Abstract
Mesenchymal stem cells (MSCs) have demonstrated considerable potential in tissue repair and the treatment of immune-related diseases, but there are problems with homing efficiency during MSCs transplantation. Exercise, as an intervention, has been shown to have an important impact on the properties of MSCs. This review summarizes the effects of exercise on the properties (including proliferation, apoptosis, differentiation, and homing) of bone marrow-derived MSCs and adipose-derived MSCs. Studies indicated that exercise enhances bone marrow-derived MSCs proliferation, osteogenic differentiation, and homing while reducing adipogenic differentiation. For adipose-derived MSCs, exercise enhances proliferation and reduces adipogenic differentiation. In addition, studies have investigated the therapeutic effects of combined therapy of MSCs transplantation with exercise on diseases of the bone, cardiac, and nervous systems. The combined therapy improves tissue repair by increasing the homing of transplanted MSCs and cytokine secretion (such as neurotrophin 4). Furthermore, MSCs transplantation also has potential for the treatment of obesity. Although the effect is not significant in weight loss, MSCs transplantation shows effects in controlling blood glucose, improving dyslipidemia, reducing inflammation, and improving liver disease. Finally, the potential role of combined MSCs transplantation and exercise therapy in addressing obesity is discussed.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesenchymal stem cells (MSCs) are fibroblast-like cells that can be extracted from various tissues such as bone marrow, adipose tissue, and umbilical cord [1]. They possess the capacity to self-renew and differentiate into osteoblasts, adipocytes, or chondrocytes [1]. MSCs secrete proteins, cytokines, and microRNAs, which exert effects such as inflammation modulation and immune regulation [2]. Consequently, MSCs are utilized for tissue regeneration, wound healing, and treatment of various diseases (e.g., bone and nervous system disorders) [3]. However, MSCs transplantation as a means of treating diseases still faces numerous challenges and hurdles, including the low survival rate and the efficiency of homing [4]. Homing refers to the process of MSCs migrating to damaged tissue, and MSCs will exert therapeutic effects after successfully homing to the damaged tissue [5, 6]. However, it is reported that after MSCs are injected into mice with fracture, most of the MSCs will be trapped in the lungs and migrate to the fracture site after 8 – 9 days [7]. Although MSCs home to the fracture site, less than 3% of MSCs survive 5 weeks after the fracture [7]. Administering a higher dose of MSCs could potentially offset the observed low survival rates. Nonetheless, this approach is associated with high costs and an elevated risk of adverse effects. Therefore, it is necessary to investigate optimal strategies to enhance the therapeutic efficacy of MSCs injections.
Exercise is recognized as a means of altering the biological properties of MSCs, as it can enhance their proliferation and osteogenic differentiation while reducing adipogenic differentiation of MSCs cultured in vitro [8,9,10]. Some previous studies have also demonstrated that treatment combined with exercise is beneficial to enhance the therapeutic effects of MSCs in various diseases [11]. This may be related to the fact that exercise can activate MSCs to secrete immune regulatory factors that promote tissue repair, while exercise also improves homing efficiency [11,12,13]. For example, in neurological disorders such as spinal cord injury (SCI), the combined treatment of MSCs transplantation and exercise has demonstrated enhanced neuroprotective effects and maintenance of motor function [12]. These results may be attributed to the exercise-induced increase in neurotrophin 4 [12]. In the acute myocardial infarction model, the combined treatment preserved left ventricular function greater than a single treatment [13]. Exercise also activated the stromal cell-derived factor 1 (SDF-1)/ CXC chemokine receptor type 4 (CXCR4) axis, which may enhance MSCs homing [13].
In addition to neurological, musculoskeletal, and cardiovascular disorders, there is increasing evidence suggesting the therapeutic potential of MSCs transplantation in addressing metabolic-related diseases, such as obesity and type 2 diabetes mellitus (T2DM) [14]. MSCs transplantation has been shown to ameliorate dyslipidemia, regulate blood glucose levels, and reduce inflammation in animal models [15,16,17].
In this review, we focus on bone marrow-derived MSCs (BMSCs) and adipose-derived MSCs (ADMSCs) and summarize the effects of exercise on the properties of MSCs. We also summarize the combination effects of MSCs transplantation and exercise on diseases, and the therapeutic efficacy of MSCs transplantation for obesity. Additionally, will explore the role of exercise in the future of MSCs treatment for obesity.
Effects of Exercise on Bone Marrow-derived MSCs (BMSCs) and Adipose-Derived MSCs (ADMSCs)
In this review, animal and cell studies were included to investigate the effects of exercise on BMSCs and ADMSCs. The exercise protocol in animal studies comprised treadmill running (8 studies), climbing exercise (1 study), and low-magnitude mechanical signals (LMMS, 1 study). Cell experiments, on the other hand, use mechanical stress and irisin pretreatment to simulate the effects of exercise. The exercise protocol and main findings from the included studies are summarized in Table 1 and Fig. 1.
Effects of exercise on bone marrow-derived and adipose-derived mesenchymal stem cells properties. ADMSCs, adipose-derived mesenchymal stem cells; ALP, alkaline phosphatase; BMP2, bone morphogenetic protein 2; BMSCs, bone marrow-derived mesenchymal stem cells; C/EBPα, CCAAT/enhancer-binding protein alpha; OCN, osteocalcin; OPN, osteopontin; PPARγ, peroxisome proliferator-activated receptor gamma; Runx2, runt-related transcription factor 2 protein coding gene
Effects of Exercise on the Proliferation and Viability of BMSCs and ADMSCs
Exercise has been shown a tendency to enhance the proliferative capacity of BMSCs and ADMSCs. The number of colony-forming units (CFU) of BMSCs was higher in mice running on a treadmill for 5 weeks (21 ± 2) than in sedentary mice (16 ± 3) (p < 0.05) [8]. Additionally, an 8-week treadmill exercise protocol resulted in an increased number of CFU for both BMSCs and ADMSCs in rats [9]. Ocarino et al., reported that 12-week treadmill running increased the viability of BMSCs in ovariectomized rats [18]. A moderate-intensity treadmill running program increased the viability of BMSCs, while low- and high-intensity exercise did not induce significant change [10]. Except for treadmill running, 6-week of LMMS also increased the number of BMSCs in mice [19].
Conversely, some studies have indicated that exercise does not affect the proliferation or viability of MSCs. Baker et al., found a 29% increase in the number of CFU in bone marrow-isolated cells after 10 weeks of treadmill running, but this difference was not statistically significant [20]. It is important to note that in this study, the bone marrow-isolated cells were c-kit-positive and Sca-1-positive, indicating they may be hematopoietic stem cells rather than MSCs [20, 21]. Hell et al., adhered to the same exercise program as Ocarino et al., yet failed to observe an increase in the BMSCs' viability, which could be attributed to the utilization of a different animal model (normal vs. ostopenic) [18, 22]. Climbing a 100 cm meshed-wire tower, which is a different form of exercise than running, did not increase the number of CFU in mice BMSCs [23].
Exercise appears to enhance the proliferation and viability of MSCs. Yet the duration of exercise, which can vary from 4 to 10 weeks, and the type of exercise, such as treadmill running, LMMS, and climbing, can affect the benefits that are reported [8,9,10, 18,19,20, 22, 23].
Effects of Exercise on the Apoptosis of BMSCs and ADMSCs
Following the transplantation of MSCs, a high apoptotic rate has been observed, potentially diminishing the therapeutic efficacy of MSCs [7]. The effect of exercise on apoptosis of MSCs is not yet clear. BMSCs (passage 4) from rats that exercised on a treadmill were cultured in osteogenic differentiation medium for 21 days and the expression level of Casp3 mRNA was analyzed [22]. When comparing the BMSCs of the exercise group with age-matched control group, the exercise group demonstrated a significant upregulation of Casp3 mRNA expression (p < 0.05) [22]. De Lisio et al., reported that exercise preconditioning can reduce the MSCs apoptosis and increase the survival rate in an animal model subjected to radiation exposure [24].
Moreover, the anti-apoptotic capability of MSCs not only depends on exercise but may also be influenced by exerkines released during exercise. In a study by Yan et al., mice ADMSCs were pretreated with or without irisin (a myokine released by muscles during exercise, 100 ng/ml) for 48 h [25, 26]. The ADMSCs were then washed to remove irisin and exposed to H2O2 (200 µM, 6 h) [25]. To assess apoptosis, protein expression levels of cleaved caspase-3 and TdT‐mediated dUTP nick‐end labeling analysis were performed [25]. The findings indicate that irisin pretreated ADMSCs had a higher anti-apoptotic capacity, suggesting that exercise may affects the apoptosis of MSCs [25].
