Abstract
Purpose of Review
Neuroendocrine prostate cancer (NEPC) is an aggressive histologic subtype of prostate cancer that most commonly arises in later stages of prostate cancer as a mechanism of treatment resistance. The poor prognosis of NEPC is attributed in part to late diagnosis and a lack of effective therapeutic agents. Here, we review the clinical and molecular features of NEPC based on recent studies and outline future strategies and directions.
Recent Findings
NEPC can arise “de novo” but most commonly develops as a result of lineage plasticity whereby prostate cancer cells adopt alternative lineage programs as a means to bypass therapy. Dependence on androgen receptor (AR) signaling is lost as tumors progress from a prostate adenocarcinoma to a NEPC histology, typically manifested by the downregulation of AR, PSA, and PSMA expression in tumors. Genomic analyses from patient biopsies combined with preclinical modeling have pointed to loss of tumor suppressors RB1 and TP53 as key facilitators of lineage plasticity. Activation of oncogenic drivers combined with significant epigenetic changes (e.g., EZH2 overexpression, DNA methylation) further drives tumor proliferation and expression of downstream neuronal and neuroendocrine lineage pathways controlled in part by pioneer and lineage determinant transcription factors (e.g., SOX2, ASCL1, BRN2). These biologic insights have provided a framework for the study of this subgroup of advanced prostate cancers and have started to provide rationale for the development of biomarker-driven therapeutic strategies.
Summary
Further study of the dynamic process that leads to NEPC is required for the development of effective strategies to identify and treat patients developing lineage plasticity as a mechanism of treatment resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most common malignancy and second leading cause of cancer-related death amongst men in the USA [1]. Despite significant advances in treatment, the prognosis of advanced prostate cancer remains variable with most men still succumbing to the disease [2]. Prostate cancer is an androgen-driven disease, and androgen deprivation therapy (ADT) combined with other potent drugs that target androgen receptor (AR) signaling such as abiraterone acetate or enzalutamide is a standard first-line approach for metastatic prostate cancer. Despite significant and often durable response, resistance to AR-directed strategies ultimately ensues [3]. Most castration-resistant prostate cancers (CRPC) are still dependent on AR signaling through acquired AR gene mutation, amplification, or other means to re-activate the AR [4,5,6]. This has led to alternative strategies to further target AR signaling [7, 8]. Approximately 15–20% of CRPC tumors will lose dependence on AR signaling at some point during their disease course but the identification of AR-independent disease in the clinic remains challenging. One apparent clinical manifestation is histologic transformation from an AR-expressing prostate adenocarcinoma to an AR-negative, poorly differentiated small cell neuroendocrine carcinoma histology [9]. This cancer phenotype is often referred to as neuroendocrine prostate cancer (NEPC) to broadly encompass both pure small cell carcinomas and mixed adenocarcinoma-neuroendocrine tumor morphologies. AR expression is typically low but even when AR is expressed, NEPC tumors tend to be less dependent, or “indifferent,” to canonical AR signaling. The diagnosis of NEPC is currently based on metastatic tumor biopsy confirming tumor morphology. Although there are no standard criteria for when to perform a biopsy to look for NEPC, one may consider this in patients with particularly aggressive disease, atypical spread, and/or progression with low or non-rising PSA levels. The NCCN guidelines currently recommend consideration of metastatic biopsy in suspected cases of NEPC transformation, as prostate cancer patients that develop small cell carcinoma could be considered for platinum-based chemotherapy regimens (similar to small cell lung cancer (SCLC).
Clinical Features of NEPC
The incidence of AR-independent prostate cancer seems to be increasing, which may be related in part to the introduction of more potent and effective drugs that target the AR. In a rapid autopsy study, 13.3% of patients harbored metastatic lesions that were AR-negative with neuroendocrine (NE) features and an additional 23.3% harbored AR-negative lesions without NE features. This is at higher frequency than observed in autopsies performed prior to the approval of potent AR signaling inhibitors (i.e., enzalutamide and abiraterone acetate) (6.3% NE, 5.4% AR-negative) [10]. In another study by the West Coast Dream Team (WCDT) evaluating metastatic biopsies from a cohort of 202 patients after progression on potent AR signaling inhibitors, 17% of patients showed histologic evidence of small cell neuroendocrine prostate cancer, and this was significantly correlated with increased risk of death (P = 0.027) [11••]. Notably, although AR was expressed in small cell NE metastatic tumors from this WCDT cohort, AR signaling was significantly lower compared with non-NE tumors.
In a systematic review, 123 NEPC patients were analyzed to evaluate for risk factors associated with time to NEPC development and survival [12]. The median time from initial diagnosis of prostate cancer to NEPC development was 20 months, and high Gleason score (≥ 8) at diagnosis was an independent risk factor for early NEPC development (HR, 1.66; P = 0.032). The median survival after NEPC diagnosis was 7 months and involvement of more than three metastatic organs was associated with shorter survival (HR, 3.31; P = 0.001).
In another retrospective analysis of 87 patients with histologically confirmed de novo or treatment-related NEPC, the median overall survival from time of prostate cancer diagnosis in de novo NEPC was 16.8 months which was shorter than those with treatment-related NEPC (53.5 months) [13]. Median time from diagnosis of prostate adenocarcinoma to treatment-related NEPC was 39.7 months. At the time of NEPC, median PSA level was less than 4 ng/ml while serum chromogranin A and LDH levels elevated in 48.3% and 62.5%, respectively. NEPC patients harbored frequent visceral metastases compared to patients with castration-resistant adenocarcinoma (62% vs. 24%, P < 0.001). Tumors with mixed adenocarcinoma-NEPC harbored better prognosis than those with pure small cell NEPC (26.1 vs. 8.9 months in median survival from the time of NEPC diagnosis, P < 0.0001).
Despite accumulating data around the clinical and pathologic features of this subset of advanced prostate cancers, the diagnosis of NEPC remains challenging. There are a number of reasons for this. Tumor biopsies are invasive to perform, and there are no guidelines for when and where to biopsy in a patient with suspected NEPC. Single-site biopsies also do not always represent the tumor burden of the patient. There is wide variability in pathology, and the diagnosis of “NEPC” is often loosely defined. According to pathology guidelines [14•], NEPC may fall into several categories based on tumor morphology [14•]. This includes (i) usual prostate adenocarcinoma with NE differentiation; (ii) adenocarcinoma with Paneth call NE differentiation; (iii) carcinoid tumor; (iv) small cell carcinoma; (v) large cell NE carcinoma; and (vi) mixed (small or large cell) NE carcinoma-acinar adenocarcinoma. These classifications are summarized in Table 1. NEPC tumors are usually associated with expression of classical NE markers (e.g., synaptophysin (SYP), chromogranin, CD56) by immunohistochemistry (IHC) but none of these are required for the diagnosis. Paneth cell and carcinoid tumors are well-differentiated and associated with a more favorable prognosis, whereas poorly differentiated NE tumors including small cell carcinomas are more aggressive [14•]. Clinical challenges arise in particular when mixed, hybrid, or amphicrine histologies are observed, with positive AR and PSA expression and/or variable NE marker expression. How to manage such patients is not defined.
