Abstract
Introduction
Heart failure (HF) is a complex clinical syndrome with diverse risk factors and etiologies, differing underlying pathophysiology, and large phenotypic heterogeneity.
Recent Findings
Advances in imaging techniques coupled with clinical trials that targeted only in those with impaired left ventricular ejection fraction (LVEF) have largely shaped the current management strategy for HF that focuses predominantly in patients with systolic HF. In contrast, there are no effective treatments for HF with preserved ejection fraction (HFpEF). Instead of this “one-size-fits-all” approach to treatment, better precision to define HF phenotypic classifications may lead to more efficient and effective HF disease management.
Conclusion
Integrating variables—including clinical variables, HF biomarkers, imaging, genotypes, metabolomics, and proteomics—can identify different pathophysiologies, lead to more precise phenotypic classification, and warrant investigation in future clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
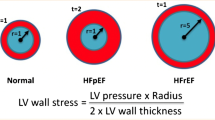
The prevalence of heart failure (HF) continues to increase and has been associated with high mortality, recurrent hospitalization, and high economic burden [1, 2]. Despite advances in medical treatment, device therapies, and transplantation, the residual risks of HF remain unacceptably high [1, 2]. Most successful randomized controlled trials in the HF population have been conducted based on left ventricular ejection fraction (LVEF) cutoff points to confirm the presence of HF with reduced ejection fraction (HFrEF) [3, 4]. In fact, there have not been any proven therapies for HF with preserved ejection fraction (HFpEF) [2].
The syndrome of HF is incompletely understood. The 2013 ACCF/AHA guideline for the management of HF defined HF as “a complex clinical syndrome that results from any structural or functional impairment of ventricular filing pressure or ejection of blood” [2]. Clearly summarized from this document is the notion that diagnostic tools and treatment approaches for HF often lack precision, which has limited our advances in both mechanistic understanding and treatment approaches. Results of most clinical trials have been reported as an average treatment effect based on the entire population rather than the specific reduced LVEF population studied. The results of different risk factors and multiple etiologies, in combination with genetic and environmental factors, lead to different clinical presentations and diverse underlying pathophysiologies that are too complex to simply use LVEF cutoff points to define HFpEF or HFrEF. One risk factor, like reduced LVEF, is insufficient to identify a specific phenotype or underlying pathophysiology in a given patient [2, 5].
Successes in the field of oncology identified specific cancer phenotypes (e.g., type of cancer, gene expression of tumor cells, and histologic subtype from tissue biopsy) allowing the disease mechanisms to be reasonably well understood, therapeutic targets to be identified, and targeted treatments to be developed, for example, HER2-targeted therapy in HER2-positive breast cancer. In the field of HF, the role of targeted therapy remains unclear [6]. Therefore, well-defined HF phenotypes are needed to identify specific therapeutic targets and to better understand each patient’s underlying biology and pathophysiology instead of the “one-size-fits-all” approach. This review will provide the current and future clinical potential of identifying unique clinical phenotypes (including biomarkers, imaging, genotype, metabolomics, and proteomics) that can ensure the application of precision medicine in HF.
Circulating Biomarkers
Over the last decade, over 6500 studies have been published in the field of HF biomarkers. Unfortunately, many of these reports had scantly described methods and studied heterogeneous HF phenotypes that have substantially limited our clinical translation [7]. Moreover, the majority of HF biomarker studies focused on prognosis prediction and confirmation of a HF diagnosis, a clinically defined entity with relatively subjective interpretation. Many of the studies utilized all-cause mortality as primary endpoint, which is relatively non-specific to the HF syndrome.