On the other hand, no significant differences were observed between BMSCs and ADMSCs in terms of the exercise-induced alterations in apoptosis. BMSCs and ADMSCs were isolated from both sedentary and exercised rats and cultured until 80% confluence [9]. Subsequently, the cells were exposed to a hypoxia and serum-deprived environment (serum-free Dulbecco's Modified Eagle Medium, chamber conditions with oxygen concentration of 3%) for 24 h [9]. To evaluate apoptosis, flow cytometry was used to compare the number of Annexin V+/propidium iodide- MSCs, while the activity of caspase-3 was assessed using a colorimetric assay [9]. The finding indicated no significant difference in the anti-apoptotic capability of BMSCs and ADMSCs from sedentary or exercise rats [9]. It was noted that BMSCs secreted more bone morphogenetic protein 2 under hypoxia and serum-deprived condition, which suggesting BMSCs isolated from exercised rats could be good source for bone repair applications [9].
Due to inconsistent findings in previous studies, the effects of exercise on MSCs apoptosis remain unclear. The effect of exercise on apoptosis seems to vary depending on the origin of MSCs [9, 25]. Future research needs to provide more evidence on the effect of exercise on MSCs apoptosis, and it is necessary to determine the role exercise plays in apoptosis during MSCs transplantation.
Effects of Exercise on the Differentiation Capacity of BMSCs and ADMSCs
Exercise is known to strengthen bones and reduce body fat [27, 28]. These changes are linked to exercise-induced changes in MSCs [29]. MSCs can differentiate into osteoblasts and adipocytes, contributing to bone and adipose tissue formation. Exercise influences this differentiation process.
Osteogenic Differentiation
Many studies proved that exercise increased the differentiation of BMSCs into osteoblasts [8,9,10, 18,19,20, 22, 23, 30,31,32,33]. BMSCs isolated from mice that trained on a treadmill for 10 weeks had higher levels of alkaline phosphatase (ALP), osteopontin, and osteocalcin compared to BMSCs from sedentary mice, showed more Alizarin Red S-positive BMSCs [8, 20]. Similarly, BMSCs isolated from rats subjected to treadmill running for 8 – 12 weeks show elevated levels of ALP activity and Alpl mRNA expression, as well as an increased number of mineralized nodules (at day 21 of osteogenic differentiation) compared to BMSCs from sedentary rats [9, 22]. However, there was no change in osteogenic differentiation of ADMSCs after exercise [9]. Following cell culture in osteogenic differentiation medium, the number of ALP+CFU was higher in BMSCs from trained mice than sedentary mice [32, 33]. In particular, moderate-intensity exercise was more effective than low- and high-intensity exercise in enhancing ALP+CFU [10, 32]. Even in an osteopenia model, exercise can also increase the osteogenic differentiation capacity of BMSCs [18]. Moreover, Mori et al., has demonstrated that climbing exercise can also enhance the osteogenic differentiation capacity of BMSCs [23].
The observed enhanced osteogenic differentiation capacity of MSCs might be related to exercise-induced mechanical signals that are transmitted to the extracellular matrix and initiate intracellular signaling cascades [34]. These mechanotransduction processes involve the activation of pathways such as p38 mitogen-activated protein kinase and WNT/β-catenin, through cell surface integrins, ultimately converting these mechanical stimuli into biochemical signals that promote osteogenic lineage commitment [34].
Previous studies have confirmed the change in osteogenic differentiation markers following exercise or mechanical stimuli. These studies showed that exercise enhances osteogenesis by increasing the osteogenic protein (runt-related transcription factor 2, Osterix) and osteogenesis-related genes (Runx2, Col1a1, Alpl and Bglap) [9, 10, 30, 31].
Adipogenic Differentiation
Some studies reported that exercise reduced the adipogenic differentiation capacity [8, 9, 19, 20, 31]. Maredziak et al., and Baker et al., (employing identical exercise protocol) reported that treadmill training for 10 weeks reduces the adipogenic differentiation capacity of mice BMSCs as measured by Oil Red O (exercise < sedentary) [8, 20]. Liu et al., found that an 8-week treadmill training can inhibit the adipogenic differentiation capacity of rats BMSCs and ADMSCs, and the gene expression levels of Pparg (peroxisome proliferator-activated receptor coding gene) and Cebpa (CCAAT/enhancer-binding protein alpha coding gene) in exercise group were lower than sedentary group [9].
The same results with animal studies were obtained in a cell culture study that mimicked exercise by applying mechanical stimulation to cells [31]. After 10 days of strain stimulation, rats BMSCs showed fewer Oil Red O-positive cells than the unstimulated group [31]. Moreover, the protein and mRNA expression of PPARγ and C/EBPα in the strain-stimulated group were lower than unstrained group [31]. PPARγ and C/EBPα proteins are known to be the key transcription factors in adipogenic differentiation of MSCs and play critical roles in adipogenesis [35]. Possibly due to the change in these adipogenic differentiation makers, MSCs reduced adipogenic differentiation.
In animal studies, LMMS (acting as an exercise mimic) alone inhibits the adipogenic lineage and promotes MSCs toward the osteogenic lineage [19]. This highlights that mechanical stimulation plays a role in the regulation of MSCs differentiation that occurs due to exercise.
Effects of Exercise on the Homing of BMSCs and ADMSCs
The migration of MSCs across vascular endothelial cells to target tissue (damaged site) is known as MSCs homing [6]. Since MSCs release cytokines at the site of damage, it is essential that injected MSCs have high homing efficiency to the damaged region. MSCs homing is facilitated by inflammation, hypoxia, and SDF-1/ CXCR4 axis activation [36, 37].
Exercise can also serve as a way to promote the homing of MSCs. Previous studies have demonstrated that performing aerobic exercise before surgical procedure-induced acute myocardial infarction can activate SDF-1/CXCR4 axis [13]. Treadmill exercise (10 weeks, 5 times/week, 60 min/time) increases the expression of inflammatory factors in heart tissue of female spontaneously hypertensive rats, thereby enhancing the regenerative capacity of ADMSCs and facilitating cardiac function recovery [13]. Furthermore, pretreatment of ADMSCs with irisin (100 ng/ml, 2 days) promoted their homing to the myocardium via CSF/CSF2RB axis in a model of ischemia–reperfusion injury [25]. This evidence suggests the potential for exercise to increase homing efficiency. However, conflicting results have been reported. De Lisio et al., showed that more MSCs did not homing to the bone marrow in mice exposed to radiation after aerobic exercise compared to sedentary mice [24].
Due to conflicting findings, a definitive association between exercise and MSCs homing has yet to be established. Future research may explore whether exercise influences MSCs homing through different pathways. In addition, previous studies have only investigated the effects of exercise preconditioning on the efficiency of injected MSCs homing, and little is known about the effects of exercise simultaneously or post-MSCs transplantation [13, 24, 25].
Summary of the Effects of Exercise on BMSCs and ADMSCs
Exercise improve proliferation, osteogenic differentiation and reduce adipogenic differentiation of MSCs and these effects may relate to exercise intensity. Moderate-intensity exercise may be optimal for enhancing the properties of MSCs [9, 10]. Exercise at low-intensity may fail to provide the necessary mechanical stimulus, while excessively high-intensity could potentially lead to bone tissue damage and cell death, thereby negating the beneficial effects on MSCs characteristics [10]. Most research has used exercise training protocols lasting 5 to 12 weeks, with a total of 30 to 60 sessions. Despite this, there remains a significant gap in understanding the impact of varying exercise durations and frequencies on MSCs. It is imperative to conduct additional studies to elucidate the optimal exercise regimen that can effectively enhance the properties and functionality of MSCs.
Therapeutic Effects of Combined Mesenchymal Stem Cells (MSCs) Transplantation and Exercise
Research on the combined MSCs transplantation and exercise had primarily focused on investigating their therapeutic effects on bone, heart tissue and nervous systems. The principal findings of studies examining the combined effects of MSCs transplantation are outlined in Table 2.
Bone Health
Exercise can enhance cartilage repair following BMSCs transplantation [38]. Osteochondral defects were induced through surgery in the center of the femoral groove of rats, and 4 weeks later, rats received injections of BMSCs (1 × 106 cells in 50 µL PBS) into the right knee and 50 µL PBS into the left knee. Two days post-injection, the exercise group started treadmill running for 2 to 8 weeks [38]. The combination of BMSCs transplantation and treadmill running led to improved cartilage repair scores, as observed in the second week [38]. Notably, the independent effects of BMSCs transplantation or exercise became apparent in the fourth week [38]. Moreover, the percent area stained with type II collagen was highest in the BMSCs transplantation and exercise combined group at week 4, but similar results were obtained at week 8 in the BMSCs transplantation group or exercise group [38]. This indicates that while the early combination of BMSCs transplantation and exercise has beneficial effects on cartilage repair, these effects may reduce over time [38].