Given these diagnostic challenges, clinical features associated with cancer aggressiveness have been proposed and studied as clinical trial criteria to select patients for small cell/NE-directed therapies such as platinum chemotherapy [15,16,17,18] or alisertib [19•] (Table 2), without the requirement for histologic confirmation of NEPC. The aggressive variant prostate cancer (AVPC) criteria developed by Aparicio and colleagues has been used as inclusion criteria for several platinum chemotherapy studies [15, 20, 21]. Notably, in the AVPC trials, approximately 25% of patients met histologic criteria, and the presence of bulky tumor and/or high serum LDH levels significantly predicted poor prognosis although serum NE markers did not [15].
With respect to imaging modalities, prostate-specific membrane antigen (PSMA), a type II transmembrane protein, is an emerging target for molecular imaging and therapy in prostate adenocarcinoma. However, NEPC tumors often lose PSMA expression [22] along with AR and, therefore, may manifest on imaging with PSMA-low or -negative lesions [23]. Conversely, FDG-PET-CT, standardly used in SCLC, may be useful in identifying NEPC tumors as they tend to be metabolically active [22, 24]. The presence of PSMA-low or PSMA/FDG-discordant lesions on imaging were seen in up to one third of patients (91 of 291 men) screened for the TheraP trial as eligibility for Lu-PSMA radionuclide therapy [25, 26], and these features have been associated with poor prognosis [27], though the precise relationship between PSMA/FDG imaging features and pathology has not been well-established. The role and application of other imaging and treatment modalities such as somatostatin receptor–targeting peptides (e.g., 68Ga-DOTATATE, 177Lu-DOTATATE) used in well-differentiated NE tumors are also being investigated in NEPC [28, 29]. Cases have been reported in which tumor lesions in prostate cancer patients with NE features were successfully detected using somatostatin receptor activity [30, 31].
Genomic Features of NEPC
Genomic studies have supported NEPC tumors evolving from a prostate adenocarcinoma precursor, with shared genomic alterations between adenocarcinoma and metastatic NEPC tumors and between different histologies within mixed tumors, particularly when considering early prostate cancer genomic events such as the TMPRSS2-ERG gene fusion [32, 33]. Preclinical studies using lineage tracing have also supported a “trans-differentiation model” with NEPC arising from a luminal precursor [34].
Alterations such as TP53 and RB1 loss, enriched in NEPC tumors, are often acquired during the course of therapy resistance. Of note, loss of RB1 and TP53 is also frequent in other small cell carcinomas and universally lost in SCLC [35,36,37]. In a prostate cancer study by Tan et al., Rb protein loss was consistently observed in small cell prostate carcinomas with 90% of tumors being negative or low by IHC analysis, with 85% of these occurring through copy number allelic loss [35]. In addition, accumulation of p53 was detected in 56% of small cell prostate cancer carcinomas, with 60% of cases harboring a TP53 mutation [35]. In another study of whole-exome sequencing (WES) of metastatic biopsies of NEPC and castration-resistant adenocarcinoma (CRPC-Adeno), RB1 loss was seen in 70% of NEPC and 32% of CRPC-adeno and mutation or deletion of TP53 in 66.7% of NEPC and 31.4% of CRPC-adeno [38]. Multiple preclinical studies now have supported combined TP53 and RB1 deficiency as key facilitators of the NE-like phenotype [39,40,41,42,43,44,45].
Understanding when and how these genomic events occur has important biomarker implications. Recent data suggests that although combined loss of RB1 and TP53 can facilitate lineage plasticity, they are not sufficient by themselves to cause NEPC transformation [46]. RB1 loss in particular is associated with poor prognosis in CRPC-Adeno [9], and future studies are warranted to address whether single or combined loss of these tumor suppressors predicates NEPC transformation and identifies patients at higher risk for developing lineage plasticity. By studying whole-exome sequencing including serial time points and circulating tumor DNA (ctDNA) profiles, a working model has been established in which NEPC tumors become less heterogeneous as they evolve from adenocarcinoma potentially due to clonal selection (of RB/TP53 clones or others) [47••].
Although it is considerably less common, de novo small cell prostate carcinoma can also occur. Chedgy et al. investigated the pre-treatment molecular profiles of 18 patients with de novo small cell prostate cancer [48]. Ten cases (55%) harbored pure small cell carcinoma histology in biopsy cores and others had mixed with adenocarcinoma. Similar genomic alterations were observed in de novo cases as seen in treatment-related NEPC including frequent biallelic deletion and/or mutation of TP53, RB1, and PTEN. Notably, biallelic loss of DNA repair genes (BRCA1, BRCA2, ATM, and MSH2/6) were seen in 5/18 patients (29%) which is of potential therapeutic relevance. Interestingly, several pure de novo small cell prostate cancers also harbored ETS gene fusions suggesting possibly a luminal cell of origin.
Epigenetic Features
Epigenetic alterations also play a key role in lineage plasticity leading to acquisition of stem-like cell properties and changes in developmental programs and differentiation [49]. These epigenetic features, including changes in DNA methylation, histone modifications, and chromatin integrity and accessibility, are responsible for transcriptional regulation, and seem to be dynamic [50]. Comparing genome-wide DNA methylation patterns in metastatic tumor biopsies of patients with NEPC and castration-resistant adenocarcinoma, it was found that DNA methylation patterns can robustly distinguish NEPC [38]. Integration of DNA methylation with transcriptome data point to epigenetic modulation of pathways involved in differentiation, development, and cell-cell adhesion [38]. Of note, these NEPC-associated DNA methylation changes are detectable in the circulation using cell-free DNA (cfDNA) which may have important biomarker implications; in a recent study of whole-genome bisulfite sequencing of cfDNA, DNA methylation patterns in cfDNA reflected matched metastatic tumor biopsies including hypermethylation of ASXL3 and SPDEF and hypomethylation of INSM1 and CDH2 in NEPC [47••].
