Abstract
Purpose of Review
We review the literature about patients 50 years and older with a recent clinical fracture for the presence of skeletal and extra-skeletal risks, their perspectives of imminent subsequent fracture, falls, mortality, and other risks, and on the role of the fracture liaison service (FLS) for timely secondary fracture prevention.
Recent Findings
Patients with a recent clinical fracture present with heterogeneous patterns of bone-, fall-, and comorbidity-related risks. Short-term perspectives include bone loss, increased risk of fractures, falls, and mortality, and a decrease in physical performance and quality of life. Combined evaluation of bone, fall risk, and the presence of associated comorbidities contributes to treatment strategies.
Summary
Since fractures are related to interactions of bone-, fall-, and comorbidity-related risks, there is no one-single-discipline-fits-all approach but a need for a multidisciplinary approach at the FLS to consider all phenotypes for evaluation and treatment in an individual patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The high and increasing burden of fractures in subjects older than 50 years has been documented worldwide [1, 2], whereas there are growing insights in fracture prediction and a wide spectrum and availability of treatments to prevent fractures [3,4,5,6]. A fracture is the result of an imbalance between skeletal competence and extra-skeletal factors, such as falls for clinical fractures, and overload activities of the spine for vertebral fractures (VFs) [7,8,9,10]. This imbalance varies substantially between patients with a recent fracture. An acute clinical VF after lifting a bucket full of water in a 65-year-old women suggests a bone-related fracture phenotype. A clavicula fracture after a fall while biking in a man of 65 years suggests a fall/trauma related fracture phenotype. An 85-year-old frail women with a hip fracture after a fall due to slipping and having two prior subclinical morphometric VFs (mVFs) suggests the presence of both fracture phenotypes. A clinical fracture in a patient with rheumatoid arthritis on glucocorticoid treatment suggests a comorbidity (disease/medication)-related fracture phenotype.
After a fracture, the long-term risk of subsequent fracture is doubled, but this risk is not constant over time. It is much higher on the short term than on the long term, the so-called imminent subsequent fracture risk [11,12,13]. A history of fracture is included in the fracture prediction calculators of FRAX, Garvan, and qFracture, in addition to more than 25 other clinical risk factors [14, 15]. Areal bone density (aBMD) measured by dual-energy X-ray absorptiometry (DXA) is included in FRAX and Garvan. Therefore, and not unexpectedly, patients 50 years and older with a recent clinical fracture present with heterogeneous characteristics of bone-, fall-, and comorbidity-related fracture phenotypes, indicating the need for individualized approaches [6, 16]. The concept of the fracture liaison service (FLS) was introduced 20 years ago by McLellan [17]. We here review recent publications on the characteristics and perspectives of patients of 50 years and older with a recent fracture and the role of the FLS and post-fracture care. Orthogeriatric care after hip fracture is outside the scope of this review.
Perspectives after a Recent Clinical Fracture
Imminent Subsequent Fracture Risk
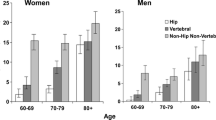
In postmenopausal women, one of the main risk factors of sustaining a fracture is a prior one. On average, the long-term risk is doubled in the presence of a prior fracture. This was confirmed in a recent meta-analysis with 2.1 million women and men between the age of 20 and 116 years and including 64 prospective cohorts in 32 countries [18]. But the subsequent fracture risk is not constant and fluctuates over time. Subsequent fractures cluster in time shortly after the first fracture (Fig. 1) [11, 19].

(adapted from van Geel et all.) [19].
Left panel: the relative risk (RR) of subsequent clinical fractures is doubled over the long term (fine red line). It is highest in the first years after a clinical fracture (bold red line circled in green) and decreases over time but remains increased at long term. Right panel: cumulative incidence of subsequent clinical fractures as percentage of all subsequent clinical fractures for 20 years follow-up. More than 50% of all subsequent clinical fractures occurred during the first five years.
This imminent subsequent fracture risk has been further documented in terms of absolute risk, cumulative incidence, index and subsequent fracture locations, gender, and age, in retrospective studies that considered the competing risk of mortality. They reported on recurrent clinical fractures, major osteoporotic fractures (MOFs; including clinical spine, hip, forearm, and shoulder), clinical VFs or mVFs, and non-vertebral fractures [8, 20,21,22,23,24,25].
The effect of gender on imminent subsequent fracture risk differed according to age and selection of sentinel and subsequent fractures [25, 26]. It was similar between sexes for low trauma fractures after the age of 65 years [27], higher in men for any recurrent clinical fractures (age 50 years and older), and higher in women for recurrent clinical MOFs (mean age 53 years) [8, 22]. The relative risk of recurrent MOFs measured as early as 6 months was similar across all age groups above 60 years. But the 2-year relative risk decreased with age [22]. However, the absolute risk is higher in women older than 80 years compared with those between 50 and 59 years [23].
Thus, any clinical fracture in subjects of 50 year and older is a signal for imminent and long-term subsequent fracture risk, in women and men, and at any age.
Other Imminent Perspectives after a Recent Clinical Fracture
The risk of falls following a fracture increased 2-fold in women and 3-fold in men with the highest risk in the first year after fracture, that gradually declined over time [28]. This finding is consistent with the strong association of falls with subsequent fracture after a FLS visit (Hazard Ratio 8.6 versus no incident fall) [29] and the post-fracture incidences of falls of 19–40% within one year [29, 30]. Furthermore, a history and the number of falls are associated with the risk of fractures, independent of aBMD, in women and men [31].
Physical performance is linked with falls risk. Women and men assessed in a FLS who had poor physical capacity had increased fall risk factors [32]. In men with fracture, there were greater declines in grip strength, sit-to-stand and balance tests post fracture compared with controls, also in muscles distant from the fracture site and for longer than the first year post fracture [33]. Importantly more rapid decline in muscle strength and performance in men has been associated with increased mortality risk [34]. To our knowledge there have not been any studies examining post fracture decline in muscle strength and performance in women. However, decline in muscle strength and performance has been associated with increased fracture risk in both women and men [35]. Together with physical performance fractures result in a decline in quality of life (QoL), particularly in the first year after fracture [36].
