Abstract
Hyperglycemic crisis episodes (HCEs)—diabetic ketoacidosis and the hyperosmolar hyperglycemic state—are the most serious acute metabolic complications of diabetes. We aimed to investigate the subsequent mortality after HCE in the non-elderly diabetic which is still unclear. This retrospective national population-based cohort study reviewed, in Taiwan’s National Health Insurance Research Database, data from 23,079 non-elder patients (≤65 years) with new-onset diabetes between 2000 and 2002: 7693 patients with HCE and 15,386 patients without HCE (1:2). Both groups were compared, and follow-up prognoses were done until 2011. One thousand eighty-five (14.1 %) patients with HCE and 725 (4.71 %) patients without HCE died (P < 0.0001) during follow-up. Incidence rate ratios (IRR) of mortality were 3.24 times higher in patients with HCE than in patients without HCE (P < 0.0001). Individual analysis of diabetic ketoacidosis and hyperosmolar hyperglycemic state also showed the similar result with combination of both. After stratification by age, mortality was significant higher in the middle age (40–64 years) [IRR 3.29; 95 % confidence interval (CI) 2.98–3.64] and young adult (18–39 years) (IRR 3.91; 95 % CI 3.28–4.66), but not in the pediatric subgroup (<18 years) (IRR 1.28; 95 % CI 0.21–7.64). The mortality risk was highest in the first month (IRR 54.43; 95 % CI 27.98–105.89), and still high after 8 years (IRR 2.05; 95 % CI 1.55–2.71). After adjusting for age, gender, and selected comorbidities, the mortality hazard ratio for patients with HCE was still four times higher than for patients without HCE. Moreover, older age, male gender, stroke, cancer, chronic obstructive pulmonary disease, congestive heart failure, and liver disease were independent mortality predictors. HCE significantly increases the subsequent mortality risk in the non-elderly with diabetes. Strategies for prevention and control of comorbidities are needed as soon as possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperglycemic crises—diabetic ketoacidosis (DKA) and the hyperosmolar hyperglycemic state (HHS)—are the two most serious acute metabolic complications of diabetes [1]. The basic underlying mechanism is the combination of absolute or relative insulin deficiency and an increase in counter regulatory hormones, viz., glucagon, catecholamines, cortisol, and growth hormone [1]. Despite recent improvements, the incidence and the cost of treating hyperglycemic crises are high and continue to rise. In the United States, the National Diabetes Surveillance Program of the Centers for Disease Control and Prevention estimated that from 1988 to 2009, the age-adjusted hospital discharge rate for DKA per 10,000 population consistently increased by 43.8 %, so the number of hospital discharges with DKA as the first-listed diagnosis increased from about 80,000 in 1988 to about 140,000 in 2009 [2]. DKA is responsible for more than 500,000 hospital days per year [3, 4] at an estimated annual direct medical expense and indirect cost of 2.4 billion USD [4, 5]. The incidence of and medical expenditure for HHS care are unknown because there are few population-based studies on the HHS, and because many patients with HHS have multiple comorbidities. The rate of hospital admissions for HHS was estimated more than a decade ago to be 1 % of all primary admissions for diabetes [6].
Because of improved awareness, prevention, and treatment guidelines, the age-adjusted death rate for hyperglycemic crises in 2009 was less than half the rate in 1980 (7.5 vs. 15.3 per 1000,000 population); however, hyperglycemic crises still caused 2417 deaths in 2009 in the United States [3]. The mortality rate for DKA is 1–9 %, for HHS is 5–45 % [1, 7, 8], and for overall hyperglycemic crises is 10.5 % [9]. Among the elderly (≥65 years old), the mortality rate was reported to be as high as 71 % [10]. Regardless of the observed decrease in the death rate in the United States, hyperglycemic crises remain a serious health problem, especially in developing and undeveloped countries [10]. The cause of death in patients with hyperglycemic crises is rarely ascribed to the metabolic complications of hyperglycemia or ketoacidosis; rather, it is usually related to the underlying precipitating illness [9, 11–13].
