Abstract
Purpose of Review
Radiation therapy (RT) is a mainstay of treatment for brain metastases from solid tumors. Treatment of these patients is complex and should focus on minimizing symptoms, preserving functional status, and prolonging survival.
Recent Findings
Whole-brain radiotherapy (WBRT) can lead to toxicity, and while it does reduce recurrence in the CNS, this has not been shown to provide a survival benefit. Recent advances focus on reducing the toxicity of WBRT or using more targeted radiation therapy. New paradigms including the use of proton RT for leptomeningeal metastases (LM) and stereotactic radiosurgery (SRS) before craniotomy hold promise in improving treatment efficacy and reducing toxicity.
Summary
Omission or replacement of WBRT is often safe and the use of SRS is expanding to include patients with more lesions and preoperative RT. Proton RT holds promise for LM. Progress is being made in improving patient-centered outcomes and reducing toxicity for patients with brain metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic brain disease is a relatively common complication of solid tumors, occurring in up to 25% of cancer patients [1], and causing clinical symptoms in 60–75% of cases [2]. As diagnostic neuroimaging has improved, and as advances in systemic therapies have led to more individuals living with cancer, the incidence of brain metastases has risen [1]. The manifestations of lesions in the brain can be debilitating, including headache, seizures, nausea, vomiting, focal neurologic deficits, and in advanced cases can lead to progressive neurological dysfunction, coma, and death [3]. The most common primary cancers that lead to brain metastases include carcinomas of the lung, breast, lower gastrointestinal system, and kidneys, as well as melanoma [4].
Treatment of brain metastases poses a unique challenge. While the mainstay of therapy for metastatic disease is systemic anticancer agents, brain metastases may be shielded from the systemic circulation by the blood–brain barrier, and these therapies are often ineffective [1]. The treatment of metastatic brain disease therefore relies heavily on local therapy, including surgery and radiation therapy (RT). Metastatic lesions in the central nervous system can cause symptoms and threaten patients’ life or functional status with only moderate progression, and therefore are more likely to require treatment than metastases elsewhere. While some systemic agents have activity in the CNS, these are generally not the mainstay of treatment, and surgery or RT to CNS lesions both pose toxicity without benefits for cancer that may be progressing elsewhere in the body. The competing risks posed by metastatic burden outside the CNS are often life-limiting, and treatment decisions for brain metastases should also account for a patient’s life expectancy based on non-CNS lesions. When oncologists counsel patients with brain metastases, they should therefore focus on palliation of symptoms and prolonging life and functionality as long as possible, while minimizing toxicity and accounting for the individual patient’s competing risks. Current research on RT for metastatic brain disease furthers this goal by working to minimize toxicity and identify practices that improve patient-centered outcomes such as survival and symptomatic disease.
Herein, we review these recent advances in radiation therapy practice for patients with brain metastases. Specifically, we will focus on the evolving indications for stereotactic radiosurgery (SRS) and whole-brain radiotherapy (WBRT), the novel use of proton RT for patients with leptomeningeal metastases (LM), and the role of preoperative SRS for patients with solitary brain metastases.
Stereotactic Radiosurgery for Multiple Brain Metastases
Stereotactic radiosurgery was pioneered in the 1950s with the goal of delivering high doses of focused radiation to targets in the brain and was initially used primarily for the ablation of arteriovenous malformations [5, 6]. When surgical resection of metastases prior to WBRT was shown to improve survival for patients with solitary brain metastases [7, 8], interest in the use of non-invasive local therapy for intracranial metastases grew. SRS was introduced for these patients as it allowed for the safe targeting of lesions deep in the brain or adjacent to vital structures and was able to provide higher doses of radiation than traditional WBRT. Early randomized studies of the addition of SRS to WBRT for metastatic disease showed superior local control and improvement in functional status for patients with a limited number of lesions, and extended survival for patients with solitary brain metastases [9, 10].
Most trials assessing the benefits of SRS for brain metastases have limited enrollment to patients with no more than 3 or 4 lesions [9,10,11,12,13]. However, a 2018 study surveyed 72 US radiation oncologists who use SRS for brain metastases and found that most physicians had increased the number and volume of lesions they were willing to treat with SRS, with 60% of respondents stating they would use SRS in patients with more than 4 brain metastases [14]. The benefits of expanding the indications for SRS are clear, as WBRT is more likely than SRS to cause neurocognitive toxicity [13], and with rare exceptions, can only be used once per patient, limiting options for salvage therapy.
