Abstract
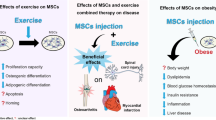
Stem cell (SC) therapy is a promising approach to improve post-myocardial infarction (MI) cardiac remodeling, but the proinflammatory microenvironment may lead to SC loss and, therefore, may have a negative impact on therapy. It appears that exercise training (ET) improves myocardial microenvironment for SC transplantation. Therefore, we tested the effect of ET on post-infarction retention of adipose-derived SCs (ADSCs) and its combined effects on the inflammatory microenvironment. Fischer-344 female rats were randomized to one of the following groups: Sham; sedentary coronary occlusion who did not receive ADSCs (sMI); sedentary coronary occlusion who received ADSCs; exercise coronary occlusion who received ADSCs. Rats were trained nine weeks prior to MI, followed by ADSCs transplantation. The MI led to left ventricle (LV) dilation and dysfunction, myocardial hypertrophy and fibrosis, and increased proinflammatory profile compared to Sham rats. Conversely, ADSCs transplanted rats exhibited, better morphological and functional LV parameters; inhibition of myocardial hypertrophy and fibrosis; and attenuation of proinflammatory cytokines (interleukins 1β and 10, tumor necrosis factor α, and transforming growth factor β) in the myocardium compared to sMI rats. Interestingly, ET enhanced the effect of ADSCs on interleukin 10 expression. There was a correlation between cytokine expression and myocardial ADSCs retention. The. ET enhanced the beneficial effects of ADSCs in infarcted myocardium, which was associated with higher ADSCs retention. These findings highlight the importance of ET in myocardial retention of ADSCs and attenuation of cardiac remodeling post-infarction. Cytokine analysis suggests improvement in ET-linked myocardial microenvironment based on its anti-inflammatory action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stem cells (SC) therapy holds significant promise to improve post-myocardial infarction (MI) cardiac remodeling [1]. SC can be isolated from several sources, including the bone marrow, umbilical cord, blood, dental pulp, skeletal muscle, skin, and adipose tissue [2]. Adipose-derived stem cells (ADSCs) have become one of the most promising stem cell populations because they can be easily harvested in large quantities and adipose tissue is relatively abundant [2, 3]. Furthermore, studies have shown the ability of ADSCs to engraft and differentiate into several types of cells, and to secrete a wide range of beneficial factors [4, 5].
Unfortunately, many factors lead to poor SC survival and retention, including cell death, limited self-renewal in hypoxic microenvironments, being pushed outwards from injection sites as a result of compressive mechanical strain in the heart, and oxidative stress [6,7,8,9,10,11]. Moreover, there is consensus that pro-inflammatory cytokines present at injury sites decrease SC survival [12,13,14]. Thus, optimized retention of SC allows sufficient time to release cell-derived bioactive factors and may be directly related to long-term beneficial therapeutic outcomes [15]. A direct association has been shown between higher myocardial homing of injected cells and improvements in cardiac performance [16,17,18].
The limitations stated above emphasize the need for approaches that improve the host myocardium before SC transplantation, thereby increasing cellular retention and efficacy in attenuating cardiac remodeling [19, 20]. Previous studies have shown that exercise training (ET) may promote a favorable microenvironment for SC. We recently showed that chronic ET prior to MI enhanced the beneficial effects of ADSCs on left ventricular (LV) dilation, myocardial performance, and capillary density [21]. In a small nontransmural MI model, Chirico et al. [22] showed that a single treadmill exercise session prior to transplantation increased GFP+ bone marrow-derived cells in the infarcted zone in mice. While the results of this study have not been associated with alterations in LV function, it is possible that an ET program could increase the retention of exogenously infused ADSCs in the myocardium, which could partially contribute to our previous results [21]. Therefore, it should be determined whether ET prior to MI has any effect on ADSC retention.
The purpose of the present study was to evaluate whether chronic ET prior to MI may improve retention of ADSCs as well as post-infarction cardiac remodeling in rats. Considering that ET is closely associated with an anti-inflammatory effect [23, 24], we hypothesized that a higher ADSC retention could be associated with an improved myocardial inflammatory profile. This issue is important because the local inflammatory milieu affects both the survival of ADSCs and the adverse remodeling of the myocardium [9].
Materials and Methods
Animal Care
Experiments were performed according to the Guide for the Care and Use of Laboratory Animals’ prepared by the Institute of Laboratory Animal Resources and published by the National Institutes of Health (NIH Publication No. 86 − 23, revised 1996). Animal ethics protocol was approved by the Institutional Research Ethics Committee of the Federal University of São Paulo (number: 2130010214) and investigation was performed in agreement with the ARRIVE guidelines. In vivo and ex vivo experiments were performed under ketamine (50 mg/kg) and xylazine (10 mg/kg) mixture (KX) or isoflurane (3%, at 2 L/min O2 flow) anesthesia, and efforts were made to minimize discomfort to animals. Animal`s hearts were removed following rapid decapitation.
Animal Experiments
Fisher-344 female rats (140–180 g) were assigned to one of the following experimental groups: Sham (n = 28); sMI, non-trained rats subjected to MI (n = 31); sADSC, non-trained rats subjected to MI and ADSC (n = 34); tADSC, trained rats subjected to MI and ADSC (n = 32). Experimental design is illustrated in the Fig. 1 (see electronic supplementary material).
ET Protocol
The 9-week ET protocol included a 90-minute swimming session a day, five days a week. The rats were preconditioned to swim six consecutive days before initiating the protocol. The duration of swimming was progressively increased by 15 min each session, to achieve a period of 90 min on the sixth day. This ET protocol has been shown to induce significant improvement in cardiorespiratory fitness and potentiate ADSC action in the infarcted myocardium [21]. Moreover, insulted ischemia/reperfusion rats that performed prior swimming training (90 min/day) for four weeks had lower concentrations of proinflammatory cytokines in their serum [25]. At the end of training/no training period, rats were subjected to infarction or simulated surgery (Sham group), and 48 h after MI, ADSC were transplanted. Sham and sMI groups received culture medium without ADSC.