The use of biomarkers in HF research has provided a better understanding of the pathophysiology of the disease process, especially in animal models. Clinically however, only the presence of HFrEF provides the most robust biomarker in selecting patients with guideline-directed medical therapies. In contrast, the role of circulating biomarkers in tailoring individual therapy in the field of HF is lagging from other cardiovascular conditions. For example, cardiac troponin has been widely used to define acute coronary syndromes (ACS) and to gauge the benefit of invasive treatment in patients with ACS [8]. There is a need to identify candidate biomarkers that reflect a specific underlying pathophysiology and may have the potential to guide therapeutics. In this section, we will focus on the role of biomarkers in the following specific HF phenotypes: (1) myocardial stress, (2) myocardial injury, (3) myocardial fibrosis, and (4) cardio-renal dysfunction.
Biomarkers of Myocardial stress
The prototype HF biomarker is the natriuretic peptide (NP) family, specifically B-type natriuretic peptide (BNP) and its prohormone fragment, N-terminal pro-B-type natriuretic peptide (NT-proBNP). Discovered over 35 years ago and successfully integrated into clinical practice as HF biomarkers over the past 15 years, NPs are useful in diagnosing and risk stratification for patients with HF [2]. Several clinical trials have examined the hypothesis that NP-guided therapy, informed by serial measurements of NPs, supported clinical outcomes in patients with HF. However, use of this NP-guided therapeutic approach continues to be debated, since previous clinical trials showed inconsistent results [9,10,11,12,13,14,15] and were limited by significant heterogeneity in HF phenotypes, poorly defined treatment strategies prescribed to various NP concentrations targeted [16]. The prospective, multicenter, randomized controlled trial, guiding evidence-based therapy using biomarkers intensifies treatment in heart failure (GUIDE-IT, NCT01685840), is ongoing and might address these issues [17••]. Regardless, NPs will never be used alone and requires interpretation in the clinical context since other cardiopulmonary disorders and comorbidities are also associated with elevated BNP or NT-proBNP concentrations (e.g., ACS, arrhythmia, pulmonary hypertension, pulmonary embolism, renal disease, catabolic diseases, or advanced age). Therefore, there is ample room for novel HF biomarkers to identify specific phenotypes, unique pathophysiologies, and potential therapeutic targets.
ST2 is another myocardial stress protein that exists in both soluble form (sST2) and membrane-bound receptor form (ST2L) and is closely associated with left ventricular (LV) strain [18], fibrosis, and remodeling [19]. ST2 gene expression is triggered in the setting of cardiomyocyte or cardiac fibroblast stretch [20], although the cardiac origin of ST2 has not been established. The binding of interleukin-33 (IL-33), the functional ligand of ST2, to ST2L has favorable antifibrotic, antiapoptotic, and antiremodeling effects [19, 21]. These cardioprotective effects are blocked by high levels of sST2 because sST2 also binds IL-33, making it unavailable to bind to the ST2 receptor form [19]. In chronic HF outpatients, sST2 has potent prognostic value, both independently and as an additive to NT-proBNP and clinical risk scores [22]. In a head-to-head comparison of ST2 with galectin-3 (Gal-3), ST2 was shown to be better than Gal-3 in risk stratification and prognosis in patients with chronic HF [23]. Meanwhile in HFpEF, sST2 was more accurate than NPs in identifying the severity of diastolic dysfunction [24]. Because of this predictive power, the role for using serial levels of sST2 to guide therapy has been suggested for both acute and chronic HF [25, 26]. Meanwhile, sST2 levels in chronic HF patients fell after treatment with higher-dose beta-blockers, and that elevated sST2 concentrations (>35 ng/mL) can identify patients who may particularly benefit from higher doses of beta-blockers [27]. However, in the Valsartan HF trial (Val-Heft), treatment with valsartan reduced the rate of increase in sST2 concentration compared with placebo, and they observed that an increase in sST2 was independently associated with patient outcomes [28]. In another study, treatment with a mineralocorticoid receptor antagonist (MRA) had a greater benefit among acute HF patients who had high sST2 concentrations [29]. There is even promise in the acute HF setting, in which sST2 levels (at a higher cutoff value) was an independent predictor of prognosis regardless of LVEF and was a stronger predictor of prognosis than NT-proBNP [30, 31]. Hence, the role of detecting activation of the IL-33/ST2 system merits further study for additional sources of targeted therapies.
