Abstract
Personalized medicine (PM) aims individualized approach to prevention, diagnosis, and treatment. Precision Medicine applies the paradigm of PM by defining groups of individuals with akin characteristics. Often the two terms have been used interchangeably. The quest for PM has been advancing for centuries as traditional nosology classification defines groups of clinical conditions with relatively similar prognoses and treatment options. However, any individual is characterized by a unique set of multiple characteristics and therefore the achievement of PM implies the determination of myriad demographic, epidemiological, clinical, laboratory, and imaging parameters. The accelerated identification of numerous biological variables associated with diverse health conditions contributes to the fulfillment of one of the pre-requisites for PM. The advent of multiplex analytical platforms contributes to the determination of thousands of biological parameters using minute amounts of serum or other biological matrixes. Finally, big data analysis and machine learning contribute to the processing and integration of the multiplexed data at the individual level, allowing for the personalized definition of susceptibility, diagnosis, prognosis, prevention, and treatment. Autoantibodies are traditional biomarkers for autoimmune diseases and can contribute to PM in many aspects, including identification of individuals at risk, early diagnosis, disease sub-phenotyping, definition of prognosis, and treatment, as well as monitoring disease activity. Herein we address how autoantibodies can promote PM in autoimmune diseases using the examples of systemic lupus erythematosus, antiphospholipid syndrome, rheumatoid arthritis, Sjögren syndrome, systemic sclerosis, idiopathic inflammatory myopathies, autoimmune hepatitis, primary biliary cholangitis, and autoimmune neurologic diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As in the Yang/Ying duality equilibrium, personalized medicine (PM) intertwines with the traditional nosology approach, as the trend for the personalized definition of patients’ illnesses coexists with the paradigm of grouping patients with similar clinical presentations under certain disease labels. Nosology allows the identification of shared clinical patterns and determination of the general response to certain therapeutic options, culminating in the elaboration of diagnostic and therapeutic guidelines. However, this occurs at the expense of obscuring individual peculiarities. On the other hand, PM recognizes that there are relevant differences among patients equally classified under a single disease entity and that the optimal therapeutic approach will be different for each of these patients. By acknowledging that true individual personalization may not be realistic, some have proposed the term Precision Medicine as the practical application of the concept of PM to restricted groups of individuals with similar pathophysiological behavior and sharing favorable outcomes from selected therapeutic approaches.
Although more fashionable in the last two decades, PM is a concept long pursued by physicians and scientists and implies narrowing down the definition of the health problems of an individual patient so that the optimal therapeutic approach is devised for that individual. A detailed anamnesis contributes to “personalizing” the assessment of the health status of any given patient by determining the subjective impact (pain, fear, anger, depression, negation) associated with the objective dimension of the disease identified in the physical examination and imaging/laboratory examinations. Information on previous health problems, life habits, response to previous medications, family health problems, religious attitude, and social-financial status is helpful for the understanding of the various relevant aspects of a given patient, fine-tuning her/his current health problem, and defining the most appropriate therapeutic strategy. The goals of PM are comprehensive and extend from identifying an individual’s potential weaknesses, prediction of potential disease(s), fine phenotyping of diseases, and thorough engagement of the social-cultural dimension of the individual [1] (Table 1).
Along the last few decades, important developments potentially relevant to PM have occurred: (1) steady incremental progress in the availability of various biomarkers of health and disease; (2) progressive understanding of the phenotypic relevance of thousands of polymorphic genes; (3) establishment of techniques for determination of the microbiome in distinct body areas and their physiological and pathological significance; (4) comprehension of epigenetic modulation of the genome and its relevance in various biologic states; (5) availability of multiplex assays that allow simultaneous determination of multiple parameters (microarrays, addressable laser bead immunoassays, next-generation sequencing); (6) artificial intelligence and machine learning required to meaningfully extract trends, conjunctions, and focal points in very large datasets. The integrated use of these elements is expected to foster the establishment of a more advanced degree of medicine personalization soon.
Autoimmune diseases are a group of chronic inflammatory conditions of unknown etiology with a putative breakdown or dysregulation of tolerance for specific sets of autoantigens. In general, it is believed that autoimmune diseases are triggered by environmental and hormonal factors acting on an organism with definable genetic predispositions. Selected inflammatory and immunologic biomarkers are observed in each set of autoimmune diseases, contributing to refining the diagnosis toward PM. Among these, autoantibodies hold a special place in managing patients with autoimmune diseases, contributing to the identification of individuals at risk and disease prediction, disease diagnosis and fine phenotyping, determination of concurrent processes, establishment of prognosis, treatment selection, and monitoring of disease activity and outcomes (Table 2).
One major group of autoimmune diseases are those with circumscribed involvement of the organism and includes organ-specific (e.g., Hashimoto’s thyroiditis), tissue-specific (e.g., Pemphigus Vulgaris), and cell-specific (e.g., immunologic thrombocytopenia) autoimmune diseases. At the other end of the spectrum is a group of systemic autoimmune diseases characterized by widespread involvement of the organism, although some organs and cells may be preferentially targeted. Systemic lupus erythematosus (SLE) is the prototype of this group and possibly the disease with the most heterogeneous autoantibodies [2]. It is noteworthy that disease-specific autoantibodies in circumscribed autoimmune diseases occur at a high frequency, therefore representing biomarkers with high sensitivity. In contrast, autoantibodies in systemic autoimmune diseases most frequently occur at moderate or low frequency, therefore typically representing biomarkers with limited sensitivity (Table 3). Over the last few decades, steady progress has been achieved in the discovery of novel autoantibodies, establishment of fine phenotype associations, and improvement in immunoassays to determine and quantify these biomarkers in several systemic autoimmune diseases.
Following, we will discuss how autoantibodies can contribute to PM, using several examples of circumscribed and systemic autoimmune diseases.
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic autoimmune inflammatory disease with multifactorial etiology, heterogeneous and pleomorphic clinical manifestations, and potential to affect several organs and systems. The disease is characterized by variable onset and then differing periods of flare and remission [3]. The prevalence varies according to ethnicity and environmental conditions, occurring in 20 to 150 cases/100,000 inhabitants in the USA [4]. Geographic regions where individuals have high exposure to the sun exhibit higher incidence rates [5]. Reflecting an important hormonal influence, it is more frequent in women (7:1 to 15:1 women/men) and the disease onset occurs between 16 and 55 years of age in 65% of the cases. Although less frequent in males and childhood, SLE is usually more severe in these gender and age groups. Regarding ethnicity, SLE is more prevalent and severe in Afro-descendant and Asian individuals [3, 4].
The interaction between hormonal, environmental, and infectious factors in individuals with an appropriate genetic predisposition is believed to lead to loss of immunological tolerance and the development of the disease. Infectious agents (e.g., Epstein–Barr virus), some medications (procainamide, hydralazine, hydrazide, biologicals, etc.), ultraviolet radiation (sunlight), and hormonal factors (increased estrogen/androgen ratio) are recognized as possible triggers. Immunological system dysregulation is characterized by the presence of multiple autoantibodies directed mainly against nuclear antigens but also a host of cytoplasmic and extracellular antigens [2]. Some autoantibodies directed against specific cell-surface antigens participate in the pathogenesis of the disease, leading to cytopenia and neuropsychiatric impairment. Tissue damage results from the deposition of immune complexes, activation of the complement system, and consequent inflammatory processes. In addition, SLE patients have a deficiency in the clearance of circulating autoantigens and immune complexes, favoring the perpetuation of the pathogenic process [3].
Given the complexity and the heterogeneous phenotypic spectrum of the disease, biomarkers that can lead to a more accurate definition of an individual patient pathology are essential for PM regarding diagnosis, treatment, and prognosis. Autoantibodies, in particular, play an important role in the prediction, diagnosis, classification, and fine phenotype definition of SLE (Table 4).
Antinuclear Antibodies
Antinuclear antibody (ANA) screening by indirect immunofluorescence on HEp-2 cells (HEp-2 IFA) is positive in up to 98% of SLE patients with active disease [6]. A positive HEp-2 IFA test has been included as a required criterion in the most recent ACR/EULAR classification criteria for SLE [6]. However, HEp-2 IFA can also be positive in other immune-mediated rheumatic diseases, such as systemic sclerosis (up to 95%), mixed connective tissue disease (100%), Sjögren’s syndrome (68–96%), and less so in immune-mediated myopathies (40–80%). In addition, as a consequence of the increased sensitivity of the method, 12.6 to 22.6% of healthy individuals may also have a positive HEp-2 IFA test [7, 8]. Interestingly, it has been reported recently that the frequency of positive HEp-2 IFA tests, but not of autoimmune diseases, has been increasing along the decades, suggesting a distinction between autoimmunity and autoimmune disease [9]. In this context, it should be noted that the immunofluorescence pattern in the HEp-2 IFA test holds relevant associations to the autoantibodies present in the sample and that several of the SLE-specific autoantibodies hold distinctive HEp-2 IFA pattern associations [10, 11]. The most relevant HEp-2 IFA patterns have been classified with alpha-numeric codes by the International Consensus on ANA Patterns (ICAP) initiative (www.anapatterns.org) [12]. Therefore, the interpretation of the HEp-2 IFA test in the context of SLE should be personalized as some patterns (e.g., DFS-like pattern/AC-2; centromere pattern/AC-3, nucleolar patterns/AC8-AC-10, NuMA-like pattern/AC-26; Scl-70-like pattern/AC-29) present no relevant relationship with SLE whereas some others (e.g., homogeneous nuclear/AC-1; coarse speckled nuclear/AC-5) are frequently observed in SLE patients [11]. These considerations are particularly relevant, as a positive ANA test is an entrance item in the ACR/EULAR SLE classification criteria [6]. Table 5 illustrates some relevant patterns occurring in SLE and other systemic autoimmune diseases.
In addition to contributing to diagnosis and classification, the HEp-2 IFA test presents additional opportunities for PM. Recent data suggest that SLE patients with positive HEp-2 IFA and/or anti-dsDNA respond better to some biological DMARD in comparison with seronegative patients [6, 13, 14]. Moreover, the HEp-2 IFA titer and pattern can change according to the disease activity status. In a cross-sectional and prospective study, Prado et al. showed that high titer HEp-2 IFA and the homogeneous nuclear pattern (AC-1) were associated with higher SLE disease activity index (SLEDAI) whereas lower titer HEp-2 IFA and fine speckled nuclear pattern (AC-4) were associated with lower SLEDAI [15]. In addition, SLE patients with a negative ANA HEp-2 IFA tend to be older and Caucasian [16].
Autoantibodies to SS-A/Ro, SS-B/La, U1-RNP, and Sm
Antibodies such as anti-U1-RNP, anti-SS-A/Ro60, and anti-SS-B/La are frequently found in patients with SLE, but they are not specific for this disease [17]. Anti-SS-A/Ro60 antibodies are present in 30–40% of SLE patients and 60–90% of patients with subacute cutaneous lupus. Both anti-SS-A/Ro60 and anti-SS-B/La are associated with sicca syndrome in SLE patients [17] and are also associated with the risk of neonatal lupus (NLE). Isolated anti-SS-B/La rarely imposes risk, but, when associated with anti-SS-A/Ro60, the risk of NLE increases. Among babies born to mothers carrying anti-SS-A/Ro60 with or without anti-SS-B/La, approximately 10% develop skin rash, 20% transient cytopenia, and 30% mild transient transaminitis [18]. These complications are short-lived and spontaneously resolve within a few months when the maternal antibodies disappear from the child`s circulation [19]. The exception is the congenital complete atrioventricular block, which, although rarer (1–2%), is irreversible. If previous maternal history of a fetus with complete atrioventricular block is present, the chance of recurrence increases to 13–18% [20]. In adult patients, anti-SS-A/Ro60 is associated with QTc interval prolongation [21] and an increased risk of developing complex ventricular arrhythmias [22].
Anti-U1-RNP and anti-Sm antibodies react with antigens in small nuclear ribonucleoprotein macromolecular complexes that function in the splicing of precursor messenger RNA [23]. Anti-Sm and anti-U1-RNP are more prevalent in African American and Afro-Caribbean as compared to Caucasian SLE patients. Anti-U1-RNP presents moderate sensitivity and is not specific for SLE, as it is also observed in SSc and MCTD [17]. SLE patients with anti-U1-RNP antibodies have increased frequency of scleroderma-like nail fold capillaroscopic abnormalities and Raynaud's phenomenon [24]. Anti-Sm antibodies are present in 12–30% of SLE patients with a specificity of 96 to 98%. Anti-Sm antibodies have been associated with lupus nephritis, especially when associated with anti-dsDNA antibodies, neuropsychiatric lupus, serositis, pulmonary fibrosis, and peripheral neuropathy [25, 26]; however, they are not associated with disease activity [17].
Anti-Double Stranded DNA (dsDNA) Antibodies
Anti-dsDNA antibodies are specific biomarkers for SLE and constitute part of the classification criteria [6]. This biomarker is widely used in daily clinical practice for diagnosis and disease monitoring as it is rarely seen in conditions other than SLE and the serum levels correlate with disease activity, especially nephritis activity. Despite its high specificity for SLE, the sensitivity is only 50–60% [17]. In clinically asymptomatic SLE patients, rising anti-dsDNA titers herald imminent risk for disease flare, especially when accompanied by decreasing serum complement concentrations [27]. Controlled studies in clinically stable SLE patients with rising anti-dsDNA titers showed that patients who receive glucocorticoids developed fewer severe flares compared to those who did not [28]. However, it is not recommended to treat clinically asymptomatic SLE patients with stable and persistent serological activity due to the risk of adverse effects of glucocorticoids and immunosuppressant therapy [27].
Anti-Nucleosome Antibodies
The nucleosome is a chromatin unit formed by dsDNA coiled around a histone octamer. Anti-nucleosome (NCS) antibodies have high sensitivity (48–100%) and specificity (90–99%) for SLE, showing association with disease activity, especially active nephritis. Anti-NCS antibodies frequently precede the appearance of anti-dsDNA antibodies and, when both coexist, anti-NCS and anti-dsDNA serum levels show a good correlation. Anti-NCS serum levels were reported to correlate with the histological activity index of lupus nephritis [29]. These autoantibodies are especially useful in lupus nephritis patients that do not present anti-dsDNA and anti-Sm antibodies [17]. Patients with clinically quiescent SLE and high anti-NCS levels have more frequent flares than their negative counterparts and should be closely monitored for early detection and timely treatment of flares [30]. The coexistence of anti-nucleosome, anti-dsDNA, and anti-histone antibodies is associated with severe kidney involvement [31] and an increased risk of renal failure requiring transplantation [32].
Anti-C1q
Anti-C1q antibodies are not specific for SLE because they are also found in patients with systemic sclerosis, Sjögren's syndrome, rheumatoid arthritis, hypocomplementemic urticarial vasculitis, antiphospholipid syndrome (APS), and dermatomyositis. However, anti-C1q is far more frequent in SLE than in other rheumatic diseases (OR 2.7, 95% CI 1.8–4, p < 0.001) [33]. In addition, anti-C1q is more frequent in lupus nephritis, showing a good correlation with nephritis activity [33,34,35]. In a multicentric cohort, anti-C1q in combination with anti-dsDNA and low complement presented the strongest serological association with renal involvement (OR 14.9; 95% CI 5.8–38.4) [30]. Concomitant anti-dsDNA and anti-C1q positivity confers a predictive value of 67% for active lupus nephritis while when both autoantibodies are absent the negative predictive value for active lupus nephritis is 74% [36]. In proliferative lupus nephritis, anti-C1q antibodies show a sensitivity of 80.5% and a specificity of 71% for the diagnosis of renal flares [37].
Anti-Ribosomal P Protein
The frequency of anti-ribosomal P protein (anti-ribosomal P) antibodies in SLE patients varies from 10 to 47% and this variability is known to be dependent on the immunoassay employed, ethnicity or regional differences, cohorts studied, and the age of disease onset. Anti-ribosomal P has specificity for SLE of 96.1 to 98.4% [38, 39]. In addition, anti-ribosomal P shows some peculiar phenotypic associations in SLE. Since the first report of an association between anti-ribosomal P and psychosis [40], the association of this antibody in neuropsychiatric SLE (NPSLE) is the subject of several studies. A recent meta-analysis confirmed the association between anti-ribosomal P and neuropsychiatric manifestations (OR 1.95; 95% CI 1.52–2.50) with considerable heterogeneity of manifestations [38]. When NPSLE was stratified by specific NPSLE features, central nervous system involvement, depression, and psychosis remained associated with anti-ribosomal P. In particular, the association of anti-ribosomal P was stronger with psychosis (OR 3.08; 95% CI 1.94–4.87) and depression (OR 3.03; 95% CI 1.32–6.95).
Anti-ribosomal P antibodies also show phenotypic associations with lupus nephritis, as the frequency of anti-ribosomal P antibodies was shown to be higher in SLE patients with class V lupus nephritis than in patients with other classes of glomerulonephritis (72% versus 28%; p = 0.005) [41]. In addition, a better long-term renal outcome was observed in SLE patients with positive anti-ribosomal P antibody and no anti-dsDNA during nephritis flares [42]. Lupus hepatitis also presents a strong association with anti-ribosomal P (OR 8.44; 95% CI 3.16–22.53), which has been reported also in 9.7% of autoimmune hepatitis patients without clinical or laboratory evidence of SLE [43].
Therefore, anti–ribosomal P antibodies provide useful information for PM and should be used more often in clinical practice. When other SLE-specific autoantibodies are lacking, anti-ribosomal P may represent a valuable biomarker for diagnosis. In the presence of other autoantibodies, anti-ribosomal P may add valuable information for fine-tuning the disease phenotype. Of interest, a clue for the presence of anti-ribosomal P antibodies is the dense fine speckled cytoplasmic pattern (AC-19) on the HEp-2 IFA test, especially if associated with weak nucleolar staining [10, 11]. Nonetheless, it should be noted that up to 40% of samples with anti-ribosomal P antibodies yield no relevant HEp-2 IFA reactivity [12].
Antiphospholipid Antibodies
Antiphospholipid antibodies (aPL) (lupus anticoagulant; anti-cardiolipin; anti-β2 glycoprotein-1) can be found in 20 to 40% of SLE patients and 10 to 20% of these will present manifestations of the antiphospholipid syndrome (APS), including vascular thrombosis (arterial or venous) and gestational morbidity. Apart from the standard APS manifestations, aPL are associated with a worse prognosis in SLE as they are also associated with some neuropsychiatric SLE manifestations (seizures, cerebrovascular disease, cognitive deficit, and myelitis), renal involvement (APS nephropathy) [44], and thrombocytopenia [45]. Thus, given their frequency and connection with potential morbidity, all SLE patients should be screened for these antibodies [17].
Complement System Interface with Autoantibodies
Complement system assessment (C3, C4, CH50) is useful for monitoring lupus disease activity [17]. In more than 50% of cases, there is evidence of complement consumption in the active phase of the disease, frequently associated with an increase in anti-dsDNA titers. Furthermore, deficiency of early components of the classical complement pathway is associated with an increased risk of SLE and related syndromes. The combination of normal C3 levels and decreased hemolytic complement (CH50) should raise the possibility of genetic complement deficiency and determination of C1q, C2, and C4 serum levels is recommended [17]. The autoantibody profile presents some peculiarities in SLE associated with inherited complement deficiency. C1q deficiency is extremely rare and is strongly associated with SLE and recurrent infections. C1q-deficient SLE presents as early-onset and severe disease with frequent skin and kidney involvement, high frequency of anti-SS-A/Ro60, and positive HEp-2 IFA, but rarely have anti-dsDNA antibodies [46]. C2 deficiency is the most frequent inherited complement deficiency and up to 30% of the C2-deficient patients develop SLE or lupus-like disease. C2-deficient SLE patients tend to present a milder disease (predominately articular and cutaneous manifestations) and have a high frequency of anti-SS-A/Ro60 antibodies [47]. Complete C4 deficiency is very rare, but 75% of such individuals develop SLE. Low gene copy number for C4 is not so rare and individuals with low copy numbers for C4A are at higher risk of SLE. C4-deficient SLE patients have a high frequency of nephritis and anti-SS-A/Ro60 antibodies, but a low frequency of anti-dsDNA antibodies [48, 49].
Antiphospholipid Syndrome
Antiphospholipid syndrome (APS) was first described in 1983 as a condition characterized by thrombosis and recurrent miscarriage possibly associated with the presence of antiphospholipid (aPL) antibodies [50]. APS-associated autoantibodies recognize predominantly protein-phospholipid complexes. In the early 1990s, β2-glycoprotein I (β2GPI) was identified as an essential component in the so-called anticardiolipin (aCL) antibody assay and as a genuine target by itself of APS autoantibodies [51]. This finding allowed discrimination between β2GPI-dependent aCL, which correlates with thrombosis and fetal loss, and β2GPI-independent aCL, which is non-specific [52].
APS is a systemic autoimmune disease, with thrombotic and inflammatory mechanisms orchestrated by aPL antibodies, and presents with a variety of clinical manifestations, including venous/arterial thrombosis and pregnancy morbidity as well as "non-classical" manifestations, such as thrombocytopenia, nephropathy, seizures, dementia, valvular heart disease, and others. APS can be classified as primary or secondary when it is associated with another autoimmune disease, most frequently SLE [53]. The 2006 Sydney APS classification criteria involve at least one clinical and one laboratory criterion (Table 6) [53]. An updated set of classification APS criteria is under consideration [54].
