Abstract
Purpose of Review
Knee and hip osteoarthritis (OA) are major public health problems worldwide causing pain, disability and impaired quality of life. This narrative paper discusses platelet-rich plasma (PRP) as a treatment for hip and knee OA, with a focus on evidence from randomised controlled trials (RCTs).
Recent Findings
Since the first RCT of PRP in 2012, there has been 15 RCTs in knee OA and three in hip OA, mostly comparing PRP to another intra-articular injection therapy, hyaluronic acid. All studies are of low to moderate methodological quality and use variable PRP protocols. In general, results showed that PRP is a safe treatment with potential to provide symptomatic benefit for OA at least in the short term (up to 12 months). Younger patients with less severe disease may be more responsive. There are no RCTs investigating the effects of PRP on OA structural changes.
Summary
No definitive conclusions can be made about the effects of PRP in OA given methodological concerns and considerable heterogeneity between studies. Further high-quality research is needed to establish the clinical and cost-effectiveness of PRP, the patients most likely to benefit and the optimal PRP protocol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a chronic musculoskeletal condition that commonly affects the knee and/or hip joints. It is a major public health problem worldwide [1] and is projected to rapidly increase as the population ages and rates of obesity escalation [2]. Osteoarthritis causes substantial pain and disability and impacts on quality-of-life. Hip and knee OA has been ranked as the 11th highest contributor to global disability and 38th highest in years lived with disability [2]. The disability associated with OA results in a considerable economic burden, both in direct costs related to treatment, particularly joint replacement surgery, and job-related indirect costs, including loss of productivity [3, 4].
There is no cure for OA, and to date, most research has focused on treatments to alleviate pain and prevent functional decline. Recommended drug therapies (such as analgesics and anti-inflammatory agents) and non-drug therapies (such as exercise) have short-term clinical benefits but effect sizes are generally small to moderate [5]. Furthermore, use of these drugs can have serious adverse consequences, while uptake and maintenance of exercise is often poor leading to lack of long-term benefit. The role of glucosamine sulphate and chondroitin sulphate as symptom- and disease-modifying agents is still being debated [6]. Hyaluronic acid (a viscosupplement) and corticosteroids are common intra-articular therapies for OA. However, hyaluronic acid (HA) is controversial with variable recommendations given across clinical guidelines [6]. Intra-articular corticosteroids are generally recommended, although not universally [6], and for short-term pain relief only given that benefits are limited to a few weeks [7]. Having failed these other treatment options, joint arthroplasty is a common procedure for advanced hip or knee OA. While it is an effective definitive treatment, it is expensive and there is a risk of serious medical and post surgical complications [8]. Furthermore, this surgical procedure is not suitable for all patients. Thus, as OA is typically progressive with symptoms and structural deterioration driving the need for joint replacement [9], identifying efficacious, safe treatments that address both symptoms and structure is an important objective.
Currently, no disease-modifying agent has been approved by regulatory agencies. However, therapies that affect the underlying biological processes responsible for OA pathogenesis have potential. One such biologic therapy receiving increasing interest is platelet-rich plasma (PRP) injections into the affected joint. There are several possible advantages of PRP as a treatment for OA. First, it is relatively easy to use because its preparation is rapid and technically straightforward, and the administration is minimally invasive requiring a simple intra-articular injection which can be performed in the office. Second, it is likely to be safe because the patient’s own proteins are used and bioactive molecules can be appropriately concentrated, thereby avoiding many adverse effects and drug interactions [10••]. Indeed, no major adverse events have been reported in the literature with those that have been reported being minor and transient, including bleeding, tenderness, swelling and/or bruising at the injection site [11•]. Third, PRP is generally not considered a drug or therapeutic substance and, therefore, in many countries, does not have the regulatory requirements that would be needed for other biologic therapies. However, PRP is often costly and, to date, the literature has not provided convincing high quality evidence of its efficacy in the management of OA.
This article will provide a narrative overview of PRP as a treatment for hip and knee OA. Its use for focal cartilage defects and intra-operative and post surgical indications will not be covered. The focus will be on summarising the evidence from randomised controlled trials (RCTs) investigating the clinical effects of PRP in hip and knee OA.
What Is Platelet-Rich Plasma?