Cardiac Disorders
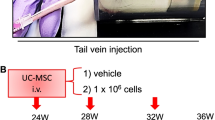
Exercise boosts the therapeutic effects of MSCs in myocardial infarction (MI) [39]. After inducing MI in rats, the combined therapy of BMSCs injection (1 × 106 cells/animal via tail vein) and a 12-week exercise program improved exercise capacity and cardiac function while reducing left ventricular collagen content [40]. A 5-week exercise program combined with BMSCs treatment also improved exercise capacity and left ventricular ejection fraction in MI mice [41]. In this study, the combined treatment increased the number of Ki67+ cells (a marker of proliferation) in the myocardial infarct area, supporting that exercise may enhance the retention of injected BMSCs in the heart and stimulate cardiomyocytes to enter the cell cycle [41]. Additionally, the study observed the effect of acute exercise on the therapeutic effect of BMSCs, revealing that injected BMSCs after acute exercise were retention in the infarcted area of the myocardium, which may be related to the activation of the SDF-1/CXCR4 axis by exercise, thereby enhancing the homing ability of MSCs [13, 41].
In addition to treadmill exercise, swimming has also been shown to enhance the therapeutic effects of MSCs, particularly when exercise preconditioning is performed [42, 43]. Prior to inducing MI in Fisher-344 rats, a 9-week swimming exercise program contributed to the preservation of ADMSCs in the myocardium and improved cardiac remodeling [42, 43]. Furthermore, the swimming and ADMSCs combined treatment showed synergy effects for MI treatment. This was attributed to exercise preconditioning, which fostered a pro-angiogenic and pro-inflammatory environment in the myocardial microenvironment [42, 43].
On the other hand, Lavorato et al., reported that BMSCs treatment restored the time-course of [Ca2+]i transient in cardiomyocytes, while exercise restored the contractile time-course and amplitude of [Ca2+]i transient in cardiomyocytes [44]. However, the therapeutic effects were not enhanced when combined with BMSCs and exercise [44].
Nervous System Disorders
SCI is a neurological disease in which damage to the spinal cord occurs due to external force [45]. MSCs transplantation has demonstrated efficacy in spinal cord repair, and exercise stans as the effective approach for improving motor function in individuals with SCI. Some studies have examined the effect of combining MSCs transplantation with exercise in SCI condition [12, 46].
In a study by Massoto et al., and his colleagues mice were transplanted with BMSCs (or culture medium as control) on the 7th day following surgery to induce SCI, and the exercise group performed treadmill running on the 14th day post-surgery [12]. In the combined therapy group (MSCs transplantation and exercise), the preserved white matter area and the level of myelinated fibers were higher than in the other treatment groups, and motor function was shown to be significantly improved [12]. Improvements in nerve regeneration ability and motor function through combined therapy are related to an increase in neurotrophin 4 level [12]. The immunomodulatory effect of MSCs and exercise are thought to release neurotrophin 4, which is known to promote nerve development [12, 47].
Similarly, in another study, after inducing SCI mice, followed by transplantation of BMSCs, treadmill running, or a combination of BMSCs transplantation and treadmill running [46]. After receiving BMSCs, the motor function improved following eight weeks of treadmill running [46]. Also, there was enhanced protection of axons and myelin, improved synaptic function, increased secretion of neurotrophic hormones, inhibited scar formation, and neuronal preservation [46]. Through in vitro experiments, the authors propose that the combination therapy of BMSCs transplantation and exercise enhances SCI recovery by activating the PI3K/AKT/mTOR pathway [46].
A combination of ADMSCs and exercise (wheel running) therapy has been reported to improve motor function recovery and mitigate SCI-induced hyperalgesia and hypoalgesia at the early stage of SCI recovery [48]. These effects may be related to the therapy-induced downregulation of lba1 and GFAP expression in the lumbar spinal cord dorsal horn [48].
In the sciatic nerve injury model, the combined therapy of swimming (30 min/day, 7 days) and MSCs transplantation shows different effects depending on water temperature [49, 50]. Sprague–Dawley rats received sciatic nerve transection surgery, and then BMSCs were transplanted, and swimming (30 °C) was started 12 h after surgery [49]. Combining transplantation of BMSCs with swimming can recover motor function as measured by sciatic function index, ankle activity, vertical locomotor activity, and electrophysiological studies [49]. However, these recoveries were greater than BMSCs transplantation alone but not greater than swimming alone [49]. Rats with a crush model of sciatic nerve injury underwent the same protocol (swimming and BMSCs) but the average water temperature was 16.5 °C [50]. In this study, the combination of BMSCs transplantation and cold-water swimming showed greater recovery effects on motor function than swimming alone or BMSCs transplantation alone [50].
The combined therapy of ADMSCs transplantation and exercise demonstrated a notable recovery in motor function in a Parkinson's disease (PD) model [51]. Following the induction of PD model in Wistar rats through 6-hydroxydopamine injection, and treadmill running exercise (16 m/min, 60 min/day, 5 days/week, 5 weeks) was performed, along with a single injection of ADMSCs [51]. Motor function was evaluated using the foot fault walking task, which showed a significantly higher total number of foot-slip in both untreated group and ADMSCs group compared to the sham, while there was no difference between exercise group and combined (exercise + ADMSCs) group compared to sham [51]. In other words, exercise can improve motor function in the PD model and can be considered an adjuvant intervention to treat PD with MSCs transplantation [51].
One study reported the effects of BMSCs and exercise combined therapy in Alzheimer's disease animal model. In this study, Alzheimer's disease was induced in Wistar rats using an intracerebroventricular injection of Amyloid-β [52]. Two weeks after the induction, treadmill exercise (25 m/min, 30 min/day, 4 days/week, 4 weeks) and BMSCs injections (1 × 106 cells/animal via tail vein) were performed [52]. The result showed that the combined therapy improved memory function, enhanced BMSCs migration and neurogenesis in the hippocampus, protected the pyramidal cells from apoptosis in hippocampus, and increased antioxidant capacity and serum level of brain-derived neurotrophic factor [52].
In summary, the combination of MSCs transplantation and exercise can effectively treat various diseases. Current research trends indicate that injecting MSCs into the site of injury is more common than intravenous injection. This could be attributed to the potential for intravenous injections to result in MSCs becoming trapped in the lungs instead of homing to the tissues requiring repair [5]. Furthermore, both forced exercises (treadmill running or swimming) and voluntary exercises (wheel running) significantly enhance the therapeutic effects of MSCs. Exercise preconditioning improves the microenvironment, which helps to increase the retention rate of MSCs, thereby enhancing their therapeutic effects [42, 43].
Nonetheless, to successfully apply these research findings to clinical practice, it is necessary to further investigate the mechanisms underlying MSCs and exercise combination therapy. This includes determining the best injection method, types of exercise, and optimal timing for exercise to achieve the best therapeutic outcomes.
MSCs and Obesity
Effects of Obesity on MSCs
Previous studies have demonstrated that obesity induces chronic inflammation, leading to an increase in the number of MSCs within adipose tissues while concurrently diminishing the migration and proliferation capacities of MSCs [53,54,55]. Treating BMSCs with tumor necrosis factor-α (TNF-α), an inflammatory factor highly expressed in obesity, increases CXCR4 expression and causes MSCs to migrate to adipose tissue [53]. When comparing ADMSCs from obese mice to those from lean mice, obese mice ADMSCs exhibited decreased proliferative capacity and diminished migratory ability [54]. Furthermore, the decreased proliferative capacity of ADMSCs due to obesity is associated with reduced telomerase activity, leading to genomic destabilization, telomere shortening, and cellular senescence [56, 57]. Additionally, the upregulation of cell cycle regulators such as p16, p21, and p53 mRNA expression in the obese state may induce apoptosis in ADMSCs [54, 55].
There is conflicting evidence in the studies on the effects of obesity on MSCs ability to differentiate into osteogenic and adipogenic lineages. Shu et al., reported that BMSCs isolated from 12-week diet-induced obesity (DIO) mice exhibited elevated expression levels of bone formation-related genes such as Runx2 (runt-related transcription factor 2), Sp7 (osterix), and Bglap (osteocalcin), as well as adipogenesis-related genes including Pparg, Cebpa, Cebpb, and Cebpd compared to the lean control group [58]. da Silva et al., reported that the protein expression levels of C/EBPα and PPARγ in BMSCs isolated from 10-week DIO mice were found to be higher compared to those in BMSCs isolated from lean mice [59]. This is probably attributed to the elevated levels of TNF-α in the bone marrow due to obesity, leading to an inflammatory bone marrow microenvironment that promotes adipogenic differentiation of BMSCs [59]. On the contrary, Wu et al., revealed that BMSCs produced from obese mice had lower osteogenic and adipogenic differentiation capacities than those derived from lean mice [60]. Also, authors found that obese mice had stronger osteogenic and adipogenic differentiation capacity in subcutaneous adipose-derived stem cells and infrapatellar fat pad-derived stem cells than lean mice [60].
