Abstract
There is significant void in establishing validated non-invasive surrogate biomarkers of liver fibrosis/cirrhosis in chronic liver diseases (CLD). Golgi protein 73 (GP73) has been suggested as a potential serum marker for the diagnosis of hepatocellular carcinoma (HCC). However, significant background of cirrhosis could have accounted for the elevation of serum GP73 in HCC. In this study, we have taken advantage of a well-defined extensive cohort of 3044 patients with either compensated cirrhosis (n = 1247), decompensated cirrhosis (n = 841) or pre-cirrhotic CLD (n = 956) and our ability to quantify serum GP73 to define the potential of serum GP73 as a biomarker of liver cirrhosis/fibrosis in CLD. The diagnostic value of GP73 was compared with aspartate aminotransferase-to-platelet ratio index (APRI), fibrosis index based on four factors (FIB-4) and liver stiffness measurement (LSM). Immunohistochemical analysis was performed to measure hepatic GP73 expression. Receiver operating characteristic curve analysis demonstrated that serum GP73 had a good diagnostic potential for compensated cirrhosis regardless of etiology. The diagnostic performance of GP73 is better than APRI, FIB-4 and similar with LSM, especially in patients with severe inflammation, steatosis and cholestasis. Notably, in patients of autoimmune liver diseases, non-alcoholic fatty liver disease and viral hepatitis, serum GP73 also exhibited diagnostic value for advanced fibrosis as well as cirrhosis. Furthermore, there is also a gradual increase in GP73 expression with disease progression from mild fibrosis to cirrhosis. In conclusion, GP73 is an effective and reliable serological marker for the diagnosis of advanced fibrosis and prediction of appearance of cirrhosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic liver diseases (CLD) pose significant health problems worldwide and account for about 1.5 million deaths annually [1,2,3,4]. Chronic hepatitis B (CHB), chronic hepatitis C (CHC) and non-alcoholic fatty liver disease (NAFLD), as well as primary biliary cholangitis (PBC) and autoimmune hepatitis (AIH), the autoimmune-mediated CLD, attribute to the end-stage liver diseases in China and worldwide [5,6,7,8,9]. Despite various means of clinical interventions in CLD, hepatic transplant remains the ultimate effective treatment for patients with end-stage CLD [10].
Liver fibrosis is a significant predictor of disease progression and clinical outcomes in patients with CLD [7, 11]. Since fibrosis or even early cirrhosis may be reversible with early clinical intervention [12,13,14,15], reliable methods for evaluating and monitoring the stage of liver fibrosis and cirrhosis are critical for optimal management of CLD [16, 17]. Liver biopsy has long been regarded as the “gold standard” for staging liver fibrosis and compensated cirrhosis [18]. However, sampling error, cost, potential medical complications and inter-observer variability have limited the use of liver biopsy [19,20,21,22,23]. Therefore, novel non-invasive biomarkers for accurate diagnosis and disease staging in CLD patients are necessary [24].
Non-invasive methods including serum markers and imaging techniques offer potential alternatives to liver biopsy. Among them, AST-to-platelet ratio index (APRI), fibrosis index based on four factors (FIB-4) and liver stiffness measurement (LSM) are relatively inexpensive and commonly accessible in most hospitals. However, various factors including necroinflammation, steatosis and cholestasis have affected their specificities [25,26,27,28,29,30].
GP73 is a resident Golgi trans-membrane glycoprotein primarily expressed in biliary epithelial cells but rarely in hepatocytes in normal livers [31]. Recently, serum GP73 was reported as a potential diagnostic marker for HCC [32,33,34,35,36]. However, serum GP73 can also elevate in patients with liver cirrhosis even at levels higher than HCC [33, 37,38,39] and has compromised its diagnostic accuracy in HCC because most HCC cases develop from cirrhosis [40,41,42].
In this study, we first examined the potential value of serum GP73 in diagnosing CLD both in cirrhotic and pre-cirrhotic CLD subjects. Then, we compared the diagnostic value between APRI, FIB-4, LSM and serum GP73 in patients with fibrosis and compensated cirrhosis with different etiologies including CHB, CHC, NAFLD as well as autoimmune-mediated liver diseases AIH and PBC. The levels of serum GP73 and GP73 protein expression in liver tissues at different fibrotic stages were also examined. Finally, we investigated IL-6/STAT3 signaling as a possible mechanism for the elevated serum GP73 in patients with fibrosis/cirrhosis.
Methods
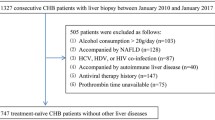
Subjects
This retrospective study includes 3044 patients with either pre-cirrhotic CLD (n = 956), compensated cirrhosis (n = 1247) or decompensated cirrhosis (n = 841) in Beijing 302 Hospital and Shanghai Renji Hospital between January 2010 and March 2016 (Fig. 1). The demographics and laboratory data including levels of GP73 of these patients were collected (Table 1). As control, 121 healthy volunteers without acute or chronic diseases, hyperlipidemia, diabetes, hypertension and BMI higher than 28 were also included, and their levels of serum GP73 were quantified.
The diagnostic criteria for compensated cirrhosis include the following: (a) typical findings of CT or MRI with one of the following observations: irregular liver surface, granular or nodular liver parenchyma with or without splenomegaly (thickness of spleen > 4 cm or > 5 pedicle-rib units); (b) platelet count of <100,000/mm3 excluding the other possible causes; (c) serum albumin <3.5 g/dL, prolonged prothrombin time or increased international normalized ratios (INR) > 1.3 (anticoagulants or thrombolytic drugs discontinued for >7 days) and (d) no history of decompensated cirrhosis defined as jaundice in the presence of cirrhosis, ascites, bleeding gastric or esophageal varies or encephalopathy.
For pre-cirrhotic CLD patients, the definition of NAFLD requires that (a) there is evidence of hepatic steatosis, either by imaging or by histology and (b) there are no causes for secondary hepatic fat accumulation such as significant alcohol consumption, use of steratogenic medication or hereditary disorders [5]. The diagnosis of CHB was based on hepatitis B surface antigen (HBsAg) positive for more than 6 months, with clinical or laboratory signs of chronic hepatitis [43]. The diagnosis of chronic hepatitis C (CHC) was based on the detection of both hepatitis C virus (HCV) antibodies and HCV RNA in the presence of signs of chronic hepatitis [44]. Autoimmune liver diseases (AILDs) including AIH and PBC were diagnosed based on established criteria [45, 46]. This study was approved by the Ethics Committee of Beijing 302 Hospital and Shanghai Renji Hospital. Informed consent was obtained from all participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Liver Histology
The scoring of liver fibrosis and necroinflammation activity was based on histopathological examination of percutaneous liver biopsy specimens. Liver tissue specimens were fixed in buffered formalin, embedded in paraffin and then subjected to hematoxylin and eosin (H & E) and Masson trichrome staining. The slides were reviewed by an experienced pathologist, who was blinded to the patients’ clinical information. Necroinflammation activity was identified according to the METAVIR system: A = histological activity (A0 = no activity, A1 = mild activity, A2 = moderate activity, and A3 = severe activity) [47]. Liver fibrosis in NAFLD, AIH and PBC patients was staged according to the Brunt staging system [5, 48] with F1 defined as perisinusoidal or periportal fibrosis, F2 as perisinusoidal fibrosis with portal or periportal involvement, F3 as bridging fibrosis and F4 as cirrhosis. In this study, significant fibrosis is defined as a score of ≥ F2 and advanced fibrosis of ≥ F3 [48].
