessed serum CTX levels between 7 and 24 months after the last Dmab injection in 37 patients (33 women and 4 men, aged 50 to 84 years). CTX levels were analyzed according to the number of Dmab injections (1 or multiple) and previous exposure to BPs.
Results
In 8 patients who had received only 1 Dmab injection, 7 out of 8 were previously on BPs and none of them showed CTX values above the premenopausal range after Dmab discontinuation. CTX also remained in the premenopausal range in 14 out of 17 patients who discontinued Dmab after multiple (4.1 ± 1.4, range 2–7) injections but were previously exposed to BPs (mean exposure 6.9 ± 5.8 years, range 11 months–15 years; mean time interval between BP exposure and Dmab initiation 25 ± 10 months, range 0–48). In contrast, in 12 patients who discontinued Dmab after multiple (5, range 3–9) injections without prior exposure to BPs, mean CTX levels as measured on average 11.3 months (range 6–23) after the last Dmab injection were above the upper limit of premenopausal range (mean +114%, range 28–320%, p = 0.003–0.005 vs previous BPs).
Conclusion
The higher CTX levels occurring after Dmab discontinuation in patients who have received multiple injections may be prevented by prior exposure to BPs. This observation may be related to the persistent effects of BPs on bone that prevent the resorbing activity of newly formed osteoclasts when RANK Ligand is no more antagonized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The monoclonal antibody denosumab (Dmab) is a potent inhibitor of bone resorption, which reduces vertebral and non-vertebral fracture risk, including the hip [1]. As shown in phase 2 and phase 3 trials, discontinuation of Dmab treatment is followed by a transient increase of bone turnover markers (BTMs) above pretreatment levels, which peaks between 12 and 18 months after the last Dmab injection, together with an accelerated bone loss at both spine and hip [2,3,4]. This raises the possibility of a transient increase in bone fragility, which is of particular concern in osteoporotic patients who remain at high fracture risk. Few cases of multiple vertebral fractures have been reported in patients who discontinued Dmab without any further antiresorptive agent [5,6,7,8,9]. A recent analysis of the FREEDOM study showed that discontinuation of Dmab was associated with an increase in vertebral fracture risk to levels observed in the placebo group but with a greater incidence of multiple events [10] Although continuous treatment with Dmab for up to 10 years has been shown to be safe and efficacious, many patients interrupt Dmab therapy earlier on for a variety of reasons (inconvenience, fear of side effects, reached apparent treatment target). Many patients on Dmab have been previously treated with bisphosphonates (BPs), in which case inhibitory effects on bone turnover may persist several years after the end of therapy [11, 12]. Indeed, BPs can remain stored for a long time in the bone matrix [13], particularly when their release from the bone surface has been slowed down by other potent antiresorptive agents such as Dmab. This raises the hypothesis that previous treatment with long-acting BPs could blunt the increase of bone turnover occurring upon Dmab discontinuation. We investigated the level of the serum bone resorption biochemical marker CTX according to their previous exposure to BPs or not, in osteoporotic patients who discontinued Dmab injections.
Patients and methods
In a retrospective observation, we assessed fasting serum CTX in 37 patients (mean age 68.2 ± 4.2, range 50–84), 11.5 ± 4.6 months after last Dmab injection. Among these 37 patients, 12 patients were BP “naive” at Dmab initiation, 17 patients were treated with BP prior to Dmab for at least 11 months, and 8 patients received only 1 Dmab injection (7 had prior BPs and 2 were on menopausal hormone therapy). The latter subjects were considered as 1 group, irrespective of previous BP, since it has been shown that a single Dmab injection was not followed by an increase in bone turnover markers above pretreatment values [3, 14]. The indications for Dmab treatment were osteoporosis (n = 35) or aromatase inhibitor therapy (n = 2). The reasons for discontinuing Dmab administration were general practioners’ decision (n = 11), patients’ unwillingness to pursue therapy (n = 10), concern about teeth problems (n = 4), fracture occurrence (n = 3), skin disorder (n = 3), end of aromatase inhibitor therapy (n = 2), hypocalcemia (n = 1), insurance coverage refusal (n = 1), and unknown (n = 2). These causes were similarly distributed among the 3 groups. In the group previously treated with bisphosphonates for up to 15 years, 12 patients received only 1 compound (10 alendronate, 1 IV ibandronate, 1 pamidronate), 3 patients received successively 2 compounds (1 risedronate then zoledronate, and 2 alendronate then ibandronate), and 2 received 3 (alendronate-risedronate-zoledronate, and alendronate-ibandronate-zoledronate). In the group with only 1 Dmab injection, 7 patients were previously treated with BP (4 alendronate, 3 alendronate followed by ibandronate).