MI Induction
Following the ET protocol, the surgical procedure to induce chronic MI was performed in both trained and non-trained rats according to a well-established technique [21]. Briefly, under anesthesia (KX, intraperitoneal) and artificial ventilation (Harvard Rodent Ventilator, Model 863; Harvard Apparatus, Holliston, MA), a left thoracotomy was performed. After the heart was exteriorized, the coronary artery was ligated with 6 − 0 polypropylene suture and the heart was placed back and the thorax immediately closed. Sham rats were submitted to a similar procedure, with the exception of coronary occlusion.
Echocardiography
Two and thirty days following the surgical procedure, rats were anesthetized (KX, intraperitoneal) and the transthoracic echocardiogram was performed using a 12 MHz transducer (Sonos-5500, Hewlett-Packard, MA, USA). The MI size was evaluated on transverse 2-dimensional view of the LV and rats with MI size < 37% were excluded from the study [26, 27]. Measurements of end-diastolic (LVAd) and end-systolic (LVAs) LV transverse areas were performed in the three transverse planes (basal, medium, and apical) and LV systolic function was estimated by the fractional area change (FAC: LVAd- LVAs/LVAd x 100). Diastolic function was not evaluated owing to the fusion of the A and E waves.
LV Hemodynamic
The hemodynamic LV evaluation was carried out 30 days after MI to analyze the following (Acknowledge Software, Biopac Systems, Santa Barbara, ca., USA): systolic (LVSP) and end-diastolic pressures (LVDP), rate of change in the pressure (dP/dt), heart rate (HR), cardiac output (CO), and stroke work (SW). Full protocol was described earlier by our laboratory [26, 27]. After baseline evaluation, the hemodynamic study was performed under afterload LV stress. Sudden afterload stress was promoted by pressure overload using a single vasoconstrictive phenylephrine injection (l-phenylephrine hydrochloride; Sigma–Aldrich), with the dose (15–25 mg/kg, i.v.) adjusted for each animal to produce comparable blood pressure increases of 50–70% over the baseline.
ADSC Extraction, Cultivation and Transplantation
Subcutaneous adipose tissue was extracted from five non-trained male rats (Fisher-344) aged 12 weeks as described earlier [21, 28]. ADSCs in 20 µL volume were stained with trypan blue (0,4%) and viability was greater than 95%. Approximately 1 × 106 ADSCs were suspended in 100 µL culture medium (DMEM, Dulbecco’s modified Eagle’s medium), and injected into the myocardium at five points along the border zone by using a 30-gauge needle (BD Ultrafine, NJ, USA) after the first echocardiography analysis [21, 28]. Both Sham and sMI animals received injections of DMEM alone.
ADSC Myocardial Detection
ADSC detection was evaluated one hour and seven days after transplantation by two methods: [i] cells labeled with (111In)indium-oxine complex [ii] sex-determining region-Y (SRY) chromosome of male donor cells [29,30,31,32]. Both analyses were performed in sADSC and tADSC animals, according to the methods described below. Figure 2; Table 1 show radiolabeling stability and PCR primer sequences, respectively (supplementary material).
111In-ADSC Preparation
111Indium-oxine (111InOx) was prepared in-house by reaction of 111InCl3 and 8-hydroxyquinoline, following published protocol and was used in experiments when the radiochemical yield was more than 95% [29, 30]. ADSC labeling was done by adopting the protocol published for leukocyte labelling [31]. ADSC suspension was centrifuged, supernatant removed, and the pellet suspended in 2 mL of phosphate buffered saline. Then, 1 mL solution containing 111InOx was added and the vial was incubated at 37 °C for 20 min. After which, 3 mL of DMEM supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin, was added and centrifuged for 5 min at 150 g. The labeling efficiency was evaluated and determined as the ratio of the radioactivity contained in the pellet to the total radioactivity (sum of radioactivity in the cells plus the discarded supernatant). The pellet was suspended in a volume of 100 µl DMEM/1 × 106 cells for subsequent transplantation in the myocardium. To analyze the radiolabeling stability, 1 × 106 labeled 111In-ADSC were incubated for 24 h and centrifuged (Fig. 2). Radioactivity was measured in the pellet and the supernatant, and values compared with the baseline measurements. The washout rate determined by the radioactivity that exited the cells during 48 h is a measure of the stability of labeling. To examine the possible deleterious effect of radiolabeling, the viability of 111In-ADSC was determined by trypan blue assay.
In vivo 111In -ADSC Imaging Distribution
Two days after the MI induction, the radiolabeled 111In-ADSCs were transplanted (12.2 ± 5.2 MBq/106 cells) and monitored (one hour and seven days after transplantation) by single-photon emission computed tomography (SPECT) imaging. One group of sMI animals received an injection of 111InCl3 (without ADSCs) to identify the radioisotope biodistribution. Animals were anesthetized with 3% isoflurane in O2 and placed in dorsal decubitus to obtain the images. Computed tomography (CT) images were acquired (plane detector, 45 kVp, and 390 µA) immediately before the SPECT images for correct positioning of the cardiac area in the center of the field of view (FOV) and to obtain anatomical information for later fusion of the two imaging modalities. Both SPECT and CT images were acquired using equipment dedicated to small animals (Triumph Trimodality, Gamma Medica Ideas Inc., ca., USA). SPECT images were acquired using a two-detector camera (CZT detectors) with 5-pinhole collimators of 1.0 mm-hole each. We obtained 64 projections of 60 s each.
Ex vivo 111In-ADSC Distribution
At 1 h and 7 days post 111In-ADSCs injection, under isoflurane anesthesia, animals were euthanized by heart extirpation. Interest organs, such as: heart, spleen, liver and kidneys were removed, weighted, and radioactivity was measured in a gamma counter. A standard radioactive sample was used allowing to express uptake as percentage of injected dose per gram of organ (% ID/g organ).
Positron Emission Tomography (PET)
Considering the radiological safety, the rats could not be submitted to echocardiogram for determination of MI size, thus, infarcted area size was evaluated by PET-CT analysis. Briefly, seven days after ADSCs transplantation, 18–35 MBq of (18F)FDG was administered in the caudal vein of the rats for the acquisition of PET images. For suitable biodistribution, images were acquired after 40 min of (18F)FDG injection. Images were acquired for 5 min with the animal’s heart positioned in the center of FOV. This analysis was to identify viable myocardial regions capable of metabolizing glucose and to estimate necrotic areas.