LSM
LSM was performed with FibroScan® (Echosens, Paris, France) within one week of liver biopsy. The measurements were performed blinded to the results of the biopsy. LSM was determined in the right hepatic lobe through the intercostal space with the patient (at least 2 h after meal) in the supine position and the right arm in maximum abduction. The results were expressed in kilopascals (kPa) corresponding to the median of ten determinations. Only valid measurements (success rate of more than 60% and interquartile range/median ratio < 0.3) were included [49].
Determination of Serum Levels of GP73, ALT, AST and Platelet Count
Quantitative detection of serum GP73 was performed with a double-antibody sandwich enzyme-linked immunosorbent assay (ELISA) kit (Hotgen Biotech Inc., Beijing, China), according to the manufacturer’s protocol. In brief, sample dilution buffer (50 μL) and 20 μL serum were added to wells precoated with monoclonal anti-GP73 and incubated for 1 h at 37 °C. The wells were washed and then incubated with 100 μL of HRP-conjugated anti-human antibody for 30 min at 37 °C. After washing for five times, the plate was developed with tetramethylbenzidine, and OD450 was measured with a microplate reader (Thermo Labsystems, Vantaa, Finland). Purified recombinant GP73 was assayed in parallel as a calibration standard. All assays were run in duplicate and repeated twice.
The levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were measured using an automatic biochemical analyzer (Beckman, CA, USA). Platelet count was measured by an electrical resistance method (Sysmex, Kobe, Japan). APRI was defined as [(AST/ULN)/platelet count (109/L)] × 100. FIB-4 was calculated according to the following formula: FIB-4 = (age × AST) / (platelet count [109/L] × ALT1/2). The upper limit of normal (ULN) for both AST and ALT was 40 U/L.
Immunohistochemistry
Immunohistochemistry for GP73 was performed using paraffin-embedded liver tissues. Firstly, liver tissues were dewaxed at 70 °C for 1 h, microwaved in 10 mM citrate buffer (pH 6.0) and cooled to room temperature. After washing with PBS (phosphate buffered saline, pH 7.6) for three times, tissues were covered with 3% H2O2 for 20 min to block endogenous peroxidase activity. Thereafter, the tissues were incubated with 25% goat serum for 45 min, washed and incubated with primary antibody 1:1000 dilution (ab109628; Abcam, UK) for 2 h at 37 °C. After washing, the tissues were incubated with universal horseradish peroxidase conjugated anti-mouse/rabbit antibody (D-3004, Supervision™, China) for 30 min at room temperature then visualized using a 3, 3-diaminobenzidine color kit (DAB-0031, Maixin Biotech, China) and counterstained with hematoxylin (G1080, Solarbio Science & Technology, China).
Cell Culture and Reverse Transcription-Quantitative PCR (RT-qPCR)
Human liver cancer cell line Huh7 was purchased from the American Type Culture Collection (ATCC) and cultured in DMEM (19217008, Sigma-Aldrich, USA) with 8% fetal bovine serum (r35-076-cv, cellgro, USA) in a 5% CO2 incubator at 37 °C. Cells were treated with 25 ng/mL IL-6 (200-06-20, PeproTech, USA) for 2 h, and total RNA was extracted with TRIzol (15596018, Invitrogen, USA). cDNA was synthesized from 1 μg RNA using an all-in-one first-strand cDNA synthesis supermix for quantitative PCR (qPCR) (AT341-02, TransGen Biotech, China). qPCR for furin and GP73 were performed with actin as housekeeping gene using FS Universal SYBR Green Master (4913914001, Roche, USA). The primers used for qPCR were listed in supplementary materials (Supplementary Table 1).
Dual-Luciferase Reporter Assay
GP73 promoter was amplified from genomic DNA extracted from Huh7 cells and cloned into pGL3-luc firefly luciferase reporter vector [50]. pGL-furin promoter-luc and pGL3-pim1 promoter-luc were constructed with similar method with specific PCR primers (Supplementary Table 2). pcDNA3.1-STAT3C (a constitutive active form of STAT3) expression plasmid was constructed as described previously [51]. For dual-luciferase reporter assay, Huh7 cells were transfected with either 300 ng pGL3-GP73 promoter-luc, 300 ng pGL3-furin promoter-luc or 300 ng pGL3-pim1 promoter-luc together with 1.2 μg pcDNA3.1-STAT3C and 50 ng pGL3-actin promoter-renilla. Fourty eight hours later, cells were harvested and analyzed by luciferase assay (E1980, Promega, USA). Briefly, cells were washed with PBS twice and lysed with 150 μL 1× passive lysis buffer for 30 min. After centrifuging for 10 min at 12,000 rpm, 20 μL of supernatant was transferred to 96-well plate in triplicate. A total of 25 μL of firefly luciferase reagent was then added and luminescence measured immediately, followed by addition of 25 μL of Renilla luciferase reagent and measurement of luminescence at 2 min. The results are expressed as ratio of firefly to Renilla luciferase activity.
Statistical Analysis
Descriptive statistics for GP73 in different patient groups were compared using box plot. The difference between groups was tested using the Mann–Whitney U test. The area under the receiver operating characteristic (ROC) curve (AUC) was used to evaluate the diagnostic performance. For the identification of significant or advanced liver fibrosis and cirrhosis, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated with an optimal cut-off value that maximized the sum of sensitivity and specificity. All statistical analyses were performed with MedCalc (15.8.1) software. All tests of significance were two-tailed, and p < 0.05 was considered statistically significant.
Results
Clinical Characteristics of Patients
A total of 3044 patients who fulfilled the study criteria were enrolled. Details of the patient groups and clinical data are shown in Fig. 1 and Table 1.
Serum Levels of GP73 Were Higher in Cirrhotic than in Pre-Cirrhotic CLD Patients
The serum levels of GP73 were significantly higher in cirrhosis patients when compared with those of the healthy controls and the pre-cirrhotic CLD groups (p < 0.001). Serum levels (median, IQR) of GP73 were 35.07 (24.97–45.37) ng/mL in healthy controls, 43.74 (28.24–61.34) ng/mL in pre-cirrhotic CLD group, 122.00 (82.33–181.28) ng/mL in compensated cirrhotic group and 149.85 (95.49–215.70) ng/mL in decompensated cirrhotic group. They all were significantly higher than that of CLD patients without cirrhosis (Supplementary Fig. 1).
