Opinion Statement
Longstanding diabetes mellitus (both type 1 and type 2) can impair gastric motor function and cause significant upper gastrointestinal symptoms which significantly degrade quality of life, cause nutritional deficits, and degrade healthcare resource use. The most commonly considered gut complication of diabetes, diabetic gastroparesis, is a syndrome of delayed gastric emptying in the absence of mechanical obstruction which leads to symptoms of nausea, vomiting, postprandial fullness, early satiation, bloating, and upper abdominal pain. Gastroparesis also can lead to loss of glycemic control. A diagnosis of gastroparesis is made by documenting delayed gastric emptying and excluding mechanical obstruction. Gastric emptying scintigraphy is the most commonly utilized test for the diagnosis of gastroparesis but novel tests of gastric function have recently been introduced including the gastric emptying breath test and wireless motility capsule. Management most often is aimed at controlling symptoms, which includes dietary modification, optimization of glycemic control, and medication therapy with prokinetics, antiemetics, and neuromodulatory agents. Endoscopic and/or surgical therapies may be considered for refractory cases of gastroparesis. Recent research has provided new insights into the pathophysiology of this disease and is characterizing potential benefits of novel therapeutic agents which show promise in the treatment of this condition. This article will review the pathophysiology, new insights into disease mechanism, and treatment options for diabetic gastroparesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus produces significant morbidity and mortality. The Centers for Disease Control and Prevention estimated the prevalence of diabetes in the USA to be 9.3% in 2014 which is projected to increase to 33% by 2050 ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4972249/#pone.0159876.ref003 ). An association between diabetic neuropathy and gut dysmotility was described in 1945 in a case series of 125 patients which observed constipation, diarrhea, anorexia, and/or nausea in 62% of patients. The term gastroparesis diabeticorum was introduced by Kassander in 1958 in patients with diabetes who exhibited gastric retention on barium studies [1].
Epidemiology
Upper GI symptoms are prevalent in diabetes. A study of 423 patients with diabetes [95% with type 2 diabetes (T2DM)] found that 8–11% reported early satiety, fullness, bloating, and nausea or vomiting [2]. Adjusting for age and sex, symptoms were more frequent in diabetes versus the general population (OR 1.75; 95% CI, 1.34–2.29) and related to poor glycemic control. Another 110 patient cohort with type 1 diabetes (T1DM) also exhibited an increased prevalence of upper GI symptoms versus controls which were prominent in women and with high hemoglobin A1c (HbA1c) levels [3]. However, others have not observed increased GI symptoms in diabetes versus control populations [4]. Nausea and vomiting are predominant symptoms of diabetic gastroparesis in nearly half of patients [5]. In a recent study, nausea was reported by 96% of patients, which was exacerbated by meals in three quarters but was constantly experienced by roughly 40% [6]. Vomiting was reported by 80% with diabetic gastroparesis; vomiting relieved nausea in one quarter of patients. In a large, multicenter study from a National Institutes of Health (NIH) funded Gastroparesis Clinical Research Consortium (GpCRC) Registry, moderate to severe upper abdominal pain was present in two thirds of patients with gastroparesis and was predominant in 20% [5]. Pain- and nausea/vomiting-predominant patients reported similar negative effects on quality of life. Gastroparesis also is associated with impaired nutrition. In a large study, patients with gastroparesis consumed only 58% of recommended energy requirements and many individuals showed significant vitamin and mineral deficiencies [7].
The prevalence of delayed gastric emptying varies widely depending on testing methods, but is noted in up to 65% of T1DM and 30% of T2DM patients. Recently, analyses from the Epidemiology of Diabetes Interventions and Complications study demonstrated that delayed gastric emptying is seen in 47% of patients with T1DM after 20 years of follow-up even with intensive insulin therapy [8••]. In one population study, the incidence of developing gastroparesis was more than five-fold higher for T1DM versus T2DM (5.2 versus 1.0%) over 12 years [9].
Natural History and Prognosis
A recent longitudinal GpCRC study provided insight into the natural history of gastroparesis in T1DM and T2DM [10••]. Baseline symptom severity measured by the gastroparesis cardinal symptom index (GCSI) was similar in T1DM and T2DM (2.8 ± 1.1 vs. 3.0 ± 1.0, P = 0.28). However, on a 48-week follow-up, T2DM patients showed significant reductions in GCSI scores while symptoms did not improve in T1DM raising the question as to whether the gastric injury associated with this diabetic subtype is more irreversible in nature.
Hospitalizations from gastroparesis increased 158% from 1995 to 2004 with longer lengths of inpatient stay [11]. Another longitudinal study in patients with diabetes observed that delayed emptying was associated with higher morbidity and increased medical resource utilization compared with diabetic patients who had similar symptoms but normal gastric emptying [12]. One study reported reduced a 5-year survival in gastroparesis patients (67%) versus controls (81%), but others have not observed increased mortality [13, 14].
Normal Physiology of Gastric Emptying
Upon meal ingestion, the proximal stomach undergoes a vagally mediated reflex called accommodation which increases gastric volume with minimal rises in intraluminal pressure. Next, ingested food is subjected to trituration with grinding and mixing by high amplitude antral contractions which reduce particle size to < 1–2 mm to begin the process of gastric emptying. Emptying rates are influenced by meal volume, caloric content, and osmolarity; in particular, large, high-fat meals slow gastric emptying [15].
Gastric Physiologic Abnormalities in Diabetic Gastroparesis
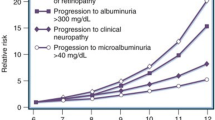
Several physiologic abnormalities are observed in diabetes. Although delayed emptying commonly is reported with longstanding disease, rapid gastric emptying is observed in early stages of diabetes [16]. Delayed gastric emptying is the cardinal finding of gastroparesis, but emptying rates show poor association with gastroparesis symptoms. In a GpCRC study of 319 diabetic and non-diabetic gastroparesis patients, GCSI scores did not correlate with 2- or 4-h gastric retention suggesting that other physiologic abnormalities are important in symptom pathogenesis [17]. Other defects are observed in diabetic patients with upper GI symptoms including blunting of fundic accommodation, hypersensitivity to gastric distention, gastric slow wave dysrhythmias, and increased tonic and phasic pyloric motor activity (Fig. 1) [18, 19].
Potential factors in the pathogenesis of symptoms in diabetic gastroparesis are shown. (1) Loss of gastric neurons containing NOS is responsible for defective accommodation reflex, leading to early satiety and postprandial fullness. (2) Impaired electromechanical activity in the myenteric plexus is responsible for delayed gastric emptying resulting in nausea and vomiting. (3) Sensory neuropathy in the gastric wall may be responsible for epigastric pain. (4) Abnormal pacemaker activity (tachybradyarrhythmia) may generate a noxious signal transmitted to the central nervous system to evoke nausea and vomiting. Reproduced with permission from reference [20].