Both women and men experience significant early bone loss in both spine and femoral neck regions following fracture [37]. Individuals experiencing the highest rates of bone loss following a fracture have up to 2-fold higher mortality risk compared to those without bone loss [38].
Undoubtedly, the most severe consequence of clinical fracture is premature mortality risk in women and men [15]. This has been documented after hip, femur, pelvis, vertebral, clavicula, rib, and humerus fracture, and particularly in older patient groups [26, 39, 40]. The excess mortality risk is highest immediately after the fracture and declines afterwards towards the general population mortality rates [41]. Subsequent fracture further increases the excess mortality [39]. Importantly, the long-term excess mortality after an initial fracture is primarily due to that related to a subsequent fracture [42].
Health status of the individuals at the time of fracture is one of the most important predictors of post-fracture adverse events. In a nationwide Danish study, researchers demonstrated that chronic conditions are common at the time of fracture and cluster in four groups. These included low multimorbidity, cardio-vascular, diabetic, and malignant, for both women and men, with an additional inflammatory/hepatic group in men only. Importantly all these identified clusters were associated with excess mortality risk, especially in people with hip, vertebral, and proximal or lower leg fracture [15, 43, 44].
Therefore, it is imperative to incorporate factors such as bone loss, susceptibility to falls, decline in physical performance and QoL into the assessment of imminent risks of subsequent fracture and mortality post-fracture. Furthermore, physicians should consider the complex health status of patients when making decisions regarding the evaluation or treatment of recent fracture.
Characteristics of Patients 50 Years and Older with a Recent Fracture
Bone-related Fracture Phenotypes are more Diverse than Reflected by aBMD: Microarchitecture of Bone
Osteoporosis is characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to reduced bone strength and an increased fracture risk. Low bone mass, measured by aBMD, is a major contributor to bone strength and thus has been the prominent attribute to assess fracture risk [45]. But it should be considered clinically as a risk factor for fracture among many other clinical risks [14]. Between subjects with or without a prior fracture, low aBMD accounted for only 14% of the difference in the 10-year risk of any clinical fracture [18]. Thus, other factors beyond aBMD contribute to overall bone strength [46]. Consequently, use of aBMD alone has suboptimal sensitivity in predicting fracture [18]. Bone microarchitecture, material properties, and geometry have been linked to increased fracture risk [47], independent of aBMD [48,49,50,51] and of FRAX [48, 50]. Patients at risk of fragility fractures typically have disrupted bone microarchitecture and reduced volumetric BMD (vBMD), measured by HR-pQCT [47]. However, the type of structural disruption varies among older individuals. Deteriorated trabecular architecture and/or diminished cortical structure (including bone size) have been associated with increased fracture risk [48, 52]. There has been growing recognition that bone attributes should be considered in the context of one another. Several strategies have been proposed, including defining microarchitectural phenotypes with unsupervised machine learning and medical imaging [53, 54] and formulation of a structural fragility score (SFS) [50, 55]. This approach has shown promise in improving stratification of fracture risk in older adults. Machine learning methods have aided in developing fracture risk assessment tools that accounts for the complex combination of bone microarchitecture and density properties [56]. Other measures of bone architecture, such as femoral neck architecture [57] and the trabecular bone sore (TBS), have been recently reviewed elsewhere [58, 59].
The Particular Case of Vertebral Fracture
Of all fractures, VFs are the most frequent. They are the most pronounced clinical representation of deteriorated microarchitecture and decreased bone strength, independent of aBMD [45, 60, 61] and of clinical risk factors [62, 63]. Thus, patients with a VF represent a distinct hallmark of a severe bone-related fracture phenotype [54].
The estimation of an individual’s future fracture risk at the FLS is based on clinical risk factors and measurement of aBMD by DXA [6, 64]. It can thus be enhanced by imaging of the spine for presence or absence of VFs [62, 63, 65]. Subjects with a VF have a five times higher risk for new VF and a two times higher risk for any subsequent fracture, independent of aBMD, and in proportion with their number and severity [64, 66]. In the placebo groups of randomized controlled trials 35.1% of participants with a baseline VF had a new VF within 4 years, and 17.4% an incident non-VF [67].
Imaging techniques for detecting VFs include vertebral fracture assessment (VFA) on conventional radiographs and DXA images [64]. Compared with standard radiography, DXA-VFA is less expensive, involves less ionizing radiation, and is more convenient since it can be performed at the same visit as DXA-aBMD measurement. MRI and CT are costly procedures and usually only performed in difficult cases or for opportunistic screening [68].
In contrast to non-VFs, only one out of four VFs are clinically diagnosed as new or worsening back pain [64]. They are consequently underdiagnosed, even on available radiographs [69]. While non-VFs are often related to falls, most VFs occur during daily activities such as lifting, holding, and non-symmetric activities, without overt trauma [10].
Reasons to perform DXA-VFA in patients visiting the FLS are that subclinical VFs are frequent. Second, that it allows physicians to discriminate between high-risk patients, usually treated with antiresorptive drugs, and very high-risk patients, in whom the osteoanabolic drugs (parathyroid hormone analogues or romosozumab) are considered. In the presence of a low aBMD with one or more moderate or severe VFs, they are superior for fracture prevention over bisphosphonates. Third, a baseline VFA allows to identify new VFs during follow up [64].
The implementation of DXA-VFA is limited by barriers, e.g., unawareness of the prognostic importance of VFs by patients and physicians [70, 71]. However, successful implementation of the Dutch guideline to combine aBMD with VFA at the FLS increased DXA-VFA from 4.7 to 97.1% and diagnosed VFs (grade ≥ 2) from 0.9 to 14.7% [72]. Targeted VFA imaging at the time of DXA substantially improved the prescription of fracture prevention medication, from 28.4 to 52.3% [66]. A novel approach is to use Artificial Intelligence (AI) to reanalyze existing CT scans in the hospital to identify patients with undiagnosed and untreated VFs [73].
