Abstract
Purpose of Review
Hospital-acquired and ventilator-associated pneumonia (VAP) are frequent causes of infection among critically ill patients. VAP is the most common hospital-acquired bacterial infection among mechanically ventilated patients. Unfortunately, many of the nosocomial Gram-negative bacteria that cause VAP are increasingly difficult to treat. Additionally, the evolution and dissemination of multi- and pan-drug resistant strains leave clinicians with few treatment options. VAP patients represent a dynamic population at risk for antibiotic failure and under-dosing due to altered antibiotic pharmacokinetic parameters. Since few antibiotic agents have been approved within the last 15 years, and no new agents specifically targeting VAP have been approved to date, it is anticipated that this problem will worsen. Given the public health crisis posed by resistant Gram-negative bacteria, it is essential to establish a firm understanding of the current epidemiology of VAP, the changing trends in Gram-negative resistance in VAP, and the current issues in drug development for Gram-negative bacteria that cause VAP.
Recent Findings
Rapid identification technologies and phenotypic methods, new therapeutic strategies, and novel treatment paradigms have evolved in an attempt to improve treatment outcomes for VAP; however, clinical data supporting alternative treatment strategies and adjunctive therapies remain sparse. Importantly, new classes of antimicrobials, novel virulence factor inhibitors, and beta-lactam/beta-lactamase inhibitor combinations are currently in development. Conscientious stewardship of new and emerging therapeutic agents will be needed to ensure they remain effective well into the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: Gram-Negative Resistance in VAP
Ventilator-associated pneumonia (VAP) is a devastating nosocomial infection responsible for excessive morbidity and mortality. Attributable mortality in VAP is roughly 9–13%, but higher mortality rates in select populations have been observed [1, 2]. VAP remains a common hospital-acquired bacterial infection among mechanically ventilated patients [3], with management complicated by increasing Gram-negative resistance [4]. The evolution and dissemination of multidrug resistance [5] among Gram-negative bacteria means that for some patients with VAP, no active reliable treatments exist [4, 6]. In this review, we focus on epidemiological trends in VAP, the evolving landscape of Gram-negative resistance, and currently available and emerging treatments options for patients with VAP caused by Gram-negative bacteria.
VAP Epidemiology: Definitions, Surveillance, and Diagnostic Testing
Consensus guidelines define VAP as a pneumonia occurring > 48 h after endotracheal intubation [7]. VAP occurs in between one tenth and one third of mechanically ventilated patients [7] with estimated incidence rates between 1.2 and 8.5 cases per 1000 ventilator days [8]. However, the frequency of VAP has been challenging to measure. No widely accepted diagnostic test for VAP is currently available [9], and reliable definitions remain elusive [10].
Evolving Definitions
Decreasing VAP rates according to the National Healthcare Safety Network (NHSN) were noted between 2006 and 2012 [11, 12]. However, a contemporaneous patient-level analysis revealed stable VAP rates [13]. Correspondingly, the updated VAP surveillance definition now classifies ventilator-associated events using clinical and temporal criteria [10]. While this definition was initially felt to be highly sensitive (93.5%, 95% CI 77.2–98.8%) and specific (100%, 95% CI 98.8–100%) for VAP [14], subsequent studies demonstrated lower operating characteristics and susceptibility to manipulation [15, 16]. Underreporting VAP within the surgical and trauma populations also remains problematic [15, 16]. Reliable VAP definitions applicable to multiple highly variable ICU populations are necessary.
Diagnostic Testing
Improved definitions paired with cutting-edge diagnostics may improve the accuracy of VAP identification. Standard culture-based testing requires specimen inoculation and growth in media, with identification and susceptibility results occurring days later. Molecular methods (i.e., rapid diagnostics) can identify Gram-negative species and detect resistance minutes to hours after specimen collection. The revolution in rapid diagnostics means that near real-time pathogen and resistance identification is possible.
Genotypic Methods
Genotypic tests, like automated real-time multiplex polymerase chain reaction (PCR) and microarray platforms, are examples of emerging diagnostic methods [17, 18]. Curetis Unyvero (Curetis AG) is a multiplex PCR hybridization system designed to identify pneumonia pathogens and resistance genes in respiratory samples [19]. A similar panel is under development for the Biofire platform. Verigene is a nanoparticle-based amplification method for identifying Gram-negative species and resistance genes, but this panel is only Food and Drug Administration (FDA)-approved for positive blood cultures identified using conventional growth detection methods [20]. Ribosomal amplification (e.g., 16S ribosomal RNA gene PCR) has also been evaluated in suspected VAP cases [21, 22].
Phenotypic Methods
Rapid phenotypic methods provide susceptibility or resistance classification and may complement rapid identification methods. The Carba NP test (Biomerieux) directly detects carbapenem hydrolysis and can identify the presence of specific carbapenemases irrespective of species [23]. Automated systems, like the Accelerate Pheno system (Accelerate Diagnostics), provide identification and susceptibility data 1–2 days faster than traditional methods [24].
Other Emerging Methods
Emerging technologies are able to identify Gram-negative bacteria directly from clinical specimens. T2Bacteria (T2Biosystems) utilizes magnetic resonance to identify pathogens directly from blood, but this panel has not been FDA cleared [25]. Deep sequencing technologies have also recently been applied to clinical specimens.
Epidemiology of Gram-Negative VAP Pathogens
Gram-negative VAP pathogens are increasingly antibiotic resistant [4, 26]. National and international surveillance databases (e.g., NHSN, INFORM, SENTRY) document the dissemination of Gram-negative resistance [26,27,28]. For example, up to 40% of select Gram-negatives in the USA exhibit multi-drug resistance (MDR) [5], suggesting that broad empiric therapy may be required. Recent trials also provide Gram-negative recovery and susceptibility rates. In the following section, we review trends from surveillance databases and clinical trials.
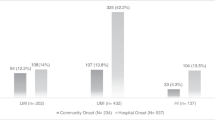
Recent Trends in Gram-Negative Rates
Gram-negative recovery in VAP varies globally; yet, specific pathogens are consistently recovered. Pseudomonas aeruginosa, Acinetobacter spp., and Enterobacteriaceae have been frequently implicated [9, 26,27,28]. Surveillance recovery rates are summarized in Table 1. Here, we review Gram-negative rates in nosocomial pneumonia.
P. aeruginosa
P. aeruginosa is the preeminent and most common Gram-negative nosocomial pneumonia and VAP pathogen in the USA, as confirmed in multiple studies (Table 1) [26,27,28, 30]. European clinical studies also support the prominent role of P. aeruginosa in VAP (14–19% of cases) [31, 32].
Acinetobacter baumannii
A. baumannii ranks among the top five VAP pathogens worldwide. NHSN surveillance identified A. baumannii as the fifth most common VAP pathogen in the USA and Europe, accounting for 6.1 to 7.5% of VAP cases (Table 1) [26, 27]. However, only 2.7 and 3.3% of US VAP isolates were A. baumannii in the SENTRY and INFORM databases, respectively [28, 30]. The prevalence of A. baumannii within Asian countries was slightly higher than US and European rates [33, 34].
Enterobacteriaceae
Members of the Enterobacteriaceae genus have also been frequently recovered in VAP; four of the top ten Gram-negative VAP pathogens are Enterobacteriaceae [27]. K. pneumoniae and Enterobacter spp. were identified in 10.2 and 8.3% of VAP cases by NHSN surveillance [27] and contributed 10.0 and 7.7% of VAP cases, respectively, within SENTRY [30]. INFORM found slightly higher rates of K. pneumoniae and Enterobacter spp. among Gram-negative VAP cases (Table 1) [28]. E. coli and Serratia spp. are also among the top ten VAP pathogens [26, 28, 30]. Within the European and Mediterranean regions, Enterobacteriaceae were also common [26] and increasing in frequency [35]. E. coli was the most common European pathogen. Klebsiella spp. were responsible for a similar proportion of infections in Europe and the USA (11.6 vs. 9.7%) (Table 1).
Recent Trends in Gram-Negative Resistance
Gram-negative resistance has become a global crisis. Among Gram-negative VAP pathogens, multidrug resistance and resistance to last-line agents (e.g., colistin) is alarmingly common. Resistance among P. aeruginosa and A. baumannii has become the norm, while carbapenem resistance among Enterobacteriaceae has emerged as an imminent threat to global health [4, 36]. In the following section, we review Gram-negative VAP pathogen resistance trends using Clinical and Laboratory Standards Institute definitions (2010–present).