Histopathologic Abnormalities
Traditionally, autonomic neuropathy has been considered the primary mechanism underlying diabetic gastroparesis. However, evidence from animal models and full-thickness gastric biopsies from gastroparesis patients indicates that other abnormalities may be more important. The most consistent findings in animal and human studies are reduced neuronal nitric oxide synthase (nNOS) expression, loss of interstitial cells of Cajal (ICC), and altered gastric macrophages.
Enteric Neuropathy
Animal models of diabetic gastroparesis show consistent nitrergic abnormalities including decreased nNOS immunoreactive cells in the gastric myenteric plexus, reduced nNOS expression, and impaired nitrergic-mediated gastric relaxation [20, 21]. In addition to serving as an inhibitory neurotransmitter, nitric oxide (NO) generated by nNOS promotes survival of ICCs [22].
Full-thickness gastric biopsies from patients with diabetic gastroparesis also exhibit significantly decreased nerve cell bodies compared to controls [23]. In a recent GpCRC study, gastric tissues from diabetic gastroparesis did not show differences in PGP9.5 (a marker of neurons) or nNOS-containing neurons versus control samples. However, ultrastructural changes were observed on electron microscopy, including loss of secretory vesicles in nerve terminals, possibly reflecting impaired neurotransmission.
Loss of Interstitial Cells of Cajal
ICCs are non-neuronal cells that generate rhythmic gastric slow waves and participate in neuromuscular transmission from enteric neurons to gastric smooth muscle. Mice with Kit gene mutations lack ICC and do not exhibit normal pacemaker activity [24]. In animal models, decreased antral ICCs are associated with impaired slow waves and delayed emptying [25]. ICC loss is the most common histologic abnormality in diabetic gastroparesis [26]. In a GpCRC study, 50% of diabetic gastroparesis patients exhibited reduced ICC numbers and nearly all showed structural changes to ICCs and the surrounding stroma under electron microscopy [27]. ICC loss is associated with slow-wave dysrhythmias in gastroparesis [28].
Altered Macrophage Populations
Mouse models suggest the importance of macrophages in developing gastroparesis. Resident macrophages in the muscularis propria are in close proximity to enteric nerves and ICCs [29]. Macrophages are polarized to classically activated pro-inflammatory M1 macrophages or anti-inflammatory M2 (CD206 positive) M2 macrophages [26]. In diabetic mice without gastric emptying delays, diabetes increased oxidative stress with subsequent upregulation of heme oxygenase 1 (HO1) expression in CD206+ M2 macrophages [21]. Conversely, mice with gastroparesis showed loss of HO1 upregulation, dropout of CD206+ M2 macrophages with increased M1 macrophages, ICC loss, and reduced nNOS expression [30]. Treatment of these diabetic mice with hemin to upregulate HO1 increased CD206+ M2 macrophages and normalized emptying delays.
Similar findings are reported in gastroparesis patients. Full-thickness gastric biopsies from diabetic gastroparesis show correlations between numbers of CD206+ cells and ICCs suggesting cytoprotection by CD206+ macrophages [31•]. However, an 8-week controlled trial of intravenous hemin did not improve gastric emptying or symptoms in a small group of diabetic gastroparesis patients [32].
Testing to Confirm Delayed Gastric Emptying
Measuring gastric emptying to make a diagnosis of gastroparesis is accomplished by gastric scintigraphy, gastric emptying breath testing (GEBT), or wireless motility capsule (WMC) testing. If possible, medications that influence gastric motility (e.g., opiates, anticholinergics, prokinetics) should be discontinued 72 h before testing. Some centers proceed with testing only when fasting glucose levels are < 275 mg/dL since hyperglycemia delays gastric emptying [33].
Gastric Scintigraphy
Scintigraphy is most commonly employed to quantify gastric emptying in the USA. A drawback of scintigraphy has been poor standardization of study protocols across centers which could influence test interpretation [34]. In 2008, the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine published consensus guidelines advocating measuring gastric retention at 1, 2, and 4 h after a 99mTc sulfur colloid-labeled egg-white meal with jam, toast, and water to provide a uniform method [34, 35]. Meal retention > 60% at 2 h and/or > 10% at 4 h is delayed and consistent with the diagnosis of gastroparesis. Simultaneous measurement of liquid emptying is sometimes performed which increases detection of emptying delays; the significance of isolated liquid emptying impairments is unknown [36].
Gastric Emptying Breath Testing
The GEBT involves ingesting a meal consisting of non-radioactive 13C bound to a substrate, either proteinaceous algae (Spirulina platensis) or medium-chain triglyceride (octanoate). The Spirulina platensis GEBT was FDA approved in the USA in 2015. Once emptied from the stomach, the substrate is metabolized and absorbed in the intestine and exhaled from the lungs as 13CO2, which is quantified on mass spectrometry. In a study comparing concurrent GEBT and scintigraphy in 38 healthy volunteers and 129 patients with suspected gastroparesis, delays in GEBT emptying were defined by t 1/2 > 86 min [37]. Using three time points (45, 150, and 180 min), GEBT showed a sensitivity of 93% and specificity of 80% to identify abnormal emptying. The two methods showed excellent correlation with Spearman correlations of − 0.82 (P < 0.001). GEBT advantages include lack of radiation exposure, standardized testing, and convenient performance in an outpatient office setting. The reliability of GEBT with intestinal, liver, pancreatic, or lung diseases requires validation.
Wireless Motility Capsule
The WMC measures 26 × 13 mm and has sensors that measure pH to identify the gut region, pressure to provide an estimate of contractility, and temperature to detect body exit. The WMC was FDA approved in 2006 to measure gastric emptying in suspected gastroparesis, but also can determine small bowel and colon transit. WMC gastric emptying times > 5 h measured by detecting > 2–3 pH unit increases as the capsule passes from the antrum into the duodenum are delayed. In a study of simultaneous testing in 61 patients with gastroparesis and 87 healthy subjects, the correlation of scintigraphic 4-h retention > 10% and WMC emptying time > 5 h was 0.73 and sensitivity and specificity for detecting emptying delays were 0.65 and 0.87, respectively [38]. In a GpCRC study of 209 patients, gastroparesis symptoms correlated poorly with emptying rates as well as other transit parameters [39]. Extragastric delays were demonstrated in the small bowel in 16%, colon in 34%, and multiple gut regions in 23% of patients with suspected gastroparesis. WMC advantages include lack of radiation exposure and the ambulatory nature of the test. WMC test results are reported to influence clinical management in retrospective series [40]. Because of its size, WMC testing is contraindicated with dysphagia or suspected bowel obstruction.
Therapy
Treating diabetic gastroparesis includes dietary modifications, avoiding medications that worsen symptoms, stricter glycemic control, drug therapies in several classes, and endoscopic and surgical options.