Almost all studies on hyperglycemic crises have focused on acute episodes [7–9, 11–14]. In 2013, Huang et al. [9] proposed predicting the hyperglycemic crisis death (PHD) score to help emergency and critical care. The PHD score consists of six factors: Absent tachycardia, Hypotension, Anemia, Severe coma, Cancer history, and Infection (Mnemonic: AHA.SCI) which are used to predict 30-day mortality and manage, in the Emergency Department, adult patients with hyperglycemic crises. Poor compliance (i.e., uncontrolled diabetes) is the most common precipitating factor of hyperglycemic crises, which suggests that close follow-up and secondary prevention after an HCE are crucial [9]. The long-term effect of uncontrolled diabetes contributes to various complications, including death [1]. A study showed that geriatric patients (≥65 years) with diabetes had a higher mortality risk after HCE during the first 6 years of follow-up [15]. However, the subsequent mortality of the non-elderly (<65 years) after HCE has never been clarified. To determine the subsequent mortality of non-elderly patients with HCE, we wanted to analyze a population-based cohort taken from Taiwan’s National Health Insurance Research Database (NHIRD).
Methods
Data sources
The Taiwan NHI Program, a universal health care system that covers 99 % of the country’s population of 23.3 million [16], has one of the largest and most complete population-based healthcare claims datasets in the world. The NHIRD contains encrypted patient identification numbers, ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes for applied clinical diagnoses and procedures, details of prescribed drugs, dates of admission and discharge, and basic sociodemographic information, including gender and date of birth. All the expenses of HCE therapy are covered by NHI (but not hospital room and board). Data used in this study came from two sub-datasets of the NHIRD. The HCE group data were obtained from the longitudinal cohort of diabetes patients (LHDB), which contains randomized selected data (120,000 patients/per year) from patients with newly diagnosed diabetes mellitus (DM). The definitions of DM in the LHDB are (a) Inpatient: at least one diagnosis of DM or a prescription for antidiabetes medication; (b) Ambulatory care: at least two diagnoses of DM or at least one diagnosis of DM with a prescription for antidiabetes medication. The comparison group (without HCE) data were obtained from the Longitudinal Health Insurance Database 2000 (LHID2000), a sub-dataset of the NHIRD, which contains all claims data of one million (4.34 % of the total population) beneficiaries who were randomly selected in 2000. There are no significant differences in age, gender, or health care costs between the sample group and all NHI enrollees.
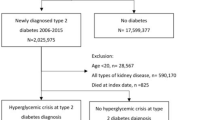
Design
In this longitudinal cohort study, we selected all non-elderly patients (<65 years) in the LHDB who had been diagnosed with HCE (ICD-9 code: DKA 250.1 or HHS 250.2) between January 1, 2000, and December 31, 2002. The comparisons (2 patients with a diagnosis of DM without HCE for every patient with HCE) were randomly selected from the LHID2000. The index date in the HCE group was the date that HCE was first diagnosed in the database; the index date in the comparison group corresponded with the index date of the HCE group. Data from patients who died between the DM diagnosis date and the HCE index date in both groups were deleted. The comparisons were matched with the patients with HCE by gender, age at which DM was diagnosed (±30 days), duration between DM diagnosis date to HCE index date, and selected comorbidities by propensity score. Figure 1 shows the flowchart of this study.
We linked to the diagnostic codes through the inpatient and ambulatory care claims databases of the NHI. Our data collection included not only the patients’ survival status, but also their date of death, demographics, and baseline comorbidities. Baseline comorbidities affecting mortality that may have presented before the index date were defined as follows: hypertension (HTN) (ICD-9 codes 401–405), renal disease (ICD-9 codes 582, 583, 585, 586, 588), coronary artery disease (CAD) (ICD-9 codes 410–414), stroke (ICD-9 codes 430–438), cancer (ICD-9 codes 140–208), chronic obstructive pulmonary disease (COPD) (ICD-9 codes 490–496, 500–505, 5064), congestive heart failure (CHF) (ICD-9 codes 428), and liver disease (ICD-9 codes 5712, 5714, 5715, 5716, 4560–4562, 5722–5728). We counted these comorbid conditions if they occurred either in the inpatient setting or in 3 or more ambulatory care claims coded before the index medical care date. Patients were followed from the index date to the date of death or December 31, 2011, the end of the database period. According to the law, enrollment NHI is mandatory for all citizens and other legal residents of Taiwan, and it must be withdrawn within 30 days after death. Therefore, those patients recorded as deceased in the inpatient claim or as withdrawing their NHI enrollment within 30 days after being discharged from their last hospitalization were presumed dead, and the discharge date was designated as the date of death. This study was conducted according to the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) at Chi-Mei Medical Center. The IRB waived the need for informed consents (written and oral) from the patients because the dataset used in this study consists of nationwide, unidentifiable, secondary data released to the public for research purposes. This waiver does not adversely affect the rights and welfare of the patients.
