Abstract
Background
The prevalence of generalized transit delay and relation to symptoms in suspected gastroparesis, intestinal dysmotility, or slow transit constipation are unknown.
Aims
The aims of this study were (1) to define prevalence of generalized dysmotility using wireless motility capsules (WMC), (2) to relate to symptoms in suspected regional delay, (3) to compare results of WMC testing to conventional transit studies to quantify new diagnoses, and (4) to assess the impact of results of WMC testing on clinical decisions.
Methods
WMC transits were analyzed in 83 patients with suspected gastroparesis, intestinal dysmotility, or slow transit constipation.
Results
Isolated regional delays were observed in 32% (9% stomach, 5% small bowel, 18% colon). Transits were normal in 32% and showed generalized delays in 35%. Symptom profiles were similar with normal transit, isolated delayed gastric, small intestinal, and colonic transit, and generalized delay (P = NS). Compared to conventional tests, WMC showed discordance in 38% and provided new diagnoses in 53%. WMC testing influenced management in 67% (new medications 60%; modified nutritional regimens 14%; surgical referrals 6%) and eliminated needs for testing not already done including gastric scintigraphy (17%), small bowel barium transit (54%), and radioopaque colon marker tests (68%).
Conclusions
WMC testing defines localized and generalized transit delays with suspected gastroparesis, intestinal dysmotility, or slow transit constipation. Symptoms do not predict the results of WMC testing. WMC findings provide new diagnoses in >50%, may be discordant with conventional tests, and can influence management by changing treatments and eliminating needs for other tests. These findings suggest potential benefits of this method in suspected dysmotility syndromes and mandate prospective investigation to further define its clinical role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tests of regional transit commonly are obtained to exclude delayed gastric emptying in gastroparesis, retarded small bowel transit in intestinal dysmotility, and impaired colon propulsion in slow transit constipation [1, 2]. Gastroparesis often presents with nausea and vomiting, symptoms considered referable to the upper gastrointestinal tract [3]. However, many gastroparesis patients report bloating, distention, abdominal pain, and bowel habit disturbances suggesting lower gut involvement as well [3, 4]. Slow transit constipation typically is characterized by passage of hard stools at infrequent intervals [2]. However, complaints of patients with slow colonic transit may also include nausea, vomiting, bloating, and distention possibly reflecting more proximal involvement [5]. These observations raise the possibility of diffuse dysmotility in cases of suspected local delays.
Indeed, studies which demonstrate regional transit delays in some patients are associated with more generalized gut motor abnormalities. Subsets of patients with slow transit constipation exhibit disturbed esophageal sphincter and body function, delayed gastric emptying, and abnormal antroduodenal motility that may have prognostic importance in predicting outcomes from aggressive therapies such as colectomy [6–17]. The prevalence and severity of lower gut abnormalities in patients with gastroparesis are less well studied. A standardized wireless motility capsule (WMC) method has been developed to measure regional transit in the stomach, small intestine, and colon by detecting characteristic pH changes in suspected gastroparesis and slow transit constipation [18, 19]. Using this technique, a subset of patients in a gastroparesis trial showed delayed colon transit [20]. A rigorous assessment of generalized transit delays in patients with suspected isolated gastroparesis, intestinal dysmotility, or slow transit constipation in routine clinical practice has not been performed.
This study accessed databases at two referral centers for disorders of gastrointestinal motility to address four specific aims. The first aim was to define the prevalence of regional versus diffuse gut transit delays in patients referred for testing of the stomach, small intestine, or colon using a WMC. The second aim was to delineate symptoms in different subsets to assess if presentations are different with localized delays in the stomach, small intestine, and colon versus with generalized dysmotility. The third aim was to compare WMC results to prior conventional studies of gut motor function to ascertain if new diagnoses were provided using the capsule method. The final aim was to assess treatment decisions and needs for additional diagnostic evaluation made after WMC testing to estimate changes in patient management. Through these studies, we hoped to characterize regional and generalized dysmotility patterns in patients referred for testing of presumed gastroparesis, intestinal dysmotility, or slow transit constipation.
Materials and Methods
Patient Population
Patients undergoing WMC testing (SmartPill, SmartPill Corporation, Buffalo, NY) to exclude delayed gastric, small intestinal, or colonic transit between September 2007 and May 2010 were identified by retrospective review of the electronic Longitudinal Medical Record database at Massachusetts General Hospital and the CareWeb and Gastrointestinal Physiology Laboratory databases at University of Michigan Hospital. Database access and data analysis protocols were approved by Institutional Review Boards at both centers and waivers of informed consent were granted at each site.
Data Acquisition and Analysis
Data were acquired relating to symptom presentations, prior diagnostic evaluations, WMC interpretations, and management decisions made after WMC testing.