The evidence supporting the use of focused radiation therapy for patients with more than 4 brain metastases is limited. A recent phase III trial comparing WBRT to SRS for patients with 4–15 non-melanoma brain metastases found superior neurocognitive outcomes in the SRS group, and no difference in LC or OS between arms despite a higher rate of distant brain failure in the SRS group [15]. These treatments have also been studied indirectly. Yamamoto et al. conducted an observational study in 1194 patients with 1–10 brain metastases treated with SRS. While they showed that patients with a single metastatic lesion had prolonged survival as compared to the rest of the cohort, the survival of patients with 2–4 lesions was not different from those with 5–10 lesions [16]. The rate of local control was also not different between the 2–4 lesion and 5–10 lesion groups, and although there was a trend toward a higher likelihood of developing new brain metastases after SRS among patients with 5–10 lesions (69% vs 63%), this did not reach statistical significance. Nichol et al. conducted a prospective single-arm study with patients receiving SRS for 1–10 brain metastases. This study also showed no difference in overall survival (OS) after SRS between individuals with 1–3 metastases and those with 4–10, though in patients with 4–10 metastases 49% went on to develop new brain lesions after treatment, compared to only 19% in those with 1–3 metastses [17]. In a retrospective analysis of 323 patients receiving SRS for brain metastases, Chang et al. report no difference in overall survival among patients with 1–5, 6–10, 11–15, and > 15 metastases, though the group with > 15 lesions did have a higher probability of developing new brain metastases after treatment compared to those with 1–15 lesions [18].
In light of this data, SRS is considered the favored treatment for patients with limited brain metastases, though the definition of this term is challenging. The NCCN defines limited brain metastases as the state in which SRS is as effective as WBRT and offers neurocognitive benefits [19], intentionally leaving ambiguity to accommodate new data on the specific indications for SRS. Guidelines from professional societies do not agree on which patients benefit from SRS either, making recommendations about when this technique should be considered based on differing criteria including number of lesions [20], volume of metastases [21], and patient prognosis [22].
We favor an approach to selecting therapy for patients with multiple brain metastases that takes into account several factors. In individuals with more than 4 metastases, the advantages of SRS over WBRT likely include improved local control for the lesions targeted [9, 10], less neurocognitive toxicity [13], and a shorter treatment schedule. This must be balanced against the advantages of WBRT, which seem to include improved regional control for patients with numerous or high volumes of metastases, and lower cost [15, 23]. However, the regional control benefit of WBRT has not yet been shown to translate to an improvement in survival in large trials [15, 17, 18, 24]. Therefore, SRS is generally favored for patients with longer expected survival, as these patients derive more benefit from durable local control of treated lesions and improved neurocognitive outcomes. SRS may also be appropriate for patients with a poor prognosis, especially considering the reduced burden of time and travel with single-fraction or several-fraction SRS treatment, and given the desire to limit intensive therapy for more frail patients. WBRT should be considered for symptomatic patients with extensive intracranial disease when palliative therapy is indicated but targeting all lesions with SRS is not feasible either technically or given time constraints. While best supportive care with dexamethasone may also be a valid option for these patients, a subset of those with a better prognosis may receive a survival benefit from WBRT [25, 26]. Furthermore, strategies to mitigate the toxicity of WBRT are being developed, as discussed below. While its use should be carefully considered in light of the less toxic alternatives of supportive care or SRS, WBRT has a role in preventing symptoms associated with CNS progression and can be beneficial for individuals with high-volume symptomatic intracranial metastases.
Studies addressing the question of which patients with multiple brain metastases will benefit from SRS are ongoing. HipSter (NCT04277403) [27] is an ongoing phase III clinical trial comparing hippocampal-avoidant WBRT with simultaneous integrated boost to intracranial metastatic lesions against SRS for patients with 4–15 brain metastases with the primary outcome of intracranial progression-free survival (PFS).
Research is also ongoing to investigate the role of SRS plus targeted therapy or immunotherapy for patients with brain metastases. While concerns about the safety of such combinations have been raised by retrospective studies [28, 29], phase I studies have shown an acceptable safety profile of ipilimumab plus SRS [30], and sorafenib plus SRS [31], and an ongoing phase I study will assess the safety of CDK4/6 inhibitors plus SRS in brain metastases from breast cancer (NCT04585724) [32]. Randomized trials are currently underway assessing the effectiveness of SRS in addition to systemic agents, including ipilimumab and nivolumab (NCT03340129) [33], and osimertinib (NCT03769103) [34]. While preliminary data for these regimens is promising, they should not be used routinely until randomized evidence is available.