Based on the findings of prior studies, it is conceivable that chronic inflammation induced by obesity impacts MSCs, and this influence may vary depending on the tissue of origin.
The Therapeutic Effects of MSCs Transplantation on Obesity
Numerous ongoing studies are dedicated to unraveling the potential of MSCs in ameliorating obesity and obesity-related complications. Most studies investigating the effects of MSCs transplantation on obesity used ADMSCs, and only some used BMSCs. A potential reason for the preference for ADMSCs versus BMSCs could be that the ADMSCs tend to secrete more insulin [61]. The main results of papers related to the effect of MSCs transplantation on obesity are summarized in Table 3.
The Impact of MSCs Transplantation on Body Weight and Body Composition
Weight loss is crucial for addressing obesity, but the effects of MSCs transplantation on DIO and T2DM animal models are inconsistent [15,16,17, 62,63,64,65,66,67,68,69,70,71,72,73,74,75]. Out of 17 studies investigating the impact of MSCs transplantation on body weight, 35% of the studies showed a reduction in body weight following the MSCs transplantation [17, 62,63,64,65,66], and 65% of the studies showed either no change in body weight or no superior effect compared to alternative treatments [15, 16, 67,68,69,70,71,72,73,74,75].
The impact of MSCs transplantation on body weight appears to be related to the injection method, injection times, and the genetic modification of MSCs. It seems that intraperitoneal injection (IP) is a more effective method for inducing weight loss. Specifically, administering IP injections two or more times can effectively reduce weight gain induced by a high-fat diet [17, 62, 63]. Moreover, genetically modified MSCs have been shown to effectively reduce high-fat diet-induced weight gain. Such as neuregulin 4-overexpressing human ADMSCs, metformin-pretreated human ADMSCs, and carnitine palmitoyltransferase 1A-expressing human ADMSCs, all of which have demonstrated the ability to induce weight loss [64,65,66].
Other studies have reported that MSCs transplantation improved body composition even without causing weight loss. Jaber et al., demonstrated that IP of human-ADMSCs in DIO mice reduced the percentage of fat mass, even though it did not lead to significant weight loss [15]. Domingues et al., reported that transplanting human-ADMSCs overexpressing Sod2 or Cat (catalase) into DIO mice reduced adipocyte area more effectively than null-human ADMSCs [68]. Additionally, Xie et al., observed a reduction in fat mass and an increase in lean mass two weeks after human-ADMSCs transplantation through tail vein injection in DIO mice [72]. Furthermore, ADMSCs transplantation resulted in decreased weight and adipocyte area in epididymal adipose tissue and inguinal subcutaneous adipose tissue [72]. Similar effects of ADMSCs injection were also observed in a DIO + streptozotocin-induced T2DM mouse model. Wang et al., reported that injecting ADMSCs from normal, T2DM, or db/db mice into T2DM mice effectively reduced adipocyte size [71].
MSCs-induced weight loss or improved body composition may be related to increased uncoupling protein-1 expression or M2 macrophage in white adipose tissue [68, 72]. Increased uncoupling protein-1 can induce heat release and enhance energy expenditure, while increased M2 macrophages have been shown to be effective in improving obesity [76, 77].
The Impact of MSCs Transplantation on Lipid Profile
MSCs transplantation seems to be effective in improving dyslipidemia. Obesity can result in the excessive accumulation of body fat, leading to dyslipidemia and an increased prevalence of cardiovascular diseases. Thus, it is important to focus on the prevention and management of dyslipidemia associated with obesity. Liu et al., transplanted human-ADMSCs into db/db mice and found that ADMSCs through activated adenosine monophosphate-activated protein kinase and hormone-sensitive lipase improved dyslipidemia and reduced weight [63]. Lee et al., transplanted human-ADMSCs into DIO mice, and the result showed that MSCs treatment improved lipid profile and liver fat accumulation, which means ADMSCs transplantation induced upregulation of Pparg and downregulation of Ppara in the liver, which is associated with increased fatty acid uptake and lipogenesis, as well as decreased triglyceride storage in the liver [17].
Daltro et al., observed that the total cholesterol levels decreased in the group that received BMSCs transplantation compared to levels before transplantation [75]. However, this reduction in cholesterol levels does not appear to be solely attributed to the effect of MSCs transplantation. Because the high-fat diet was withdrawn at the same time as MSCs transplantation [75].
The Impact of MSCs Transplantation on Blood Glucose and Insulin
The transition from obesity to T2DM occurs due to a gradual decline in insulin secretion accompanied by a gradual increase in insulin resistance and is also associated with glucose dysregulation [78]. Insulin sensitivity and disturbed blood glucose homeostasis in obesity and T2DM have been demonstrated to improve with MSCs transplantation [15,16,17, 62,63,64,65,66,67,68,69,70,71, 74, 79, 80]. The improvement in insulin sensitivity and fasting blood glucose levels can probably be ascribed to the protective effects on pancreatic β-cells [67]. Particularly, studies have demonstrated that ADMSCs transplantation increases pancreatic β-cells mass in both DIO mice and T2DM mice [67, 71]. This protects these cells from inflammation by reducing the mRNA expression of Tnf-α and Adgre1 [67, 71]. Moreover, the transplantation of MSCs decreases pro-inflammatory factors such as IL-6, IL-1β, and TNF-α, while concurrently increasing the levels of anti-inflammatory factors such as IL-10 [15,16,17, 62, 64,65,66,67,68,69,70,71,72,73,74].
The Impact of MSCs Transplantation on Liver
MSCs transplantation in obese animals also has notable effects on the liver [16, 17, 64, 67,68,69, 71, 73, 74, 80]. Studies have demonstrated that ADMSCs transplantation effectively reduced liver fat accumulation and triglyceride levels [16, 17, 67, 68], while also alleviating liver fibrosis and steatosis [17, 71, 73, 74].
Limitations of MSCs Transplantation on Obesity Treatment
The existing research findings suggest that MSCs transplantation, particularly ADMSCs, has a therapeutic effect on improving obesity and obesity complications. However, the protocols employed in the investigations (cell-derived tissue, number and frequency of injections, injection site, observation period after injection, etc.) are different, making it challenging to compare results between studies. Therefore, there is a need to establish an optimal protocol for the treatment of obesity in future investigations.
On the other hand, it is necessary to find ways to enhance the therapeutic potential of MSCs for obesity, as some studies have shown that transplanted MSCs exhibit lower survival and proliferation rates, which may reduce the effectiveness of obesity treatment [81]. Recently, genetic modification was used to enhance the therapeutic potential of MSCs. For example, before MSCs transplantation it was treated by Sod2 or Cat, to upregulate antioxidants, or neuregulin 4 (a factor that can regulate lipogenesis in the liver) was overexpressed in ADMSCs to improve insulin resistance and other obesity-related metabolic disorders [65, 68].
Side Effects and Adverse Events in MSCs Treatment
Several reviews have previously summarized the side effects and adverse events linked to MSCs transplantation [82, 83]. These reviews point out that although MSCs transplantation has shown great potential in several diseases, its application still carries various risks [82, 83]. The side effects and adverse events may include immune rejection, fever, and cancer.
Autologous or allogeneic MSCs can be used for MSCs treatment. Autologous MSCs has advantage in reducing the risk of immune rejection. However, the donor’s health state may exert an influence on the therapeutic efficacy of MSCs. For example, inflammation caused by obesity can lead to reduced proliferative capacity in MSCs [54]. Furthermore, MSCs isolated from T2DM patients exhibit enhanced characteristics such as apoptosis and autophagy, which may reduce their therapeutic efficacy [84]. Although MSCs lack major histocompatibility complex class II molecules, which makes them hypoimmunogenic and makes them commonly utilized in allogeneic MSCs treatment, some studies suggest that allogeneic MSCs treatment can still induce immune response [2]. Fever represents a commonly observed adverse event after MSCs treatment, potentially associated with immune response [82]. Therefore, it is necessary to consider some strategies to reduce the potential immune response.
To perform gene editing and expand a sufficient number for transplantation, MSCs in vitro culture are often used. However, with the increase in the number of cell divisions, the accumulation of mutations within the cells also increases, thereby elevating the risk of oncogenic mutations [85].