Clinical Data
Outpatient clinic notes from several ordering physicians were reviewed to assess demographic data and symptom presentations of patients with presumed gastroparesis, intestinal dysmotility, or slow transit constipation. Demographic factors included numbers and percentages of patients who were female versus male, mean age, numbers and percentages of patients >50 years old, mean body mass index (BMI), numbers and percentages of patients who were obese (BMI > 30 kg/m2) or underweight (BMI < 18.5 kg/m2), and numbers and percentages of patients with diabetes, prior gastrointestinal surgery or resection (only including fundoplication, partial or total gastric resection, bariatric surgery, small bowel resection, or partial or total colectomy), prior malignancy anywhere in the body, prior or current psychiatric illness, and prior or current neurologic disease. Symptoms were stratified into those referable to the upper gut (nausea, vomiting, fullness, early satiety, and symptoms of gastroesophageal reflux disease [GERD]), to the lower gut (constipation, straining, hard stools, <3 bowel movements/week, incomplete evacuation, need for digital disimpaction, and diarrhea), and not localizable to a specific region (anorexia, bloating, distention, and abdominal pain or discomfort). Symptoms were recorded as being present or not present (either specifically denied in the medical record or not referred to). Outpatient records describing rationales for obtaining WMC testing were reviewed to ascertain if referral was for a suspicion of or to exclude delayed gastric, small intestinal, or colonic transit. Records prior to WMC recordings were reviewed for prior diagnostic tests of gastric, small intestinal, and/or colonic motor activity including gastric scintigraphy, small intestinal barium radiography for transit determination, radioopaque marker assessment of colon transit, and measures of anorectal outlet obstruction (anorectal manometry and balloon expulsion testing). Most prior transit tests were performed at outside community institutions and many did not adhere to published practice guidelines [1]. Methodologies employed were diverse and inconsistent and the listed definitions for transit abnormality frequently were not validated. For example, gastric scintigraphy testing often employed scans of 90–240 min duration with variable reporting of t 1/2 or % emptying/retained at 90, 120, or 240 min. Methods to measure small intestinal transit are not rigorously validated; in the absence of widely accepted techniques, many centers (including both in this study) employ barium radiography to measure transit with normal ranges defined from each institution. At both academic centers, a small bowel transit time >4 h is considered delayed. Most referring centers employed a radioopaque marker colon transit protocol involving performance of a single radiograph 5 days after swallowing a marker capsule; conversely, both academic institutions perform colon transit testing using the Metcalf method of serial radiographs [21]. Clinic notes were reviewed to assess if these tests were or were not performed (this includes notes which stated the tests were not performed and notes in which no mention of the tests were made).
Wireless Motility Capsule Data Analysis
Interpretations of results of WMC testing were gleaned from outpatient records. pH tracings quantified times for gastric emptying, small intestinal transit, and colon transit using accepted methods (MotiliGI, SmartPill Corporation, Buffalo, NY) [18, 19]. Prior to WMC ingestion at both centers, patients discontinued proton pump inhibitors for 7 days, histamine H2 receptor antagonists for 3 days, opiates for 3–7 days, laxatives for at least 3 days, and anticholinergic agents for 3 days. Patients on stable doses of antihypertensives or antidepressants for at least 3 months were allowed to remain on these drugs during testing. Gastric emptying times were calculated from the time of WMC ingestion to pyloric passage, as determined by an abrupt ≥2 pH unit increase from the lowest postprandial value to at least 4 that did not decrease below 4 for >10 min at any subsequent time. Delayed gastric emptying was diagnosed when the emptying time exceeded 5 h [18]. Small intestinal transit times were calculated from the time of pyloric passage to ileocecal junction transit, as determined by an abrupt pH decrease of ≥1.0 pH unit at least 30 min after gastric evacuation that persisted for at least 10 min. Delayed small intestinal transit was determined when transit times exceeded 6 h, based on 95% cutoff values from control studies [19]. Colon transit times were calculated from the time of ileocecal junction transit to the time of anal expulsion, as determined by abrupt 0.045°F/second temperature decreases. Delayed colon transit was diagnosed when transit times exceeded 59 h [19]. Previous studies have observed that rare patients (<10%) do not exhibit pH decreases as the capsule passes the ileocecal junction [19, 22]. In such instances, specific values for small intestinal and colonic transit can not be determined. Small intestinal and colonic transit values were not calculated for individuals not exhibiting ileocecal junction pH decreases in this study. Sensitivities of conventional test and WMC findings were calculated by dividing the number of patients exhibiting a transit abnormality in the region of suspected delay by the total number of patients with suspected delay in the same region undergoing testing. The specificity of WMC testing was calculated by dividing the number of patients with normal transit in a given region by the total number of patients with a suspicion of normal transit in the same target region. Positive test agreement was calculated by determining the percentage with abnormal transit on conventional testing who also exhibited abnormal WMC transit in a given target region. Negative test agreement was calculated by determining the percentage with normal transit on conventional testing who also exhibited normal WMC transit in a target region.