Biomarkers of Myocardial Injury
The principle biomarkers of myocardial injury are two cardiac-specific troponins (cTn), cardiac troponin I, and cardiac troponin T (cTnI and cTnT, respectively). Cardiac troponins are widely used primarily for the diagnosis and management of ACS. Elevated cTn concentrations have also been shown to predict an adverse prognosis in both acute and chronic HF [2], but the mechanism controlling the release of cTn in HF remains unclear, and the release is generally considered to be secondary to myocardial injury (e.g., ischemia, necrosis, or apoptosis) [5]. The prevalence of elevated cTn in patients with HF was non-specific, with differences based on the sample population, clinical setting, and troponin assay used. For example, using a standard cTn assay, abnormally elevated cTn has been detected in about one-quarter of HF patients and was associated with a poorer prognosis [5]. While using a high-sensitivity assay (hs-cTn), abnormally elevated hs-cTn has been detected in virtually all patients with acute HF [32] and in a majority of patients of chronic HF [33]. Elevated cTn (using either a standard or high-sensitivity assay) is independently associated with an adverse prognosis in patients with HF. Importantly, acute HF may be precipitated by ACS; therefore, cTn measurements are recommended in all patients with acute HF to detect ACS and inform treatment [2]. However, specific therapies have not yet been identified to reduce the development or rise of cTn in HF patients, even though cTn can be more sensitive than standard imaging techniques to detect cardiotoxicity.
Biomarkers of Myocardial Fibrosis
Traditional research-based markers of myocardial fibrosis have been plagued with assay variability and lack of specificity. Galectin-3 (Gal-3) is a glycoprotein secreted by activated macrophages. Previous studies have shown that Gal-3 is associated with cell adhesion, inflammation, myocardial hypertrophy, fibroblast proliferation, and tissue fibrosis, all of which play an integral role in myocardial remodeling [33, 34]. Direct Gal-3 infusion results in myocardial fibrosis in HF [35], whereas genetic disruption and pharmacological inhibition of Gal-3 prevents myocardial fibrosis, remodeling, and subsequent HF development [36]. High Gal-3 levels (both systemic and myocardial) has been associated with cardiac remodeling and a poorer prognosis in patients with HF, with a stronger predictive value in HFpEF patients when compared with HFrEF patients [37,38,39]. Gal-3 was also associated with aldosterone-induced myocardial fibrosis in experimental models [40], but MRA treatment failed to show a benefit when studied in chronic HFrEF patients [41]. Currently, the ability for Gal-3 to risk stratifies HF patients’ rests on the diminishing propensity to recover with increasing levels. Specifically, patients with low plasma Gal-3 levels showed a benefit when treated with rosuvastatin [42] or valsartan [43] for HFrEF, while increasing galectin-3 was associated with worse outcome, independent of treatment, or NT-proBNP [38, 44]. Renal insufficiency is likely a major and often overlooked confounder for these observations, and it may still suffer from lack of specificity [45, 46].
Biomarkers of Cardio-Renal Dysfunction
Renal dysfunction (RD) is commonly associated with a poor prognosis in all phenotypes of HF [47]. Blood urea nitrogen (BUN) and creatinine levels are widely used as renal function markers, but they can vary non-specifically according to sex, age, race, illness, and muscle mass. Moreover, RD in HF patients with cardiorenal syndrome (CRS) is complex and multifactorial. Therefore, there is a need to identify candidate renal biomarkers for the early diagnosis, prognosis, and therapeutic target discovery in CRS.
Cystatin C (CysC) is a cysteine protease inhibitor that is ubiquitously produced at a constant rate, freely filtered, and neither secreted from nor reabsorbed into the bloodstream. CysC has been suggested as a newer more accurate way to calculate the estimated glomerular filtration rate (eGFR) than creatinine-based measures [48]. Moreover, an elevated CysC concentration was associated with poor prognosis in both acute and chronic HF [49]. Unfortunately, the ability of CysC to differentiate between specific mechanisms or phenotypes of CRS, or to serve as a therapeutic target in HF, has been less well established [49]. Furthermore, direct head-to-head comparison across various RD biomarkers in the acute HF setting suggested that BUN remained the strongest prognosticator [50].