P. aeruginosa Resistance
P. aeruginosa has the capacity to develop resistance to all VAP antibiotics. Carbapenem resistance has been documented in 16.1–28.4% of US nosocomial pneumonia isolates [26,27,28, 30]. Among VAP isolates, P. aeruginosa resistance to anti-pseudomonal penicillins (e.g., piperacillin-tazobactam, 15.6–19.1%) and anti-pseudomonal cephalosporins (e.g., ceftazidime or cefepime, 9.5–29.4%) is increasingly common [26,27,28, 30]. The aminoglycosides tobramycin and amikacin appear to retain good individual activity against P. aeruginosa in some studies (> 90% susceptible) [26, 28]. However, resistance to ≥ 1 aminoglycoside (e.g., amikacin or gentamicin or tobramycin) is increasingly common among VAP isolates (18.2–23.3% resistant) [27]. Colistin remains active against P. aeruginosa (98–99.6% susceptible) [26, 28]. Resistance among European and Mediterranean isolates was also common. With the exception of colistin, European isolates were more likely than US isolates to exhibit resistance [26]. Beta-lactam resistance among P. aeruginosa respiratory isolates is alarmingly common, while aminoglycosides and colistin remain fairly active.
A. baumannii Resistance
A. baumannii is frequently MDR and often carbapenem resistant. Over 50% of US A. baumannii VAP isolates were MDR, and up to 64% of isolates exhibited carbapenem resistance (55.5–63.5%) [26, 27]. With resistance rates less than 5%, colistin appears active against A. baumannii [26]. Resistance to minocycline was found in 14.8% of isolates, and tigecycline MICs exceeding the FDA Enterobacteriaceae breakpoint [37] were found in 1.6% of isolates [26]. European and Mediterranean A. baumannii pneumonia isolates demonstrated similar resistance patterns, with slightly higher meropenem and minocycline resistance (67.1 and 22.2%, respectively) [26]. Few VAP agents have reliable activity against A. baumannii. Colistin, minocycline, and tigecycline may retain activity, but susceptibility testing is essential.
Enterobacteriaceae Resistance
Resistance among Enterobacteriaceae is particularly concerning and often varies by genera. In the USA, cefepime or ceftazidime resistance varies widely (2.7–30%) [26, 27]. Carbapenem resistance in E. coli and Enterobacter spp. remains relatively low (0.5–2.2% and 1–3.2%, respectively) [26,27,28]. Klebsiella spp. have demonstrably higher carbapenem-resistance rates (6.9–11.5%) [26,27,28]. European and Mediterranean Enterobacteriaceae were more likely to exhibit MDR and to carry genes encoding extended-spectrum beta-lactamases (ESBLs) [26]. Similar to the US, carbapenem resistance among Klebsiella spp. was common [26]. Carbapenem-resistant Enterobacteriaceae (CRE) were found in 58 centers in 18 European countries, comprising 2% of all Enterobacteriaceae; however, large inter-country variability exists [30]. Cases of colistin-resistant mcr-1-carrying Enterobacteriaceae infections have been documented in the USA, Europe, and Asia [37,38,40]. The global dissemination of CRE and mcr-1-carrying isolates has significantly impacted the management of VAP patients, leaving clinicians with few or no safe and effective treatments.
Contemporary Treatment Strategies for Gram-Negative VAP
While new therapeutic agents and novel treatment approaches are currently being investigated, clinicians caring for patients with Gram-negative VAP are caught between two opposing forces: increasing resistance on one hand and a dwindling antibiotic armamentarium on the other. In the following section, we describe new antibiotics, new uses of older antibiotics, and novel strategies for Gram-negative VAP pathogens.
Agents for the Treatment of VAP Caused by MDR Gram-Negative Bacteria
The increasing frequency with which MDR Gram-negative bacteria cause VAP has forced clinicians and pharmaceutical companies to become more creative. Old antibiotics have been recycled, established antibiotics have been used in new ways, new antibiotics have been developed, and entirely novel therapeutic strategies are being investigated (Table 2).
Renaissance Antibiotics
Antimicrobial resistance has become so pervasive and extreme that formerly discarded antibiotics are being recycled in attempts to find agents that retain activity against MDR bacteria. Some of these “renaissance antibiotics” now play an important role in clinical practice.
Fosfomycin
Fosfomycin is a derivative of phosphonic acid that blocks an early stage in the synthesis of peptidoglycan, a component of the bacterial cell wall [41]. First discovered in 1969 [42], fosfomycin has recently received renewed interest for MDR Gram-negative bacteria. Approximately three fourths of carbapenem-resistant K. pneumoniae isolates are susceptible to fosfomycin [43]. However, fosfomycin monotherapy is less active against P. aeruginosa and A. baumannii, with resistance emerging rapidly [44]. Although not currently available in the USA, intravenous fosfomycin penetrates the lung well, and limited data suggest it may be efficacious in this setting [45].
Polymyxins
First used in the 1950s, systemic polymyxins [B and E (i.e., colistin)] were abandoned by the early 1980s due to toxicity and availability of safer alternatives. In recent years, they have re-emerged for the treatment of MDR Gram-negative bacteria, including P. aeruginosa, Acinetobacter spp., E. coli, and Klebsiella spp. However polymyxins lack activity against some other Gram-negatives, such as Proteus and Serratia spp. Susceptibility notwithstanding, polymyxins suffer from two disadvantages. High-dose systemic polymyxin regimens that are necessary for serious infections like VAP have been associated with renal toxicity rates of 20% or more [46], and cure rates with monotherapy are low [47]. Thus, current VAP guidelines suggest avoiding systemic polymyxins when alternatives exist [9].
Minocycline
Minocycline, an FDA-approved semisynthetic tetracycline derivative first developed in the 1960s [48], has only recently been used for MDR Gram-negative VAP [49]. Like tigecycline, minocycline has Gram-negative activity [50] but yields higher blood levels than tigecycline [51]. Minocycline is active against some Acinetobacter and Stenotrophomonas spp. and some Enterobacteriaceae but not Serratia spp., Proteus spp., or P. aeruginosa [50]. Minocycline has garnered interest for MDR A. baumannii VAP, with a number of clinical responses reported across 23 cases [49]. Though controlled VAP trials are lacking, minocycline exhibits good lung penetration [measured by the epithelial lining fluid to serum (ELF/serum) AUC ratio ~2.5] and A. baumannii killing in a mouse model [52].
New Antibiotics
Approved Antibiotics
Tigecycline
Tigecycline, a glycylcycline antibiotic approved by the FDA in 2005, has broad Gram-negative activity including some CRE [30] but not P. aeruginosa or Proteus mirabilis. In a randomized controlled trial of 945 people with HAP/VAP, tigecycline was associated with lower response rates than imipenem [53]. Tigecycline was also associated with excess mortality in several studies [50,54,56], driven primarily by patients with nosocomial pneumonia. For these reasons, tigecycline should primarily be used as a component of combination therapy [9].
Doripenem
Doripenem, a carbapenem approved by the FDA in 2007, initially showed promise for treatment of patients with Gram-negative VAP [57]. In vitro testing showed slightly lower MICs against P. aeruginosa compared to other carbapenems [58]. However, a subsequent study of 274 patients with Gram-negative VAP randomly assigned to receive a 7-day course of doripenem or a 10-day course of imipenem-cilastatin was stopped prematurely due to a lower cure rate (45.6 vs. 56.8%; 95% CI, − 26.3 to 3.8%) and higher all-cause 28-day mortality (21.5 vs. 14.8%; 95% CI, − 5.0 to 18.5) in the doripenem treatment arm [59]. As a result, current VAP guidelines do not recommend the use of doripenem [9].
Ceftazidime-Avibactam
Unlike other approved beta-lactamase inhibitors, avibactam is not a beta-lactam but does bind beta-lactamases. Ceftazidime-avibactam has enhanced activity against Enterobacteriaceae (including ceftazidime-resistant strains) and P. aeruginosa. Arguably, the most useful aspect of this antibiotic is its ability to inhibit ESBLs, AmpC beta-lactamases, and serine carbapenemases [60]. However, metallo-beta-lactamases (e.g., IMP, VIM, NDM) are not inhibited by avibactam [60]. Accordingly, ceftazidime-avibactam has good activity against Enterobacteriaceae and P. aeruginosa, but not Acinetobacter and Stenotrophomonas spp. A phase III non-inferiority nosocomial pneumonia trial [61] found that ceftazidime-avibactam was non-inferior to meropenem with respect to 28-day mortality [risk difference (RD) 1.5%; 95% CI − 2.4-5.3] and cure [RD 1.9%; 95% CI − 8.1-4.3] without the emergence of resistance [62]. Of concern, though, are numerous reports of resistance to this agent are already appearing [61,63,65] including treatment-emergent resistance [66].