SPECT, PET, and CT Image Processing
PET images were reconstructed by three-dimensional ordered subset expectation maximization (3D-OSEM) algorithm using 20 iterations and 4 subsets. SPECT images were reconstructed by OSEM using five iterations and eight subsets and using point spread function modeling. CT was reconstructed by filtered back projection method using a general-purpose filter. Images were analyzed by the cardiac module of the PMOD™ software (PMOD Technologies Ltd., Zurich, Switzerland).
mRNA Quantification Analysis
The mRNA expression analysis was conducted to: [i] quantify donor male ADSC in the sADSC and tADSC groups as evaluated by SRY expression; [ii] to verify the inflammatory profile as a consequence of MI, in the sham, sMI, sADSC, and tADSC groups. The remote MI site (septum) was collected from each animal, and mRNA assay was conducted as described earlier [32]. Primers used are shown in Table 1 (supplemental data).
Histology
Thirty days after MI, LV samples were collected and stained with hematoxylin and eosin for nuclear volume measurement and Picrosirius red for fibrosis evaluation, as described before [26, 33].
Statistical Analysis
Shapiro-Wilk’s test was used to verify normality data and Levene’s test was applied to assess the equality of variances. Results were presented as a mean ± standard error of the mean. The comparisons between the groups were made by unpaired Student’s t-test, one-way ANOVA (post hoc: Newman–Keuls) or two-way ANOVA (post hoc: Bonferroni). Pearson’s correlation was used in the correlations. Kaplan-Meier curves were used to define mortality. A p-value ≤ 0.05 was regarded as statistically significant.
Results
LV Morphology and Performance
The infarct size two days post-coronary occlusion was not different between the experimental groups. There was an increase in infarct size in the sMI group after a 30-day follow-up, while infarcts were proportionally smaller in all ADSCs-treated groups (Fig. 1a). LV areas were significantly increased over 30 days, and ADSCs therapy attenuated cavity dilation without the additive effect of ET (Fig. 1b-c). Decreased FAC was seen after two days of coronary occlusion, in which significant improvements in FAC were noted only in the tADSC group over 30 days (Fig. 1d). Infarcted rats had overt LV dysfunction as indicated by an increased LVEDP and decreased LVSP, +dP/dt and CO (Fig. 1e-i). The animals treated with ADSCs injections (sADSC group) presented a higher + dP/dt than the sMI group. There was an additional effect of ET on ADSCs therapy as it restored LVSP, +dP/dt, -dP/dt, and LVEDP as well as improved CO. On afterload stress (Fig. 1j), all infarcted groups showed lower LVSP and higher LVEDP values than the Sham group. CO and SW were reduced in the sMI group compared to those in Sham rats, and there was no beneficial effect from isolated ADSCs treatment. Nevertheless, there was a positive effect from the combination of ET with ADSCs as it restored CO and improved SW.
Morphologic and functional data. Panel A: MI size; Panel B: left ventricle diastolic area (LVAd); Panel C: left ventricle systolic area (LVAs); Panel D: fractional area change (FAC); Panel E: left ventricular systolic pressure (LVSP); Panel F: maximal rate of pressure rise (+ dP/dtmax); Panel G: maximal rate of pressure decline (–dP/dtmax); Panel H: left ventricular end-diastolic pressure (LVEDP); Panel I: cardiac output (CO); Panel J: changes in the hemodynamic parameters induced by sudden afterload stress, expressed as percent change from baseline. SW, stroke work. Positive or negative values result from an increase or decrease in the related parameter, respectively. Two-way repeated ANOVA and Bonferroni were applied in CO comparisons. One-way ANOVA and Newman-Keuls were applied for comparisons in the hemodynamic evaluation (n = 10/group). *p < 0.05 vs.. Sham; †p < 0.05 vs.. sMI; ‡p < 0.05 vs.. sADSC
LV mass (Fig. 2a), the nuclear volume of the cardiomyocytes (Fig. 2b/f), and collagen content (Fig. 2c/g) were increased by MI at 30 days after MI. ADSC therapy abolished myocardial hypertrophy and fibrosis without any additive effect from ET. Figure 2d-e shows the expression of the myosin heavy chain β (β-MHC) gene associated with cardiac hypertrophy at one hour and seven days after transplantation, respectively. sMI group shows marked activation of the fetal gene. Attenuation of β-MHC values comparable to levels seen in the Sham group is seen in the ADSC treated rats, especially the tADSC group.
Biometric data. Panel A: left ventricle mass (LV mass); Panel B: nuclear volume (arrows); Panel C: collagen (%); Panel D: levels of the mRNA of myosin heavy chain β (β-MHC) following one hour post-ADSC transplantation; Panel E: levels of the mRNA of β-MHC following seven days post-ADSC transplantation; Panel F: representative photomicrographs of hematoxylin-eosin stain (magnification x40; arrows illustrate cardiomyocyte nuclei; scale bar: 50 µm); Panel G: representative photomicrographs of picrosirius red (magnification x40; Scale bar: 50 µm). One-way ANOVA and Newman-Keuls were applied for comparisons in the histologic (n = 06/group) and mRNA (n = 06/group) *p < 0.05 vs.. Sham; †p < 0.05 vs.. sMI; ‡p < 0.05 vs.. sADSC
Stem Cell Detection
Rats received 111In-ADSC transplantation with mean radioactivity of 11.7 ± 5 MBq (Fig. 3a-b). At one hour post-transplantation, higher ADSCs content was reported in the tADSC group than in the sADSC group (Fig. 3d). Seven-day post-transplantation analysis results show a significant decrease in ADSCs, without a beneficial effect from ET. Results of SRY expression show that the tADSC group had significantly higher values of ADSCs at both time points when compared to the sADSC group (Fig. 3e). Other sites (i.e., spleen, liver, and kidney) show no differences in radioactivity between the sADSC and tADSC groups (Fig. 3f).