Management Decisions
WMC findings were compared to results of prior conventional motility testing in outpatient notes to determine if a new diagnosis was provided and if there was discordance between capsule and conventional methods. One criterion for a new diagnosis would be satisfied if the WMC was the only abnormal transit test performed for a particular gut region. A second criterion for a new diagnosis could also be satisfied in individuals who had undergone prior transit testing. For example, if prior scintigraphy showed normal gastric emptying but wireless capsule emptying time was abnormal, this finding would indicate a new diagnosis of gastroparesis. If prior barium series showed normal transit but capsule recordings revealed abnormal small bowel transit, this finding would be a new diagnosis of impaired small intestinal transit. If radioopaque marker testing was normal but capsule recordings showed abnormal colon transit, this finding would indicate a new diagnosis of slow transit constipation.
Clinic records dictated after WMC testing were analyzed to determine if management decisions were influenced by diagnostic findings. Specifically, notes were reviewed to determine if new medication regimens, modification of nutritional programs (including diet changes or initiation of enteral or parenteral feedings), or surgical referrals for colectomy for refractory slow transit constipation were ordered after obtaining WMC results.
Finally, outpatient notes recorded after WMC performance were reviewed to determine if capsule testing eliminated needs for additional tests of motor function. If testing was performed for presumed gastroparesis and the patient did not undergo gastric scintigraphy before or after WMC recording, this indicated elimination of the need for nuclear medicine gastric emptying scanning. If testing was performed for presumed small intestinal delay and the patient did not undergo barium transit testing before or after WMC recording, this indicated elimination of the need for radiographic transit studies. If testing was performed for presumed slow transit constipation and the patient did not undergo radioopaque marker studies before or after WMC recording, this indicated elimination of the need for marker studies.
Statistical Analysis
Simple frequencies and relative frequencies were used to summarize data. Associations between categorical variables were evaluated using contingency tables and observed associations were statistically assessed using Fisher’s exact test in the case of 2 by 2 tables, and using the procedure of Freeman and Halton for larger tables [23]. A nominal significance level of 0.05 was used in all testing and all analyses were performed using SAS version 9.2.
Results
Demographic Information
Demographic data on 83 patients referred to the two institutions for WMC definition of dysmotility syndromes are shown in Table 1. Patients were predominantly female (79.5%) with a mean age of 43.7 ± 1.6 years. Mean BMI was 24.9 ± 0.7 kg/m2; some were obese or overweight. A small number (14.6%) were diabetics. Very few had undergone prior gastrointestinal surgery or resection (7.2%) (2 Nissen fundoplication, 2 bariatric surgery, 2 hemicolectomy) or had received treatment for malignancy (8.5%) (1 colon carcinoma, 1 appendiceal carcinoma, 1 breast carcinoma, 1 renal cell carcinoma, 1 cervical carcinoma, 1 ovarian carcinoma, 1 basal cell carcinoma). No individual had a known active neoplasm at the time of WMC study. Psychiatric diseases were prevalent (52.4%) (25 depression, 4 bipolar, 9 anxiety disorder, 7 eating disorder, 1 autism). Likewise, neurologic conditions were commonly reported (26.8%) (9 headaches including migraines, 3 seizure disorder, 2 multiple sclerosis, 2 cerebral palsy, 3 mitochondrial disorder, 1 dysautonomia, 1 postural orthostatic tachycardia syndrome, 1 reflex sympathetic dystrophy, 1 myotonia congenita, 1 traumatic brain injury, 1 corpus callosum agenesis).
Clinical Data
Reasons for WMC testing were assessed by medical record review. Thirteen of 83 patients (15.7%) were referred with a suspicion of or to exclude delayed gastric emptying only, 3 (3.6%) were referred with a suspicion of or to exclude delayed small intestinal transit only, 23 (27.8%) were referred with a suspicion of or to exclude delayed colon transit only, and 41 (49.4%) were referred with a suspicion of or to exclude generalized transit delays involving ≥2 gut regions. Clinical suspicion could not be gleaned for 3 patients (3.6%). Of 41 patients with suspected generalized delays, 3 (3.6% of total) had suspected delays in the stomach and small intestine, 2 (2.4%) had suspected delays in the small intestine and colon, 31 (37.3%) had suspected delays in the stomach and colon, and 5 (6.0%) had suspected delays in all 3 regions.