Disorder of epigenetic processes impairs the differentiation status, along with other reprogramming factors such as the enhancer of zeste homolog 2 (EZH2) in NEPC [9, 39, 51,52,53,54]. EZH2 is a histone methyltransferase and the catalytic component of the Polycomb repressive complex 2 (PRC2). EZH2 tri-methylates the histone H3 lysine-27 (H3K27me3), and this activity is required for PRC2-mediated gene silencing [55]. EZH2 is highly expressed in many types of cancers including NEPC [32, 38]. In preclinical models of NEPC, EZH2 inhibition restored AR expression and sensitivity to AR-targeted therapy [39], suggesting that this may be a targetable modulator of lineage plasticity [52, 56, 57].
Biology of NEPC
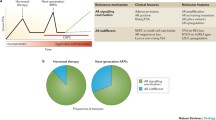
Facilitated by both genomic and epigenomic changes, NEPC is characterized by the expression of genes involved in neuronal and neuroendocrine differentiation, epithelial-mesenchymal transition, stem-like/developmental pathways, and cell-cycle markers [38]. During the transition from adenocarcinoma to NEPC, luminal markers of prostate lineage are typically downregulated and AR activity is suppressed [49]. Critical dysregulation of key oncogenic drivers as well as pioneer and lineage determinant transcription factors (such as SOX2, ASCL1, BRN2, MYCN, and ONECUT2) drives plasticity and maintains the NE state (Fig. 1).
Prostate cancer progression from CSPC (castrate-sensitive prostate cancer) to CRPC-Adeno to treatment-related NEPC (t-NEPC). Lineage plasticity towards t-NEPC is characterized by loss of tumor suppressors, activation of oncogenic drivers, and epigenetic changes. This results in a proliferative, poorly differentiated tumor with NE morphology, low AR signaling, and expression of neuronal and neuroendocrine lineage markers
N-myc is a transcription factor upregulated in NEPC and also implicated as a key oncogenic driver in other neuroendocrine tumors [58, 59]. In preclinical studies, N-myc functions as a suppressor of AR signaling and driver of lineage plasticity [51, 60, 61•]. Overexpression of N-myc is frequently observed in NEPC and a subset of CRPC-Adeno while N-myc is not normally expressed in normal prostate cells [19•, 32, 59]. Tumor overexpression of N-myc has been associated with shorter OS in patients with CRPC-Adeno and NEPC [61•]. N-myc interacts directly with AR, EZH2, and other PRC2 components to drive epigenetic changes [51]. Aurora kinase A (AURKA), a protein involved in mitosis and spindle assembly [62], also stabilizes N-Myc and prevents N-Myc degradation [32], and the AURKA inhibitor alisertib has been investigated as means to inhibit the N-Myc-AURKA complex and NEPC tumor growth [19•, 63].
The master neural transcription factor BRN2 is another lineage transcription factor and driver of NEPC [54]. BRN2 is directly suppressed by AR and regulates expression of the stem cell transcription factor SRY-box2 (SOX2). SOX2 is also downstream of RB1 and TP53 and may be involved in reverting cells to a stem-like/pluripotent state prior to differentiation towards a neuroendocrine lineage [39, 64]. The repressive role of SOX2 has also been attributed to hypomethylation of histone H3 caused by the activation of lysine-specific demethylase 1 [53]. Recent investigations revealed that elevated SOX2 expression can also transactivate SPINK1 which has a role in sustaining the NE phenotype [65].
There are several other emerging biologic factors implicated in NEPC pathogenesis including overexpression of the placental gene PEG10 which facilitates cell-cycle progression and lineage plasticity [66], upregulation of the RNA-splicing factor SRRM4 [67,68,69], and downregulation of the master repressor of neuronal differentiation REST [70]. REST can bind to target regions within genes crucial for a neuronal phenotype and prevent their transcription [71]. Expression of REST is regulated in part by SRRM4 [67, 72, 73]. Recently, MUC-1 was demonstrated as highly expressed in NEPC [74]. MUC-1 could facilitate lineage plasticity via activation of the MYC-BRN2 pathway, MYCN, and EZH2; inhibition of MUC-1 suppressed BRN2 and self-renewal in vivo.
Metabolic vulnerabilities have also been reported in NEPC [75]. Reina-Campos et al. identified protein kinase C (PKC) λ/ι to be downregulated in de novo and treatment-related NEPC compared with prostate adenocarcinoma. They revealed that PKCλ/ι functions as a tumor suppressor and its deficiency results in upregulation of serine biosynthesis via the mTORC1/ATF4 pathway. Metabolic modifications lead to elevated intracellular S-adenosyl methionine (SAM) levels which impacts the DNA methylation, facilitating the development of NEPC [75]. Tumor hypoxia in NEPC has been found to be regulated in part by the transcription factor ONECUT2 [76]. ONECUT2 activates SMAD3 which impacts hypoxia signaling and also drives a NE phenotype. Rotinen et al. found that ONECUT2 is a master regulator that acts to repress the AR network via regulation of FOXA1 and activates neural differentiation-related genes in prostate cancer [77]. Inhibition of ONECUT2 suppresses tumor progression and metastasis in vivo, suggesting that ONECUT2 could be a therapeutic target for NEPC [76, 77].
Although there has been significant progress in the field’s overall understanding of the biology of NEPC, a better understanding of how and when these factors emerge in the context of AR therapy resistance and potentially cooperate to drive NEPC is still required.
Treatment of NEPC
Platinum-based chemotherapy is commonly administered to patients with pure small cell carcinoma based on SCLC data and the accumulating data for AVPC. This may consist of a combination of carboplatin (or sometimes cisplatin) plus either etoposide (based on SCLC) or a taxane (especially if mixed histology or AVPC features). A combination regimen of cisplatin, etoposide and doxorubicin has been studied in 36 patients with small cell prostate cancer [18]. Twenty patients (61%) showed partial response. Median time to progression and overall survival were 5.8 months (95% CI, 4.1–6.9 months) and 10.5 months (95% CI, 7.5–14.3 months), respectively. With respect to toxicity, severe neutropenia was observed and three patients died due to toxicity. Given these therapeutic and toxicity data, this regimen is not recommended for patients with NEPC [18]. Flechon et al. evaluated treatment response of carboplatin and etoposide every 3 weeks in 60 patients with CRPC who were considered to have NE differentiation based on elevated serum CgA and NSE levels and/or visceral metastases [16]. In this study, the objective response rate of this regimen was low in patients with measurable disease (8.9%) and PSA response rate was 8%. The median progression-free survival (PFS) and OS were 2.9 months and 9.6 months, respectively. Culine et al. investigated combination therapy with docetaxel and cisplatin in 41 patients with mCRPC [17]; in this study, serum NE marker (NSE and/or CgA) response rate (≥ 50%) was 33% and objective response rate was 41%.