Although many studies have reported side effects associated with MSCs treatment, few studies on MSCs and exercise combined treatment have reported such side effects. Future research should focus on whether MSCs and exercise combined treatment may elicit any side effects.
Future Research
Exercise is known to be an effective approach for improving obesity, as it leads to reductions in body fat mass, improvements in insulin resistance, and alleviation of inflammation [28, 86, 87]. Under normal conditions, exercise has been shown to enhance the proliferation, differentiation, and migration of MSCs. However, it is also unknown whether exercise may have the potential to restore MSCs function impaired by inflammation under obese conditions. Furthermore, while weight loss through MSCs transplantation alone may be challenging, exercise has been demonstrated as an effective means to achieve this goal and enhance the quality of life in obese individuals [88]. Nonetheless, there remains a lack of research investigating the combined therapy of exercise and MSCs transplantation for improving obesity.
Conclusions
Exercise can impact the properties of MSCs through mechanical signaling. The improvement in proliferation, osteogenic differentiation, and homing of MSCs induced by exercise suggests potential for improving the homing efficiency of transplanted MSCs. However, conflicting research findings relate to various exercise protocols, origin tissue of MSCs, and cell culture protocols. More research is needed to determine the specific effects of exercise on MSCs, and for this purpose, experiments considering the differences between MSCs in vivo and in vitro should also be performed.
MSCs transplantation plays a pivotal role in treating bone, cardiac, and neurological disorders, and exercise serves as a factor to enhance that role. Exercise increased the homing efficiency of transplanted MSCs and promoted cytokine secretion, resulting in better therapeutic effects.
In obesity, the properties of MSCs change, leading to a propensity for adipose tissue differentiation. Despite these changes, MSCs transplantation has demonstrated efficacy in addressing obesity. Several studies have shown that improving blood glucose levels, dyslipidemia, insulin resistance, inflammation, and liver diseases without significant alterations in body weight. Exercise represents another approach that can help improve the quality of life of obese patients, improve body weight, blood glucose, and dyslipidemia, and perhaps also enhance the effectiveness of obesity treatment along with MSCs transplantation. In the future, it will be necessary to confirm the treatment effect more clearly on obesity by combining exercise and MSCs transplantation.
Data Availability
Not applicable.
References
Ding, D. C., Shyu, W. C., & Lin, S. Z. (2011). Mesenchymal stem cells. Cell Transplantation, 20(1), 5–14. https://doi.org/10.3727/096368910X
Nauta, A. J., & Fibbe, W. E. (2007). Immunomodulatory properties of mesenchymal stromal cells. Blood, The Journal of the American Society of Hematology, 110(10), 3499–3506. https://doi.org/10.1182/blood-2007-02-069716
Pittenger, M. F., Discher, D. E., Peault, B. M., Phinney, D. G., Hare, J. M., & Caplan, A. I. (2019). Mesenchymal stem cell perspective: Cell biology to clinical progress. NPJ regenerative medicine, 4, 22. https://doi.org/10.1038/s41536-019-0083-6
Jiang, Y. H., Zhang, P., Zhang, X., Lv, L. W., & Zhou, Y. S. (2021). Advances in mesenchymal stem cell transplantation for the treatment of osteoporosis. Cell Proliferation, 54(1). https://doi.org/10.1111/cpr.12956
Fischer, U. M., Harting, M. T., Jimenez, F., Monzon-Posadas, W. O., Xue, H., Savitz, S. I., Laine, G. A., & Cox, C. S., Jr. (2009). Pulmonary passage is a major obstacle for intravenous stem cell delivery: The pulmonary first-pass effect. Stem Cells and Development, 18(5), 683–692. https://doi.org/10.1089/scd.2008.0253
Karp, J. M., & Leng Teo, G. S. (2009). Mesenchymal stem cell homing: The devil is in the details. Cell Stem Cell, 4(3), 206–216. https://doi.org/10.1016/j.stem.2009.02.001
Huang, S., Xu, L., Sun, Y., Zhang, Y., & Li, G. (2015). The fate of systemically administrated allogeneic mesenchymal stem cells in mouse femoral fracture healing. Stem Cell Research & Therapy, 6, 206. https://doi.org/10.1186/s13287-015-0198-7
Maredziak, M., Smieszek, A., Chrzastek, K., Basinska, K., & Marycz, K. (2015). Physical Activity Increases the Total Number of Bone-Marrow-Derived Mesenchymal Stem Cells, Enhances Their Osteogenic Potential, and Inhibits Their Adipogenic Properties. Stem Cells Int, 2015, 379093. https://doi.org/10.1155/2015/379093
Liu, S. Y., He, Y. B., Deng, S. Y., Zhu, W. T., Xu, S. Y., & Ni, G. X. (2017). Exercise affects biological characteristics of mesenchymal stromal cells derived from bone marrow and adipose tissue. International Orthopaedics, 41(6), 1199–1209. https://doi.org/10.1007/s00264-017-3441-2
Liu, S. Y., Li, Z., Xu, S. Y., Xu, L., Yang, M., & Ni, G. X. (2018). Intensity-dependent effect of treadmill running on differentiation of rat bone marrow stromal cells. Molecular Medicine Reports, 17(6), 7746–7756. https://doi.org/10.3892/mmr.2018.8797
Bourzac, C., Bensidhoum, M., Pallu, S., & Portier, H. (2019). Use of adult mesenchymal stromal cells in tissue repair: Impact of physical exercise. American Journal of Physiology. Cell Physiology, 317(4), C642–C654. https://doi.org/10.1152/ajpcell.00530.2018
Massoto, T. B., Santos, A. C. R., Ramalho, B. S., Almeida, F. M., Martinez, A. M. B., & Marques, S. A. (2020). Mesenchymal stem cells and treadmill training enhance function and promote tissue preservation after spinal cord injury. Brain Research, 1726, 146494. https://doi.org/10.1016/j.brainres.2019.146494
Schaun, M. I., Kristochek, M., Dias, L. D., Peres, T. R., Lehnen, A. M., Irigoyen, M. C., & Markoski, M. M. (2020). Physical training prior to myocardial infarction potentializes stem cell therapy, SDF-1/CXCR4 axis activation and inhibits the vasoconstrictor response in hypertensive rats. Cytokine, 126, 154912. https://doi.org/10.1016/j.cyto.2019.154912
Miklosz, A., Nikitiuk, B. E., & Chabowski, A. (2022). Using adipose-derived mesenchymal stem cells to fight the metabolic complications of obesity: Where do we stand? Obesity Reviews, 23(5), e13413. https://doi.org/10.1111/obr.13413
Jaber, H., Issa, K., Eid, A., & Saleh, F. A. (2021). The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice. Scientific Reports, 11(1). https://doi.org/10.1038/s41598-021-85917-9
Shree, N., Venkategowda, S., Venkatranganna, M. V., Datta, I., & Bhonde, R. R. (2019). Human adipose tissue mesenchymal stem cells as a novel treatment modality for correcting obesity induced metabolic dysregulation. International Journal of Obesity, 43(10), 2107–2118. https://doi.org/10.1038/s41366-019-0438-5
Lee, C. W., Hsiao, W. T., & Lee, O. K. (2017). Mesenchymal stromal cell-based therapies reduce obesity and metabolic syndromes induced by a high-fat diet. Translational Research, 182(61–74), e68. https://doi.org/10.1016/j.trsl.2016.11.003
Ocarino, N. M., Boeloni, J. N., Goes, A. M., Silva, J. F., Marubayashi, U., & Serakides, R. (2008). Osteogenic differentiation of mesenchymal stem cells from osteopenic rats subjected to physical activity with and without nitric oxide synthase inhibition. Nitric Oxide, 19(4), 320–325. https://doi.org/10.1016/j.niox.2008.08.004
Luu, Y. K., Capilla, E., Rosen, C. J., Gilsanz, V., Pessin, J. E., Judex, S., & Rubin, C. T. (2009). Mechanical stimulation of mesenchymal stem cell proliferation and differentiation promotes osteogenesis while preventing dietary-induced obesity. Journal of Bone and Mineral Research, 24(1), 50–61. https://doi.org/10.1359/jbmr.080817
Baker, J. M., De Lisio, M., & Parise, G. (2011). Endurance exercise training promotes medullary hematopoiesis. FASEB Journal, 25(12), 4348–4357. https://doi.org/10.1096/fj.11-189043
Goldberg, L. R., Dooner, M. S., Papa, E., Pereira, M., Del Tatto, M., Cheng, Y., Wen, S., & Quesenberry, P. J. (2022). Differentiation Epitopes Define Hematopoietic Stem Cells and Change with Cell Cycle Passage. Stem Cell Rev Rep, 18(7), 2351–2364. https://doi.org/10.1007/s12015-022-10374-4
Hell, R. C., Ocarino, N. M., Boeloni, J. N., Silva, J. F., Goes, A. M., Santos, R. L., & Serakides, R. (2012). Physical activity improves age-related decline in the osteogenic potential of rats’ bone marrow-derived mesenchymal stem cells. Acta Physiologica, 205(2), 292–301. https://doi.org/10.1111/j.1748-1716.2011.02397.x