Fasting blood samples were collected for the determination of the bone resorption biochemical marker CTX. Various assays were used (Elecsys-Roche, n = 5; IDS-ISYS, n = 26; ECLIA-Cobas 8000-Roche, n = 6). All the clinical chemistry laboratories were applying a central quality control program (Swiss quality control program). When several sequential serum values were available, we selected the blood sample collected nearest to the 12 to 18 months interval after the last Dmab injection. This period corresponds to the highest values of bone turnover markers as reported during the offset of the phase 2 trial [2].
Data are reported as medians and interquartile ranges unless otherwise specified. Differences in CTX levels between groups were assessed using nonparametric tests (Mann-Whitney test). The data were analyzed using STATA software, version 14.0. (StataCorp LP, College Station, TX, USA).
Results
Thirty-seven patients who had discontinued Dmab treatment for various reasons (as detailed in “Patients and methods” section) were segregated into 3 groups for comparison, namely (1) those who received a single Dmab injection, irrespective of previous exposure to BPs; (2) those who received multiple injections of Dmab and who were not previously treated with BPs (BP naïve); (3) and those who received multiple Dmab injections after BP therapy (Table 1).
In the group who discontinued Dmab treatment after a single injection, most patients (7/8) were previously on BPs and no elevated CTX was seen (Fig. 1). In the 2 groups who stopped Dmab after repeated injections, Dmab treatment had lasted 1 to 4.5 years (2 to 9 subcutaneous injections), with no difference in treatment duration between BP naïves and previous BP groups (Table 1). In the BP-naïve group, post-denosumab CTX levels were above the premenopausal range in 9 out of 12 patients, among whom 3 were actually above the postmenopausal range. In those 9 patients, mean CTX as measured on average 11.3 months (range 6–23) after the last Dmab injection was increased +114% (range 28–320%) above the upper premenopausal threshold. As shown in Fig. 1, only 3 patients in this group had apparently normal CTX values, as measured 6 (1 patient) and 8 (2 patients) months after the last Dmab injection. In this case, we cannot exclude that later sampling could have shown some higher values.
Serum CTX values according to time after last denosumab (Dmab) injection in naive-treated patients ( ), in patients previously treated with bisphosphonate (BP) (
), in patients previously treated with bisphosphonate (BP) ( ), or in patients who stopped after receiving only 1 Dmab injection (
), or in patients who stopped after receiving only 1 Dmab injection ( ). One dotted line (
). One dotted line ( ) corresponds to the upper limit of premenopausal values and the other (
) corresponds to the upper limit of premenopausal values and the other ( ) to the upper limit of premenopausal values of CTX
) to the upper limit of premenopausal values of CTX
Among the 17 patients who discontinued Dmab after multiple injections but were previously exposed to BPs, BP therapy had lasted 11 months to 15 years, and the interval between the last BP and the first Dmab administration varied between 0 and 72 months. All but 3 of them kept CTX levels within the premenopausal range after Dmab discontinuation (Fig. 1). Hence, median CTX values were significantly higher in BP naïve compared to previously exposed subjects (Fig. 2). Among the 3 with elevated CTX despite previous BP exposure, 1 patient had similarly high values during her previous alendronate therapy (data not shown), raising the possibility of poor compliance and/or absorption; the 2 others had received ibandronate, which has a time-limited effect on bone resorption [14].