Multivariate analysis was performed to determine if the increased levels of serum GP73 were liver fibrosis/cirrhosis relevant. The results indicated that higher serum GP73 level was independently associated with several fibrosis/cirrhosis relevant markers, including higher collagen type IV (CIV), hyalurona (HA), total bilirubin (Tbil), collagen type III N-terminal peptide (PIIINP), monocytes (MNC), globulin, fibrinogen (FIB), collagen type IV (C IV) and lower platelet count (PLT), respectively (Supplementary Table 3).
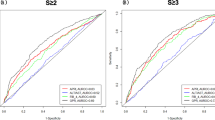
Serum Levels of GP73 Exhibited Better Diagnostic Value than APRI and FIB-4 in Patients with Compensated Cirrhosis
Analysis of the ROC values between GP73, APRI and FIB-4 indicated that GP73 had a better diagnostic value for compensated cirrhosis (AUC 0.899, 95% CI 0.886 to 0.911, p < 0.001) (Fig. 2a). To further confirm the diagnostic value of GP73 in compensated cirrhotic patients, stratified analysis was conducted based on the different etiologies of those compensated cirrhosis patients. ROC analysis indicated that the AUCs for cirrhosis due to CHB, chronic hepatitis C (CHC), AILDs, NAFLD and other causes were 0.880 (95% CI 0.857 to 0.900), 0.926 (95% CI 0.897 to 0.948), 0.885 (95% CI 0.846 to 0.917), 0.962 (95% CI 0.917 to 0.987) and 0.935 (95% CI 0.906 to 0.958), respectively (Fig. 2b–f).
Diagnostic values of serum GP73 for liver cirrhosis were analyzed using ROC curves. a The ROC curve of GP73 for diagnosing compensated cirrhosis regardless of etiologies (case number varies depending on the data available). b–f The ROC curve for diagnosing compensated cirrhosis among patients with different etiologies (case number varies depending on data availability. “Others” means causative factor other than HBV, HCV, AILDs or NAFLD)
Serum GP73 Had Better Performance for Diagnosing Cirrhosis in Patients with Active Hepatic Necroinflammation and Steatosis
To compare the performance of serum GP73 and LSM in the diagnosis of cirrhosis, we analyzed GP73 and LSM data within a subgroup of 1230 compensated cirrhotic patients. The AUC was 0.873 (95% CI 0.854 to 0.892) for GP73 and was 0.856 (95% CI 0.835 to 0.875) for LSM. When GP73 and LSM were combined, AUC was increased to 0.923 (95% CI 0.906 to 0.938), sensitivity was increased to 87.14% and specificity was increased to 86.71% (Fig. 3a). Even the negative predictive value (NPV) was also increased (Fig. 3a and Table 2).
It has been suggested that the application of LSM in clinical practice had some limitations. Therefore, additional evaluation of GP73 as a diagnostic marker was conducted. Noticeably, compared with LSM, serum GP73 had a better diagnostic value in patients with hepatic inflammation score of A ≥ 2 (AUC 0.888 vs 0.809), increased ALT (≥ 2 ULN, AUC 0.922 vs 0.858), increased fatty liver (AUC 0.959 vs 0.867), increased TBIL (≥ 1.5 ULN, AUC 0.919 vs 0.835) or increased TBA (≥ 2 ULN, AUC 0.962 vs 0.818) (Fig. 3b–f).
A Stepwise and Significant Increase of Serum GP73 Levels Was Observed with Fibrosis Disease Progression Among CLD Patients with Virus Hepatitis, AILDs or NAFLD
In order to investigate whether GP73 has potential value in predicting liver fibrosis in patients with viral hepatitis, AILDs or NAFLD, the levels (median, IQR) of serum GP73 of patients with different fibrotic stages were analyzed in several subgroups of patients with CHB and/or CHC (n = 271), AILDs (n = 168) and NAFLD (n = 143). The serum GP73 levels in CHB and/or CHC, AILDs and NAFLD correlated with the stage of fibrosis. The serum GP73 levels (median, IQR) in virus hepatitis in each stage were 38.48 (22.71–55.65) ng/mL (F0–1), 45.03 (28.67–58.01) ng/mL (F2), 65.35 (43.92–90.64) ng/mL (F3) and 129.50 (90.59–188.83) ng/mL (F4), respectively. A similar tendency was also observed in AILDs and NAFLD patients where serum GP73 levels (median, IQR) were 36.29 (27.67–47.11) ng/mL (F0–1), 53.37 (36.53–72.25) ng/mL (F2), 81.83 (59.34–129.40) ng/mL (F3) and 136.78 (111.72–221.50) ng/mL (F4) (for AILDs), and 32.54 (22.91–48.68) ng/mL (F0–1), 54.85 (45.72–77.12) ng/mL (F2), 69.52 (53.19–94.88) ng/mL (F3) and 127.60 (98.43–211.40) ng/mL (F4) (for NAFLD) (Fig. 4a–c).
Serum GP73 and hepatic GP73 were increased with liver fibrosis stage regardless of etiologies. Correlation between serum GP73 and liver fibrosis stages F0–F4 in virus hepatitis (a), AILDs (b) and NAFLD (c) patients; immunohistochemistry of GP73 protein in different degrees of fibrotic liver tissues, CHB (d), AILDs (e) and NAFLD (f) patients. *p value < 0.05, **p value < 0.01 based on differences between medians with the Mann–Whitney U test
To further validate the correlation between levels of GP73 expression in liver tissue and the fibrosis stage, the expression of GP73 protein in liver tissues with different fibrotic scores from patients of viral hepatitis, AILDs and NAFLD was analyzed by immunohistochemistry. Notably, a stepwise increase of GP73 expression in the liver tissue was observed with the increasing severity of liver fibrosis (Fig. 4d–f, Supplementary Fig. 2), and Spearman correlation analysis revealed that the expression of GP73 in situ was well correlated with the severity of fibrosis in viral hepatitis patients (r = 0.854, p < 0.001), in AILDs (r = 0.704, p < 0.001) and also in NAFLD (r = 0.671, p < 0.001).
Validation of the Diagnostic Value of Serum GP73 for Significant and Advanced Fibrosis As Well As Cirrhosis in Patients with Viral Hepatitis, AILDs or NAFLD
The AUC indicated that serum GP73 exhibited a potential to differentiate patients at different fibrotic stages in virus hepatitis, AILDs or NAFLD. The AUC for GP73 to predict significant fibrosis (≥ F2), severe fibrosis (≥ F3) and cirrhosis (F4) was 0.772, 0.854 and 0.890, respectively, for virus hepatitis, 0.855, 0.852 and 0.880, respectively, for AILDs, and 0.897, 0.935 and 0.960, respectively, for NAFLD (Table 3).