The aPL antibody profile is an important factor in determining the risk of thrombotic and obstetric events. Interestingly, the relationship between the presence of aPL antibodies and thrombosis is not an “all or nothing” phenomenon and is related to the type, titer, and persistence of the antibody, number of different antibodies, the coexistence of other thrombosis risk factors, and the presence of associated autoimmune diseases [55]. In addition to the aPL antibodies belonging to the APS criteria, other antibodies have been implicated in APS such as IgA aCL, IgA anti-β2GPI, anti-phosphatidylserine/prothrombin (aPS/PT) complex, anti-domain I β2GPI, anti-prothrombin, anti-vimentin, anti-annexin, anti-phosphatidylserine, and anti-phosphatidylethanolamine [56].
Lupus Anticoagulant (LAC) Antibody
In 1952, Conley and Hartmann were the first to identify a circulating factor that prolonged blood-clotting time in two SLE patients; aptly named lupus anticoagulant (LAC). In a retrospective analysis, it is noteworthy that these two patients also had a false-positive test for syphilis, later recognized as a clue for APS. In 1963, it was noticed that LAC was unexpectedly associated with in vivo thrombotic manifestations and eventually shown to be associated with pregnancy morbidity [57]. In APS patients, LAC is the autoantibody most frequently associated with thrombotic and obstetric events and its presence, per se, classifies patients as at high risk for thrombotic events and pregnancy morbidity. A meta-analysis with LAC-positive patients found the odds ratio (OR) to be 6.14 (95% CI 2.7–13.8) for venous thrombosis and 3.6 (95% CI 2.7–13.8) for arterial thrombosis [58].
The methodology of LAC detection is based on a three-step procedure including a screening step, a mixing step, and a confirmation step. Strict adherence to the method and appropriate pre-analytical precautions in obtaining and handling the blood sample are essential for reliable results. Of clinical importance and a limitation of the assay, patients must not be on anticoagulation therapy as this and other factors such as C-reactive protein can be associated with false-positive results [59].
Anticardiolipin Antibodies (aCL)
aCL antibodies are directed against the complex of β2GPI and cardiolipin, a phospholipid found almost exclusively in the mitochondrial membrane and cell walls of bacteria. aCL is associated with an increased risk of thrombosis when present in moderate or high titer (> 40 GPL/MPL or > 99th percentile, measured by a standardized ELISA). A meta-analysis found that the presence of aCL has an OR of 1.46 (95% CI 1.06–2.03) for venous thrombosis and 2.65 (95% CI 1.75–4.00) for arterial thrombosis [58].
IgG and IgM are the predominant aCL isotypes. The frequency of aCL IgA antibodies in APS is variable and their clinical significance is still uncertain. Although some studies suggest a pathophysiological role for IgA aCL, its presence does not seem to lead to clinical manifestations in a significant number of patients. Furthermore, the prevalence of aCL IgA antibodies is very low in APS patients lacking IgG and IgM aCL, which restricts substantially their diagnostic value [60]. aPL antibodies must always be interpreted taking into account the clinical context, as aCL and anti-β2GPI antibodies, especially IgM isotype, can also be found as epiphenomena in infectious diseases without correlation with thrombotic events.
Anti-Beta 2-Glycoprotein I (β2GPI) Antibodies
Anti-β2GPI antibodies target the multifunctional plasma protein Beta-2-Glycoprotein I, which undergoes a conformational change in its structure upon binding to cardiolipin. The β2GPI/cardiolipin complex increases the expression of tissue factors and leads to activation of endothelial cells, monocytes, neutrophils, fibroblasts, and trophoblasts, which results in a pro-coagulant state. Anti-β2GPI antibodies of IgG and/or IgM isotypes at titer greater than the 99th percentile, measured by a standardized ELISA, are clinically relevant [53].
Unlike aCL IgA antibodies, IgA anti-β2GPI antibodies are reported to be related to thrombotic phenomena. A retrospective study in 2013 suggested that IgA anti-β2GPI may be useful in identifying patients with APS negative for IgG and IgM anti-β2GPI [61]. In fact, in three different cohorts, it was observed that a significant portion of patients with clinical manifestations of APS was positive only for IgA anti-β2GPI [60]. In kidney transplant patients, IgA anti-β2GPI confers a high risk for early graft loss caused by thrombosis and a high risk of delayed graft dysfunction [62]. However, more studies are necessary to understand the precise pathogenic action of this antibody and to standardize currently available commercial laboratory tests.
Phosphatidylserine/Prothrombin Complex (aPS/PT) Antibodies
A meta-analysis that included more than 7000 patients and controls found that aPS/PT seemed to represent a stronger risk factor for arterial (OR 5.11; 95% CI 4.2–6.3) and venous (OR 1.82; 95% CI 1.44–2.75) thrombosis than antibodies to isolated prothrombin [63]. In addition, a strong association between aPS/PT IgG and LAC has been reported [64]. Despite not being included in the current APS classification criteria, this antibody has been incorporated into the two scores currently available to evaluate thrombosis risk in APS patients: the Antiphospholipid Score (aPL-S) [65] and the Global Antiphospholipid Syndrome Score (GAPSS) [66]. aPS/PT antibodies may be especially useful in cases with high suspicion of APS and negative results for “classic (or criteria) aPL” antibodies or in patients in whom the LAC test is unreliable due to anticoagulation therapy.
Anti-Domain I β2GPI (anti-DI β2GPI) Antibody
β2GPI is a plasma glycoprotein composed of five highly homologous regions called domains I to V, from the N terminus to the C terminus. When in solution, β2GPI presents a circular conformation, but its structure becomes linear and elongated by binding to phospholipids and the point of attachment with the phospholipid corresponds to a hydrophobic loop surrounded by positively charged amino acids located in domain V [52]. Domain I is hidden in the circular conformation of β2GPI but becomes exposed upon elongation promoted by binding to phospholipids. Currently, antibodies against β2GPI are understood as a heterogeneous family of antibodies, which recognize different domains of the glycoprotein. Some studies suggest that domain 1 anti-β2GPI (DI β2GPI) antibodies are the most pathogenic in APS and have a higher association with thrombotic events than antibodies to the intact anti-β2GPI where antibodies may bind to the other domains [60]. A systematic review that included 1585 patients confirmed a strong association of anti-DI β2GPI antibody with thrombotic events [67]. Anti-DI β2GPI antibody is more frequently detected in triple aPL-positive patients, correlates with medium–high titer aPL, and is associated with clinical manifestations such as thrombosis and pregnancy morbidity [68]. It has been shown recently that the combination of anti-DI β2GPI and IgG/IgM aPS/PT antibodies confers a high positive predictive value for APS diagnosis and high risk for thrombosis [69].
APS Risk Profile Assessment
One of the objectives of PM is to offer the possibility of risk stratification using easily accessible and reproducible biomarkers. The determination of LAC, aCL, and anti-β2GPI antibodies allows stratifying patients at low and high risk for APS-related events (Table 7). The presence of LAC has been associated with a higher risk for thromboembolic events (OR 4.4; 95% CI 1.5–13.3) when compared to aCL or anti-β2GPI. On the other hand, triple positivity for these autoantibodies confers the highest risk for thrombotic events (OR 33.3; 95% CI 7.0–157.6) [70] as well as a worse prognosis for obstetric morbidity [71].
Scores that include the presence of aPL antibodies have been developed for assessing the diagnosis of APS and thrombosis risk (aPL-S) [65] and the risk for thrombosis and pregnancy loss, taking into account the aPL profile, traditional cardiovascular risk factors, and the autoimmune antibody profile (Global Anti-Phospholipid Syndrome Score—GAPSS) [66]. GAPSS includes hyperlipidemia (3 points), arterial hypertension (1 point), aCL IgG/IgM (5 points), LAC (4 points), and aPS/PT IgG/IgM (3 points). Scores of 10, 12, and 15 had a sensitivity of 0.709, 0.578, and 0.378, respectively, and a specificity of 0.793, 0.817, and 0.950, respectively, for thrombotic events. The Adjusted GAPSS (aGAPSS) excludes aPS/PT antibodies from the scoring algorithm, recognizing that these antibodies are currently not included in the APS criteria classification and are not assayed routinely [72].
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a promising clinical scenario where PM plays a rapidly emerging significant role. The prevalence of RA ranges from 0.3 to 1% of the adult population with a bimodal peak of incidence affecting predominantly women between 40 and 70 years of age [73, 74]. Recent studies reveal that during a 10-year course of RA about half of the patients cannot maintain a full-time job, confirming that pain, stiffness, articular edema, and joint destruction significantly limit work efficiency in RA patients [73]. Growing evidence has demonstrated that the discrete mechanisms that operate across the RA pathophysiological continuum are suitable to therapeutic interventions that might abrogate or even prevent RA [75]. A better understanding of the mechanisms and biological interactions addressing genetic factors, environmental contributors, neo-antigen generation, innate and adaptive immune cell responses, autoantibodies, and cytokines has been crucial for the advancement in RA treatment [76]. Individual-specific interventions should be feasible and effective for preventive strategy in high-risk individuals and treatment in patients with established disease.
RA presents a heterogeneous disease phenotype and considerable variability is observed in terms of individual patient progression from pre-clinical stages to established RA, disease severity, and treatment response. Over the natural history of RA, including loss of self-tolerance at pre-clinical stages, different triggers and mechanisms come into play at different time frames depending on the patient. This represents an opportunity to individualize RA management and ultimately put it forward as a genuine application of PM [77]. In that sense, clinical and biological markers might serve as a research and clinical diagnostic and prognostic tools, contributing to therapeutic precision in RA. Such an approach would address the challenge and unmet need of early identification and diagnosis of individuals at high risk or with established early RA, classification of disease severity, and choice of the right pharmacological intervention at the individual level [78]. In other words, PM in RA might allow the clinicians to better diagnose (RA vs. non-RA), to understand the prognosis of the disease (progressor vs. non-progressor; responder vs. non-responder), and to search for clinical or biological markers to guide target treatment selection in an individual patient with uncontrolled disease.
RA encompasses a temporal disease spectrum in which genetically predisposed individuals under the influence of the appropriate environmental factors evolve through successive stages, with an initial preclinical asymptomatic phase when the only evidence is the presence of RA-associated autoantibodies [79, 80]. Gradually some of these individuals develop non-specific clinical manifestations, including malaise, weight loss, poor appetite, and arthralgia. Eventually, patients will evolve with initial synovitis (early RA) and further progress to full-blown RA [81].
RA etiopathogenesis has been linked to multiple mechanisms involving both innate and adaptive immune responses. Genetically predisposed individuals can recognize and mount an adaptive immune response to post-translational modifications (PTM) of autoantigens. This phenomenon occurs mainly in the mucosa of the lungs and the gut, where smoking and the microbiota, respectively, promote PTM of several self-constituents by diverse biochemical mechanisms including citrullination, acetylation, carbamylation, and malondialdehyde acetaldehydation [82,83,84,85,86,87,88]. Once the neo-antigens are presented by dendritic cells and macrophages to T cells, activation of the adaptive immune response in lymphoid tissues takes place leading to the initiation of the autoimmune reactivity characteristic of RA. Activation of B cells follows in the process with autoantibody formation, mainly rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPA). Clonal activation and expansion of Th1 and B cells further stimulate stromal cells in the synovial layer (such as fibroblast-like synoviocytes, dendritic cells, and macrophages) that will then produce a range of cytokines and inflammatory factors that perpetuate the inflammatory milieu and ultimately lead to cartilage degradation and osteoclast engagement in subchondral bone destruction [83, 89]. The American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) established classification criteria for RA based on the presence of a combination of tender and swollen joints, duration of symptoms, acute-phase reactants, and autoantibodies, including ACPA and RF. Despite different biologic bases and predictive abilities, ACPA and RF carry the same weight in the classification criteria [90], while the marked difference in the predictive ability for ACPA titer (low versus high) is somewhat neglected [91]. A meta-analysis on RF and anti-CCP2 showed a sensitivity of 69% and 67% and a specificity of 85% and 95%, respectively, in the discrimination of RA patients and healthy individuals [92]. Up to 80% of RA patients present detectable autoantibodies [93], the presence of which identifies a subgroup of RA patients that are more homogenous regarding risk factors and clinical disease course (Table 8). However, the field needs further progress toward better disease prediction and prevention, accurate diagnosis, prognosis, and individualized treatment.
Rheumatoid Factor
RF, an autoantibody directed against the Fc part of aggregated human IgG, was the first autoantibody system to be described in RA. RF has a sensitivity ranging from 60 to 90% and a specificity ranging from 48 to 92%, according to different studies (reviewed in 88). Particularly at low titer, RF occurs in variable frequency in other systemic autoimmune diseases, chronic infections, and cancer. Healthy individuals usually present low-titer and low-affinity polyreactive RF, with increasing frequency in older individuals. RF may occur as an IgM, IgA, or IgG isotype and the IgM RF is most commonly tested in the clinical laboratory. The coexistence of IgM and IgA RF has higher specificity of the diagnosis of RA, especially at moderate to high titer.
Anti-Citrullinated Peptide Antibodies
Although the definitive antigenic characterization was achieved in 1998, the first reports on this class of autoantibodies date decades before, with the anti-perinuclear factor reported by IFA on oral mucosa cells in 1964 and the anti-keratin antibodies reported by IFA on rat esophagus in 1989 [94]. Citrullination is a process by which the enzyme peptidyldeaminase converts histidine into citrulline in the presence of Ca++. Citrullination is particularly evident in inflammation, apoptosis, and keratinization. Different citrullinated peptides can be recognized by ACPA from different patients, including citrullinated self-proteins, such as vimentin, fibrinogen, filaggrin, fibronectin, and α-enolase (reviewed in 90). ACPA occurs in circa 70% of RA patients and has a specificity of 98%. With higher specificity for RA, ACPA were included in the 2010 ACR-EULAR classification criteria for RA [91].
Patients with ACPA and/or RF show a clear association with HLA-DRB1 alleles containing the shared epitope (HLA-DRB1-SE). As discussed ahead, ACPA/RF-positive RA is associated with increased radiographic progression and joint damage, especially in the case of multiple autoantibodies [95,96,97]. Despite being instrumental in the diagnosis and classification of RA, there are still significant limitations and challenges in the use of ACPA and RF in clinical practice. There is significant variability in the performance characteristics of the available RF and ACPA immunoassays and that impacts RA classification and further management [91].
Antibodies to Post-Translational Modifications of Autoantigens
Proteins are sequences of amino acids encoded by specific genes; however, a substantial proportion of proteins suffer chemical modifications after translation at the rough endoplasmic reticulum. Frequent post-translational modifications (PTM) are glycosylation, citrullination, methylation, acetylation, and ubiquitination of specific amino acids. PTM has relevant structural and functional consequences, allowing plasticity and functional diversity. Of special interest, PTM can have also immunogenic consequences, as autoantibodies recognizing specifically peptides with a modified amino acid are observed in RA. ACPA were the first autoantibodies against PTM proteins. Other RA-associated autoantibodies against proteins with PTM, such as carbamylation and acetylation, have been identified [88, 98]. These novel autoantibodies have been investigated in many studies aiming to discover and validate novel markers for diagnosis, disease activity assessment, and prognosis in RA. Only a few of these novel markers have come into clinical use.
How Autoantibodies Can Contribute to PM in Rheumatoid Arthritis
Multiple parameters contribute to estimating the potential disease severity and therapeutic requirements of patients with RA, including female gender, the clinical level of disease activity at presentation (joint count, extra-articular manifestations), acute-phase tests (C-reactive protein, erythrocyte sedimentation rate), and early imaging findings [99]. Autoantibodies (RF, ACPA, anti-carbamylated peptide) are among the variables associated with more aggressive disease [86, 100,101,102]. ACPA and RF have been demonstrated to be associated also with extra-articular manifestations, cardiovascular disease, and premature mortality in RA [103]. The genetic make-up also contributes to the severity of the disease. HLA-DRB1-SE alleles are associated with more severe disease and extra-articular manifestations, especially when present in both chromosomes [104]. In a more refined phenotypic analysis, it has been demonstrated that the coexistence of ACPA, RF, and HLA-DRB1-SE alleles is associated with the predominance of erosions over joint narrowing in RA patients [105]. Polymorphism in other genes, such as FOXO3, IL2RA, DKK1, GRZB, MMP9, and SPAG16, is associated with more severe disease [106,107,108]. Finally, the time to the introduction of disease-modifying therapy is an adjustable variable that also can affect the prognosis.
Although RA is a potentially severe and crippling disease, very early treatment has proven successful in avoiding an unfavorable evolution. It is now established that there is a window of opportunity for optimal therapeutic intervention at the earliest stages of the disease [109]. It is relevant that RF and ACPA are detectable in the serum of individuals for several years before the clinical onset of the disease [110, 111]. Two-thirds of individuals ultimately diagnosed with RA were positive for ACPA 6 to 10 years before their diagnosis [112]. Therefore, these autoantibodies have been instrumental in the very early identification of arthralgia patients that are bound to develop RA. The presence of such autoantibodies might enable the identification of people at increased risk of developing RA as well as patients at early stages of the disease, contributing to the timely treatment of patients within the RA period. However, the positive predictive value is moderate (~70%) and about 2–5% of the healthy population have ACPA. In addition, less than 50% of arthralgia patients with ACPA and/or RF develop RA within 1 year [113, 114]. Thus, the post-test probability for ACPA in RA has been estimated at only 50%, although it might be increased with very high titers of ACPA or by combining ACPA with other biomarkers [74]. Autoantibodies against an array of PTM proteins may contribute to increasing the accuracy in spotting very early RA patients. A recent meta-analysis investigating healthy controls, RA first degree relatives, pre-RA individuals, and RA patients indicated that the positivity for RF and/or ACPA yields a specificity and sensitivity of 65–100% and 59–88%, respectively, for the correct identification of RA and pre-RA patients, whereas the triple positivity of RF, ACPA, and anti-carbamylated peptide (CarP) antibody yielded a specificity of 98–100% and a sensitivity of 11–39% [115].
The conjugation of information on the genetic make-up should strengthen the prediction capability for the identification of very early RA, especially when analyzing arthralgia patients. In addition to the HLA-DRB1-SE alleles, over 100 RA susceptibility loci have been identified. Although most of these alleles have a weak association with RA, the cumulative effect of several of them under the appropriate environmental stimuli may result in a strong trend for RA development [74]. Interestingly, some susceptibility alleles (e.g., AFF3, CD28, and TNFAIP3) are associated with ACPA-positive RA whereas others (e.g., PRL and NFIA) occur in ACPA-negative RA [116, 117]. The interaction of genetic background, environmental agents, and autoantibodies can be relevant to the personalized management of individuals at risk for RA development. This is well illustrated by the observation that the association between tobacco exposure and RA development is strongest in ACPA-positive individuals with at least one copy HLA-DRB1-SE allele [103, 118]. It should be noted that not all autoantibodies against PTM show association in terms of relationship to tobacco exposure and HLA-DRB1 gene susceptibility [84]. This information may be relevant when recommending absolute smoking cessation in a particular individual. In addition to genetic and autoantibody parameters, inflammatory biomarkers may also contribute to PM in RA. For example, in conjugation with other biomarkers, calprotectin has been reported to have a role in the early diagnosis of RA [119, 120], as well as in predicting relapse after therapy discontinuation [121].
Finally, autoantibodies can contribute also to the selection of the appropriate therapeutic agent to be used in an individual patient. By identifying patients at risk of more severe disease, RF and ACPA help segregate potential candidates for the use of biological DMARD. In addition, the presence of RF and/or ACPA indicates a higher chance of response to some specific targeted-therapy agents. Thus, a recent pooled analysis from 16 European RA registries found that RA patients with RF and/or ACPA have a higher frequency of sustained remission under rituximab (5.9%; 95% CI 4.7–7.3) and abatacept (1.5%; 95% CI 1.1–1.9) than double-negative RA patients. Seropositive patients also had a slightly better response with tocilizumab compared to seronegative patients and no difference was observed regarding TNF inhibitors [122]. Tofacitinib, an oral Janus kinase (JAK) inhibitor approved for RA treatment, has been also found to be more effective in seropositive patients. Pooled data from five phase-III studies showed that a higher proportion of double-positive (ACPA and RF) RA patients achieved a favorable response to JAK-inhibitors than double-negative patients did [123]. Autoantibodies may also help in the decision of discontinuation of biological DMARD in RA, as observed in a systematic review that indicated that low levels or absent ACPA and RF predict successful discontinuation of therapy [124]. These observations indicate the potential of autoantibodies to help tailor the therapeutic strategy in RA.
Primary Sjögren’s Syndrome
Primary Sjögren’s syndrome (pSjS) is a systemic inflammatory disease characterized by lymphocytic infiltrates in exocrine glands, mainly salivary and lacrimal glands, with ensuing dryness of affected areas clinically manifested most often as xerostomia and keratoconjunctivitis sicca (sicca syndrome). In addition, there is a wide range of extra glandular manifestations, including interstitial nephritis, small vessel vasculitis with palpable purpura, peripheral neuropathy, lymphadenopathy, and splenomegaly [125]. pSjS affects predominantly middle-aged women with an estimated incidence of 6.92 per 100,000 person-years and prevalence of 60.8 cases per 100,000 inhabitants [126]. The clinical spectrum is heterogeneous, varying from mild benign sicca syndrome to heterogeneous degrees of lymphoid infiltration in different tissues/organs and evolving to lymphomatous lesions (non-Hodgkin lymphoma) in some patients [127].
The pathogenesis of pSjS is characterized by B-cell hyperactivation, which is the basis for the clinical and laboratory manifestations, such as hypergammaglobulinemia, high titer RF, lymph node enlargement, and lymphoid infiltration in several tissues and organs [128]. Ocular and oral mucosal dryness are characteristic phenotypic features in pSjS. However, sicca syndrome (i.e., oral and ocular mucosal dryness) and Sjögren’s syndrome are not synonymous, and most elderly adults with sicca syndrome do not have Sjögren’s syndrome. In Sjögren’s syndrome, there is autoimmune-based lymphocytic infiltrate and inflammation of the lacrimal and salivary glands, resulting in impaired tear and saliva production [125]. In contrast, several distinct mechanisms may lead to non-inflammatory sicca syndrome, including age-related atrophy and drug-related gland dysfunction. The correct identification of the basis for the sicca syndrome is very important since the identification of those patients with an autoimmune basis for their sicca manifestations is the first step in deciding whether therapies directed at the immune system might be beneficial and whether close monitoring for the appearance of lymphoma should be undertaken. In contrast, such therapies and their attendant risks should be avoided in patients with non-autoimmune sicca syndrome. Autoantibodies play a significant role in that matter.