PRP is an autologous blood product that contains an elevated concentration of platelets above that of whole blood. While the preparation technique can vary (discussed in detail later in the article), in general, PRP requires venesection of a small amount of peripheral blood followed by centrifugation to concentrate the platelets in plasma. Degranulation of the platelets releases growth factors while the plasma contains cytokines, thrombin and other growth factors with biological and adhesive properties [10••]. Basic centrifugation can follow single- or double-spinning protocols and controversy exists about the effects of these two protocols on separation [10••]. Commercial PRP kits are now also available. The concentration of platelets differs depending on the different systems and manufacturers, gravity forces and times of centrifugation, as well as patient sex and personal physical characteristics. The product is then injected into the joint, sometimes under ultrasound guidance. The generic term ‘PRP’ has been expanded to include a range of final products based on their leukocyte and fibrin content with other terms also used such as autologous conditioned plasma (ACP) and platelet concentrate. Although not covered in this review, other blood therapies that are related to PRP include autologous blood injection whereby venous blood is drawn from the patient and then injected into the area, as well as autologous conditioned serum (currently marketed under the name Orthokine®) where venous blood is prepared in a manner leading to an accumulation of interleukin-1 receptor antagonist and several growth factors.
Proposed Biological Mechanisms of PRP in the Context of Osteoarthritis
Osteoarthritis is a disease affecting all tissues of the joint including the cartilage, bone, ligament and muscle. It has long been considered the result of mechanical overloading causing damage to the joint. However, more recent progress in molecular biology has provided new understandings regarding OA pathophysiology in which inflammatory mediators, growth factors, chondrocyte apoptosis and imbalance between anabolic and catabolic mechanisms play an important role [12]. It is now thought that inflammation might be a major driver of the OA process, rather than inflammation being a secondary consequence of the disease. Several cytokines, such as interleukin-1β and transforming growth factor β, proteases and nitric oxide synthetase all appear to be essential for cartilage degradation in the pathogenesis of OA [12].
Although the biology of PRP is not completely understood, PRP may be beneficial in OA by interfering with catabolic and inflammatory events and by subsequently promoting anabolic responses. Activation of PRP releases an initial burst then a sustained release of biologically active growth factors and other molecules, including platelet-derived growth factor, transforming growth factor-β, type I insulin-like growth factor and vascular endothelial growth factor [13]. These proteins are responsible for a range of critical tissue healing roles such as chondrocyte apoptosis inhibition, bone and vessel remodelling, inflammatory modulation and, importantly, collagen synthesis [13, 14]. Additionally, other bioactive molecules released by platelets, such as fibrin, act as a scaffold and chemo-attractant for further migration of stem and other cells to the damaged tissue that trigger a healing response [13].
In general, pre-clinical literature provides support for the potential use of PRP injections to regenerate damaged joint tissue in OA due to its influence on the whole joint environment. In vitro studies mostly show a positive effect of PRP on cartilage with increases in chondrocyte proliferation without affecting chondrogenesis and enhanced production of type II collagen and proteoglycans [15,16,17]. Effects on meniscal cells [18] and synoviocytes [19] have also been reported. In studies using animal models of OA, PRP has been reported as leading to better cartilage regeneration [20], although this is not necessarily a consistent finding [21]. There is evidence that PRP has a complex role in inflammation with an initial pro-inflammatory action [22] followed by a reduction in inflammatory molecules [16]. There is also research suggesting a direct analgesic effect via augmentation of certain cannabinoid receptors [23].
Thus, the basic science evidence showing that PRP enhances the repair and slows deterioration of tissue provides at least biological plausibility for the use of PRP as a disease-modifying therapeutic modality in OA. Even if PRP does not lead to cartilage regeneration, it may still offer symptomatic and functional benefits via modulation of inflammation and direct analgesia. For more detailed accounts of the basic science PRP literature in relation to OA, readers are referred to reviews by Zhu et al. [10••] and Filardo et al. [24].
Effects on Osteoarthritis Symptoms
Although PRP has been used in various medical fields including dentistry, dermatology and ophthalmology, to name a few, its use to treat OA is relatively recent. This section summarises the evidence, with a focus on RCTs, investigating the efficacy and comparative effectiveness of PRP in the management of hip and knee OA.
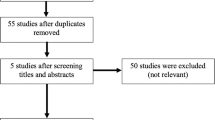
The first investigation into the use of intra-articular PRP injections to treat OA was a retrospective observational study of 60 patients with knee OA published by Sanchez et al. [25] in 2008. It was not until 2012 that the first RCT was published and, to our knowledge, there have now been 15 RCTs in knee OA and three in hip OA (published in English) to date (Table 1), reflecting the growing interest in PRP for treating this condition. However, the literature is often difficult to interpret given methodological concerns (such as questionable blinding, failure to conceal allocation, selective reporting, small sample sizes and inappropriate statistical analyses [11•, 44•]) and considerable heterogeneity between studies in terms of patient populations, outcome measures and PRP regimens. The latter, in particular, is problematic as variations in PRP preparation affect the biological activity of PRP and potentially patient outcomes. The long-term effects of PRP are also not clear given that the RCTs are confined to follow-ups of 12 months or less.