Statistical analysis
The significance of the differences in baseline characteristics and comorbid variables between the two cohorts was evaluated using Student’s t test for continuous variables and Pearson χ 2 tests for categorical variables. The risk of death between patients in the HCE and comparison groups was compared by estimating the incidence rate ratio (IRR) with Poisson regression. Kaplan–Meier analysis was used to calculate the cumulative survival rate between different age groups in the 2 cohorts, and the log-rank test was used to analyze the differences between the survival curves. Thereafter, separate Cox proportional hazard regressions were done to compute the risk of death between the HCE and comparison groups after adjusting for possible confounding factors. SAS for Windows 9.3.1 (SAS Institute, Inc, Cary, NC, USA) was used for all analyses. Significance was set at P < 0.05.
Results
Demographic data
Between 2000 and 2002, we recruited 7693 patients with HCE and 15,386 age-, gender-, and selected comorbidities-matched comparisons, after ineligible patients had been excluded. The mean age in the HCE group at the DM date was 45.60 ± 10.86 years and of the comparison group was 45.66 ± 10.86 years. We classified these patients into three age subgroups: 0–17 years old (pediatric), 18–39 years old (young adult), and 40–64 years old (middle age). Pearson χ 2 tests revealed no significant difference between to the distribution of the comorbidities of HTN, renal disease, CAD, stroke, cancer, COPD, CHF, and liver disease in patients with HCE and comparisons after matching (Table 1).
Incidence rates of mortality
Of the 23,079 patients recruited, 1810 (7.84 %) died during the follow-up period: 1085 of 7693 patients with HCE (14.1 %) and 725 of 15,386 comparisons (4.71 %) (Table 2). The incidence rates of mortality were 21.59 (HCE group) and 6.61 (comparison group) per 1000 person-years (PY), which was significantly higher for the HCE group (IRR 3.24; 95 % CI 2.94–3.55) (Table 2).
The mortality risk was significantly higher in the HCE group during the entire follow-up period: first month after HCE (IRR 54.43; 95 % CI 27.98–105.89), 1–6 months after (IRR 4.85; 95 % CI 3.39–6.94), 6–12 months after (IRR 3.96; 95 % CI 2.78–5.64), 1–2 years after (IRR 3.66; 95 % CI 2.79–4.80), 2–4 years after (IRR 2.27; 95 % CI 1.84–2.81), 4–6 years after (IRR 1.72; 95 % CI 1.35–2.18), 6–8 years after (IRR 2.21; 95 % CI 1.70–2.86), and ≥8 years after (IRR 2.05; 95 % CI 1.55–2.71) (Table 2). Individual analysis of DKA (Table 3) and HHS (Table 4) was also performed, which showed significantly increased mortality, similar results with the combination of both.
Kaplan–Meier survival analyses and log-rank tests showed that patients in the HCE group (subclassified into HCE ≥2 and HCE = 1) had significantly (P < 0.0001) lower survival rates than did comparisons during the follow-up period (Fig. 2). Subsequent mortality in patients with HCE ≥2 was significantly higher than patients with HCE = 1 and patients without HCE (Fig. 2).
HCE age subgroups of middle age (IRR 3.29; 95 % CI 2.98–3.64) and young adult (IRR 3.91; 95 % CI 3.28–4.66) had a higher IRR than did their comparison group counterparts, however, pediatric age subgroup did not (IRR 1.28; 95 % CI 0.21–7.64) (Table 2).
Male patients with HCE had a mortality rate of 24.31/1000 PY, whereas male comparisons had a death rate of only 7.99 per 1000 PY (IRR 3.01; 95 % CI 2.69–3.37) (Table 2). The difference between female patients with HCE and female comparisons was also significant (IRR 3.91; 95 % CI 3.28–4.66).