The complexity and heterogeneity of pSjS, with its wide spectrum of glandular and extra glandular features, indicate the need for biomarkers for better discrimination and contribution to PM [129]. Autoantibodies contribute to the early diagnosis and stratification of patients according to the risk for systemic complications and development of lymphoma, thus contributing to individualized surveillance of pertinent complications and custom-made treatment of the patients. Immunological patterns defined by serology and other biomarkers contribute to predicting the phenotypic expression of the disease already at the time of diagnosis and may guide physicians to design specific personalized management during the follow-up of patients with pSjS [130, 131].
ANA, RF, anti-SS-A/Ro60, and anti-SS-B/La autoantibodies are key serological findings in pSjS. Autoantibodies to the Sjögren-related antigen A (also known as anti-SS-A/Ro60 antibodies) and the Sjögren-related antigen B (also known as anti-SS-B/La antibodies) are central for the pathobiology and diagnosis of this disease. Together with the development of sicca symptoms, systemic involvement, lymphocytic infiltration to exocrine glands, and the increased risk of lymphoma, these autoantibodies are pivotal elements in this disease [129]. As in other autoimmune diseases, the presence of autoantibodies can precede pSjS development for years. In seropositive pSjS patients, at least one autoantibody specificity (ANA, RF, anti-SS-A/Ro60, or anti-SS-B/La) was detected in 81% of these patients up to 20 years (median 4.3–5.1 years) before diagnosis [132].
Antinuclear Antibodies and Rheumatoid Factor
ANA are found in over 80% of patients with pSjS and have been proven very helpful in identifying the disease in patients presenting with sicca features. ANA frequently occur at moderate to high titer and typically present as a fine speckled nuclear pattern (AC-4 according to ICAP nomenclature), which is frequently associated with anti-SS-A/Ro60 and anti-SS-B/La [12]. In addition, some pSjS patients may present a peculiar nuclear and mitotic apparatus pattern (AC-26) characteristic of anti-NuMA antibodies. Anti-NuMA is also observed in SLE and other diseases but occurs at a higher frequency in pSjS [133]. RF is an autoantibody directed against the Fc region of IgG, being present at high titer in 50% of patients with pSjS and bearing association with several clinical, histopathological, and laboratory features [129]. Despite being helpful for diagnostic assessment, ANA and RF are not included in the current classification criteria for pSjS [134], as they are common in a range of autoimmune diseases and present low specificity for pSjS.
Anti-SS-A/Ro and Anti-SS-B/La Antibodies
Anti-SS-A/Ro antibodies are detected in up to 70% of patients with pSjS and have been detected several years before the diagnosis of pSjS [132]. The SS-A/Ro system includes two distinct and independent proteins of 60 and 52 kDa, respectively, although the original description probably referred only to the 60-kDa component [135]. Ro60 is a component of small cytoplasmic ribonucleoprotein complexes (hY-RNA) and binds misfolded noncoding RNA [136]. Ro52, also known as TRIM21, belongs to the Tripartite Motif Protein (TRIM) family, being involved in protein ubiquitination [137]. Antibodies to Ro52 and Ro60 may coexist in the same patient but frequently occur as independent autoantibodies. It should be noted that anti-Ro52 is best detected in immunoblot/immunodot and ELISA assays because it is not detected by HEp-2 IFA, immunoprecipitation, and/or double immunodiffusion [138]. It has been demonstrated that anti-Ro52 and anti-Ro60 antibodies have different clinical associations; however, some controversy exists probably as a result of different immunoassays used in the studies. Anti-Ro52 antibodies are preferentially detected in specific anti-Ro52 immunoassays and not detected in “general” anti-SS-A/Ro immunoassays [139]. The combination of Ro52 and Ro60 in some immunoassays represents a major confounding factor in the literature. Although most frequently observed in autoimmune patients, the exclusive presence of anti-Ro52 (absence of anti-Ro60) frequently occurs also in non-autoimmune patients. In addition, anti-Ro52 occurs in a wider spectrum of autoimmune patients as compared to anti-Ro60 antibodies [140]. Patients with anti-Ro52 and anti-Ro60 have a higher probability of presenting anti-SS-B/La compared to those with just one anti-SS-A/Ro component. The “triad” (anti-Ro-60, anti-Ro-52, and anti-SS-B/La) is strongly associated with pSjS and indicates more severe pSjS with higher severity of salivary gland lymphocytic infiltration, parotid enlargement, and hypergammaglobulinemia [140, 141]. In addition, anti-Ro52 antibodies have been associated with an increased risk of interstitial lung disease in pSjS patients [142]. In general, the presence of anti-SS-A/Ro (with or without anti-SS-B/La) is associated with more severe disease, characterized by systemic manifestations and a higher frequency of non-Hodgkin lymphoma. In a large series of 548 pSjS patients with documented salivary gland histopathological pSjS-specific alterations, Quartuccio et al. showed that the 342 patients with antibodies to SS-A/Ro and/or SS-B/La had a higher frequency of salivary glandular enlargement, purpura, leukopenia, decreased serum C3 and C4, hypergammaglobulinemia, ANA, RF, serum cryoglobulins and lymphoma as compared to 206 patients without anti-SS-A/Ro and anti-SS-B/La [143].
SS-B/La is a 48 kDa phosphoprotein involved in RNA metabolism and anti-SS-B/La antibodies are detected in up to 50% of patients with pSjS. The presence of anti-SS-B/La, especially when associated with anti-SS-A/Ro, indicates a less benign disease phenotype, with a higher prevalence of lymphoproliferative manifestations and a higher risk of evolution to lymphoma [144]. The presence of anti-SS-B/La antibodies without concomitant anti-SS-A/Ro antibodies is rather infrequent and usually marks less severe disease with fewer clinical and immunological features of the syndrome and with a relatively low frequency of severe organ-specific involvement [145, 146].
A small percentage of pSjS patients present ACPA and anti-centromere antibodies. Anti-centromere antibodies were associated with older age, more severe salivary gland dysfunction, lower frequency of anti-SS-A/Ro, anti-SS-B/La, and RF, as well as lower serum immunoglobulin. These patients have a higher frequency of Raynaud’s phenomenon, sclerodactyly, and dilated nail fold capillaries [147]. The presence of ACPA in pSjS patients is associated with a higher frequency of arthralgia and progression to RA [148].
Cryoglobulins
Also seen in pSjS patients, cryoglobulins are immunoglobulins that precipitate in vitro at temperatures below 37 °C and become soluble after rewarming. Circulating cryoglobulins are present in about 10% of the patients with pSjS and are associated with more severe disease [149]. Since mixed cryoglobulinemia is traditionally regarded as a crossroads between autoimmune disease and cancer [150], closer monitoring should be done in the presence of this immunological marker. Cryoglobulins in pSjS patients are associated with a higher frequency of systemic disease with extra glandular involvement, increased risk of B cell lymphoma, and higher mortality [151, 152]. Lower levels of complement C4, higher levels of RF, and serum monoclonal IgM gammopathy are associated with cryoglobulinemia in pSjS patients [149].
Low Complement Levels
The complement cascade and regulatory proteins are involved in the pathogenesis of the SjS and other autoimmune diseases [153]. Found in 10–25% of patients with pSjS, low levels of complement (C3 and/or C4) have been associated with more severe disease and poor prognosis. A recent multi-ethnic international cohort comprising 10,500 pSjS patients from 22 countries has found a prevalence of low C3 and C4 levels of 13.4% and 14.5%, respectively [130]. Besides cryoglobulin, low C3 and low C4 levels significantly correlated with systemic activity [130]. Like cryoglobulin, hypocomplementemia has been associated with a higher risk for B cell lymphoma progression and death [151]. Type II mixed cryoglobulins with RF activity and hypocomplementemia are the strongest and most validated predictors of lymphoma in pSjS [152, 154].
Monoclonal Gammopathy
Monoclonal gammopathy related to pSjS has been recognized as a key marker of disease prognosis and outcome. Circulating monoclonal immunoglobulins have been found in up to 22% of patients with pSjS, with monoclonal IgGκ being the most frequent band type [151, 155]. Parotid enlargement, vasculitis, neurological involvement, higher frequency of progression to lymphoma, and lower survival have all been associated with monoclonal gammopathy in pSjS patients [155].
Systemic Sclerosis
Systemic sclerosis (SSc) is a chronic autoimmune rheumatic disease characterized by a triad of abnormalities including vasculopathy, fibrosis of the skin and internal organs, and immune dysregulation [156]. The reported incidence and prevalence of SSc vary widely depending on geographic location and methods used in each study. The prevalence of SSc varies from 7 to 489 cases per million and the annual incidence from 0.6 to 122 cases per million inhabitants [157]. SSc is more frequent in women with a female to male ratio of 4:1 to 6:1 and a peak incidence between ages of 45 and 64 years.
The clinical manifestations of the disease are highly heterogeneous, although a common feature heralding the onset of the disease is Raynaud’s phenomenon. Once the diagnosis has been made, classification into disease subsets, as well as stratification of risk of future organ involvement and other prognostic features are extremely important in clinical practice [158]. Patients with SSc are classified based on the extent of skin involvement: (1) diffuse cutaneous SSc (dcSSc) with skin involvement proximal to the elbows and knees and/or truncal involvement; (2) limited cutaneous SSc (lcSSc) with restricted involvement affecting the hands and limbs below the elbows or knees, with or without face and neck involvement. In general, these two subsets have distinct clinical courses as well as organ involvement and specific serum autoantibody profiles, with a more severe prognosis in patients with dcSSc [158, 159]. A small number of patients have clinical features of SSc but no evidence of cutaneous involvement (SSc sine scleroderma).
A hallmark of SSc is the presence of circulating autoantibodies reactive with various cellular components in over 95% of the patients. Anti-topoisomerase I, anti-centromere (ACA), and RNA polymerase III (RNAP) represent the three most frequently detected autoantibodies in SSc and are considered highly specific for this disease [160]. Other SSc-specific autoantibodies include anti-U3-RNP/fibrillarin, anti-Th/To, anti-RNA-polymerase I and II, and anti-U11/U12 RNP [161]. Some autoantibodies, including anti-PM/Scl, anti-Ku, anti-U1-RNP, anti-SS-A/Ro60, anti-Ro52/TRIM21, and anti-NOR 90, reported in other autoimmune diseases, are also found in SSc patients [160]. The most frequent antibodies in SSc and their clinical association are depicted in Table 9. As autoantibodies may precede the onset of symptoms, they are helpful for the early diagnosis of the disease [162]. In addition to contributing to the diagnosis, autoantibodies are associated with distinctive clinical manifestations and prognostic profiles in SSc. Therefore, they are attractive biomarkers for SSc and might help identify and predict the clinical outcome of SSc patients [163].
Anti-Topoisomerase I
Anti-topoisomerase I (anti-Topo I or anti-Scl-70) was originally isolated as an antibody that reacted with a 70 k-Da protein in immunoblot, in retrospect realized to be a degradation product of the full-length protein that was later identified as the 100-kDa DNA topoisomerase I, an enzyme that catalyzes relaxation of supercoiled double-stranded DNA [159]. Anti-topo I antibodies are detected in 17–41% of patients and are highly specific for SSc [159,160,161,162]. Anti-topo I is typically associated with dcSSc, although it can be found also in some cases of lcSSc [163]. Anti-topo I antibodies are associated with a higher risk of severe interstitial lung disease (ILD) [162], presence of digital ulcers, cardiomyopathy, high skin score [164], and a more severe phenotype with an increased risk of mortality [159, 160, 162, 165]. Finally, anti-topo I antibodies have been associated with malignancies in some studies [166]. Thus, all SSc patients with anti-topo I should be screened and closely monitored for the presence of ILD and cardiac involvement with high-resolution chest CT (HRCT), pulmonary function testing, electrocardiogram, and transthoracic echocardiogram, especially in the first five years of disease [167].
Anti-Centromere (ACA)
The main targets of ACA are centromere proteins (CENP) CENP-A, CENP-B, and CENP-C, although CENP-B, an 80-kDa kinetochore protein, seems to be the primary autoantigenic target with several reactive epitopes recognized by ACA in SSc [168]. ACA were first described when HEp-2 cells came into use as the substrate of choice for ANA testing because they produce a characteristic centromere staining pattern [160]. The frequency of ACA in SSc has been reported to be 20–42% in many ethnic groups [161, 169].
These antibodies are associated with lcSSc, long-standing Raynaud’s phenomenon, presence of calcinosis, and a higher risk of developing pulmonary arterial hypertension (PAH) [169]. When found in patients with Raynaud's phenomenon, ACA indicates a high probability of progression to SSc [170]. Survival rates of patients with ACA are better than those of patients with most of the other SSc-associated antibodies including anti-topo I [165]. The presence of ACA is not exclusive of SSc and has been detected in patients with primary biliary cholangitis, pSjS and even in SLE [171].
Anti-RNA Polymerase III (RNAP III)
Anti-RNAP III antibodies target the 115-kDa and 138-kDa components of RNA polymerase III and are detected in 5 to 25% of SSc patients with high variability among different ethnic-geographic groups [159, 160]. As anti-RNAP III antibodies frequently coexist with antibodies to RNAP I and RNAP II, the HEp-2 IFA pattern may show as fine speckled nucleoplasmic staining with additional coarse speckles and speckled nucleolar pattern [11]. Anti-RNAP III is highly specific for SSc, especially the dcSSc subset, and indicates a high risk of severe, rapidly progressing cutaneous thickening and higher risk of renal crisis [172, 173]. Scleroderma renal crisis has been reported in RNAP III-positive patients with SSc sine scleroderma [174]. It has also been shown that patients with anti-RNAP III antibodies present a higher risk of development of malignancy, especially within the first years of disease onset [166, 173]. Anti-RNAP III has also been associated with a higher risk for gastric antral vascular ectasia (GAVE) [173, 175].
Of special interest for SSc, anti-RNAP III antibody-positive patients should have regular screening for age-appropriate cancer and be alert to the increased risk of renal crisis. Appropriate monitoring of blood pressure should be performed for early detection of renal crisis since the prompt initiation of angiotensin-converting enzyme inhibitor can be life-saving [160, 167].
Anti-U3-RNP/Fibrillarin
Anti-U3-RNP/fibrillarin antibodies target the nucleolar U3-RNP complex, involved in pre-rRNA processing. Anti-fibrillarin is detected in 4–10% of SSc patients and is more frequent in African-Americans [176, 177]. They are more frequent in patients with dcSSc and are associated with multi-organ involvement [159, 160], increased risk of cardiac involvement, renal crisis, ILD, PAH, and small bowel and muscle involvement. In a study of an African-American SSc cohort, anti-fibrillarin was associated with younger age of onset, higher frequency of digital ulcers, pericarditis, and severe lower gastrointestinal involvement, but less severe ILD and no change in survival [176]. Altogether, anti-U3-RNP/fibrillarin antibodies indicate a worse prognosis in SSc patients [159, 177]. A limitation of detecting anti-fibrillarin is the lack of a high-sensitivity and -specificity immunoassay in the clinical laboratory.
Anti-Th/To
Anti-Th/To antibodies target proteins 18–120 kDa associated with Th/7–2 and To/8–2 RNA. Anti-Th/To is relatively specific for SSc and occurs in 1–13% of patients, especially in those with lcSSc [159,160,161]. Anti-Th/To is associated with a higher frequency of ILD, PAH, and scleroderma renal crisis. The increased frequency of organ involvement results in reduced survival among these patients [178]. Patients with idiopathic ILD and a homogeneous nucleolar HEp-2 IFA pattern (AC-8) frequently have anti-Th/To antibodies and may progress to full-blown SSc or systemic sclerosis sine scleroderma [179].
Other Antibodies Associated with SSc
Other antibodies found in patients with SSc include anti-PM/Scl, anti-U1-RNP, anti-Ku, anti-U11/U12 RNP, anti-Ro52, and anti-NOR-90. Anti-Ro52 occurs in up to 20% of SSc patients and is reported to be associated with ILD and overlap syndrome [180]. Anti-U11/U12 RNP is highly specific for SSc, but occurs in only 1–3% of patients with this disease, being associated with severe ILD and severe pulmonary involvement [181]. Anti-PM/Scl antibodies are detected in 3–13% of SSc patients [236] and are more frequent in patients with lcSSc as well as in overlap syndrome with myositis, joint involvement, and calcinosis. Anti-PM/Scl antibodies may also be detected in the serum of patients with polymyositis, dermatomyositis, and undifferentiated connective tissue disease [182, 183]. Severe organ involvement is rare, and therefore anti-PM/Scl antibodies indicate a favorable prognosis.
Anti-U1-RNP are detected in 6–7% of patients with SSc. Anti-U1 RNP was first characterized as an antibody associated with mixed connective tissue disease (MCTD), but it can be also detected in patients with pure SSc as well as in other autoimmune rheumatic diseases, such as SLE [159,160,161]. In SSc, anti-U1-RNP is associated with limited skin involvement, Raynaud’s phenomenon, arthritis, myositis, and overlap syndrome. The association with PAH is observed in some cohorts. The general prognosis tends to be favorable.
Anti-Ku is detected in 2–4% of SSc patients [159,160,161] and has been associated with lcSSc, presence of myositis, ILD, arthritis, and less vascular involvement [184]. This autoantibody has also been described in patients with SLE, dermatomyositis (DM), and polymyositis (PM). Anti-NOR-90 antibodies can be detected in 4–6% of patients with SSc but are also present in other autoimmune diseases such as RA, SLE, and Sjögren’s syndrome [185] as well as in sera of some patients with malignancy [163]. When it is the only autoantibody in the sample, anti-NOR-90 yields a characteristic HEp-2 IFA pattern (AC-10) characterized by nucleolar speckled pattern and up to 10 discrete bright dots at the metaphase plate [11]. Although large-scale studies are not available, anti-NOR 90 antibodies may be considered a marker of limited SSc and mild involvement of internal organs.
Idiopathic Inflammatory Myopathies
Idiopathic inflammatory myopathies (IIM) are a heterogeneous and rare group of autoimmune disorders that affects the skeletal muscles and multiple organs. Historically, IIM was classified into two main subgroups: polymyositis and dermatomyositis (DM) [186, 187]. The progressive discovery of myositis-specific antibodies (MSA) and the refinement of specific clinical and histopathological features have gradually improved and expanded the classification into a more comprehensive and personalized framework. Although not established as a formal classification system for inflammatory myopathies, distinct subsets of IIM have been recognized, including PM, adult DM, juvenile DM, amyopathic DM, sporadic inclusion body myositis (sIBM), immune-mediated necrotizing myopathy (IMNM), and anti-synthetase syndrome (ASS). In view of the current classification system, PM has now largely been considered a diagnosis of exclusion [188, 189].
The annual incidence of IIM ranges from 0.58 to 19 per million and the prevalence from 2.4 to 33.8 per 100,000 inhabitants [190]. It should be noted, though, that epidemiological data are quite variable since IIM are rare and diagnostic and classification criteria have changed significantly during the last decades. In general, IIM are most common in females with a female/male ratio of 2:1 with a peak prevalence between 45 and 60 years of age.
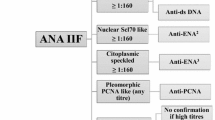
As in other autoimmune rheumatic diseases, autoantibodies are useful biomarkers for the diagnosis and classification of IIM. Autoantibodies, detected in up to 60% of IIM patients, have been classified into myositis-specific autoantibodies (MSA) and myositis-associated autoantibodies (MAA) [191]. Classic MSA include anti-Jo-1 (histidyl transfer RNA synthetase) and antibodies to other aminoacyl transfer RNA synthetases (ARS), anti-Mi-2, and anti-signal recognition particle (SRP) antibodies (Fig. 1). The most frequent MAA include anti-PM/Scl, anti-Ku, anti-U1-RNP, and anti-Ro52, which are found also in other conditions including SSc, SLE, and overlap syndromes [192].
Myositis-specific autoantibodies. Jo-1: histidyl transfer RNA synthetase; PL7: threonyl-tRNA synthetase; PL12: antalanyl-tRNA synthetase; EJ: glycyl tRNA synthetase; OJ: isoleucyl-tRNA synthetase; Ha: tyrosyl-tRNA synthetase; KS: anti-asparagyl-tRNA synthetase; Zo: phenylalanyl-tRNA synthetase; Mi-2: complex nucleosome remodeling histone deacetylase; TIF1γ: transcriptional intermediary factor 1; NXP-2: nuclear matrix protein 2; MDA-5: melanoma differentiation-associated protein 5; SAE: small ubiquitin-like modifier activating enzyme; SRP: signal recognition particle; HMGCR: 3‑hydroxy‑3‑methylglutaryl CoA reductase: cN1A: cytosolic 5′-nucle-otidase 1A
In recent years, major advances have been made in the characterization and the discovery of new autoantibodies in IIM. As such, a major shift has been made including the recognition of autoantibodies specifically associated with sIBM, distinct subsets of DM, and a higher risk of cancer or ILD. The detection of MSA and MAA has become a key feature for early diagnosis and classification of IIM, contributing decisively to the definition of clinically distinguishable IIM subsets, stratification of risk of organ involvement, and to a more personalized approach [191, 192]. The most noteworthy autoantibodies identified to date and their clinical associations, summarized in Table 10, are discussed as follows.