Neutrophil gelatinase-associated lipocalin (NGAL) is a small protein found in neutrophil granules. Both urine and plasma NGAL levels are increased in response to tubular kidney injury and predict adverse prognosis in patients with HF, but the differences between urinary and plasma NGAL levels are what may help identify specific CRS phenotypes [49]. In acute decompensated heart failure (ADHF), the majority of patients demonstrated urine NGAL levels lower than acute kidney injury levels [51], while serum NGAL was strongly associated with eGFR and predicted RD development [52]. Clearly, serum and urine NGAL represents different physiologic aspects of renal dysfunction [53].
N-acetyl-β-d-glucosaminidase (NAG) is a lysosomal enzyme originating in proximal tubular cells and is indicative of proximal tubular damage when detected in the urine. Urine NAG predicted worsening renal function and mortality in patients with chronic HF [49, 54]. However, the ability to use NAG to identify a specific CRS phenotype has been limited since NAG is also increased in diabetes and hypertension [49].
Kidney injury molecule-1 (KIM-1) is a glycoprotein expressed in the proximal renal tubule in kidney injury but not expressed in the normal kidney. KIM-1 levels were inversely associated with LVEF and directly associated with worsening HF symptoms (defined by NYHA class) among chronic HF patients without RD [55, 56]. Furthermore, plasma KIM-1 is associated with poor prognosis and worsening renal function in the acute HF setting, yet its prognostic value diminished following covariate adjustments [57]. Further study may determine whether the changes of KIM-1 with treatment can mirror improved renal function and prognosis in patients with HF.
The candidate biomarkers discussed above may each, with further research, help classify specific patients into distinct subgroups of HF phenotypes. Then, as each of these subgroups may respond differently to treatment, the candidate biomarkers may also aid in the development of tailored therapies. Ahmad et al. recently described three commonly used biomarker study designs, each with their own advantages and disadvantages: biomarker-stratified, enrichment, and biomarker strategy [8]. Importantly, each method can be combined or altered according to the research question. For example, although Gal-3 and ST2 have been approved by the Food and Drug Administration to predict prognosis in HF, the appropriate role of these two biomarkers is still limited because of the small numbers of studies to date. So, a future study could use the enrichment design to test the hypothesis that, in HFpEF patients, Gal-3/ST2 could have a potential role in distinct patient subgroups that might benefit from a specific treatment (e.g., MRA/anti-Gal3).
Multimarker Biomarker Strategies
Recently, there has been an interest in “multiple biomarker strategies” since each biomarker reflects a different pathophysiologic pathway, and the application of a single biomarker is insufficient to evaluate patients with HF. Therefore, multiple biomarker strategies provide the opportunity to evaluate multiple pathophysiologic pathways in patients with HF, such as myocardial stretch, myocardial fibrosis, myocardial injury, and cardiorenal. Combining different biomarkers that reflect different pathophysiologic insights integrate various aspects of the disease and provide a specific HF phenotype. In a study of chronic HFrEF patients, Ky et al.[58] used multiple biomarker panels, consisting of biomarkers that represented different pathophysiology pathways, to generate a multimarker score and found it significantly improved prediction of adverse events and appropriate reclassification of patients. Community-based populations showed that a multimarker score consisting of ST2, hs-cTn, GDF-15, high-sensitivity C-reactive protein (hsCRP), and BNP provided incremental value in predicting onset of HF [59]. Recently, Sanders-van et al.[60], demonstrated that 15 biomarkers that reflect distinct pathophysiological pathways—such as NT-proBNP, hs-cTn, hemoglobin (a marker of hematopoiesis), ST2, hsCRP, and CysC—were expressed differently between HFrEF and HFpEF. These studies provide keys to the differing pathophysiological pathways in HFrEF and HFpEF. Therefore, biomarker data may help to identify subgroups of patients that respond to a specific drug and using multiple biomarkers to improve pathophysiological insight could lead to personalized HF therapy. Although these strategies are important to risk stratification, further studies are needed to determine the appropriate combinations of biomarkers that will allow for the classification of specific HF phenotypes as molecular “fingerprints” of the disease and the corresponding therapeutic implications.