DXA-VFA is therefore advocated in all patients visiting the FLS to have a full fracture history, to refine bone-related risk evaluation, and for treatment decisions.
The Need for Evaluation besides Bone
The FRAX, Garvan, and qFracture risk estimation algorithms moved management of osteoporosis from the binary presence or absence of osteoporosis based on WHO criteria to a range of fracture risk from very high to low. All include a prior fracture as a risk for subsequent fracture and aBMD in FRAX and Garvan [14].
Patients with a recent clinical fracture at the FLS can therefore have, besides low aBMD and the presence of VFs, additional risk factors that are associated with the occurrence of a sentinel and subsequent fracture. The FRAXplus has added (for a fee), additional assessment of recency and site of previous fracture, falls, lumbar spine BMD, Type 2 diabetes, and high exposure to oral glucocorticoids, but only as single risk adjustments. Three or more falls in the last year had the highest impact (https://www.fraxplus.org/on/).
Fractures Secondary to Other Diseases: Examples of Comorbidity-Related Fracture Phenotypes
Around 25% of patients visiting the FLS report known associated metabolic bone diseases. This was documented in women and men, at any age, after any fracture, and at any level of aBMD [74] and are also reported in patients with a recent fracture in primary care [75].
It is critical to exclude secondary causes of osteoporosis in patients with fragility fractures even when traditional clinical risk factors for osteoporosis are present [76], as associated diseases may contribute to osteoporosis severity or inadequate treatment responses [76].
Rare diseases presenting with fractures as a first symptom should also be considered in the presence of specific clinical presentations. Examples are multiple VFs with typical skin involvement (such as urticaria pigmentosa (maculopapular cutaneous in mastocytosis)), blue sclerae and childhood fractures (osteogenesis imperfecta), proximal muscle weakness and low fasting serum phosphate (tumor induced osteomalacia), and weight gain with diabetes (Cushing’s disease). Myeloma and monoclonal gammopathy of undetermined significance (MGUS) remain important diseases to diagnose. Early diagnosis of myeloma predicts survival, and 1% of (MGUS) patients will transform annually to myeloma [77]. Hypophosphatasia can present with fragility fractures, typically of the metatarsals, and occasionally with atypical femoral fractures with low serum alkaline phosphatase. For these patients routine use of bisphosphonates should be avoided unless under expert center advice [78].
Fall-Related Fracture Phenotype
The most prominent extra-skeletal risk for fractures is the risk of falls. Fall risks were reported in the medical history by 35% at 50–59 years and up to 60% in 80+, on top of the falls that resulted in the current fracture [29, 79].
The 2022 “World guidelines for falls prevention and management for older adults: a global initiative” provide a framework for identifying the high-risk faller after an injurious fall and present assessment and treatment recommendations [79]. Falls risk evaluation and fall prevention strategies have been recently reviewed in a meta-analysis [80].
Other Considerations for Evaluation at the FLS
All evaluations at the FLS should also consider general health, cognitive status, mental, emotional, and social health, as well as mortality risk. These factors contribute to not only imminent subsequent fracture risk, but also the likelihood of adherence to therapy. This can help in the selection of patients for evaluation, types of treatment recommended, and methods of monitoring [9].
The role of patient communication and co-decision making is receiving increasing attention [81,82,83,84]. In patients at high risk and lower health literacy, this needs to be considered when delivering effective communication with the patient about why bone health evaluation and treatment is important from the patient’s perspective.
Evaluation and integration of secondary causes of bone fragility, comorbidities, and fall risk are therefore important considerations for an FLS to deliver on reducing fracture risk for its patients.
The Fracture Liaison Service
The FLS has been widely regarded as the most effective organizational approach for the prevention of subsequent fractures in subjects 50 years of age and older [6, 85]. Recent studies and meta-analyses have demonstrated that interventions by a well-structured FLS have resulted in a significant increase in clinical evaluation, the prescription of DXA measurement of aBMD, laboratory and falls risk evaluation, diagnosis and treatment of underlying diseases, adequate calcium, vitamin D, and protein intake, treatment initiation based on further specification of very high risk after a recent fracture, and taking into account the additional risk factors according to the patient’s phenotype and persistence of treatment [85, 86]. Systematic implementation of VFA by DXA increased diagnosis of subclinical VFs from 2.2 to 26.6% [72]. Most importantly, several studies and meta-analyses of FLS care have indicated a decrease in the risk of subsequent fractures and mortality [87, 88].
However, studies that have examined the efficacy of FLS care in reducing the risk of subsequent fractures and mortality are heterogeneous in study design (i.e., comparing post-FLS versus pre-FLS care or comparing hospitals with and without FLS), age, the type of index fractures, classifications of fracture groups, duration of follow-up, and lack of a competing mortality risk analysis [85, 88].
There are still challenges and gaps in the care of fragility fracture patients that need to be addressed. Several factors are independently associated with non-attendance, including older age, male gender, frailty, living alone, low income, having a low general education, having a low interest in bone health, not perceiving the risk of subsequent fracture risk, and, most importantly, the lack of perceiving to have had advice to have a DXA and a visit at the FLS [70]. Adherence declines during follow up [89, 90]. Enhancements in clinical governance frameworks are crucial for optimizing the effects of FLS care [85].
Even in FLS attenders who are treated with anti-osteoporosis medication, subsequent fractures still occur. A recent study by Vranken et al. in FLS attenders, adequately evaluated and treated according to the Dutch Guideline, showed that the 3-year subsequent fracture incidence was 10%. Incident falls were the main cause of these subsequent fractures [29]. Furthermore, there is an imminent fall risk after a fracture regardless of age or type of index fracture [28].
