Abstract
Multiple endocrine neoplasia type 1 (MEN1) is a hereditary syndrome predisposing to many endocrine and neuroendocrine tumors (NET). Conventional imaging (CI) cannot provide satisfactory results for all the different types of MEN1-related tumors. Objective of this prospective observational study was to evaluate the role of 68Ga-DOTATATE PET/CT in MEN1 compared to CI. Diagnostic performance of 68Ga-DOTATATE PET/CT for the detection of NET was evaluated as well as the prognostic role of SUVmax. Eighteen patients with genetically confirmed MEN1 were evaluated by 68Ga-DOTATATE PET/CT, endoscopic ultrasounds, multidetector-row computed tomography, magnetic resonance imaging, and hormone/markers serum measurements. Four MEN1-related tumor sites (pancreas, pituitary, parathyroids, adrenals) were considered. Sensitivity and specificity of 68Ga-DOTATATE PET/CT for the detection of NET were calculated. There was 68Ga-DOTATATE PET/CT uptake in 11/11 patients with pancreatic lesions, in 9/12 with pituitary adenoma, in 5/15 with parathyroid enlargements, and in 5/7 with adrenal lesions. 68Ga-DOTATATE PET/CT showed sensitivity and specificity of 100 and 100 % in pancreas, 75 and 83 % in pituitary, 28 and 100 % in parathyroids, and 62.5 and 100 % in adrenals, respectively. Compared with CI, no significant difference in sensitivity for pancreas, pituitary, and adrenals was found, while CI had a better sensitivity for parathyroids (p = 0.002). On the ROC analysis, progression of pancreatic lesions was significantly associated to SUVmax <12.3 (p < 0.05). 68Ga-DOTATATE PET/CT is greatly helpful in the work-up of MEN1 providing a panoramic view of MEN1-related lesions. There is also a prognostic role of 68Ga-PET in patients with MEN1-pancreatic lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multiple endocrine neoplasia type 1 (MEN1) is a rare, hereditary syndrome, [1]. Nowadays, the diagnosis of MEN1 is frequently achieved in asymptomatic subjects through the familial genetic screenings [2]. This implies a gradual change in the management of these patients. The available imaging armamentarium offers a wide range of techniques useful to achieve an early diagnosis of MEN1 tumors, although it does not exist a unique and well-established diagnostic path. Color doppler ultrasonography (US), contrast-enhanced computed tomography (CT), and contrast-enhanced magnetic resonance imaging (MRI) cannot always provide satisfactory results in diagnosing all different types of MEN1-related tumors, being the rate of detection negatively influenced by lesions smaller than 10 mm [3]. Endoscopic US (EUS) is one of the most valuable diagnostic tool in pancreatic NET (pNET) with sensitivity up to 90 %, even for lesions <10 mm. However, EUS has less efficacy in detecting small lesions in the tail, it is considered invasive, strongly operator dependent, and its accuracy is not reproducible in all centers [4]. 111In-DTPA-octreotide scintigraphy (SRS), successfully used in clinics for staging and follow-up of NET, has variable sensitivity depending on the density and type of expressed somatostatin receptors (SSTRs) on tumor cell surface and size of the lesions [5]. SRS is considered the gold standard in diagnosis and staging of NET. In genetically confirmed MEN1 patients, SRS showed a low sensitivity for detecting primary small tumors but resulted as the test of choice in metastatic disease. 68Ga PET/CT labeled with somatostatin analog peptides showed greater sensitivities than SRS in the management of NET [6–8]. Such significant improvement is related to higher binding affinities of the PET ligands for SSTR-2, -3, -5, higher spatial resolution, which allow detection of tumors <10 mm with better target-to-background ratios [9–11]. Recently, an overall sensitivity/specificity of 91.7/93.5 % of 68Ga-DOTATOC PET/CT for detecting NET lesions in MEN syndromes has been reported [12]. However, it has not been previously investigated the role of 68Ga PET/CT in MEN1 patients pointing attention on each of the main anatomical sites involved in the syndrome.