Only three studies [30••, 34, 35] including one designed as a feasibility study [35], all in patients with knee OA, have evaluated the efficacy of PRP by comparing it to placebo (saline). All reported significant benefits of PRP at 6 or 12 months in the PRP group compared to placebo although methodological issues (such as small sample sizes in each group, inappropriate statistics and lack of improvement in the placebo group, which goes against the well documented placebo effect with saline injection [45]), limit the conclusions that can be drawn.
The majority of RCTs in knee OA [26,27,28,29, 30••, 31, 32, 35, 36, 38,39,40] and all three in hip OA [41, 42•, 43] have compared PRP to HA, a commonly used intra-articular therapy. Results of RCTs at the hip have been conflicting. While the study by Dallari et al. [42•] found significantly reduced pain with PRP at 2 and 6 months, but not 12 months, compared with HA, the two other studies failed to find differences between groups, although this could be due to limited statistical power due to small sample sizes in each group [41, 43]. At the knee, most, but not all, studies reported significantly greater improvements in clinical outcomes with PRP compared with HA. These benefits have been seen up until 12 months follow-up, although they appear to decline over time. However, while results may be statistically significant, the magnitude of the effect of PRP can be small bringing into question the clinical relevance of the improvements. It is possible that PRP may also have different effects depending on patient characteristics. There is suggestion that PRP may be more effective in younger patients with less severe structural damage [30••, 38].
While HA has been the comparator for most OA PRP trials to date, HA itself is controversial. It could be argued that it is more important to compare PRP to other more accepted treatments commonly used in the management of OA, such as exercise and analgesics, although this has received little research attention. One small study in knee OA found no difference between PRP and exercise plus transcutaneous electrical nerve stimulation, although it was likely underpowered [33] while another trial showed that PRP resulted in better clinical outcomes compared to acetaminophen (500 mg every 8 h) [37]. However, this result may be explained by lack of blinding given that oral products have much smaller placebo effects than injectable products [45]. The only other comparative effectiveness trial found PRP to be more efficacious at 12 months compared to ozone therapy, a controversial alternative medicine therapy not recommended in the management of OA [39].
Although there has been a large number of systematic reviews in the field [24, 46,47,48,49,50,51,52,53], these have generally included observational studies given the lack of RCTs at the time of review. Two recent systematic reviews have confined their analyses to RCTs [11•, 44•]. Kanchanatawan et al. [11•] included nine RCTs that compared PRP to either HA or placebo in patients with knee OA [11•]. Meta-analysis found significantly better outcomes with PRP on some clinical measures but not others when compared with HA but no differences when compared with placebo. Rates of adverse events were similar between groups. Limitations of this review include the small number of studies pooled in the different analyses for the various outcomes and the medium to high risk of bias in the studies. A greater number of RCTs (n = 14 in knee OA) were included in the systematic review by Shen et al. [44•], but again none of the studies were deemed to have a low risk of bias. Meta-analysis revealed significant benefits of PRP for knee pain and physical function at 3, 6 and 12 months post treatment compared with other intra-articular injections combined. However, blinding of participants, which is crucial to controlling placebo effects (that are large in injectable osteoarthritis trials [45]), was only deemed to have been successfully performed in around half the trials. This is likely to overestimate the reported effects of PRP. Importantly, PRP has been found to be a safe treatment. Side effects are few and minor such as tenderness at the injection site.
While most studies have evaluated PRP as a monotherapy for OA, PRP could be given in combination with other therapies in clinical practice. It has been postulated that PRP may have an additive effect with HA. This has been examined in two RCTs, one in 105 patients with knee OA [36] and the other in 111 patients with hip OA [42•]. However, the studies reported conflicting results. In the knee OA study, the combination of PRP and HA led to better pain and function outcomes up to 1 year when compared with HA alone and better function outcomes up to 3 months when compared with PRP alone [36]. Conversely, the hip OA trial found that PRP alone was actually more effective than the combination of PRP and HA at 2, 6 and 12 month follow-up [42•]. The authors suggested that the diminution of benefit could be due to dilution in the amount of PRP growth factors or excessive capsular distension. Differences between studies may reflect differences in the joint affected, sample demographics and PRP protocol. Further research is needed in this area including the effects with concurrent use of non-steroidal anti-inflammatories, corticosteroids and analgesics. This research area needs to be particularly cognisant of the risks of interactions, adverse events and costs associated with combination of pharmacologic products.
In summary, on the basis of current evidence from RCTs and meta-analyses, there is some support for a positive effect of PRP on clinical outcomes and benefits over and above that of another intra-articular injection therapy (HA). However, given the moderate to high risk of bias in the RCTs to date, short-term follow-up and limited number of studies comparing to placebo, further research is needed to allow definitive conclusions to be drawn about the effects of PRP in people with OA. A greater number of studies also need to compare PRP to core recommended non-surgical, non-drug treatments such as exercise and weight loss. Furthermore, given fiscally constrained health care environments, clinical trials should also include a health economic evaluation so that the cost-effectiveness of PRP can be determined.