Current research on the impact of subsequent fracture prevention at the FLS is mainly based on treatment with anti-resorptive dugs [91]. Anabolic treatments are more effective in reducing fractures compared to anti-resorptives, particularly in high-risk populations, such as those with low BMD in combination with prevalent VFs, or after recent or multiple fractures with a very high risk. Therefore, it appears more rational to initiate anabolic treatment upfront for FLS patients at very high risk of subsequent fractures, followed by a treatment course with anti-resorptive medication [92].
Real world persistence and adherence to treatment for osteoporosis is low [93]. Early follow-up is recommended in the FLS [94]. Long-term follow-up will require improvement in the collaboration with the general practitioner [95] and fracture nurses, and may be facilitated by the implementation of digital monitoring [96].
The introduction of FLS care has significantly contributed to the improvement of care for high-risk patients with a recent fracture. To further enhance FLS care, there is a need to increase attendance rates, to consider the choice between anti-resorptive and anabolic drugs, and the utilization of large real-world databases for further insights into the impact of FLS care.
Outlook and Further Directions
The heterogeneous patterns of bone-, fall-, and comorbidity-related fracture phenotypes in patients 50 years or older with a recent clinical fracture underlines the necessity of implementing a comprehensive clinical evaluation and improving stratification of fracture risk in older adults. This allows identification of patients with a recent clinical fracture who are at high or very high imminent and long-term fracture risk. Fracture risk is determined based on the bone-related fracture phenotype (e.g., a low aBMD and the presence of VFs), fall-related fracture phenotype (e.g., based on recent fall history), or comorbidity-related fracture phenotype (e.g., using FRAX, without aBMD, or glucocorticoid users with rheumatoid arthritis). This will contribute to decisions about bone-, fall-, and comorbidity-directed treatments. Higher aBMD increases were found when combining low- or high-intensity exercise programs with bisphosphonates [97]. But, it remains to be demonstrated whether such combinations also reduce fracture risk.
The implementation of an FLS raises both opportunities and challenges. First, given that an FLS is a clinically and cost-effective intervention for the prevention of subsequent fractures, the deployment of FLS should be increased, and further work is needed to make the FLS cases more accessible for FLS practitioners.
Second, poor identification, attendance, and treatment adherence have been recognized as a huge problem in most FLS clinics that significantly blunt their expected effect to improve bone health and reduce fracture risk. It is therefore important to integrate data driven service improvement by using organizational and patient level indicators as a core component in their day to day running [94]. Simply setting up an FLS is insufficient to close the fracture care gap as evidenced by national registries for FLS in England, Wales, the Republic of Ireland and New Zealand (www.rcplondon.ac.uk/projects). FLSs need to keep their staff upskilled in service improvement methodology, such as working with patients as equal partners, analyzing patient level performance data, and including time for meaningful service improvement as part of what it means to be an FLS practitioner. Sustaining short- and long-term persistence and adherence to treatment will also require a well-considered and organized follow up in the collaboration of the FLS with the primary care physician, eventually with the help of non-physician health professionals [96, 98].
Third, emphasis on the need for early fall risk assessment and effective fall prevention strategies at the FLS is crucial to optimize the effects of FLS care, but this requires scaling community-based interventions to meet the volume of FLS patients that maintains the fall interventions effectiveness, patient acceptability, and short- and long-term adherence, with particular reference to cognitive impairment and the disability from a recent fracture. A recent cluster randomized study of 9803 persons aged 70 years and over to different community-based falls interventions has confirmed that a local falls prevention program without rigor is of little value and may increase harm [99].
Fourth, the effectiveness of secondary fracture prevention at the FLS should extend to early use of bone-forming agents, moving away from their use as rescue medications as the only way to reduce the imminent fracture risk for non-vertebral fractures in high-risk patients. Whether such treatments should only focus on patients with a high clinical or bone-related phenotype or be expanded to patients with a high fall-related phenotype remains to be demonstrated.
Finally, FLSs need to acknowledge the significant workforce capacity and capability challenges in healthcare settings globally and develop realistic local and national mitigation plans. These may include: (1) standardized national competency based training programs to improve the quality of FLS practitioners, as are being developed by the Fragility Fracture Network, (2) open access digital tools to optimize how patients flow through the FLS pathway, minimizing the time of healthcare workers spent on repetitive low value administrative tasks, improving patient safety, and diversifying patient engagement, and (3) working with AI, which has already identified thousands of patients with vertebral fractures from existing CT scans [68]. In the next phase, AI will link the orthopedic and radiology data with the patient’s existing health and wider socially available data to seamlessly deliver a step change in a massively scalable highly personalized approach to assessment, treatment decision making, and monitoring for patients after their fractures, often better reflecting the patients’ concerns and needs and as well as those of their families.
Conclusions
The increasing insights in the imminence of the risk of subsequent fractures, falls, physical performance, QoL, and mortality and the presence of comorbidities have contributed to the recognition that a recent clinical fracture in subjects of 50 years and older is a signal for imminent and long-term subsequent fracture risk. Evaluation of bone-, fall-, and comorbidity-related fracture phenotypes allows treatment decisions based on the presence of high and very high risk. Implementation of the FLS has been shown to increase evaluation and treatment and to decrease the risk of subsequent fractures and mortality.
Major questions need to be answered. How can the attendance rate be increased at the FLS? What is the effect of fall prevention on fracture risk in subgroups of high-risk fallers? What is the effect of optimizing treatment of comorbidities? What is the effect of combining fall prevention in subgroups of high fall risk with osteoanabolic drugs in high-risk patients based on comorbidity- or bone-related risks? The imminent subsequent fracture risk therefore opens a window of opportunity for timely evaluation and treatment, but also for further research.
Data Availability
No datasets were generated or analysed during the current study.
References
Collaborators GBDF. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the global burden of Disease Study 2019. Lancet Healthy Longev. 2021;2(9):e580–92.