Dietary Management
Dietary modification is a cornerstone of therapy for diabetic gastroparesis. Frequent, small meals, low in fat and fiber, with liquid predominance are preferred. A recent challenge study indicated that high-fat meals elicit worse symptoms than low-fat foods [41]. Preliminary research from the GpCRC suggests that meals high in fermentable carbohydrates are associated with worse pain in gastroparesis [42]. When queried on a standardized survey, gastroparesis patients identify fatty, acidic, spicy, and roughage-based foods as exacerbating their symptoms while bland, sweet, salty, and starchy foods are tolerable (Table 1) [43]. In the only controlled diet trial in diabetic gastroparesis (N = 56), nausea, vomiting, fullness, and bloating decreased more on a small particle diet versus a control diet over 20 weeks [44••].
Avoiding Offending Medications
Medications that elicit nausea and vomiting or delay emptying, including opiates, should be avoided in diabetic gastroparesis if possible. Some agents that treat diabetes may contribute to symptoms in gastroparesis. Amylin analogs (e.g., pramlintide) and glucagon-like peptide 1 analogs (e.g., exenatide, liraglutide) delay emptying and cause nausea in roughly one quarter of patients [45, 46]. However, dipeptidyl peptidase IV inhibitors (e.g., sitagliptin, vildagliptin) do not impair emptying and rarely cause nausea. Among immunosuppressants potentially taken by patients with renal or pancreas transplants, calcineurin inhibitors (e.g., cyclosporine A) but not other agents (e.g., tacrolimus, mycophenylate) slow emptying.
Glucose Control
Optimizing glycemic control is recommended in diabetic gastroparesis as acute hyperglycemia delays gastric emptying and reduces fundic tone, increases gastric sensitivity to distention, disrupts slow wave rhythm, and causes spastic pyloric contractions [33, 47, 48, 49]. In 78 T1DM patients followed over 20 years, emptying delays were associated with higher HbA1c levels [8••].
Evidence suggests that improving glycemic control may improve manifestations of diabetic gastroparesis. In 30 T2DM patients, improving glucose control with oral agents only (12 patients), insulin only (12 patients), lifestyle changes (2 patients), or other regimens (4 patients) had no effect on gastric emptying [50]. However, HbA1c levels decreased only from 10.6 to 9.0% suggesting this approach may not have been aggressive enough. In 26 subjects with poorly controlled diabetes, insulin pump therapy reduced median yearly hospitalizations from 8.5 to 0 days [51]. Most recently in preliminary GpCRC data in 45 patients with poorly controlled T1DM or T2DM and gastroparesis, combined insulin pump therapy with continuous glucose monitoring for 24 weeks did not increase hypoglycemia, lowered HbA1c levels 1.1%, and reduced gastroparesis symptoms 22% [52].
Prokinetics
By virtue of their ability to accelerate gastric emptying, prokinetic drugs have been considered first-line agents for diabetic gastroparesis.
Metoclopramide
Metoclopramide is the only medication FDA approved for gastroparesis. It has prokinetic action as a peripheral dopamine (D2) antagonist and 5-hydroxytryptamine (5-HT4) agonist, and has antiemetic effects as an antagonist on central D2 and 5-HT3 receptors. Metoclopramide is available as an oral tablet, oral dissolution tablet, liquid solution, and parenteral formulation. Metoclopramide improved symptoms and accelerated emptying in four randomized controlled trials (RCTs) and two active, short-duration (≤ 4 week) comparator-controlled trials [53]. Three small (≤ 12 subjects), open-label studies did not support long-term (> 3 weeks) metoclopramide use. Recently, an intranasal metoclopramide formulation which can be taken even when the patient is vomiting produced superior symptom reductions versus oral tablets but improved gastroparesis symptom scores only in women in a phase 2b RCT (Table 2) [54, 55].
Because it crosses the blood-brain barrier, metoclopramide elicits prominent extrapyramidal manifestations. In one study, 95% of 479 metoclopramide extrapyramidal side effects were acute dystonia, 4% were parkinsonian movements, and 1% represented tardive dyskinesia (TD) which may be irreversible [56]. TD risks appear to be greatest in patients > 70 years old, on doses > 30 mg/day, and on long-term therapy (> 20 months) [57]. Because of concerns, the FDA issued a black-box warning on metoclopramide in 2009. In 2013, it was estimated this recommendation reduced prescription rates for metoclopramide from 70 to 24% of gastroparesis patients [58]. Current guidelines recommend metoclopramide use for ≤ 12 weeks at the lowest dose, careful side effect surveillance, and consideration of drug holidays.
Domperidone
Domperidone is a peripheral D2 antagonist with both prokinetic and antiemetic effects. The drug is available as oral tablets and orally dissolving tablets. Domperidone efficacy in diabetic gastroparesis was evaluated in 6 RCTs and several open-label studies [53]. In four RCTs, domperidone showed benefit over placebo or baseline symptoms and was equivalently effective as metoclopramide. Small, uncontrolled series report symptom reductions up to 6 months. A systematic review of 11 articles and 17 abstracts found that domperidone improved symptoms in diabetic gastroparesis in 64% and gastric emptying in 60% [59]. However, methodologic concerns were raised and the authors concluded there is only level 3 evidence supporting domperidone use in diabetic gastroparesis.
Because of its limited penetrance of the blood-brain barrier, domperidone has minimal central nervous system side effects. However, domperidone can prolong the QT interval and promote ventricular arrhythmias. Two large case-control studies suggest that doses > 30 mg/day and age > 60 years increase the risk of sudden cardiac death [60, 61]. Domperidone is not FDA approved but is available to clinicians who submit an Investigational New Drug application to the FDA and obtain approval from their local Institutional Review Board. Current guidelines recommend that a baseline electrocardiogram (EKG) be obtained before starting domperidone and withholding the medication if the corrected QT interval is > 450 msec in men and > 470 msec in women. EKGs are repeated every 2 months for 1 year and every 6 months thereafter and more frequently if domperidone doses are increased or if other drugs are started that interact with domperidone.
Erythromycin
Erythromycin is a motilin agonist that elicits intense gastroduodenal contractions that mimic fasting migrating motor complexes and potently accelerate gastric emptying. It is available as oral tablets, liquid suspension, or intravenous infusion. Similar prokinetic benefits are observed with azithromycin [62]. A systematic review identified three studies that assessed oral erythromycin in diabetic and/or idiopathic gastroparesis and two postsurgical gastroparesis studies [63]. Overall, 43% reported symptom reductions although emptying improvements were the primary endpoint in all studies. The authors concluded that the evidence for erythromycin benefit in gastroparesis was limited due to small samples, short-study durations (≤ 4 weeks), inadequate symptom assessments, and uncontrolled study designs. Chronic erythromycin use is limited by tachyphylaxis likely from motilin receptor downregulation.
Erythromycin elicits significant GI side effects including abdominal pain, nausea, and vomiting which may limit use in diabetic gastroparesis. The drug also prolongs QT intervals and is associated with a twofold increased risk of sudden cardiac death versus prior erythromycin or current amoxicillin users [64]. This risk is increased in those also taking CYP3A inhibitors, such as antifungal drugs (e.g., fluconazole) and calcium channel blockers (e.g., diltiazem, verapamil). Given this risk, it is reasonable to consider EKG surveillance when prescribing erythromycin. Drug holidays may be recommended to permit motilin receptor upregulation.