In patients with AVPC clinical criteria, carboplatin plus docetaxel was evaluated followed by next-line cisplatin plus etoposide in a phase 2 clinical trial [15]. PFS rate after 4 cycles of carboplatin plus docetaxel and etoposide plus cisplatin were 65.4% and 33.8%, respectively. Notably, serum neuroendocrine markers were not associated with outcome or response [15]. In a follow-up randomized study of cabazitaxel with or without carboplatin in mCRPC including AVPC, the median PFS was 7.3 months with combination therapy compared with 4.5 months with cabazitaxel alone (P = 0.018) [78••]. Molecular characterization of tumors from patients with AVPC [20] has revealed frequently combined tumor suppressor loss (RB1, TP53, and/or PTEN) which are also frequent gene alterations in histologic confirmed NEPC [32]. Post hoc analysis of the cabazitaxel with or without carboplatin study found that patients with ≥ 2 alterations in TP53, RB1, and/or PTEN experienced longer median PFS (7.5 vs. 1.7 months) and median OS (20.2 vs. 8.5 months) when treated with the combination vs. cabazitaxel alone [78••]. Thus, clinically defined AVPC shares genomic features with NEPC, and furthermore, biomarker-driven strategies targeting these characteristics are planned.
Beyond platinum, therapy for NEPC is not well-established [15]. Based on clinical and pathologic features, second-line SCLC regimens or alternative CRPC therapies could be considered. There may be rationale for using immune checkpoint inhibitor therapy based on SCLC data either upfront such as atezolizumab with platinum chemotherapy [79] or in the second line such as nivolumab plus ipilimumab [80], but studies focused on NEPC have not yet been reported. A phase 2 study of nivolumab plus ipilimumab for advanced rare GU tumors including small cell/NEPC is ongoing (NCT03333616).
Other drugs have been evaluated for NEPC based on preclinical studies. In light of the interaction between MYCN and AURKA, the AURKA inhibitor alisertib was evaluated in a phase II trial [19•]. There is also a rationale for exploring AURKA inhibition in the context of RB1 loss based on synthetic lethality [81]. The inclusion criteria for the alisertib study were broad (Table 2). Sixty patients were treated with alisertib 50 mg twice daily for 7 days every 21 days. Six-month radiographic PFS was 13.4%, and median survival was 9.5 months in this study. Notably, four patients showed outstanding response to alisertib with disappearance of liver metastases and durable stable disease, suggesting that patient selection (potentially by MYCN or RB1 biomarker status) may be important [52].
Delta-like protein 3 (DLL3) is a protein expressed on the cell surface of various neuroendocrine tumors including SCLC and NEPC [82, 83]. In a recent study, DLL3 expression was observed in the majority of NEPC tumors (76.6%) and also a subset of CRPC-Adeno (12.5%), with minimal or absent expression in localized prostate cancer and benign tissues [83]. Several drugs targeting DLL3 are in clinical development with planned investigation in NEPC.
Based on integrative analyses of transcriptomic and cell-surface proteomic data, Lee et al. identified carcinoembryonic antigen-related cell adhesion molecule 5 (CEACAM5) as another cell-surface antigen overexpressed in NEPC [84]. Targeting CEACAM5 with chimeric antigen receptor T cells provided antigen-specific cytotoxic activity, and therefore, targeting CEACAM5 could represent a novel therapeutic approach for NEPC.
The epigenetic regulator, EZH2, is of potential therapeutic relevance in NEPC as described above, and EZH2 expression is higher in NEPC tissues compared to CRPC, localized prostate cancer, and benign prostate tissues [38]. In preclinical studies, EZH2 inhibitors have shown activity in NEPC [38, 51]. One study reported that EZH2 inhibitor GSK503 could restore enzalutamide sensitivity in RB1 and PTEN double-knockout mouse model of NEPC [39]. Thus, EZH2 is a candidate therapeutic target for NEPC. Trials of EZH2 inhibitors in mCRPC are ongoing (NCT03480646, NCT03460977, NCT0419864) and correlative analyses within these studies may provide additional insights.
Other drugs directed at epigenetic modulators have been investigated in mCRPC and may also be relevant for targeting plasticity and NEPC. Lysine-specific demethylase 1 (LSD1) catalyzes the histone H3 lysine 4 demethylase and is involved in stemness and differentiation; LSD1 activates a lethal prostate cancer network through interaction with the LSD-1 binding protein ZNF217 [85]. LSD1 is also an emerging target for SCLC [86] and may have relevance in NEPC. Aggarwal et al. reported a phase 1b/2a study with the bromodomain extra-terminal (BET) inhibitor ZEN-3694 in combination with enzalutamide in patients with mCRPC previously treated with abiraterone and/or enzalutamide [87]. The median PSA level was 26.99 ng/ml (range 0.15–1701.8), and 28% of patients harbored visceral metastasis at study entry. Median radiographic PFS was 9.0 months. Seventeen percent and 5% of patients continued the treatment for more than 12 and 24 months without progression, respectively. Notably, lower canonical AR activity in baseline biopsy was correlated with longer rPFS (median rPFS, 10.4 months vs. 4.3 months). Furthermore, patients who met clinical criteria for AVPC had prolonged time to progression compared with those without AVPC (11.6 months vs. 5.5 months, P = 0.24).
Conclusions
NEPC is an increasingly recognized histologic subtype of prostate cancer that most commonly arises in later stages of the disease as a mechanism of treatment resistance. The current diagnosis depends on tissue biopsy, and effective therapy targeting the molecular features of NEPC has not yet been developed. Advances in our understanding of the genomic, epigenomic, and biologic features are pointing to new opportunities to help improve diagnosis and guide therapy. In order to undergo treatment at the optimal timing, it will be important to identify biomarkers that can detect the emergence of lineage plasticity during the course of sequential therapies. A further understanding of biological characteristics of NEPC is required to conquer this lethal form of prostate cancer.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
Litwin MS, Tan HJ. The diagnosis and treatment of prostate cancer: a review. Jama. 2017;317(24):2532–42. https://doi.org/10.1001/jama.2017.7248.
Pishgar F, Ebrahimi H, Saeedi Moghaddam S, Fitzmaurice C, Amini E. Global, regional and national burden of prostate cancer, 1990 to 2015: results from the global burden of disease study 2015. J Urol. 2018;199(5):1224–32. https://doi.org/10.1016/j.juro.2017.10.044.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371(5):424–33. https://doi.org/10.1056/NEJMoa1405095.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995–2005. https://doi.org/10.1056/NEJMoa1014618.
Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med. 2018;378(15):1408–18. https://doi.org/10.1056/NEJMoa1715546.
Proof-of-Concept with PROTACs in Prostate Cancer. Cancer Discov. 2020. https://doi.org/10.1158/2159-8290.Cd-nb2020-054.
Liu J, He D, Cheng L, Huang C, Zhang Y, Rao X, et al. p300/CBP inhibition enhances the efficacy of programmed death-ligand 1 blockade treatment in prostate cancer. Oncogene. 2020;39(19):3939–51. https://doi.org/10.1038/s41388-020-1270-z.
Abida W, Cyrta J, Heller G, Prandi D, Armenia J, Coleman I, et al. Genomic correlates of clinical outcome in advanced prostate cancer. Proc Natl Acad Sci U S A. 2019;116(23):11428–36. https://doi.org/10.1073/pnas.1902651116.
Bluemn EG, Coleman IM, Lucas JM, Coleman RT, Hernandez-Lopez S, Tharakan R et al. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. Cancer Cell. 2017;32(4):474–89.e6. doi:https://doi.org/10.1016/j.ccell.2017.09.003.
•• Aggarwal R, Huang J, Alumkal JJ, Zhang L, Feng FY, Thomas GV, et al. Clinical and genomic characterization of treatment-emergent small-cell neuroendocrine prostate cancer: a multi-institutional prospective study. J Clin Oncol. 2018;36(24):2492–503. https://doi.org/10.1200/jco.2017.77.6880This multi-institutional, prospective study by the West Coast SU2C-PCF Dream Team identified the frequency of therapy-related small cell prostate cancer histology in biopsies of patients progressing on abiraterone and/or enzalumide, as well as their clinical and molecular characteristics. Therapy-related small cell prostate cancers harbored AR amplification and protein expression, a distinct transcriptome signature, and were associated with short OS.
Wang HT, Yao YH, Li BG, Tang Y, Chang JW, Zhang J. Neuroendocrine Prostate CANCER (NEPC) progressing from conventional prostatic adenocarcinoma: factors associated with time to development of NEPC and survival from NEPC diagnosis-a systematic review and pooled analysis. J Clin Oncol. 2014;32(30):3383–90. https://doi.org/10.1200/jco.2013.54.3553.
Conteduca V, Oromendia C, Eng KW, Bareja R, Sigouros M, Molina A, et al. Clinical features of neuroendocrine prostate cancer. Eur J Cancer. 2019;121:7–18. https://doi.org/10.1016/j.ejca.2019.08.011.
• Epstein JI, Amin MB, Beltran H, Lotan TL, Mosquera JM, Reuter VE, et al. Proposed morphologic classification of prostate cancer with neuroendocrine differentiation. Am J Surg Pathol. 2014;38(6):756–67. https://doi.org/10.1097/pas.0000000000000208This pathology study used tumor morphology to subclassify prostate cancers with neuroendocrine differentiation.
Aparicio AM, Harzstark AL, Corn PG, Wen S, Araujo JC, Tu SM, et al. Platinum-based chemotherapy for variant castrate-resistant prostate cancer. Clin Cancer Res. 2013;19(13):3621–30. https://doi.org/10.1158/1078-0432.Ccr-12-3791.
Flechon A, Pouessel D, Ferlay C, Perol D, Beuzeboc P, Gravis G, et al. Phase II study of carboplatin and etoposide in patients with anaplastic progressive metastatic castration-resistant prostate cancer (mCRPC) with or without neuroendocrine differentiation: results of the French Genito-Urinary Tumor Group (GETUG) P01 trial. Ann Oncol. 2011;22(11):2476–81. https://doi.org/10.1093/annonc/mdr004.
Culine S, El Demery M, Lamy PJ, Iborra F, Avances C, Pinguet F. Docetaxel and cisplatin in patients with metastatic androgen independent prostate cancer and circulating neuroendocrine markers. J Urol. 2007;178(3 Pt 1):844–8; discussion 8. https://doi.org/10.1016/j.juro.2007.05.044.
Papandreou CN, Daliani DD, Thall PF, Tu SM, Wang X, Reyes A, et al. Results of a phase II study with doxorubicin, etoposide, and cisplatin in patients with fully characterized small-cell carcinoma of the prostate. J Clin Oncol. 2002;20(14):3072–80. https://doi.org/10.1200/jco.2002.12.065.
• Beltran H, Oromendia C, Danila DC, Montgomery B, Hoimes C, Szmulewitz RZ, et al. A phase II trial of the aurora kinase a inhibitor alisertib for patients with castration-resistant and neuroendocrine prostate cancer: efficacy and biomarkers. Clin Cancer Res. 2019;25(1):43–51. https://doi.org/10.1158/1078-0432.Ccr-18-1912This was a phase II clinical trial of the aurora kinase inhibitor alisertib for patients with neuroendocrine prostate cancer.
Aparicio AM, Shen L, Tapia EL, Lu JF, Chen HC, Zhang J, et al. Combined tumor suppressor defects characterize clinically defined aggressive variant prostate cancers. Clin Cancer Res. 2016;22(6):1520–30. https://doi.org/10.1158/1078-0432.Ccr-15-1259.
Beltran H, Tomlins S, Aparicio A, Arora V, Rickman D, Ayala G, et al. Aggressive variants of castration-resistant prostate cancer. Clin Cancer Res. 2014;20(11):2846–50. https://doi.org/10.1158/1078-0432.Ccr-13-3309.
Bakht MK, Derecichei I, Li Y, Ferraiuolo RM, Dunning M, Oh SW, et al. Neuroendocrine differentiation of prostate cancer leads to PSMA suppression. Endocr Relat Cancer. 2018;26(2):131–46. https://doi.org/10.1530/erc-18-0226.
Tosoian JJ, Gorin MA, Rowe SP, Andreas D, Szabo Z, Pienta KJ, et al. Correlation of PSMA-targeted (18)F-DCFPyL PET/CT findings with immunohistochemical and genomic data in a patient with metastatic neuroendocrine prostate cancer. Clin Genitourin Cancer. 2017;15(1):e65–e8. https://doi.org/10.1016/j.clgc.2016.09.002.
Bakht MK, Lovnicki JM, Tubman J, Stringer KF, Chiaramonte J, Reynolds MR, et al. Differential expression of glucose transporters and hexokinases in prostate cancer with a neuroendocrine gene signature: a mechanistic perspective for (18)F-FDG imaging of PSMA-suppressed tumors. J Nucl Med. 2020;61(6):904–10. https://doi.org/10.2967/jnumed.119.231068.
Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, et al. [(177)Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19(6):825–33. https://doi.org/10.1016/s1470-2045(18)30198-0.
Reed DR, Pierce EJ, Sen JM, Keng MK. A prospective study on urine alkalization with an oral regimen consisting of sodium bicarbonate and acetazolamide in patients receiving high-dose methotrexate. Cancer Manag Res. 2019;11:8065–72. https://doi.org/10.2147/cmar.S190084.
Thang SP, Violet J, Sandhu S, Iravani A, Akhurst T, Kong G, et al. Poor outcomes for patients with metastatic castration-resistant prostate cancer with low prostate-specific membrane antigen (PSMA) expression deemed ineligible for (177)Lu-labelled PSMA radioligand therapy. Eur Urol Oncol. 2019;2(6):670–6. https://doi.org/10.1016/j.euo.2018.11.007.
Ballinger JR. Theranostic radiopharmaceuticals: established agents in current use. Br J Radiol. 2018;91(1091):20170969. https://doi.org/10.1259/bjr.20170969.
Desai H, Borges-Neto S, Wong TZ. Molecular imaging and therapy for neuroendocrine tumors. Curr Treat Options in Oncol. 2019;20(10):78. https://doi.org/10.1007/s11864-019-0678-6.
Mori H, Nakajima K, Kadomoto S, Mizokami A, Ikeda H, Wakabayashi H, et al. Imaging somatostatin receptor activity in neuroendocrine-differentiated prostate cancer. Intern Med. 2018;57(21):3123–8. https://doi.org/10.2169/internalmedicine.0630-17.
Hope TA, Aggarwal R, Simko JP, VanBrocklin HF, Ryan CJ. Somatostatin imaging of neuroendocrine-differentiated prostate cancer. Clin Nucl Med. 2015;40(6):540–1. https://doi.org/10.1097/rlu.0000000000000776.
Beltran H, Rickman DS, Park K, Chae SS, Sboner A, MacDonald TY, et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. Cancer Discov. 2011;1(6):487–95. https://doi.org/10.1158/2159-8290.Cd-11-0130.
Lotan TL, Gupta NS, Wang W, Toubaji A, Haffner MC, Chaux A, et al. ERG gene rearrangements are common in prostatic small cell carcinomas. Mod Pathol. 2011;24(6):820–8. https://doi.org/10.1038/modpathol.2011.7.
Zou M, Toivanen R, Mitrofanova A, Floch N, Hayati S, Sun Y, et al. Transdifferentiation as a mechanism of treatment resistance in a mouse model of castration-resistant prostate cancer. Cancer Discov. 2017;7(7):736–49. https://doi.org/10.1158/2159-8290.Cd-16-1174.
Tan HL, Sood A, Rahimi HA, Wang W, Gupta N, Hicks J, et al. Rb loss is characteristic of prostatic small cell neuroendocrine carcinoma. Clin Cancer Res. 2014;20(4):890–903. https://doi.org/10.1158/1078-0432.Ccr-13-1982.
Kaye FJ. RB and cyclin dependent kinase pathways: defining a distinction between RB and p16 loss in lung cancer. Oncogene. 2002;21(45):6908–14. https://doi.org/10.1038/sj.onc.1205834.
Tsai H, Morais CL, Alshalalfa M, Tan HL, Haddad Z, Hicks J, et al. Cyclin D1 loss distinguishes prostatic small-cell carcinoma from most prostatic adenocarcinomas. Clin Cancer Res. 2015;21(24):5619–29. https://doi.org/10.1158/1078-0432.Ccr-15-0744.
Beltran H, Prandi D, Mosquera JM, Benelli M, Puca L, Cyrta J, et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. Nat Med. 2016;22(3):298–305. https://doi.org/10.1038/nm.4045.
Ku SY, Rosario S, Wang Y, Mu P, Seshadri M, Goodrich ZW, et al. Rb1 and Trp53 cooperate to suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. Science. 2017;355(6320):78–83. https://doi.org/10.1126/science.aah4199.
Mu P, Zhang Z, Benelli M, Karthaus WR, Hoover E, Chen CC, et al. SOX2 promotes lineage plasticity and antiandrogen resistance in TP53- and RB1-deficient prostate cancer. Science. 2017;355(6320):84–8. https://doi.org/10.1126/science.aah4307.
Zhou Z, Flesken-Nikitin A, Corney DC, Wang W, Goodrich DW, Roy-Burman P, et al. Synergy of p53 and Rb deficiency in a conditional mouse model for metastatic prostate cancer. Cancer Res. 2006;66(16):7889–98. https://doi.org/10.1158/0008-5472.Can-06-0486.
Zhou Z, Flesken-Nikitin A, Nikitin AY. Prostate cancer associated with p53 and Rb deficiency arises from the stem/progenitor cell-enriched proximal region of prostatic ducts. Cancer Res. 2007;67(12):5683–90. https://doi.org/10.1158/0008-5472.Can-07-0768.
Gingrich JR, Barrios RJ, Kattan MW, Nahm HS, Finegold MJ, Greenberg NM. Androgen-independent prostate cancer progression in the TRAMP model. Cancer Res. 1997;57(21):4687–91.
Gingrich JR, Barrios RJ, Foster BA, Greenberg NM. Pathologic progression of autochthonous prostate cancer in the TRAMP model. Prostate Cancer Prostatic Dis. 1999;2(2):70–5. https://doi.org/10.1038/sj.pcan.4500296.
Kaur H, Samarska I, Lu J, Faisal F, Maughan BL, Murali S, et al. Neuroendocrine differentiation in usual-type prostatic adenocarcinoma: molecular characterization and clinical significance. Prostate. 2020;80:1012–23. https://doi.org/10.1002/pros.24035.
Nyquist MD, Corella A, Coleman I, De Sarkar N, Kaipainen A, Ha G, et al. Combined TP53 and RB1 loss promotes prostate cancer resistance to a spectrum of therapeutics and confers vulnerability to replication stress. Cell Rep. 2020;31(8):107669. https://doi.org/10.1016/j.celrep.2020.107669.
•• Beltran H, Romanel A, Conteduca V, Casiraghi N, Sigouros M, Franceschini GM et al. Circulating tumor DNA profile recognizes transformation to castration-resistant neuroendocrine prostate cancer. J Clin Invest. 2020. https://doi.org/10.1172/jci131041. Whole-exome and whole-genome bisulfite sequencing of plasma cell-free DNA and matched tumor biopsies from patients with castration-resistant adenocarcinoma and NEPC. Circulating tumor DNA detected genomic and epigenomic features of NEPC and also identified clonal/subclonal alterations involved in treatment resistance.