A range of symptoms was reported by patients undergoing WMC testing, including 62 (74.7%) with upper gut, 70 (84.3%) with lower gut, and 75 (90.4%) with non-localizable symptoms. Symptom profiles were not recorded for 2 patients (2.4%). Numbers reporting individual upper gut symptoms were 50 (60.2%) for nausea, 37 (44.6%) for vomiting, 16 (19.3%) for fullness, 30 (36.1%) for early satiety, and 14 (16.9%) for GERD symptoms. Reports of lower gut symptoms included 59 (71.1%) for constipation, 32 (38.6%) for straining, 18 (21.7%) for hard stools, 35 (42.2%) for <3 bowel movements/week, 17 (20.5%) for incomplete evacuation, 8 (9.6%) for digital disimpaction, and 26 (31.3%) for diarrhea. Reports of non-localizable symptoms included 18 (21.7%) for anorexia, 39 (47.0%) for bloating, 18 (21.7%) for distention, and 67 (80.7%) for pain or discomfort. Figure 1 shows rates of symptom reporting for suspected delayed gastric, small intestinal, or colonic transit. Upper gut symptoms were reported more often with suspected delayed gastric emptying than in those without suspected delayed gastric emptying, while lower gut symptoms were reported more often with suspected delayed colonic transit than in those without suspected delayed colonic transit (both P < 0.0001). There was a trend to reduced reports of lower gut symptoms with suspected delayed gastric emptying (P = 0.09). Reports of upper gut (87.8%), lower gut (95.1%), and non-localizable (92.7%) symptoms were similar in 41 patients with suspected generalized delays.
Percentages of patients reporting different symptom profiles are presented in those with suspected delays in gastric emptying, small bowel (SB) transit, and colon transit. Symptoms of upper gut dysmotility (a) were reported in a higher percentage of patients with presumed gastric emptying delay (N = 52) versus those with presumed normal gastric emptying (N = 28) (P < 0.0001), but also were prominent in those with delayed (N = 13) versus normal (N = 66) SB transit and delayed (N = 60) versus normal (N = 19) colon transit. Symptoms of lower gut dysmotility (b) were reported in a higher percentage of those with presumed colon transit delay versus patients with normal colon transit (P < 0.0001), but trended lower in those with presumed gastric emptying delay versus normal gastric emptying (P = 0.09). Non-localizable symptoms (c) were reported by similar numbers of patients regardless of gastric, SB, or colon transit time. P values determined from Fisher’s exact test
Medical record review revealed which conventional motility tests were performed before WMC testing. Forty-four of 52 patients with suspected delayed gastric emptying (84.6%) underwent gastric scintigraphy; 17 of these (38.6%) exhibited abnormal emptying. Six of 13 with suspected delayed small intestinal transit (46.2%) underwent small bowel barium radiography; 4 of these (66.7%) exhibited abnormal small intestinal transit. Sixteen of 61 with suspected slow colonic transit (26.2%) underwent radioopaque marker testing; 9 of these (56.2%) exhibited abnormal colonic transit. Forty-two of this group (68.9%) underwent anorectal outlet function testing; 27 of these (64.3%) exhibited outlet dysfunction.
Wireless Motility Capsule Recording Data
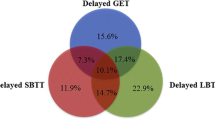
WMC studies provided complete recordings of gastric, small intestinal, and colonic transit in 77 of 83 patients (92.8%). Two (2.4%) did not exhibit pH decreases reflecting ileocecal junction transit and 2 (2.4%) had not evacuated the capsule at the time the recorder was returned. In 2 (2.4%), the capsule did not leave the stomach during the recording period and no small intestinal or colonic data were obtained (in both individuals, capsule passage was documented after the study was completed). Of the 77 complete recordings, 7 (9.1%) showed isolated delayed gastric emptying, 4 (5.2%) showed isolated delayed small intestinal transit, 14 (18.2%) showed isolated delayed colonic transit, 27 (35.1%) showed generalized abnormalities in ≥2 regions, and 25 (32.5%) showed normal transit in all three regions. Of the 27 with generalized abnormalities, 1 (1.3% of the total evaluated) had abnormal transit in the stomach and small intestine, 4 (5.2%) had abnormal transit in the small intestine and colon, 20 (26.0%) had abnormal transit in the stomach and colon, and 2 (2.6%) had abnormal transit in all regions. In those with either suspected gastric emptying delay or colon transit delay, sensitivities of conventional and WMC tests were similar (Table 2). The sensitivity of barium testing was 66.7% for finding a small bowel transit abnormality versus 9.1% for WMC testing. Specificities of WMC testing for confirmation of normal transit in the target region (e.g. normal gastric emptying in those with no suspicion of delay) ranged from 61.1 to 84.4%. Patients with suspected delays in one region often exhibited abnormal WMC transit in other regions (Table 2).
Complete WMC transit data in all three regions facilitated determination of diagnosis in 77 cases. Diagnoses also were provided for six patients with incomplete data collection, but confident exclusion of transit delays in all three regions was not possible in these individuals. Compared to conventional testing, WMC analyses provided new diagnoses in 44 cases (53.0%), including 7 (8.4%) new gastroparesis diagnoses (based on isolated delayed gastric emptying), 3 (3.6%) new small intestinal dysmotility diagnoses (based on isolated delayed small intestinal transit), 11 (13.3%) new slow transit constipation diagnoses (based on isolated delayed colonic transit), and 23 (27.7%) new generalized dysmotility cases. Of these 23 cases, 1 (1.2% of the total) had abnormal transit in the stomach and small intestine, 4 (4.8%) had abnormal transit in the small intestine and colon, 16 (19.3%) had abnormal transit in the stomach and colon, and 2 (2.4%) had abnormal transit in all three regions. Discordance was noted in 38% of patients for regional WMC findings versus scintigraphy measures of gastric emptying, barium radiography measures of small intestinal transit, and radioopaque marker measures of colonic transit. Table 3 presents concordance and discordance for WMC and conventional test findings and positive and negative test agreements.