Preparation and Injection Protocol
In the literature (Table 2) and clinically, a variety of PRP protocols are used. This reflects the lack of evidence supporting one particular protocol over another. It is evident there are many unanswered questions with regard to the best volume and formulation of PRP, the number and frequency of injections, the use of a single- or double-spinning cycle, the speed and duration of spins to isolate the PRP, the leukocyte concentration, whether an activating agent is necessary, and injection procedures such as the use of ultrasound guidance, co-administration with a local anaesthetic and the injection approach.
Platelet-rich plasma can be prepared, frozen and then re-thawed before injection or used fresh without freezing. While freezing has the advantage of not requiring additional patient venesection when using multiple injections, the majority of studies use fresh PRP because it is perceived to be more effective. While this has not been formally tested, it is interesting to note that out of the six studies using re-thawed PRP, only two (33%) reported beneficial effects above the control group [34, 42•] compared to over 80% of trials using fresh PRP.
Most RCTs in OA have administered PRP injections weekly; however, others have used fortnightly, every 3-week and monthly injections. Injection volumes have ranged from 3 to 8 mL with 5 and 8 mL the most commonly reported volumes. Between one and four PRP injections have been used, with the most common being three injections. Two RCTs [30••, 34] have directly compared the effect of different injection numbers on patient outcomes. One found that both one and two PRP injections led to significantly greater improvements compared with saline at 6 months follow-up, but no difference between the two PRP regimens [30••]. However, the sample size was small and likely underpowered for these between-treatment group comparisons. Conversely, the other study showed that three knee injections were significantly better in terms of pain and function compared to a single injection in patients with early OA but not for patients with advanced OA [34].
Different activation methods are likely to affect the concentration of growth factors. Regarding activating agents, most RCTs have used calcium to activate platelets; however, some do not activate platelets prior to injection and many do not report whether they used an activating agent or not. In fact, some authors suggest exogenous activation of PRP may not be necessary given activation can also be achieved through endogenous mechanisms following injection [54].
Perhaps one of the most variable aspects of the PRP preparation protocol is the centrifugation process, with studies using single- or double-spin protocols, inconsistent spin speed and times and inconsistent reporting. This has compounded the uncertainty regarding which aspects of the PRP preparation protocol are optimal. Of the studies that have used a single-spin protocol, most used spin speeds around 1500 rpm and spin times around 8 min. While these relatively slow and short spin protocols are effective at isolating and concentrating platelets and plasma, they also specifically aim to exclude leukocytes, and neutrophils in particular, thus creating a leukocyte-poor PRP [55•]. In contrast, the studies that have used a double-spinning approach generally used spin speeds and times of up to 3400 rpm and 15 min for the second spin. This longer and faster centrifugation process aims to capture and concentrate as many platelets as possible; however, in doing so, the technique also harvests leukocytes [55•]. This preparation is said to yield a leukocyte-rich PRP product, although there is at least one reported exception [37]. Leukocytes are a controversial PRP component [24]. Some believe that better outcomes are gained with leukocyte-poor PRP because of supposed deleterious effects of reactive oxygen species and proteases released from white cells. Others consider leukocytes as a source of cytokines and enzymes that may also be important for infections [56]. Riboh et al. [57••] conducted a meta-analysis comparing leukocyte-poor and leukocyte-rich PRP for the management of knee OA. They included six RCTs and three observational studies. They found that injection of leukocyte-poor PRP resulted in significantly better WOMAC scores than did injection of HA and placebo whereas no such difference was observed with leukocyte-rich PRP. Both types of PRP had similar safety profiles although both seemed to induce more transient reactions than HA.
No RCT has directly compared single and double-spin PRP protocols. However, a non-randomised trial allocated knee OA participants to one of two centres, with each centre preparing PRP using one of the two spin protocols [56]. The study found no significant difference in pain and functional outcomes up to 12 months; however, more adverse events were reported by those who received PRP produced using a double-spin protocol. This latter finding was attributed to the higher concentration of leukocytes in this approach, which can produce a greater number of pro-inflammatory mediators [58], thereby potentially triggering an acute inflammatory response.
In addition to the variety of methods used to prepare PRP, there is also variation in the injection protocols used to deliver PRP in to the knee and hip joints. Relatively few studies have used a local anaesthetic prior to infiltration of PRP, possibly due to concerns from in vitro research showing that anaesthetics may reduce platelet aggregation [59]. However, it is unclear whether a local subcutaneous injection of a local anaesthetic, as opposed to an intra-articular injection, would have similar adverse effects on platelet function. Only two knee OA RCTs performed the PRP injection under ultrasound guidance, whereas ultrasound was used in all of the hip OA studies. This is somewhat surprising given the use of ultrasound for intra-articular knee injections has been shown to improve injection accuracy, clinical outcomes and cost-effectiveness and to reduce procedural pain [60,61,62]. A variety of injections sites have been used in knee OA studies. Finally, while both hip OA studies that reported the injection approach used lateromedial and caudocranial directions, the injection approach varied widely in the knee OA studies. It is currently unknown whether one approach has more favourable outcomes on the effects of PRP in knee and hip OA.