Anti-ARS
Autoantibodies against ARS represent the most common MSA and can be detected in 22–35% of IIM patients [191,192,193]. These autoantibodies target a family of cytoplasmic amino acid-charging enzymes, named aminoacyl transfer RNA (tRNA) synthetases (ARS). At least eight anti-ARS have been identified including anti Jo-1 (anti-histidyl-tRNA synthetase), anti‑PL7 (anti-threonyl-tRNA synthetase), anti‑PL12 (anti-alanyl-tRNA synthetase), anti‑EJ (anti-glycyl tRNA synthetase), anti‑OJ (anti-isoleucyl-tRNA synthetase), anti‑Ha (anti-tyrosyl-tRNA synthetase), anti‑KS (anti-asparaginyl-tRNA synthetase), and anti‑Zo (anti-phenylalanyl-tRNA synthetase) antibodies (Fig. 1). Anti-Jo-1 antibodies are the most common, occurring in approximately 20% of adult patients with IIM, and the other anti-ARS are collectively found in 1–6% of patients [192, 194].
Anti-ARS autoantibodies are associated with the anti-synthetase syndrome, which is characterized by a spectrum of typical clinical manifestations including myositis, ILD, arthritis, fever, Raynaud’s phenomenon, and mechanic’s hands. However, anti-ARS antibodies seem to be associated with heterogeneous disease expression and severity, and not every patient with an anti-ARS autoantibody has every feature of the anti-synthetase syndrome. For example, muscle involvement and arthritis are more common in patients with anti‑Jo-1 compared to non-Jo-1 patients [195], whereas the presence of anti‑PL7 or anti‑PL12 antibodies is associated with a higher rate of ILD and a higher risk of mortality [195, 196]. Anti-ARS autoantibodies are rare in DM, JDM, and other autoimmune rheumatic diseases.
Dermatomyositis-Specific Autoantibodies
To date, five dermatomyositis-specific autoantibodies are identified: anti-complex nucleosome remodeling histone deacetylase (Mi-2), anti-transcriptional intermediary factor 1 (TIF1) γ, anti-nuclear matrix protein 2 (NXP-2), anti-melanoma differentiation-associated protein 5 (MDA5), and anti-small ubiquitin-like modifier activating enzyme (SAE) [189].
Anti-Mi-2, the first specific autoantibody described in DM, is the most common antibody associated with DM, occurring in up to 20% of adult patients and up to 10% of JDM. Anti-Mi-2 is associated with classic features of DM including Gottron papules/sign, heliotrope rash, nail fold erythema, and violaceous rash including the V-sign and Holster sign. These patients tend to present with severe myositis, but they typically respond well to steroid therapy and have a good prognosis and a decreased risk of cancer compared with DM patients who are anti-Mi-2-negative [192, 196, 197].
Anti-TIF1γ was first described as a macromolecular complex of 155/140-kDa proteins and was subsequently identified as the main autoantibody target of the TIF1 (α, β, γ subunits) family of proteins [198]. Anti-TIF1γ antibodies are strongly associated with malignancies in adult DM patients. In clinical practice, given the high association of anti-TIF1γ with malignancy, this antibody is considered a key biomarker for cancer in the setting of DM [191, 192]. Anti-TIF1γ is also associated with typical skin rash, photosensitivity, and low frequency of Raynaud’s phenomenon and ILD. Interestingly, these antibodies might also be detected in patients with JDM, but the association with cancer does not apply to children and adolescents [191].
Anti-NXP-2 is an autoantibody first described in a cohort of JDM and juvenile polymyositis patients. Of interest, anti-NXP-2 antibody is characteristically associated with a HEp-2 IFA pattern of multiple discrete nuclear dots (AC-6) [199]. When detected in adult DM, it is strongly associated with malignancy. Anti-NXP-2 is more frequent in JDM with a frequency of 15 to 22% and is associated with a higher risk of developing calcinosis and severe muscle involvement [195, 196].
The anti-MDA-5 antibody, originally named anti-CADM-140 antibody, binds to a 140-kDa cytoplasmic protein and was first described in Asian cohorts as strongly associated with clinically amyopathic DM (CADM) [192, 197]. In addition, anti-MDA-5 antibodies are associated with rapidly progressive ILD and a high risk of mortality [200]. Patients with anti-MDA-5 antibodies might also have atypical skin lesions with cutaneous ulcerations, characteristic palmar violaceous macules/papules, hand swelling, and arthritis [201].
Antibodies to SAE were first identified in 2007 by Betteridge et al. in 11 DM patients [202]. Since then, anti-SAE has been described in several adult DM cohorts with varying frequencies of 1.5–8%. Patients tend to present with extensive skin rash, followed by muscle weakness and systemic manifestations including gastro-intestinal involvement with dysphagia [202].
Autoantibodies Associated with Immune-Mediated Necrotizing Myositis (IMNM)
IMNM is a subtype of myositis characterized by distinct clinical and histopathological features and strong association with antibodies to SRP and to 3‑hydroxy‑3‑methylglutaryl CoA reductase (HMGCR). Patients with IMNM typically present with acute severe muscle weakness, with very high creatine kinase levels, as well as resistance to conventional immunosuppressive therapy. Characteristically, muscle biopsy histopathology shows marked myofibril necrosis with minimal or no inflammatory infiltrate [203].
Anti-SRP antibodies are reported in approximately 5% of all IIM patients and are associated with severe necrotizing myositis, intense muscle weakness, dysphagia, cardiac involvement, and ILD. Anti-HMGCR autoantibodies are associated with IMNM and with the use of statins, although not all patients with these autoantibodies have a history of exposure to prescribed statins. The relationship of anti-HMGCR antibodies and statins is intriguing as HMGCR is the pharmacologic target of statins [203]. Patients with anti-HMGCR-associated myopathy present with weakness, myalgia, and high CK levels, although not always as dramatic as seen with SRP myopathy. Statin-naïve IMNM patients with anti-HMGCR antibodies were reported to be younger, with higher CK levels, and less responsive to treatment as compared to those that received statins.
Anti‑cN1A Antibody and Sporadic Inclusion Body Myositis
Sporadic inclusion body myositis (sIBM) is a distinct form of IIM characterized by insidious onset of muscle weakness, an asymmetric pattern of muscle involvement, typical involvement of long finger flexors, quadriceps, and tibialis anterior, but only mild elevation of CK. Dysphagia is common and may present as the initial symptom [188]. The therapeutic response to immunosuppression is poor. In contrast to other inflammatory myopathies, until recently myositis-specific autoantibodies had not been found in sIBM patients. Autoantibodies directed against major epitopes of cN-1A (also known as Mup-44, NT5c1A) are found in 30–50% of patients with sIBM, which has helped distinguish sIBM patients within the context of inflammatory myopathy [204]. Anti-cN1A has moderate sensitivity and high specificity for sIBM. The presence of anti-cN1A antibodies may be associated with muscle weakness but were not associated with a specific HEp-2 IFA staining pattern, hence screening using HEp-2 substrates is unlikely to be a useful predictor for the presence of these autoantibodies [205]. Anti-cN-1A has been observed also in other autoimmune diseases, particularly Sjögren's syndrome and SLE [205, 206]. There are reports of anti-cN1A in JDM [205], but this is at variance with another recent study [207]. Hence, standardization and harmonization of anti-cN1A assays are very important for future clinical use.
Autoimmune Liver Diseases
Autoantibodies are important biomarkers for the investigation of hepatitis and cholestasis of unknown origin and are part of the criteria in the diagnostic scoring system of autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) (Fig. 2) [208,209,210]. Herein, we address the clinical associations of autoantibodies in autoimmune liver diseases and their contribution to PM.
Autoantibodies associated with autoimmune hepatitis and primary biliary cirrhosis. AIH: autoimmune hepatitis; SMA: smooth muscle antibody; LKM: liver kidney microsome; SLA/LP: soluble liver antigen/liver-pancreas; ASGRP: asyalo glycoprotein receptor protein; LC: liver cytosol; ANA: antinuclear antibody; TRIM21: tripartite motif family of proteins; ANCA: anti-neutrophil cytoplasm antibody; AMA: anti-mitochondria antibody; gp210: glycoprotein 210; KLHL12: kelch-like 12; HK-1: hexokinase 1
Autoimmune Hepatitis
AIH is a chronic inflammatory liver disease with unknown underlying etiology. Distinctive findings are the presence of autoantibodies, high serum levels of immunoglobulin G (IgG) and gamma globulin, and plasma cell hepatic infiltrates [211]. Most autoantibodies in AIH are not disease specific and should be considered along with other clinical, laboratory, and histological elements. Moreover, autoantibodies are lacking in 10–15% of AIH patients, although some of these “seronegative” patients may develop autoantibodies later in the disease course [212]. In addition to pointing to an autoimmune basis and contributing to the diagnosis, autoantibodies help in the differentiation of the two types of AIH (Table 11; Fig. 2). Type I AIH affects mainly adults and is the most prevalent form of AIH, whereas type 2 AIH occurs at a younger age, frequently in children, and has a more aggressive course [213]. Antinuclear antibody (ANA), anti-smooth muscle antibodies (SMA), and anti-F-actin antibodies are typically associated with type 1 AIH [208], whereas antibodies to LKM-1 (liver/kidney microsome 1) and LC-1 (liver/cytosol 1) occur almost exclusively in type 2 AIH [214, 215].
SMA occur in circa 50% of type 1 AIH patients and can be the only autoantibody present [211, 212]; however, SMA, especially at low titer, may occur in other diseases, including non-alcoholic fatty liver disease (NAFLD) and other liver diseases [216]. In the stomach/kidney/liver indirect immunofluorescence assay (SKL-IFA), SMA reacts with microfilaments in several locations, including transversal fibers in gastric mucosa, muscularis mucosae, muscular layer of arteries, glomerulus, and renal tubules. Higher specificity of SMA for AIH occurs with the reactivity to the vascular, glomerular, and tubular components (VGT pattern) [217]. Filamentous actin (F-actin) is the main target of autoantibodies in samples that have the VGT pattern and anti-F-actin antibodies are rather specific for AIH. Anti-F-actin antibodies are determined preferentially by IFA on fibroblasts treated to display the filamentous form of actin. The preservation of filamentous F-actin in ELISA tests may be an issue, resulting in lower specificity for AIH [218, 219].
Anti-neutrophil cytoplasmic antibodies (ANCA) occur in a series of diseases and the immunofluorescence pattern helps trim down the spectrum of associated diseases. The cANCA pattern is associated with anti-proteinase 3 (PR3) antibodies and occurs predominantly in granulomatosis with polyangiitis. The pANCA pattern is associated with anti-myeloperoxidase (MPO) antibodies and occurs in several conditions, including microscopic polyangiitis, rapidly progressive glomerulonephritis with crescents, and small-vessel vasculitis. Of interest to liver autoimmunity, the atypical pANCA pattern is most frequently associated with type 1 AIH, progressive sclerosing cholangitis (PSC), and ulcerative colitis, and the identity of the target autoantigens is a matter of debate [217, 220].
Anti-LKM-1 antibodies target cytochrome P450 CYP 2D6 and are relatively specific for type 2 AIH, although they occur in occasional patients with hepatitis C (HCV), PBC, and PSC [221,222,223]. Anti-LC1 antibodies target the enzyme formiminotransferase cyclodeaminase and occur in ~25% of patients with type 2 AIH, most frequently in association with anti-LKM-1 antibodies [224, 225]. Although highly suggestive of AIH, anti-LC1 may occur in occasional HCV patients [225]. On the other hand, anti-SLA/LP is highly specific for type 1 AIH and is associated with a more severe disease course [226, 227]. Anti-SLA/LP recognizes the cytosolic protein O-phosphoseryl-tRNA:selenocysteine-tRNA synthase and is not amenable to detection by IFA on HEp-2 cells or rodent tissue cryosections [220]. Anti-SLA/LP adds value in the laboratory workup of AIH because it can occur as the only autoantibody and has prognostic implications. It is present in no more than 20% of the patients and indicates a more severe disease, especially when associated with anti-Ro52 antibodies [228]. Anti-Ro52 antibodies are observed in ~30% of AIH patients and have been associated with more severe disease with higher probability of cirrhosis, hepatic failure, and liver transplantation [228]. In addition to AIH, anti-Ro52 occurs in several autoimmune rheumatic diseases, including SLE, pSjS, SSc, and immune-mediated inflammatory myopathies. Antibodies against the hepatocyte membrane asialoglycoprotein receptor (ASGPR) occur in 25–80% of patients with AIH and seem to be associated with histologic disease activity, as ASGPR titer and frequency drop with disease remission. ASGPR is observed at low titer in other liver diseases, including viral hepatitis and PBC [229]. Therefore, moderate to high titers anti-ASGPR are more reliable as a biomarker for AIH.
The HEp-2 IFA test is very informative in the investigation of patients with autoimmune liver diseases, as a homogeneous or fine speckled nuclear pattern is present in 50–80% of type 1 AIH patients [230]. However, it should be noted that a positive HEp-2 IFA test occurs in 13–22% of the general population [8, 231, 232] as well as in patients with non-autoimmune diseases including non-alcoholic fatty liver disease (NAFLD) [233]. Interestingly, several of the liver autoantibodies produce distinctive HEp-2 IFA patterns (Fig. 3) and the recognition of such patterns should guide disease-specific immunoassays for definitive autoantibody identification. A very distinctive cytoplasmic HEp-2 IFA pattern, observed in HCV patients treated with interferon-alpha and ribavirin, is characterized by a cytoplasmic discrete “rods and rings” IFA pattern (AC-23) (Fig. 3). The target antigen is inosine-5′-monophosphate dehydrogenase 2 (IMPDH2) and the cognate autoantibodies appear a few months after initiation of ribavirin therapy [234]. Of interest for PM, Carcamo et al. found that higher titer anti-IMPDH2 antibodies indicate a poor response to therapy [235]. However, this has not been generally observed in other studies [234, 236].
HEp-2 indirect immunofluorescence assay (HEp-2 IFA) patterns associated with autoimmune liver diseases. a Multiple discrete nuclear dots pattern (AC-6) associated with anti-sp100 antibodies and cytoplasmic reticular mitochondria-like pattern (AC-21). b Punctate nuclear envelope pattern (AC-11), associated with anti-gp210 antibodies. c Centromere pattern (AC-3), associated with antibodies to centromere protein A (CENP-A), CENP-B, and CENP-C. d Cytoplasmic rods and rings pattern (AC-23), associated with anti-inosine monophosphate dehydrogenase 2 (IMPDH-2) antibodies
It should be noted that several liver autoantibodies do not yield relevant IFA reactivity on HEp-2 cells, as occurs with antibodies to LKM-1, LC1, ASGPR, SLA/LP, and atypical pANCA. In contrast, the SKL-IFA provides useful information regarding antibodies to LKM-1, LC1, SMA, and mitochondria (AMA) (Fig. 4). Once the pattern associated with one of these autoantibodies is identified in testing a given sample, the suggested autoantibody specificity can be confirmed using antibody-specific tests based on ELISA, chemiluminescence immunoassay (CLIA), western blot, line blot, or other solid-phase immunoassays. Again, some liver autoantibodies yield no reactivity in SKL-IFA or HEp-2 IFA, such as anti-SLA/LP and anti-ASGPR.
Immunofluorescence patterns observed in the indirect immunofluorescence assay on rodent tissue cryosections. a Smooth muscle antibodies staining the muscularis mucosae and muscle layer (M) in the gastric mucosa, glomeruli (G), and extracellular fibrils around renal tubules (white arrows). b Smooth muscle antibodies staining the muscle layer of an arteriole (A) and extracellular fibrils around renal tubules (white arrows). c Anti-mitochondria antibodies cause a cytoplasmic coarse speckled staining of hepatocytes (left) and kidney tubular cells (right). d Anti-LKM-1 antibodies cause a strong and dense fine speckled staining of the cytoplasm of hepatocytes (left) and proximal tubule cells (right); distal tubules are weakly or not stained at all (counterstained in red)
The considerable heterogeneity in the prognosis of AIH is of relevance for PM. While most patients have good long-term survival upon early diagnosis and treatment, some have a severe course culminating in liver failure and the need for liver transplantation [237]. The linkage of autoantibodies to information about other relevant parameters adds value to the definition of disease phenotype, thus contributing to the goals of PM. In the context of AIH, a more severe prognosis is heralded by the presence of anti-SLA/LP antibodies, disease onset before 18 years, and histologic evidence of fibrosis at diagnosis [227, 238, 239]. In contrast, the presence of the HLA-DRB1*0401 allele speaks for a better prognosis [227, 240]. The presence of AMA in the context of AIH indicates the possibility of an AIH/PBC overlap syndrome. Such patients should be monitored for the development of increased serum alkaline phosphatase and the need for specific treatment with ursodeoxycholic acid [241, 242].
Primary Biliary Cholangitis
PBC is a chronic non-suppurative granulomatous inflammation affecting the small intrahepatic bile ducts [209]. PBC predominates in women and has a very insidious onset and course, being frequently diagnosed only at late stages when cirrhosis is established. Chronic pruritus and malaise are hints that should prompt investigation of PBC. Elevated serum canalicular liver enzymes (mainly alkaline phosphatase and gamma-glutamyl transferase) indicate the possibility of biliary tract involvement, whereas elevated IgM and cholesterol bring PBC to attention.
Over 98% of the patients have autoantibodies, most commonly directed to mitochondrial targets (AMA). AMA bind a series of enzymes in the outer mitochondria membrane with E2 pyruvate dehydrogenase complex (PDC-E2) being the main one. The presence of AMA is highly specific for PBC and is one of the three criteria for the diagnosis of the disease [210]. It should be noted, however, that some patients with acute liver injury may have transient AMA [243]. In a chronic cholestatic patient with no evidence of another underlying disease, the presence of sustained high alkaline phosphatase levels and AMA (or other PBC-associated autoantibodies) is accepted for the diagnosis of PBC [209]. In patients with established PBC, anti-PDC-E2 antibodies of the IgA class or IgG3 subclass indicate a more aggressive disease [244]. Other autoantibodies specifically associated with PBC are anti-gp210 and anti-sp100. In addition, circa 30% of the patients have anti-centromere antibodies, which are more commonly associated with systemic sclerosis.
The incidental finding of a cytoplasmic mitochondria-like pattern (AC-21) in the HEp-2 IFA test is suggestive of AMA and, therefore, often leads to reflex AMA-specific tests and when these are positive a diagnostic dilemma ensues. If serum alkaline phosphatase levels are normal and there is no evidence of cholestasis or other PBC-related features, no specific treatment is warranted. However, these patients should have follow-up alkaline phosphatase levels monitored and eventual elevation should prompt further investigation with imaging studies, e.g., acoustic radiation force impulse imaging (ARFI) or magnetic resonance, which may culminate in indication for liver biopsy. This approach may contribute to the prognosis as it has been demonstrated that early treatment with ursodeoxycholic acid is crucial for optimal outcome [245].
Up to 50% of the AMA-negative PBC patients have other autoantibodies detected in the HEp-2 IFA test (Table 11; Fig. 2), yielding characteristic patterns, such as the multiple discrete nuclear dots pattern (AC-6), associated with anti-sp100 and anti-PML, the punctate nuclear envelope pattern (AC-12), associated with anti-gp210, and the centromere pattern (AC-3), associated with anti-CENP-B/A. Anti-sp100 occurs in circa 30% of PBC patients and may occasionally occur in other systemic autoimmune diseases and in AIH [246]. Anti-PML antibodies occur in approximately 20% of PBC patients and frequently coexist with anti-sp100 antibodies [247]. The co-occurrence of anti-sp100 and anti-PML antibodies has been associated to a more rapid and severe progression of PBC [248]. Anti-gp210 antibodies occur in 20% of all PBC patients and in 30–50% of AMA-negative PBC. The coexistence of AMA frequently obscures the punctate nuclear envelope pattern (AC-12) associated with anti-gp210 antibodies, which can be resolved by using gp210-specific immunoassays. The presence of anti-gp210 has been associated with more aggressive disease [249, 250] and higher incidence of hepatocellular carcinoma [251]. In addition, anti-gp210 is associated with higher frequency of PBC/AIH overlap syndrome. Anti-centromere antibodies are observed in up to 30% of PBC patients and have been associated to increased frequency of portal hypertension [250] and more aggressive disease [249, 252]. Other autoantibodies that may add key evidence for PM include antibodies to kelch-like 12 (KLHL12) and hexokinase 1 (HK-1), which were recently identified as new biomarkers for PBC and notably identified patients who are negative for conventional autoantibodies described above [253].
The PBC/AIH overlap syndrome occurs in circa 10% of PBC patients [254], who tend to present worse prognosis, with lower 5-year survival rate and higher frequency of esophageal varices, gastrointestinal bleeding and liver transplantation [255] as well as poorer response to treatment with ursodeoxycholic acid [256]. Therefore, non-invasive parameters for the identification of PBC/AIH overlap syndrome can help the design of personalized management of such patients. Different authors have shown that PBC/AIH overlap syndrome is particularly associated with antibodies to gp210 [249, 257] and to double-stranded DNA (dsDNA) [257, 258]. Autoantibodies to the tumor suppressor p53 were found to be highly associated with PBC/AIH overlap syndrome in Japanese patients (344), but this was not confirmed in a Canadian cohort [259]. Of interest, the combination of antibodies to dsDNA and elevated serum levels of IgG and alanine aminotransferase (ALT) is highly predictive of PBC/AIH overlap syndrome [257].