The aim of this prospective observational study was to evaluate the diagnostic performance and the prognostic role of 68Ga-DOTATATE PET/CT (GaTate) in subjects with MEN1.
Patients and methods
Patients
All consecutive patients with genetic diagnosis of MEN1 between 2008 and 2011 followed at the University of Naples Federico II were included in this study. These patients derived from cascade screening of close biological relatives of patients with MEN1. Eighteen individuals with MEN1 (median age 40 ± 14 years) were identified and included (Table 1). At diagnosis, all patients underwent physical, laboratory, and radiological examination. Timing was in accordance with current guidelines for MEN1 [1]. Four different tumor sites were considered: pancreas, pituitary, parathyroids, and adrenals. Conventional radiological and functional imaging examinations (CI) were as follows: abdominal contrast-enhanced multidetector-row CT, pituitary contrast-enhanced MRI, cervical color Doppler US, duodeno-pancreatic EUS, SRS, 99mTc-sestamibi scintigraphy. Imaging results were validated by surgery and cytology/histology in 9 patients, by clinical follow-up in the remaining 9 cases. Follow-up schedule included clinical, biochemical, and radiological evaluation. Patients’ outcome was evaluated according to RECIST criteria.
GaTate was performed after genetic diagnosis in all patients. The results were then compared to those obtained by CI, considered as gold standard. In some cases, which were CI negative, the presence of specific MEN1 lesions was considered according to the clinical contest (i.e., Zollinger–Ellison syndrome, hyperprolactinemia, primary hyperparathyroidism, adrenal hypersecretion).
Methods
Gallium-68 was eluted from a 68Ge/68Ga generator and radiolabeling was performed as previously reported [13]. For GaTate imaging, 120–220 MBq of activity was administered. The images were acquired 45–60 min post-injection. Imaging was performed using a dedicated GE Discovery 600 camera combining a PET tomograph and a 16-slice multidetector-row CT. PET scans were acquired at a rate of 3 min per bed position; PET images were reconstructed using CT for attenuation correction. Images were corrected for scatter, random, dead time, and count losses and were reconstructed using an iterative image reconstruction method (3 iteration, 16 subset, 5-mm post-filter). PET results were evaluated by two experienced nuclear medicines. The GaTate studies were reviewed for areas of abnormally increased tracer uptake. The pattern of tracer uptake and a semiquantitative parameter [maximum standardized uptake value (SUVmax)] were documented in all lesions. Tracer uptake was correlated with the anatomic extent of tumor. In those patients with multiple positive lesions, the SUVmax was calculated for all lesions. A positive scan was defined as significant accumulation of tracer based on visual assessment by the two observers.
Statistical analysis
The statistical analysis was performed by SPSS for Windows version 20 (SPSS, Inc., Chicago, IL). Data were expressed as mean ± SEM. The comparison between the categorical data was performed by the χ 2 test. Receiver operator characteristic (ROC) curves were used to find a significant SUVmax score cut-offs to predict prognosis. Progression-free survival (PFS) was calculated using the Kaplan–Meier method with log-rank test. The significance was set at 5 %.
Results
Eleven of 18 patients (61 %) had one or more pNET, 12 (67 %) had a pituitary adenoma, 15 (83 %) had primary hyperparathyroidism, and 7 (39 %) had one or both adrenal glands enlarged or harboring lesions (Table 1). In total, 15 pNET, 12 pituitary adenomas, 18 parathyroid lesions (considering 2 cases with biochemical diagnosis but radiologically inapparent), and 8 enlarged adrenals were found. Mean follow-up time was 50.5 months (range 32–70 months). During follow-up, 3 (27 %) out 11 patients with pNET (all non-functioning pNET) progressed after a mean time of 13 months.