Currently, the optimal PRP preparation and injection protocol is unknown. However, based on PRP protocol characteristics from previous RCTs reporting positive findings, taking fresh blood prior to each injection, using a single slower and shorter spin, at around 1500 rpm and for around 5–8 min to prepare leukocyte-poor PRP, and administering three injections at weekly intervals may be an appropriate protocol to test in future trials. It is also important that reporting of PRP protocols in trials is improved. DeLong et al. [55•] propose a classification system (PAW) based on three components: (1) the absolute number of platelets, (2) the manner in which platelet activation occurs, and (3) the presence or absence of white cells. This will allow more accurate comparison of protocols and results and effective grouping of studies together for meta-analysis.
Effects on Joint Structure
Although there is biologic plausibility for a structural benefit arising from PRP, to date, there are no published RCTs in OA that include structural outcomes. Two uncontrolled case series show a potential benefit. Using ultrasonography, Sampson and colleagues [63] reported that nearly 50% of their 13 patients with knee OA showed greater cartilage volume at the lateral and medial femoral condyles, as well as the intercondylar notch, at 6 months following three PRP injections administered at monthly intervals. However, the use of ultrasound to quantify knee cartilage has limitations and the study was underpowered to detect meaningful within-group changes. Another uncontrolled study involved 15 patients with no or early knee OA (based on Kellgren and Lawrence grades 0 to 2) who received a single PRP injection [64]. The study found no significant structural worsening at 12-month follow-up assessed using the Outerbridge score on magnetic resonance imaging in 73% of those with medial compartment involvement, 80% of those with patellofemoral involvement and 83% of those with lateral compartment involvement. However, given the lack of a control group in both studies, no conclusions can be made at this time about the ability of PRP to slow structural disease progression in those with knee or hip OA. Studies using MRI to assess joint structural changes [65] with PRP are needed.
Clinical Implications
Current clinical guidelines either do not mention [7, 66, 67] or are unable to recommend for or against the use of PRP for the management of OA [68], based on the lack of high-quality studies and questions regarding the clinical relevance of statistically significant findings of some studies. Clarity around its efficacy and the appropriate protocol are required before guidelines are likely to change their current position. In many countries, PRP treatment is not covered by insurance bodies and therefore must be borne by the patient. This raises the issue of access for many patients. Given that PRP can be relatively expensive and that clinical guidelines currently provide no recommendations, clinicians should be cautious in its use. Instead, we recommend that knee OA is managed using core treatments of education, exercise and, if appropriate, weight loss [6]. If PRP is to be offered, we suggest that clinicians inform patients about the inconclusive evidence supporting its use so that patients can make an informed decision about whether or not to consent to this currently unproven therapy.
Conclusions
Collectively, basic science and clinical studies suggest that PRP could be a promising non-operative treatment for OA. Evidence from studies of low to moderate methodological quality show that intra-articular PRP injection therapy is a safe treatment with potential to provide symptomatic benefit for OA at least in the short term (up to 12 months) and more efficacious than those of HA. These results need to be confirmed in high-quality RCTs. While there is some suggestion that younger patients and those with less structural change may be more responsive to PRP, further research is needed to establish whether patient characteristics moderate PRP outcomes. Effects of PRP on OA structural disease progression are unknown due to lack of studies in this area. Currently, no recommendations can be made about the optimal PRP protocol for patients with OA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarth Cart. 2011;19:1270–85. doi:10.1016/j.joca.2011.08.009.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 Study. Ann Rheum Dis. 2014;73:1323–30. doi:10.1136/annrheumdis-2013-204763.
Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective: a population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs. 2012;31:85–91. doi:10.1097/NOR.0b013e31824fcd42.
United Kingdom National Joint Registry. 12th Annual Report. 2015.
Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarth Cart. 2010;18:476–99. doi:10.1136/ard.2009.113100.
Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the U.S. Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43:701–12. doi:10.1016/j.semarthrit.2013.11.012.
McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014;22:363–88. doi:10.1016/j.joca.2014.01.003.
Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, et al. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373:1597–606. doi:10.1056/NEJMoa1505467.
Boutron I, Rannou F, Jardinaud-Lopez M, Meric G, Revel M, Poiraudeau S. Disability and quality of life of patients with knee or hip osteoarthritis in the primary care setting and factors associated with general practitioners’ indication for prosthetic replacement within 1 year. Osteoarth Cart. 2008;16:1024–31. doi:10.1016/j.joca.2008.01.001.