The Opportunity of Fine-Tuning the Diagnostic Scoring Systems of AIH and PBC Aiming at Improvement in PM in Liver Autoimmune Diseases
Specific autoantibodies play different roles in the scoring systems of AIH and PCB. Thus, for the diagnosis of AIH, the presence of anti-SMA, anti-LKM-1, and ANA scores one to three positive points each according to the titer (1/40, 1/80, and > 1/80, respectively), whereas the presence of AMA scores one negative point [207]. In contrast, for the diagnosis of PBC, the presence of AMA is one of the diagnostic criteria [208]. Since the antinuclear antibody (ANA) test demonstrates autoantibodies against antigens in the nucleus, cytoplasm, and mitotic apparatus, this test has been recently renamed as indirect immunofluorescence assay on HEp-2 cells (HEp-2 IFA) [11]. The HEp-2 IFA test provides useful elements for the scoring system of AIH and PBC, such as the demonstration of ANA that integrates the scoring system for AIH as well as several nuclear (AC-3, AC-6, AC-11) and cytoplasmic (AC-21) patterns associated with autoantibody systems relevant to the diagnosis of PBC [257]. The presence of a positive HEp-2 IFA test at titer > 1/80 scores three positive points in favor of AIH. It should be noted, though, that the recommended criteria do not specify what pattern in the HEp-2 IFA test is relevant for the diagnosis of AIH. However, each pattern is associated with a specific set of autoantibodies and some IFA patterns may have confounding significance for the diagnosis of autoimmune hepatic diseases. For example, the cytoplasmic reticular-dotted pattern, classified as AC-21 by ICAP [11, 12], is strongly associated with AMA, thus representing a positive point for PBC diagnosis and a negative point for AIH diagnosis. In contrast, the homogeneous (AC-1) and the fine speckled (AC-4) nuclear patterns are regularly found in 50–80% of AIH patients. Moreover, the cytoplasmic fibrillary linear pattern (AC-15) is associated with SMA and anti-F actin antibodies that are relevant for the diagnosis of AIH. Therefore, the diagnostic recommendations for AIH and PBC should detail the pattern in the HEp-2 IFA test, as this would add value to the interpretation of this autoantibody test in the diagnosis and ultimately in the personalized approach to the patients.
Autoimmune Neurologic Diseases
Over the last 15 years, the field of neuroimmunology has experienced a remarkable development, mostly driven by the discovery of several autoantibodies against an array of neuronal surface and intracellular antigens, as well as glial and synaptic antigens. These autoantibodies were shown to be associated with a variety of clinical syndromes involving several regions of the central nervous system [260]. The utilization of tissue-based array (TBA) and cell-based array (CBA) platforms was instrumental to the discovery and now the routine detection of such autoantibodies. Each of the neurologic autoantibodies is associated with a peculiar spectrum of clinical manifestations (Table 12). Accordingly, the detection of neuronal autoantibodies helps in the differential diagnosis of several neurologic syndromes, and establishment of prognosis and therapeutic decisions, thus contributing substantially to the advancement of PM in neurology. Herein, we address the neuromyelitis optica spectrum disorders (NMOSD), the myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD), autoimmune encephalitis (AIE), paraneoplastic encephalitis, and other neurologic conditions specifically associated with some autoantibodies.
NMOSD comprehends a group of demyelinating conditions characterized by episodes of myelitis, optic neuritis, and other neurological manifestations that mimic multiple sclerosis (MS) [261]. Approximately 80% of the NMOSD patients have antibodies against the water channel astrocyte protein aquaporin 4 (AQP4), detected by IFA on aquaporin 4–transfected cells (CBA) and/or IFA on rat cerebellum, contributing substantially to the differentiation of NMOSD from MS [262]. Anti-AQP4 discovery led to the recognition of limited forms of the disease (i.e., recurrent transverse myelitis without optic neuritis) as well as symptoms beyond the spectrum associated with optic nerve and spinal cord involvement, such as the area postrema syndrome characterized by intractable nausea or hiccups [263]. Consequently, anti-AQP4 allowed the expansion of the scope of neuromyelitis optica eventually consolidated under the term NMOSD. Recent studies showed that NMOSD may coexist with other autoimmune conditions such as SLE and pSjS [261, 263]. Anti-AQP4 is best tested in peripheral blood as cerebrospinal fluid (CSF) testing is less sensitive. CBA for anti-AQP4 yields sensitivity of 75 to 80% and specificity greater than 99% for the diagnosis of NMOSD [263]. Anti-AQP4 activates complement and plays a role in promoting the cascade of immune-mediated inflammation. These findings suggest that some AQP4-seronegative patients with clinical and neuroimaging features of NMOSD have a different underlying pathogenesis requiring differentiated therapeutic approach [261]. Identification of anti-AQP4 helps personalizing treatment, as eculizumab, a C5 complement inhibitor, was shown to decrease relapse rates by 94% in seropositive NMOSD patients [264].
Myelin oligodendrocyte glycoprotein (MOG) is important in the myelination of nerves in the central nervous system (CNS). Anti-MOG antibodies have been known for many decades and the initial studies suggested it was a biomarker of MS, but these results were hampered by older-generation immunoassays (ELISA, Western blot) that did not use MOG in its native conformation [265]. With the availability of CBA exposing native MOG at the cell surface, it was demonstrated that anti-MOG is a specific biomarker of a spectrum of CNS inflammatory disorders, often called MOG antibody-associated disease (MOGAD) [261, 266], composed of a constellation of clinical presentations, including myelitis, optic neuritis (often bilateral), NMOSD, acute demyelinating encephalomyelitis (ADEM), and more recently, encephalitis [267, 268]. MOGAD appears to have a particular predilection for children and young adults, but individuals at any age are at risk [269]. The clinical course may be monophasic or relapsing, and higher titers and persistence of anti-MOG over time predict a higher risk of relapse in children and adults [269, 270]. This feature is particularly helpful in the follow-up and personalized therapy of patients.
Glutamic acid decarboxylase (GAD) is the rate-limiting enzyme in the synthesis of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) located in the neuron synaptic cleft [271]; thus, it is considered a synaptic antigen. Neurological syndromes associated to anti-GAD antibodies include the stiff-person syndrome (SPS), epilepsy, limbic encephalitis, downbeat nystagmus, cerebellar ataxia, and progressive encephalomyelitis with rigidity and myoclonus (PERM) [271, 272]. Anti-GAD is considered specific for an autoimmune neurological syndrome only when detected at high titer (more than 500 UI/mL) using ELISA assays, especially in the cerebrospinal fluid (CSF), as low titer anti-GAD is regularly present in the peripheral blood of patients with type 1 diabetes mellitus [272, 273]. Approximately 80% of the patients with GAD-associated neurologic disease have concomitant organ-specific autoimmune disorders, such as type 1 diabetes mellitus, thyroiditis, pernicious anemia, or vitiligo [271]. Paraneoplastic association is very rare, but when a neoplasia is present, there is partial improvement after tumor treatment [271, 273].
AIE constitutes a group of inflammatory brain diseases characterized by prominent neuropsychiatric symptoms associated with autoantibodies against neuronal cell-surface proteins, ion channel molecules, and neurotransmitter receptors [274, 275]. Autoantibodies target molecules of the neuronal cell surface involved mostly in gabaergic and glutamatergic neurotransmission leading to a heterogeneous presentation of neuronal dysfunction. Autoantibodies may have agonistic or antagonistic receptor effects, block ion channel pores, disrupt the interaction with neighboring molecules, alter receptor localization at the membrane, or cause receptor internalization [276]. The epitope specificity of the autoantibodies influences the functional consequences upon the affected cells. Diverse conditions may trigger AIE, including tumors (paraneoplastic) and infections (parainfectious), but many cases are cryptogenic [275, 277,278,279]. AIE is the main consideration in the differential diagnosis of infectious encephalitis and its clinical manifestations include acute and subacute psychosis, various behavior changes, movement disorders, reduced level of consciousness, and seizures [279]. It is estimated that 20% of all encephalitis cases in northern Europe are immune-mediated [280] and 47% of encephalitis in patients under 30 years of age in the California Encephalitis Project were found to have AIE [281]. The estimated AIE annual incidence is 8–13 cases/100,000, occurring in all ages, although some types affect predominantly children and young adults [282, 283].
The most common type of AIE is anti-N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis, characterized by acute/subacute psychosis, seizures, memory and speech impairment, as well as abnormal movements such as orofacial dyskinesias, dystonia, and choreoathetosis. Patients are usually children or young adults and may be severely ill, requiring mechanical ventilation and admission to intensive care unit due to decreased level of consciousness, refractory status epilepticus, autonomic dysfunction, or central hypoventilation [282]. Complementary investigation shows normal brain MRI in half of the patients and EEG findings include seizures or slow waves, although 30% of the cases show a specific pattern known as “extreme delta brush” [284]. Clinical criteria for anti-NMDAR encephalitis have been established and the presence of antibodies to the GluN1 subunit of the NMDA receptor is required for definite diagnosis [275].
Early autoantibody detection is of paramount importance as recent studies showed that the interval between initial symptoms and treatment is associated with prognosis in anti-NMDAR encephalitis [285]. Despite severe symptoms or prolonged coma, 81% of the patients show substantial recovery at 24 months upon early treatment, with an estimated mortality of 7% at 24 months [282]. Patients with AIE are treated with steroids combined with intravenous gamma globulin (IVIG) or plasma exchange. Approximately 50% fail to respond to the first-line therapy, requiring second-line treatment with rituximab and/or cyclophosphamide [275, 279, 282].
Other autoantibodies associated with AIE are anti-leucine-rich glioma-inactivated-1 (LGI1), anti-contactin-associated protein-like 2 (CASPR2), anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR), anti-gamma-aminobutyric acid B receptor (GABA-BR), anti-gamma-aminobutyric acid A receptor (GABA-AR), anti-glycine, anti-dipeptidyl peptidase-like protein 6 (DPPX), anti-IgLON family member 5 (IgLON5), anti-metabotropic glutamate receptor 1 (mGluR1), and anti-neurexin. Certain autoantibodies are associated with specific syndromes recognizable on clinical grounds [274], such as ataxia, hyperexcitability syndrome, Morvan syndrome, brainstem impairment, or fasciobrachial dystonic seizures [269, 286,287,288,289,290,291,292,293,294,295]. Tables 12 and 13 summarize the most common clinical syndromes, phenotypes, and associated autoantibodies in autoimmune neurological syndromes.
Response to immunotherapy, recurrence rates, and frequency of paraneoplastic etiology vary among AIE subtypes [279]. For example, anti-AMPAR encephalitis has a paraneoplastic basis in 64% of the cases, while anit-LGI1 encephalitis is rarely associated with malignancy [289, 295]. Moreover, tumors also vary according to the AIE subtypes. Thus, anti-NMDAR encephalitis frequently associates with ovary teratoma, whereas 40% of anti-CASPR2 encephalitis patients harbor a thymoma [287, 296]. Early testing and identification of onconeurologic autoantibodies can contribute to personalize paraneoplastic screening.
Autoantibodies targeting intraneuronal antigens are classically named onconeuronal antibodies (e.g., Anti-Hu, anti-amphiphysin, anti-Ma) because they are most frequently associated with paraneoplastic neurological syndromes. Paraneoplastic encephalomyelitis involves two or more regions of the nervous system and consequently the neurological involvement may present as different syndromes (Table 14). The identification of onconeural antibodies allows a personalized approach and the possibility of early detection and treatment of an incipient underlying neoplastic disease. In fact, each onconeural autoantibody has particular associations with specific neurologic manifestations and underlying neoplasia (Table 13).
The Manifold Conundrums of Autoantibody Determination
The determination of autoantibodies is not as straightforward as the determination of simple analytes, such as electrolytes and common biochemical analytes (glucose, albumin, creatine phosphokinase, hemoglobin, etc.). A simple analyte is homogeneous in terms of chemical and physical properties, and this allows the development of laboratory assays that will perform equally in samples from any individual. In addition, it is relatively easy to establish reference material for standardization and quality assessment, which contributes to the excellence of laboratory methods for determination of simple analytes. In contrast, autoantibodies represent a polyclonal immune response to a given autoantigen formed by a collection of immunoglobulins highly heterogeneous in terms of serum concentration, isotype, Fc glycosylation, epitope targeting, and avidity. Consequently, the collection of autoantibodies to antigen X in patient A is necessarily distinct from the collection of autoantibodies to antigen X in patient B. On the other hand, the various commercially available immunoassays have peculiarities in terms of the preferentially expressed epitopes, avidity requirement, sensitivity to serum concentration, isotype specificity, etc. As a consequence, the various available immunoassays for anti-X antibody frequently yield different results for the same anti-X-positive sample [92, 297,298,299]. This heterogeneity poses an overwhelming challenge in the establishment of reference materials for standardization and quality assessment, as any chosen reference material tends not to be representative to all individuals to be assayed.
One other perplexing aspect of autoantibody testing is the possibility of interference of natural autoantibodies, which occur frequently in the normal population and belong to the pool of natural antibodies. These are immunoglobulins produced by B1 lymphocytes with no previous immunization and being derived from germ-line genes not modified by mutations induced by antigenic stimulation [300, 301]. Isoagglutinins that react with blood group proteins A and B represent a prototype natural antibody. In general, natural autoantibodies occur at low titer and present low avidity and broad cross-reactivity. Natural autoantibodies can cause positive reactivity in very sensitive immunoassays, yielding clinically unexpected results. In particular, solid phase immunoassays (ELISA, western blot, other solid phase immunoassays) are particularly prone to detect antibodies with low concentration and low avidity that frequently can cause reactivity at the low positive range [302]. Therefore, the interpretation of results from these sensitive immunoassays should take into consideration the intensity of reactivity of the sample of interest with respect to the cut-off value for that assay.
These limitations imply that a positive result from an autoantibody immunoassay should be strictly interpreted taking into consideration the clinical context. A request for autoantibody immunoassays in a low pre-test probability context frequently generates unexpected positive results that may ensue misdiagnosis, inappropriate treatment, and increase in health costs. On the other hand, the detection of a specific autoantibody in individuals with ill-defined clinical disease may contribute to early diagnosis and treatment, promoting optimal outcomes for the patient as well as savings in health costs [303]. The thin line separating the above scenarios requires clinical expertise, optimal laboratory practice, and communication between the clinician and the laboratory clinical pathologist.
Fine-Tuning the Results of Autoantibody Assays Ahead of the “Positive/Negative Paradigm” as a Step Forward to PM
Possibly because of early methodological approaches (e.g., gel immunodiffusion/immunoprecipitation), the “qualitative paradigm” is prevalent in the interpretation and reporting of autoantibodies. Usually, a patient is frequently referred to as being “positive” or “negative” for a given autoantibody. However, current immunoassays provide semi-quantitative results that allow exploring the quantitative dimension of the humoral autoimmune response. In fact, various autoantibodies have specific clinical relevance at higher autoantibody serum concentrations. For example, anti-cardiolipin antibodies are considered a criterion for the classification of anti-phospholipid syndrome only at titer equal to or greater than 40GPL or 40MPL [53] and increasing titers of anti-dsDNA antibodies are frequently associated with active lupus nephritis [27]. The “semi quantitative paradigm” is also relevant to the HEp-2 IFA, as the titer plays an important role in the clinical relevance of a positive HEp-2 IFA test in a given individual. By using receiver-operator characteristic (ROC) curve analysis, it has been shown that the performance of the HEp-2 IFA test for the diagnosis of systemic autoimmune diseases is significantly higher at titer equal to or greater that 1/1280 and that low titers are frequently observed in healthy individuals and patients with non-autoimmune diseases [8, 15, 233]. The result-specific likelihood ratio has been shown to increase with increasing HEp-2 IFA titer [304]. Therefore, aiming at the advancement of PM, the mindset of clinicians and clinical pathologists regarding autoantibody test results should be changed toward the “semi quantitative paradigm.”
Another opportunity for fine-tuning the interpretation of autoantibody tests is the recognition of specific patterns. The HEp-2 IFA test is widely used for detection of autoantibodies to a vast array of autoantigens in several systemic autoimmune diseases [11, 12]. However, this test has low specificity, as a positive result is observed also in healthy individuals [7, 8, 133, 232, 305] and in patients with non-autoimmune diseases [15, 233]. Nonetheless, there is opportunity for increasing the specificity of HEp-2 IFA results by the refined definition of the HEp-2 IFA pattern. In analogy to the importance of pattern definition in chest and brain MRI, the definition of the HEP-2 IFA pattern can discriminate various specificities of a positive HEp-2 IFA test, indicating the most probable involved autoantibody specificities and the possible clinical relevance. Thus, the homogeneous nuclear pattern (AC-1) is frequently associated with antibodies to dsDNA, nucleosome, and histones, and is frequently found in patients with SLE, juvenile rheumatoid arthritis, and autoimmune hepatitis [11]. In contrast, the dense fine speckled nuclear pattern (AC-2) is strongly associated with antibodies to DFS70 and rarely occurs in systemic autoimmune diseases, but is frequently observed in healthy individuals [8, 306] and patients with non-autoimmune diseases [233, 307,308,309]. Recognizing the importance of HEp-2 IFA pattern in the interpretation of the test, an international group of specialists launched the ICAP, an initiative committed to define and harmonize the nomenclature of HEp-2 IFA patterns [12]. The most relevant and frequent patterns have been consented and organized into a classification algorithm and each HEp-2 IFA pattern was assigned an alpha-numeric code (AC-#, for Anti-Cell). The ICAP website www.anapattern.org displays an interactive content including the HEp-2 IFA classification tree with representative images from each pattern, recommended nomenclature, immunologic associations, clinical relevance, pertinent bibliography, and frequently asked questions.
Concluding Remarks
Precision Medicine has been pursued along the history of medicine and in retrospect it is clear that a tremendous progress has been made, as nosology groups and subgroups have been defined progressively allowing continuous optimization of therapeutic strategies for each of these subgroups. However, it is also clear that much progress is needed to achieve the ultimate fulfillment of the conception of precision medicine. The path for such progress has been increasingly accelerated in the last decades with the steady incremental discovery of various biomarkers, progressive understanding of the phenotypic relevance of thousands of polymorphic genes, determination of the microbiome associated with physiological and pathological scenarios, determination of the epigenetic modifications in various biologic states, availability of multiplex assays, and use of artificial intelligence and machine learning required to meaningfully extract trends, conjunctions, and focal points in very large datasets. Autoantibodies and other immunological parameters constitute important elements in the complex network being integrated for the establishment of a more advanced degree of medicine personalization in the near future.