Ceftolozane-Tazobactam
Whereas ceftazidime-avibactam combines an old cephalosporin with a novel beta-lactamase inhibitor, ceftolozane-tazobactam combines an old beta-lactamase inhibitor with a novel cephalosporin. Ceftolozane has features of ceftazidime but has a bulkier side chain, which prevents cleavage by AmpC beta-lactamases [67], enhancing activity against P. aeruginosa. The combination also appears to have activity against non-CRE ESBL-producing Enterobacteriaceae [68, 69]. Like ceftazidime-avibactam, ceftolozane-tazobactam has little activity against A. baumannii and Stenotrophomonas spp. [60]. The ELF/serum AUC ratio for ceftolozane was approximately 50% [70, 71•], indicating a potential role in VAP. The efficacy of ceftolozane-tazobactam in VAP is currently being studied (NCT02070757).
Meropenem-Vaborbactam
Meropenem-vaborbactam was approved by the FDA in 2017. Vaborbactam is a boronic acid serine β-lactamase inhibitor with activity against ESBLs, AmpCs, and serine carbapenemases but not metallo-beta-lactamases. Meropenem-vaborbactam has broad activity against E. coli, K. pneumoniae, and Enterobacter spp., including ESBL and CRE isolates, but activity against non-fermenting Gram-negatives is similar to meropenem alone [72]. The TANGO-2 phase III clinical trial of meropenem-vaborbactam for the treatment of infections of the lung, blood, urinary tract, and abdomen was stopped prematurely following enrollment of 72 patients (43 had confirmed CRE), because the interim analysis showed a statistically significant difference in clinical cure favoring meropenem-vaborbactam over best available therapy for patients with CRE [73]. Mortality rates were also lower in patients treated with meropenem-vaborbactam. Both meropenem and vaborbactam achieve ≥ 65% ELF/serum AUC ratios in healthy adults, suggestive of activity in HAP and VAP [74]. However, pharmacokinetic data from patients with VAP indicate that meropenem ELF/serum AUC ratios may be lower (median < 30%) and highly variable [75]. The efficacy of meropenem-vaborbactam in HAP and VAP is currently being studied (NCT03006679).
Ceftobiprole
Ceftobiprole, a cephalosporin broadly active against Gram-positives and Gram-negatives including P. aeruginosa, is approved in several European countries but not the USA. A recent phase III trial of 781 patients found ceftobiprole to be equivalent to linezolid plus ceftazidime in the clinical cure of HAP but perhaps inferior among VAP patients [76]. Additional studies are necessary to evaluate the effectiveness of ceftobiprole in VAP.
Antibiotics in Clinical Trials
Imipenem-Cilastatin/Relebactam
Relebactam is a non-β-lactam inhibitor of β-lactamases with structural similarity to avibactam. It too has good activity against ESBLs, AmpCs, and serine carbapenemases but not metallo-beta-lactamases [77, 78]. Relebactam extends imipenem’s spectrum to include otherwise resistant E. coli, K. pneumoniae, and Enterobacter spp. strains. Relebactam’s activity against non-fermenting Gram-negative bacteria such as P. aeruginosa, A. baumannii, and S. maltophilia appears more limited [78]. Both imipenem and relebactam showed good lung penetration, suggesting potential efficacy in VAP [79]. Phase III clinical trials of imipenem-cilastatin/relebactam vs. imipenem-cilastatin or piperacillin/tazobactam in HAP and VAP are underway [80, 81].
Plazomicin
Plazomicin, an aminoglycoside derivative, avoids modification and inactivation by many of the enzymes that typically cause aminoglycoside resistance [82]. Plazomicin does not inhibit bacteria that express ribosomal methyltransferases (e.g., 16s rRNA methylases) [83]. Plazomicin has good activity against MDR Enterobacteriaceae, including ESBL and serine carbapenemase producers. Against P. aeruginosa and A. baumannii, plazomicin may be more active than amikacin [84]. In a phase III trial (CARE) studying nosocomial pneumonia caused by CRE, plazomicin exhibited a mortality benefit relative to colistin when both agents were used with either meropenem or tigecycline [85]. The efficacy of plazomicin for the treatment of VAP is unknown, and the ELF/serum AUC ratio was ~ 13% [83]. Of note, plazomicin’s renal toxicity profile appeared favorable compared with colistin [86, 87].
Eravacycline
Eravacycline has structural similarity to tigecycline and also acts by binding the ribosome to inhibit protein synthesis [88]. It has broad activity against aerobic and facultative Gram-positive and Gram-negative bacteria. Eravacycline has potent activity against Enterobacteriaceae, including ESBL-, KPC-, and NDM-producing isolates [89, 90]. Compared to tigecycline, eravacycline exhibited modestly lower MICs against A. baumannii and S. maltophilia but no enhanced activity against P. aeruginosa [89, 90]. One potential advantage of eravacycline is the availability of an oral formulation. In the phase III IGNITE1 and IGNITE4 clinical trials twice daily IV eravacycline was non-inferior to ertapenem or meropenem among patients with complicated intra-abdominal infections [91, 92]. In a phase III (IGNITE2) clinical trial of hospitalized patients with complicated urinary tract infections, eravacycline was inferior to levofloxacin [93]; however, patients receiving IV eravacycline responded better than those receiving oral eravacycline. The role of eravacycline in VAP is currently unclear.
New Tactics: Unconventional Uses of Existing Agents
Another approach to treating patients with VAP caused by MDR bacteria is to use currently approved antibiotics in new ways to enhance efficacy.
Inhaled Antibiotics
Aerosolized administration of antibiotics has the theoretical advantage of achieving high local concentrations of antimicrobial agents in the lungs, perhaps even exceeding the MICs of resistant Gram-negative bacteria. A meta-analysis of a randomized controlled trial and observational studies (437 total patients) examined the use of adjunctive nebulized antibiotics in MDR VAP and showed significantly higher clinical resolution among patients receiving nebulization (OR 1.96; 95% CI 1.30–2.96) [94]. Nebulization has been used with the following Gram-negative antibiotics: gentamicin, tobramycin, amikacin, aztreonam, ceftazidime, and colistin [95]. Current guidelines recommend adjunctive inhaled antibiotics for the treatment of VAP caused by Gram-negative bacteria susceptible to only aminoglycosides or polymyxins.
Macrolides
Macrolides do not exhibit in vitro activity against most Gram-negative VAP pathogens. Yet, these agents can produce potentially beneficial immunomodulatory changes in pneumonia. A multicenter, double-blinded study of 200 ICU patients with sepsis and VAP found that adjunctive clarithromycin led to earlier VAP resolution and faster mechanical ventilation weaning [96, 97].
Prolonged Infusions of Beta-Lactams
Prolonged infusion (PI) dosing of beta-lactams includes extended infusion (3–4 h; EI) and continuous infusion (24 h; CI) dosing. VAP clinical cure was greater [98, 99], but mortality was similar with PI piperacillin-tazobactam versus standard infusion [98,99,100]. VAP clinical cure was also higher with PI ceftazidime (89 vs. 52%: P < 0.001) and PI meropenem (90 vs. 60%: P < 0.001) versus standard infusion [101, 102]. Randomized trials have evaluated CI vs. standard infusion [103,104,105]. CI-treated patients had a lower risk of mortality (RR 0.74; 95% CI 0.56–1.00; P = 0.045) and a greater chance of clinical cure (RR 1.2; 95% CI 1.03–1.40; P = 0.021) in a patient-level meta-analysis of three trials [106••]. The majority of patients had a respiratory source of infection (55%) [106••]. Until high-quality trials evaluating VAP outcomes are available, PI dosing appears reasonable [9].