Symptom profiles were relatable to WMC transit profiles for 75 patients (Fig. 2). There were no differences in prevalences of upper gut (P = 0.17), lower gut (P = 0.28), or non-localizable (P = 0.75) symptoms with isolated gastric, small intestinal, or colonic transit abnormalities, generalized transit abnormalities, or normal transit in all regions.
Percentages of patients reporting different symptom profiles are presented in those with documented isolated transit delays, generalized delays, or normal transit on WMC testing. Reports of upper gut symptoms (P = 0.17), lower gut symptoms (P = 0.28), and non-localizable symptoms (P = 0.75) were similar in those with isolated transit delays in the stomach, small bowel (SB), and colon, patients with generalized transit delays, and individuals with normal transit throughout
Management Decisions
Changes in clinical management were ordered after WMC testing in 65 patients (Table 4). Changes in medication regimens were recommended for 39 patients (60.0%), while changes in nutritional programs were made in 9 cases (13.8%). Medication changes were recommended less often in those with normal transit in all gut regions versus other transit delays (P = 0.03). Referrals to surgery for colectomy were placed in 4 patients (6.2%), mainly in those with colon transit abnormalities. Changes in management were related to abnormal versus normal regional transit in 69 patients (Fig. 3). Findings of abnormal versus normal gastric emptying time or small intestinal transit time did not influence any management change (all P = NS). Findings of abnormal versus normal colonic transit time did not influence changes in nutritional programs (P = 0.72). Finding abnormal colon transit increased the percentage of patients with changes in medication regimens (P = 0.02) and showed trends to increasing surgical referrals (P = 0.12).
Percentages of patients who were recommended to change medication regimens (a), change nutritional programs (b), or be referred to surgery (c) after performance of WMC testing are presented as a function of delayed versus normal gastric emptying, small bowel (SB) transit, or colon transit. Higher percentages of patients with delayed colon transit received recommendations to change medications versus those with normal colon transit (P = 0.02). Similar percentages of patients were given medication recommendations in those with delayed versus normal gastric emptying and SB transit. Similar percentages were given nutritional recommendations or surgical referrals in those with delayed versus normal transit in all regions. P values determined from Fisher’s exact test
WMC testing avoided additional studies in some patients for whom no regional transit testing had been performed. Needs for nuclear gastric emptying testing were eliminated in 9 of 52 patients (17.3%). Many individuals had undergone prior gastric scintigraphy prior to referral for WMC testing. Barium radiography to assess small intestinal transit was avoided in 7 of 13 cases (53.8%). Needs for radioopaque marker testing were eliminated in 41 of 60 patients (68.3%); anorectal outlet function testing was not avoided by WMC performance (0%).
Discussion
Gastric emptying scans are obtained for symptoms of gastroparesis, while tests of small intestinal or colonic transit are ordered if intestinal dysmotility or slow transit constipation is suspected [1, 2]. Yet, many patients with typical gastroparesis symptoms like nausea and vomiting report bloating or distention that could refer to the distal gut while constipated patients may note nausea or vomiting suggesting possible upper gut dysfunction [2–5]. In using WMCs to measure gastric, intestinal, and colonic transit in one test, this study provides detailed description of generalized dysfunction in presumed regional dysmotility syndromes.
Some slow transit constipation patients also have abnormal upper gut function. Upper and lower esophageal sphincter and body dysfunctions are found in constipated individuals [6]. Twenty to 60% of patients with slow transit constipation show delayed scintigraphic gastric or small bowel transit [7–11, 24]. Small bowel manometry was disrupted in 12 of 20 patients with delayed colon transit (60%) in one study, and 3 of 20 patients (15%) in another [12, 13]. Abnormal lower gut transit in gastroparesis is less well described, but there is evidence for generalized dysmotility in this disorder. In separate analyses, colon transit and contractility on WMC testing were impaired in gastroparetics versus patients with normal emptying [20, 25].
Findings of this study provide new data regarding isolated versus generalized transit delays in suspected gastroparesis, intestinal dysmotility, or slow transit constipation. WMC tests recorded regional transit in >90%. Abnormal transit was found in about 70% of cases, many of whom showed abnormalities in ≥2 regions. New diagnoses were provided in >50%, and included previously uninvestigated findings as well as abnormal transit in regions previously normal on conventional tests. In contrast to pretest expectations, symptom profiles did not relate to transit delays, suggesting clinical presentations may not reliably predict motor dysfunction. For example, though all 14 patients with isolated delayed colon transit noted lower gut symptoms, so did 9 of 11 with isolated delayed gastric or small bowel transit. Given our sample size and limitations of symptom extraction from clinic reports, our findings do not exclude subtly distinct symptom presentations with isolated transit delays in different regions.