References
Auffray C, Charron D, Hood L (2010) Predictive, preventive, personalized and participatory medicine: Back to the future. Genome Med 2:57
Yaniv G, Twig G, Shor DB, Furer A, Sherer Y, Mozes O et al (2015) A volcanic explosion of autoantibodies in systemic lupus erythematosus: a diversity of 180 different antibodies found in SLE patients. Autoimmun Rev 14:75–79
Fava A, Petri M (2019) Systemic lupus erythematosus: Diagnosis and clinical management. J Autoimmun 96:1–13
Pons-Estel GJ, Alarcon GS, Scofield L, Reinlib L, Cooper GS (2010) Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum 39:257–268
Vilar MJ, Sato EI (2002) Estimating the incidence of systemic lupus erythematosus in a tropical region (Natal, Brazil). Lupus 11:528–532
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R et al (2019) 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann Rheum Dis 78:1151–1159
Fernandez SA, Lobo AZ, Oliveira ZN, Fukumori LM, Périgo AM, Rivitti EA (2003) Prevalence of antinuclear autoantibodies in the serum of normal blood donors. Rev Hosp Clin Fac Med Sao Paulo. 58:315–319
Mariz HA, Sato EI, Barbosa SH, Rodrigues SH, Dellavance A, Andrade LE (2011) Pattern on the antinuclear antibody-HEp-2 test is a critical parameter for discriminating antinuclear antibody-positive healthy individuals and patients with autoimmune rheumatic diseases. Arthritis Rheum 63:191–200
Dinse GE, Parks CG, Weinberg CR, Co CA, Wilkerson J, Zeldin DC et al (2020) Increasing prevalence of antinuclear antibodies in the United States. Arthritis Rheumatol 72:1026–1035
Dellavance A, Gabriel AJ, Nuccitelli B, Taliberti T, von Mühlen C, Bichara CDA et al (2009) Third Brazilian consensus for autoantibody research in HEp-2 cells (FAN). Recommendations for standardization of the autoantibody screening assay in HEp-2 cells, quality control and clinical associations. Rev Bras Rheumatol 49:89–109
Damoiseaux J, Andrade LEC, Carballo OG, Conrad K, Francescantonio PLC, Fritzler MJ et al (2019) Clinical relevance of HEp-2 indirect immunofluorescent patterns: the International Consensus on ANA patterns (ICAP) perspective. Ann Rheum Dis 78:879–889
Chan EKL, Damoiseaux J, Carballo OG, Conrad K, Cruvinel WM, Francescantonio PLC et al (2015) Report of the first international consensus on standardized nomenclature of antinuclear antibody HEp-2 cell patterns 2014–2015. Front Immunol 6:412
Wallace DJ, Stohl W, Furie RA, Lisse JR, McKay JD, Merrill JT et al (2009) A phase II, randomized, double-blind, placebo-controlled, dose-ranging study of belimumab in patients with active systemic lupus erythematosus. Arthritis Rheum 61:1168–1178
Furie R, Petri M, Zamani O, Cervera R, Wallace DJ, Tegzová D et al (2011) A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus. Arthritis Rheum 63:3918–3930
Prado MS, Dellavance A, Rodrigues SH, Marvulle V, Andrade LEC (2020) Changes in the result of antinuclear antibody immunofluorescence assay on HEp-2 cells reflect disease activity status in systemic lupus erythematosus. Clin Chem Lab Med 58:1271–1281
Choi MY, Clarke AE, St Pierre Y, Hanly JG, Urowitz MB, Romero-Diaz J et al (2018) Antinuclear antibody-negative systemic lupus erythematosus in an international inception cohort. Arthritis Care Res (Hoboken) 71:893–902
Quismorio F, Torralba K (2013) Clinical application of serologic tests, serum protein abnormalities, and other clinical laboratory test in SLE. In: Wallace D, Hahn B (eds) Dubois’ lupus erythematosus and related syndromes, 8th edn. Elsevier Saunders, Philadelphia, PA, pp 526–540
Brito-Zerón P, Izmirly P, Ramos-Casals M, Buyon J, Khamashta M (2015) The clinical spectrum of autoimmune congenital heart block. Nat Rev Rheumatol 11:301–312
Wahren-Herlenius M, Sonesson SE, Clowse ME (2012) Neonatal lupus erythematosus. In: Wallace D, Hahn B (eds) Dubois’ lupus erythematosus and related syndromes, 8th edn. Saunders, Philadelphia, pp 464–472
Sammaritano L, Bermas B, Chakravarty E, Chambers C, Clowse M, Lockshin M et al (2020) 2020 American college of rheumatology guideline for the management of reproductive health in rheumatic and musculoskeletal diseases. Arthritis Rheumatol 72:529–556
Lazzerini PE, Acampa M, Guideri F, Capecchi PL, Campanella V, Morozzi G et al (2004) Prolongation of the corrected QT interval in adult patients with anti-Ro/SSA-positive connective tissue diseases. Arthritis Rheum 50:1248–1252
Lazzerini PE, Capecchi PL, Guideri F, Bellisai F, Selvi E, Acampa M et al (2007) Comparison of frequency of complex ventricular arrhythmias in patients with positive versus negative anti-Ro/SSA and connective tissue disease. Am J Cardiol 100:1029–1034
Satoh M, Fritzler MF, Chan EKL (2020) Antihistone and antispliceosome antibodies. In: Tsokos GC (ed) Lupus erythematosus: basic, applied and clinical aspects, 1st edn. Academic Press, New York, pp 237–247
Furtado R, Pucinelli M, Cristo V, Andrade L, Sato E (2002) Scleroderma-like nailfold capillaroscopic abnormalities are associated with anti-U1-RNP antibodies and Raynaud’s phenomenon in SLE patients. Lupus 11:35–41
Migliorini P, Baldini C, Rocchi V, Bombardieri S (2005) Anti-Sm and anti-RNP antibodies. Autoimmunity 38:47–54
Alba P, Bento L, Cuadrado MJ, Karim Y, Tungekar MF, Abbs I et al (2003) Anti-dsDNA, anti-Sm antibodies, and the lupus anticoagulant: Significant factors associated with lupus nephritis. Ann Rheum Dis 62:556–560
van Vollenhoven RF, Fly M, Bertsias G, Isenberg D, Kuhn A, Lerstrom K et al (2014) Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis 73:958–967
Tseng C, Buyon J, Kim M, Belmont H, Mackay M, Diamond B et al (2006) The effect of moderate-dose corticosteroids in preventing severe flares in patients with serologically active, but clinically stable, systemic lupus erythematosus: Findings of a prospective, randomized, double-blind, placebo-controlled trial. Arthritis Rheum 54:3623–3632
Hung W, Chen Y, Lan J, Chen H, Chen Y, Chen D et al (2011) Antinucleosome antibodies as a potential biomarker for the evaluation of renal pathological activity in patients with proliferative lupus nephritis. Lupus 20:1404–1410
Ng K, Manson J, Rahman A, Isenberg D (2006) Association of antinucleosome antibodies with disease flare in serologically active clinically quiescent patients with systemic lupus erythematosus. Arthritis Rheum 55:900–904
Sui M, Sui M, Lin Q, Xu Z, Han X, Xie R et al (2013) Simultaneous positivity for anti-DNA, anti-nucleosome and anti-histone antibodies is a marker for more severe lupus nephritis. J Clin Immunol 33:378–387
Stinton LM, Barr SG, Tibbles LA, Yilmaz S, Sar A, Benedikttson H et al (2007) Autoantibodies in lupus nephritis patients requiring renal transplantation. Lupus 16:394–400
Sinico R, Radice A, Ikehata M, Giammarresi G, Corace C, Arrigo G et al (2005) Anti-C1q autoantibodies in lupus nephritis: Prevalence and clinical significance. Ann New York Acad of Sci 1050:193–200
Siegert C, Daha M, Westedt ML, van der Voort E, Breedveld F (1991) IgG autoantibodies against C1q are correlated with nephritis, hypocomplementemia, and dsDNA antibodies in systemic lupus erythematosus. J Rheumatol 18:230–234
Orbai A-M, Truedsson L, Sturfelt G, Nived O, Fang H, Alarcón GS et al (2015) Anti- C1q antibodies in systemic lupus erythematosus. Lupus 24:42–49
Matrat A, Veysseyre-Balter C, Trolliet P, Villar E, Dijoud F, Bienvenu J et al (2011) Simultaneous detection of anti-C1q and anti-double stranded DNA autoantibodies in lupus nephritis: Predictive value for renal flares. Lupus 20:28–34
Moroni G, Radice A, Giammarresi G, Quaglini S, Gallelli B, Leoni A et al (2009) Are laboratory tests useful for monitoring the activity of lupus nephritis? A 6-year prospective study in a cohort of 228 patients with lupus nephritis. Ann Rheum Dis 68:234–237
Choi M, FitzPatrick R, Buhler K, Mahler M, Fritzler M (2020) A review and meta-analysis of anti-ribosomal P autoantibodies in systemic lupus erythematosus. Autoimmun Rev 19:102463
Haddouk S, Marzouk S, Jallouli M, Fourati H, Frigui M, Hmida Y et al (2009) Clinical and diagnostic value of ribosomal P autoantibodies in systemic lupus erythematosus. Rheumatology (Oxford) 48:953–957
Bonfa E, Golombek S, Kaufman L, Skelly S, Weissbach H, Brot N et al (1987) Association between lupus psychosis and anti-ribosomal P protein antibodies. New Eng J Med 317:265–271
do Nascimento A, Viana VDS, Testagossa LDA, Leon E, Borba E, Barros R et al (2006) Antibodies to ribosomal P proteins: a potential serologic marker for lupus membranous glomerulonephritis. Arthritis Rheum 54:1568–1572
Macedo P, Borba E, Viana VDS, Leon E, Testagossa L, Barros R et al (2011) Antibodies to ribosomal P proteins in lupus nephritis: is a surrogate marker for a better renal survival? Autoimmun Rev 10:126–130
Calich A, Viana V, Cancado E, Tustumi F, Terrabuio D, Leon E et al (2013) Anti-ribosomal P protein: a novel antibody in autoimmune hepatitis. Liver Int 336:909–913
Tektonidou M, Sotsiou F, Nakopoulou L, Vlachoyiannopoulos P, Moutsopoulos H (2004) Antiphospholipid syndrome nephropathy in patients with systemic lupus erythematosus and antiphospholipid antibodies:Pprevalence, clinical associations, and long-term outcome. Arthritis Rheum 50:2569–2579
Fayyaz A, Igoe A, Kurien BT, Danda D, James JA, Stafford HA et al (2015) Haematological manifestations of lupus. Lupus Sci Med 2:e000078
Stegert M, Bock M, Trendelenburg M (2015) Clinical presentation of human C1q deficiency: How much of a lupus? Mol Immunol 67:3–11
Araujo MNT, Silva NP, Andrade LEC, Sato EI, Gerbase-DeLima M, Leser PG (1997) C2 deficiency in blood donors and lupus patients: prevalence, clinical characteristics and HLA-associations in the Brazilian population. Lupus 6:462–466
Yang Y, Chung EK, Wu YL, Savelli SL, Nagaraja HN, Zhou B et al (2007) Gene copy-number variation and associated polymorphisms of complement component C4 in human systemic lupus erythematosus (SLE): Low copy number is a risk factor for and high copy number is a protective factor against SLE susceptibility in European Americans. Am J Hum Genet 80:1037–1054
Pereira KMC, Perazzio S, Faria AGA, Moreira ES, Santos VC, Grecco M et al (2019) Impact of C4, C4A and C4B gene copy number variation in the susceptibility, phenotype and progression of systemic lupus erythematosus. Adv Rheumatol 59:36–42
Hughes G (1983) Thrombosis, abortion, cerebral disease, and the lupus anticoagulant. Br Med J (Clin Res Ed) 287:1088–1089
McNeil H, Simpson R, Chesterman C, Krilis S (1990) Anti-phospholipid antibodies are directed against a complex antigen that includes a lipid-binding inhibitor of coagulation: Beta 2-glycoprotein I (apolipoprotein H). Proc Nati Acad Sci U S A 87:4120–4124
Groot P, Urbanus R (2012) The significance of autoantibodies against β2-glycoprotein I. Blood 120:266–274
Miyakis S, Lockshin M, Atsumi T, Branch D, Brey R, Cervera R et al (2006) International consensus statement on an update of the classification criteria for a definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
Barbhaiya M, Zuily S, Ahmadzadeh Y, Amigo MC, Avcin T, Bertolaccini ML et al (2020) Development of new international antiphospholipid syndrome classification criteria phase I/II Report: Generation and reduction of candidate criteria. Arthritis Care Res (Hoboken). Online ahead of print: https://doi.org/10.1002/acr.24520
Urbanus R, Siegerink B, Roest M, Rosendaal F, de Groot P, Algra A (2009) Antiphospholipid antibodies and risk of myocardial infarction and ischaemic stroke in young women in the RATIO study: a case-control study. Lancet Neurol 8:998–1005
Devreese KMJ (2020) Testing for antiphospholipid antibodies: advances and best practices. Int J Lab Hematol 42(Suppl 1):49–58
Jayakody Arachchillage D, Greaves M (2014) The checked history of the antiphospholipid syndrome. British J Haematol 165:609–617
Reynaud Q, Lega J, Mismetti P, Chapelle C, Wahl D, Cathébras P et al (2014) Risk of venous and arterial thrombosis according to type of antiphospholipid antibodies in adults without systemic lupus erythematosus: a systematic review and meta-analysis. Autoimmun Rev 13:595–608
Schouwers SM, Delanghe JR, Devreese KM (2010) Lupus anticoagulant (LAC) testing in patients with inflammatory status: Does C-reactive protein interfere with LAC test results? Thromb Res 125:102–104
Nayfe R, Uthman I, Aoun J, Saad Aldin E, Merashli M, Khamashta M (2013) Seronegative antiphospholipid syndrome. Rheumatology (Oxford) 52:1358–1367
Murthy V, Willis R, Romay-Penabad Z, Ruiz-Limón P, Martínez-Martínez L, Jatwani S et al (2013) Value of isolated IgA anti-β2 -glycoprotein I positivity in the diagnosis of the antiphospholipid syndrome. Arthritis Rheum 65:3186–3193
Morales J, Martinez-Flores J, Serrano M, Castro M, Alfaro F, García F et al (2015) Association of early kidney allograft failure with preformed IgA antibodies to β2-glycoprotein I. J Am Soc Nephrol (JASN) 26:735–745
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta M, Bertolaccini M (2014) Anti-prothrombin (aPT) and anti-phosphatidylserine/prothrombin (aPS/PT) antibodies and the risk of thrombosis in the antiphospholipid syndrome. A systematic review. Thromb Haemost 111:354–364
Litvinova E, Darnige L, Kirilovsky A, Burnel Y, Luna G, Dragon-Durey M (2018) Prevalence and significance of non-conventional antiphospholipid antibodies in patients with clinical APS criteria. Front Immunol 9:2971
Otomo K, Atsumi T, Amengual O, Fujieda Y, Kato M, Oku K et al (2012) Efficacy of the antiphospholipid score for the diagnosis of antiphospholipid syndrome and its predictive value for thrombotic events. Arthritis Rheum 64:504–512
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta M, Bertolaccini M (2013) GAPSS: The global anti-phospholipid syndrome score. Rheumatology (Oxford) 52:1397–1403
Radin M, Cecchi I, Roccatello D, Meroni P, Sciascia S (2018) Prevalence and thrombotic risk assessment of anti-β2 Glycoprotein I domain I antibodies: a systematic review. Semin Thromb Hemost 44:466–474
Pengo V, Ruffatti A, Tonello M, Cuffaro S, Banzato A, Bison E et al (2015) Antiphospholipid syndrome: Antibodies to Domain 1 of β2-glycoprotein 1 correctly classify patients at risk. J Thromb Haemost 13:782–787
Nakamura H, Oku K, Amengual O, Ohmura K, Fujieda Y, Kato M et al (2018) First-line, non-criterial antiphospholipid antibody testing for the diagnosis of antiphospholipid syndrome in clinical practice: The combination of anti-β 2-glycoprotein I domain I and anti-phosphatidylserine/prothrombin complex antibodies tests. Arthritis Care Res (Hoboken) 70:627–634
Pengo V, Biasiolo A, Pegoraro C, Cucchini U, Ninety F, Iliceto S (2005) Antibody profiles for the diagnosis of antiphospholipid syndrome. Thromb Haemost 93:1147–1152
Ruffatti A, Calligaro A, Hoxha A, Trevisanuto D, Ruffatti A, Gervasi M et al (2010) Laboratory and clinical features of pregnant women with antiphospholipid syndrome and neonatal outcome. Arthritis Care Res (Hoboken) 62:302–307
Radin M, Sciascia S, Erkan D, Pengo V, Tektonidou M, Ugarte A et al (2019) The adjusted global antiphospholipid syndrome score (aGAPSS) and the risk of recurrent thrombosis: Results from the APS ACTION cohort. Semin Arthritis Rheum 49:464–468
Burgos-Vargas R, Catoggio LJ, Galarza-Maldonado C, Ostojich K, Cardiel MH (2013) Current therapies in rheumatoid arthritis: a Latin American perspective. Reumatol Clin 9:106–112
Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS et al (2018) Rheumatoid arthritis. Nat Rev Dis Primers 4:18001
Greenblatt HK, Kim HA, Bettner LF, Deane KD (2020) Preclinical rheumatoid arthritis and rheumatoid arthritis prevention. Curr Opin Rheumatol 32:289–296
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A et al (2020) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 79:685–699
Wu CY, Yang HY, Luo SF, Lai JH (2021) From rheumatoid factor to anti-citrullinated protein antibodies and anti-carbamylated protein antibodies for diagnosis and prognosis prediction in patients with rheumatoid arthritis. Int J Mol Sci 22:686
Aletaha D (2020) Precision medicine and management of rheumatoid arthritis. J Autoimmun 110:102405
Tarn JR, Lendrem DW, Isaacs JD (2020) In search of pathobiological endotypes: a systems approach to early rheumatoid arthritis. Expert Rev Clin Immunol 16:621–630
Bettner LF, Peterson RA, Bergstedt DT, Kelmenson LB, Demoruelle MK, Mikuls TR et al (2021) Combinations of anticyclic citrullinated protein antibody, rheumatoid factor, and serum calprotectin positivity are associated with the diagnosis of rheumatoid arthritis within 3 years. ACR Open Rheumatol 20. https://doi.org/10.1002/acr2.11309
Deane KD, Holers VM (2021) Rheumatoid arthritis pathogenesis, prediction, and prevention: an emerging paradigm shift. Arthritis Rheumatol 73:181–193
Masi AT (1983) Articular patterns in the early course of rheumatoid arthritis. Am J Med 75:16–26
Firestein GS (2003) Evolving concepts of rheumatoid arthritis. Nature 423:356–361
Trouw LA, Huizinga TW, Toes RE (2013) Autoimmunity in rheumatoid arthritis: Different antigens—common principles. Ann Rheum Dis 72(Suppl 2):ii132–ii136
Carubbi F, Alunno A, Gerli R, Giacomelli R (2019) Post-translational modifications of proteins: Novel insights in the autoimmune response in rheumatoid arthritis. Cells 8(7):657
Grönwall C, Amara K, Hardt U, Krishnamurthy A, Steen J, Engstrom M et al (2017) Autoreactivity to malondialdehyde-modifications in rheumatoid arthritis is linked to disease activity and synovial pathogenesis. J Autoimmun 84:29–45
Juarez M, Bang H, Hammar F, Reimer U, Dyke B, Sahbudin I et al (2016) Identification of novel antiacetylated vimentin antibodies in patients with early inflammatory arthritis. Ann Rheum Dis 75:1099–1107
Shi J, Knevel R, Suwannalai P, van der Linden MP, Janssen GM, van Veelen PA et al (2011) Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci USA 108:17372–17377
de Brito RS, Baldo DC, Andrade LEC (2019) Clinical and pathophysiologic relevance of autoantibodies in rheumatoid arthritis. Adv Rheumatol 59:2
Grönwall C, Liljefors L, Bang H, Hensvold AH, Hansson M, Mathsson-Alm L et al (2021) A comprehensive evaluation of the relationship between different IgG and IgA anti-modified protein autoantibodies in rheumatoid arthritis. Front Immunol 12:627986
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO et al (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581
Van Hoovels L, Jacobs J, Vander Cruyssen B, Van den Bremt S, Verschueren P, Bossuyt X (2018) Performance characteristics of rheumatoid factor and anti-cyclic citrullinated peptide antibody assays may impact ACR/EULAR classification of rheumatoid arthritis. Ann Rheum Dis 77:667–677
Nishimura K, Sugiyama D, Kogata Y, Tsuji G, Nakazawa T, Kawano S et al (2007) Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med 146:797–808
Schellekens GA, de Jong BA, van den Hoogen FH, van de Putte LB, van Venrooij WJ (1998) Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest 101:273–281
Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC et al (2000) The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum 43:155–163
van der Helm-van Mil AH, Verpoort KN, Breedveld FC, Toes RE, Huizinga TW (2005) Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res Ther 7:R949–R958
Derksen VF, Ajeganova S, Trouw LA, van der Helm-van Mil AH, Hafström I, Huizinga TW et al (2017) Rheumatoid arthritis phenotype at presentation differs depending on the number of autoantibodies present. Ann Rheum Dis 76:716–720
Juarez M, Bang H, Hammar F, Reimer U, Dyke B, Sahbudin I et al (2016) Identification of novel anti-acetylated vimentin antibodies in patients with early inflammatory arthritis. Ann Rheum Dis 75:1099–1107
Combe B, Dougados M, Goupille P, Cantagrel A, Eliaou JF, Sibilia J et al (2001) Prognostic factors for radiographic damage in early rheumatoid arthritis: a multi parameter prospective study. Arthritis Rheum 44:1736–1743
Bukhari M, Thomson W, Naseem H, Bunn D, Silman A, Symmons D et al (2007) The performance of anti-cyclic citrullinated peptide antibodies in predicting the severity of radiologic damage in inflammatory polyarthritis: Results from the Norfolk Arthritis Register. Arthritis Rheum 56:2929–2935
Visser K, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Ronday HK, Seys PE, Kerstens PJ et al (2010) A matrix risk model for the prediction of rapid radiographic progression in patients with rheumatoid arthritis receiving different dynamic treatment strategies: Post hoc analyses from the BeSt study. Ann Rheum Dis 69:1333–1337