Standard Versus Long Treatment Durations
Several studies have compared the clinical efficacy of standard (≤ 8 days) versus long (> 8 days) treatment durations [59, 107, 108•, 109,109,111]. A systematic review and meta-analysis failed to identify a benefit of long durations on 28-day mortality (n = 3 studies; OR = 1.18, 95% CI 0.77–1.8), 28-day mortality among patients with non-fermenting Gram-negatives (n = 2 studies; OR = 0.95, 95% CI 0.39–2.27), or overall pneumonia recurrence (n = 19 studies; OR = 1.41, 95% CI 0.94–2.12) [112]. In the subset of patients with non-fermenting Gram-negatives, the risk of recurrence favored a long duration (n = 2 studies; OR = 2.18. 95% CI 1.14–4.16) [112]. A randomized, open-label, non-inferiority study (iDIAPASON) will compare 8 versus 15 days for P. aeruginosa VAP specifically [113]. The shortest effective duration of VAP treatment also remains unclear. Recent (NCT00410527, NCT01554657) and ongoing (NCT01994980) trials will evaluate short (i.e., 3–5 days) durations. Currently, 7- to 8-day durations are reasonable for improving patients [9].
Novel Strategies
Perhaps predictably, the pressures on the conventional antibiotic pipeline have led to efforts to use unconventional approaches to treat MDR Gram-negatives. Here, we briefly discuss several examples.
Cefiderocol
Cefiderocol is a siderophore-cephalosporin conjugate that works as a “Trojan horse.” It binds iron and then uses the bacterium’s iron uptake system to penetrate the outer membrane [114]. In so doing, it overcomes multiple resistance mechanisms (e.g., porin channel deletion, efflux pump overexpression) while localizing the cephalosporin within the periplasm, adjacent to PBPs. Cefiderocol has in vitro activity against many Gram-negative bacteria, including CRE, P. aeruginosa, A. baumannii, and S. maltophilia. In a study of 753 MDR clinical isolates, including carbapenemase- and ESBL-producing bacteria, cefiderocol had superior in vitro activity to meropenem, ceftazidime, and ceftazidime-avibactam and equivalent activity to colistin and tigecycline [115]. A clinical trial for the treatment of nosocomial pneumonias comparing cefiderocol to meropenem, each in combination with linezolid, is underway (NCT03032380).
Anti-Virulence Therapies
Disabling a bacterium’s virulence factors may prevent it from damaging tissues and make it vulnerable to clearance by the host immune system. Such approaches are not new; antibody-containing serum that bound and inactivated diphtheria toxin was used in the 1800s [116]. Advanced agents currently under development are inhibitors of type III secretion systems [117], complex multi-protein needle-like apparatuses used by some Gram-negative bacteria to intoxicate human cells. MEDI3902 (AstraZeneca) is a chimeric bispecific monoclonal antibody that recognizes both the tip of the P. aeruginosa type III secretion needle and surface polysaccharide Psl [118]. The presence of both antigen-binding sites confers synergistic protection against P. aeruginosa in animal models [118]. A phase II clinical trial examining the efficacy of MEDI3902 in preventing P. aeruginosa pneumonia among mechanically ventilated patients is currently enrolling patients. Additional antibody therapeutics (e.g., Aerubumab, Adiris Pharmaceuticals) are in development and entering clinical trials (NCT03027609).
Quorum-Sensing Inhibition
Quorum sensing (QS) is a cell density-dependent communication system that utilizes signaling molecules (auto-inducers) to regulate virulence in many bacteria. Several natural and engineered compounds block quorum-sensing by preventing the synthesis of auto-inducers or by blocking auto-inducer receptor binding [119] and have shown efficacy in mouse models [120, 121].
Biofilm Prevention
Endotracheal tube biofilms are thought to play an important role in VAP. Biofilm eradication can be difficult, in part, because biofilm-forming bacteria can persist in the presence of antibiotics and a robust immune response [122, 123]. Endotracheal tubes coated with silver may prevent or delay development of biofilms and VAP [124].
Phage Therapy
Phages (viruses that infect bacteria) specifically target an individual bacterial species or strain, do not infect human cells, and have little or no effect on normal microbial flora. However, the development of resistance, neutralizing host immune responses, and formulation and stability issues are concerns [125]. Phages are exquisitely specific, so phage cocktails are required to target multiple species or strains within a species. Such cocktails showed promise in phase I/II clinical studies against P. aeruginosa-mediated chronic otitis [126]. Recent anecdotal reports suggest efficacy in humans against MDR P. aeruginosa and A. baumannii [127, 128].
Other Strategies
Host-directed therapies [129], microbiome alterations (e.g., probiotics) [130], nanotechnology [131], endolysins [132], and bacteriocins [133] have all been investigated as novel treatments for bacterial infections.
Summary
Gram-negative bacteria appear poised to win the antibiotic resistance war. The pace of the development and spread of MDR strains has outstripped the medical community’s ability to develop novel antimicrobial agents. However, the number and breadth of new and exciting approaches currently being explored is reason for hope that the balance will soon shift. The results of preclinical, clinical, and epidemiological studies over the coming years will demonstrate whether these new approaches will indeed fulfill their promise and provide clinicians with effective treatments for VAP patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Melsen WG, Rovers MM, Koeman M, Bonten MJ. Estimating the attributable mortality of ventilator-associated pneumonia from randomized prevention studies. Crit Care Med. 2011;39(12):2736–42. https://doi.org/10.1097/CCM.0b013e3182281f33.
Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13(8):665–71. https://doi.org/10.1016/S1473-3099(13)70081-1.
Hunter JD. Ventilator associated pneumonia. BMJ. 2012;344(may29 1):e3325. https://doi.org/10.1136/bmj.e3325.
Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf. Accessed: 06/19/2017. Last updated: 07/14/2014.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81. https://doi.org/10.1111/j.1469-0691.2011.03570.x.
Boucher HW, Ambrose PG, Chambers HF, Ebright RH, Jezek A, Murray BE, et al. White paper: developing antimicrobial drugs for resistant pathogens, narrow-spectrum indications, and unmet needs. J Infect Dis. 2017;216(2):228–36. https://doi.org/10.1093/infdis/jix211.
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. https://doi.org/10.1164/rccm.200405-644ST.
Skrupky LP, McConnell K, Dallas J, Kollef MH. A comparison of ventilator-associated pneumonia rates as identified according to the National Healthcare Safety Network and American College of Chest Physicians criteria. Crit Care Med. 2012;40(1):281–4. https://doi.org/10.1097/CCM.0b013e31822d7913.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–e111. https://doi.org/10.1093/cid/ciw353.
Centers for Disease Control and Prevention. Device Associated Module - Ventilator Associated Event (VAE). 2017. https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf.
Edwards JR, Peterson KD, Andrus ML, Tolson JS, Goulding JS, Dudeck MA, et al. National Healthcare Safety Network (NHSN) Report, data summary for 2006, issued June 2007. Am J Infect Control. 2007;35(5):290–301. https://doi.org/10.1016/j.ajic.2007.04.001.
Dudeck MA, Weiner LM, Allen-Bridson K, Malpiedi PJ, Peterson KD, Pollock DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control. 2013;41(12):1148–66. https://doi.org/10.1016/j.ajic.2013.09.002.
Metersky ML, Wang Y, Klompas M, Eckenrode S, Bakullari A, Eldridge N. Trend in ventilator-associated pneumonia rates between 2005 and 2013. JAMA. 2016;316(22):2427–9. https://doi.org/10.1001/jama.2016.16226.
Stevens JP, Silva G, Gillis J, Novack V, Talmor D, Klompas M, et al. Automated surveillance for ventilator-associated events. Chest. 2014;146(6):1612–8. https://doi.org/10.1378/chest.13-2255.
Zosa BM, Golob JF, Conrad-Schnetz KJ, Schechtman D, Kreiner LA, Claridge JA. Current pneumonia surveillance methodology: similar underestimation in trauma and surgical patients in the intensive care unit. Surg Infect. 2017;18(5):558–62. https://doi.org/10.1089/sur.2016.152.
Leonard KL, Borst GM, Davies SW, Coogan M, Waibel BH, Poulin NR, et al. Ventilator-associated pneumonia in trauma patients: different criteria, different rates. Surg Infect. 2016;17(3):363–8. https://doi.org/10.1089/sur.2014.076.
Osei Sekyere J, Govinden U, Bester LA, Essack SY. Colistin and tigecycline resistance in carbapenemase-producing Gram-negative bacteria: emerging resistance mechanisms and detection methods. J Appl Microbiol. 2016;121(3):601–17. https://doi.org/10.1111/jam.13169.
Osei Sekyere J, Govinden U, Essack SY. Review of established and innovative detection methods for carbapenemase-producing Gram-negative bacteria. J Appl Microbiol. 2015;119(5):1219–33. https://doi.org/10.1111/jam.12918.