The results of these studies will help clinicians decide between treating subclinical disease with regimens that target the whole brain and treating part of the brain with SRS, potentially improving local control and neurocognitive outcomes. There remains no one-size-fits-all approach for radiation treatment for multiple brain metastases, and radiation oncologists must balance the benefits and toxicity of therapy for each individual patient.
Adjuvant Whole-Brain Radiotherapy After Stereotactic Radiosurgery for Brain Metastases
As previously discussed, early trials of stereotactic radiosurgery for brain metastases studied SRS as an adjuvant to WBRT, the standard of care at the time [9, 10]. However, WBRT carries a significant risk of neurocognitive toxicity [35], and the omission of WBRT for patients undergoing SRS for metastatic disease has been an area of active research. Multiple clinical trials have shown that omission of WBRT leads to improved neurocognitive outcomes compared to SRS + WBRT and that while the addition of WBRT does improve CNS disease control, this does not translate to a survival benefit [11,12,13, 24, 36, 37]. Due to the need to reduce potentially toxic and time-consuming care for patients with a limited prognosis, the use of adjuvant WBRT is no longer routine for patients with limited brain metastases. This has been reflected by recent clinical practice guidelines, which do not recommend the use of WBRT in addition to SRS for limited brain metastases [19, 21].
Patients with brain metastases from small cell lung cancer (SCLC) represent a unique case. Historically, these patients have been treated with prophylactic cranial irradiation (PCI), which has led to their omission from clinical trials studying treatment for brain metastases. Recently, however, as systemic therapy and SRS improve, some have questioned whether PCI is necessary. Two new immunotherapy options for these patients have recently been approved [38, 39], further prolonging survival, including for patients with brain metastases at baseline. Data is also accumulating for the effectiveness of SRS alone for SCLC brain metastases, with a recent cohort study showing a shorter time to CNS progression but no difference in overall survival as compared to historical controls receiving WBRT alone [40].
Further randomized studies addressing the role of SRS alone in SCLC are ongoing. ENCEPHALON (NCT03297788) is an ongoing phase II trial comparing neurocognitive outcomes in patients receiving WBRT versus SRS for up to 10 SCLC brain metastases [41]. NCT03391362 is an ongoing single-arm phase II study investigating the cause-specific mortality for patients with 1–10 SCLC brain metastases [42]. Because randomized trials establishing the benefit of PCI for limited SCLC were conducted before SRS was widely used [43, 44], and given the changing landscape of systemic therapy for these patients, future trials revisiting the effectiveness of PCI in the era of modern immunotherapy and RT may be warranted.
Recent research has also focused on strategies to prevent neurocognitive toxicity in patients who must undergo WBRT. The vascular hypothesis of radiation-induced injury to the CNS posits that vascular injury caused by radiation leads to atherosclerosis and mineralizing microangiopathy, resulting in vascular insufficiency [45]. The mechanism of injury is therefore similar to what is observed in vascular dementia, which has created interest in the use of agents studied for vascular dementia to prevent radiation-induced CNS injury. Memantine is a non-competitive, low-affinity antagonist of the N-methyl-d-aspartate (NMDA) receptor which has been shown in phase III clinical trials to be effective in the treatment of vascular dementia [46, 47]. Based on this data, RTOG 0614 randomized 508 patients undergoing WBRT for brain metastases to placebo or 24 weeks of memantine with an escalating dosing schedule that resulted in 10 mg twice daily starting in the fourth week [48]. The study’s retention was low, with 149 evaluable patients at 24 weeks, resulting in no statistically significant difference in delayed recall between the arms at 24 weeks (p = 0.06). However, memantine did lead to a significantly longer time to cognitive decline and improved executive function and processing speed [48]. We therefore feel that memantine is warranted for neuroprotection in patients undergoing WBRT.
Another strategy for reducing the neurocognitive toxicity of WBRT is hippocampal avoidance, which uses intensity-modulated radiation therapy to reduce the dose delivered to the hippocampal neural stem cells. This is based on the observation that patients who receive lower doses of radiation to the hippocampus may have improved scores on cognitive function testing [49]. NRG CC001 is a phase III trial which randomized 518 patients with brain metastases not within 5 mm of the hippocampus to WBRT plus memantine or hippocampal-avoidant WBRT (HA-WBRT) plus memantine [50]. This study found that patients undergoing HA-WBRT had a significantly lower risk of cognitive failure (hazard ratio 0.74, p = 0.02) than those undergoing WBRT, a difference which was driven by preserved executive function at 4 months after RT, and better learning and memory at 6 months after RT. We therefore favor the use of hippocampal-avoidant techniques for patients who require WBRT for brain metastases.