Mori, T., Okimoto, N., Sakai, A., Okazaki, Y., Nakura, N., Notomi, T., & Nakamura, T. (2003). Climbing exercise increases bone mass and trabecular bone turnover through transient regulation of marrow osteogenic and osteoclastogenic potentials in mice. Journal of Bone and Mineral Research, 18(11), 2002–2009. https://doi.org/10.1359/jbmr.2003.18.11.2002
De Lisio, M., Baker, J. M., & Parise, G. (2013). Exercise promotes bone marrow cell survival and recipient reconstitution post-bone marrow transplantation, which is associated with increased survival. Experimental Hematology, 41(2), 143–154. https://doi.org/10.1016/j.exphem.2012.10.003
Yan, W., Chen, Y., Guo, Y., Xia, Y., Li, C., Du, Y., Lin, C., Xu, X., Qi, T., Fan, M., Zhang, F., Hu, G., Gao, E., Liu, R., Hai, C., & Tao, L. (2022). Irisin Promotes Cardiac Homing of Intravenously Delivered MSCs and Protects against Ischemic Heart Injury. Advanced Science (Weinh), 9(7), e2103697. https://doi.org/10.1002/advs.202103697
Bostrom, P., Wu, J., Jedrychowski, M. P., Korde, A., Ye, L., Lo, J. C., Rasbach, K. A., Bostrom, E. A., Choi, J. H., Long, J. Z., Kajimura, S., Zingaretti, M. C., Vind, B. F., Tu, H., Cinti, S., Hojlund, K., Gygi, S. P., & Spiegelman, B. M. (2012). A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature, 481(7382), 463–468. https://doi.org/10.1038/nature10777
Guadalupe-Grau, A., Fuentes, T., Guerra, B., & Calbet, J. A. (2009). Exercise and bone mass in adults. Sports Medicine, 39(6), 439–468. https://doi.org/10.2165/00007256-200939060-00002
Bellicha, A., van Baak, M. A., Battista, F., Beaulieu, K., Blundell, J. E., Busetto, L., Carraca, E. V., Dicker, D., Encantado, J., Ermolao, A., Farpour-Lambert, N., Pramono, A., Woodward, E., & Oppert, J. M. (2021). Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: An overview of 12 systematic reviews and 149 studies. Obesity Reviews, 22 Suppl 4(Suppl 4)e13256. https://doi.org/10.1111/obr.13256
Chen, Q., Shou, P., Zheng, C., Jiang, M., Cao, G., Yang, Q., Cao, J., Xie, N., Velletri, T., Zhang, X., Xu, C., Zhang, L., Yang, H., Hou, J., Wang, Y., & Shi, Y. (2016). Fate decision of mesenchymal stem cells: Adipocytes or osteoblasts? Cell Death and Differentiation, 23(7), 1128–1139. https://doi.org/10.1038/cdd.2015.168
Huang, X., Zhu, Y., Sun, S., Gao, X., Yang, Y., Xu, H., Jin, A., Liu, Y., Jia, H., Dai, Q., & Jiang, L. (2023). Exercise maintains bone homeostasis by promoting osteogenesis through STAT3. International Journal of Biological Sciences, 19(7), 2021–2033. https://doi.org/10.7150/ijbs.82744
Li, R., Liang, L., Dou, Y., Huang, Z., Mo, H., Wang, Y., & Yu, B. (2015). Mechanical strain regulates osteogenic and adipogenic differentiation of bone marrow mesenchymal stem cells. BioMed Research International, 2015, 873251. https://doi.org/10.1155/2015/873251
Zhang, L., Chen, X., Wu, J., Yuan, Y., Guo, J., Biswas, S., Li, B., & Zou, J. (2017). The effects of different intensities of exercise and active vitamin D on mouse bone mass and bone strength. Journal of Bone and Mineral Metabolism, 35(3), 265–277. https://doi.org/10.1007/s00774-016-0764-9
Zhang, L., Yuan, Y., Wu, W., Sun, Z., Lei, L., Fan, J., Gao, B., & Zou, J. (2020). Medium-Intensity Treadmill Exercise Exerts Beneficial Effects on Bone Modeling Through Bone Marrow Mesenchymal Stromal Cells. Front Cell Dev Biol, 8, 600639. https://doi.org/10.3389/fcell.2020.600639
Chen, J., Zhou, R., Feng, Y., & Cheng, L. (2022). Molecular mechanisms of exercise contributing to tissue regeneration. Signal Transduction and Targeted Therapy, 7(1), 383. https://doi.org/10.1038/s41392-022-01233-2
Matsushita, K., & Dzau, V. J. (2017). Mesenchymal stem cells in obesity: Insights for translational applications. Laboratory Investigation, 97(10), 1158–1166. https://doi.org/10.1038/labinvest.2017.42
Lin, W., Xu, L., Zwingenberger, S., Gibon, E., Goodman, S. B., & Li, G. (2017). Mesenchymal stem cells homing to improve bone healing. Journal of Orthopaedic Translation, 9, 19–27. https://doi.org/10.1016/j.jot.2017.03.002
Wynn, R. F., Hart, C. A., Corradi-Perini, C., O’Neill, L., Evans, C. A., Wraith, J. E., Fairbairn, L. J., & Bellantuono, I. (2004). A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood, 104(9), 2643–2645. https://doi.org/10.1182/blood-2004-02-0526
Yamaguchi, S., Aoyama, T., Ito, A., Nagai, M., Iijima, H., Tajino, J., Zhang, X., Kiyan, W., & Kuroki, H. (2016). The Effect of Exercise on the Early Stages of Mesenchymal Stromal Cell-Induced Cartilage Repair in a Rat Osteochondral Defect Model. PLoS ONE, 11(3), e0151580. https://doi.org/10.1371/journal.pone.0151580
de Souza Vieira, S., de Melo, B. L., Dos Santos, L. F., Cummings, C. O., Tucci, P. J. F., & Serra, A. J. (2021). Exercise Training in Boosting Post-Mi Mesenchymal Stem Cell Therapy. Stem Cell Reviews and Reports, 17(6), 2361–2363. https://doi.org/10.1007/s12015-021-10274-z
de Freitas, J. S., Neves, C. A., Del Carlo, R. J., Belfort, F. G., Lavorato, V. N., Silame-Gomes, L. H. L., Ramos, R. M. S., Cunha, D., Okano, B. S., Pereira, V. G., de Oliveira, E. M., Carneiro-Junior, M. A., & Natali, A. J. (2019). Effects of exercise training and stem cell therapy on the left ventricle of infarcted rats. Revista Portuguesa de Cardiologia (English Edition), 38(9), 649–656. https://doi.org/10.1016/j.repc.2019.02.013
Chirico, E. N., Ding, D., Muthukumaran, G., Houser, S. R., Starosta, T., Mu, A., Margulies, K. B., & Libonati, J. R. (2015). Acute aerobic exercise increases exogenously infused bone marrow cell retention in the heart. Physiological Reports, 3(10). https://doi.org/10.14814/phy2.12566
de Souza Vieira, S., Antonio, E. L., de Melo, B. L., Portes, L. A., Montemor, J., Oliveira, H. A., Martins, F. L., Zogbi, C., Girardi, A. C., Silva, J. A., Jr., Camillo de Carvalho, P. T., Tucci, P. J. F., & Serra, A. J. (2019). Exercise Training Potentiates The Cardioprotective Effects of Stem Cells Post-infarction. Heart, Lung & Circulation, 28(2), 263–271. https://doi.org/10.1016/j.hlc.2017.11.005
Souza Vieira, S., Antonio, E. L., de Melo, B. L., Neves Dos Santos, L. F., Santana, E. T., Feliciano, R., Marques, F. L. N., de Paula Faria, D., Buchpiguel, C. A., Silva, J. A., Jr., Tucci, P. J. F., & Serra, A. J. (2020). Increased Myocardial Retention of Mesenchymal Stem Cells Post-MI by Pre-Conditioning Exercise Training. Stem Cell Reviews and Reports, 16(4), 730–741. https://doi.org/10.1007/s12015-020-09970-z
Lavorato, V. N., Del Carlo, R. J., da Cunha, D. N., Okano, B. S., Belfort, F. G., de Freitas, J. S., da Mota Gde, F., Quintao-Junior, J. F., Silame-Gomes, L. H., Drummond, F. R., Carneiro-Junior, M. A., de Oliveira, E. M., Monteiro, B. S., Primola-Gomes, T. N., & Natali, A. J. (2016). Mesenchymal stem cell therapy associated with endurance exercise training: Effects on the structural and functional remodeling of infarcted rat hearts. Journal of Molecular and Cellular Cardiology, 90, 111–119. https://doi.org/10.1016/j.yjmcc.2015.12.012
McDonald, J. W., & Sadowsky, C. (2002). Spinal-cord injury. Lancet, 359(9304), 417–425. https://doi.org/10.1016/S0140-6736(02)07603-1
Sun, X., Huang, L. Y., Pan, H. X., Li, L. J., Wang, L., Pei, G. Q., Wang, Y., Zhang, Q., Cheng, H. X., He, C. Q., & Wei, Q. (2023). Bone marrow mesenchymal stem cells and exercise restore motor function following spinal cord injury by activating PI3K/AKT/mTOR pathway. Neural Regeneration Research, 18(5), 1067–1075. https://doi.org/10.4103/1673-5374.355762
Cobianchi, S., Arbat-Plana, A., Lopez-Alvarez, V. M., & Navarro, X. (2017). Neuroprotective Effects of Exercise Treatments After Injury: The Dual Role of Neurotrophic Factors. Current Neuropharmacology, 15(4), 495–518. https://doi.org/10.2174/1570159X14666160330105132
Cheng, X., Mao, G. P., Hu, W. J., Yu, Z. R., Xu, Y. Y., Chen, W., Li, X., Zeng, X. L., Zhang, W. W., Chen, J. W., Wan, Y., & Wang, L. (2023). Exercise combined with administration of adipose-derived stem cells ameliorates neuropathic pain after spinal cord injury. Neural Regeneration Research, 18(8), 1841–1846. https://doi.org/10.4103/1673-5374.361533
Wang, J., Yang, C. C., Chen, S. C., & Hsieh, Y. L. (2010). No synergistic effect of mesenchymal stem cells and exercise on functional recovery following sciatic nerve transection. Functional Neurology, 25(1), 33–43. https://www.ncbi.nlm.nih.gov/pubmed/20626995.