Other Prokinetics
Other prokinetics have not been studied in diabetic gastroparesis, but are sometimes considered for patients unresponsive to other drugs. The acetylcholinesterase inhibitor pyridostigmine improved symptoms in a small series of patients with autoimmune dysmotility [65]. In a preliminary RCT, the 5-HT4 agonist prucalopride reduced symptoms in 28 idiopathic gastroparesis patients (Table 2 ) [66]. This medication is approved for chronic constipation in Europe and Canada.
Antiemetics
Antiemetics without prokinetic capability are frequently prescribed for diabetic gastroparesis, with limited evidence to support this practice.
Traditional Antiemetics
Antiemetics act on diverse receptor subtypes in several classes including antihistamines (e.g., promethazine, dimenhydrinate), antidopaminergics (e.g., prochlorperazine), anticholinergics (e.g., transdermal scopolamine), and 5-HT3 antagonists (e.g., ondansetron). Other than case reports, none of these agents have been studied in diabetic gastroparesis. However, two recent open-label studies of transdermal granisetron, a 5-HT3 antagonist, reported improvements in 18 of 36 patients with gastroparesis (50%) in the first investigation and 39 of 51 patients (76%) in the second (Table 2 ) [67, 68•].
Cannabinoids (e.g., dronabinol) acting on cannabinoid receptor type 1 (CB1) and type 2 (CB2) have orexigenic and antiemetic effects with theoretical benefits in gastroparesis. A systematic review of > 30 RCTs found that cannabinoids relieved nausea and vomiting from chemotherapy better than placebo or other antiemetics (e.g., prochlorperazine, metoclopramide, chlorpromazine, triethylperazine, haloperidol, domperidone, alizapride) (NNT = 6 for complete control of nausea, NNT = 7 for complete control of vomiting), but commonly elicited side effects including dizziness, dysphoria, hallucinations, and paranoia [69]. As chronic marijuana use has been associated with a cyclic vomiting syndrome variant (cannabinoid hyperemesis syndrome), some urged caution when prescribing cannabinoid pharmaceutical agents in gastroparesis [70].
Neurokinin-1 Receptor Antagonists
Neurokinin (NK1) antagonists (e.g., aprepitant) are potent antiemetic agents approved for chemotherapy-induced and postoperative nausea and vomiting that may be useful for refractory gastroparesis. A small number of case reports have suggested that aprepitant reduces nausea and vomiting in gastroparesis cases unresponsive to other antiemetic drugs [71]. A recent 4-week controlled GpCRC trial in 126 patients with symptoms of gastroparesis found no difference between aprepitant (46%) and placebo (40%) in achieving the primary endpoint of reducing nausea by ≥ 25 mm or achieving absolute nausea level of < 25 mm on a 100-mm visual analog scale (Table 2) [72••]. However, secondary outcomes (GCSI nausea scores, percent of nausea free days, daily hours of nausea, overall symptoms) all improved more on aprepitant than placebo suggesting potential benefits of this drug class. This represents the first RCT of an antiemetic medication in gastroparesis.
Neuromodulators
Neuromodulators are medications proposed to reduce gastroparesis symptoms by blunting gastric sensory nerve function. Although no RCTs have been conducted in diabetic gastroparesis, the drugs show promise in related conditions.
Tricyclic antidepressants
Tricyclic antidepressants (TCAs) have been proposed as neuromodulators in several GI disorders. In a retrospective study of 24 diabetic patients with nausea and vomiting unresponsive to prokinetics, 77% reported at least moderate improvement with TCAs and 68% stated that TCAs were the most effective treatment they received [73]. However, enthusiasm for TCAs for treating gastroparesis waned after the 15-week controlled nortriptyline for idiopathic gastroparesis (NORIG) trial in 130 idiopathic gastroparesis patients which reported no difference in GCSI improvements on nortriptyline up to 75 mg daily versus placebo [74]. Furthermore, another controlled trial in functional dyspepsia reported superior responses to amitriptyline versus placebo and the selective serotonin reuptake inhibitor escitalopram, but subgroup analysis revealed a lack of efficacy in patients with delayed gastric emptying [75].
Mirtazapine
Mirtazapine is a tetracyclic antidepressant acting as an antagonist on histamine H1, α2 adrenergic, and serotonin 5-HT2C and 5-HT3 receptors. In an 8-week controlled trial in 34 functional dyspepsia patients, mirtazapine 15 mg daily improved symptoms, including early satiation, weight gain, GI-specific anxiety, and overall quality of life versus placebo and improved tolerance of a liquid nutrient challenge [76].
Olanzapine
Olanzapine is an antipsychotic with antagonism on dopamine D1, D2, D3, D4, serotonin 5-HT2a, 5-HT2c, 5-HT3, 5-HT6, and histamine H1 receptors. In a controlled phase 3 trial of 380 patients, olanzapine improved nausea prevention after cancer chemotherapy when given in combination with dexamethasone, a neurokinin-1 receptor antagonist, and a 5-HT3 receptor antagonist [77]. Sedation was the most common side effect (severe in 5%).
Endoscopic and Surgical Treatments
Several non-pharmacologic options are available for diabetic gastroparesis patients unresponsive to or intolerant of medication therapy.
Pyloric Botulinum Toxin Injection
Intrapyloric botulinum toxin injection is performed as therapy for presumed increases in pyloric tonic and phasic contractility in diabetic gastroparesis. Several open-label studies reported symptom and emptying improvements in gastroparesis with botulinum toxin injection, including one large 179 patient series that identified 200 unit dosing, female sex, age < 50 years, and idiopathic etiology as predictors of response [53, 78]. However, two small, underpowered, controlled trials did not show symptom or emptying benefits of botulinum toxin [79, 80]. Consequently, clinical guidelines have not supported this treatment for gastroparesis. Investigators are evaluating utility of functional lumen imaging probes (EndoFLIP) which measure distensibility using impedance planimetry to determine if patients with stiffer pyloric walls respond better to therapies such as botulinum toxin [81•].
Gastric Per Oral Endoscopic Myotomy (G-POEM)
G-POEM is a new technique involving endoscopic performance of pyloromyotomy via a submucosal tunnel that has gained attention as an alternative therapy of pylorospasm. Case series of 14 to 30 patients report 70–86% responses up to 6 months after G-POEM including symptom reductions and emptying acceleration (Table 2) [82, 83, 84•]. Additional long-term study is warranted as its presumed mechanism is similar to botulinum toxin, which also was enthusiastically promoted in early reports.
Gastric Electrical Stimulation
Gastric electrical stimulation with high frequency, low energy pulses may modulate vagal afferent transmission leading to decreased symptoms in gastroparesis. A misconception is that the device is a pacemaker as gastric stimulators do not affect gastric emptying or slow waves. Several uncontrolled series have reported benefits of stimulation, including reduced symptoms, improved glycemic control, enhanced quality of life, and reduced resource utilization. These series also have defined predictors of poor response including idiopathic gastroparesis etiology, predominant pain instead of vomiting, and chronic opiate use [85]. The FDA-approved gastric stimulation as a humanitarian use device (HUD) in 2000.