Validation of Serum GP73 Levels and Liver Expression in a Sub-Cohort of Patients with AIH and PBC
The levels (median, IQR) of serum GP73 were 35.18 (26.52–52.57) ng/mL (F0–1), 62.46 (36.41–86.37) ng/mL (F2), 92.10 (58.65–141.25) ng/mL (F3) and 150.48 (114.73–193.30) ng/mL (F4) in patients with AIH. A similar tendency was also observed in PBC patients where serum GP73 levels (median, IQR) were 36.43 (27.59–44.98) ng/mL (F0–1), 45.95 (36.41–60.87) ng/mL (F2), 77.18 (61.09–124.63) ng/mL (F3) and 125.90 (91.63–258.28) ng/mL (F4) (Fig. 5). The serum GP73 level in healthy controls was 35.07 (24.97–45.37) ng/mL, similar with those in fibrosis stage 0–1 patients. To determine whether increased serum GP73 is derived from the liver, immunohistochemical staining for GP73 was performed in 38 AIH patients and 36 PBC patients. As shown in Fig. 5, serum levels of GP73 were positively correlated with liver GP73 IH score for both AIH (r = 0.788, p < 0.0001) and PBC (r = 0.716, p < 0.0001), respectively.
Serum GP73 was increased with hepatic GP73 as liver fibrosis stage in AIH and PBC. a, d Serological GP73 levels of AIH and PBC patients at different fibrotic stages. b, c, e, f Analysis of immunohistochemical staining score of GP73 in liver tissues of patients with AIH and PBC and correlation between serum GP73 and liver fibrosis stages in AIH and PBC patients. *p value < 0.05, **p value < 0.01 based on differences between medians with the Mann–Whitney U test
GP73 Can Be Induced by IL-6 Through the STAT3 Signal Pathway
To investigate the mechanism of GP73 expression in fibrosis, we focused on IL-6/STAT3 signaling. Online prediction software (http://alggen.lsi.upc.es/, http://jaspar.genereg.net/) indicated that the STAT3 binding site is within the GP73 promoter region. Hence, we applied RT-qPCR and dual-luciferase reporter assay to detect whether GP73 could be up-regulated by IL-6/STAT3 signaling. After treatment with recombinant human IL-6 (rhIL-6), the mRNA level of GP73 in huh7 cell lysis increased about 0.5-fold. Interestingly, furin, which could slice GP73 from the Golgi membrane [52], was also increased in parallel with GP73 upon IL-6 simulation. Consistently, overexpression of STAT3C in Huh7 cells also increased the expression of GP73 as compared to control. Because a STAT3 binding site is found within the GP73 promoter, we performed the dual-luciferase reporter assay to detect the transcription activation of IL-6/STAT3 signaling on GP73 and furin promoter. The result showed that both IL-6 treatment and STAT3C overexpression could increase transcription of GP73 and furin (Supplementary Fig. 3). Taken together, the data here suggested that the increase of serum GP73 in liver fibrosis may be associated with transcriptional activation of GP73 and furin genes by IL-6/STAT3 signaling.
Discussion
The human GP73 is a 73-kDa protein of the cis-Golgi membrane. It is highly conserved in other species and normally expressed in epithelial tissues [53]. In normal liver, expression of GP73 is limited to biliary epithelial cells [54, 55]. Elevation of GP73 protein has also been reported in patients with giant-cell hepatitis and viral infections [53, 56], but the majority of data are from studies of HCC patients, which suggest GP37 as a serum marker for HCC. However, despite extensive data linking GP73 to cell proliferation in HCC [57,58,59,60,61], there is a paucity of evidence indicating that aberrant expression of GP73 is a driver of hepato-carcinogenesis. In contrast, our group and others have reported that GP73 is not necessarily relevant to the pathogenesis of HCC but rather increased in fibrosis and cirrhosis [62].
In this study, we demonstrated that the levels of serum GP73 are elevated in patients with fibrosis/cirrhosis and correlated well with its protein levels in fibrotic/cirrhotic liver tissues, which implicated the fibrosis/cirrhosis diagnosing value of serum GP73. Our data demonstrated that serum GP73 had a higher AUC in the diagnosis of compensated cirrhosis when compared with FIB-4 and APRI, the two most widely validated non-invasive modalities for cirrhosis [63, 64]. This observation is similar to previous study on patients with chronic HBV infection-related cirrhosis [65]. Nevertheless, our data indicated GP73 is a reliable CLD biomarker for predicting fibrosis in viral hepatitis, AILDs or NAFLD regardless of their etiologies (Table 3).
LSM is one of the validated non-invasive methods in evaluating liver cirrhosis and monitoring disease progression. However, one limiting issue is that optimal cut-off values vary for different etiologies [66]. In addition, several other factors including hepatic necroinflammation, steatosis and cholestasis can also affect the diagnostic accuracy of LSM [26,27,28,29]. Notably, our data showed that serum GP73 had relative good diagnostic performance in patients with fatty liver, significant liver necroinflammation (A ≥ 2 and/or ALT ≥ 2 ULN) and cholestasis (TBIL ≥ 1.5 ULN and/or TBA ≥ 2 ULN). It should be emphasized that, for the diagnosis of compensate cirrhosis, combination of GP73 and LSM increased the NPV, which reflects the reduction misdiagnosis rate.
AILDs progress rapidly and can lead to serious complications with high mortality [9, 67]. Although alkaline phosphatase is accepted in PBC as a surrogate marker of transplant-free survival, there is a significant void in predicting the development of fibrosis, not only in PBC but also in AIH [68, 69]. In the study herein, we evaluated the diagnostic potential of serum GP73 for liver fibrosis in AIH and PBC patients. AUCs analysis demonstrated that GP73 performed as well as widely used serum index APRI and FIB-4 in predicting AIH and PBC-related fibrosis stage. Furthermore, our data also demonstrated that GP73 measurements exhibit similar accuracy in predicting fibrosis and the diagnosis of cirrhosis in AIH and PBC patients to LSM. As a serum marker, GP73 measuring is easy and relatively inexpensive. Moreover, it avoids the sample errors and reduces the cost of transient elastography and discomfort of liver biopsy. Considering that AIH and PBC and other CLD require long-term follow-up, serum GP73 is potentially useful for serial monitoring of patients undergoing treatment and monitoring efficacy of new drugs.