Jilani AA, Mackworth-Young CG (2015) The role of citrullinated protein antibodies in predicting erosive disease in rheumatoid arthritis: a systematic literature review and meta-analysis. Int J Rheumatol 2015:728610. https://doi.org/10.1155/2015/728610
Klareskog L, Catrina AI, Paget S (2009) Rheumatoid arthritis. Lancet 373:659–672
Jawaheer D, Thomson W, MacGregor AJ, Carthy D, Davidson J, Dyer PA et al (1994) Homozygosity for the HLA-DR shared epitope contributes the highest risk for rheumatoid arthritis concordance in identical twins. Arthritis Rheum 37:681–686
Alarcon RT, Fernandes AR, Laurindo IM, Bértolo MB, Pinheiro GC, Andrade LE (2015) Characterization of cumulative joint damage patterns in patients with rheumatoid arthritis: a clinical, serological, and gene polymorphism perspective. J Rheumatol 42:405–412
Viatte S, Lee JC, Fu B, Espéli M, Lunt M, De Wolf JN et al (2016) Association between genetic variation in FOXO3 and reductions in inflammation and disease activity in inflammatory polyarthritis. Arthritis Rheumatol 68:2629–2636
Krabben A, Huizinga TW, Mil AH (2015) Biomarkers for radiographic progression in rheumatoid arthritis. Curr Pharm Des 21:147–169
Lee JC, Espéli M, Anderson CA, Linterman MA, Pocock JM, Williams NJ et al (2013) Human SNP links differential outcomes in inflammatory and infectious disease to a FOXO3-regulated pathway. Cell 155:57–69
van Nies JA, Tsonaka R, Gaujoux-Viala C, Fautrel B, van der Helm-van Mil AH (2015) Evaluating relationships between symptom duration and persistence of rheumatoid arthritis: Does a window of opportunity exist? Results on the Leiden early arthritis clinic and ESPOIR cohorts. Ann Rheum Dis 74:806–812
Aho K, Palosuo T, Raunio V, Puska P, Aromaa A, Salonen JT (1985) When does rheumatoid disease start? Arthritis Rheum 28:485–489
Rantapää-Dahlqvist S, de Jong BA, Berglin E, Hallmans G, Wadell G, Stenlund H et al (2003) Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum 48:2741–2749
Nielen MM, van Schaardenburg D, Reesink HW, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH et al (2004) Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum 50:380–386
Rakieh C, Nam JL, Hunt L, Hensor EM, Das S, Bissell LA et al (2015) Predicting the development of clinical arthritis in anti-CCP positive individuals with non-specific musculoskeletal symptoms: a prospective observational cohort study. Ann Rheum Dis 74:1659–1666
Bos WH, Wolbink GJ, Boers M, Tijhuis GJ, de Vries N, van der Horst-Bruinsma IE et al (2010) Arthritis development in patients with arthralgia is strongly associated with anti-citrullinated protein antibody status: a prospective cohort study. Ann Rheum Dis 69:490–494
Verheul MK, Böhringer S, van Delft MAM, Jones JD, Rigby WFC, Gan RW et al (2018) Triple positivity for anti-citrullinated protein autoantibodies, rheumatoid factor, and anti-carbamylated protein antibodies conferring high specificity for rheumatoid arthritis: Implications for very early identification of at-risk individuals. Arthritis Rheumatol 70:1721–1731
Viatte S, Plant D, Bowes J, Lunt M, Eyre S, Barton A et al (2012) Genetic markers of rheumatoid arthritis susceptibility in anti-citrullinated peptide antibody negative patients. Ann Rheum Dis 71:1984–1990
Viatte S, Massey J, Bowes J, Duffus K, arcOGEN Consortium, Eyre S et al (2016) Replication of associations of genetic loci outside the HLA region with susceptibility to anti-cyclic citrullinated peptide-negative rheumatoid arthritis. Arthritis Rheumatol 68:1603–1613
Källberg H, Ding B, Padyukov L, Bengtsson C, Rönnelid J, Klareskog L et al (2011) Smoking is a major preventable risk factor for rheumatoid arthritis: Estimations of risks after various exposures to cigarette smoke. Ann Rheum Dis 70:508–511
Bettner LF, Peterson RA, Bergstedt DT, Kelmenson LB, Demoruelle MK, Mikuls TR et al (2021) Combinations of anti-cyclic citrullinated protein antibody, rheumatoid factor, and serum calprotectin positivity are associated with the diagnosis of rheumatoid arthritis within 3 years. ACR Open Rheumatol. https://doi.org/10.1002/acr2.11309
Jarlborg M, Courvoisier DS, Lamacchia C, Martinez-Prat L, Mahler M, Bentow C et al (2020) Serum calprotectin: a promising biomarker in rheumatoid arthritis and axial spondyloarthritis. Arthritis Res Ther 22:105
de Moel EC, Rech J, Mahler M, Roth J, Vogl T, Schouffoer A et al (2019) Circulating calprotectin (S100A8/A9) is higher in rheumatoid arthritis patients that relapse within 12 months of tapering anti-rheumatic drugs. Arthritis Res Ther 21:268
Courvoisier DS, Chatzidionysiou K, Mongin D, Lauper K, Mariette X, Morel J et al (2021) The impact of seropositivity on the effectiveness of biologic anti-rheumatic agents: Results from a collaboration of 16 registries. Rheumatology (Oxford) 60:820–828
Bird P, Hall S, Nash P, Connell CA, Kwok K, Witcombe D et al (2019) Treatment outcomes in patients with seropositive versus seronegative rheumatoid arthritis in phase III randomised clinical trials of tofacitinib. RMD Open 5:e000742
Schlager L, Loiskandl M, Aletaha D, Radner H (2020) Predictors of successful discontinuation of biologic and targeted synthetic DMARDs in patients with rheumatoid arthritis in remission or low disease activity: a systematic literature review. Rheumatology (Oxford) 59:324–334
Fox RI (2005) Sjögren’s syndrome. Lancet 366:321–331
Qin B, Wang J, Yang Z, Yang M, Ma N, Huang F et al (2015) Epidemiology of primary Sjögren’s syndrome: a systematic review and meta-analysis. Ann Rheum Dis 74:1983–1989
Voulgarelis M, Dafni UG, Isenberg DA, Moutsopoulos HM (1999) Malignant lymphoma in primary Sjögren’s syndrome: a multicenter, retrospective, clinical study by the European Concerted Action on Sjögren’s Syndrome. Arthritis Rheum 42:1765–1772
Kroese FG, Abdulahad WH, Haacke E, Bos NA, Vissink A, Bootsma H (2014) B-cell hyperactivity in primary Sjögren’s syndrome. Expert Rev Clin Immunol 10:483–499
Ramos-Casals M, Tzioufas AG, Font J (2005) Primary Sjögren’s syndrome: New clinical and therapeutic concepts. Ann Rheum Dis 64:347–354
Brito-Zerón P, Acar-Denizli N, Ng WF, Zeher M, Rasmussen A, Mandl T et al (2018) How immunological profile drives clinical phenotype of primary Sjögren’s syndrome at diagnosis: Analysis of 10,500 patients (Sjögren Big Data Project). Clin Exp Rheumatol 36(Suppl 112(3)):102–112
Goules AV, Exarchos TP, Pezoulas VC, Kourou KD, Venetsanopoulou AI, De Vita S et al (2019) Sjögren’s syndrome towards precision medicine: the challenge of harmonisation and integration of cohorts. Clin Exp Rheumatol 37(Suppl 118):175–184
Theander E, Jonsson R, Sjöström B, Brokstad K, Olsson P, Henriksson G (2015) Prediction of Sjögren’s syndrome years before diagnosis and identification of patients with early onset and severe disease course by autoantibody profiling. Arthritis Rheumatol 67:2427–2436
Andrade LE, Chan EK, Peebles CL, Tan EM (1996) Two major autoantigen-antibody systems of the mitotic spindle apparatus. Arthritis Rheum 39:1643–1653
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM et al (2017) 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis 76:9–16
Alspaugh MA, Talal N, Tan EM (1976) Differentiation and characterization of autoantibodies and their antigens in Sjögren’s syndrome. Arthritis Rheum 19:216–222
Wolin SL, Reinisch KM (2006) The Ro 60 kDa autoantigen comes into focus: Interpreting epitope mapping experiments on the basis of structure. Autoimmun Rev 5:367–372
Oke V, Wahren-Herlenius M (2012) The immunobiology of Ro52 (TRIM21) in autoimmunity: a critical review. J Autoimmun 39:77–82
Mekinian A, Nicaise-Roland P, Chollet-Martin S, Fain O, Crestani B (2013) Anti-SSA Ro52/Ro60 antibody testing by immunodot could help the diagnosis of Sjogren’s syndrome in the absence of anti-SSA/SSB antibodies by ELISA. Rheumatology (Oxford) 52:2223–2228
Robbins A, Hentzien M, Toquet S, Didier K, Servettaz A, Pham BN et al (2019) Diagnostic utility of separate anti-Ro60 and anti-Ro52/TRIM21 antibody detection in autoimmune diseases. Front Immunol 10:444. https://doi.org/10.3389/fimmu.2019.00444
Ghillani P, André C, Toly C, Rouquette AM, Bengoufa D, Nicaise P et al (2011) Clinical significance of anti-Ro52 (TRIM21) antibodies non-associated with anti-SSA 60kDa antibodies: Results of a multicentric study. Autoimmun Rev 10:509–513
Retamozo S, Akasbi M, Brito-Zerón P, Bosch X, Bove A, Perez-de-Lis M et al (2012) Anti-Ro52 antibody testing influences the classification and clinical characterisation of primary Sjögren’s syndrome. Clin Exp Rheumatol 30:686–692
Buvry C, Cassagnes L, Tekath M, Artigues M, Pereira B, Rieu V et al (2020) Anti-Ro52 antibodies are a risk factor for interstitial lung disease in primary Sjögren syndrome. Respir Med 163:105895. https://doi.org/10.1016/j.rmed.2020.105895
Quartuccio L, Baldini C, Bartoloni E, Priori R, Carubbi F, Corazza L et al (2015) Anti-SSA/SSB-negative Sjögren’s syndrome shows a lower prevalence of lymphoproliferative manifestations, and a lower risk of lymphoma evolution. Autoimmun Rev 14:1019–1022
ter Borg EJ, Kelder JC (2014) Lower prevalence of extra-glandular manifestations and anti-SSB antibodies in patients with primary Sjögren’s syndrome and widespread pain: Evidence for a relatively benign subset. Clin Exp Rheumatol 32:349–353
Baer AN, McAdams DeMarco M, Shiboski SC, Lam MY, Challacombe S, Daniels TE et al (2015) The SSB-positive/SSA-negative antibody profile is not associated with key phenotypic features of Sjögren’s syndrome. Ann Rheum Dis 74:1557–1561
Acar-Denizli N, Horváth IF, Mandl T, Priori R, Vissink A, Hernandez-Molina G et al (2020) Systemic phenotype related to primary Sjögren’s syndrome in 279 patients carrying isolated anti-La/SSB antibodies. Clin Exp Rheumatol 38(Suppl 126):85–94
Baer AN, Medrano L, McAdams-DeMarco M, Gniadek TJ (2016) Association of anticentromere antibodies with more severe exocrine glandular dysfunction in Sjögren’s syndrome: Analysis of the Sjögren’s International Collaborative Clinical Alliance Cohort. Arthritis Care Res (Hoboken) 68:1554–1559
Ryu YS, Park SH, Lee J, Kwok SK, Ju JH, Kim HY et al (2013) Follow-up of primary Sjogren’s syndrome patients presenting positive anti-cyclic citrullinated peptides antibody. Rheumatol Int 33:1443–1446
Ramos-Casals M, Stone JH, Cid MC, Bosch X (2012) The cryoglobulinaemias. Lancet 379:348–360
La Civita L, Zignego AL, Monti M, Longombardo G, Pasero G, Ferri C (1995) Mixed cryoglobulinemia as a possible preneoplastic disorder. Arthritis Rheum 38:1859–1860
Brito-Zerón P, Kostov B, Solans R, Fraile G, Suárez-Cuervo C, Casanovas A et al (2016) Systemic activity and mortality in primary Sjögren syndrome: Predicting survival using the EULAR-SS Disease Activity Index (ESSDAI) in 1045 patients. Ann Rheum Dis 75:348–355
Quartuccio L, Isola M, Baldini C, Priori R, Bocci EB, Carubbi F et al (2014) Biomarkers of lymphoma in Sjögren’s syndrome and evaluation of the lymphoma risk in prelymphomatous conditions: results of a multicenter study. J Autoimmun 51:75–80
Legatowicz-Koprowska M, Nitek S, Czerwińska J (2020) The complement system in primary Sjögren’s syndrome: The expression of certain cascade and regulatory proteins in labial salivary glands – observational study. Reumatologia 58:357–366
Baimpa E, Dahabreh IJ, Voulgarelis M, Moutsopoulos HM (2009) Hematologic manifestations and predictors of lymphoma development in primary Sjögren syndrome: Clinical and pathophysiologic aspects. Medicine (Baltimore) 88:284–293
Brito-Zerón P, Retamozo S, Gandía M, Akasbi M, Pérez-De-Lis M, Diaz-Lagares C et al (2012) Monoclonal gammopathy related to Sjögren syndrome: a key marker of disease prognosis and outcomes. J Autoimmun 39:43–48
Denton CP, Khanna D (2017) Systemic sclerosis. Lancet 390:1685–1699
Chifflot H, Fautrel B, Sordet C, Chatelus E, Sibilia J (2008) Incidence and prevalence of systemic sclerosis: a systematic literature review. Semin Arthritis Rheum 37:223–235
Medsger TA Jr (2003) Natural history of systemic sclerosis and the assessment of disease activity, severity, functional status, and psychologic well-being. Rheum Dis Clin North Am 29:255–273
Steen VD (2005) Autoantibodies in systemic sclerosis. Semin Arthritis Rheum 35:35–42
Kayser C, Fritzler MJ (2015) Autoantibodies in systemic sclerosis: Unanswered questions. Front Immunol 6:167
Mehra S, Walker J, Patterson K, Fritzler MJ (2013) Autoantibodies in systemic sclerosis. Autoimmun Rev 12:340–354
Sirotti S, Generali E, Ceribelli A, Isailovic N, De Santis M, Selmi C (2017) Personalized medicine in rheumatology: The paradigm of serum autoantibodies. Autoimmun Highlights 8:10
Walker UA, Tyndall A, Czirják L, Denton C, Farge-Bancel D, Kowal-Bielecka O et al (2007) Clinical risk assessment of organ manifestations in systemic sclerosis: a report from the EULAR Scleroderma Trials and Research group database. Ann Rheum Dis 66:754–763
Hu PQ, Fertig N, Medsger TA Jr, Wright TM (2003) Correlation of serum anti-DNA topoisomerase I antibody levels with disease severity and activity in systemic sclerosis. Arthritis Rheum 48:1363–1373
Kuwana M, Kaburaki J, Okano Y, Tojo T, Homma M (1994) Clinical and prognostic associations based on serum antinuclear antibodies in Japanese patients with systemic sclerosis. Arthritis Rheum 37:75–83
Shah AA, Hummers LK, Casciola-Rosen L, Visvanathan K, Rosen A, Wigley FM (2015) Examination of autoantibody status and clinical features associated with cancer risk and cancer associated scleroderma. Arthritis Rheumatol 67:1053–1061
Roofeh D, Khanna D (2020) Management of systemic sclerosis: The first five years. Curr Opin Rheumatol 32:228–237
Saito A, Muro Y, Sugiura K, Akiyama M (2013) Low prevalence of autoantibodies to CENP-H, -I, -K, -L, -M, -N, -T and -U in a Japanese cohort of anti-centromere positive samples. Immunopharmacol Immunotoxicol 35:57–63
Patterson KA, Roberts-Thomson PJ, Lester S, Tan JA, Hakendorf P, Rischmueller M et al (2015) Interpretation of an extended autoantibody profile in a well-characterized Australian systemic sclerosis (scleroderma) cohort using principal components analysis. Arthritis Rheumatol 67:3234–3244
Kallenberg CG, Wouda AA, Hoet MH, van Venrooij WJ (1988) Development of connective tissue disease in patients presenting with Raynaud’s phenomenon: a six-year follow-up with emphasis on the predictive value of antinuclear antibodies as detected by immunoblotting. Ann Rheum Dis 47:634–641
Salliot C, Gottenberg JE, Bengoufa D, Desmoulins F, Miceli-Richard C, Mariette X (2007) Anti-centromere antibodies identify patients with Sjögren’s syndrome and autoimmune overlap syndrome. J Rheumatol 34:2253–2258
Hamaguchi Y, Kodera M, Matsushita T, Hasegawa M, Inaba Y, Usuda T et al (2015) Clinical and immunologic predictors of scleroderma renal crisis in Japanese systemic sclerosis patients with anti-RNA polymerase III autoantibodies. Arthritis Rheumatol 67:1045–1052
Lazzaroni MG, Cavazzana I, Colombo E, Dobrota R, Hernandez J, Hesselstrand R et al (2017) Malignancies in patients with anti-RNA polymerase III antibodies and systemic sclerosis: Analysis of the EULAR scleroderma trials and research cohort and possible recommendations for screening. J Rheumatol 44:639–647
Phan TG, Cass A, Gillin A, Trew P, Fertig N, Sturgess A (1999) Anti-RNA polymerase III antibodies in the diagnosis of scleroderma renal crisis sine scleroderma. J Rheumatol 26:2489–2492
Ceribelli A, Cavazzana I, Airo P, Franceschini F (2010) Anti-RNA polymerase III antibodies as a risk marker for early gastric antral vascular ectasia (GAVE) in systemic sclerosis. J Rheumatol 37:1544
Sharif R, Fritzler MJ, Mayes MD, Gonzalez EB, McNearney TA, Draeger H et al (2011) Anti-fibrillarin antibody in African American patients with systemic sclerosis: Immunogenetics, clinical features, and survival analysis. J Rheumatol 38:1622–1630
Aggarwal R, Lucas M, Fertig N, Oddis CV, Medsger TA Jr (2009) Anti-U3 RNP autoantibodies in systemic sclerosis. Arthritis Rheum 60:1112–1118
Mitri GM, Lucas M, Fertig N, Steen VD, Medsger TA Jr (2003) A comparison between anti-Th/To- and anticentromere antibody-positive systemic sclerosis patients with limited cutaneous involvement. Arthritis Rheum 48:203–209
Fischer A, Pfalzgraf FJ, Feghali-Bostwick CA, Wright TM, Curran-Everett D, West SG et al (2006) Anti-Th/To-positivity in a cohort of patients with idiopathic pulmonary fibrosis. J Rheumatol 33:1600–1605
Hudson M, Pope J, Mahler M, Tatibouet S, Steele R, Baron M et al (2012) Clinical significance of antibodies to Ro52/TRIM21 in systemic sclerosis. Arthritis Res Ther 14:R50
Fertig N, Domsic RT, Rodriguez-Reyna T, Kuwana M, Lucas M, Medsger TA Jr et al (2009) Anti-U11/U12 RNP antibodies in systemic sclerosis: a new serologic marker associated with pulmonary fibrosis. Arthritis Rheum 61:958–965
Mierau R, Moinzadeh P, Riemekasten G, Melchers I, Meurer M, Reichenberger F et al (2011) Frequency of disease-associated and other nuclear autoantibodies in patients of the German Network for Systemic Scleroderma: Correlation with characteristic clinical features. Arthritis Res Ther 13:R172
Muro Y, Hosono Y, Sugiura K, Ogawa Y, Mimori T, Akiyama M (2015) Anti-PM/Scl antibodies are found in Japanese patients with various systemic autoimmune conditions besides myositis and scleroderma. Arthritis Res Ther 17:57
Hoa S, Hudson M, Troyanov Y, Proudman S, Walker J, Stevens W et al (2016) Single-specificity anti-Ku antibodies in an international cohort of 2140 systemic sclerosis subjects: Clinical associations. Medicine (Baltimore) 95:e4713
Fujii T, Mimori T, Akizuki M (1996) Detection of autoantibodies to nucleolar transcription factor NOR 90/hUBF in sera of patients with rheumatic diseases, by recombinant autoantigen-based assays. Arthritis Rheum 39:1313–1318
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292:344–347
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292:403–407
Mariampillai K, Granger B, Amelin D, Guiguet M, Hachulla E, Maurier F et al (2018) Development of a new classification system for idiopathic inflammatory myopathies based on clinical manifestations and myositis-specific autoantibodies. JAMA Neurol 75:1528–1537
Tanboon J, Uruha A, Stenzel W, Nishino I (2020) Where are we moving in the classification of idiopathic inflammatory myopathies? Curr Opin Neurol 33:590–603
Meyer A, Meyer N, Schaeffer M, Gottenberg JE, Geny B, Sibilia J (2015) Incidence and prevalence of inflammatory myopathies: a systematic review. Rheumatology (Oxford) 54:50–63
Riddell V, Bagby S, McHugh N (2020) Myositis autoantibodies: recent perspectives. Curr Opin Rheumatol 32:548–552
Satoh M, Tanaka S, Ceribelli A, Calise SJ, Chan EKL (2017) Comprehensive overview on myositis-specific antibodies: New and old biomarkers in idiopathic inflammatory myopathy. Clin Rev Allergy Immunol 52:1–19
Mahler M, Miller FW, Fritzler MJ (2014) Idiopathic inflammatory myopathies and the anti-synthetase syndrome: a comprehensive review. Autoimmun Rev 13:367–371
Brouwer R, Hengstman GJ, Vree Egberts W, Ehrfeld H, Bozic B, Ghirardello A et al (2001) Autoantibody profiles in the sera of European patients with myositis. Ann Rheum Dis 60:116–123
Aggarwal R, Cassidy E, Fertig N, Koontz DC, Lucas M, Ascherman DP et al (2014) Patients with non-Jo-1 anti-tRNA-synthetase autoantibodies have worse survival than Jo-1 positive patients. Ann Rheum Dis 73:227–232
Mammen AL (2011) Autoimmune myopathies: Autoantibodies, phenotypes and pathogenesis. Nat Rev Neurol 7:343–354
Okiyama N (2021) Clinical features and cutaneous manifestations of juvenile and adult patients of dermatomyositis associated with myositis-specific autoantibodies. J Clin Med 10:1725
Fujimoto M, Hamaguchi Y, Kaji K, Matsushita T, Ichimura Y, Kodera M et al (2012) Myositis-specific anti-155/140 autoantibodies target transcription intermediary factor 1 family proteins. Arthritis Rheum 64:513–522
Palterer B, Vitiello G, Carraresi A, Giudizi MG, Cammelli D, Parronchi P (2018) Bench to bedside review of myositis autoantibodies. Clin Mol Allergy 16:5–22
Koga T, Fujikawa K, Horai Y, Okada A, Kawashiri SY, Iwamoto N et al (2012) The diagnostic utility of anti-melanoma differentiation-associated gene 5 antibody testing for predicting the prognosis of Japanese patients with DM. Rheumatology (Oxford) 51:1278–1284