Three-blinded, sham-controlled trials of gastric stimulation have been published. In the first study in 33 patients (17 diabetic), gastric stimulation reduced weekly vomiting frequencies mainly in diabetics during active but not sham stimulation although total symptoms did not benefit from therapy [86]. Subsequent blinded controlled studies in diabetic (n = 55) and idiopathic (n = 32) patients did not observe greater reductions in weekly vomiting frequencies or other symptoms during active versus sham stimulation, calling into question the efficacy of the method [87, 88]. However, recent large preliminary studies offer more convincing evidence for its benefits in gastroparesis. In a 48-week follow-up report of 634 gastroparesis patients from the GpCRC, the 92 patients (38% diabetic) who underwent stimulator implantation exhibited superior reductions in GCSI scores versus 542 patients managed medically [89]. Although patients who underwent stimulator surgery had higher symptoms and slower emptying at baseline, propensity score matching after adjusting for these baseline differences confirmed the benefits of gastric stimulation with an odds ratio of 2.35. Most recently in a blinded, multicenter French study of 172 patients with diabetic or idiopathic gastroparesis, vomiting scores during 4 months of active stimulation were lower than during sham stimulation [90].
Other Surgical Therapies
Other operations have shown efficacy in uncontrolled series of refractory gastroparesis. Retrospective studies in 26 and 42 patients undergoing laparoscopic pyloroplasty reported improved symptoms and emptying with lesser prokinetic medication needs when followed for 1–12 months [91, 92]. Similarly, case series of 31 and 35 patients (34% diabetics) reported 69–87% symptom reductions after subtotal or completion gastrectomy when followed for up to 1 year [93, 94]. These optimistic observations warrant confirmation in prospective studies using validated outcomes.
Investigational Therapies
Prokinetic medications in several classes are in testing for treating gastroparesis.
Ghrelin Receptor Agonists
Ghrelin is an orexigenic signal, inhibits glucose-induced insulin release and has prokinetic effects via action on the growth hormone secretagogue-1a receptor. Several long-acting synthetic ghrelin agonists have been proposed for diabetic gastroparesis. Relamorelin is a novel pentapeptide agonist with 100-fold higher potency than human ghrelin in accelerating gastric emptying in animal models of ileus. In a recent 4-week phase 2a trial of 204 diabetic gastroparesis patients, twice daily subcutaneous relamorelin 10 μg improved emptying and reduced vomiting frequency versus placebo (Table 2) [95•]. Patients with baseline vomiting exhibited additional reductions in nausea, abdominal pain, bloating, and early satiety. A preliminary 12-week phase 2b trial in 393 diabetic gastroparesis patients reported reductions in key symptoms of nausea, fullness, abdominal pain, and bloating with associated emptying acceleration [96]. Phase 3 trials are ongoing to confirm benefits of this agent.
5-HT4 Receptor Agonists
5-HT4 agonists like cisapride were used in diabetic gastroparesis, but were withdraw because of the potential for dangerous cardiac dysrhythmias due to antagonism of the human ether-a-go-go related gene [97]. Newer agents without adverse cardiac events, like velusetrag, show greater 5-HT4 receptor selectively and specificity. In a preliminary phase 2a trial, 34 subjects with diabetic or idiopathic gastroparesis showed improved emptying on daily velusetrag 30 mg versus placebo (Table 2 ) [98]. A phase 2b trial is underway.
Motilin Receptor Agonists
Camicinal is a long-acting, non-peptide motilin agonist with gastric prokinetic effects which may exhibit less tachyphylaxis versus erythromycin. In a 28-day controlled phase 2 study, 79 diabetic gastroparesis patients showed minimal emptying acceleration but improved fullness and early satiety at the 10 and 50 mg daily doses of camicinal versus placebo but acceleration of gastric emptying only at the 125 mg dose emphasizing the inconsistent relationship between prokinetic and symptom responses to therapy (Table 2 ) [99].
Conclusions
Our understanding of diabetic gastroparesis pathophysiology has increased with work by the GpCRC and others. It remains uncertain whether treatments should focus on symptoms or focus on accelerating emptying or correcting other physiologic abnormalities. Some important symptoms (e.g., pain), are unaddressed despite their prevalence and severity. A preliminary draft FDA guidance document advocates using patient-reported outcome measures comprised of the five cardinal symptoms of gastroparesis (nausea, vomiting, fullness, bloating, and pain) with quantification of prokinetic effects on gastric emptying reserved as secondary endpoints (www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM455645.pdf). This offers promise of standardized trial guidelines that will accelerate new drug development in diabetic gastroparesis.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kassander P. Asymptomatic gastric retention in diabetics (gastroparesis diabeticorum). Ann Intern Med. 1958;48:797–812.
Bytzer P, Talley NJ, Leemon M, Young LJ, Jones MP, Horowitz M. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161:1989–96.
Schvarcz E, Palmér M, Ingberg CM, Aman J, Berne C. Increased prevalence of upper gastrointestinal symptoms in long-term type 1 diabetes mellitus. Diabet Med. 1996;13:478–81.
Maleki D, Locke GR, Camilleri M, Zinsmeister AR, Yawn BP, Leibson C, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Arch Intern Med. 2000;160:2808–16.
Hasler WL, Wilson LA, Parkman HP, Koch KL, Abell TL, Nguyen L, et al. Factors related to abdominal pain in gastroparesis: contrast to patients with predominant nausea and vomiting. Neurogastroenterol Motil. 2013;25:427–38.
Parkman HP, Hallinan EK, Hasler WL, Farrugia G, Koch KL, Calles J, et al. Nausea and vomiting in gastroparesis: similarities and differences in idiopathic and diabetic gastroparesis. Neurogastroenterol Motil. 2016;28:1902–14.
Parkman HP, Yates KP, Hasler WL, Nguyen L, Pasricha PJ, Snape WJ, et al. Dietary intake and nutritional deficiencies in patients with diabetic or idiopathic gastroparesis. Gastroenterology. 2011;141:486–98.
•• Bharucha AE, Batey-Schaefer B, Cleary PA, Murray JA, Cowie C, Lorenzi G, et al. Delayed gastric emptying is associated with early and long-term hyperglycemia in type 1 diabetes mellitus. Gastroenterology. 2015;149:330–9. This investigation assessed gastric emptying using breath testing in 78 patients with type 1 diabetes from the original Diabetes Control and Complications Trial and showed worse gastric emptying delays in those with early and long-term hyperglycemia. This represents the best article correlating emptying defects with glycemic control in diabetes
Choung RS, Locke GR, Schleck CD, Zinsmeister AR, Melton LJ, Talley NJ. Risk of gastroparesis in subjects with type 1 and 2 diabetes in the general population. Am J Gastroenterol. 2012;107:82–8.