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Archives Osteoporos. 2021;16(1):82.
Borgstrom F, Karlsson L, Ortsater G, Norton N, Halbout P, Cooper C, et al. Fragility fractures in Europe: burden, management and opportunities. Archives Osteoporos. 2020;15(1):59.
Fuggle NR, Beaudart C, Bruyere O, Abrahamsen B, Al-Daghri N, Burlet N, et al. Evidence-based Guideline for the management of osteoporosis in men. Nat Rev Rheumatol. 2024;20(4):241–51.
Schini M, Johansson H, Harvey NC, Lorentzon M, Kanis JA, McCloskey EV. An overview of the use of the fracture risk assessment tool (FRAX) in osteoporosis. J Endocrinol Invest. 2024;47(3):501–11.
Javaid MK, Pinedo-Villanueva R, Shah A, Mohsin Z, Hiligsmann M, Motek-Soulie A, et al. The capture the fracture(R) Partnership: an overview of a global initiative to increase the secondary fracture prevention care for patient benefit. Osteoporos Int. 2023;34(11):1827–35.
Leslie WD, Schousboe JT, Morin SN, Martineau P, Lix LM, Johansson H, et al. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int. 2020;31(6):1059–67.
Axelsson KF, Litsne H, Lorentzon M. The importance of recent prevalent fracture site for imminent risk of fracture - A Retrospective, Nationwide Cohort Study of Older Swedish men and women. J Bone Min Res. 2023.
Barron RL, Oster G, Grauer A, Crittenden DB, Weycker D. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos Int. 2020;31(11):2103–11.
Mokhtarzadeh H, Anderson DE, Allaire BT, Bouxsein ML. Patterns of load-to-strength ratios along the spine in a Population-based cohort to evaluate the contribution of spinal loading to vertebral fractures. J Bone Min Res. 2021;36(4):704–11.
Roux C, Briot K. Imminent fracture risk. Osteoporos Int. 2017;28(6):1765–9.
Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K, et al. Adjusting conventional FRAX estimates of fracture probability according to the recency of sentinel fractures. Osteoporos Int. 2020;31(10):1817–28.
Baim S, Blank R. Approaches to Fracture Risk Assessment and Prevention. Curr Osteoporos Rep. 2021;19(2):158–65.
Todorov G, Brook S, Quah Qin Xian N, Von Widekind S, Freudenthal B, Comninos AN. Comparison of fracture risk calculators in elderly fallers: a hospital-based cross-sectional study. BMJ Open. 2022;12(7):e060282.
Tran T, Bliuc D, Ho-Le T, Abrahamsen B, van den Bergh JP, Chen W, et al. Association of Multimorbidity and excess mortality after fractures among Danish adults. JAMA Netw Open. 2022;5(10):e2235856.
Geusens P, Lems WF, Bours S, Vd Bergh JP. Secondary fracture prevention: drug treatment, fall prevention and nutrition requirements. Best Pract Res Clin Rheumatol. 2019;33(2):290–300.
McLellan AR, Gallacher SJ, Fraser M, McQuillian C. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003;14(12):1028–34.
Kanis JA, Johansson H, McCloskey EV, Liu E, Akesson KE, Anderson FA, et al. Previous fracture and subsequent fracture risk: a meta-analysis to update FRAX. Osteoporos Int. 2023;34(12):2027–45.
van Geel TA, van Helden S, Geusens PP, Winkens B, Dinant GJ. Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis. 2009;68(1):99–102.
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019;30(1):79–92.
Toth E, Banefelt J, Akesson K, Spangeus A, Ortsater G, Libanati C. History of previous fracture and imminent fracture risk in Swedish Women aged 55 to 90 years presenting with a fragility fracture. J Bone Min Res. 2020;35(5):861–8.
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, et al. Imminent risk of fracture after fracture. Osteoporos Int. 2017;28(3):775–80.
Banefelt J, Akesson KE, Spangeus A, Ljunggren O, Karlsson L, Strom O, et al. Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int. 2019;30(3):601–9.
Dong Y, Peng R, Kang H, Song K, Guo Q, Zhao H, et al. Global incidence, prevalence, and disability of vertebral fractures: a systematic analysis of the global burden of disease study 2019. Spine J. 2022;22(5):857–68.
Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K, et al. The effect on subsequent fracture risk of age, sex, and prior fracture site by recency of prior fracture. Osteoporos Int. 2021;32(8):1547–55.
Praveen AD, Aspelund T, Ferguson SJ, Sigurethsson S, Guethnason V, Palsson H et al. Refracture and mortality risk in the elderly with osteoporotic fractures: the AGES-Reykjavik study. Osteoporos Int. 2024.
Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297(4):387–94.
Schene MR, Wyers CE, Driessen AMH, Souverein PC, Gemmeke M, van den Bergh JP et al. Imminent fall risk after fracture. Age Ageing. 2023;52(10).
Vranken L, Wyers CE, Van der Velde RY, Janzing HMJ, Kaarsemakers S, Driessen J, et al. Association between incident falls and subsequent fractures in patients attending the fracture liaison service after an index fracture: a 3-year prospective observational cohort study. BMJ Open. 2022;12(7):e058983.
Chang CB, Yang RS, Chang LY, Peng JK, Tsai KS, Huang WJ, et al. Fracture types affect clinical outcomes of patients managed within the fracture liaison and osteoporosis medication management services. Sci Rep. 2019;9(1):10089.
Vandenput L, Johansson H, McCloskey EV, Liu E, Schini M, Akesson KE, et al. A meta-analysis of previous falls and subsequent fracture risk in cohort studies. Osteoporos Int. 2024;35(3):469–94.
Schene MR, Meijer K, Cheung D, Willems HC, Driessen JHM, Vranken L, et al. Physical functioning in patients with a recent fracture: the can do, do do Framework Applied to explore physical capacity, physical activity and fall risk factors. Calcif Tissue Int. 2023;113(2):195–206.