Yang, C. C., Wang, J., Chen, S. C., Jan, Y. M., & Hsieh, Y. L. (2015). Enhanced functional recovery from sciatic nerve crush injury through a combined treatment of cold-water swimming and mesenchymal stem cell transplantation. Neurological Research, 37(9), 816–826. https://doi.org/10.1179/1743132815Y.0000000060
Cucarian, J. D., Berrio, J. P., Rodrigues, C., Zancan, M., Wink, M. R., & de Oliveira, A. (2019). Physical exercise and human adipose-derived mesenchymal stem cells ameliorate motor disturbances in a male rat model of Parkinson’s disease. Journal of Neuroscience Research, 97(9), 1095–1109. https://doi.org/10.1002/jnr.24442
Abshenas, R., Artimani, T., Shahidi, S., Ranjbar, A., Komaki, A., Salehi, I., Amiri, I., & Soleimani Asl, S. (2020). Treadmill exercise enhances the promoting effects of preconditioned stem cells on memory and neurogenesis in Abeta-induced neurotoxicity in the rats. Life Sciences, 249, 117482. https://doi.org/10.1016/j.lfs.2020.117482
de Assis-Ferreira, A., Saldanha-Gama, R., de Brito, N. M., Renovato-Martins, M., Simoes, R. L., Barja-Fidalgo, C., & Vargas da Silva, S. (2021). Obesity enhances the recruitment of mesenchymal stem cells to visceral adipose tissue. Journal of Molecular Endocrinology, 67(1), 15–26. https://doi.org/10.1530/JME-20-0229
Perez, L. M., Bernal, A., de Lucas, B., San Martin, N., Mastrangelo, A., Garcia, A., Barbas, C., & Galvez, B. G. (2015). Altered metabolic and stemness capacity of adipose tissue-derived stem cells from obese mouse and human. PLoS ONE, 10(4), e0123397. https://doi.org/10.1371/journal.pone.0123397
Pham, D. V., Nguyen, T. K., & Park, P. H. (2023). Adipokines at the crossroads of obesity and mesenchymal stem cell therapy. Experimental & Molecular Medicine, 55(2), 313–324. https://doi.org/10.1038/s12276-023-00940-2
Siraj, Y., Galderisi, U., & Alessio, N. (2023). Senescence induces fundamental changes in the secretome of mesenchymal stromal cells (MSCs): Implications for the therapeutic use of MSCs and their derivates. Front Bioeng Biotechnol, 11, 1148761. https://doi.org/10.3389/fbioe.2023.1148761
Lyamina, S., Baranovskii, D., Kozhevnikova, E., Ivanova, T., Kalish, S., Sadekov, T., Klabukov, I., Maev, I., & Govorun, V. (2023). Mesenchymal Stromal Cells as a Driver of Inflammaging. International Journal of Molecular Sciences, 24(7). https://doi.org/10.3390/ijms24076372
Shu, L., Beier, E., Sheu, T., Zhang, H., Zuscik, M. J., Puzas, E. J., Boyce, B. F., Mooney, R. A., & Xing, L. (2015). High-fat diet causes bone loss in young mice by promoting osteoclastogenesis through alteration of the bone marrow environment. Calcified Tissue International, 96(4), 313–323. https://doi.org/10.1007/s00223-015-9954-z
da Silva, S. V., Renovato-Martins, M., Ribeiro-Pereira, C., Citelli, M., & Barja-Fidalgo, C. (2016). Obesity modifies bone marrow microenvironment and directs bone marrow mesenchymal cells to adipogenesis. Obesity (Silver Spring), 24(12), 2522–2532. https://doi.org/10.1002/oby.21660
Wu, C. L., Diekman, B. O., Jain, D., & Guilak, F. (2013). Diet-induced obesity alters the differentiation potential of stem cells isolated from bone marrow, adipose tissue and infrapatellar fat pad: The effects of free fatty acids. International Journal of Obesity, 37(8), 1079–1087. https://doi.org/10.1038/ijo.2012.171
Karaoz, E., Okcu, A., Unal, Z. S., Subasi, C., Saglam, O., & Duruksu, G. (2013). Adipose tissue-derived mesenchymal stromal cells efficiently differentiate into insulin-producing cells in pancreatic islet microenvironment both in vitro and in vivo. Cytotherapy, 15(5), 557–570. https://doi.org/10.1016/j.jcyt.2013.01.005
Ji, A. T., Chang, Y. C., Fu, Y. J., Lee, O. K., & Ho, J. H. (2015). Niche-dependent regulations of metabolic balance in high-fat diet-induced diabetic mice by mesenchymal stromal cells. Diabetes, 64(3), 926–936. https://doi.org/10.2337/db14-1042
Liu, G. Y., Liu, J., Wang, Y. L., Liu, Y., Shao, Y., Han, Y., Qin, Y. R., Xiao, F. J., Li, P. F., Zhao, L. J., Gu, E. Y., Chen, S. Y., Gao, L. H., Wu, C. T., Hu, X. W., & Duan, H. F. (2016). Adipose-Derived Mesenchymal Stem Cells Ameliorate Lipid Metabolic Disturbance in Mice. Stem Cells Translational Medicine, 5(9), 1162–1170. https://doi.org/10.5966/sctm.2015-0239
Shree, N., & Bhonde, R. R. (2016). Metformin preconditioned adipose derived mesenchymal stem cells is a better option for the reversal of diabetes upon transplantation. Biomedicine & Pharmacotherapy, 84, 1662–1667. https://doi.org/10.1016/j.biopha.2016.10.086
Wang, W., Zhang, Y., Yang, C., Wang, Y., Shen, J., Shi, M., & Wang, B. (2019). Transplantation of neuregulin 4-overexpressing adipose-derived mesenchymal stem cells ameliorates insulin resistance by attenuating hepatic steatosis. Experimental Biology and Medicine (Maywood), 244(7), 565–578. https://doi.org/10.1177/1535370219839643
Soler-Vazquez, M. C., Romero, M. D. M., Todorcevic, M., Delgado, K., Calatayud, C., Benitez-Amaro, A., La Chica Lhoest, M. T., Mera, P., Zagmutt, S., Bastias-Perez, M., Ibeas, K., Casals, N., Escola-Gil, J. C., Llorente-Cortes, V., Consiglio, A., Serra, D., & Herrero, L. (2023). Implantation of CPT1AM-expressing adipocytes reduces obesity and glucose intolerance in mice. Metabolic Engineering, 77, 256–272. https://doi.org/10.1016/j.ymben.2023.04.010
Cao, M., Pan, Q., Dong, H., Yuan, X., Li, Y., Sun, Z., Dong, X., & Wang, H. (2015). Adipose-derived mesenchymal stem cells improve glucose homeostasis in high-fat diet-induced obese mice. Stem Cell Research & Therapy, 6, 208. https://doi.org/10.1186/s13287-015-0201-3
Domingues, C. C., Kundu, N., Kropotova, Y., Ahmadi, N., & Sen, S. (2019). Antioxidant-upregulated mesenchymal stem cells reduce inflammation and improve fatty liver disease in diet-induced obesity. Stem Cell Research & Therapy, 10(1), 280. https://doi.org/10.1186/s13287-019-1393-8
Hu, J., Fu, Z., Chen, Y., Tang, N., Wang, L., Wang, F., Sun, R., & Yan, S. (2015). Effects of autologous adipose-derived stem cell infusion on type 2 diabetic rats. Endocrine Journal, 62(4), 339–352. https://doi.org/10.1507/endocrj.EJ14-0584
Ishida, M., Tatsumi, K., Okumoto, K., & Kaji, H. (2020). Adipose Tissue-Derived Stem Cell Sheet Improves Glucose Metabolism in Obese Mice. Stem Cells and Development, 29(8), 488–497. https://doi.org/10.1089/scd.2019.0250