There was GaTate uptake in 11/11 patients with pancreatic lesions, in 9/12 with pituitary adenoma, in 5/15 with hyperparathyroidism, and in 5/7 with adrenal lesions. In seven patients, GaTate documented lesions in three out the four considered MEN1 tumor sites, in four patients, lesions were found in two MEN1 tumor sites, and in two patients, lesions were found in only one MEN1 tumor site.
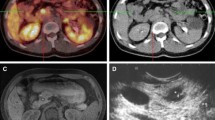
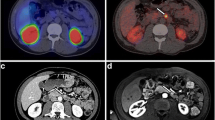
With regard to tumor site, GaTate detected 15 of 15 pNET, 9 of 12 pituitary adenomas, 5 of 18 parathyroid lesions and 5 of 8 adrenal lesions. GaTate showed sensitivity and specificity of 100 and 100 % in pancreas, 75 and 83 % in pituitary, 28 and 100 % in parathyroids, and 62.5 and 100 % in adrenals, respectively. By comparing GaTate and CI results, CI had a better significant sensitivity for parathyroids (p = 0.002). No significant difference for pNET (p = 1.000), pituitary (p = 0.584), and adrenal lesions (p = 0.564) was observed. Specificity was not significantly different. To note, in a patient, a pNET of the tail was not initially detected with CI (both EUS and CT), but it was retrospectively displayed after image revision of contrast-enhanced multidetector-row CT on the basis of the GaTate result (Fig. 1).
Patient with pancreatic neuroendocrine tumors: a lesion in pancreatic body at 68Ga-DOTATATE PET/CT (a) and contrast-enhanced multidetector-row computed tomography (b); a lesion in pancreatic tail at 68Ga-DOTATATE PET/CT (c) and contrast-enhanced multidetector-row computed tomography (d) (Patient 14)
Among the GaTate-positive/CI-negative cases, clinical context confirmed the presence of a true tumor lesion in the parathyroids (primary hyperparathyroidism) and in one of the two pituitary lesions (hyperprolactinemia).
SUVmax ranged from 3.9 to 85.8. The mean SUVmax was 28 ± 23 in pNET, 9.9 ± 2.4 in pituitary adenomas, 7.5 ± 7.3 in parathyroid enlargements, and 19.8 ± 10.3 in adrenal lesions. In pituitary adenomas, by the adoption of a SUVmax threshold of 2.9, in nine patients, the uptake was classified as “pathological” and was in agreement with MRI results or clinical context; in one case, the elevated uptake was classified as a false positive. In pNET, a significant cut-off of SUVmax (12.3) was found on the ROC analysis according to progression (area under the curve: 0.03; SE = 0.045; p = 0.016). Median PFS was 14 months in pNET with SUVmax <12.3, while it was not reached in pNET with SUVmax >12.3 (p = 0.009).
Discussion
SRS is currently the accepted gold standard for the nuclear medicine diagnosis of SSTR-positive NET [14]. However, 68Ga-radiolabeled somatostatin analogs seems to improve diagnosis, therapy monitoring, and follow-up [15].
Recently, detection of pNET, parathyroid and pituitary adenoma by GaTate in a MEN1 patient has been reported [16]. 68Ga-DOTATOC PET/CT overall sensitivity/specificity was 91.7/93.5 % for detecting NET lesions in a retrospective study including 19 MEN1 patients [12]. These results are not comparable with those reported in the current study firstly because of the different radiotracer and study design, secondly because Froelig study evaluated patients in different stage of disease and did not describe pituitary and adrenal lesions. The current study prospectively enrolled a homogeneous population of patients newly diagnosed as MEN1 through the genetic screening. Finally, all main sites of MEN1-related tumors were systematically investigated.