Szulc P, Lewis J, Chapurlat R. Decline in muscle strength and physical function after fracture in men - the prospective STRAMBO study. J Bone Min Res. 2024.
Alajlouni D, Tran T, Bliuc D, Blank RD, Cawthon PM, Orwoll ES, et al. Muscle strength and physical performance improve fracture risk prediction beyond Garvan and FRAX: the osteoporotic fractures in men (MrOS) study. J Bone Min Res. 2022;37(3):411–9.
Alajlouni D, Bliuc D, Tran T, Eisman JA, Nguyen TV, Center JR. Decline in muscle strength and performance predicts fracture risk in Elderly women and men. J Clin Endocrinol Metab. 2020;105(9).
Li N, van Oostwaard M, van den Bergh JP, Hiligsmann M, Boonen A, van Kuijk SMJ, et al. Health-related quality of life of patients with a recent fracture attending a fracture liaison service: a 3-year follow-up study. Osteoporos Int. 2022;33(3):577–88.
Orwig DL, Kopperdahl D, Keaveny T, Magaziner J, Hochberg M. Change in vertebral strength and bone mineral density in men and women over the year post-hip fracture: a subgroup analysis. Archives Osteoporos. 2021;16(1):37.
Bliuc D, Nguyen ND, Alarkawi D, Nguyen TV, Eisman JA, Center JR. Accelerated bone loss and increased post-fracture mortality in elderly women and men. Osteoporos Int. 2015;26(4):1331–9.
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–21.
Vincent G, Adachi JD, Schemitsch E, Tarride JE, Ho N, Wani RJ, et al. Postfracture survival in a population-based study of adults aged >/=66 year: a call to action at hospital discharge. JBMR Plus. 2024;8(5):ziae002.
Tran T, Bliuc D, Hansen L, Abrahamsen B, van den Bergh J, Eisman JA et al. Persistence of excess mortality following individual non-hip fractures: a relative survival analysis. J Clin Endocrinol Metab. 2018.
Bliuc D, Nguyen ND, Nguyen TV, Eisman JA, Center JR. Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men. J Bone Min Res. 2013;28(11):2317–24.
Bliuc D, Tran T, Chen W, Alarkawi D, Alajlouni DA, Blyth F, et al. The association between multimorbidity and osteoporosis investigation and treatment in high-risk fracture patients in Australia: a prospective cohort study. PLoS Med. 2023;20(1):e1004142.
Alarkawi D, Tran TS, Chen W, March LM, Blyth FM, Blank RD, et al. Health perceptions, Multimorbidity, and New fractures and Mortality among patients with a fracture. JAMA Netw Open. 2024;7(4):e248491.
Lorentzon M, Cummings SR. Osteoporosis: the evolution of a diagnosis. J Intern Med. 2015;277(6):650–61.
Loundagin LL, Bredbenner TL, Jepsen KJ, Edwards WB. Bringing mechanical context to image-based measurements of Bone Integrity. Curr Osteoporos Rep. 2021;19(5):542–52.
Mikolajewicz N, Bishop N, Burghardt AJ, Folkestad L, Hall A, Kozloff KM, et al. HR-pQCT measures of bone microarchitecture predict fracture: systematic review and Meta-analysis. J Bone Min Res. 2020;35(3):446–59.
Samelson EJ, Broe KE, Xu H, Yang L, Boyd S, Biver E, et al. Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the bone microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol. 2019;7(1):34–43.
Johansson L, Sundh D, Zoulakis M, Rudang R, Darelid A, Brisby H, et al. The prevalence of vertebral fractures is Associated with reduced hip bone density and inferior peripheral appendicular volumetric bone density and structure in Older Women. J Bone Min Res. 2018;33(2):250–60.
Chapurlat R, Bui M, Sornay-Rendu E, Zebaze R, Delmas PD, Liew D, et al. Deterioration of cortical and trabecular microstructure identifies women with Osteopenia or normal bone Mineral density at Imminent and Long-Term risk for fragility fracture: a prospective study. J Bone Min Res. 2020;35(5):833–44.
Rufus-Membere P, Holloway-Kew KL, Diez-Perez A, Appelman-Dijkstra NM, Bouxsein ML, Eriksen EF, et al. Reference intervals for bone impact microindentation in healthy adults: a Multi-centre International Study. Calcif Tissue Int. 2023;112(3):338–49.
Whittier DE, Manske SL, Billington E, Walker RE, Schneider PS, Burt LA, et al. Hip fractures in older adults are Associated with the low density bone phenotype and heterogeneous deterioration of bone microarchitecture. J Bone Min Res. 2022;37(10):1963–72.
Whittier DE, Samelson EJ, Hannan MT, Burt LA, Hanley DA, Biver E, et al. Bone microarchitecture phenotypes identified in older adults are Associated with different levels of osteoporotic fracture risk. J Bone Min Res. 2022;37(3):428–39.
Whittier DE, Bevers M, Geusens P, van den Bergh JP, Gabel L. Characterizing bone phenotypes related to skeletal fragility using Advanced Medical Imaging. Curr Osteoporos Rep. 2023;21(6):685–97.
Zebaze R, Atkinson EJ, Peng Y, Bui M, Ghasem-Zadeh A, Khosla S, et al. Increased cortical porosity and reduced trabecular density are not necessarily synonymous with bone loss and Microstructural Deterioration. JBMR Plus. 2019;3(4):e10078.
Whittier DE, Samelson EJ, Hannan MT, Burt LA, Hanley DA, Biver E, et al. A fracture risk Assessment Tool for High Resolution Peripheral quantitative computed tomography. J Bone Min Res. 2023;38(9):1234–44.
Fajar JK, Taufan T, Syarif M, Azharuddin A. Hip geometry and femoral neck fractures: a meta-analysis. J Orthop Translat. 2018;13:1–6.