Chedgy EC, Vandekerkhove G, Herberts C, Annala M, Donoghue AJ, Sigouros M, et al. Biallelic tumour suppressor loss and DNA repair defects in de novo small-cell prostate carcinoma. J Pathol. 2018;246(2):244–53. https://doi.org/10.1002/path.5137.
Chen R, Dong X, Gleave M. Molecular model for neuroendocrine prostate cancer progression. BJU Int. 2018;122(4):560–70. https://doi.org/10.1111/bju.14207.
Ge R, Wang Z, Montironi R, Jiang Z, Cheng M, Santoni M, et al. Epigenetic modulations and lineage plasticity in advanced prostate cancer. Ann Oncol. 2020;31(4):470–9. https://doi.org/10.1016/j.annonc.2020.02.002.
Dardenne E, Beltran H, Benelli M, Gayvert K, Berger A, Puca L, et al. N-Myc induces an EZH2-mediated transcriptional program driving neuroendocrine prostate cancer. Cancer Cell. 2016;30(4):563–77. https://doi.org/10.1016/j.ccell.2016.09.005.
Puca L, Bareja R, Prandi D, Shaw R, Benelli M, Karthaus WR, et al. Patient derived organoids to model rare prostate cancer phenotypes. Nat Commun. 2018;9(1):2404. https://doi.org/10.1038/s41467-018-04495-z.
Li H, Wang L, Li Z, Geng X, Li M, Tang Q, et al. SOX2 has dual functions as a regulator in the progression of neuroendocrine prostate cancer. Lab Investig. 2020;100(4):570–82. https://doi.org/10.1038/s41374-019-0343-5.
Bishop JL, Thaper D, Vahid S, Davies A, Ketola K, Kuruma H, et al. The master neural transcription factor BRN2 is an androgen receptor-suppressed driver of neuroendocrine differentiation in prostate cancer. Cancer Discov. 2017;7(1):54–71. https://doi.org/10.1158/2159-8290.Cd-15-1263.
Lee TI, Jenner RG, Boyer LA, Guenther MG, Levine SS, Kumar RM, et al. Control of developmental regulators by Polycomb in human embryonic stem cells. Cell. 2006;125(2):301–13. https://doi.org/10.1016/j.cell.2006.02.043.
Zhang Y, Zheng D, Zhou T, Song H, Hulsurkar M, Su N, et al. Androgen deprivation promotes neuroendocrine differentiation and angiogenesis through CREB-EZH2-TSP1 pathway in prostate cancers. Nat Commun. 2018;9(1):4080. https://doi.org/10.1038/s41467-018-06177-2.
Kleb B, Estécio MR, Zhang J, Tzelepi V, Chung W, Jelinek J, et al. Differentially methylated genes and androgen receptor re-expression in small cell prostate carcinomas. Epigenetics. 2016;11(3):184–93. https://doi.org/10.1080/15592294.2016.1146851.
Fletcher JI, Ziegler DS, Trahair TN, Marshall GM, Haber M, Norris MD. Too many targets, not enough patients: rethinking neuroblastoma clinical trials. Nat Rev Cancer. 2018;18(6):389–400. https://doi.org/10.1038/s41568-018-0003-x.
Beltran H. The N-myc oncogene: maximizing its targets, regulation, and therapeutic potential. Mol Cancer Res. 2014;12(6):815–22. https://doi.org/10.1158/1541-7786.Mcr-13-0536.
Lee JK, Phillips JW, Smith BA, Park JW, Stoyanova T, McCaffrey EF, et al. N-Myc drives neuroendocrine prostate cancer initiated from human prostate epithelial cells. Cancer Cell. 2016;29(4):536–47. https://doi.org/10.1016/j.ccell.2016.03.001.
• Berger A, Brady NJ, Bareja R, Robinson B, Conteduca V, Augello MA, et al. N-Myc-mediated epigenetic reprogramming drives lineage plasticity in advanced prostate cancer. J Clin Invest. 2019;130:3924–40. https://doi.org/10.1172/jci127961This study showed that N-myc suppresses AR-signaling and drives lineage plasticity.
Katayama H, Wang J, Treekitkarnmongkol W, Kawai H, Sasai K, Zhang H, et al. Aurora kinase-A inactivates DNA damage-induced apoptosis and spindle assembly checkpoint response functions of p73. Cancer Cell. 2012;21(2):196–211. https://doi.org/10.1016/j.ccr.2011.12.025.
Zhang W, Liu B, Wu W, Li L, Broom BM, Basourakos SP, et al. Targeting the MYCN-PARP-DNA damage response pathway in neuroendocrine prostate cancer. Clin Cancer Res. 2018;24(3):696–707. https://doi.org/10.1158/1078-0432.Ccr-17-1872.
Metz EP, Wilder PJ, Dong J, Datta K, Rizzino A. Elevating SOX2 in prostate tumor cells upregulates expression of neuroendocrine genes, but does not reduce the inhibitory effects of enzalutamide. J Cell Physiol. 2020;235(4):3731–40. https://doi.org/10.1002/jcp.29267.
Tiwari R, Manzar N, Bhatia V, Yadav A, Nengroo MA, Datta D, et al. Androgen deprivation upregulates SPINK1 expression and potentiates cellular plasticity in prostate cancer. Nat Commun. 2020;11(1):384. https://doi.org/10.1038/s41467-019-14184-0.
Akamatsu S, Wyatt AW, Lin D, Lysakowski S, Zhang F, Kim S, et al. The placental gene PEG10 promotes progression of neuroendocrine prostate cancer. Cell Rep. 2015;12(6):922–36. https://doi.org/10.1016/j.celrep.2015.07.012.
Li Y, Donmez N, Sahinalp C, Xie N, Wang Y, Xue H, et al. SRRM4 drives neuroendocrine transdifferentiation of prostate adenocarcinoma under androgen receptor pathway inhibition. Eur Urol. 2017;71(1):68–78. https://doi.org/10.1016/j.eururo.2016.04.028.
Li Y, Xie N, Chen R, Lee AR, Lovnicki J, Morrison EA, et al. RNA splicing of the BHC80 gene contributes to neuroendocrine prostate cancer progression. Eur Urol. 2019;76(2):157–66. https://doi.org/10.1016/j.eururo.2019.03.011.