Boxplots of CTX levels per group, showing medians, quartiles, minimum and maximum and outlier values after Dmab cessation in bisphosphonate (BP)-naive patients, in patients previously treated with BP, and in patients having received only 1 Dmab injection. There is a significant statistical difference between BP-naïve and previously BP-treated patients. One dotted line ( ) corresponds to the upper limit of premenopausal values and the other (
) corresponds to the upper limit of premenopausal values and the other ( ) to the upper limit of premenopausal values of CTX
) to the upper limit of premenopausal values of CTX
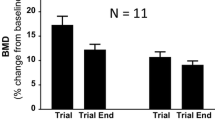
In a subgroup of patients (n = 8) who discontinued Dmab after several injections and who were previously treated with BPs, we were able to compare serum CTX levels 1 year after the last Dmab with pre-denosumab values. In all but 1 patient, serum CTX values remained in the premenopausal range 1 year after Dmab and were similar to pre-treatment levels (difference after-before Dmab, 0.03 ± 0.04 ng/mL, t = 0.88) (Fig. 3).
Serum CTX values of individuals in a subgroup of 8 patients who received more than 1 Dmab injection and previously treated with bisphosphonate, before the first Dmab injection and 1 year after the last one. One dotted line ( ) corresponds to the upper limit of premenopausal values and the other (
) corresponds to the upper limit of premenopausal values and the other ( ) to the upper limit of premenopausal values of CTX
) to the upper limit of premenopausal values of CTX
Discussion
In this retrospective observation, CTX levels in patients having discontinued Dmab treatment for various reasons remained within the premenopausal range several months after cessation of Dmab therapy when they had received long-acting bisphosphonates before Dmab. In contrast, patients not previously treated with BPs displayed elevated values compatible with a bone turnover increase upon discontinuation of Dmab therapy, as reported during the offset of both phase 2 and 3 clinical studies [2, 3]. The highest bone turnover marker values have previously been reported to occur between 12 and 18 months after the last Dmab injection [2]. For our analysis, we selected serum samples around these time points.
Bisphosphonates are potent inhibitors of bone resorption, with biological effects lasting much longer that their period of administration. This is particularly true for alendronate and zoledronate, for which decreased bone turnover has been found at least 5 years after treatment discontinuation, as assessed by either biochemical markers or bone biopsies [11, 12]. The duration of biological activity of those agents is still unknown, although pamidronate has been found in the circulation even 7 years after the last BP injection [13]. Under these conditions, it could be expected that the increase of bone turnover occurring after Dmab discontinuation, which is explained by a synchronous restoration of all bone remodeling units following the withdrawal of RANK Ligand inhibition, could be blunted or even fully prevented by prior long-acting BP treatment. Our observation is compatible with this hypothesis. In particular, the subgroup of patients previously treated with BPs showed similarly low serum CTX values before and after Dmab, suggesting that the bone turnover increase was prevented. Surprisingly though, we observed a lack of higher values even in a patient who had been exposed to alendronate 14 years before denosumab. In this case, the BP may have been stored in the bone matrix below the surface. It remains possible however that even in this case, the reactivation of bone resorption by newly formed osteoclasts once Dmab is discontinued has eroded the bone surface and released alendronate to the bone-resorbing cells, thus preventing their action to be initiated. Multiple vertebral fractures after Dmab cessation have been reported through sporadic cases or post hoc analysis, which might be a consequence of a rapid increase in bone turnover [5,6,7,8,9]. In this case, our data may suggest that bone fragility in patients discontinuing Dmab might be less in those previously treated with bisphosphonates. In contrast, those who were poorly compliant with BPs or had received ibandronate, which has a time-limited effect on bone resorption [15], did show elevated CTX values.