The goal of RT for brain metastases is to palliate symptoms and prolong life when possible without compromising the quality of life for a cohort of patients with extensive competing risk and poor prognosis. One component of meeting this goal is to avoid the toxicity of WBRT when more conformal techniques are likely to provide benefits. Nonetheless, WBRT remains a valid option for patients with the extensive intracranial disease, and novel techniques to minimize its toxicity are vital to maximizing quality of life for patients with brain metastases.
Neoadjuvant Stereotactic Radiosurgery Prior to Surgery for Single Brain Metastases
In 1990, Patchell et al. showed that surgical resection led to improved functional status and survival as compared to WBRT alone for patients with solitary brain metastases [7]. However, the rate of postoperative local recurrence for these patients was high, with a subsequent trial placing this risk at almost 50% after surgery alone, compared with 10% with the addition of adjuvant WBRT [51]. Despite the dramatic improvement in intracranial disease control, adjuvant WBRT causes significant neurocognitive toxicity and has not been shown to impact overall survival [51]. Clinicians have been using postoperative SRS to the surgical bed in order to spare patients the toxicity of WBRT for many years, though this strategy had not been supported by evidence from a randomized trial until recently. In 2017, Brown et al. randomized patients undergoing resection for a single brain metastasis to postoperative WBRT or SRS to the surgical cavity, showing no difference in overall survival and improved neurocognitive outcomes with SRS [52]. Mahajan et al. also investigated this question, randomizing patients who had undergone complete resection of 1–3 brain metastases to SRS to the resection cavity versus observation [53]. This study demonstrated local control of 43% at 1 year with observation, compared to 72% with SRS, thus cementing postoperative SRS as the standard of care for patients with completely resected limited brain metastases.
While postoperative SRS provides a survival benefit with minimal neurocognitive toxicity, it does have limitations. Resection beds of tumors are often irregular and difficult to contour, and intraoperative dissemination of tumor cells may lead to microscopic areas of disease outside the resection cavity. It has been suggested that including a margin of normal tissue around the target may improve local control for postoperative patients. A retrospective analysis of 72 patients showed that when delivering postoperative SRS to the tumor bed, highly conformal plans correlate with markedly better local control than less conformal plans, an observation which led the investigators to recommend the inclusion of a 2-mm margin around the tumor bed for postoperative SRS [54]. This involves a tradeoff though, as the use of a 2-mm margin for SRS has been associated with a higher rate of severe parenchymal complications [55].
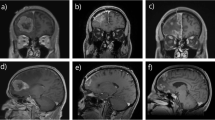
Due to these limitations of postoperative RT, investigators have begun to study the use of neoadjuvant SRS prior to surgical resection. This strategy provides the theoretical benefits of a well-circumscribed target not requiring an additional margin to cover uncertainty in the target volume or areas of intraoperative dissemination. Asher et al. reported the results of 47 patients treated for 51 lesions with preoperative SRS. With a median follow-up time of 12 months, this cohort demonstrated good local control, which was estimated at 98%, 86%, and 72% at 6, 12, and 24 months, with no episodes of radionecrosis reported [56]. Similarly, Prabhu et al. reported on a cohort of 117 patients with 125 lesions treated with preoperative SRS. At 6 months after RT, local control was 75%, regional control of 40%, and the rate of symptomatic radionecrosis was 5% [57]. Based on these results, prospective studies are now underway. A phase II trial in Canada aims to assess the rate of symptomatic radiation toxicity in patients treated with neoadjuvant SRS for up to 10 brain metastases, followed by surgical resection of at least one lesion [58]. NCT03741673 is an ongoing phase III clinical trial comparing preoperative with postoperative SRS with the primary outcome of leptomeningeal disease-free rate [59].
Neoadjuvant SRS for brain metastases is promising, as early results suggest high rates of local control and limited toxicity. Furthermore, completing RT prior to surgery may reduce cost, as RT simulation scans were acceptable as preoperative imaging, and the ability to treat with SRS and surgery in quick succession may help minimize time off systemic therapy. At this time, however, insufficient data exists to justify the treatment of patients with neoadjuvant SRS outside of a clinical trial.
Proton Craniospinal Irradiation for Leptomeningeal Metastasis
Leptomeningeal metastasis (LM) is characterized by the spread of cancer cells within the subarachnoid space in the cerebrospinal fluid (CSF) and is a late complication of several cancers. The prognosis for patients with LM is poor, with a median survival without treatment on the order of 2–4 months [60,61,62]. Treatment for LM historically consists of supportive care, focused RT for bulky deposits of disease or WBRT for symptomatic but not radiologically apparent disease, and intrathecal chemotherapy for select individuals with high-performance status. While some modern targeted therapies can cross the blood–brain barrier, the low CNS activity of many drugs continues to limit the effectiveness of systemic therapy against LM.