In MEN1 patients, early diagnosis of pNET is crucial. The sensitivity of preoperative assessment of MEN1-related pNET was reported to be 81 % for CT, 88 % for MRI, and 84 % for SRS [17]. Recently, EUS has shown excellent sensitivity in pNET, also in tumors too small to be detected with CT or MRI [18, 19]. However, it has been reported a not negligible percentage of significant size lesions (≥10 mm) which are not detected not only at MRI but also at EUS. This finding could be explained by the difficulty to explore the pancreas tail by EUS and by the fact that some tumors can be isoechogenic with the pancreas [20]. So multidetector-row CT and EUS need to be both performed to identify all pNET in MEN1 patients [21]. In the current study, a pNET, localized in the tail, initially not recognized on CT and EUS, was displayed at CT after images revision guided by the results of the GaTate. To note, no patient in this series had pNET in the uncinate process of pancreas, a region in which there is a physiological high 68Ga-DOTATATE uptake and where EUS is well established to be the imaging technique of choice.
Contrast-enhanced MRI, in particular dynamic-MRI, is the investigation of choice for the evaluation of pituitary adenomas with a sensitivity and specificity of 89 % each [22]. Pituitary gland and pituitary adenomas are known to express SSTR. However, contribute of SRS in the diagnosis of pituitary tumors is very limited, particularly in microadenomas. No study is available demonstrating the utility of GaTate for such tumors in MEN1, but a clinical case [23]. In our experience, GaTate achieved a sensitivity of 75 % and a specificity of 83 %, resulting in similar diagnostic performance as compared to MRI in diagnosis of pituitary lesions.
The overall sensitivity and specificity of cervical color doppler US in the diagnosis of parathyroid adenoma have been reported as 97 and 100 %, respectively [24]. However, it is less clear that the value of cervical color Doppler US and sestamibi in MEN1-related hyperparathyroidism can be due to asymmetric and multigland enlargement or parathyroid tumors. Similarly to findings from the Froeling study [12], 68Ga PET/CT sensitivity was poor (28 %) in the current study, with high rate of false negative. This is likely to be explained by scarce or no expression of SSTR in these lesions [25].
GaTate had lower but not significantly different sensitivity than CI in detection of MEN1-related adrenal lesions. Besides, because of the high physiological uptake of 68Ga-labeled somatostatin analogs in the adrenal gland (average SUVmax 6), this imaging technique is not considered of choice for the detection of adrenal abnormalities.
In conclusion, in MEN1, GaTate provides a panoramic view of lesions within pancreas, pituitary, and adrenals, producing the same information that a combination of different CI techniques could show. Less sensitivity is found for detection of parathyroid lesions which are much better visualized by CI. Although the higher cost of this procedure than SRS, GaTate shows peculiar advantages in terms of radiation dose to the patient and reduction of the length of the exam. For all these reasons, GaTate may guide the initial work-up in MEN1 carriers. However, this point needs to be better clarified in further studies. At the present, it could be reasonable to perform 68Ga PET/CT as functional imaging instead of SRS using the same timing, according to guidelines [1]. In patients with pNET with 68Ga-DOTATATE SUVmax <12.3, an aggressive course is expected regardless from the size. To definitely answer the question if GaTate is convenient/appropriate in MEN1 patients, general conclusions cannot be drawn because the limited number of patients in this series and new prospective studies have to be performed.