Patients with HCE comorbid with HTN (23.72/1000 PY), CAD (28.22/1000 PY), stroke (52.63/1000 PY), cancer (130.63/1000 PY), COPD (34.67/1000 PY), CHF (83.57/1000 PY), and those comorbid with a liver disease (54.99/1000 PY) had a higher IRR for mortality than did comparisons comorbid with the same diseases (Table 2).
Risk factors for all-cause mortality in DM patients
Cox proportional hazard regressions were used to determine crude and adjusted hazard ratios (HRs) for mortality during the follow-up period by cohort for the total sample. After adjusting for patient age, gender, and selected comorbidities, HCE (HCE ≥2, adjusted HR 3.29, 95 % CI 2.98–3.63; HCE = 1, adjusted HR 4.64, 95 % CI 3.92–5.49) was still an independent risk factor for mortality in the total sample (Table 5). Other risk factors for mortality included older age (≥18 years old), male gender, renal disease, stroke, cancer, COPD, CHF, and liver disease.
Discussion
Our study analyzed follow-up claim data on 7693 HCE patients and 15,386 comparison patients. Our results suggest that HCE raises the risk of subsequent mortality. This present study found that the incidence rate of mortality was significantly high during the entire follow-up period after HCE. The risks of mortality were 54.43, 4.85, 3.96, 3.66, 2.27, 1.72, 2.21, and 2.05 times higher in the HCE group than in the comparison group during the first 1 month after HCE, the first 6 months after, 6–12 months after, 1–2 years after, 2–4 years after, 4–6 years after, 6–8 years after, and ≥8 years. In the age subgroups, HCE patients of middle age and young adult had a higher mortality than comparisons, but not in the pediatric subgroup. Individual analysis of DKA and HHS also showed the similar result with combination of both. After adjusting for potential confounding factors, the risk of mortality associated with HCE was still near four times that of patients without HCE. Early referral of patients with HCE for proper patient education, better access to medical care, effective communication with a health care provider during an intercurrent (occurring during and modifying the course of another disease) illness [1], and secondary prevention of mortality, such as controlling renal disease, stroke, cancer, COPD, CHF, and liver disease, may be done as soon as possible.
The most common precipitating factor of HCE is poor compliance [1, 9]. A recent study [13] reported that the mean glycosylated hemoglobin (HbA1c) of patients with HCE was 11.8 %; therefore, the occurrence of HCE indicated uncontrolled diabetes, which may have long-term effects that contribute to various complications such as renal disease, CAD, and stroke [1]. Even more, uncontrolled diabetes is associated with all-cause mortality and cardiovascular mortality [17]. Resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs [1]. Recent studies suggest that any type of education for nutrition has resulted in reduced hospitalization [18]. In fact, the guidelines for diabetes self-management education were developed by a recent task force to identify ten detailed standards for diabetes self-management education [19].
Older age is an independent mortality predictor in the total sample. In the pediatric population, HCE patients did not have a higher mortality. However, it does not suggest that HCE did not increase the subsequent mortality in the pediatric population. The mortality number in HCE patients and comparisons was too few (2 and 3, respectively) which may cause statistically insignificant (Table 2). Other explanations for the lower mortality in the pediatric population are that more than half of children got HCE as the initial diagnosis of DM [20] and adult HCE were always due to poor compliance, infection, and long-term DM [9]. It needs further study with more number to clarify this issue.
The present study showed that cancer patients with comorbid DM who also had HCE had higher all-cause mortality than did comparisons. CLUE II (Give Us a Clue to Cancer and Heart Disease), a recent community-based, prospective study [21] provides support for the association between cancer and DM. This study revealed that of patients who developed cancer, adults with DM had a higher cancer mortality risk [HR 1.34 (95 % CI 1.002–1.79)] and all-cause mortality risk [1.61 (1.29–2.01)]. Despite there being no direct results about patients with HCE comorbid with cancer in the CLUE II study, it seems reasonable to conclude that uncontrolled diabetes leads to poorer outcomes in patients with cancer.