Craniospinal irradiation (CSI) is an RT technique which consists of delivering photon irradiation to the entire leptomeningeal compartment and is commonly used in the treatment of pediatric CNS tumors which have spread to the spinal cord [19]. CSI for LM was initially studied in the 1990s using photon-based techniques and has consistently led to significant improvement in neurologic function and survival, but has also caused toxicity from radiation dose passing through the spine to reach the esophagus, bowel, and bone marrow [63, 64]. Because of the poor prognosis of LM patients and the relatively severe associated toxicity, photon CSI for LM is rarely used in clinical practice [65].
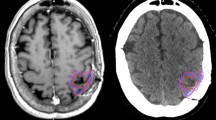
In contrast to traditional photon beam radiotherapy, protons deposit the majority of their energy at the end of their range creating a narrow dose/depth curve or Bragg peak. The narrow Bragg peak allows radiation oncologists to prescribe dose precisely at the desired depth of tissue [66] (Fig. 1). Proton beam radiotherapy is therefore promising for patients with LM, as CSI using protons can confine dose to the CSF while sparing the anterior structures, and may provide the survival and neurologic benefits of radiation of the full neuroaxis without the associated toxicity seen with photon CSI [67].
This technique has only recently been assessed in clinical studies. Our group published the results of a phase I prospective trial evaluating the toxicity and efficacy of hypofractionated proton CSI in patients with LM [68]. The regimen was well tolerated, with 2 of 20 evaluable patients experiencing dose-limiting toxicities, all of which resolved without medical intervention [68]. Despite the small sample size, proton CSI did provide durable CNS disease control in some patients, with 4 of 21 individuals being free of CNS progression 12 months after therapy [68]. A subsequent phase II trial, NCT04343573, is currently underway comparing proton CSI against involved-field photon RT including WBRT and/or focal spine RT in patients with LM from breast cancer or non-small cell lung cancer [69].
Further complicating efforts to study treatment strategies for LM is the lack of a standardized method to assess response to therapy. The Leptomeningeal Assessment in Neuro-Oncology (LANO) is a scorecard based on MRI findings that has been proposed [70] and revised [71], but is yet to be prospectively validated. Furthermore, the revised scorecard relies solely on imaging findings, not accounting for CSF cytology or clinical symptoms. Traditionally, diagnosis and response assessment for LM has included CSF cytology, though the diagnostic sensitivity is low and multiple lumbar punctures are often required to make a diagnosis [72]. Recent efforts to improve the detection of LM have included the isolation of circulating tumor cells (CTCs) in the CSF, which has been shown to be a robust tool for diagnosis and response assessment for patients with LM [73,74,75]. Tumor-derived cell-free DNA (cfDNA) isolated from CSF has also been shown to contain relevant information about the disease of patients with cancer in the CSF [76]. Therefore NCT04343573, our group’s phase II study of proton CSI, also includes a sampling of CSF CTCs and cfDNA to prospectively assess their value in determining treatment response.
Despite these advances, proper selection of patients for aggressive treatment of LM remains challenging. Patients with LM often have a high burden of systemic disease, and while LM itself can be a fatal complication of solid tumors, it is important to avoid aggressive and time-intensive treatment for patients near the end-of-life whose functional status is limited by competing risks. Nonetheless, proton CSI holds promise as a novel therapy for LM which may provide disease control benefits without severe toxicities.
Conclusion
Recent advances and ongoing research in the use of RT for brain metastases are largely focused on the reduction of toxicity. WBRT and photon craniospinal irradiation are being replaced by newer, more targeted techniques, including SRS, hippocampal avoidance, and proton RT. In addition to reducing side effects for patients requiring therapy, these innovations allow for more aggressive treatment of metastatic disease without compromising the quality of life. Furthermore, recent efforts have focused on improving patient-centered outcomes and avoidance of intensive therapy that does not further an individual patient’s goals. These advances help improve the available treatment options for metastatic brain disease, allowing individuals living with metastatic cancer to live longer, minimize symptoms, and preserve the ability to function.
References
Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neurooncol. 2005;75:5–14.
Soffietti R, Cornu P, Delattre JY, et al. EFNS Guidelines on diagnosis and treatment of brain metastases: report of an EFNS Task Force. Eur J Neurol. 2006;13:674–81.