References
R.V. Thakker, P.J. Newey, G.V. Walls, J. Bilezikian, H. Dralle, P.R. Ebeling, S. Melmed, A. Sakurai, F. Tonelli, M.L. Brandi, Endocrine society: clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J. Clin. Endocrinol. Metab. 97, 2990–3011 (2012)
V. Ramundo, F. Milone, R. Severino, S. Savastano, C. Di Somma, L. Vuolo, L. De Luca, G. Lombardi, A. Colao, A. Faggiano, Clinical and prognostic implications of the genetic diagnosis of hereditary NET syndromes in asymptomatic patients. Horm. Metab. Res. 43, 794–800 (2011)
M. Imamura, Recent standardization of treatment strategy for pancreatic neuroendocrine tumors. World J. Gastroenterol. 16, 4519–4525 (2010)
R.B. Lewis, G.E. Lattin Jr, E. Paal, Pancreatic endocrine tumors: radiologic-clinicopathologic correlation. Radiographics 30, 1445–1464 (2010)
E.P. Krenning, D.J. Kwekkeboom, W.H. Bakker, W.A. Breeman, P.P. Kooij, H.Y. Oei, M. van Hagen, P.T. Postema, M. de Jong, J.C. Reubi et al., Somatostatin receptor scintigraphy with [111In-DTPA-D-Phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur. J. Nucl. Med. 20, 716–731 (1993)
M. Hofmann, H. Maecke, R. Börner, E. Weckesser, P. Schöffski, L. Oei, J. Schumacher, M. Henze, A. Heppeler, J. Meyer, H. Knapp, Biokinetics and imaging with the somatostatin receptor PET radioligand (68)Ga-DOTATOC: preliminary data. Eur. J. Nucl. Med. 28, 1751–1757 (2001)
I. Kayani, J.B. Bomanji, A. Groves, G. Conway, S. Gacinovic, T. Win, J. Dickson, M. Caplin, P.J. Ell, Functional imaging of neuroendocrine tumors with combined PET/CT using 68Ga-DOTATATE (DOTA-DPhe1, Tyr3-octreotate) and 18F-FDG. Cancer 112, 2447–2455 (2008)
I. Virgolini, V. Ambrosini, J.B. Bomanji, R.P. Baum, S. Fanti, M. Gabriel, N.D. Papathanasiou, G. Pepe, W. Oyen, C. De Cristoforo, A. Chiti, Procedure guidelines for PET/CT tumor imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. Eur. J. Nucl. Med. Mol. Imaging 37, 2004–2010 (2010)
A. Al-Nahhas, Z. Win, T. Szyszko, A. Singh, C. Nanni, S. Fanti, D. Rubello, Gallium-68 PET: a new frontier in receptor cancer imaging. Anticancer Res. 27, 4087–4094 (2007)
M. Ginj, J. Chen, M.A. Walter, V. Eltschinger, J.C. Reubi, H.R. Maecke, Preclinical evaluation of new and highly potent analogues of octreotide for predictive imaging and targeted radiotherapy. Clin. Cancer. Res. 11, 1136–1145 (2005)
D. Wild, J.S. Schmitt, M. Ginj, H.R. Mäcke, B.F. Bernard, E. Krenning, M. De Jong, S. Wenger, J.C. Reubi, DOTA-NOC, a high-affinity ligand of somatostatin receptor subtypes 2, 3 and 5 for labelling with various radiometals. Eur. J. Nucl. Med. Mol. Imaging 30, 1338–1347 (2003)
V. Froeling, F. Elgeti, M.H. Maurer, C. Scheurig-Muenkler, A. Beck, T.J. Kroencke, U.F. Pape, B. Hamm, W. Brenner, N.F. Schreiter, Impact of Ga-68 DOTATOC PET/CT on the diagnosis and treatment of patients with multiple endocrine neoplasia. Ann. Nucl. Med. 26, 738–743 (2012)
M.S. Hofman, G. Kong, O.C. Neels, P. Eu, E. Hong, R.J. Hicks, High management impact of Ga-68 DOTATATE (GaTate) PET/CT for imaging neuroendocrine and other somatostatin expressing tumours. J. Med. Imaging. Radiat. Oncol. 56, 40–47 (2012)