There is a significant increase in the risk of COPD with increasing baseline HbA1c in patients with DM [22]. The lung is also a target organ for diabetic microangiopathy in patients with both type 1 and type 2 DM [23], and decrements in lung function have been reported in patients with DM over the past two decades [24–26]. Decrements in the lung function of patients with DM are believed to be the consequence of biochemical alterations in the connective tissue constituents of the lung, particularly collagen and elastin, as well as microangiopathy due to the nonenzymatic glycosylation of proteins induced by chronic hyperglycemia [27, 28].
The CHF problem is magnified in people with diabetes, in whom incidence rates are two to five times greater than those in the general population [29]. Poorer glycemic control was an important predictor of CHF development [30]. DM not only increases the risk of CHF, but also accelerates its occurrence [30] and even mortality.
Liver disease is an important cause of death for people with DM [30]. In the population-based Verona Diabetes Study [31], cirrhosis was the fourth leading cause of death and accounted for 4.4 % of DM-related deaths. The standardized mortality ratio, i.e., the relative rate of an event compared with the background rate, for cirrhosis was 2.52 compared with 1.34 for cardiovascular disease [31]. In another prospective cohort study [32], cirrhosis accounted for 12.5 % of deaths in patients with DM. DM is also the most common cause of liver disease in the United States [33]. Cryptogenic cirrhosis, of which DM is, by far, the most common cause, has become the third leading indication for liver transplantation in the United States [33]. Thus, patients with DM have a high prevalence of liver disease and patients with liver disease have a high prevalence of DM [33].
The major difference of long-term mortality after HCE between non-elderly and elderly was that HCE significantly increases the subsequent mortality risk even more than 8 years in the non-elderly but limited to ≤6 years in the elderly [15]. The elderly have more comorbidites which may dilute the HCE effect on the long-term mortality after 6 years.
Because of the increased long-term mortality, prevention for HCE is paramount especially in the patients who have previous HCE. The prevention strategies include proper patient and family member education such as emphasizing the important of keeping insulin treatment and sick day management [1], better access and effective communication to medical care such as early contact with the health care provider [1], keeping attention to probable infection [9], and controlling concurrent comorbidities such as renal disease, stroke, cancer, COPD, CHF, and liver disease.
There are several limitations to this study. First, the comorbidities relied on the claim data and ICD-9-CM diagnosis codes, which may have resulted in potential disease misclassification. Second, although we stratified our patients by age, gender, and comorbidities, like other studies that have used administrative data, we did not control for some unmeasured confounding variables: type of DM, antidiabetes treatment, etc. Third, some important sociodemographic characteristics, such as education level, stress level, body mass index, and alcohol drinking habits, results of clinical examinations, and laboratory data such as HbA1c, and cause of death were not available in the NHIRD. Therefore, we could not adjust for these variables as contributing factors in this study. Fourth, we were unable to take into account the severity of the diseases, which reduced our chances of showing the severity-related effects of comorbidities. Fifth, despite our database being national, our findings may not be generalizable to cohorts in other nations.
Conclusions
In summary, our study shows that non-elderly patients with HCE had a significantly higher mortality risk than did controls during the entire follow-up period and beyond. HCE signified uncontrolled diabetes, which may have long-term effects that contribute to various complications, including death. Strategies for prevention such as education, better access to medical care, effective communication with a healthcare provider, and control of comorbidities are needed as soon as possible.