In vivo and ex vivo distribution of radiolabeled compounds. Panel A: control experiment. The activity of 111Indium-oxine (111InOx) complex without ADSC binding. White arrows indicate the distribution of 111InOx. Panel B: representative images of the activity of 111In-ADSC. White arrows indicate the distribution of 111In-ADSC. Panel C: cardiac tissue metabolism after (18F)FDG injection. (18F)FDG rich regions are marked in red, according to scale. White arrows indicate MI area. Panel D: amount of 111In-ADSC in the heart after one hour and seven days of transplantation. Values are expressed as mean percentage of radioactivity immediately post-transplantation (sADSC, n = 03 and tADSC, n = 05). Panel E: levels of SRY gene, one hour and seven days after transplantation (n = 05/group). Panel F: 111In-ADSC in spleen, liver and kidney, 7 days after transplantation (n = 05/group). Unpaired Student’s t/group -test was applied for the comparisons
Myocardial Inflammation
Rats with infarction had higher levels of pro-inflammatory cytokines as well as interleukin 10 (IL-10) compared to Sham rats (Fig. 4a/h). ADSCs therapy resulted in lower interleukin 1β (IL-1β), interleukin 6 (IL-6), and tumor necrosis factor α (TNF-α) levels, and increased IL-10 expression was noted only after seven days of cell transplantation. All proinflammatory cytokines (i.e. IL-1β, IL-6, TNF-α, and transforming growth factor β (TGF-β)) were lower in the tADSC group compared to those in sMI rats. It is noteworthy that tADSC group had significantly higher IL-10 levels than other experimental groups at one hour and seven days post-transplantation. An analysis of the ratio of anti/pro-inflammatory cytokines confirms enhanced activity of the combination therapy (ET + ADSC) in an improvement of the anti-inflammatory profile (Fig. 4b/I). The increases in IL-1β, TNF-α, and TGF-β were negatively correlated with the reduced ADSC content at one hour (Fig. 4c-f) and seven days (Fig. 4j-m) post-transplantation, respectively. On the other hand, increased IL-10 expression was positively correlated with larger amounts of ADSCs (Fig. 4g/n).
Inflammatory profile, one hour and seven days after ADSC transplantation (n = 10/group). Panel A: mRNA levels of the inflammatory cytokines, one hour after transplantation. IL-1β: interleukin 1β; IL-6: interleukin 6; TNF-ɑ: tumor necrosis factor ɑ; TGF-β: transforming growth factor β1; IL-10, interleukin 10; Panel B: anti/pro-inflammatory cytokine ratios. Panels C-G: correlation between the gene expression of inflammatory cytokines and SRY, one hour after transplantation; Panel H: mRNA levels of the inflammatory cytokines, seven days after transplantation. Panel I: anti/pro-inflammatory cytokine ratios. Panels J-N: correlation between the gene expression of inflammatory cytokines and SRY, seven days after transplantation. One-way ANOVA and Newman-Keuls were applied for the comparisons. Pearson’s correlation was used for the correlations. *p < 0.05 vs.. Sham; †p < 0.05 vs.. sMI; ‡p < 0.05 vs.. sADSC
Survival
Thirty-day follow-up showed lower survival of sMI and sADSC rats compared to sham rats (Fig. 5). However, the survival in the tADSC group was higher compared to rats in the sMI group but similar to the Sham group.
Discussion
The present study evaluated the combined effect of prior ET and ADSCs transplantation in post-infarction cardiac remodeling. It appears that ET enhanced the effects of ADSCs therapy. Our data also illustrate that cardiac ADSC retention can be further improved by ET, and these findings were associated with a lower pro-inflammatory profile.
We undertook this study to know and overcome one of the main limitations for successful SCs therapy, a high inflammatory response post-infarction promoting an unfavourable microenvironment [34, 35] leading to low ADSCs retention and survival [35]. Thus, developing approaches to increase cell viability and retention seem to improve SCs therapy [6, 36]. Zhang et al. reported that application of photobiomodulation to myocardium prior to SC transplantation enhances cell survival rate by 2-fold and increase the number of newly formed capillaries [20]. Recently, we showed preconditioning by ET potentiates the cardioprotective effects of ADSCs after MI by inducing an angiogenic milieu that stimulates survival factors such as Akt signalling [21]. In this study, ET was used to create a propitious microenvironment for ADSCs, and this premise was based on the evidence that ET may promote significant anti-inflammatory profile in animals [37, 38]. In this regard, we have previously shown that prior ET decreased cytokine expression after MI [24], and other authors have reported lower plasma levels of TNF-α and IL-6 and higher blood levels of IL-10 in rats subjected to treadmill running post-MI [23]. The association between decrease in pro-inflammatory cytokines and ADSCs with reduction/inhibition of inflammation may benefit cellular therapy, as shown in earlier studies of attenuated apoptosis and increased SC survival in rats receiving cytokine antagonists [12, 14].
Our findings support the hypothesis that aerobic exercise increases the retention of exogenously infused SC. This was originally shown by Chirico et al. [22] in exercised mice with small epicardial MIs subjected to GFP+ bone marrow-derived cells. Here, ADSCs were detected based on two monitoring methods. As seen in Fig. 3, there was an inconsistency between radiolabeling with indium-oxine and the SYR gene expression findings at seven days. Although we have found that there is no loss of cellular radioactivity at 48 h post-indium incubation (Fig. 2, in supplementary data), it is possible that radionuclides decay with longer incubation (i.e. seven days). This was found consistently using 111In-oxine incorporation in human SC, which was an adequate method for monitoring transplanted cells by serial SPECT/CT imaging for at least two days with the following decline in radioactivity [31]. Together with SPECT/CT analysis, we also used qRT-PCR as an established method to evaluate homing of the implanted SC [29, 39]. Consequently, it can be assumed, at least experimentally, that long-term myocardial ADSCs measurements require more than one detection method because SYR gene expression is far more reliable than direct ADSCs radiolabeling.