Our previous results had shown that GP73 is not necessarily relevant to the pathogenesis of HCC, but rather it increased in fibrosis and cirrhosis [62], which suggested the involvement of GP73 in the disease progression of fibrosis and cirrhosis. Imbalance between liver necroinflammation and regeneration during persistent liver injury is the key factor that leads to hepatic fibrosis and cirrhosis regardless of etiology. Because plenty of evidences have linked GP73 to cell proliferation [57,58,59,60,61], it is reasonable to speculate that GP73 may play a positive role in liver regeneration and that enhanced GP73 expression may reflect the proliferative potential for hepatic parenchymal cells. In line with this, it has been reported that overexpression of GP73 could assist EGFR/RTK recycling, resulting in prolonged activation of the downstream signal pathway and proliferation of a variety of HCC cell lines [70]. IL-6 is considered one of the most significant factors for liver regeneration [71,72,73,74]. Importantly, previous studies have shown that GP73 expression can be affected by IL-6 [59]. In HepG2 cells, IL-6 could transcriptionally induce GP73 expression [75], implicating a role of GP73 in IL-6-mediated liver inflammation and regeneration. STAT3 is one of the most important downstream mediators of IL-6 signaling. Enhanced STAT3 binding and SNPs in STAT3 gene are associated with various multi-organ autoimmunities [76, 77]. By using online prediction software, we identified potential STAT3 binding site within the GP73 promoter region, as well as in the promoter region of the furin gene. By luciferase reporter assay, we demonstrated that STAT3c, the active form of STAT3 slightly increased the promoter activity of both GP73 and furin genes (Supplementary Fig. 3). Since the release of GP73 into serum is furin proteinase enzyme activity-dependent [52], our data further suggested the multiple roles of IL-6 which contribute to the aberrant elevation of serum GP73 seen in cirrhotic CLD patients.
In summary, we report that serum GP73 is a reliable marker for the diagnosis of compensated cirrhosis, with noticeably improved performance when compared with FIB-4 and APRI. In addition to diagnosing cirrhosis, serum GP73 could also differentiate significant and advanced fibrosis in AILDs or NAFLD patients. In viral hepatitis, serum GP73 could perform well in diagnosing advanced fibrosis. This study has significant clinical applications that may help to fill the void of reliable surrogate markers for fibrosis and cirrhosis in CLD. Future study is needed to define the molecular basis of the binding site of STAT3 and the GP73 promoter in the pathogenesis of CLD. Future multicenter study with prospective design is needed to validate the potential use of GP73 as a surrogate biomarker of liver cirrhosis/fibrosis in chronic liver disease.
Abbreviations
- GP73:
-
Golgi protein 73
- HCC:
-
hepatocellular carcinoma
- ALT:
-
alanine aminotransferase
- AST:
-
aspartate aminotransferase
- ALP:
-
alkaline phosphatase
- GGT:
-
gamma glutamyl transpeptidase
- TBA:
-
total bile acid
- ALB:
-
albumin
- PA:
-
prealbumin
- qPCR:
-
quantitative real-time PCR
- PLT:
-
platelet count
- IQR:
-
interquartile range
- APRI:
-
AST-to-platelet ratio index
- FIB-4:
-
fibrosis index based on four factors
- LSM:
-
liver stiffness measurement
- AILDs:
-
autoimmune liver diseases
- NAFLD:
-
non-alcoholic fatty liver disease
- CLD:
-
chronic liver diseases
- HBV:
-
hepatitis B virus
- CHB:
-
chronic hepatitis B
- HBsAg:
-
hepatitis B surface antigen
- HCV:
-
hepatitis C virus
- CHC:
-
chronic hepatitis C
- H & E:
-
hematoxylin and eosin
- HRP:
-
horseradish peroxidase
- ROC:
-
receiver operating characteristic curve
- AUC:
-
the area under the receiver operating characteristic curve
- PPV:
-
positive predictive value
- NPV:
-
negative predictive value
- BMI:
-
Body Mass Index
References
Ganem D, Prince AM (2004) Hepatitis B virus infection—natural history and clinical consequences. N Engl J Med 350(11):1118–1129. https://doi.org/10.1056/NEJMra031087
Lok AS, McMahon BJ (2007) Chronic hepatitis B. Hepatology 45(2):507–539. https://doi.org/10.1002/hep.21513
Thein HH, Yi Q, Dore GJ, Krahn MD (2008) Estimation of stage-specific fibrosis progression rates in chronic hepatitis C virus infection: a meta-analysis and meta-regression. Hepatology 48(2):418–431. https://doi.org/10.1002/hep.22375
Yang JD, Roberts LR (2010) Hepatocellular carcinoma: a global view. Nat Rev Gastroenterol Hepatol 7(8):448–458. https://doi.org/10.1038/nrgastro.2010.100
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ (2012) The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 55(6):2005–2023. https://doi.org/10.1002/hep.25762
Fan JG, Farrell GC (2009) Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol 50(1):204–210. https://doi.org/10.1016/j.jhep.2008.10.010
Kaswala DH, Lai M, Afdhal NH (2016) Fibrosis assessment in nonalcoholic fatty liver disease (NAFLD) in 2016. Dig Dis Sci 61(5):1356–1364. https://doi.org/10.1007/s10620-016-4079-4
Wang Z, Sheng L, Yang Y, Yang F, Xiao X, Hua J, Guo C, Wei Y, Tang R, Miao Q, Zhang J, Li Y, Fang J, Qiu D, Krawitt EL, Bowlus CL, Gershwin ME, Wang Q, Ma X (2017) The management of autoimmune hepatitis patients with decompensated cirrhosis: real-world experience and a comprehensive review. Clin Rev Allergy Immunol 52(3):424–435. https://doi.org/10.1007/s12016-016-8583-2
Yang F, Wang Q, Wang Z, Miao Q, Xiao X, Tang R, Chen X, Bian Z, Zhang H, Yang Y, Sheng L, Fang J, Qiu D, Krawitt EL, Gershwin ME, Ma X (2016) The natural history and prognosis of primary biliary cirrhosis with clinical features of autoimmune hepatitis. Clin Rev Allergy Immunol 50(1):114–123. https://doi.org/10.1007/s12016-015-8516-5
Neuberger J (2016) An update on liver transplantation: a critical review. J Autoimmun 66:51–59. https://doi.org/10.1016/j.jaut.2015.08.021
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, Hultcrantz R (2015) Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 61(5):1547–1554. https://doi.org/10.1002/hep.27368