References
A.E. Kitabchi, G.E. Umpierrez, J.M. Miles, J.N. Fisher, Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32(7), 1335–1343 (2009)
Centers for Disease Control and Prevention, National hospital discharge survey (2014), http://www.cdc.gov/nchs/nhds.htm. Accessed 14 May 2014
National Center for Health Statistics, National hospital discharge and ambulatory surgery data [article online] (2014), http://www.cdc.gov/nchs/ and at: http://www.cdc.gov/nchs/ahcd.htm. Accessed 14 May 2014
S. Kim, Burden of hospitalizations primarily due to uncontrolled diabetes: implications of inadequate primary health care in the United States. Diabetes Care 30(5), 1281–1282 (2007)
Agency for Healthcare Research and Quality, Databases and related tools from HCUP: fact sheet [article online], National Center for Health Statistics, Centers for Disease Control (2014), http://www.ahrq.gov/research/findings/factsheets/tools/hcupdata/index.html. Accessed 14 May 2014
H.A. Fishbein, P.J. Palumbo, Acute metabolic complications in diabetes, in National Diabetes Data Group. Diabetes in America, (National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, 1995), pp. 283–292
S.T. Chung, G.G. Perue, A. Johnson, N. Younger, C.S. Hoo, R.W. Pascoe, M. BoyneS, Predictors of hyperglycaemic crises and their associated mortality in Jamaica. Diabetes Res. Clin. Pract. 73(2), 184–190 (2006)
R.J. MacIsaac, L.Y. Lee, K.J. McNeil, C. Tsalamandris, G. Jerums, Influence of age on the presentation and outcome of acidotic and hyperosmolar diabetic emergencies. Intern. Med. J. 32(8), 379–385 (2002)
C.C. Huang, S.C. Kuo, T.W. Chien, H.J. Lin, H.R. Guo, W.L. Chen, J.H. Chen, S.H. Chang, S.B. Su, Predicting the hyperglycemic crisis death (PHD) score: a new decision rule for emergency and critical care. Am. J. Emerg. Med. 31(5), 830–834 (2013)
J. Wang, D.E. Williams, K.M. Narayan, L.S. Geiss, Declining death rates from hyperglycemic crisis among adults with diabetes, U.S., 1985–2002. Diabetes Care 29(9), 2018–2022 (2006)
C.C. Huang, H.J. Lin, S.C. Chen, S.C. Kuo, W.L. Chen, J.H. Chen, H.Y. Wang, H.R. Guo, Cancer history, bandemia, and serum creatinine are independent mortality predictors in patients with infection-precipitated hyperglycemic crises. BMC Endocr. Disord. 13, 23 (2013)
C.C. Huang, T.W. Chien, S.B. Su, H.R. Guo, W.L. Chen, J.H. Chen, S.H. Chang, H.J. Lin, Y.F. Wang, Infection, absent tachycardia, cancer history, and severe coma are independent mortality predictors in geriatric patients with hyperglycemic crises. Diabetes Care 36(9), e151–e152 (2013)
W. Chou, M.H. Chung, H.Y. Wang, J.H. Chen, W.L. Chen, H.R. Guo, H.J. Lin, S.B. Su, C.C. Huang, C.C. Hsu, Clinical characteristics of hyperglycemic crises in patients without a history of diabetes. J. Diabetes Investig. 5(6), 657–662 (2014)
S.P. Efstathiou, A.G. Tsiakou, D.I. Tsioulos, I.D. Zacharos, A.G. Mitromaras, S.E. Mastorantonakis, T.N. Panagiotou, T.D. Mountokalakis, A mortality prediction model in diabetic ketoacidosis. Clin. Endocrinol. (Oxf) 57(5), 595–601 (2002)
C.C. Huang, S.F. Weng, K.T. Tsai, P.J. Chen, H.J. Lin, J.J. Wang, S.B. Su, W. Chou, H.R. Guo, C.C. Hsu, Long-term mortality risk after hyperglycemic crisis episodes in geriatric patients with diabetes: a national population-based cohort study. Diabetes Care 38(5), 746–751 (2015)
T.M. Cheng, Taiwan’s national health insurance system: high value for the dollar, in Six countries, six reform models: the healthcare reform experience of Israel, the Netherlands, New Zealand, Singapore, Switzerland and Taiwan, ed. by K.G. Okma, L. Crivelli (World Scientific, Hackensack, 2009), pp. 171–204
R.E. Brown, M.C. Riddell, A.K. Macpherson, K.L. Canning, J.L. Kuk, All-cause and cardiovascular mortality risk in U.S. adults with and without type 2 diabetes: influence of physical activity, pharmacological treatment and glycemic control. J. Diabetes Complicat. 28(3), 311–315 (2014)
J.M. Robbins, G.E. Thatcher, D.A. Webb, V.G. Valmanis, Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care 31(4), 655–660 (2008)