Chang EL, Lo S. Diagnosis and management of central nervous system metastases from breast cancer. Oncologist. 2003;8:398–410.
Barnholtz-Sloan JS, Sloan AE, Davis FG, et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004;22:2865–72.
Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951;102:316–9.
Leksell L. Stereotactic radiosurgery. J Neurol Neurosurg Psychiatry. 1983;46:797–803.
Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322:494–500.
Vecht CJ, Haaxma-Reiche H, Noordijk EM, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol. 1993;33:583–90.
Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004;363:1665–72.
Kondziolka D, Patel A, Lunsford LD, et al. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999;45:427–34.
Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol. 2011;29:134–41.
Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 2006;295:2483–91.
Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10:1037–44.
Blomain ES, Kim H, Garg S, et al. Stereotactic radiosurgery practice patterns for brain metastases in the United States: a national survey. J Radiat Oncol. 2018;7:241–6.
Li J, Ludmir EB, Wang Y, et al. Stereotactic radiosurgery versus whole-brain radiation therapy for patients with 4–15 brain metastases: a phase III randomized controlled trial. Int J Radiat Oncol Biol Phys. 2020;108:S21–2.
Yamamoto M, Serizawa T, Shuto T, et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 2014;15:387–95.
Nichol A, Ma R, Hsu F, et al. Volumetric radiosurgery for 1 to 10 brain metastases: a multicenter, single-arm, phase 2 study. Int J Radiat Oncol Biol Phys. 2016;94:312–21.
Chang WS, Kim HY, Chang JW, et al. Analysis of radiosurgical results in patients with brain metastases according to the number of brain lesions: is stereotactic radiosurgery effective for multiple brain metastases? J Neurosurg. 2010;113(Suppl):73–8.
Central nervous system cancers (Version 1.2021). In: Comprehensive cancer network clinical practice guidelines in oncology. National Comprehensive Cancer Network; 2021. https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf. Accessed 10 Aug 2021.
Milano MT, Chiang VLS, Soltys SG, et al. Executive summary from American Radium Society’s appropriate use criteria on neurocognition after stereotactic radiosurgery for multiple brain metastases. Neuro Oncol. 2020;22:1728–41.
Gaspar LE, Prabhu RS, Hdeib A, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the role of whole brain radiation therapy in adults with newly diagnosed metastatic brain tumors. Neurosurgery. 2019;84:E159–62.
Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): an American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol. 2012;2:210–25.
Lester-Coll NH, Dosoretz AP, Magnuson WJ, et al. Cost-effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for up to 10 brain metastases. J Neurosurg. 2016;125:18–25.
Tsao MN, Xu W, Wong RKS, Lloyd N, Laperriere N, Sahgal A, Rakovitch E, Chow E. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018;1(1):CD003869. https://doi.org/10.1002/14651858.CD003869.pub4.
Mulvenna P, Nankivell M, Barton R, et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet. 2016;388:2004–14.
Cagney DN, Alexander BM, Aizer AA. Whole brain radiotherapy for non-small cell lung cancer. Lancet. 2017;389:1394–5.
Ganswindt U. HA-WBRT vs SRS in patients with multiple brain metastases (HipSter). In: ClinicalTrials.gov. Natl Inst Health; 2020. https://clinicaltrials.gov/ct2/show/NCT04277403. Accessed 10 Aug 2021.
Kim JM, Miller JA, Kotecha R, et al. The risk of radiation necrosis following stereotactic radiosurgery with concurrent systemic therapies. J Neurooncol. 2017;133:357–68.
Martin AM, Cagney DN, Catalano PJ, et al. Immunotherapy and symptomatic radiation necrosis in patients with brain metastases treated with stereotactic radiation. JAMA Oncol. 2018;4:1123–4.
Williams NL, Wuthrick EJ, Kim H, et al. Phase 1 Study of ipilimumab combined with whole brain radiation therapy or radiosurgery for melanoma patients with brain metastases. Int J Radiat Oncol Biol Phys. 2017;99:22–30.
Arneson K, Mondschein J, Stavas M, et al. A phase I trial of concurrent sorafenib and stereotactic radiosurgery for patients with brain metastases. J Neurooncol. 2017;133:435–42.
Zhong J. Stereotactic radiosurgery with abemaciclib, ribociclib, palbociclib in treating patients with hormone receptor positive breast cancer with brain metastases. In: ClinicalTrials.gov. Natl Inst Health; 2020. https://clinicaltrials.gov/ct2/show/NCT04585724. Accessed 11 Aug 2021.