Chang TT, Liaw YF, SS W, Schiff E, Han KH, Lai CL, Safadi R, Lee SS, Halota W, Goodman Z, Chi YC, Zhang H, Hindes R, Iloeje U, Beebe S, Kreter B (2010) Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B. Hepatology 52(3):886–893. https://doi.org/10.1002/hep.23785
Shiratori Y, Imazeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, Kuroki T, Nishiguchi S, Sata M, Yamada G, Fujiyama S, Yoshida H, Omata M (2000) Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med 132(7):517–524. https://doi.org/10.7326/0003-4819-132-7-200004040-00002
Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, Dixon JS, Gray DF, Sabbat J (2004) Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med 351(15):1521–1531. https://doi.org/10.1056/NEJMoa033364
Kerkar N, Yanni G (2016) ‘De novo’ and ‘recurrent’ autoimmune hepatitis after liver transplantation: a comprehensive review. J Autoimmun 66:17–24. https://doi.org/10.1016/j.jaut.2015.08.017
European Association for the Study of the Liver, Asociacion Latinoamericana para el Estudio del Higado (2015) EASL-ALEH clinical practice guidelines: non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol 63(1):237–264. https://doi.org/10.1016/j.jhep.2015.04.006
European Association for the Study of the Liver (2012) EASL clinical practice guidelines: management of chronic hepatitis B virus infection. J Hepatol 57(1):167–185. https://doi.org/10.1016/j.jhep.2012.02.010
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of D, European Association for the Study of O (2016) EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 64(6):1388–1402. https://doi.org/10.1016/j.jhep.2015.11.004
Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, Feng ZZ, Reddy KR, Schiff ER (2002) Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol 97(10):2614–2618. https://doi.org/10.1111/j.1572-0241.2002.06038.x
Bedossa P, Dargere D, Paradis V (2003) Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 38(6):1449–1457. https://doi.org/10.1016/j.hep.2003.09.022
Brunetti E, Silini E, Pistorio A, Cavallero A, Marangio A, Bruno R, Filice C (2004) Coarse vs. fine needle aspiration biopsy for the assessment of diffuse liver disease from hepatitis C virus-related chronic hepatitis. J Hepatol 40(3):501–506. https://doi.org/10.1016/j.jhep.2003.11.008
Rousselet MC, Michalak S, Dupre F, Croue A, Bedossa P, Saint-Andre JP, Cales P (2005) Sources of variability in histological scoring of chronic viral hepatitis. Hepatology 41(2):257–264. https://doi.org/10.1002/hep.20535
Bravo AA, Sheth SG, Chopra S (2001) Liver biopsy. N Engl J Med 344(7):495–500. https://doi.org/10.1056/nejm200102153440706
Tozzoli R, Villalta D, Bizzaro N (2016) Challenges in the standardization of autoantibody testing: a comprehensive review. Clin Rev Allergy Immunol 53(1):68–77. https://doi.org/10.1007/s12016-016-8579-y
Lieber CS, Weiss DG, Morgan TR, Paronetto F (2006) Aspartate aminotransferase to platelet ratio index in patients with alcoholic liver fibrosis. Am J Gastroenterol 101(7):1500–1508. https://doi.org/10.1111/j.1572-0241.2006.00610.x
Arena U, Vizzutti F, Corti G, Ambu S, Stasi C, Bresci S, Moscarella S, Boddi V, Petrarca A, Laffi G, Marra F, Pinzani M (2008) Acute viral hepatitis increases liver stiffness values measured by transient elastography. Hepatology 47(2):380–384. https://doi.org/10.1002/hep.22007
Coco B, Oliveri F, Maina AM, Ciccorossi P, Sacco R, Colombatto P, Bonino F, Brunetto MR (2007) Transient elastography: a new surrogate marker of liver fibrosis influenced by major changes of transaminases. J Viral Hepat 14(5):360–369. https://doi.org/10.1111/j.1365-2893.2006.00811.x
Nobili V, Vizzutti F, Arena U, Abraldes JG, Marra F, Pietrobattista A, Fruhwirth R, Marcellini M, Pinzani M (2008) Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 48(2):442–448. https://doi.org/10.1002/hep.22376
Millonig G, Reimann FM, Friedrich S, Fonouni H, Mehrabi A, Buchler MW, Seitz HK, Mueller S (2008) Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology 48(5):1718–1723. https://doi.org/10.1002/hep.22577
Trivedi PJ, Bruns T, Cheung A, Li KK, Kittler C, Kumagi T, Shah H, Corbett C, Al-Harthy N, Acarsu U, Coltescu C, Tripathi D, Stallmach A, Neuberger J, Janssen HL, Hirschfield GM (2014) Optimising risk stratification in primary biliary cirrhosis: AST/platelet ratio index predicts outcome independent of ursodeoxycholic acid response. J Hepatol 60(6):1249–1258. https://doi.org/10.1016/j.jhep.2014.01.029
Munro S (1998) Localization of proteins to the Golgi apparatus. Trends Cell Biol 8(1):11–15. https://doi.org/10.1016/S0962-8924(97)01197-5
Mao Y, Yang H, Xu H, Lu X, Sang X, Du S, Zhao H, Chen W, Xu Y, Chi T, Yang Z, Cai J, Li H, Chen J, Zhong S, Mohanti SR, Lopez-Soler R, Millis JM, Huang J, Zhang H (2010) Golgi protein 73 (GOLPH2) is a valuable serum marker for hepatocellular carcinoma. Gut 59(12):1687–1693. https://doi.org/10.1136/gut.2010.214916
Marrero JA, Romano PR, Nikolaeva O, Steel L, Mehta A, Fimmel CJ, Comunale MA, D’Amelio A, Lok AS, Block TM (2005) GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J Hepatol 43(6):1007–1012. https://doi.org/10.1016/j.jhep.2005.05.028
Hu JS, Wu DW, Liang S, Miao XY (2010) GP73, a resident Golgi glycoprotein, is sensibility and specificity for hepatocellular carcinoma of diagnosis in a hepatitis B-endemic Asian population. Med Oncol 27(2):339–345. https://doi.org/10.1007/s12032-009-9215-y
Li X, Wu K, Fan D (2009) Serum Golgi phosphoprotein 2 level: a better marker than alpha-fetoprotein for diagnosing early hepatocellular carcinoma. Hepatology 50(1):325. https://doi.org/10.1002/hep.23028
Wang Y, Yang H, Xu H, Lu X, Sang X, Zhong S, Huang J, Mao Y (2014) Golgi protein 73, not glypican-3, may be a tumor marker complementary to alpha-fetoprotein for hepatocellular carcinoma diagnosis. J Gastroenterol Hepatol 29(3):597–602. https://doi.org/10.1111/jgh.12461
Wang M, Long RE, Comunale MA, Junaidi O, Marrero J, Di Bisceglie AM, Block TM, Mehta AS (2009) Novel fucosylated biomarkers for the early detection of hepatocellular carcinoma. Cancer Epidemiol Biomark Prev 18(6):1914–1921. https://doi.org/10.1158/1055-9965.epi-08-0980