Jamal W, Al Roomi E, AbdulAziz LR, Rotimi VO. Evaluation of Curetis Unyvero, a multiplex PCR-based testing system, for rapid detection of bacteria and antibiotic resistance and impact of the assay on management of severe nosocomial pneumonia. J Clin Microbiol. 2014;52(7):2487–92. https://doi.org/10.1128/JCM.00325-14.
Hill JT, Tran KD, Barton KL, Labreche MJ, Sharp SE. Evaluation of the nanosphere Verigene BC-GN assay for direct identification of gram-negative bacilli and antibiotic resistance markers from positive blood cultures and potential impact for more-rapid antibiotic interventions. J Clin Microbiol. 2014;52(10):3805–7. https://doi.org/10.1128/JCM.01537-14.
Conway Morris A, Gadsby N, McKenna JP, Hellyer TP, Dark P, Singh S, et al. 16S pan-bacterial PCR can accurately identify patients with ventilator-associated pneumonia. Thorax. 2017;72(11):1046–8. https://doi.org/10.1136/thoraxjnl-2016-209065.
Clavel M, Barraud O, Moucadel V, Meynier F, Karam E, Ploy MC, et al. Molecular quantification of bacteria from respiratory samples in patients with suspected ventilator-associated pneumonia. Clin Microbiol Infect. 2016;22(9):812 e1- e7. https://doi.org/10.1016/j.cmi.2016.06.013.
Tijet N, Boyd D, Patel SN, Mulvey MR, Melano RG. Evaluation of the Carba NP test for rapid detection of carbapenemase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57(9):4578–80. https://doi.org/10.1128/AAC.00878-13.
Accelerate Pheno system. Accelerate Diagnostics. Tuscon, AZ. Available: http://acceleratediagnostics.com/products/accelerate-pheno-system/#stewardship. Accessed 11 July 2017.
Overview: T2Bacteria Panel. https://www.t2biosystems.com/t2sepsis-solution/t2bacteria-panel/overview-t2bacteria-panel.
Sader HS, Farrell DJ, Flamm RK, Jones RN. Antimicrobial susceptibility of Gram-negative organisms isolated from patients hospitalised with pneumonia in US and European hospitals: results from the SENTRY Antimicrobial Surveillance Program, 2009–2012. Int J Antimicrob Agents. 2014;43(4):328–34. https://doi.org/10.1016/j.ijantimicag.2014.01.007.
Weiner LM, Webb AK, Limbago B, Dudeck MA, Patel J, Kallen AJ, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(11):1288–301. https://doi.org/10.1017/ice.2016.174.
Sader HS, Castanheira M, Flamm RK. Antimicrobial activity of ceftazidime-avibactam against gram-negative bacteria isolated from patients hospitalized with pneumonia in U.S. Medical Centers, 2011 to 2015. Antimicrob Agents Chemother. 2017;61(4). https://doi.org/10.1128/AAC.02083-16.
Sader HS, Rhomberg PR, Farrell DJ, Jones RN. Arbekacin activity against contemporary clinical bacteria isolated from patients hospitalized with pneumonia. Antimicrob Agents Chemother. 2015;59(6):3263-70. https://doi.org/10.1128/AAC.04839-14.
Sader HS, Castanheira M, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Tigecycline activity tested against carbapenem-resistant Enterobacteriaceae from 18 European nations: results from the SENTRY surveillance program (2010–2013). Diagn Microbiol Infect Dis. 2015;83(2):183–6. https://doi.org/10.1016/j.diagmicrobio.2015.06.011.
Delle Rose D, Pezzotti P, Fortunato E, Sordillo P, Gini S, Boros S, et al. Clinical predictors and microbiology of ventilator-associated pneumonia in the intensive care unit: a retrospective analysis in six Italian hospitals. Eur J Clin Microbiol Infect Dis. 2016;35(9):1531–9. https://doi.org/10.1007/s10096-016-2694-9.
Bruyere R, Vigneron C, Bador J, Aho S, Toitot A, Quenot JP, et al. Significance of prior digestive colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae in patients with ventilator-associated pneumonia. Crit Care Med. 2016;44(4):699–706. https://doi.org/10.1097/CCM.0000000000001471.
Choi JY, Kwak YG, Yoo H, Lee SO, Kim HB, Han SH, et al. Trends in the distribution and antimicrobial susceptibility of causative pathogens of device-associated infection in Korean intensive care units from 2006 to 2013: results from the Korean Nosocomial Infections Surveillance System (KONIS). J Hosp Infect. 2016;92(4):363–71. https://doi.org/10.1016/j.jhin.2015.12.012.
Chen Y, Zhao JY, Shan X, Han XL, Tian SG, Chen FY, et al. A point-prevalence survey of healthcare-associated infection in fifty-two Chinese hospitals. J Hosp Infect. 2017;95(1):105–11. https://doi.org/10.1016/j.jhin.2016.08.010.
Fihman V, Messika J, Hajage D, Tournier V, Gaudry S, Magdoud F, et al. Five-year trends for ventilator-associated pneumonia: correlation between microbiological findings and antimicrobial drug consumption. Int J Antimicrob Agents. 2015;46(5):518–25. https://doi.org/10.1016/j.ijantimicag.2015.07.010.
Compain F, Arthur M. Impaired inhibition by avibactam and resistance to the Ceftazidime-Avibactam combination due to the D179Y substitution in the KPC-2 beta-lactamase. Antimicrob Agents Chemother. 2017;61(7). https://doi.org/10.1128/AAC.00451-17.
Tygacil [package insert]. Wyeth Pharmaceuticals Inc. Philadelphia, PA. Available: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021821s021lbl.pdf. Accessed July 2010.
Mediavilla JR, Patrawalla A, Chen L, Chavda KD, Mathema B, Vinnard C, et al. Colistin- and carbapenem-resistant escherichia coli harboring mcr-1 and blaNDM-5, causing a complicated urinary tract infection in a patient from the United States. MBio. 2016;7(4). https://doi.org/10.1128/mBio.01191-16.
Prim N, Rivera A, Rodriguez-Navarro J, Espano lM, Turbau M, Coll P, et al. Detection of mcr-1 colistin resistance gene in polyclonal Escherichia coli isolates in Barcelona, Spain, 2012 to 2015. Euro Surveill. 2016;21(13). https://doi.org/10.2807/1560-7917.ES.2016.21.13.30183.
Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–8. https://doi.org/10.1016/S1473-3099(15)00424-7.
Silver LL. Fosfomycin: mechanism and resistance. Cold Spring Harb Perspect Med. 2017;7(2). https://doi.org/10.1101/cshperspect.a025262.
Kahan FM, Kahan JS, Cassidy PJ, Kropp H. The mechanism of action of fosfomycin (phosphonomycin). Ann N Y Acad Sci. 1974;235(0):364–86.
Vardakas KZ, Legakis NJ, Triarides N, Falagas ME. Susceptibility of contemporary isolates to fosfomycin: a systematic review of the literature. Int J Antimicrob Agents. 2016;47(4):269–85. https://doi.org/10.1016/j.ijantimicag.2016.02.001.
Falagas ME, Kastoris AC, Karageorgopoulos DE, Rafailidis PI. Fosfomycin for the treatment of infections caused by multidrug-resistant non-fermenting Gram-negative bacilli: a systematic review of microbiological, animal and clinical studies. Int J Antimicrob Agents. 2009;34(2):111–20. https://doi.org/10.1016/j.ijantimicag.2009.03.009.
Grabein B, Graninger W, Rodriguez Bano J, Dinh A, Liesenfeld DB. Intravenous fosfomycin-back to the future. Systematic review and meta-analysis of the clinical literature. Clin Microbiol Infect. 2017;23(6):363–72. https://doi.org/10.1016/j.cmi.2016.12.005.
Kofteridis DP, Alexopoulou C, Valachis A, Maraki S, Dimopoulou D, Georgopoulos D, et al. Aerosolized plus intravenous colistin versus intravenous colistin alone for the treatment of ventilator-associated pneumonia: a matched case-control study. Clin Infect Dis. 2010;51(11):1238–44. https://doi.org/10.1086/657242.
Hirsch EB, Tam VH. Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection. J Antimicrob Chemother. 2010;65(6):1119–25. https://doi.org/10.1093/jac/dkq108.
Redin GS. Antibacterial activity in mice of minocycline, a new tetracycline. Antimicrob Agents Chemother (Bethesda). 1966;6:371–6.
Ritchie DJ, Garavaglia-Wilson A. A review of intravenous minocycline for treatment of multidrug-resistant Acinetobacter infections. Clin Infect Dis. 2014;59(Suppl 6):S374–80. https://doi.org/10.1093/cid/ciu613.