•• Koch KL, Hasler WL, Yates KP, Parkman HP, Pasricha PJ, Calles-Escandon J, et al. Baseline features and differences in 48 week clinical outcomes in patients with gastroparesis and type 1 vs type 2 diabetes. Neurogastroenterol Motil. 2016;28:1001–15. This evaluation of diabetic patients from the GpCRC shows that, although T1DM and T2DM patients report similar symptoms at baseline, only T2DM patients experience symptom improvements over 48 weeks of follow-up. This study represents the most comprehensive short term natural history report in diabetic gastroparesis
Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States: trends, characteristics, and outcomes, 1995-2004. Am J Gastroenterol. 2008;103:313–22.
Hyett B, Martinez FJ, Gill BM, Mehra S, Lembo A, Kelly CP, et al. Delayed radionucleotide gastric emptying studies predict morbidity in diabetics with symptoms of gastroparesis. Gastroenterology. 2009;137:445–52.
Jung H, Choung RS, Locke I, Schleck CD, Zinsmeister AR, Szarka LA, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136:1225–33.
Chang J, Rayner CK, Jones KL, Horowitz M. Prognosis of diabetic gastroparesis—a 25-year evaluation. Diabet Med. 2013;30:e185–8.
Camilleri M. Integrated upper gastrointestinal response to food intake. Gastroenterology. 2006;131:640–58.
Phillips WT, Schwartz JG, McMahan CA. Rapid gastric emptying in patients with early non-insulin-dependent diabetes mellitus. N Engl J Med. 1991;324:130–1.
Pasricha PJ, Colvin R, Yates K, Hasler WL, Abell TL, Unalp-Arida A, et al. Characteristics of patients with chronic unexplained nausea and vomiting and normal gastric emptying. Clin Gastroenterol Hepatol. 2011;9:567–76.
Hasler WL, Li BU, Koch KL, Parkman HP, Kovacic K, McCallum RW. Methodologic considerations for studies of chronic nausea and vomiting in adults and children. Auton Neurosci. 2017;202:28–39.
Owyang C. Phenotypic switching in diabetic gastroparesis: mechanism directs therapy. Gastroenterology. 2011;141:1134–7.
Takahashi T, Nakamura K, Itoh H, Sima A, Owyang C. Impaired expression of nitric oxide synthase in the gastric myenteric plexus of spontaneously diabetic rats. Gastroenterology. 1997;113:1535–44.
Choi KM, Gibbons SJ, Nguyen TV, Stoltz GJ, Lurken MS, Ordog T, et al. Heme oxygenase-1 protects interstitial cells of Cajal from oxidative stress and reverses diabetic gastroparesis. Gastroenterology. 2008;135:2055–64.
Choi KM, Gibbons SJ, Roeder JL, Lurken MS, Zhu J, Wouters MM, et al. Regulation of interstitial cells of Cajal in the mouse gastric body by neuronal nitric oxide. Neurogastroenterol Motil. 2007;19:585–95.
Faussone-Pellegrini MS, Grover M, Pasricha PJ, Bernard CE, Lurken MS, Smyrk TC, et al. Ultrastructural differences between diabetic and idiopathic gastroparesis. J Cell Mol Med. 2012;16:1573–81.
Hulzinga JD, Thuneberg L, Klüppel M, Malysz J, Mikkelsen HB, Bernstein A. W/kit gene required for interstitial cells of Cajal and for intestinal pacemaker activity. Nature. 1995;373:347–9.
Wang X, Huizinga JD, Diamond J, Liu LW. Loss of intramuscular and submuscular interstitial cells of Cajal and associated enteric nerves is related to decreased gastric emptying in streptozotocin-induced diabetes. Neurogastroenterol Motil. 2009;21:1095–e92.
Farrugia G. Histological changes in diabetic gastroparesis. Gastroenterol Clin N Am. 2015;44:31–8.
Grover M, Farrugia G, Lurken MS, Bernard CE, Faussone-Pellegrini MS, Smyrk TC, et al. Cellular changes in diabetic and idiopathic gastroparesis. Gastroenterology. 2011;140:1575–85.
O’Grady G, Angeli TR, Du P, Lahr C, Lammers WJ, Windsor JA, et al. Abnormal initiation and conduction of slow-wave activity in gastroparesis, defined by high-resolution electrical mapping. Gastroenterology. 2012;143:589–98.
Muller PA, Koscsó B, Rajani GM, Stevanovic K, Berres M-L, Hashimoto D, et al. Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell. 2014;158:300–13.
Choi KM, Kashyap PC, Dutta N, Stoltz GJ, Ordog T, Donohue TS, et al. CD206-positive M2 macrophages that express heme oxygenase-1 protect against diabetic gastroparesis in mice. Gastroenterology. 2010;138:2399–409.
• Bernard C, Gibbons SJ, Mann IS, Froschauer L, Parkman HP, Harbison S, et al. Association of low numbers of CD206-positive cells with loss of ICC in the gastric body of patients with diabetic gastroparesis. Neurogastroenterol Motil. 2014;26:1275–84. This histopathologic evaluation of full-thickness gastric biopsies from diabetic gastroparesis patients shows a strong correlation of decreased ICC numbers with loss of CD206+ M2 macrophages. This study presents novel information on the possible pathogenesis of diabetic gastroparesis
Bharucha AE, Daley SL, Low PA, Gibbons SJ, Choi KM, Camilleri M, et al. Effects of hemin on heme oxygenase-1, gastric emptying, and symptoms in diabetic gastroparesis. Neurogastroenterol Motil. 2016;28:1731–40.
Fraser RJ, Horowitz M, Maddox AF, Harding PE, Chatterton BE, Dent J. Hyperglycaemia slows gastric emptying in type 1 (insulin-dependent) diabetes mellitus. Diabetologia. 1990;33:675–80.
Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–63.
Tougas G, Eaker EY, Abell TL, Abrahamsson H, Boivin M, Chen J, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–62.
Sachdeva P, Malhotra N, Pathikonda M, Khayyam U, Fisher RS, Maurer AH, et al. Gastric emptying of solids and liquids for evaluation for gastroparesis. Dig Dis Sci. 2011;56:1138–46.
Szarka LA, Camilleri M, Vella A, Burton D, Baxter K, Simonson J, et al. A stable isotope breath test with a standard meal for abnormal gastric emptying of solids in the clinic and in research. Clin Gastroenterol Hepatol. 2008;6:635–43.
Kuo B, McCallum RW, Koch KL, Sitrin MD, Wo JM, Chey WD, et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment Pharmacol Ther. 2008;27:186–96.
Hasler WL, May KP, Wilson LA, Van Natta M, Parkman HP, Pasricha PJ, et al. Relating gastric scintigraphy and symptoms to motility capsule transit and pressure findings in suspected gastroparesis. Neurogastroenterol Motil. 2017 (In press).
Kuo B, Maneerattanaporn M, Lee AA, Baker JR, Wiener SM, Chey WD, et al. Generalized transit delay on wireless motility capsule testing in patients with clinical suspicion of gastroparesis, small intestinal dysmotility, or slow transit constipation. Dig Dis Sci. 2011;56:2928–38.