Despite challenges of understanding relations of symptoms to motor patterns, objective data provided by transit testing form the basis for determining management decisions in many cases. In this study, results of WMC testing altered many treatment decisions by changing medications, influencing nutrition regimens, and promoting surgical referrals. Medication changes were made less often with normal transit versus delay in any region, which was most significant comparing normal versus abnormal colon transit. This may reflect the impact of a positive test or incomplete documentation of clinical decision making. Examples included prescribing prokinetics (metoclopramide, domperidone) to patients with suspected slow transit constipation with delayed gastric emptying on WMC testing and use of laxatives (PEG 3350) in some with suspected gastroparesis found to have slow colon transit. WMC findings replaced or eliminated needs for most additional conventional transit tests, but did not eliminate anorectal outlet testing. Gastric scintigraphy was avoided less often as many with suspected gastroparesis underwent prior scintigraphy based on practice patterns at one center before introducing WMC methods. As recent trials validate WMCs as reliable tests of gastric emptying, it is likely that newer data would show a lesser need to perform both WMC and scintigraphy in any individual.
WMC has been directly compared to conventional testing in prior prospective studies to validate the capsule technique [18–20, 22]. In the stomach and colon, WMC results correlate well with comparator tests when standardized methods such as 4-h retention on gastric scintigraphy and the Metcalf test of colon transit are used [18, 22]. However in this retrospective study, WMC results were compared with prior conventional tests often obtained months earlier in the clinical course that were conducted utilizing varied methods. Standardized methods recommended by gastroenterology and nuclear medicine societies commonly are not widely applied [1]. Many centers use non-standardized gastric scintigraphy techniques that quantify 90–120 min values or half times of emptying, which correlate less well with WMC emptying times than do 4 h retention values [18]. Half times of emptying detect 30% fewer cases than 4 h values [1, 18]. Colon transit is most often assessed with one X-ray 5 days after radioopaque marker ingestion, which correlates poorly with more rigorous conventional methods and WMC findings [19]. Thus, some of the discordance in this study may stem from comparing WMC results with poorly standardized, unreliable conventional tests. Observed differences also may relate to technical factors. Gastric emptying of indigestible and digestible solids is regulated by distinct processes. Colon transit of large capsules also may follow different profiles from small plastic markers. It is uncertain if measuring transit of a large, indigestible object such as the WMC provides more meaningful information than of digestible solids or liquids. Finally, inconsistencies in gastric and colon physiology in patients with dysmotility may lead to major day-to-day variability on repeat transit testing and may contribute to discordance. To test if WMC results are more clinically relevant than conventional tests, prospective studies comparing responses to treatment regimens based on detecting transit abnormalities must be performed.
In addition to prescribing medications targeting regions distant from the organ of presumed dysmotility, results of this study may have clinical implications. Characterizing delayed small bowel transit might promote evaluation for bacterial overgrowth. Detecting slow gastric or small intestinal transit by methods other than WMC has been proposed to influence decisions in slow transit constipation. Some studies suggest outcomes from colectomy (including self reports of treatment success, postoperative complications, and hospitalizations) may be worse in constipated patients with associated upper gut dysmotility [10, 14–17, 26, 27]. These observations raise the possibility that future studies measuring WMC gastric and small bowel transit could stratify risk in those being considered for colectomy for constipation.
The ability to measure gastric, small bowel, and colon transit in one WMC study offers advantages over other protocols. Scintigraphy is the only other test combining all three measures, but small bowel and colon scintigraphy are done at few centers because of personnel needs and the inconvenience of having patients travel to the imaging facility multiple times over several days to follow tracer progression [2, 28]. More often, measuring transit in the three regions mandates different tests, requiring repeated visits and exposing patients to significant radiation. Further center-to-center variability in test meals, sampling intervals, and analysis algorithms undermine gastric scintigraphy accuracy [1]. The most common radioopaque colon transit test (Hinton) obtains one radiograph 5 days after marker ingestion and may be less accurate than the more intensive Metcalf method of serial X-rays after 3 days of marker ingestion [21, 29, 30]. Barium testing of small bowel transit is not standardized, while lactulose breath tests are unreliable due to artificial acceleration of small bowel propulsion by the substrate [31, 32].