Hou SC, Xiao MB, Ni RZ, Ni WK, Jiang F, Li XY, Lu CH, Chen BY (2013) Serum GP73 is complementary to AFP and GGT-II for the diagnosis of hepatocellular carcinoma. Oncol Lett 6(4):1152–1158. https://doi.org/10.3892/ol.2013.1522
Morota K, Nakagawa M, Sekiya R, Hemken PM, Sokoll LJ, Elliott D, Chan DW, Dowell BL (2011) A comparative evaluation of Golgi protein-73, fucosylated hemopexin, alpha-fetoprotein, and PIVKA-II in the serum of patients with chronic hepatitis, cirrhosis, and hepatocellular carcinoma. Clin Chem Lab Med 49(4):711–718. https://doi.org/10.1515/CCLM.2011.097
Sangiovanni A, Prati GM, Fasani P, Ronchi G, Romeo R, Manini M, Del Ninno E, Morabito A, Colombo M (2006) The natural history of compensated cirrhosis due to hepatitis C virus: a 17-year cohort study of 214 patients. Hepatology 43(6):1303–1310. https://doi.org/10.1002/hep.21176
Ioannou GN, Splan MF, Weiss NS, McDonald GB, Beretta L, Lee SP (2007) Incidence and predictors of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol 5(8):938–945, 945.e931–934. https://doi.org/10.1016/j.cgh.2007.02.039
Lok AS, Seeff LB, Morgan TR, di Bisceglie AM, Sterling RK, Curto TM, Everson GT, Lindsay KL, Lee WM, Bonkovsky HL, Dienstag JL, Ghany MG, Morishima C, Goodman ZD (2009) Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology 136(1):138–148. https://doi.org/10.1053/j.gastro.2008.09.014
Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH, American Association for the Study of Liver D (2016) AASLD guidelines for treatment of chronic hepatitis B. Hepatology 63(1):261–283. https://doi.org/10.1002/hep.28156
AASLD/IDSA HCV Guidance Panel (2015) Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology 62(3):932–954. https://doi.org/10.1002/hep.27950
Hennes EM, Zeniya M, Czaja AJ, Pares A, Dalekos GN, Krawitt EL, Bittencourt PL, Porta G, Boberg KM, Hofer H, Bianchi FB, Shibata M, Schramm C, Eisenmann de Torres B, Galle PR, McFarlane I, Dienes HP, Lohse AW, International Autoimmune Hepatitis G (2008) Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 48(1):169–176. https://doi.org/10.1002/hep.22322
Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ, American Association for Study of Liver D (2009) Primary biliary cirrhosis. Hepatology 50(1):291–308. https://doi.org/10.1002/hep.22906
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24(2):289–293. https://doi.org/10.1002/hep.510240201
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR (1999) Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 94(9):2467–2474. https://doi.org/10.1111/j.1572-0241.1999.01377.x
Castera L, Forns X, Alberti A (2008) Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol 48(5):835–847. https://doi.org/10.1016/j.jhep.2008.02.008
Gong Y, Long Q, Xie H, Zhang T, Peng T (2012) Cloning and characterization of human Golgi phosphoprotein 2 gene (GOLPH2/GP73/GOLM1) promoter. Biochem Biophys Res Commun 421(4):713–720. https://doi.org/10.1016/j.bbrc.2012.04.067
Schmetterer KG, Neunkirchner A, Wojta-Stremayr D, Leitner J, Steinberger P, Pickl WF (2015) STAT3 governs hyporesponsiveness and granzyme B-dependent suppressive capacity in human CD4+ T cells. FASEB J 29(3):759–771. https://doi.org/10.1096/fj.14-257584
Bachert C, Fimmel C, Linstedt AD (2007) Endosomal trafficking and proprotein convertase cleavage of cis Golgi protein GP73 produces marker for hepatocellular carcinoma. Traffic 8(10):1415–1423. https://doi.org/10.1111/j.1600-0854.2007.00621.x
Kladney RD, Bulla GA, Guo L, Mason AL, Tollefson AE, Simon DJ, Koutoubi Z, Fimmel CJ (2000) GP73, a novel Golgi-localized protein upregulated by viral infection. Gene 249(1–2):53–65. https://doi.org/10.1016/S0378-1119(00)00136-0
Yamamoto K, Imamura H, Matsuyama Y, Kume Y, Ikeda H, Norman GL, Shums Z, Aoki T, Hasegawa K, Beck Y, Sugawara Y, Kokudo N (2010) AFP, AFP-L3, DCP, and GP73 as markers for monitoring treatment response and recurrence and as surrogate markers of clinicopathological variables of HCC. J Gastroenterol 45(12):1272–1282. https://doi.org/10.1007/s00535-010-0278-5
Shi Y, Chen J, Li L, Sun Z, Zen L, Xu S, Zhang Y, Zhang L (2011) A study of diagnostic value of Golgi protein GP73 and its genetic assay in primary hepatic carcinoma. Technol Cancer Res Treat 10(3):287–294. https://doi.org/10.7785/tcrt.2012.500205
Iftikhar R, Kladney RD, Havlioglu N, Schmitt-Graff A, Gusmirovic I, Solomon H, Luxon BA, Bacon BR, Fimmel CJ (2004) Disease- and cell-specific expression of GP73 in human liver disease. Am J Gastroenterol 99(6):1087–1095. https://doi.org/10.1111/j.1572-0241.2004.30572.x
Chen X, Wang Y, Tao J, Shi Y, Gai X, Huang F, Ma Q, Zhou Z, Chen H, Zhang H, Liu Z, Sun Q, Peng H, Chen R, Jing Y, Yang H, Mao Y, Zhang H (2015) mTORC1 up-regulates GP73 to promote proliferation and migration of hepatocellular carcinoma cells and growth of xenograft tumors in mice. Gastroenterology 149(3):741–752 e714. https://doi.org/10.1053/j.gastro.2015.05.005
Liu Y, Zhang X, Sun T, Jiang J, Li Y, Chen M, Wei Z, Jiang W, Zhou L (2016) Knockdown of Golgi phosphoprotein 2 inhibits hepatocellular carcinoma cell proliferation and motility. Oncotarget 7(16):21404–21415. 10.18632/oncotarget.7271
Wei H, Li B, Zhang R, Hao X, Huang Y, Qiao Y, Hou J, Li X, Li X (2013) Serum GP73, a marker for evaluating progression in patients with chronic HBV infections. PLoS One 8(2):e53862. https://doi.org/10.1371/journal.pone.0053862
Zhang YL, Zhang YC, Han W, Li YM, Wang GN, Yuan S, Wei FX, Wang JF, Jiang JJ, Zhang YW (2014) Effect of GP73 silencing on proliferation and apoptosis in hepatocellular cancer. World J Gastroenterol 20(32):11287–11296. https://doi.org/10.3748/wjg.v20.i32.11287
Zhao J, Xu T, Wang F, Cai W, Chen L (2017) miR-493-5p suppresses hepatocellular carcinoma cell proliferation through targeting GP73. Biomed Pharmacother 90:744–751. https://doi.org/10.1016/j.biopha.2017.04.029
Liu T, Yao M, Liu S, Wang L, Wang L, Hou J, Ma X, Jia J, Zhao J, Zhuang H, Lu F (2017) Serum Golgi protein 73 is not a suitable diagnostic marker for hepatocellular carcinoma. Oncotarget 8(10):16498–16506. https://doi.org/10.18632/oncotarget.14954