Li Y, Zhang Q, Lovnicki J, Chen R, Fazli L, Wang Y, et al. SRRM4 gene expression correlates with neuroendocrine prostate cancer. Prostate. 2019;79(1):96–104. https://doi.org/10.1002/pros.23715.
Ooi L, Wood IC. Chromatin crosstalk in development and disease: lessons from REST. Nat Rev Genet. 2007;8(7):544–54. https://doi.org/10.1038/nrg2100.
Lapuk AV, Wu C, Wyatt AW, McPherson A, McConeghy BJ, Brahmbhatt S, et al. From sequence to molecular pathology, and a mechanism driving the neuroendocrine phenotype in prostate cancer. J Pathol. 2012;227(3):286–97. https://doi.org/10.1002/path.4047.
Zhang X, Coleman IM, Brown LG, True LD, Kollath L, Lucas JM, et al. SRRM4 expression and the loss of REST activity may promote the emergence of the neuroendocrine phenotype in castration-resistant prostate cancer. Clin Cancer Res. 2015;21(20):4698–708. https://doi.org/10.1158/1078-0432.Ccr-15-0157.
Nakano Y, Wiechert S, Bánfi B. Overlapping activities of two neuronal splicing factors switch the GABA effect from excitatory to inhibitory by regulating rest. Cell Rep. 2019;27(3):860–71.e8. https://doi.org/10.1016/j.celrep.2019.03.072.
Yasumizu Y, Rajabi H, Jin C, Hata T, Pitroda S, Long MD, et al. MUC1-C regulates lineage plasticity driving progression to neuroendocrine prostate cancer. Nat Commun. 2020;11(1):338. https://doi.org/10.1038/s41467-019-14219-6.
Reina-Campos M, Linares JF, Duran A, Cordes T, L’Hermitte A, Badur MG, et al. Increased serine and one-carbon pathway metabolism by PKClambda/iota deficiency promotes neuroendocrine prostate cancer. Cancer Cell. 2019;35(3):385–400.e9. https://doi.org/10.1016/j.ccell.2019.01.018.
Guo H, Ci X, Ahmed M, Hua JT, Soares F, Lin D, et al. ONECUT2 is a driver of neuroendocrine prostate cancer. Nat Commun. 2019;10(1):278. https://doi.org/10.1038/s41467-018-08133-6.
Rotinen M, You S, Yang J, Coetzee SG, Reis-Sobreiro M, Huang WC, et al. ONECUT2 is a targetable master regulator of lethal prostate cancer that suppresses the androgen axis. Nat Med. 2018;24(12):1887–98. https://doi.org/10.1038/s41591-018-0241-1.
•• Corn PG, Heath EI, Zurita A, Ramesh N, Xiao L, Sei E, et al. Cabazitaxel plus carboplatin for the treatment of men with metastatic castration-resistant prostate cancers: a randomised, open-label, phase 1-2 trial. The Lancet Oncology. 2019;20(10):1432–43. https://doi.org/10.1016/s1470-2045(19)30408-5In this phase 2 trial, carboplatin added to cabazitaxel demonstrated improved efficacy compared with cabazitaxel alone for prostate cancer patients with AVPC features.
Horn L, Mansfield AS, Szczęsna A, Havel L, Krzakowski M, Hochmair MJ, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220–9. https://doi.org/10.1056/NEJMoa1809064.
Antonia SJ, López-Martin JA, Bendell J, Ott PA, Taylor M, Eder JP, et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): a multicentre, open-label, phase 1/2 trial. The Lancet Oncology. 2016;17(7):883–95. https://doi.org/10.1016/s1470-2045(16)30098-5.
Gong X, Du J, Parsons SH, Merzoug FF, Webster Y, Iversen PW, et al. Aurora a kinase inhibition is synthetic lethal with loss of the RB1 tumor suppressor gene. Cancer Discov. 2019;9(2):248–63. https://doi.org/10.1158/2159-8290.Cd-18-0469.
Owen DH, Giffin MJ, Bailis JM, Smit MD, Carbone DP, He K. DLL3: an emerging target in small cell lung cancer. J Hematol Oncol. 2019;12(1):61. https://doi.org/10.1186/s13045-019-0745-2.
Puca L, Gavyert K, Sailer V, Conteduca V, Dardenne E, Sigouros M, et al. Delta-like protein 3 expression and therapeutic targeting in neuroendocrine prostate cancer. Sci Transl Med. 2019;11(484). https://doi.org/10.1126/scitranslmed.aav0891.
Lee JK, Bangayan NJ, Chai T, Smith BA, Pariva TE, Yun S, et al. Systemic surfaceome profiling identifies target antigens for immune-based therapy in subtypes of advanced prostate cancer. Proc Natl Acad Sci U S A. 2018;115(19):E4473–e82. https://doi.org/10.1073/pnas.1802354115.
Sehrawat A, Gao L, Wang Y, Bankhead A 3rd, McWeeney SK, King CJ, et al. LSD1 activates a lethal prostate cancer gene network independently of its demethylase function. Proc Natl Acad Sci U S A. 2018;115(18):E4179–e88. https://doi.org/10.1073/pnas.1719168115.
Stewart CA, Byers LA. Altering the course of small cell lung cancer: targeting cancer stem cells via LSD1 inhibition. Cancer Cell. 2015;28(1):4–6. https://doi.org/10.1016/j.ccell.2015.06.011.
Aggarwal RR, Schweizer MT, Nanus DM, Pantuck AJ, Heath EI, Campeau E, et al. A phase 1b/2a study of the pan-BET bromodomain inhibitor ZEN-3694 in combination with enzalutamide in patients with metastatic castration resistant prostate cancer. Clin Cancer Res. 2020;26:5338–47. https://doi.org/10.1158/1078-0432.Ccr-20-1707.
Funding
Y.Y. is supported by a Uehara Memorial Foundation Fellowship. H.B. is supported by the Prostate Cancer Foundation, National Cancer Institute R37 CA241486-01A1, and Department of Defense PCRP W81XWH-17-1-0653.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Y.Y. reports no conflicts of interest. H.B. has received research funding from Janssen, Abbvie Stemcentryx, Astellas, Eli Lilly, and Millenium and has served as an advisor/consultant for Janssen, Pfizer, Astellas, Amgen, AstraZeneca, and Sanofi Genzyme.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Genitourinary Cancers
Rights and permissions
About this article
Cite this article
Yamada, Y., Beltran, H. Clinical and Biological Features of Neuroendocrine Prostate Cancer. Curr Oncol Rep 23, 15 (2021). https://doi.org/10.1007/s11912-020-01003-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-020-01003-9