In the present study, ET enhanced the benefits of ADSC by reducing IL-1β at one hour and IL-6 at seven days post-transplantation. Moreover, the combination of ADSC with prior ET may be the most effective treatment for increasing myocardial IL-10 levels. These results have important implications because a hostile proinflammatory microenvironment is linked to reduced retention and functionality of the SCs [8, 40]. For example, using skeletal muscle precursor cells, Suzuki et al. reported that the number of cells was two-fold greater in mouse hearts subjected to IL-1β inhibition compared with that of the control group [12]. In fact, a hostile microenvironment with a burst of inflammatory cytokines has an inverse relationship with the survival of transplanted cells [12, 14]. To our knowledge, there are no studies examining the repercussions of an increased level of IL-10 on the graft and function of ADSCs in the infarcted myocardium. However, a study showed that treatment with IL-10 increased retention of transplanted endothelial progenitor cells in the myocardium and was associated with minor apoptosis post-MI [41]. Thus, increased IL-10 levels may have contributed to greater myocardial ADSCs in exercised rats. However, it is necessary to clarify how the mode of cell death, whether by necrosis or apoptosis, could be influenced by lower IL-1β and IL-6 expression as well as by higher IL-10 expression in tADSC rats. We also may not be able to determine if the phenotypic and functional characteristics of ADSCs were changed in the trained animals compared to sADSC rats.
Although the cause-effect relationship of inflammation and ADSCs retained in the myocardium cannot be obtained from our data because correlation analyses indicate the inferential direction of the variables, a less proinflammatory environment found in the tADSC group as demonstrated by the IL-10/proinflammatory cytokine ratio has important implications. It is likely that various complicating factors are involved in cytokine-related inflammation as in increased necrosis and apoptosis [42]. Moreover, there is a body of data showing that high levels of proinflammatory cytokines and lower levels of anti-inflammatory IL-10 contribute to cardiac remodeling and increased morbidity and mortality risk in patients with ischemic heart failure [43]. Therefore, it could be that a better inflammatory profile in trained rats may have improved the effect of ADSCs on post-infarct LV remodeling. It is important to emphasize the most pronounced IL-10 content in tADSC rats because a key role of IL-10 has been reported to mediate the beneficial effects of cell therapy [29, 41]. Improved ADSCs retention in the tADSC group may also be a result of increased Akt and angiogenic factors in the myocardium. It has recently been shown that the combination of ADSCs therapy with prior ET was associated with increased Akt activity, improved VEGF expression and increased capillarity in the border zone [21]. Therefore, it is assumed that this improved myocardial capillarity may benefit the survival of transplanted ADSCs as a result of better oxygen and nutrient intake.
Earlier studies are unclear whether ET could synergize with SC to improve cardiac performance. Chirico et al. [22] inoculated mice with bone marrow SC after myocardial cryoinjury and demonstrated no additive effect of ET on ejection fraction. Likewise, Lovaroto et al. [44] showed no additional benefit in LV function in infarcted rats treated with ET combined with bone marrow SCs. On the other hand, Cosmo et al. [45] injected bone marrow SC in infarcted rats, and 30 days after injury subjected the animals to 30 days of swimming. They found that the LV ejection fraction was improved only in animals with a combined treatment. Such improvement of cardiac function was recently shown by us, in which ET before ADSCs transplantation appeared to prevent LV systolic dysfunction and to boost the effects of cellular therapy on myocardial inotropism [21]. We present here an extension to these findings by showing that ET combined with post-ADSCs transplantation resulted in superior functional benefits such as enhanced FAC, +dP/dt, -dP/dt, LVEDP, and CO compared to isolated ADSCs therapy. These effects persisted even under LV afterload stress, in which CO and SW was better in the tADSC group than in the sADSC group. It is important for the maintenance of cardiac ejection up to certain levels of overload, indicating that the heart is able to respond effectively to increased resistance to LV emptying, even though they have large infarcts [27]. The best cardiac function results in this study compared to that of previous investigations may be explained by differences in the route of administration of SC. In studies by Chirico et al. [22] and Lavaroto et al. [44], the SCs were injected into the vein, while we and Cosmo et al. [45] have adopted an intramyocardial route. It has been previously demonstrated that intramyocardial injection is the most efficient route in terms of cardiac cell retention [35]. Therefore, a greater amount of SC in the myocardium could enable a greater interaction with ET and result in more pronounced cardiac functional benefits. Previous studies have started ET after multiple weeks [45] or near SC transplantation [22, 44]. However, in the present study, the rats were trained for several weeks prior to cell transplantation and thus, the myocardial milieu was likely most appropriate for ADSCs therapy. It is more important to consider translating greater ADSC retention to potentiate restorative processes in myocardium including including activation of resident or remote endogenous stem cells, secretion of immunomodulatory and trophic factors, stabilization of the extracellular matrix, and enhanced vascularization [46, 47].
Our last finding was the distinction between the survival curves of tADSC and sMI rats. Although the mechanisms by which ET prolong survival in advanced cardiopathy of ADSCs-treated rats have yet to be established, a better systolic performance can have significant influence. For example, only tADSC rats exhibited FAC values greater than 40% during the follow-up study. According to the univariate analysis of our previous study on female rats with post-infarction heart failure, FAC values less than or equal to 37% were associated with a shorter survival time [48]. It should be noted that survival curves between the sADSC and tADSC groups were separated early in the follow-up, but no significant differences were detected. The current study was not designed to primarily examine survival, which requires a more expressive sample of animals and a longer follow-up period [49, 50]. These factors limit the interpretation of our survival data because they may reduce the power of analysis.
Some limitations of the study related to the experimental design show to be addressed. Although our main aim was to evaluate the role of prior ET on ADSC retention and cardiac remodeling in infarcted rats, the effect of the isolated ET on the LV function, myocardial inflammation and micro-environment cannot be clarified because of the lack of trained rats submitted to MI without ADSC. Additionally, our study is limited to evaluate the gene profile of inflammatory cytokines and will require protein level validation at the same myocardial site in which mRNA samples were harvested. Lastly, it is well established that high levels of physical fitness are associated with reduced developing heart failure and mortality in patients with cardiovascular disease [51,52,53]. This issue was not addressed in this study, which would clarify whether the combination of ADSCs therapy with ET could result in a more effective improvement in the functional fitness of infarcted rats.
In summary, this study highlights the beneficial role of ET preconditioning in increasing myocardial retention of ADSCs and attenuating cardiac remodeling post-MI in rats. Analysis of anti-inflammatory cytokine expression shows an improvement in the ET linked myocardial microenvironment. The broad and significant impact of increased ADSC retention and further improvement in cardiac remodeling contributes to longer survival found only in the tADSC group.