Wang, M., Song, L., Strange, C., Dong, X., & Wang, H. (2018). Therapeutic Effects of Adipose Stem Cells from Diabetic Mice for the Treatment of Type 2 Diabetes. Molecular Therapy, 26(8), 1921–1930. https://doi.org/10.1016/j.ymthe.2018.06.013
Xie, Z., Cheng, Y., Zhang, Q., Hao, H., Yin, Y., Zang, L., Wang, X., & Mu, Y. (2021). Anti-obesity effect and mechanism of mesenchymal stem cells influence on obese mice. Open Life Sci, 16(1), 653–666. https://doi.org/10.1515/biol-2021-0061
Yamato, M., Sakai, Y., Mochida, H., Kawaguchi, K., Takamura, M., Usui, S., Seki, A., Mizukoshi, E., Yamashita, T., Yamashita, T., Ishida, K., Nasti, A., Tuyen, H. T. B., Komura, T., Yoshida, K., Wada, T., Honda, M., & Kaneko, S. (2019). Adipose tissue-derived stem cells prevent fibrosis in murine steatohepatitis by suppressing IL-17-mediated inflammation. Journal of Gastroenterology and Hepatology, 34(8), 1432–1440. https://doi.org/10.1111/jgh.14647
Yu, S., Cheng, Y., Zhang, L., Yin, Y., Xue, J., Li, B., Gong, Z., Gao, J., & Mu, Y. (2019). Treatment with adipose tissue-derived mesenchymal stem cells exerts anti-diabetic effects, improves long-term complications, and attenuates inflammation in type 2 diabetic rats. Stem Cell Research & Therapy, 10(1), 333. https://doi.org/10.1186/s13287-019-1474-8
Daltro, P. S., Barreto, B. C., Silva, P. G., Neto, P. C., Sousa Filho, P. H. F., Santana Neta, D., Carvalho, G. B., Silva, D. N., Paredes, B. D., de Alcantara, A. C., Freitas, L. A. R., Couto, R. D., Santos, R. R., Souza, B. S. F., Soares, M. B. P., & Macambira, S. G. (2017). Therapy with mesenchymal stromal cells or conditioned medium reverse cardiac alterations in a high-fat diet-induced obesity model. Cytotherapy, 19(10), 1176–1188. https://doi.org/10.1016/j.jcyt.2017.07.002
Baek, K. W., Lee, D. I., Kang, S. A., & Yu, H. S. (2020). Differences in macrophage polarization in the adipose tissue of obese mice under various levels of exercise intensity. Journal of Physiology and Biochemistry, 76(1), 159–168. https://doi.org/10.1007/s13105-020-00731-7
Poher, A. L., Veyrat-Durebex, C., Altirriba, J., Montet, X., Colin, D. J., Caillon, A., Lyautey, J., & Rohner-Jeanrenaud, F. (2015). Ectopic UCP1 Overexpression in White Adipose Tissue Improves Insulin Sensitivity in Lou/C Rats, a Model of Obesity Resistance. Diabetes, 64(11), 3700–3712. https://doi.org/10.2337/db15-0210
Golay, A., & Ybarra, J. (2005). Link between obesity and type 2 diabetes. Best Practice and Research Clinical Endocrinology and Metabolism, 19(4), 649–663. https://doi.org/10.1016/j.beem.2005.07.010
Hao, H., Liu, J., Shen, J., Zhao, Y., Liu, H., Hou, Q., Tong, C., Ti, D., Dong, L., Cheng, Y., Mu, Y., Liu, J., Fu, X., & Han, W. (2013). Multiple intravenous infusions of bone marrow mesenchymal stem cells reverse hyperglycemia in experimental type 2 diabetes rats. Biochemical and Biophysical Research Communications, 436(3), 418–423. https://doi.org/10.1016/j.bbrc.2013.05.117
Xie, M., Hao, H. J., Cheng, Y., Xie, Z. Y., Yin, Y. Q., Zhang, Q., Gao, J. Q., Liu, H. Y., Mu, Y. M., & Han, W. D. (2017). Adipose-derived mesenchymal stem cells ameliorate hyperglycemia through regulating hepatic glucose metabolism in type 2 diabetic rats. Biochemical and Biophysical Research Communications, 483(1), 435–441. https://doi.org/10.1016/j.bbrc.2016.12.125
Preda, M. B., Neculachi, C. A., Fenyo, I. M., Vacaru, A. M., Publik, M. A., Simionescu, M., & Burlacu, A. (2021). Short lifespan of syngeneic transplanted MSC is a consequence of in vivo apoptosis and immune cell recruitment in mice. Cell Death and Disease, 12(6), 566. https://doi.org/10.1038/s41419-021-03839-w
Wang, Y., Yi, H., & Song, Y. (2021). The safety of MSC therapy over the past 15 years: A meta-analysis. Stem Cell Research & Therapy, 12(1), 545. https://doi.org/10.1186/s13287-021-02609-x
Baranovskii, D. S., Klabukov, I. D., Arguchinskaya, N. V., Yakimova, A. O., Kisel, A. A., Yatsenko, E. M., Ivanov, S. A., Shegay, P. V., & Kaprin, A. D. (2022). Adverse events, side effects and complications in mesenchymal stromal cell-based therapies. Stem Cell Investigation, 9, 7. https://doi.org/10.21037/sci-2022-025
Kornicka, K., Houston, J., & Marycz, K. (2018). Dysfunction of Mesenchymal Stem Cells Isolated from Metabolic Syndrome and Type 2 Diabetic Patients as Result of Oxidative Stress and Autophagy may Limit Their Potential Therapeutic Use. Stem Cell Rev Rep, 14(3), 337–345. https://doi.org/10.1007/s12015-018-9809-x
Derks, L. L. M., & van Boxtel, R. (2023). Stem cell mutations, associated cancer risk, and consequences for regenerative medicine. Cell Stem Cell, 30(11), 1421–1433. https://doi.org/10.1016/j.stem.2023.09.008
Way, K. L., Hackett, D. A., Baker, M. K., & Johnson, N. A. (2016). The Effect of Regular Exercise on Insulin Sensitivity in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Diabetes and Metabolism Journal, 40(4), 253–271. https://doi.org/10.4093/dmj.2016.40.4.253
You, T., Arsenis, N. C., Disanzo, B. L., & Lamonte, M. J. (2013). Effects of exercise training on chronic inflammation in obesity : Current evidence and potential mechanisms. Sports Medicine, 43(4), 243–256. https://doi.org/10.1007/s40279-013-0023-3
Stephenson, J., Smith, C. M., Kearns, B., Haywood, A., & Bissell, P. (2021). The association between obesity and quality of life: A retrospective analysis of a large-scale population-based cohort study. BMC Public Health, 21(1), 1990. https://doi.org/10.1186/s12889-021-12009-8
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant number: 2021R1I1A1A01044495).
Author information
Authors and Affiliations
Contributions
YYX wrote the original draft and prepared the figure and table; JHW provided assistance with the writing and prepared the figure and table; SJL provided assistance with the writing; KWB revised and proofread the original draft; All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiang, YY., Won, JH., Lee, SJ. et al. The Effect of Exercise on Mesenchymal Stem Cells and their Application in Obesity Treatment. Stem Cell Rev and Rep (2024). https://doi.org/10.1007/s12015-024-10755-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s12015-024-10755-x