Li J, Gordon SC, Rupp LB, Zhang T, Boscarino JA, Vijayadeva V, Schmidt MA, Lu M (2014) The validity of serum markers for fibrosis staging in chronic hepatitis B and C. J Viral Hepat 21(12):930–937. https://doi.org/10.1111/jvh.12224
Xiao G, Yang J, Yan L (2015) Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: a systemic review and meta-analysis. Hepatology 61(1):292–302. https://doi.org/10.1002/hep.27382
Qiao Y, Chen J, Li X, Wei H, Xiao F, Chang L, Zhang R, Hao X, Wei H (2014) Serum gp73 is also a biomarker for diagnosing cirrhosis in population with chronic HBV infection. Clin Biochem 47(16–17):216–222. https://doi.org/10.1016/j.clinbiochem.2014.08.010
Fraquelli M, Rigamonti C, Casazza G, Donato MF, Ronchi G, Conte D, Rumi M, Lampertico P, Colombo M (2011) Etiology-related determinants of liver stiffness values in chronic viral hepatitis B or C. J Hepatol 54(4):621–628. https://doi.org/10.1016/j.jhep.2010.07.017
Czaja AJ (1984) Natural history, clinical features, and treatment of autoimmune hepatitis. Semin Liver Dis 4(1):1–12. https://doi.org/10.1055/s-2008-1040641
Liberal R, Krawitt EL, Vierling JM, Manns MP, Mieli-Vergani G, Vergani D (2016) Cutting edge issues in autoimmune hepatitis. J Autoimmun 75:6–19. https://doi.org/10.1016/j.jaut.2016.07.005
Ma WT, Chang C, Gershwin ME, Lian ZX (2017) Development of autoantibodies precedes clinical manifestations of autoimmune diseases: a comprehensive review. J Autoimmun 83:95–112. https://doi.org/10.1016/j.jaut.2017.07.003
Ye Q-H, Zhu W-W, Zhang J-B, Qin Y, Lu M, Lin G-L, Guo L, Zhang B, Lin Z-H, Roessler S, Forgues M, Jia H-L, Lu L, Zhang X-F, Lian B-F, Xie L, Dong Q-Z, Tang Z-Y, Wang XW, Qin L-X (2016) GOLM1 modulates EGFR/RTK cell-surface recycling to drive hepatocellular carcinoma metastasis. Cancer Cell 30(3):444–458. https://doi.org/10.1016/j.ccell.2016.07.017
Geier A, Jahn D, Hermanns H (2017) Interleukin-6—the dark side of liver regeneration in chronic liver disease. Hepatology 66(2):667–668. https://doi.org/10.1002/hep.29136
Lanton T, Shriki A, Nechemia-Arbely Y, Abramovitch R, Levkovitch O, Adar R, Rosenberg N, Paldor M, Goldenberg D, Sonnenblick A, Peled A, Rose-John S, Galun E, Axelrod JH (2017) Interleukin 6-dependent genomic instability heralds accelerated carcinogenesis following liver regeneration on a background of chronic hepatitis. Hepatology 65(5):1600–1611. https://doi.org/10.1002/hep.29004
Tachibana S, Zhang X, Ito K, Ota Y, Cameron AM, Williams GM, Sun Z (2014) Interleukin-6 is required for cell cycle arrest and activation of DNA repair enzymes after partial hepatectomy in mice. Cell Biosci 4(1):6. https://doi.org/10.1186/2045-3701-4-6
Xu MJ, Feng D, Wu H, Wang H, Chan Y, Kolls J, Borregaard N, Porse B, Berger T, Mak TW, Cowland JB, Kong X, Gao B (2015) Liver is the major source of elevated serum lipocalin-2 levels after bacterial infection or partial hepatectomy: a critical role for IL-6/STAT3. Hepatology 61(2):692–702. https://doi.org/10.1002/hep.27447
Liang H, Block TM, Wang M, Nefsky B, Long R, Hafner J, Mehta AS, Marrero J, Gish R, Norton PA (2012) Interleukin-6 and oncostatin M are elevated in liver disease in conjunction with candidate hepatocellular carcinoma biomarker GP73. Cancer Biomark 11(4):161–171. https://doi.org/10.3233/CBM-2012-00276
Taher TE, Bystrom J, Ong VH, Isenberg DA, Renaudineau Y, Abraham DJ, Mageed RA (2017) Intracellular B lymphocyte signalling and the regulation of humoral immunity and autoimmunity. Clin Rev Allergy Immunol 53(2):237–264. https://doi.org/10.1007/s12016-017-8609-4
Fujimura T, Fujimoto T, Itaya-Hironaka A, Miyaoka T, Yoshimoto K, Sakuramoto-Tsuchida S, Yamauchi A, Takeda M, Tsujinaka H, Tanaka Y, Takasawa S (2017) Significance of interleukin-6/STAT pathway for the gene expression of REG Ialpha, a new autoantigen in Sjogren’s syndrome patients, in salivary duct epithelial cells. Clin Rev Allergy Immunol 52(3):351–363. https://doi.org/10.1007/s12016-016-8570-7
Funding
This work was supported by the National S&T Major Project for Infectious Diseases (No. 2017ZX10302201 and 2017ZX10202203), the project from Beijing Municipal Science and Technology Commission (Z161100000116047 and D161100002716003), the National Natural Science Foundation of China Grant (No. 81372603, 81471938, 81325002 and 81620108002), the 111 Project (B07001), Research Fund of the Capital Medical Development (Grant No. 2014-2-5032) and the project from the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (code XMLX201606).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic Supplementary Material
Supplementary Figure 1
The serum levels of GP73 in different patient populations. HC: healthy controls; CLC: compensated cirrhosis; DLC: decompensated cirrhosis. ***p value < 0.001 based on differences between medians with the Mann–Whitney U test. (TIFF 96 kb)
Supplementary Figure 2
Immunohistochemistry of GP73 protein in different stages of fibrotic liver tissues (×400); CHB (a), AILDs (b) and NAFLD (c). (TIFF 9559 kb)
Supplementary Figure 3
Expression of GP73 can be induced by IL-6 and STAT3C. (a) Quantitative real-time PCR detection of mRNA level of GP73 and furin in huh7 cells after stimulation with 25 ng/mL IL-6 for 2 h. (b) Quantitative real-time PCR detection of mRNA of GP73 and furin in huh7 cells after transient-transfected STAT3C after 48 h. (c) Dual-luciferase assay in huh7 indicates that STAT3C activates the GP73 promoter. The experiments were repeated at least twice. (TIFF 178 kb)
Supplementary Table 1
(DOC 64 kb)
Supplementary Table 2
(DOC 57 kb)
Supplementary Table 3
(DOC 67 kb)
Rights and permissions
About this article
Cite this article
Yao, M., Wang, L., Leung, P.S.C. et al. The Clinical Significance of GP73 in Immunologically Mediated Chronic Liver Diseases: Experimental Data and Literature Review. Clinic Rev Allerg Immunol 54, 282–294 (2018). https://doi.org/10.1007/s12016-017-8655-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-017-8655-y