References
Cai, B., Wang, G., Chen, N., Liu, Y., Yin, K., Ning, C., & Lu, Y. (2014). Bone marrow mesenchymal stem cells protected post-infarcted myocardium against arrhythmias via reversing potassium channels remodelling. Journal of Cellular and Molecular Medicine , 18(7), 1407–1416. https://doi.org/10.1111/jcmm.12287
Si, Z., Wang, X., Sun, C., Kang, Y., Xu, J., Wang, X., & Hui, Y. (2019). Adipose-derived stem cells: Sources, potency, and implications for regenerative therapies. Biomedicine & Pharmacotherapy, 114, 108765. https://doi.org/10.1016/j.biopha.2019.108765
Bacakova, L., Zarubova, J., Travnickova, M., Musilkova, J., Pajorova, J., Slepicka, P., & Molitor, M. (2018). Stem cells: their source, potency and use in regenerative therapies with focus on adipose-derived stem cells - a review. Biotechnology Advances, 36(4), 1111–1126. https://doi.org/10.1016/j.biotechadv.2018.03.011
de Oliveira, T. S., Serra, A. J., Manchini, M. T., Bassaneze, V., de Krieger, J. E. Tarso Camillo de Carvalho, P.,.. . Silva, J. A. Jr. (2015). Effects of low level laser therapy on attachment, proliferation, and gene expression of VEGF and VEGF receptor 2 of adipocyte-derived mesenchymal stem cells cultivated under nutritional deficiency. Lasers in Medical Science, 30(1), 217–223. https://doi.org/10.1007/s10103-014-1646-9.
Song, S. Y., Chung, H. M., & Sung, J. H. (2010). The pivotal role of VEGF in adipose-derived-stem-cell-mediated regeneration. Expert Opinion on Biological Therapy, 10(11), 1529–1537. https://doi.org/10.1517/14712598.2010.522987
Samper, E., Diez-Juan, A., Montero, J. A., & Sepulveda, P. (2013). Cardiac cell therapy: boosting mesenchymal stem cells effects. Stem Cell Reviews, 9(3), 266–280. https://doi.org/10.1007/s12015-012-9353-z
Wu, J. Y., Chen, C. H., Wang, C. Z., Ho, M. L., Yeh, M. L., & Wang, Y. H. (2013). Low-power laser irradiation suppresses inflammatory response of human adipose-derived stem cells by modulating intracellular cyclic AMP level and NF-kappaB activity. PLoS One, 8(1), e54067. https://doi.org/10.1371/journal.pone.0054067
Wu, K. H., Mo, X. M., Han, Z. C., & Zhou, B. (2011). Stem cell engraftment and survival in the ischemic heart. The Annals of Thoracic Surgery, 92(5), 1917–1925. https://doi.org/10.1016/j.athoracsur.2011.07.012
Bruyneel, A. A., Sehgal, A., Malandraki-Miller, S., & Carr, C. (2016). Stem Cell Therapy for the Heart: Blind Alley or Magic Bullet? Journal of Cardiovascular Translational Research, 9(5–6), 405–418. https://doi.org/10.1007/s12265-016-9708-y
Fish, K. M., Ishikawa, K., & Hajjar, R. J. (2018). Stem cell therapy for acute myocardial infarction: on the horizon or still a dream? Coronary Artery Disease , 29(2), 89–91. https://doi.org/10.1097/MCA.0000000000000589
Shafei, A. E., Ali, M. A., Ghanem, H. G., Shehata, A. I., Abdelgawad, A. A., Handal, H. R., & El-Shal, A. S. (2018). Mechanistic effects of mesenchymal and hematopoietic stem cells: New therapeutic targets in myocardial infarction. Journal of Cellular Biochemistry, 119(7), 5274–5286. https://doi.org/10.1002/jcb.26637
Suzuki, K., Murtuza, B., Beauchamp, J. R., Brand, N. J., Barton, P. J., Varela-Carver, A., & Yacoub, M. H. (2004). Role of interleukin-1beta in acute inflammation and graft death after cell transplantation to the heart. Circulation, 110(11 Suppl 1), II219-I224. https://doi.org/10.1161/01.CIR.0000138388.55416.06
Yang, Y. J., Qian, H. Y., Huang, J., Geng, Y. J., Gao, R. L., Dou, K. F., & Zhao, S. H. (2008). Atorvastatin treatment improves survival and effects of implanted mesenchymal stem cells in post-infarct swine hearts. European Heart Journal, 29(12), 1578–1590. https://doi.org/10.1093/eurheartj/ehn167
Wang, L., Wei, F. X., Cen, J. S., Ping, S. N., Li, Z. Q., Chen, N. N., & Liu, S. Y. (2014). Early administration of tumor necrosis factor-alpha antagonist promotes survival of transplanted neural stem cells and axon myelination after spinal cord injury in rats. Brain Research, 1575, 87–100. https://doi.org/10.1016/j.brainres.2014.05.038
Menasche, P. (2018). Cell therapy trials for heart regeneration - lessons learned and future directions. Nature Reviews. Cardiology, 15(11), 659–671. https://doi.org/10.1038/s41569-018-0013-0
Vrtovec, B., Poglajen, G., Lezaic, L., Sever, M., Domanovic, D., Cernelc, P., & Wu, J. C. (2013). Effects of intracoronary CD34 + stem cell transplantation in nonischemic dilated cardiomyopathy patients: 5-year follow-up. Circulation Research, 112(1), 165–173. https://doi.org/10.1161/CIRCRESAHA.112.276519
Ziebart, T., Yoon, C. H., Trepels, T., Wietelmann, A., Braun, T., Kiessling, F., & Dimmeler, S. (2008). Sustained persistence of transplanted proangiogenic cells contributes to neovascularization and cardiac function after ischemia. Circulation Research, 103(11), 1327–1334. https://doi.org/10.1161/CIRCRESAHA.108.180463
Kanda, P., & Davis, D. R. (2017). Cellular mechanisms underlying cardiac engraftment of stem cells. Expert Opinion on Biological Therapy , 17(9), 1127–1143. https://doi.org/10.1080/14712598.2017.1346080
Liu, Y., & Zhang, H. (2016). Low-Level Laser Irradiation Precondition for Cardiac Regenerative Therapy. Photomedicine and Laser Surgery , 34(11), 572–579. https://doi.org/10.1089/pho.2015.4058
Zhang, H., Hou, J. F., Shen, Y., Wang, W., Wei, Y. J., & Hu, S. (2010). Low level laser irradiation precondition to create friendly milieu of infarcted myocardium and enhance early survival of transplanted bone marrow cells. Journal of Cellular and Molecular Medicine, 14(7), 1975–1987. https://doi.org/10.1111/j.1582-4934.2009.00886.x
de Souza Vieira, S., Antonio, E. L., de Melo, B. L., Portes, L. A., Montemor, J., Oliveira, H. A., & Serra, A. J. (2019). Exercise Training Potentiates The Cardioprotective Effects of Stem Cells Post-infarction. Heart, Lung & Circulation, 28(2), 263–271. https://doi.org/10.1016/j.hlc.2017.11.005
Chirico, E. N., Ding, D., Muthukumaran, G., Houser, S. R., Starosta, T., Mu, A.,.. . Libonati, J. R. (2015). Acute aerobic exercise increases exogenously infused bone marrow cell retention in the heart. Physiological Reports, 3(10). https://doi.org/10.14814/phy2.12566.