D.J. Kwekkeboom, P.P. Kooij, W.H. Bakker, H.R. Mäcke, E.P. Krenning, Comparison of 111In-DOTA-Tyr3-octreotide and 111In-DTPA-octreotide in the same patients: biodistribution, kinetics, organ and tumor uptake. J. Nucl. Med. 40, 762–767 (1999)
C. Wehrmann, S. Senftleben, C. Zachert, D. Müller, R.P. Baum, Results of individual patient dosimetry in peptide receptor radionuclide therapy with 177Lu DOTA-TATE and 177Lu DOTA-NOC. Cancer Biother. Radiopharm. 22, 406–416 (2007)
S. Kumar Gupta, S. Singla, N.A. Damle, K. Agarwal, C. Bal, Diagnosis of Men-I syndrome on (68)Ga-DOTANOC PET-CT and role of peptide receptor radionuclide therapy with (177)Lu-DOTATATE. Int. J Endocrinol. Metab. 10, 629–633 (2012)
M.A. Lewis, G.B. Thompson, W.F. Young Jr, Preoperative assessment of the pancreas in multiple endocrine neoplasia type 1. World J. Surg. 36, 1375–1381 (2012)
A. McLean, Endoscopic ultrasound in the detection of pancreatic islet cell tumors. Cancer Imaging 4, 84–91 (2004)
S. Philips, S.N. Shah, R. Vikram, S. Verma, A.K. Shanbhogue, S.R. Prasad, Pancreatic endocrine neoplasms: a current update on genetics and imaging. Br. J. Radiol. 85, 682–696 (2012)
C. Barbe, A. Murat, B. Dupas, P. Ruszniewski, A. Tabarin, M.P. Vullierme, A. Penfornis, V. Rohmer, E. Baudin, M. Le Rhun, D. Gaye, C. Marcus, G. Cadiot, Groupe d’étude des Tumeurs Endocrines (GTE), Magnetic resonance imaging versus endoscopic ultrasonography for the detection of pancreatic tumors in multiple endocrine neoplasia type 1. Dig. Liver. Dis. 44, 228–234 (2012)
L. Camera, S. Paoletta, C. Mollica, F. Milone, V. Napolitano, L. De Luca, A. Faggiano, A. Colao, M. Salvatore, Screening of pancreaticoduodenal endocrine tumors in patients with MEN 1: multidetector-row computed tomography vs. endoscopic ultrasound. Radiol. Med. 116, 595–606 (2011)
R. Gao, H. Isoda, T. Tanaka, S. Inagawa, H. Takeda, Y. Takehara, S. Isogai, H. Sakahara, Dynamic gadolinium-enhanced MR imaging of pituitary adenomas: usefulness of sequential sagittal and coronal plane images. Eur. J. Radiol. 39, 139–146 (2001)
N. Naswa, C.J. Das, P. Sharma, S. Karunanithi, C. Bal, R. Kumar, Ectopic pituitary adenoma with empty sella in the setting of MEN-1 syndrome: detection with 68Ga-DOTANOC PET/CT. Jpn. J. Radiol. 30, 783–786 (2012)
S. Piciucchi, D. Barone, G. Gavelli, A. Dubini, D. Oboldi, F. Matteuci, Primary hyperparathyroidism: imaging to pathology. J. Clin. Imaging Sci. 2, 59 (2012)
A. Faggiano, L.B. Tavares, L. Tauchmanova, F. Milone, G. Mansueto, V. Ramundo, M.L. De Caro, G. Lombardi, G. De Rosa, A. Colao, Effect of treatment with depot somatostatin analogue octreotide on primary hyperparathyroidism (PHP) in multiple endocrine neoplasia type 1 (MEN1) patients. Clin. Endocrinol. 69, 756–762 (2008)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Secondo Lastoria and Francesca Marciello have equally contributed to the article.
On the behalf of the Multidisciplinary Group for Neuroendocrine Tumors of Naples.
Rights and permissions
About this article
Cite this article
Lastoria, S., Marciello, F., Faggiano, A. et al. Role of 68Ga-DOTATATE PET/CT in patients with multiple endocrine neoplasia type 1 (MEN1). Endocrine 52, 488–494 (2016). https://doi.org/10.1007/s12020-015-0702-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0702-y