Castanheira M, Mendes RE, Jones RN. Update on Acinetobacter species: mechanisms of antimicrobial resistance and contemporary in vitro activity of minocycline and other treatment options. Clin Infect Dis. 2014;59(Suppl 6):S367–73. https://doi.org/10.1093/cid/ciu706.
MINOCIN. Minocycline for Injection [package insert]. The Medicines Company. Parsippany, NJ. Last updated: April 2015.
Zhou J, Ledesma KR, Chang KT, Abodakpi H, Gao S, Tam VH. Pharmacokinetics and pharmacodynamics of minocycline against Acinetobacter baumannii in a neutropenic murine pneumonia model. Antimicrob Agents Chemother. 2017;61(5). https://doi.org/10.1128/AAC.02371-16.
Freire AT, Melnyk V, Kim MJ, Datsenko O, Dzyublik O, Glumcher F, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68(2):140–51. https://doi.org/10.1016/j.diagmicrobio.2010.05.012.
FDA Drug Safety Communication: FDA warns of increased risk of death with IV antibacterial Tygacil (tigecycline) and approves new Boxed Warning. https://www.fda.gov/Drugs/DrugSafety/ucm369580.htm.
Prasad P, Sun J, Danner RL, Natanson C. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012;54(12):1699–709. https://doi.org/10.1093/cid/cis270.
Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2017;8(4):403–16. https://doi.org/10.1080/21505594.2016.1207834.
Chastre J, Wunderink R, Prokocimer P, Lee M, Kaniga K, Friedland I. Efficacy and safety of intravenous infusion of doripenem versus imipenem in ventilator-associated pneumonia: a multicenter, randomized study. Crit Care Med. 2008;36(4):1089–96. https://doi.org/10.1097/CCM.0b013e3181691b99.
Sahm D. In vitro activity of doripenem. Clin Infect Dis. 2009;49(Suppl. 1):S11–S6. https://doi.org/10.1086/599811.
Kollef MH, Chastre J, Clavel M, Restrepo MI, Michiels B, Kaniga K, et al. A randomized trial of 7-day doripenem versus 10-day imipenem-cilastatin for ventilator-associated pneumonia. Crit Care. 2012;16(6):R218. https://doi.org/10.1186/cc11862.
van Duin D, Bonomo RA. Ceftazidime/avibactam and ceftolozane/tazobactam: second-generation beta-lactam/beta-lactamase inhibitor combinations. Clin Infect Dis. 2016;63(2):234–41. https://doi.org/10.1093/cid/ciw243.
A Study Comparing Ceftazidime-Avibactam Versus Meropenem in Hospitalized Adults With Nosocomial Pneumonia. https://clinicaltrials.gov/ct2/show/NCT01808092. Accessed 26 Sept 2017.
Torres A, Rank D, Rekeda L, Chen X, Riccobene T, Critchley I, et al. Abstract 1864. Phase 3, randomized, double-blind noninferiority (NI) study of ceftazidime-avibactam (CAZ-AVI) versus meropenem (MER) in the treatment of patients with hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP): analyses of the REPROVE study per US FDA Endpoints. IDWeek 2017; San Diego, CA 2017.
Nelson K, Hemarajata P, Sun D, Rubio-Aparicio D, Tsivkovski R, Yang S, et al. Resistance to ceftazidime-avibactam is due to transposition of KPC in a porin-deficient strain of Klebsiella pneumoniae with increased efflux activity. Antimicrob Agents Chemother. 2017;61(10). https://doi.org/10.1128/AAC.00989-17.
Both A, Buttner H, Huang J, Perbandt M, Belmar Campos C, Christner M, et al. Emergence of ceftazidime/avibactam non-susceptibility in an MDR Klebsiella pneumoniae isolate. J Antimicrob Chemother. 2017;72(9):2483–8. https://doi.org/10.1093/jac/dkx179.
Shields RK, Potoski BA, Haidar G, Hao B, Doi Y, Chen L, et al. Clinical outcomes, drug toxicity, and emergence of Ceftazidime-Avibactam resistance among patients treated for carbapenem-resistant enterobacteriaceae infections. Clin Infect Dis. 2016;63(12):1615–8. https://doi.org/10.1093/cid/ciw636.
Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, et al. Emergence of ceftazidime-avibactam resistance due to plasmid-borne blakpc-3 mutations during treatment of carbapenem-resistant Klebsiella pneumoniae infections. Antimicrob Agents Chemother. 2017;61(3). https://doi.org/10.1128/AAC.02097-16.
Murano K, Yamanaka T, Toda A, Ohki H, Okuda S, Kawabata K, et al. Structural requirements for the stability of novel cephalosporins to AmpC beta-lactamase based on 3D-structure. Bioorg Med Chem. 2008;16(5):2261–75. https://doi.org/10.1016/j.bmc.2007.11.074.
Shortridge D, Pfaller MA, Castanheira M, Flamm RK. Antimicrobial activity of ceftolozane-tazobactam tested against Enterobacteriaceae and Pseudomonas aeruginosa with various resistance patterns isolated in U.S. hospitals (2013–2016) as part of the surveillance program: program to assess ceftolozane-tazobactam susceptibility. Microb Drug Resist. 2017; https://doi.org/10.1089/mdr.2017.0266.
Popejoy MW, Paterson DL, Cloutier D, Huntington JA, Miller B, Bliss CA, et al. Efficacy of ceftolozane/tazobactam against urinary tract and intra-abdominal infections caused by ESBL-producing Escherichia coli and Klebsiella pneumoniae: a pooled analysis of phase 3 clinical trials. J Antimicrob Chemother. 2017;72(1):268–72. https://doi.org/10.1093/jac/dkw374.
Chandorkar G, Huntington JA, Gotfried MH, Rodvold KA, Umeh O. Intrapulmonary penetration of ceftolozane/tazobactam and piperacillin/tazobactam in healthy adult subjects. J Antimicrob Chemother. 2012;67(10):2463–9. https://doi.org/10.1093/jac/dks246.
• Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic-derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2016;56(1):56–66. https://doi.org/10.1002/jcph.566. Article discusses the use of Ceftolozane/tazobactam dose justification in phase 3 studies.
Lomovskaya O, Sun D, Rubio-Aparicio D, Nelson K, Tsivkovski R, Griffith DC, Dudley MN. Vaborbactam: spectrum of Beta-Lactamase inhibition and impact of resistance mechanisms on activity in enterobacteriaceae. Antimicrob Agents Chemother. 2017;61(11). https://doi.org/10.1128/AAC.01443-17.
The Medicines Company announces TANGO-2 trial of meropenem-vaborbactam (formerly, Carbavance) stopped early for superior benefit-risk compared to best available therapy for CRE. http://www.themedicinescompany.com/investors/news/medicines-company-announces-tango-2-trial-meropenem-vaborbactam-formerly-carbavance.
Wenzler E, Gotfried MH, Loutit JS, Durso S, Griffith DC, Dudley MN, et al. Meropenem-RPX7009 concentrations in plasma, epithelial lining fluid, and alveolar macrophages of healthy adult subjects. Antimicrob Agents Chemother. 2015;59(12):7232–9. https://doi.org/10.1128/AAC.01713-15.
Lodise TP, Sorgel F, Melnick D, Mason B, Kinzig M, Drusano GL. Penetration of meropenem into epithelial lining fluid of patients with ventilator-associated pneumonia. Antimicrob Agents Chemother. 2011;55(4):1606–10. https://doi.org/10.1128/AAC.01330-10.
Awad SS, Rodriguez AH, Chuang YC, Marjanek Z, Pareigis AJ, Reis G, et al. A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin Infect Dis. 2014;59(1):51–61. https://doi.org/10.1093/cid/ciu219.
Drawz SM, Papp-Wallace KM, Bonomo RA. New beta-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob Agents Chemother. 2014;58(4):1835–46. https://doi.org/10.1128/AAC.00826-13.
Livermore DM, Warner M, Mushtaq S. Activity of MK-7655 combined with imipenem against Enterobacteriaceae and Pseudomonas aeruginosa. J Antimicrob Chemother. 2013;68(10):2286–90. https://doi.org/10.1093/jac/dkt178.
Falagas ME, Mavroudis AD, Vardakas KZ. The antibiotic pipeline for multi-drug resistant gram negative bacteria: what can we expect? Expert Rev Anti-Infect Ther. 2016;14(8):747–63. https://doi.org/10.1080/14787210.2016.1204911.