Shevroja E, Reginster JY, Lamy O, Al-Daghri N, Chandran M, Demoux-Baiada AL, et al. Update on the clinical use of trabecular bone score (TBS) in the management of osteoporosis: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal diseases (ESCEO), and the International Osteoporosis Foundation (IOF) under the auspices of WHO Collaborating Center for Epidemiology of Musculoskeletal Health and Aging. Osteoporos Int. 2023;34(9):1501–29.
Goel H, Binkley N, Hans D, Leslie WD. Fracture risk gradient assessed by categories of bone mineral density and trabecular bone score: the Manitoba BMD Registry. Archives Osteoporos. 2023;18(1):73.
Vranken L, Wyers CE, van Rietbergen B, Driessen JHM, Geusens P, Janzing HMJ, et al. The association between prevalent vertebral fractures and bone quality of the distal radius and distal tibia as measured with HR-pQCT in postmenopausal women with a recent non-vertebral fracture at the fracture Liaison Service. Osteoporos Int. 2019;30(9):1789–97.
Schroder G, Reichel M, Spiegel S, Schulze M, Gotz A, Bugaichuk S, et al. Breaking strength and bone microarchitecture in osteoporosis: a biomechanical approximation based on load tests in 104 human vertebrae from the cervical, thoracic, and lumbar spines of 13 body donors. J Orthop Surg Res. 2022;17(1):228.
Ye C, Leslie WD, Morin SN, Lix LM, McCloskey EV, Johansson H, et al. Adjusting FRAX estimates of fracture probability based on a positive vertebral fracture Assessment. JAMA Netw Open. 2023;6(8):e2329253.
Johansson L, Johansson H, Axelsson KF, Litsne H, Harvey NC, Liu E, et al. Improved fracture risk prediction by adding VFA-identified vertebral fracture data to BMD by DXA and clinical risk factors used in FRAX. Osteoporos Int. 2022;33(8):1725–38.
Lems WF, Paccou J, Zhang J, Fuggle NR, Chandran M, Harvey NC, et al. Vertebral fracture: epidemiology, impact and use of DXA vertebral fracture assessment in fracture liaison services. Osteoporos Int. 2021;32(3):399–411.
Leslie WD, Lix LM, Binkley N. Osteoporosis treatment considerations based upon fracture history, fracture risk assessment, vertebral fracture assessment, and bone density in Canada. Archives Osteoporos. 2020;15(1):93.
Schousboe JT, Lix LM, Morin SN, Derkatch S, Bryanton M, Alhrbi M, et al. Prevalent vertebral fracture on bone density lateral spine (VFA) images in routine clinical practice predict incident fractures. Bone. 2019;121:72–9.
Porcu G, Biffi A, Ronco R, Adami G, Alvaro R, Bogini R, et al. Refracture following vertebral fragility fracture when bone fragility is not recognized: summarizing findings from comparator arms of randomized clinical trials. J Endocrinol Invest. 2024;47(4):795–818.
Skjodt MK, Nicolaes J, Smith CD, Olsen KR, Cooper C, Libanati C, et al. Fracture risk in men and women with vertebral fractures identified opportunistically on routine computed tomography scans and not treated for osteoporosis: an Observational Cohort Study. JBMR Plus. 2023;7(5):e10736.
Pandya J, Ganda K, Ridley L, Seibel MJ. Identification of patients with osteoporotic vertebral fractures via simple text search of routine Radiology reports. Calcif Tissue Int. 2019;105(2):156–60.
van den Berg P, van Haard PMM, Geusens PP, van den Bergh JP, Schweitzer DH. Challenges and opportunities to improve fracture liaison service attendance: fracture registration and patient characteristics and motivations. Osteoporos Int. 2019;30(8):1597–606.
Malacon K, Beach I, Touponse G, Rangwalla T, Lee J, Zygourakis C. Trends in management of osteoporosis following primary vertebral Compression fracture. J Endocr Soc. 2023;7(7):bvad085.
van der Velde RY, Bours SPG, Wyers CE, Lems WF, Geusens P, van den Bergh JPW. Effect of implementation of guidelines on assessment and diagnosis of vertebral fractures in patients older than 50 years with a recent non-vertebral fracture. Osteoporos Int. 2017;28(10):3017–22.
Nicolaes J, Skjodt MK, Raeymaeckers S, Smith CD, Abrahamsen B, Fuerst T, et al. Towards Improved Identification of Vertebral fractures in Routine computed tomography (CT) scans: Development and External Validation of a machine learning algorithm. J Bone Min Res. 2023;38(12):1856–66.
Bours SP, van Geel TA, Geusens PP, Janssen MJ, Janzing HM, Hoffland GA, et al. Contributors to secondary osteoporosis and metabolic bone diseases in patients presenting with a clinical fracture. J Clin Endocrinol Metab. 2011;96(5):1360–7.
Merlijn T, Swart KMA, Niemeijer C, van der Horst HE, Netelenbos CJ, Elders PJM. The yield of routine laboratory examination in osteoporosis evaluation in primary care. Osteoporos Int. 2024.
Ebeling PR, Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F. Secondary osteoporosis. Endocr Rev. 2022;43(2):240–313.
Landgren O, Hofmann JN, McShane CM, Santo L, Hultcrantz M, Korde N, et al. Association of Immune marker changes with progression of Monoclonal Gammopathy of undetermined significance to multiple myeloma. JAMA Oncol. 2019;5(9):1293–301.
Kim SM, Korkmaz F, Sims S, Ryu V, Yuen T, Zaidi M. Musculoskeletal and neurocognitive clinical significance of adult hypophosphatasia. Osteoporos Sarcopenia. 2023;9(4):115–20.
Montero-Odasso M, van der Velde N, Martin FC, Petrovic M, Tan MP, Ryg J et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. 2022;51(9).
Colon-Emeric CS, McDermott CL, Lee DS, Berry SD. Risk Assessment and Prevention of Falls in Older Community-Dwelling adults: a review. JAMA. 2024.