This observation suffers some limitations. It is retrospective, describes a limited number of heterogeneous patients attending an outpatient clinic, and uses CTX data obtained in various clinical chemistry laboratories. Different assays and the lack of batchwise assessment have likely increased the variability of the determinations. Furthermore, it is based on only one time point and, therefore, does not allow to evaluate the kinetics of CTX changes upon Dmab discontinuation. Finally, without BMD measurements, we could not evaluate the effects of previous exposure to BPs on the rate of bone loss post-Dmab.
In conclusion, higher CTX levels after discontinuation of Dmab therapy were not systematically detected in patients previously treated with long-acting BPs. This observation is likely reflecting the persistent effects of BPs on bone turnover. Larger, prospective studies are needed to eventually confirm this observation and to evaluate the impact of previous BP therapy on post-denosumab bone loss and vertebral fracture risk.
References
Cummings SR, San Martin J, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Miller PD, Bolognese MA, Lewiecki EM et al (2008) Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone 43:222–229
Brown JP, Roux C, Törring O et al (2013) Discontinuation of denosumab and associated fracture incidence: analysis from the fracture reduction evaluation of denosumab in osteoporosis every 6 months (FREEDOM) trial. J Bone Miner Res 28:746–752
McClung MR, Wagman RB, Miller PD et al (2017) Observations following discontinuation of long-term denosumab therapy. Osteoporos Int. doi:10.1007/s00198-017-3919-1
Aubry-Rozier B, Gonzalez-Rodriguez E, Stoll D et al (2016) Severe spontaneous vertebral fractures after denosumab discontinuation: three case reports. Osteoporos Int 27:1923–1925
Popp AW, Zysset PK, Lippuner K (2016) Rebound-associated vertebral fractures after discontinuation of denosumab—from clinic and biomechanics. Osteoporos Int 27:1917–1921
Anastasilakis AD, Makras P (2016) Multiple clinical vertebral fractures following denosumab discontinuation. Osteoporos Int 27:1929–1930
Lamy O, Gonzalez-Rodriguez E, Stoll D et al (2016) Severe rebound-associated vertebral fractures after denosumab discontinuation: nine clinical cases report. J Clin Endocrinol Metab. doi:10.1210/jc.2016-3170
Anastasilakis AD, Polyzos SA, Makras P et al (2017) Clinical features of 24 patients with rebound-associated vertebral fractures following denosumab discontinuation: systematic review and additional cases. J Bone Miner Res. doi:10.1002/jbmr.3110
Brown JP, Ferrari S, Gilchrist N. Discontinuation of denosumab and associated fracture incidence: analysis from FREEDOM and its extension. ASBMR, Atlanta 16–19 sept 2016, abstract 1100
Black DM, Schwarz AV, Ensrud KE et al (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–2938
Black DM, Reid IR, Cauley JA et al (2015) The effects of 6 versus 9 years of zoledronic acid treatment in osteoporosis: a randomized second extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 30:934–944
Papapoulos SE, Cremers S (2007) Prolonged bisphosphonate release after treatment in children. N Engl J Med 356:1075–1076
Bekker PJ, Holloway DL, Rasmussen AS et al (2004) A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res 19:1059–1066
Thiebaud D, Burckhardt P, Kriegbaum H et al (1997) Three monthly intravenous injections of ibandronate in the treatment of postmenopausal osteoporosis. Am J Med 103:298–307
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
BU received consulting fees from Amgen, Eli Lilly, and MSD. RR received fees for advisory board or lectures from Danone, Labatec, Nestlé, ObsEva, and Radius Health. SF received consulting fees from Agnovos, Amgen, Eli Lilly, MSD, Radius Health, and UCB.
Rights and permissions
About this article
Cite this article
Uebelhart, B., Rizzoli, R. & Ferrari, S.L. Retrospective evaluation of serum CTX levels after denosumab discontinuation in patients with or without prior exposure to bisphosphonates. Osteoporos Int 28, 2701–2705 (2017). https://doi.org/10.1007/s00198-017-4080-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4080-6