M.M. Funnell, T.L. Brown, B.P. Childs, L.B. Haas, G.M. Hosey, B. Jensen, M. Maryniuk, M. Peyrot, J.D. Piette, D. Reader, L.M. Siminerio, K. Weinger, M.A. Weiss, National standards for diabetes self-management education. Diabetes Care 32(S1), S87–S94 (2009)
J.I. Malone, A.W. Root, Plasma free insulin concentrations: keystone to effective management of diabetes mellitus in children. J. Pediatr. 99(6), 862–867 (1981)
H.C. Yeh, E.A. Platz, N.Y. Wang, K. Visvanathan, K.J. Helzlsouer, F.L. Brancati, A prospective study of the associations between treated diabetes and cancer outcomes. Diabetes Care 35(1), 113–118 (2012)
S.F. Ehrlich, C.P. Quesenberry Jr, S.K. Van Den Eeden, J. Shan, A. Ferrara, Patients diagnosed with diabetes are at increased risk for asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, and pneumonia but not lung cancer. Diabetes Care 33(1), 55–60 (2010)
C.C. Hsia, P. Raskin, Lung function changes related to diabetes mellitus. Diabetes Technol. Ther. 9(S1), S73–S82 (2007)
A.A. Litonjua, R. Lazarus, D. Sparrow, D. Demolles, S.T. Weiss, Lung function in type 2 diabetes: the normative aging study. Respir. Med. 99(12), 1583–1590 (2005)
T.M. McKeever, P.J. Weston, R. Hubbard, A. Fogarty, Lung function and glucose metabolism: an analysis of data from the Third National Health and Nutrition Examination Survey. Am. J. Epidemiol. 161(6), 546–556 (2005)
D.A. Lawlor, S. Ebrahim, G.D. Smith, Associations of measures of lung function with insulin resistance and type 2 diabetes: findings from the British Women’s Heart and Health Study. Diabetologia 47(2), 195–203 (2004)
F. Innocenti, A. Fabbri, R. Anichini et al., Indications of reduced pulmonary function in type 1 (insulin-dependent) diabetes mellitus. Diabetes Res. Clin. Pract. 25(3), 161–168 (1994)
D.C. Weir, P.E. Jennings, M.S. Hendy, A.H. Barnett, P.S. Burge, Transfer factor for carbon monoxide in patients with diabetes with and without microangiopathy. Thorax 43(9), 725–726 (1998)
G.A. Nichols, T.A. Hillier, J.R. Erbey, J.B. Brown, Congestive heart failure in type 2 diabetes: prevalence, incidence, and risk factors. Diabetes Care 24(9), 1614–1619 (2001)
G.A. Nichols, C.M. Gullion, C.E. Koro, S.A. Ephross, J.B. Brown, The incidence of congestive heart failure in type 2 diabetes: an update. Diabetes Care 27(8), 1879–1884 (2004)
R. de Marco, F. Locatelli, G. Zoppini, G. Verlato, E. Bonora, M. Muggeo, Cause-specific mortality in type 2 diabetes. The Verona Diabetes Study. Diabetes Care 22(5), 756–761 (1999)
B. Balkau, A. Randrianjohany, L. Papoz, E. Eschwège, Re: “A prospective population-based study of alcohol use and non-insulin-dependent diabetes mellitus”. Am. J. Epidemiol. 134(12), 1469–1470 (1991)
K.G. Tolman, V. Fonseca, A. Dalpiaz, M.H. Tan, Spectrum of liver disease in type 2 diabetes and management of patients with diabetes and liver disease. Diabetes Care 30(3), 734–743 (2007)
Acknowledgments
This study was supported by grants CMFHR10384 from the Chi-Mei Medical Center. This study is based in part on data from the Taiwan National Health Insurance Research Database provided by the National Health Insurance Administration, Ministry of Health and Welfare, and managed by National Health Research Institutes (Registered number NHIRD-100-057, NHIRD-102-024). The interpretation and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare or National Health Research Institutes. We thank Bill Franke for his invaluable advice and editorial assistance.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
No potential conflicts of interest relevant to this article were reported.
Additional information
Yuan Kao and Chien-Chin Hsu have contributed equally to this work as first authors.
Rights and permissions
About this article
Cite this article
Kao, Y., Hsu, CC., Weng, SF. et al. Subsequent mortality after hyperglycemic crisis episode in the non-elderly: a national population-based cohort study. Endocrine 51, 72–82 (2016). https://doi.org/10.1007/s12020-015-0669-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0669-8