Cornelissen D, Boonen A, Bours S, Evers S, Dirksen C, Hiligsmann M. Understanding patients’ preferences for osteoporosis treatment: the impact of patients’ characteristics on subgroups and latent classes. Osteoporos Int. 2020;31(1):85–96.
Beaudart C, Hiligsmann M, Li N, Lewiecki EM, Silverman S. Effective communication regarding risk of fracture for individuals at risk of fragility fracture: a scoping review. Osteoporos Int. 2022;33(1):13–26.
Beaudart C, Sharma M, Clark P, Fujiwara S, Adachi JD, Messina OD, et al. Patients’ preferences for fracture risk communication: the risk communication in osteoporosis (RICO) study. Osteoporos Int. 2024;35(3):451–68.
Bullock L, Crawford-Manning F, Cottrell E, Fleming J, Leyland S, Edwards J, et al. Developing a model Fracture Liaison Service consultation with patients, carers and clinicians: a Delphi survey to inform content of the iFraP complex consultation intervention. Archives Osteoporos. 2021;16(1):58.
Cianferotti L, Porcu G, Ronco R, Adami G, Alvaro R, Bogini R, et al. The integrated structure of care: evidence for the efficacy of models of clinical governance in the prevention of fragility fractures after recent sentinel fracture after the age of 50 years. Archives Osteoporos. 2023;18(1):109.
Martin J, Viprey M, Castagne B, Merle B, Giroudon C, Chapurlat R, et al. Interventions to improve osteoporosis care: a systematic review and meta-analysis. Osteoporos Int. 2020;31(3):429–46.
Vranken L, de Bruin IJA, Driessen AHM, Geusens PPM, Eisman JA, Center JR, et al. Decreased mortality and subsequent fracture risk in patients with a major and hip fracture after the introduction of a fracture Liaison Service: a 3-Year Follow-Up survey. J Bone Min Res. 2022;37(10):2025–32.
Li N, Hiligsmann M, Boonen A, van Oostwaard MM, de Bot R, Wyers CE, et al. The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int. 2021;32(8):1517–30.
Koller G, Goetz V, Vandermeer B, Homik J, McAlister FA, Kendler D, et al. Persistence and adherence to parenteral osteoporosis therapies: a systematic review. Osteoporos Int. 2020;31(11):2093–102.
van Maren MA, Wyers CE, Driessen JHM, Visser JV, de Vries F, van de Wijdeven K, et al. Two-year persistence with teriparatide improved significantly after introduction of an educational and motivational support program. Osteoporos Int. 2019;30(9):1837–44.
Li N, Beaudart C, Cauley JA, Ing SW, Lane NE, Reginster JY et al. Cost Effectiveness Analyses of Interventions for Osteoporosis in Men: A Systematic Literature Review. Pharmacoeconomics. 2023.
McClung MR, Rothman MS, Lewiecki EM, Hanley DA, Harris ST, Miller PD et al. The role of osteoanabolic agents in the management of patients with osteoporosis. Postgrad Med. 2022:1–11.
Fatoye F, Smith P, Gebrye T, Yeowell G. Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open. 2019;9(4):e027049.
Javaid MK, Sami A, Lems W, Mitchell P, Thomas T, Singer A, et al. A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int. 2020;31(7):1193–204.
Bennett MJ, Center JR, Perry L. Establishing consensus recommendations for long-term osteoporosis care for patients who have attended an Australian fracture liaison service: a Delphi study. Osteoporos Int. 2024;35(3):373–89.
Lems WF, van den Bergh JP, Geusens P. Follow-up in fracture liaisons services: the involvement of general practitioners and fracture nurses is urgently needed. Osteoporos Int. 2024.
Kistler-Fischbacher M, Yong JS, Weeks BK, Beck BR. A comparison of bone-targeted Exercise with and without antiresorptive bone medication to reduce indices of fracture risk in Postmenopausal Women with Low Bone Mass: the MEDEX-OP Randomized Controlled Trial. J Bone Min Res. 2021;36(9):1680–93.
Adams J, Wilson N, Hurkmans E, Bakkers M, Balazova P, Baxter M, et al. 2019 EULAR points to consider for non-physician health professionals to prevent and manage fragility fractures in adults 50 years or older. Ann Rheum Dis. 2021;80(1):57–64.
Lamb SE, Bruce J, Hossain A, Ji C, Longo R, Lall R, et al. Screening and intervention to Prevent Falls and fractures in Older people. N Engl J Med. 2020;383(19):1848–59.
Author information
Authors and Affiliations
Contributions
The manuscript is based on the lecture of P.G. at the occasion of the Steven Boonen Award at the European Calcified Tissue Society (ECTS) congress in Liverpool in 2023. Each author wrote one of the subsections of the paper, and the whole manuscript (finished by P.G.) was reviewed, adapted and finally approved by all authors.All authors have reviewed, contributed and approved the paper the revised version.
Corresponding author
Ethics declarations
Competing Interests
P.G. Grants from Sandoz, Celltrion, Fresenius, MSD, Amgen, Galapagos, Viatrix, Biocon. None in the context of this paperJ.V. Grants from UCB and AmgenC.R. Grants from Alexion. None in the context of this paperR.C. Amgen, UCB, Lilly, BMS, Pfizer, Alfasigma, Galapagos, Amolyt, Alexion, Biocon, Novartis, Fresenius-Kabi, Medac, Nordic, Viatris, AbbvieJ.C. Honoraria and advisory board for Amgen. None related to this paperD.B. noneC.W. noneN.L. noneD.W. noneW.L. speakers fee/advisory boards Amgen, UCB, Pfizer, Galapagos.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geusens, P., van den Bergh, J., Roux, C. et al. The Fracture Phenotypes in Women and Men of 50 Years and Older with a Recent Clinical Fracture. Curr Osteoporos Rep (2024). https://doi.org/10.1007/s11914-024-00885-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s11914-024-00885-z