Merck Sharp & Dohme Corp. Efficacy and safety of imipenem+cilastatin/relebactam (MK-7655A) versus colistimethate sodium + imipenem+cilastatin in imipenem resistant bacterial infection (MK-7655A-013) (RESTORE-IMI 1). https://clinicaltrials.gov/ct2/show/NCT02452047.
Merck Sharp & Dohme Corp. Imipenem/relebactam/cilastatin versus piperacillin/tazobactam for treatment of participants with bacterial pneumonia (MK-7655A-014) (RESTORE-IMI 2). https://clinicaltrials.gov/ct2/show/NCT02493764.
Aggen JB, Armstrong ES, Goldblum AA, Dozzo P, Linsell MS, Gliedt MJ, et al. Synthesis and spectrum of the neoglycoside ACHN-490. Antimicrob Agents Chemother. 2010;54(11):4636–42. https://doi.org/10.1128/AAC.00572-10.
Zhanel GG, Lawson CD, Zelenitsky S, Findlay B, Schweizer F, Adam H, et al. Comparison of the next-generation aminoglycoside plazomicin to gentamicin, tobramycin and amikacin. Expert Rev Anti-Infect Ther. 2012;10(4):459–73. https://doi.org/10.1586/eri.12.25.
Landman D, Kelly P, Backer M, Babu E, Shah N, Bratu S, et al. Antimicrobial activity of a novel aminoglycoside, ACHN-490, against Acinetobacter baumannii and Pseudomonas aeruginosa from New York City. J Antimicrob Chemother. 2011;66(2):332–4. https://doi.org/10.1093/jac/dkq459.
Connolly LE, Jubb AM, O’Keeffe B, Serio AW, Smith A, Gall J, et al. Plazomicin is associated with improved survival and safety compared to colistin in serious carbapenem-resistant Enterobacteriaceae (CRE) infections: results of the CARE study. Annual Meeting of the American Society for Microbiology; New Orleans, LA 2017.
Karaiskos I, Giamarellou H. Multidrug-resistant and extensively drug-resistant gram-negative pathogens: current and emerging therapeutic approaches. Expert Opin Pharmacother. 2014;15(10):1351–70. https://doi.org/10.1517/14656566.2014.914172.
McKinnell JA, Connolly LE, Pushkin R, Jubb AM, O'Keeffe B, Serio AW, et al.1853. Improved outcomes with plazomicin (PLZ) compared with colistin (CST) in patients with bloodstream infections (BSI) caused by carbapenem-resistant enterobacteriaceae (CRE): results from the CARE Study. IDweek 2017; San Diego, CA. 2017.
Zhanel GG, Cheung D, Adam H, Zelenitsky S, Golden A, Schweizer F, et al. Review of eravacycline, a novel fluorocycline antibacterial agent. Drugs. 2016;76(5):567–88. https://doi.org/10.1007/s40265-016-0545-8.
Abdallah M, Olafisoye O, Cortes C, Urban C, Landman D, Quale J. Activity of eravacycline against Enterobacteriaceae and Acinetobacter baumannii, including multidrug-resistant isolates, from New York City. Antimicrob Agents Chemother. 2015;59(3):1802–5. https://doi.org/10.1128/AAC.04809-14.
Sutcliffe JA, O'Brien W, Fyfe C, Grossman TH. Antibacterial activity of eravacycline (TP-434), a novel fluorocycline, against hospital and community pathogens. Antimicrob Agents Chemother. 2013;57(11):5548–58. https://doi.org/10.1128/AAC.01288-13.
Solomkin J, Evans D, Slepavicius A, Lee P, Marsh A, Tsai L, et al. Assessing the efficacy and safety of eravacycline vs ertapenem in complicated intra-abdominal infections in the investigating gram-negative infections treated with eravacycline (IGNITE 1) trial: a randomized clinical trial. JAMA Surg. 2017;152(3):224–32. https://doi.org/10.1001/jamasurg.2016.4237.
Tetraphase announces positive top-line results from phase 3 IGNITE4 clinical trial in complicated intra-abdominal infections. 2017. http://www.globenewswire.com/news-release/2017/07/25/1058079/0/en/Tetraphase-Announces-Positive-Top-Line-Results-from-Phase-3-IGNITE4-Clinical-Trial-in-Complicated-Intra-Abdominal-Infections.html.
Tsai L. Intravenous eravacycline with transition to oral therapy for treatment of complicated urinary tract infections (cUTI) including pyelonephritis: results from a randomized, double-blind, multicenter, phase 3 trial (IGNITE2). American Society for Microbiology Microbe Meeting; 2016; Boston, MA.
Sole-Lleonart C, Rouby JJ, Blot S, Poulakou G, Chastre J, Palmer LB, et al. Nebulization of antiinfective agents in invasively mechanically ventilated adults: a systematic review and meta-analysis. Anesthesiology. 2017;126(5):890–908. https://doi.org/10.1097/ALN.0000000000001570.
Palmer LB. Inhaled antibiotics for ventilator-associated infections. Infect Dis Clin N Am. 2017;31(3):577–91. https://doi.org/10.1016/j.idc.2017.05.006.
Giamarellos-Bourboulis EJ, Pechere JC, Routsi C, Plachouras D, Kollias S, Raftogiannis M, et al. Effect of clarithromycin in patients with sepsis and ventilator-associated pneumonia. Clin Infect Dis. 2008;46(8):1157–64. https://doi.org/10.1086/529439.
Tsaganos T, Raftogiannis M, Pratikaki M, Christodoulou S, Kotanidou A, Papadomichelakis E, et al. Clarithromycin leads to long-term survival and cost benefit in ventilator-associated pneumonia and sepsis. Antimicrob Agents Chemother. 2016;60(6):3640–6. https://doi.org/10.1128/AAC.02974-15.
Lorente L, Jimenez A, Martin MM, Iribarren JL, Jimenez JJ, Mora ML. Clinical cure of ventilator-associated pneumonia treated with piperacillin/tazobactam administered by continuous or intermittent infusion. Int J Antimicrob Agents. 2009;33(5):464–8. https://doi.org/10.1016/j.ijantimicag.2008.10.025.
Bao H, Lv Y, Wang D, Xue J, Yan Z. Clinical outcomes of extended versus intermittent administration of piperacillin/tazobactam for the treatment of hospital-acquired pneumonia: a randomized controlled trial. Eur J Clin Microbiol Infect Dis. 2017;36(3):459–66. https://doi.org/10.1007/s10096-016-2819-1.
Fahimi F, Ghafari S, Jamaati H, Baniasadi S, Tabarsi P, Najafi A, et al. Continuous versus intermittent administration of piperacillin-tazobactam in intensive care unit patients with ventilator-associated pneumonia. Indian J Crit Care Med. 2012;16(3):141–7. https://doi.org/10.4103/0972-5229.102083.
Lorente L, Jimenez A, Palmero S, Jimenez JJ, Iribarren JL, Santana M, et al. Comparison of clinical cure rates in adults with ventilator-associated pneumonia treated with intravenous ceftazidime administered by continuous or intermittent infusion: a retrospective, nonrandomized, open-label, historical chart review. Clin Ther. 2007;29(11):2433–9. https://doi.org/10.1016/j.clinthera.2007.11.003.
Lorente L, Lorenzo L, Martin MM, Jimenez A, Mora ML. Meropenem by continuous versus intermittent infusion in ventilator-associated pneumonia due to gram-negative bacilli. Ann Pharmacother. 2006;40(2):219–23. https://doi.org/10.1345/aph.1G467.
Dulhunty JM, Roberts JA, Davis JS, Webb SA, Bellomo R, Gomersall C, et al. Continuous infusion of beta-lactam antibiotics in severe sepsis: a multicenter double-blind, randomized controlled trial. Clin Infect Dis. 2013;56(2):236–44. https://doi.org/10.1093/cid/cis856.
Dulhunty JM, Roberts JA, Davis JS, Webb SA, Bellomo R, Gomersall C, et al. A multicenter randomized trial of continuous versus intermittent beta-lactam infusion in severe sepsis. Am J Respir Crit Care Med. 2015;192(11):1298–305. https://doi.org/10.1164/rccm.201505-0857OC.
Abdul-Aziz MH, Sulaiman H, Mat-Nor MB, Rai V, Wong KK, Hasan MS, et al. Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016;42(10):1535–45. https://doi.org/10.1007/s00134-015-4188-0.