Concerns can be raised about the present study. All patients were investigated at two academic centers specializing in managing severe dysmotility syndromes. In a representative community sample, gastroparetics might have less impaired colon transit or constipated patients might not show impressive gastric emptying delays. Our patients also may differ from a typical community population because they are a more refractory subset referred after conventional studies failed to positively influence outcomes. Further, as with any retrospective investigation, this study involved analyses of preexisting databases and data recording was not standardized; thus reporting of a lack of a given symptom or test result might not equate with symptom absence or test non-performance. Sensitivities of WMC testing were comparable to comparator tests in the stomach and colon. However, WMC sensitivity to detect small bowel transit delays in those with suspicion of such abnormalities was lower than for barium testing. Symptoms of small bowel dysmotility overlap with those relating both to the stomach and colon. It is probable that some symptoms thought by referring clinicians to originate from the small intestine by history may be coming from the stomach or colon instead. Indeed, a recent study noted that bloating (a symptom often considered to have a small intestinal source) of at least moderate severity is reported by 76% of patients with documented delayed gastric emptying [33]. Of note, the WMC method does not permit localization in a specific small bowel region, thus it cannot be determined if there are selected areas (e.g. the ileocecal junction) with capsule hang up. To date, there are no reports using concurrent fluoroscopy and WMC testing to localize the device within the small intestine. Future studies will test if the low sensitivity observed in this study relates to clinician inability to predict small bowel transit impairment from symptoms, a lack of accuracy of the WMC method to measure overall small bowel transit, or specific abnormalities in regional small bowel WMC propulsion that confound interpretation of overall transit times in this organ. Finally, determining effects of WMC testing on management decisions or needs for further testing is subjective. Although new therapy may be recommended because of a given test result, it is uncertain if similar decisions might have been made if testing had not been performed. In this study, limited follow-up was performed after WMC testing and no treatment outcomes made in response to WMC findings were reported. The true benefits of a given test may not be evident until outcomes of any test-related decisions become apparent weeks or months later. Alternatively it is conceivable that finding localized or generalized transit delays might not have clinical importance or influence response to therapies that accelerate propulsion.
The analyses performed in this investigation mirror those of other significant studies assessing the utility of tests of gut motor function. In a study assessing utility of gastric scintigraphy, “the influence of the result of gastric emptying studies upon the subsequent clinical management” was determined from hospital case reviews [34]. In descriptions of the utility of antroduodenal manometry, one study reviewed clinic records to determine the positive impact of testing defined as implying “that the results of manometry helped to choose a specific treatment for the patient”, while a second used case records to determine positive outcomes defined as “the outcome of the study resulted in alteration of the management of the patient, … prompted further medical investigation, or …resulted in referral to another specialist” [35, 36]. Concerns about the present study also can be raised for these important, authoritative published papers. Future prospective studies for both conventional and WMC methods characterizing generalized delays with predetermined management protocols would provide definitive evidence for the utility of whole gut transit measurements in suspected gastroparesis or slow transit constipation.
To conclude, WMC tests define localized and diffuse transit delays in suspected gastroparesis, intestinal dysmotility, or slow transit constipation. WMC analyses may be discordant with conventional tests and new diagnoses are provided in >50% of cases. WMC methods influence management by changing treatments and eliminating additional tests. These retrospective analyses emphasize potential benefits of WMC testing of regional and generalized transit for suspected dysmotility and mandate prospective study to further define its clinical role.
References
Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–763.
Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastrointest Endosc Clin N Am. 2009;19:117–139.
Hasler WL. Gastroparesis: symptoms, evaluation, and treatment. Gastroenterol Clin North Am. 2007;36:619–647.
Hoogerwerf WA, Pasricha PJ, Kalloo AN, Schuster MM. Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol. 1999;94:1029–1033.
Agrawal A, Houghton LA, Reilly B, et al. Bloating and distention in irritable bowel syndrome: the role of gastrointestinal transit. Am J Gastroenterol. 2009;104:1998–2004.
Watier A, Devroede G, Duranceau A, et al. Constipation with colonic inertia. A manifestation of systemic disease? Dig Dis Sci. 1983;28:1025–1033.
Reynolds JC, Ouyang A, Lee CA, et al. Chronic severe constipation. Prospective motility studies in 25 consecutive patients. Gastroenterology. 1987;92:414–420.
Stivland T, Camilleri M, Vassallo M, et al. Scintigraphic measurement of regional gut transit in idiopathic constipation. Gastroenterology. 1991;101:107–115.
Van der Sijp JR, Kamm MA, Nightingale JM, et al. Disturbed gastric and small bowel transit in severe idiopathic constipation. Dig Dis Sci. 1993;38:837–844.
Ghosh S, Papachrysostomou M, Batool M, Eastwood MA. Long-term results of subtotal colectomy and evidence of noncolonic involvement in patients with idiopathic slow-transit constipation. Scand J Gastroenterol. 1996;31:1083–1091.
MacDonald A, Baxter JN, Bessent RG, et al. Gastric emptying in patients with constipation following childbirth and due to idiopathic slow transit. Br J Surg. 1997;84:1141–1143.
Bassotti G, Stanghellini V, Chiarioni G, et al. Upper gastrointestinal motor activity in patients with slow-transit constipation. Further evidence for an enteric neuropathy. Dig Dis Sci. 1996;41:1999–2005.
Glia A, Lindberg G. Antroduodenal manometry findings in patients with slow-transit constipation. Scand J Gastroenterol. 1998;33:55–62.