Nunes, R. B., Alves, J. P., Kessler, L. P., & Dal Lago, P. (2013). Aerobic exercise improves the inflammatory profile correlated with cardiac remodeling and function in chronic heart failure rats. Clinics, 68(6), 876–882. https://doi.org/10.6061/clinics/2013(06)24
Santos, M. H., Mde, H., Tucci, L., Garavelo, P. J., Reis, S. M., Antonio, M. M., & Maranhao, E. L. (2016). Previous exercise training increases levels of PPAR-alpha in long-term post-myocardial infarction in rats, which is correlated with better inflammatory response. Clinics, 71(3), 163–168. https://doi.org/10.6061/clinics/2016(03)08
Sharma, A. K., Kumar, A., Sahu, M., Sharma, G., Datusalia, A. K., & Rajput, S. K. (2018). Exercise preconditioning and low dose copper nanoparticles exhibits cardioprotection through targeting GSK-3beta phosphorylation in ischemia/reperfusion induced myocardial infarction. Microvascular Research, 120, 59–66. https://doi.org/10.1016/j.mvr.2018.06.003
Manchini, M. T., Antonio, E. L., Silva Junior, J. A., de Carvalho, P. T., Albertini, R., Pereira, F. C., & Serra, A. J. (2017). Low-Level Laser Application in the Early Myocardial Infarction Stage Has No Beneficial Role in Heart Failure. Frontiers in Physiology, 8, 23. https://doi.org/10.3389/fphys.2017.00023
dos Santos, L., Antonio, E. L., Souza, A. F., & Tucci, P. J. (2010). Use of afterload hemodynamic stress as a practical method for assessing cardiac performance in rats with heart failure. Canadian Journal of Physiology and Pharmacology, 88(7), 724–732. https://doi.org/10.1139/y10-062
de Lima, R. D. N., Vieira, S. S., Antonio, E. L., de Carvalho, C., de Paula Vieira, P. T., Mansano, R., & Serra, B. (2019). Low-level laser therapy alleviates the deleterious effect of doxorubicin on rat adipose tissue-derived mesenchymal stem cells. Journal of Photochemistry and Photobiology. B, 196, 111512. https://doi.org/10.1016/j.jphotobiol.2019.111512
Zhang, H., Song, P., Tang, Y., Zhang, X. L., Zhao, S. H., Wei, Y. J., & Hu, S. S. (2007). Injection of bone marrow mesenchymal stem cells in the borderline area of infarcted myocardium: heart status and cell distribution. The Journal of Thoracic and Cardiovascular Surgery , 134(5), 1234–1240. https://doi.org/10.1016/j.jtcvs.2007.07.019
Scheffel, U., Tsan, M. F., & McIntyre, P. A. (1979). Labeling of human platelets with [111In) 8-hydroxyquinoline. Journal of Nuclear Medicine, 20(6), 524–531. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/119834.
Gildehaus, F. J., Haasters, F., Drosse, I., Wagner, E., Zach, C., Mutschler, W., & Schieker, M. (2011). Impact of indium-111 oxine labelling on viability of human mesenchymal stem cells in vitro, and 3D cell-tracking using SPECT/CT in vivo. Molecular Imaging and Biology, 13(6), 1204–1214. https://doi.org/10.1007/s11307-010-0439-1
de Oliveira, H. A., Antonio, E. L., Silva, F. A., de Carvalho, P. T. C., Feliciano, R., Yoshizaki, A., & Serra, A. J. (2018). Protective effects of photobiomodulation against resistance exercise-induced muscle damage and inflammation in rats. Journal of Sports Sciences, 36(20), 2349–2357. https://doi.org/10.1080/02640414.2018.1457419
Serra, A. J., Higuchi, M. L., Ihara, S. S., Antonio, E. L., Santos, M. H., Bombig, M. T., & Tucci, P. J. (2008). Exercise training prevents beta-adrenergic hyperactivity-induced myocardial hypertrophy and lesions. European Journal of Heart Failure, 10(6), 534–539. https://doi.org/10.1016/j.ejheart.2008.03.016
Frangogiannis, N. G. (2014). The inflammatory response in myocardial injury, repair, and remodelling. Nature Reviews. Cardiology, 11(5), 255–265. https://doi.org/10.1038/nrcardio.2014.28
Nakamuta, J. S., Danoviz, M. E., Marques, F. L., dos Santos, L., Becker, C., Goncalves, G. A., & Krieger, J. E. (2009). Cell therapy attenuates cardiac dysfunction post myocardial infarction: effect of timing, routes of injection and a fibrin scaffold. PLoS One, 4(6), e6005. https://doi.org/10.1371/journal.pone.0006005
Richardson, J. D., Nelson, A. J., Zannettino, A. C., Gronthos, S., Worthley, S. G., & Psaltis, P. J. (2013). Optimization of the cardiovascular therapeutic properties of mesenchymal stromal/stem cells-taking the next step. Stem Cell Reviews, 9(3), 281–302. https://doi.org/10.1007/s12015-012-9366-7
Petersen, A. M., & Pedersen, B. K. (2005). The anti-inflammatory effect of exercise. Journal of Applied Physiology (1985), 98(4), 1154–1162. https://doi.org/10.1152/japplphysiol.00164.2004
Petersen, A. M., & Pedersen, B. K. (2006). The role of IL-6 in mediating the anti-inflammatory effects of exercise. Journal of Physiology and Pharmacology, 57 Suppl 10, 43–51. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17242490.