Long G. Anti-PD 1 brain collaboration + radiotherapy extension (ABC-X Study) (ABC-X). In: ClinicalTrials.gov. Natl Inst Health; 2017. https://clinicaltrials.gov/ct2/show/NCT03340129. Accessed 10 Aug 2021.
Lefresne SH, C. Study of osimertinib + SRS vs osimertinib alone for brain metastases in EGFR positive patients with NSCLC. In: ClinicalTrials.gov. Natl Inst Health; 2018. https://clinicaltrials.gov/ct2/show/NCT03769103. Accessed 10 Aug 2021.
Laack NN, Brown PD. Cognitive sequelae of brain radiation in adults. Semin Oncol. 2004;31:702–13.
Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA. 2016;316:401–9.
Hong AM, Fogarty GB, Dolven-Jacobsen K, et al. Adjuvant whole-brain radiation therapy compared with observation after local treatment of melanoma brain metastases: a multicenter, randomized phase III trial. J Clin Oncol. 2019;37:3132–41.
Paz-Ares L, Dvorkin M, Chen Y, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–39.
Horn L, Mansfield AS, Szczesna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–9.
Rusthoven CG, Yamamoto M, Bernhardt D, et al. Evaluation of first-line radiosurgery vs whole-brain radiotherapy for small cell lung cancer brain metastases: the FIRE-SCLC cohort study. JAMA Oncol. 2020;6:1028–37.
Rieken S. Whole brain radiation therapy alone vs. radiosurgery for SCLC patients with 1-10 brain metastases (ENCEPHALON). In: ClinicalTrials.gov. Natl Inst Health; 2017. https://clinicaltrials.gov/ct2/show/NCT03297788. Accessed 10 Aug 2021.
Aizer AA. Stereotactic radiation in patients with small cell lung cancer and 1-10 brain metastases. In: ClinicalTrials.gov. Natl Inst Health; 2018. https://clinicaltrials.gov/ct2/show/NCT03391362. Accessed 10 Aug 2021.
Auperin A, Arriagada R, Pignon JP, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med. 1999;341:476–84.
Meert AP, Paesmans M, Berghmans T, et al. Prophylactic cranial irradiation in small cell lung cancer: a systematic review of the literature with meta-analysis. BMC Cancer. 2001;1:5.
Monje ML, Palmer T. Radiation injury and neurogenesis. Curr Opin Neurol. 2003;16:129–34.
Orgogozo JM, Rigaud AS, Stoffler A, et al. Efficacy and safety of memantine in patients with mild to moderate vascular dementia: a randomized, placebo-controlled trial (MMM 300). Stroke. 2002;33:1834–9.
Wilcock G, Mobius HJ, Stoffler A, et al. A double-blind, placebo-controlled multicentre study of memantine in mild to moderate vascular dementia (MMM500). Int Clin Psychopharmacol. 2002;17:297–305.
Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15:1429–37.
Gondi V, Hermann BP, Mehta MP, et al. Hippocampal dosimetry predicts neurocognitive function impairment after fractionated stereotactic radiotherapy for benign or low-grade adult brain tumors. Int J Radiat Oncol Biol Phys. 2013;85:348–54.
Brown PD, Gondi V, Pugh S, et al. Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: phase III trial NRG Oncology CC001. J Clin Oncol. 2020;38:1019–29.
Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280:1485–9.
Brown PD, Ballman KV, Cerhan JH, et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18:1049–60.
Mahajan A, Ahmed S, McAleer MF, et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18:1040–8.
Soltys SG, Adler JR, Lipani JD, et al. Stereotactic radiosurgery of the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys. 2008;70:187–93.
Nataf F, Schlienger M, Liu Z, et al. Radiosurgery with or without A 2-mm margin for 93 single brain metastases. Int J Radiat Oncol Biol Phys. 2008;70:766–72.
Asher AL, Burri SH, Wiggins WF, et al. A new treatment paradigm: neoadjuvant radiosurgery before surgical resection of brain metastases with analysis of local tumor recurrence. Int J Radiat Oncol Biol Phys. 2014;88:899–906.
Prabhu RS, Miller KR, Asher AL, et al. Preoperative stereotactic radiosurgery before planned resection of brain metastases: updated analysis of efficacy and toxicity of a novel treatment paradigm. J Neurosurg. 2018;132(5):1387–94.
Takami H, Nassiri F, Moraes FY, et al. A phase II study of neoadjuvant stereotactic radiosurgery for large brain metastases: clinical trial protocol. Neurosurgery. 2020;87:403–7.