Fiorentino D, Chung L, Zwerner J, Rosen A, Casciola-Rosen L (2011) The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol 65:25–34
Betteridge Z, Gunawardena H, North J, Slinn J, McHugh N (2007) Identification of a novel autoantibody directed against small ubiquitin-like modifier activating enzyme in dermatomyositis. Arthritis Rheum 56:3132–3137
Basharat P, Christopher-Stine L (2015) Immune-mediated necrotizing myopathy: Update on diagnosis and management. Curr Rheumatol Rep 17:72
Pluk H, van Hoeve BJ, van Dooren SH, Stammen-Vogelzangs J, van der Heijden A, Schelhaas HJ et al (2013) Autoantibodies to cytosolic 5’-nucleotidase 1A in inclusion body myositis. Ann Neurol 73:397–407
Amlani A, Choi MY, Tarnopolsky M, Brady L, Clarke AE, Garcia-De La Torre I et al (2019) Anti-NT5c1A autoantibodies as biomarkers in inclusion body myositis. Front Immunol 10:745
Herbert MK, Stammen-Vogelzangs J, Verbeek MM, Rietveld A, Lundberg IE, Chinoy H et al (2016) Disease specificity of autoantibodies to cytosolic 5’-nucleotidase 1A in sporadic inclusion body myositis versus known autoimmune diseases. Ann Rheum Dis 75:696–701
Rietveld A, Wienke J, Visser E, Vree Egberts W, Schlumberger W, van Engelen B et al (2021) Juvenile Dermatomyositis Research Group and the Dutch Myositis Consortium. Anti-Cytosolic 5'-nucleotidase 1A autoantibodies are absent in juvenile dermatomyositis. Arthritis Rheumatol 73:1329–1333
European Association for the Study of the Liver (2015) EASL clinical practice guidelines: Autoimmune hepatitis. J Hepatol 63:971–1004
European Association for the Study of the Liver (2017) EASL clinical practice guidelines: The diagnosis and management of patients with primary biliary cholangitis. J Hepatol 67:145–172
Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ et al (2009) Primary biliary cirrhosis. Hepatology 50:291–308
Manns MP, Lohse AW, Vergani D (2015) Autoimmune hepatitis – update 2015. J Hepatol 62:100–111
Sebode M, Weiler-Normann C, Liwinski T, Schramm C (2018) Autoantibodies in autoimmune liver disease-clinical and diagnostic relevance. Front Immunol 9:609
Gregorio GV, Portmann B, Reid F, Donaldson PT, Doherty DG, McCartney M et al (1997) Autoimmune hepatitis in childhood: a 20-year experience. Hepatology 25:541–547
Homberg JC, Abuaf N, Bernard O, Islam S, Alvarez F, Khalil SH et al (1987) Chronic active hepatitis associated with anti-liver/kidney microsome antibody type 1: a second type of autoimmune hepatitis. Hepatology 7:1333–1339
Martini E, Abuaf N, Cavalli F, Durand V, Johanet C, Homberg JC (1988) Antibody to liver cytosol (anti-LC1) in patients with autoimmune chronic active hepatitis type 2. Hepatology 8:1662–1666
Cotler SJ, Kanji K, Keshavarzian A, Jensen DM, Jakate S (2004) Prevalence and significance of autoantibodies in patients with non-alcoholic steatohepatitis. J Clin Gastroenterol 38:801–804
Vergani D, Alvarez F, Bianchi FB, Cançado EL, Mackay IR, Manns MP et al (2004) Liver autoimmune serology: a consensus statement from the Committee for Autoimmune Serology of the International Autoimmune Hepatitis Group. J Hepatol 41:677–683
Frenzel C, Herkel J, Lüth S, Galle PR, Schramm C, Lohse AW (2006) Evaluation of F-actin ELISA for the diagnosis of autoimmune hepatitis. Am J Gastroenterol 101:2731–2736
Liaskos C, Bogdanos DP, Davies ET, Dalekos GN (2007) Diagnostic relevance of anti-filamentous actin antibodies in autoimmune hepatitis. J Clin Pathol 60:107–108
Terjung B, Worman HJ, Herzog V, Sauerbruch T, Spengler U (2001) Differentiation of antineutrophil nuclear antibodies in inflammatory bowel and autoimmune liver diseases from antineutrophil cytoplasmic antibodies (p-ANCA) using immunofluorescence microscopy. Clin Exp Immunol 126:37–46
Gueguen M, Meunier-Rotival M, Bernard O, Alvarez F (1988) Anti-liver kidney microsome antibody recognizes a cytochrome P450 from the IID subfamily. J Exp Med 168:801–806
Manns MP, Johnson EF, Griffin KJ, Tan EM, Sullivan KF (1989) Major antigen of liver kidney microsomal autoantibodies in idiopathic autoimmune hepatitis is cytochrome P450db1. J Clin Invest 83:1066–1072
Zanger UM, Hauri HP, Loeper J, Homberg JC, Meyer UA (1988) Antibodies against human cytochrome P-450db1 in autoimmune hepatitis type II. Proc Natl Acad Sci USA 85:8256–8260
Lapierre P, Hajoui O, Homberg JC, Alvarez F (1999) Formiminotransferase cyclo-deaminase is an organ-specific autoantigen recognized by sera of patients with autoimmune hepatitis. Gastroenterology 116:643–649
Lenzi M, Manotti P, Muratori L, Cataleta M, Ballardini G, Cassani F et al (1995) Liver cytosolic 1 antigen-antibody system in type 2 autoimmune hepatitis and hepatitis C virus infection. Gut 36:749–754
Kanzler S, Weidemann C, Gerken G, Löhr HF, Galle PR, zum Büschenfelde KHM et al (1999) Clinical significance of autoantibodies to soluble liver antigen in autoimmune hepatitis. J Hepatol 31:635–640
Kirstein MM, Metzler F, Geiger E, Heinrich E, Hallensleben M, Manns MP et al (2015) Prediction of short- and long-term outcome in patients with autoimmune hepatitis. Hepatology 62:1524–1535
Montano-Loza AJ, Shums Z, Norman GL, Czaja AJ (2012) Prognostic implications of antibodies to Ro/SSA and soluble liver antigen in type 1 autoimmune hepatitis. Liver Int 32:85–92
Rigopoulou EI, Roggenbuck D, Smyk DS, Liaskos C, Mytilinaiou MG, Feist E et al (2012) Asialoglycoprotein receptor (ASGPR) as target autoantigen in liver autoimmunity: Lost and found. Autoimmun Rev 12:260–269
Liberal R, Mieli-Vergani G, Vergani D (2013) Clinical significance of autoantibodies in autoimmune hepatitis. J Autoimmun 46:17–24
Selmi C, Ceribelli A, Generali E, Scirè CA, Alborghetti F, Colloredo G et al (2016) Serum antinuclear and extractable nuclear antigen antibody prevalence and associated morbidity and mortality in the general population over 15 years. Autoimmun Rev 15:162–166
Satoh M, Chan EK, Ho LA, Rose KM, Parks CG, Cohn RD et al (2012) Prevalence and sociodemographic correlates of antinuclear antibodies in the United States. Arthritis Rheum 64:2319–2327
Agustinelli RA, Rodrigues SH, Mariz HA, Prado MS, Andrade LEC (2019) Distinctive features of positive anti-cell antibody tests (indirect immunofluorescence on HEp-2 cells) in patients with non-autoimmune diseases. Lupus 28:629–634
Keppeke GD, Nunes E, Ferraz ML, Silva EA, Granato C, Chan EK et al (2012) Longitudinal study of a human drug-induced model of autoantibody to cytoplasmic rods/rings following HCV therapy with ribavirin and interferon-α. PLoS One 7:e45392
Carcamo WC, Ceribelli A, Calise SJ, Krueger C, Chen L, Daves M et al (2013) Differential reactivity to IMPDH2 by anti-rods/rings autoantibodies and unresponsiveness to pegylated interferon-alpha/ribavirin therapy in US and Italian HCV patients. J Clin Immunol 33:420–426
Calise SJ, Chan EKL (2020) Anti-rods/rings autoantibody and IMPDH filaments: an update after fifteen years of discovery. Autoimmun Rev19:102643
Desmet VJ, Gerber M, Hoofnaagle JH, Manns M, Scheuer PJ (1994) Classification of chronic hepatitis: Diagnosis, grading and staging. Hepatology 19:1513–1520
Manns M, Gerken G, Kyriatsoulis A, Staritz M, zum Buschenfelde KHM (1987) Characterisation of a new subgroup of autoimmune chronic active hepatitis by autoantibodies against a soluble liver antigen. Lancet 1:292–294
Baeres M, Herkel J, Czaja AJ, Wies I, Kanzler S, Cancado EL et al (2002) Establishment of standardised SLA/LP immunoassays: Specificity for autoimmune hepatitis, worldwide occurrence, and clinical characteristics. Gut 51:259–264
Czaja AJ, Carpenter HA, Santrach PJ, Moore SB (1993) Significance of HLA DR4 in type 1 autoimmune hepatitis. Gastroenterology 105:1502–1507
O’Brien C, Joshi S, Feld JJ, Guindi M, Dienes HP, Heathcote EJ (2008) Long-term follow-up of antimitochondrial antibody-positive autoimmune hepatitis. Hepatology 48:550–556
Dinani AM, Fischer SE, Mosko J, Guindi M, Hirschfield GM (2012) Patients with autoimmune hepatitis who have antimitochondrial antibodies need longterm follow-up to detect late development of primary biliary cirrhosis. Clin Gastroenterol Hepatol 10:682–684
Leung PS, Rossaro L, Davis PA, Park O, Tanaka A, Kikuchi K et al (2007) Antimitochondrial antibodies in acute liver failure: Implications for primary biliary cirrhosis. Hepatology 46:1436–1442
Rigopoulou EI, Davies ET, Bogdanos DP, Liaskos C, Mytilinaiou M, Koukoulis GK et al (2007) Antimitochondrial antibodies of immunoglobulin G3 subclass are associated with a more severe disease course in primary biliary cirrhosis. Liver Int 27:1226–1231
Corpechot C, Chazouilleres O, Poupon R (2011) Early primary biliary cirrhosis: biochemical response to treatment and prediction of long-term outcome. J Hepatol 55:1361–1367
Muratori P, Muratori L, Cassani F, Terlizzi P, Lenzi M, Rodrigo L et al (2002) Anti-multiple nuclear dots (anti-MND) and anti-SP100 antibodies in hepatic and rheumatological disorders. Clin Exp Immunol 127:172–175
Andre C, Guillemin MC, Zhu J, Koken MH, Quignon F, Herve L et al (1996) The PML and PML/RARalpha domains: From autoimmunity to molecular oncology and from retinoic acid to arsenic. Exp Cell Res 229:253–260
Zuchner D, Sternsdorf T, Szostecki C, Heathcote EJ, Cauch-Dudek K, Will H (1997) Prevalence, kinetics, and therapeutic modulation of autoantibodies against Sp100 and promyelocytic leukemia protein in a large cohort of patients with primary biliary cirrhosis. Hepatology 26:1123–1130
Czaja AJ (2010) Autoantibodies as prognostic markers in autoimmune liver disease. Dig Dis Sci 55:2144–2161
Nakamura M, Kondo H, Mori T, Komori A, Matsuyama M, Ito M et al (2007) Anti-gp210 and anti-centromere antibodies are different risk factors for the progression of primary biliary cirrhosis. Hepatology 45:118–127
Sfakianaki O, Koulentaki M, Tzardi M, Tsangaridou E, Theodoropoulos PA, Castanas E et al (2010) Peri-nuclear antibodies correlate with survival in Greek primary biliary cirrhosis patients. World J Gastroenterol 16:4938–4943
Liberal R, Grant CR, Sakkas L, Bizzaro N, Bogdanos DP (2013) Diagnostic and clinical significance of anti-centromere antibodies in primary biliary cirrhosis. Clin Res Hepatol Gastroenterol 37:572–585
Norman GL, Reig A, Viñas O, Mahler M, Wunsch E, Milkiewicz P et al (2019) The prevalence of anti-hexokinase-1 and anti-Kelch-like 12 peptide antibodies in patients with primary biliary cholangitis is similar in Europe and North America: a large international, multi-center study. Front Immunol 10:662
Chazouillères O (2015) Overlap syndromes. Dig Dis Basel Switz 33(Suppl 2):181–187
Silveira MG, Talwalkar JA, Angulo P, Lindor KD (2007) Overlap of autoimmune hepatitis and primary biliary cirrhosis: Long-term outcomes. Am J Gastroenterol 102:1244–1250
Chazouillères O, Wendum D, Serfaty L, Montembault S, Rosmorduc O, Poupon R (1998) Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: clinical features and response to therapy. Hepatol Baltim Md 28:296–301
Nguyen HH, Shaheen AA, Baeza N, Lytvyak F, Urbanski SJ, Mason AL et al (2018) Evaluation of classical and novel autoantibodies for the diagnosis of primary biliary cholangitis–autoimmune hepatitis overlap syndrome (PBC-AIH OS). PLoS One 13:e0193960
Muratori P, Granito A, Pappas G, Pendino GM, Quarneti C, Cicola R et al (2009) The serological profile of the autoimmune hepatitis/primary biliary cirrhosis overlap syndrome. Am J Gastroenterol 104:1420–1425
Himoto T, Yoneyama H, Kurokohchi K, Inukai M, Masugata H, Goda F et al (2012) Clinical significance of autoantibodies to p53 protein in patients with autoimmune liver diseases. Can J Gastroenterol 26:125–129
Höftberger R (2015) Neuroimmunology: an expanding frontier in autoimmunity. Front Immunol 6:1–5
Flanagan EP (2019) Neuromyelitis optica spectrum disorder and other non-multiple sclerosis central nervous system inflammatory diseases. Continuum (Minneap Minn) 25:815–844
Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K et al (2004) A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet 364:2106–2112
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Pittock SJ, Berthele A, Fujihara K, Kim HJ, Levy M, Palace J et al (2019) Eculizumab in aquaporin-4–positive neuromyelitis optica spectrum disorder. N Engl J Med 381:614–625
Reindl M, Jarius S, Rostasy K, Berger T (2017) Myelin oligodendrocyte glycoprotein antibodies: How clinically useful are they? Curr Opin Neurol 30:295–301
Jarius S, Paul F, Aktas O, Asgari N, Dale RC, de Seze J et al (2018) MOG encephalomyelitis: International recommendations on diagnosis and antibody testing. Nervenarzt 89:1388–1399
dos Passos GR, Oliveira LM, da Costa BK, Apostolos-Pereira SL, Callegaro D, Fujihara K et al (2018) MOG-IgG-associated optic neuritis, encephalitis, and myelitis: Lessons learned from neuromyelitis optica spectrum disorder. Front Neurol 9:1–10
Sato DK, Callegaro D, Lana-Peixoto MA, Waters PJ, De Haidar Jorge FM, Takahashi T et al (2014) Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology 82:474–481
Hennes EM, Baumann M, Schanda K, Anlar B, Bajer-Kornek B, Blaschek A et al (2017) Prognostic relevance of MOG antibodies in children with an acquired demyelinating syndrome. Neurology 89:900–908
López-Chiriboga AS, Majed M, Fryer J, Dubey D, McKeon A, Flanagan EP et al (2018) Association of MOG-IgG serostatus with relapse after acute disseminated encephalomyelitis and proposed diagnostic criteria for MOG-IgG–associated disorders. JAMA Neurol 75:1355–1363
Graus F, Saiz A, Dalmau J (2020) GAD antibodies in neurological disorders — insights and challenges. Nat Rev Neurol 16:353–365
Ariño H, Höftberger R, Gresa-Arribas N, Martínez-Hernández E, Armangue T, Kruer MC et al (2015) Paraneoplastic neurological syndromes and glutamic acid decarboxylase antibodies. JAMA Neurol 72:1–8
Muñoz-Lopetegi A, de Bruijn MAAM, Boukhrissi S, Bastiaansen AEM, Nagtzaam MMP, Hulsenboom ESP et al (2020) Neurologic syndromes related to anti-GAD65. Neurol Neuroimmunol Neuroinflammation 7:e696
Dalmau J, Graus F (2018) Antibody-mediated encephalitis. N Engl J Med 378:840–851
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Van Coevorden-Hameete MH, de Graaff E, Titulaer MJ, Hoogenraad CC, Sillevis Smitt PAE (2014) Molecular and cellular mechanisms underlying anti-neuronal antibody mediated disorders of the central nervous system. Autoimmun Rev 13:299–312
Linnoila JJ, Binnicker MJ, Majed M, Klein CJ, McKeon A (2016) CSF herpes virus and autoantibody profiles in the evaluation of encephalitis. Neurol Neuroimmunol NeuroInflammation 3:1–10
Danieli D, Moraes ACM, Alves MP, Dutra LA, Höftberger R, Barsottini OGP et al (2017) Anti-N-methyl-D-aspartate receptor encephalitis and Epstein-Barr virus: Another tale on autoimmunity? Eur J Neurol 24:e46–e47
Dutra LA, Abrantes F, Toso FF, Pedroso JL, Barsottini OGP, Hoftberger R (2018) Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuropsiquiatr 76:41–49
Granerod J, Ambrose HE, Davies NWS, Clewley JP, Walsh AL, Morgan D et al (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10:835–844
Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA (2012) The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California encephalitis project. Clin Infect Dis 54:899–904
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165
Dubey D, Pittock SJ, Kelly CR, McKeon A, Lopez-Chiriboga AS, Lennon VA et al (2018) Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol 83:166–177
Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D (2012) Extreme delta brush; a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology 79:1094–1100
Balu R, Mccracken L, Lancaster E, Graus F, Dalmau J, Titulaer MJ (2019) A score that predicts 1-year functional status in patients with anti-NMDA receptor encephalitis. Neurology 92:e244–e252
Van Sonderen A, Ariño H, Petit-Pedrol M, Leypoldt F, Körtvélyessy P, Wandinger KP et al (2016) The clinical spectrum of Caspr2 antibody-associated disease. Neurology 87:521–528
Vale TC, Pedroso JL, Dutra LA, Azevedo L, Filho LHP, Prado LBF et al (2017) Morvan syndrome as a paraneoplastic disorder of thymoma with anti-CASPR2 antibodies. Lancet 389:1367–1368
Lopez-Chiriboga AS, Komorowski L, Kümpfel T, Probst C, Hinson SR, Pittock SJ et al (2016) Metabotropic glutamate receptor type 1 autoimmunity. Neurology 86:1009–1013
Höftberger R, van Sonderen A, Leypoldt F, Houghton D, Geschwind MD, Gelfand J et al (2015) Encephalitis and AMPA receptor antibodies. Neurology 84:2403–2412
Sabater L, Gaig C, Gelpi E, Bataller L, Lewerenz J, Torres-Vega E et al (2014) A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol 13:575–586
Gresa-Arribas N, Planagumà J, Petit-Pedrol M, Kawachi I, Katada S, Glaser CA et al (2016) Human neurexin-3α antibodies associate with encephalitis and alter synapse development. Neurology 86:2235–2242
Spatola M, Petit-Pedrol M, Simabukuro MM, Armangue T, Castro FJ, Artigues MIB et al (2017) Investigations in GABAA receptor antibody-associated encephalitis. Neurology 88:1012–1020
Hara M, Ariño H, Petit-Pedrol M, Sabater L, Titulaer MJ, Hernandez EM et al (2017) DPPX antibody-associated encephalitis main syndrome and antibody effects. Neurology 88:1340–1348
Höftberger R, Titulaer MJ, Sabater L, Dome B, Rózsás A, Hegedus B et al (2013) Encephalitis and GABAB receptor antibodies: Novel findings in a new case series of 20 patients. Neurology 81:1500–1506
Van Sonderen A, Thijs RD, Coenders EC, Jiskoot LC, Sanchez E, De Bruijn MAAM et al (2016) Anti-LGI1 encephalitis. Neurology 87:1449–1456
Kayser MS, Titulaer MJ, Gresa-Arribas N, Dalmau J (2013) Frequency and characteristics of isolated psychiatric episodes in anti-N-methyl-d-aspartate receptor encephalitis. JAMA Neurol 70:1133–1139
Bizzaro N, Tozzoli R, Tonutti E, Piazza A, Manoni F, Ghirardello A et al (1998) Variability between methods to determine ANA, anti-dsDNA and anti-ENA auto antibodies: a collaborative study with the biomedical industry. J Immunol Methods 219:99–107
Pereira KM, Dellavance A, Andrade LE (2014) The challenge of identification of autoantibodies specific to systemic autoimmune rheumatic diseases in high throughput operation: Proposal of reliable and feasible strategies. J Immunol Methods 437:203–210
Mummert E, Fritzler MJ, Sjowall C, Bentow C, Mahler M (2018) The clinical utility of anti-double-stranded DNA antibodies and the challenges of their determination. J Immunol Methods 459:11–19
Avrameas S (2016) Autopolyreactivity confers a holistic role in the immune system. Scand J Immunol 83:227–234
Nagele EP, Han M, Acharya NK, DeMarshall C, Kosciuk MC, Nagele RG (2013) Natural IgG autoantibodies are abundant and ubiquitous in human sera, and their number is influenced by age, gender, and disease. PLoS One 8:e60726
Kemeny DM (1991) A practical guide to ELISA. Pergamon Press, Oxford, England
Choi MY, Barber MR, Barber CE, Clarke AE, Fritzler MJ (2016) Preventing the development of SLE: Identifying risk factors and proposing pathways for clinical care. Lupus 25:838–849
Bossuyt X, Claessens J, Belmondo T, De Langhe E, Westhovens R, Poesen K et al (2019) Harmonization of clinical interpretation of antinuclear antibody test results by solid phase assay and by indirect immunofluorescence through likelihood ratios. Autoimmun Rev 18:102386
Fritzler MJ, Pauls JD, Kinsella TD, Bowen TJ (1985) Antinuclear, anticytoplasmic, and anti-Sjögren’s syndrome antigen A (SS-A/Ro) antibodies in female blood donors. Clin Immunol Immunopathol 36:120–128
Watanabe A, Kodera M, Sugiura K, Usuda T, Tan EM, Takasaki Y et al (2004) Anti-DFS70 antibodies in 597 healthy hospital workers. Arthritis Rheum 50:892–900
Dellavance A, Viana VS, Leon EP, Bonfa ES, Andrade LE, Leser PG (2005) The clinical spectrum of antinuclear antibodies associated with the nuclear dense fine speckled immunofluorescence pattern. J Rheumatol 32:2144–2149
Ochs RL, Stein TW Jr, Peebles CL, Gittes RF, Tan EM (1994) Autoantibodies in interstitial cystitis. J Urol 151:587–592
Ayaki M, Ohoguro N, Azuma N, Majima Y, Yata K, Ibaraki N et al (2002) Detection of cytotoxic anti-LEDGF autoantibodies in atopic dermatitis. Autoimmunity 35:319–327
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kayser, C., Dutra, L.A., dos Reis-Neto, E.T. et al. The Role of Autoantibody Testing in Modern Personalized Medicine. Clinic Rev Allerg Immunol 63, 251–288 (2022). https://doi.org/10.1007/s12016-021-08918-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-021-08918-6