•• Zhu Y, Yuan M, Meng HY, Wang AY, Guo QY, Wang Y, et al. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarth Cart. 2013;21:1627–37. doi:10.1016/j.joca.2013.07.017. This paper is a very useful review of the biology of PRP and outlines some of the key early pre-clinical and clinical studies.
• Kanchanatawan W, Arirachakaran A, Chaijenkij K, Prasathaporn N, Boonard M, Piyapittayanun P, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1665–77. doi:10.1007/s00167-015-3784-4. A recent systematic review and meta-analysis that included only RCTs.
Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarth Cart. 2013;21:16–21. doi:10.1016/j.joca.2012.11.012.
Sundman EA, Cole BJ, Karas V, Della Valle C, Tetreault MW, Mohammed HO, et al. The anti-inflammatory and matrix restorative mechanisms of platelet-rich plasma in osteoarthritis. Am J Sports Med. 2013; doi:10.1177/0363546513507766.
Drengk A, Zapf A, Stürmer EK, Stürmer KM, Frosch K-H. Influence of platelet-rich plasma on chondrogenic differentiation and proliferation of chondrocytes and mesenchymal stem cells. Cells Tissues Organs. 2008;189:317–26.
Muraglia A, Ottonello C, Spano R, Dozin B, Strada P, Grandizio M, et al. Biological activity of a standardized freeze-dried platelet derivative to be used as cell culture medium supplement. Platelets. 2014;25:211–20. doi:10.3109/09537104.2013.803529.
Wu CC, Chen WH, Zao B, Lai PL, Lin TC, Lo HY, et al. Regenerative potentials of platelet-rich plasma enhanced by collagen in retrieving pro-inflammatory cytokine-inhibited chondrogenesis. Biomaterials. 2011;32:5847–54. doi:10.1016/j.biomaterials.2011.05.002.
Akeda K, An HS, Okuma M, Attawia M, Miyamoto K, Thonar EJMA, et al. Platelet-rich plasma stimulates porcine articular chondrocyte proliferation and matrix biosynthesis. Osteoarth Cart. 2006;14:1272–80. doi:10.1016/j.joca.2006.05.008.
Ishida K, Kuroda R, Miwa M, Tabata Y, Hokugo A, Kawamoto T, et al. The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng. 2007;13:1103–12. doi:10.1089/ten.2006.0193.
Anitua E, Sanchez M, Nurden AT, Zalduendo MM, de la Fuente M, Azofra J, et al. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology (Oxford). 2007;46:1769–72. doi:10.1093/rheumatology/kem234.
Kwon DR, Park GY, Lee SU. The effects of intra-articular platelet-rich plasma injection according to the severity of collagenase-induced knee osteoarthritis in a rabbit model. Ann Rehabil Med. 2012;36:458–65. doi:10.5535/arm.2012.36.4.458.
Guner S, Buyukbebeci O. Analyzing the effects of platelet gel on knee osteoarthritis in the rat model. Clin Appl Thromb Hemost. 2013;19:494–8. doi:10.1177/1076029612452117.
Pereira RC, Scaranari M, Benelli R, Strada P, Reis RL, Cancedda R, et al. Dual effect of platelet lysate on human articular cartilage: a maintenance of chondrogenic potential and a transient proinflammatory activity followed by an inflammation resolution. Tissue Eng Part A. 2013;19:1476–88. doi:10.1089/ten.TEA.2012.0225.
Lee HR, Park KM, Joung YK, Park KD, Do SH. Platelet-rich plasma loaded hydrogel scaffold enhances chondrogenic differentiation and maturation with up-regulation of CB1 and CB2. J Control Release. 2012;159:332–7. doi:10.1016/j.jconrel.2012.02.008.
Filardo G, Kon E, Roffi A, Di Matteo B, Merli M, Marcacci M. Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc. 2013;9:1–16. doi:10.1007/s00167-013-2743-1.
Sanchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26:910–3.
Cerza F, Carni S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, et al. Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis. Am J Sports Med. 2012;40:2822–7. doi:10.1177/0363546512461902.
Filardo G, Kon E, Di Martino A, Di Matteo B, Merli M, Cenacchi A, et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord. 2012a;13:229. doi:10.1186/1471-2474-13-229.
Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, Garcia Gutierrez A, et al. A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy. 2012;28:1070–8. doi:10.1016/j.arthro.2012.05.011.
Vaquerizo V, Plasencia MA, Arribas I, Seijas R, Padilla S, Orive G, et al. Comparison of intra-articular injections of plasma rich in growth factors (PRGF-Endoret) versus Durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: a randomized controlled trial. Arthroscopy. 2013;29:1635–43. doi:10.1016/j.arthro.2013.07.264.
•• Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41:356–64. doi:10.1177/0363546512471299. This was the first study to compare PRP to placebo and found superior clinical effects at 6 months.
Raeissadat SA, Rayegani SM, Hassanabadi H, Fathi M, Ghorbani E, Babaee M, et al. Knee osteoarthritis injection choices: platelet-rich plasma (PRP) versus hyaluronic acid (a one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. doi:10.4137/CMAMD.S17894.
Filardo G, Di Matteo B, Di Martino A, Merli ML, Cenacchi A, Fornasari P, et al. Platelet-rich plasma intra-articular knee injections show no superiority versus viscosupplementation: a randomized controlled trial. Am J Sports Med. 2015;43:1575–82. doi:10.1177/0363546515582027.
Angoorani H, Mazaherinezhad A, Marjomaki O, Younespour S. Treatment of knee osteoarthritis with platelet-rich plasma in comparison with transcutaneous electrical nerve stimulation plus exercise: a randomized clinical trial. Med J Islam Repub Iran. 2015;29:223.
Gormeli G, Gormeli CA, Ataoglu B, Colak C, Aslanturk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2015; doi:10.1007/s00167-015-3705-6.
Smith PA. Intra-articular autologous conditioned plasma injections provide safe and efficacious treatment for knee osteoarthritis: an FDA-sanctioned, randomized, double-blind, placebo-controlled clinical trial. Am J Sports Med. 2016;44:884–91. doi:10.1177/0363546515624678.
Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12:69–78.
Simental-Mendia M, Vilchez-Cavazos JF, Pena-Martinez VM, Said-Fernandez S, Lara-Arias J, Martinez-Rodriguez HG. Leukocyte-poor platelet-rich plasma is more effective than the conventional therapy with acetaminophen for the treatment of early knee osteoarthritis. Arch Orthop Trauma Surg. 2016;136:1723–32. doi:10.1007/s00402-016-2545-2.
Montanez-Heredia E, Irizar S, Huertas PJ, Otero E, Del Valle M, Prat I, et al. Intra-articular injections of platelet-rich plasma versus hyaluronic acid in the treatment of osteoarthritic knee pain: a randomized clinical trial in the context of the Spanish National Health Care System. Int J Mol Sci. 2016;17 doi:10.3390/ijms17071064.
Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc. 2016; doi:10.1007/s00167-016-4110-5.
Paterson KL, Nicholls M, Bennell KL, Bates D. Intra-articular injection of photo-activated platelet-rich plasma in patients with knee osteoarthritis: a double-blind, randomized controlled pilot study. BMC Musculoskelet Disord. 2016;17:67. doi:10.1186/s12891-016-0920-3.
Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, et al. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013;36:e1501–8.
• Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P, et al. Ultrasound-guided injection of platelet-rich plasma and hyaluronic acid, separately and in combination, for hip osteoarthritis: a randomized controlled study. Am J Sports Med. 2016;44:664–71. doi:10.1177/0363546515620383. One of the few RCTs in hip OA and also investigates the effects of PRP alone and in combination with HA.
Di Sante L, Villani C, Santilli V, Valeo M, Bologna E, Imparato L, et al. Intra-articular hyaluronic acid vs platelet-rich plasma in the treatment of hip osteoarthritis. Med Ultrason. 2016;18:463–8. doi:10.11152/mu-874.
• Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12:16. doi:10.1186/s13018-017-0521-3. A recent systematic review and meta-analysis that included only RCTs.
Bannuru RR, McAlindon TE, Sullivan MC, Wong JB, Kent DM, Schmid CH. Effectiveness and implications of alternative placebo treatments: a systematic review and network meta-analysis of osteoarthritis trials. Ann Intern Med. 2015;163:365–72. doi:10.7326/M15-0623.
Dold AP, Zywiel MG, Taylor DW, Dwyer T, Theodoropoulos J. Platelet-rich plasma in the management of articular cartilage pathology: a systematic review. Clin J Sport Med. 2014;24:31–43. doi:10.1097/01.jsm.0000432855.85143.e5.
Tietze DC, Geissler K, Borchers J. The effects of platelet-rich plasma in the treatment of large-joint osteoarthritis: a systematic review. Phys Sportsmed. 2014;42:27–37. doi:10.3810/psm.2014.05.2055.
Lai LP, Stitik TP, Foye PM, Georgy JS, Patibanda V, Chen B. Use of platelet-rich plasma in intra-articular knee injections for osteoarthritis: a systematic review. PM R. 2015;7:637–48. doi:10.1016/j.pmrj.2015.02.003.
Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy. 2016;32:495–505. doi:10.1016/j.arthro.2015.08.005.
Chang KV, Hung CY, Aliwarga F, Wang TG, Han DS, Chen WS. Comparative effectiveness of platelet-rich plasma injections for treating knee joint cartilage degenerative pathology: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2013; doi:10.1016/j.apmr.2013.11.006.