Homko CJ, Duffy F, Friedenberg FK, Boden G, Parkman HP. Effect of dietary fat and food consistency on gastroparesis symptoms in patients with gastroparesis. Neurogastroenterol Motil. 2015;27:501–8.
Hasler WL, Belt P, Wilson L, McCallum RW, Parkman HP, Koch KL, et al. Correlation of fermentable carbohydrate consumption with symptoms and quality of life in patients with diabetic and idiopathic gastroparesis (abstract). Gastroenterology. 2014;146:S-610.
Wytiaz V, Homko C, Duffy F, Schey R, Parkman HP. Foods provoking and alleviating symptoms in gastroparesis: patient experiences. Dig Dis Sci. 2015;60:1052–8.
•• Olausson EA, Störsrud S, Grundin H, Isaksson M, Attvall S, Simrén M. A small particle size diet reduces upper gastrointestinal symptoms in patients with diabetic gastroparesis: a randomized controlled trial. Am J Gastroenterol. 2014;109:375–85. As the only published controlled diet trial in diabetic gastroparesis, these findings provide strong support for consuming a small particle diet with predominantly low residue foods to improve symptoms in this condition
Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705.
Trujillo JM, Nuffer W, Ellis SL. GLP-1 receptor agonists: a review of head-to-head clinical studies. Ther Adv Endocrinol Metab. 2015;6:19–28.
Hebbard GS, Samsom M, Sun WM, Dent J, Horowitz M. Hyperglycemia affects proximal gastric motor and sensory function during small intestinal triglyceride infusion. Am J Phys. 1996;271:G814–9.
Hasler WL, Soudah HC, Dulai G, Owyang C. Mediation of hyperglycemia-evoked gastric slow-wave dysrhythmias by endogenous prostaglandins. Gastroenterology. 1995;108:727–36.
Fraser R, Horowitz M, Dent J. Hyperglycaemia stimulates pyloric motility in normal subjects. Gut. 1991;32:475–8.
Bharucha AE, Kudva Y, Basu A, Camilleri M, Low PA, Vella A, et al. Relationship between glycemic control and gastric emptying in poorly controlled type 2 diabetes. Clin Gastroenterol Hepatol. 2015;13:466–76.
Sharma D, Morrison G, Joseph F, Purewal TS, Weston PJ. The role of continuous subcutaneous insulin infusion therapy in patients with diabetic gastroparesis. Diabetologia. 2011;54:2768–70.
Calles-Escandon J, Van Natta ML, Koch KL, Hasler WL, Tonascia J, Parkman HP, et al. Pilot study of the safety, feasibility, and efficacy of continuous glucose monitoring (CGM) and insulin pump therapy in diabetic gastroparesis (GLUMIT-DG): a multicenter, longitudinal trial by the NIDDK Gastroparesis Clinical Research Consortium (GPCRC)(abstract). Gastroenterology. 2015;148:S-64.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108:18–38.
Parkman HP, Carlson MR, Gonyer D. Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet. Neurogastroenterol Motil. 2014;26:521–8.
• Parkman HP, Carlson MR, Gonyer D. Metoclopramide nasal spray reduces symptoms of gastroparesis in women, but not men, with diabetes: results of a phase 2b randomized study. Clin Gastroenterol Hepatol. 2015;13:1256–63. This is a large RCT of a new metoclopramide nasal spray in diabetic gastroparesis which demonstrated symptom benefits which were restricted to women
Bateman DN, Rawlins MD, Simpson JM. Extrapyramidal reactions with metoclopramide. Br Med J (Clin Res Ed). 1985;291:930–2.
Lee A, Kuo B. Metoclopramide in the treatment of diabetic gastroparesis. Expert Rev Endocrinol Metab. 2010;5:653–62.
Ehrenpreis ED, Deepak P, Sifuentes H, Devi R, Du H, Leikin JB. The metoclopramide black box warning for tardive dyskinesia: effect on clinical practice, adverse event reporting, and prescription drug lawsuits. Am J Gastroenterol. 2013;108:866–72.
Sugumar A, Singh A, Pasricha PJ. A systematic review of the efficacy of domperidone for the treatment of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2008;6:726–33.
Noord C, Dieleman JP, Herpen G, Verhamme K, Sturkenboom IC. Domperidone and ventricular arrhythmia or sudden cardiac death. Drug Saf. 2010;11:1003–14.
Johannes CB, Varas-Lorenzo C, McQuay LJ, Midkiff KD, Fife D. Risk of serious ventricular arrhythmia and sudden cardiac death in a cohort of users of domperidone: a nested case-control study. Pharmacoepidemiol Drug Saf. 2010;19:881–8.
Potter TG, Snider KR. Azithromycin for the treatment of gastroparesis. Ann Pharmacother. 2013;47:411–5.
Maganti K, Onyemere K, Jones MP. Oral erythromycin and symptomatic relief of gastroparesis: a systematic review. Am J Gastroenterol. 2003;98:259–63.
Ray WA, Murray KT, Meredith S, Narasimhulu SS, Hall K, Stein CM. Oral erythromycin and the risk of sudden death from cardiac causes. N Engl J Med. 2004;351:1089–96.
Pasha SF, Lunsford TN, Lennon VA. Autoimmune gastrointestinal dysmotility treated successfully with pyridostigmine. Gastroenterology. 2006;131:1592–6.
Carbone F, Rotondo A, Andrews CN, Holvoet L, Van Oudenhove L, Vanuytsel T, et al. A controlled cross-over trial shows benefit of prucalopride for symptom control and gastric emptying enhancement in idiopathic gastroparesis (abstract). Gastroenterology. 2016;150:S-213-4.
Simmons K, Parkman HP. Granisetron transdermal symptoms improves refractory nausea and vomiting in gastroparesis. Dig Dis Sci. 2014;59:1231–4.
• Midani D, Parkman HP. Granisetron transdermal system for treatment of symptoms of gastroparesis: a prescription registry study. J Neurogastroenterol Motil. 2016;22:650–5. This open-label study provided support for use of the transdermal granisetron patch in gastroparesis showing symptom benefits in three quarters of patients
Tramèr MR, Carroll D, Campbell FA, Reynolds DJ, Moore RA, McQuay HJ. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. BMJ. 2001;323:16–21.
Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, et al. Gastroduodenal disorders. Gastroenterology. 2016;150:1380–92.
Fahler J, Wall GC, Leman BI. Gastroparesis-associated refractory nausea treated with aprepitant. Ann Pharmacother. 2012;46:e38.
•• Pasricha PJ, Yates KP, Sarosiek I, McCallum RW, Abell TL, Koch KL, et al. Aprepitant for nausea relief in patients with gastroparesis and related disorders: the APRON randomized clinical trial. Gastroenterology. 2017 (In press)This recently published study represents the only placebo-controlled trial demonstrating effectiveness of an antiemetic medication in relieving symptoms of gastroparesis
Sawhney MS, Prakash C, Lustman PJ, Clouse RE. Tricyclic antidepressants for chronic vomiting in diabetic patients. Dig Dis Sci. 2007;52:418–24.