Yeboa DN. Pre-operative SRS or post-operative SRS in treating cancer patients with brain metastases. ClinicalTrials.gov, Natl Inst Health. 2018.
Morris PG, Reiner AS, Szenberg OR, et al. Leptomeningeal metastasis from non-small cell lung cancer: survival and the impact of whole brain radiotherapy. J Thorac Oncol. 2012;7:382–5.
Le Rhun E, Taillibert S, Zairi F, et al. A retrospective case series of 103 consecutive patients with leptomeningeal metastasis and breast cancer. J Neurooncol. 2013;113:83–92.
Brower JV, Saha S, Rosenberg SA, et al. Management of leptomeningeal metastases: prognostic factors and associated outcomes. J Clin Neurosci. 2016;27:130–7.
Hermann B, Hultenschmidt B, Sautter-Bihl ML. Radiotherapy of the neuroaxis for palliative treatment of leptomeningeal carcinomatosis. Strahlenther Onkol. 2001;177:195–9.
Harada H, Mitsuya K, Asakura H, et al. Cranio-spinal irradiation for leptomeningeal carcinomatosis: a pilot study. Int J Radiat Oncol Biol Phys. 2014;90:S310.
El Shafie RA, Bohm K, Weber D, et al. Outcome and prognostic factors following palliative craniospinal irradiation for leptomeningeal carcinomatosis. Cancer Manag Res. 2019;11:789–801.
Pankuch M, Mohammed N, Hecksel D, Laub S, Boyer S, Hartsell WF. In: Small W, Tarbell NJ, Yao M, editors. Clinical radiation oncology: indications, techniques, and results. 3rd ed. Wiley-Blackwell; 2017. pp. 115–40.
Barney CL, Brown AP, Grosshans DR, et al. Technique, outcomes, and acute toxicities in adults treated with proton beam craniospinal irradiation. Neuro Oncol. 2014;16:303–9.
Yang TJ, Wijetunga NA, Yamada J, et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol. 2021;23:134–43.
Yang JT. Proton craniospinal radiation therapy vs. partial photon radiation therapy for leptomeningeal metastasis from solid tumors. In: ClinicalTrials.gov. Natl Inst Health; 2020. https://clinicaltrials.gov/ct2/show/NCT04343573. Accessed 10 Aug 2021.
Chamberlain M, Junck L, Brandsma D, et al. Leptomeningeal metastases: a RANO proposal for response criteria. Neuro Oncol. 2017;19:484–92.
Le Rhun E, Devos P, Boulanger T, et al. The RANO Leptomeningeal Metastasis Group proposal to assess response to treatment: lack of feasibility and clinical utility and a revised proposal. Neuro Oncol. 2019;21:648–58.
Glantz MJ, Cole BF, Glantz LK, et al. Cerebrospinal fluid cytology in patients with cancer: minimizing false-negative results. Cancer. 1998;82:733–9.
Lin X, Fleisher M, Rosenblum M, et al. Cerebrospinal fluid circulating tumor cells: a novel tool to diagnose leptomeningeal metastases from epithelial tumors. Neuro Oncol. 2017;19:1248–54.
Malani R, Fleisher M, Lin X, et al. Cerebrospinal fluid circulating tumor cells (CSF CTC) for real-time patient monitoring and response to treatment. J Clin Oncol. 2017;35:11549–11549.
Wijetunga NA, Boire AA, Yamada Y, et al. Cerebrospinal fluid circulating tumor cells as a predictive biomarker for proton craniospinal irradiation for leptomeningeal metastases. J Clin Oncol. 2021;39:2011–2011.
Pentsova EI, Shah RH, Tang J, et al. Evaluating cancer of the central nervous system through next-generation sequencing of cerebrospinal fluid. J Clin Oncol. 2016;34:2404–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Noah J. Mathis has received funding for a research fellowship from eContour. Neil Ari Wijetunga declares that he has no conflict of interest. Brandon S. Imber declares that he has no conflict of interest. Luke R.G. Pike has received compensation for service as a consultant from Blackstone Investments/Clarus Ventures, Third Rock Ventures, Galera Therapeutics, Dynamo Therapeutics, Myst Therapeutics, Monte Rosa Therapeutics, and Best Doctors/Teladoc Inc., and owns stock/equity in Schrödinger, Novavax, and Clovis Oncology. Jonathan T. Yang declares that he has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Mathis, N.J., Wijetunga, N.A., Imber, B.S. et al. Recent Advances and Applications of Radiation Therapy for Brain Metastases. Curr Oncol Rep 24, 335–342 (2022). https://doi.org/10.1007/s11912-022-01209-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01209-z