Motawi, T. M., Atta, H. M., Sadik, N. A., & Azzam, M. (2014). The therapeutic effects of bone marrow-derived mesenchymal stem cells and simvastatin in a rat model of liver fibrosis. Cell Biochemistry and Biophysics, 68(1), 111–125. https://doi.org/10.1007/s12013-013-9698-1
Fan, W., Cheng, K., Qin, X., Narsinh, K. H., Wang, S., Hu, S., & Cao, F. (2013). mTORC1 and mTORC2 play different roles in the functional survival of transplanted adipose-derived stromal cells in hind limb ischemic mice via regulating inflammation in vivo. Stem Cells, 31(1), 203–214. https://doi.org/10.1002/stem.1265
Krishnamurthy, P., Thal, M., Verma, S., Hoxha, E., Lambers, E., Ramirez, V., & Kishore, R. (2011). Interleukin-10 deficiency impairs bone marrow-derived endothelial progenitor cell survival and function in ischemic myocardium. Circulation Research, 109(11), 1280–1289. https://doi.org/10.1161/CIRCRESAHA.111.248369
Suzuki, K., Murtuza, B., Smolenski, R. T., Sammut, I. A., Suzuki, N., Kaneda, Y., & Yacoub, M. H. (2001). Overexpression of interleukin-1 receptor antagonist provides cardioprotection against ischemia-reperfusion injury associated with reduction in apoptosis. Circulation, 104(12 Suppl 1), I308–I303. https://doi.org/10.1161/hc37t1.094871
Borow, K. M., Yaroshinsky, A., Greenberg, B., & Perin, E. C. (2019). Phase 3 DREAM-HF Trial of Mesenchymal Precursor Cells in Chronic Heart Failure. Circulation Research, 125(3), 265–281. https://doi.org/10.1161/CIRCRESAHA.119.314951
Lavorato, V. N., Carlo, D., da Cunha, R. J., Okano, D. N., Belfort, B. S., de Freitas, F. G., & Natali, J. S. (2016). Mesenchymal stem cell therapy associated with endurance exercise training: Effects on the structural and functional remodeling of infarcted rat hearts. Journal of Molecular and Cellular Cardiology, 90, 111–119. https://doi.org/10.1016/j.yjmcc.2015.12.012
Cosmo, S., Francisco, J. C., Cunha, R. C., Macedo, R. M., Faria-Neto, J. R., Simeoni, R., & Guarita-Souza, L. C. (2012). Effect of exercise associated with stem cell transplantation on ventricular function in rats after acute myocardial infarction. Revista Brasileira de Cirurgia Cardiovascular, 27(4), 542–551. https://doi.org/10.5935/1678-9741.20120096
Bernal, A., & Galvez, B. G. (2013). The potential of stem cells in the treatment of cardiovascular diseases. Stem Cell Reviews and Reports, 9(6), 814–832. https://doi.org/10.1007/s12015-013-9461-4
Madigan, M., & Atoui, R. (2018). Therapeutic Use of Stem Cells for Myocardial Infarction. Bioengineering (Basel), 5(2). https://doi.org/10.3390/bioengineering5020028.
Santos, A. A., Helber, I., Flumignan, R. L., Antonio, E. L., Carvalho, A. C., Paola, A. A., & Moises, V. A. (2009). Doppler echocardiographic predictors of mortality in female rats after myocardial infarction. Journal of Cardiac Failure, 15(2), 163–168. https://doi.org/10.1016/j.cardfail.2008.10.017
Helber, I., Dos Santos, A. A., Antonio, E. L., Flumignan, R. L., Bocalini, D. S., Piccolo, C., & Tucci, P. J. (2009). Digitoxin prolongs survival of female rats with heart failure due to large myocardial infarction. Journal of Cardiac Failure, 15(9), 798–804. https://doi.org/10.1016/j.cardfail.2009.05.002
dos Santos, A. A., Helber, I., Antonio, E. L., Franco, M. F., & Tucci, P. J. (2013). Severity of the cardiac impairment determines whether digitalis prolongs or reduces survival of rats with heart failure due to myocardial infarction. International Journal of Cardiology, 167(2), 357–361. https://doi.org/10.1016/j.ijcard.2011.12.097
Lavie, C. J., Arena, R., Swift, D. L., Johannsen, N. M., Sui, X., Lee, D. C., & Blair, S. N. (2015). Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circulation Research, 117(2), 207–219. https://doi.org/10.1161/CIRCRESAHA.117.305205
O’Connor, G. T., Buring, J. E., Yusuf, S., Goldhaber, S. Z., Olmstead, E. M., Paffenbarger, R. S., Jr., & Hennekens, C. H. (1989). An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation, 80(2), 234–244. https://doi.org/10.1161/01.cir.80.2.234
Pandey, A., Patel, M., Gao, A., Willis, B. L., Das, S. R., Leonard, D., & Berry, J. D. (2015). Changes in mid-life fitness predicts heart failure risk at a later age independent of interval development of cardiac and noncardiac risk factors: the Cooper Center Longitudinal Study. American Heart Journal, 169(2), 290-297 e291. https://doi.org/10.1016/j.ahj.2014.10.017
Acknowledgements
Authors are grateful to Editage company for English assistance and proofreading the article. This work was supported by São Paulo Research Foundation – FAPESP [09/54225-8, 15/11028-9, 2018/06865-7) and Brazilian National Council for Scientific and Technological Development – CNPq [305527/2017-7]. Funding sources had no involvement in study design or collection, analysis and interpretation of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors have no conflicts of interest to disclose. Authors confirm that that the work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form in English or in any other language, without the written consent of the copyright holder.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 172 kb)
Rights and permissions
About this article
Cite this article
Souza Vieira, S., Antonio, E.L., de Melo, B.L. et al. Increased Myocardial Retention of Mesenchymal Stem Cells Post-MI by Pre-Conditioning Exercise Training. Stem Cell Rev and Rep 16, 730–741 (2020). https://doi.org/10.1007/s12015-020-09970-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-020-09970-z