Khoshbin A, Leroux T, Wasserstein D, Marks P, Theodoropoulos J, Ogilvie-Harris D, et al. The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesis. Arthroscopy. 2013;29:2037–48. doi:10.1016/j.arthro.2013.09.006.
Laudy AB, Bakker EW, Rekers M, Moen MH. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med. 2014; doi:10.1136/bjsports-2014-094036.
Campbell KA, Saltzman BM, Mascarenhas R, Khair MM, Verma NN, Bach Jr BR, et al. Does intra-articular platelet-rich plasma injection provide clinically superior outcomes compared with other therapies in the treatment of knee osteoarthritis? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:2213–21. doi:10.1016/j.arthro.2015.03.041.
Mishra A, Woodall Jr J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med. 2009;28:113–25. doi:10.1016/j.csm.2008.08.007.
• DeLong JM, Russell RP, Mazzocca AD. Platelet-rich plasma: the PAW classification system. Arthroscopy. 2012;28:998–1009. doi:10.1016/j.arthro.2012.04.148. A useful framework for classifying PRP based on platelet and white blood cell concentration, and activation method.
Filardo G, Kon E, Pereira Ruiz MT, Vaccaro F, Guitaldi R, Di Martino A, et al. Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg Sports Traumatol Arthrosc. 2012b;20:2082–91. doi:10.1007/s00167-011-1837-x.
•• Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of leukocyte concentration on the efficacy of platelet-rich plasma in the treatment of knee osteoarthritis. Am J Sports Med. 2016;44:792–800. doi:10.1177/0363546515580787. A systematic review that demonstrated the superiority of leucocyte-poor over leucocyte-rich PRP for clinical outcomes in knee OA.
Braun HJ, Kim HJ, Chu CR, Dragoo JL. The effect of platelet-rich plasma formulations and blood products on human synoviocytes: implications for intra-articular injury and therapy. Am J Sports Med. 2014;42:1204–10. doi:10.1177/0363546514525593.
Bausset O, Magalon J, Giraudo L, Louis M-L, Serratrice N, Frere C, et al. Impact of local anaesthetics and needle calibres used for painless PRP injections on platelet functionality. Muscles, Ligaments Tendons J. 2014;4:18–23.
Sibbitt WL, Kettwich LG, Band PA, Chavez-Chiang NR, DeLea SL, Haseler LJ, et al. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012;41:66–72. doi:10.3109/03009742.2011.599071.
Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging. 2012;7:89–95. doi:10.2147/CIA.S29265.
Sibbitt Jr WL, Band PA, Kettwich LG, Chavez-Chiang NR, DeLea SL, Bankhurst AD. A randomized controlled trial evaluating the cost-effectiveness of sonographic guidance for intra-articular injection of the osteoarthritic knee. J Clin Rheumatol. 2011;17:409–15. doi:10.1097/RHU.0b013e31823a49a4.
Sampson S, Reed M, Silvers H, Meng M, Mandelbaum B. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot study. Am J Phys Med Rehabil. 2010;89:961–9. doi:10.1097/PHM.0b013e3181fc7edf.
Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, et al. Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clin J Sport Med. 2013;23:238–9. doi:10.1097/JSM.0b013e31827c3846.
Eckstein F, Charles HC, Buck RJ, Kraus V, Remmers AE, Hudelmaier M, et al. Accuracy and precision of quantitative assessment of cartilage morphology by magnetic resonance imaging at 3.0T. Arthritis & Rheum. 2005;52:3132–26. doi:10.1002/art.21348.
National Institute for Health and Care Excellence (UK). Osteoarthritis: Care and Management in Adults. National Clinical Guideline Centre (UK). Clinical Guidelines No. 177. 2014; Feb.
Hochberg MC, Altman RD, Toupin April K, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64:465–74. doi:10.1002/acr.21596.
Jevsevar DS. Treatment of Osteoarthritis of the Knee: Evidence‐Based Guideline. Journal of the American Academy of Orthopaedic Surgeons. 2013;21(9):571–576.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bennell reports grants from National Health and Medical Research Council, outside the submitted work.
Dr. Hunter reports personal fees from Consultant for Merck Serono and Flexion and personal fees from Royalties for patellofemoral brace, outside the submitted work.
Dr. Paterson has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Complementary and Alternative Medicine
Rights and permissions
About this article
Cite this article
Bennell, K.L., Hunter, D.J. & Paterson, K.L. Platelet-Rich Plasma for the Management of Hip and Knee Osteoarthritis. Curr Rheumatol Rep 19, 24 (2017). https://doi.org/10.1007/s11926-017-0652-x
Published:
DOI: https://doi.org/10.1007/s11926-017-0652-x