Parkman HP, Van Natta ML, Abell TL, McCallum RW, Sarosiek I, Nguyen L, et al. Effect of nortriptyline on symptoms of idiopathic gastroparesis: the NORIG randomized clinical trial. JAMA. 2013;310:2640–9.
Talley NJ, Locke GR, Saito YA, Almazar AE, Bouras EP, Howden CW, et al. Effect of amitriptyline and escitalopram on functional dyspepsia: a multicenter, randomized controlled study. Gastroenterology. 2015;149:340–9.
Tack J, Ly HG, Carbone F, Vanheel H, Vanuytsel T, Holvoet L, et al. Efficacy of mirtazapine in patients with functional dyspepsia and weight loss. Clin Gastroenterol Hepatol. 2016;14:385–92.
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, et al. Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;375:134–42.
Coleski R, Anderson MA, Hasler WL. Factors associated with symptom response to pyloric injection of botulinum toxin in a large series of gastroparesis patients. Dig Dis Sci. 2009;54:2634–42.
Arts J, Holvoet L, Caenepeel P, Bisschops R, Sifrim D, Verbeke K, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26:1251–8.
Friedenberg FK, Palit A, Parkman HP, Hanlon A, Nelson DB. Botulinum toxin A for the treatment of delayed gastric emptying. Am J Gastroenterol. 2008;103:416–23.
• Gourcerol G, Tissier F, Melchior C, Touchais JY, Huet E, Prevost G, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41:360–7. Using EndoFLIP methods, this study observed reduced fasting pyloric compliance in patients with gastroparesis which related to worse gastric emptying impairments, symptoms, and quality of life and improved with pyloric dilation. These observations raise the possibility that physiologic testing may identify gastroparesis subgroups who might respond to pyloric therapies
Xue HB, Fan HZ, Meng XM, Cristofaro S, Mekaroonkamol P, Dacha S, et al. Fluoroscopy-guided gastric peroral endoscopic pyloromyotomy (G-POEM): a more reliable and efficient method for treatment of refractory gastroparesis. Surg Endosc. 2017 (In press).
Khashab MA, Ngamruengphong S, Carr-Locke D, Bapaye A, Benias PC, Serouya S, et al. Gastric per-oral endoscopic myotomy for refractory gastroparesis: results from the first multicenter study on endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2017;85:123–8.
• Gonzalez JM, Benezech A, Vitton V, Barthet M. G-POEM with antro-pyloromyotomy for the treatment of refractory gastroparesis: mid-term follow-up and factors predicting outcome. Aliment Pharmacol Ther. 2017 (In press). This open-label series of 29 gastroparesis patients reported 6 month follow-up data showing 69% success in reducing GCSI scores and 70% normalization of gastric emptying results.
Lacy BE. Neuroenteric stimulation for gastroparesis. Curr Treat Options Gastroenterol. 2015;13:409–17.
Abell T, McCallum R, Hocking M, Koch K, Abrahamsson H, Leblanc I, et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology. 2003;125:421–8.
McCallum RW, Snape W, Brody F, Wo J, Parkman HP, Nowak T. Gastric electrical stimulation with Enterra therapy improves symptoms from diabetic gastroparesis in a prospective study. Clin Gastroenterol Hepatol. 2010;8:947–54.
McCallum RW, Sarosiek I, Parkman HP, Snape W, Brody F, Wo J, et al. Gastric electrical stimulation with Enterra therapy improves symptoms of idiopathic gastroparesis. Neurogastroenterol Motil. 2013;25:815–e636.
Abell TL, McCallum RW, May KP, Wilson L, Parkman HP, Hasler WL, et al. Effectiveness of gastric electrical stimulation in gastroparesis: results from a large prospectively collected database of a national gastroparesis registry (abstract). Gastroenterology. 2015;148:S-65.
Ducrotté P, Coffin B, Mathieu N, Fontaine S, Bruley des Varannes S, Zerbib F, et al. Gastric electrical stimulation (GES) for refractory vomiting: results of a prospective multicenter double-blinded randomized controlled cross-over trial (abstract). Gastroenterology. 2017;152:778e.
Hibbard ML, Dunst CM, Swanström LL. Laparoscopic and endoscopic pyloroplasty for gastroparesis results in sustained symptom improvement. J Gastrointest Surg. 2011;15:1513–9.
Mancini SA, Angelo JL, Peckler Z, Philp FH, Farah KF. Pyloroplasty for refractory gastroparesis. Am Surg. 2015;81:738–46.
Zehetner J, Ravari F, Ayazi S, Skibba A, Darehzereshki A, Pelipad D, et al. Minimally invasive surgical approach for the treatment of gastroparesis. Surg Endosc. 2013;27:61–6.
Bhayani NH, Sharata AM, Dunst CM, Kurian AA, Reavis KM, Swanstrom LL. End of the road for a dysfunctional end organ: laparoscopic gastrectomy for refractory gastroparesis. J Gastrointest Surg. 2015;19:411–7.
• Lembo A, Camilleri M, McCallum R, Sastre R, Breton C, Spence S, et al. Relamorelin reduces vomiting frequency and severity and accelerates gastric emptying in adults with diabetic gastroparesis. Gastroenterology. 2016;151:87–96. In this RCT, the ghrelin agonist relamorelin accelerated gastric emptying and decreased vomiting in 204 patients with diabetic gastroparesis and further reduced other symptoms in patients with baseline vomiting. This represents a promising new therapy in this condition
Camilleri M, McCallum RW, Tack JF, Spence SC, Gottesdiener K, Fiedorek FT. Relamorelin in patients with diabetic gastroparesis: efficacy and safety results from a phase 2b randomized, double-blind, placebo-controlled, 12-week study (RM-131-009)(abstract). Gastroenterology. 2017;152:638.
Rampe D, Roy M-L, Dennis A, Brown AM. A mechanism for the proarrhythmic effects of cisapride (Propulsid): high affinity blockade of the human cardiac potassium channel HERG. FEBS Lett. 1997;417:28–32.
Ahn A, Barnes C, Shaywitz D, Grimaldi M, Canafax DM. Velusetrag improves gastric emptying time in subjects with diabetic or idiopathic gastroparesis (abstract). Gastroenterology. 2015;148:S-507.
Barton ME, Otiker T, Johnson LV, Robertson DC, Dobbins RL, Parkman HP, et al. A randomized, double-blind, placebo-controlled phase II study (MOT114479) to evaluate the safety and efficacy and dose response of 28 days of orally administered camicinal, a motilin receptor agonist, in diabetics with gastroparesis (abstract). Gastroenterology. 2014;146:S-20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Allen A. Lee and William L. Hasler each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Motility
Rights and permissions
About this article
Cite this article
Lee, A.A., Hasler, W.L. Diabetes and the Stomach. Curr Treat Options Gastro 15, 441–459 (2017). https://doi.org/10.1007/s11938-017-0146-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-017-0146-y