•• Roberts JA, Abdul-Aziz MH, Davis JS, Dulhunty JM, Cotta MO, Myburgh J, et al. Continuous versus intermittent beta-lactam infusion in severe sepsis. A meta-analysis of individual patient data from randomized trials. Am J Respir Crit Care Med. 2016;194(6):681–91. https://doi.org/10.1164/rccm.201601-0024OC. Article discusses intermittent and continuous infusion dosing of β-lactam antibiotics in critically ill patients with severe sepsis, showing that continuous infusion dosing was associated with decreased hospital mortality.
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000;162(2 Pt 1):505–11. https://doi.org/10.1164/ajrccm.162.2.9909095.
• Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290(19):2588–98. https://doi.org/10.1001/jama.290.19.2588. Article compares 8 vs 15 days of antibiotic therapy within critically ill patients.
Medina JC, Perez Protto SE, Pacie lD, Pontet J, Saldun P, Berro M. Antibiotic treatment for the ventilator-associated pneumonia: 8 vs. 12 days randomized trial preliminary data. Annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); Chicago, IL 2007.
Fekih Hassen M, Ayed S, Ben Sik Ali H, Gharbi R, Marghli S, Elatrous S. Duration of antibiotic therapy for ventilator-associated pneumonia: comparison of 7 and 10 days. A pilot study. Ann Fr Anesth Reanim. 2009;28(1):16–23. https://doi.org/10.1016/j.annfar.2008.10.021.
Capellier G, Mockly H, Charpentier C, Annane D, Blasco G, Desmettre T, et al. Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PLoS One. 2012;7(8):e41290. https://doi.org/10.1371/journal.pone.0041290.
Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev. 2015;8:CD007577. https://doi.org/10.1002/14651858.CD007577.pub3.
Bougle A, Foucrier A, Dupont H, Montravers P, Ouattara A, Kalfon P, et al. Impact of the duration of antibiotics on clinical events in patients with Pseudomonas aeruginosa ventilator-associated pneumonia: study protocol for a randomized controlled study. Trials. 2017;18(1):37. https://doi.org/10.1186/s13063-017-1780-3.
Ito A, Kohira N, Bouchillon SK, West J, Rittenhouse S, Sader HS et al. In vitro antimicrobial activity of S-649266, a catechol-substituted siderophore cephalosporin, when tested against non-fermenting Gram-negative bacteria. J Antimicrob Chemother. 2016;71(3):670-7. https://doi.org/10.1093/jac/dkv402.
Dobias J, Denervaud-Tendon V, Poirel L, Nordmann P. Activity of the novel siderophore cephalosporin cefiderocol against multidrug-resistant Gram-negative pathogens. Eur J Clin Microbiol Infect Dis. 2017;36(12):2319–27. https://doi.org/10.1007/s10096-017-3063-z.
Eastes T. Diphtheria cured by antitoxin. Br Med J. 1894;2(1751):125. https://doi.org/10.1136/bmj.2.1751.125.
Marshall NC, Finlay BB. Targeting the type III secretion system to treat bacterial infections. Expert Opin Ther Targets. 2014;18(2):137–52. https://doi.org/10.1517/14728222.2014.855199.
DiGiandomenico A, Keller AE, Gao C, Rainey GJ, Warrener P, Camara MM, et al. A multifunctional bispecific antibody protects against Pseudomonas aeruginosa. Sci Transl Med. 2014;6(262):262ra155. https://doi.org/10.1126/scitranslmed.3009655.
Rampioni G, Leoni L, Williams P. The art of antibacterial warfare: deception through interference with quorum sensing-mediated communication. Bioorg Chem. 2014;55:60–8. https://doi.org/10.1016/j.bioorg.2014.04.005.
Hentzer M, Wu H, Andersen JB, Riedel K, Rasmussen TB, Bagge N, et al. Attenuation of Pseudomonas aeruginosa virulence by quorum sensing inhibitors. EMBO J. 2003;22(15):3803–15. https://doi.org/10.1093/emboj/cdg366.
Starkey M, Lepine F, Maura D, Bandyopadhaya A, Lesic B, He J, et al. Identification of anti-virulence compounds that disrupt quorum-sensing regulated acute and persistent pathogenicity. PLoS Pathog. 2014;10(8):e1004321. https://doi.org/10.1371/journal.ppat.1004321.
Kester JC, Fortune SM. Persisters and beyond: mechanisms of phenotypic drug resistance and drug tolerance in bacteria. Crit Rev Biochem Mol Biol. 2014;49(2):91–101. https://doi.org/10.3109/10409238.2013.869543.
Ribeiro SM, Felicio MR, Boas EV, Goncalves S, Costa FF, Samy RP, et al. New frontiers for anti-biofilm drug development. Pharmacol Ther. 2016;160:133–44. https://doi.org/10.1016/j.pharmthera.2016.02.006.
Kollef MH, Afessa B, Anzueto A, Veremakis C, Kerr KM, Margolis BD, et al. Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA. 2008;300(7):805–13. https://doi.org/10.1001/jama.300.7.805.
Pires DP, Vilas Boas D, Sillankorva S, Azeredo J. Phage therapy: a step forward in the treatment of Pseudomonas aeruginosa infections. J Virol. 2015;89(15):7449–56. https://doi.org/10.1128/JVI.00385-15.
Wright A, Hawkins CH, Anggard EE, Harper DR. A controlled clinical trial of a therapeutic bacteriophage preparation in chronic otitis due to antibiotic-resistant Pseudomonas aeruginosa; a preliminary report of efficacy. Clin Otolaryngol. 2009;34(4):349–57. https://doi.org/10.1111/j.1749-4486.2009.01973.x.
Schooley RT, Biswas B, Gill JJ, Hernandez-Morales A, Lancaster J, Lessor L, et al. Development and use of personalized bacteriophage-based therapeutic cocktails to treat a patient with a disseminated resistant Acinetobacter baumannii infection. Antimicrob Agents Chemother. 2017;61(10). https://doi.org/10.1128/AAC.00954-17.
Duplessis C, Biswas B, Hanisch B, Perkins M, Henry M, Quinones J, et al. Refractory Pseudomonas bacteremia in a 2-year-old sterilized by bacteriophage therapy. J Pediatric Infect Dis Soc. 2017; https://doi.org/10.1093/jpids/pix056.
Kaufmann SHE, Dorhoi A, Hotchkiss RS, Bartenschlager R. Host-directed therapies for bacterial and viral infections. Nat Rev Drug Discov. 2017;17(1):35–56. https://doi.org/10.1038/nrd.2017.162.
Karacaer F, Hamed I, Ozogul F, Glew RH, Ozcengiz D. The function of probiotics on the treatment of ventilator-associated pneumonia (VAP): facts and gaps. J Med Microbiol. 2017;66(9):1275–85. https://doi.org/10.1099/jmm.0.000579.
Taylor E, Webster TJ. Reducing infections through nanotechnology and nanoparticles. Int J Nanomedicine. 2011;6:1463–73. https://doi.org/10.2147/IJN.S22021.
Gerstmans H, Rodriguez-Rubio L, Lavigne R, Briers Y. From endolysins to Artilysin®s: novel enzyme-based approaches to kill drug-resistant bacteria. Biochem Soc Trans. 2016;44(1):123–8. https://doi.org/10.1042/BST20150192.
Brown CL, Smith K, McCaughey L, Walker D. Colicin-like bacteriocins as novel therapeutic agents for the treatment of chronic biofilm-mediated infection. Biochem Soc Trans. 2012;40(6):1549–52. https://doi.org/10.1042/BST20120241.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
NJR: discloses reciept of travel expenses and honoria from American Society of Healthsystem Pharmacists
CC: no relevant disclosures
JNO: no relevant disclosures
RGW: discloses reciept of payment for continuing medical education from Medscape and consulting fees from Meiji-Seiko, Merck, Nabriva, Polyphor, Roche/Genetech, Shionogi, The Medicines Company, Accelerate Diagnostics, Curetis, and bioMerieux
ARH: discloses board membership with Microbiotix, NIH grant funding, travel funds and expenses from Cystic Fibrosis Foundation and American Society of Microbiology, and consulting fees from MedImmune
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Antimicrobial Development and Drug Resistance
Rights and permissions
About this article
Cite this article
Rhodes, N.J., Cruce, C.E., O’Donnell, J.N. et al. Resistance Trends and Treatment Options in Gram-Negative Ventilator-Associated Pneumonia. Curr Infect Dis Rep 20, 3 (2018). https://doi.org/10.1007/s11908-018-0609-x
Published:
DOI: https://doi.org/10.1007/s11908-018-0609-x