Kuijpers HC. Application of the colorectal laboratory in diagnosis and treatment of functional constipation. Dis Colon Rectum. 1990;33:35–39.
Redmond JM, Smith GW, Barofsky I, et al. Physiological tests to predict long-term outcome of total abdominal colectomy for intractable constipation. Am J Gastroenterol. 1995;90:748–753.
Verne GN, Hocking MP, Davis RH, et al. Long-term response to subtotal colectomy in colonic inertia. J Gastrointest Surg. 2002;6:738–744.
Glia A, Akerlund JE, Lindberg G. Outcome of colectomy for slow-transit constipation in relation to presence of small-bowel dysmotility. Dis Colon Rectum. 2004;47:96–102.
Kuo B, McCallum RW, Koch KL, et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment Pharmacol Ther. 2008;27:186–196.
Rao SS, Kuo B, McCallum RW, et al. Investigation of colonic and whole-gut transit with wireless motility capsule and radiopaque markers in constipation. Clin Gastroenterol Hepatol. 2009;7:537–544.
Sarosiek I, Selover KH, Katz LA, et al. The assessment of regional gut transit times in healthy controls and patients with gastroparesis using wireless motility technology. Aliment Pharmacol Ther. 2010;31:313–322.
Metcalf AM, Phillips SF, Zinsmeister AR, et al. Simplified assessment of segmental colonic transit. Gastroenterology. 1987;92:40–47.
Camilleri M, Thorne KK, Ringel Y, et al. Wireless pH-motility capsule for colonic transit: prospective comparison with radiopaque markers in chronic constipation. Neurogastroenterol Motil. 2010;22:874–882.
Freeman GH, Halton JH. Note on an exact treatment of contingency, goodness of fit and other problems of significance. Biometrika. 1951;38:141–149.
Bannister JJ, Timms JM, Barfield LJ, et al. Physiological studies in young women with chronic constipation. Int J Colorectal Dis. 1986;1:175–182.
Hasler WL, Coleski R, Sarosiek I, et al. Colon transit, regional colon motor activity in diabetics with gastroparesis compared to healthy volunteers, diabetics with near normal gastric emptying (abstract). Gastroenterology. 2007;132:M2143.
Mollen RM, Kuijpers HC, Claassen AT. Colectomy for slow-transit constipation: preoperative functional evaluation is important but not a guarantee for a successful outcome. Dis Colon Rectum. 2001;44:577–580.
Zmora O, Colquhoun P, Katz J, et al. Small bowel transit does not correlate with outcome of surgery in patients with colonic inertia. Surg Innov. 2005;12:215–218.
Van der Sijp JR, Kamm MA, Nightingale JM, et al. Radioisotope determination of regional colonic transit in severe constipation: comparison with radio opaque markers. Gut. 1993;34:402–408.
Chaussade S, Khyari A, Roche H, et al. Determination of total and segmental colonic transit time in constipated patients. Results in 91 patients with a new simplified method. Dig Dis Sci. 1989;34:1168–1172.
Jankowski M, Chey WD, Maneerattanaporn M, et al. A comparison of two radioopaque marker methodologies in the assessment of colonic transit of adults with constipation (abstract). Gastroenterology. 2010;138:S231.
Kim SK. Small intestine transit time in the normal small bowel study. Am J Roentgenol. 1968;104:522–524.
Miller MA, Parkman HP, Urbain JL, et al. Comparison of scintigraphy and lactulose breath hydrogen test for assessment of orocecal transit: lactulose accelerates small bowel transit. Dig Dis Sci. 1997;42:10–18.
Hasler WL, Wilson LA, Parkman HP, et al. Bloating in gastroparesis: severity, impact, and associated factors. Am J Gastroenterol. Epub 2011/04/12.
Galil MA, Critchley M, Mackie CR. Isotope gastric emptying tests in clinical practice: expectation, outcome, and utility. Gut. 1993;34:916–919.
Soffer E, Thongsawat S. Clinical value of duodenojejunal manometry: its usefulness in diagnosis and management of patients with gastrointestinal symptoms. Dig Dis Sci. 1996;41:859–863.
Verhagen MA, Samsom M, Jebbink RJ, Smout AJ. Clinical relevance of antroduodenal manometry. Eur J Gastroenterol Hepatol. 1999;11:523–528.
Acknowledgments
Dr. Kuo has received research funding and is on the Advisory Board for SmartPill Corp. Dr. Chey is on the Advisory Board for SmartPill Corp. Dr. Wilding has served as a consultant for SmartPill Corp. Dr. Hasler has served as a consultant and has received research funding from SmartPill Corp.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuo, B., Maneerattanaporn, M., Lee, A.A. et al. Generalized Transit Delay on Wireless Motility Capsule Testing in Patients with Clinical Suspicion of Gastroparesis, Small Intestinal Dysmotility, or Slow Transit Constipation. Dig Dis Sci 56, 2928–2938 (2011). https://doi.org/10.1007/s10620-011-1751-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1751-6