Genotype
It has been increasingly recognized that subtypes of HF and cardiomyopathies may have a genetic basis, which is largely overlooked in the development of pharmacologic and device therapies for HF. The genetic contribution to cardiac structure and function is complex, which can lead to variable clinical phenotypes [61]. For example, hypertrophic cardiomyopathy (HCM), the most common inherited cardiomyopathy, is the result of one or more of 400+ disease-causing variants in 9 sarcomeric protein-encoding genes. Therefore, there is the potential for substantial phenotypic heterogeneity [61]. Recently, research strategies have focused on scanning the entire genome to search for “candidate genes” that are associated with specific diseases [5] or responses to specific HF therapeutics [62]. As HF is a complex syndrome, new sequencing techniques have the potential to identify patterns of genetic variants that may have an effect on HF development. While these findings can potentially yield mechanistic insights that can further guide therapeutic targets [63,64,65,66,67], discoveries in this area have yet to expand toward treatment decisions.
Micro-RNAs (miRNAs) are small endogenous non-coding RNAs that control gene expression by binding to targeted mRNAs. Recently, miRNAs have been detected in various body fluids, including the bloodstream, and may have potential as novel biomarkers. They have been associated with disordered cardiac structure and function and may have the potential to identify specific HF phenotypes and specific therapeutic targets [68]. Several studies have shown the potential of miRNAs as biomarkers in cardiovascular diseases. Cardiac-enriched miRNAs (e.g., miRNA-1, miRNA-208a/b, and miRNA-499) were significantly increased in plasma early after myocardial infarction (MI) or transcoronary ablation of septal hypertrophy [69], mimicking the kinetics of a conventional myocardial injury biomarker like cTnT. These miRNAs are likely released from damaged cardiac myocytes into the bloodstream [69, 70]. Tijsen et al. showed that circulating miR423-5p are useful biomarkers for distinguishing HF in dyspnea patients [71]. Moreover, specific miRNAs have the potential to differentiate between HFrEF and HFpEF [72]. Matsumoto et al. found that p53-responsive miRNAs predicted subsequent HF in post-MI patients [73]. The absence of miRNA-22 in genetically altered mice was associated with reduced activity of SERCA2 in their myocytes, LV dilatation, and an impaired response to cardiac overload, all of which enhanced propensity to HF development [74]. Conversely, genetic deletion of miRNA-208a prevents pathological cardiac remodeling [75]. Therefore, the specific treatment-induced changes in the activity of mRNAs could have potentially therapeutic targets in HF.
Metabolomics
Metabolomics is the systematic study of circulating metabolites in order to understand the cellular processes that lead to their production. It has the potential to provide insights into the underlying molecular mechanisms of cardiovascular disease in general, and HF specifically [76]. As discussed previously, traditional HF biomarkers, even BNP and NT-proBNP, did not provide additional therapeutic target possibilities. Therefore, determining specific groups of circulating metabolites, labeling them as metabolic profiles, and using those profiles as biomarkers may lead to better prognostication and tailored treatments in specific subgroups of patients. In fact, several human clinical studies of metabolomics in HF have identified unique circulating metabolic profiles that differ between patients with HF and healthy subjects, as well as between different HF stages and HF phenotypes [77]. Recently, Cheng et al.[78] identified a panel of metabolites, including histidine, phenylalanine, spermidine, and phosphatidylcholine C34:4, which differentiated stage C HF patients from healthy control subjects with a diagnostic value similar to that of BNP. The values of this panel were significantly improved at 6 and 12 months in those patients who recovered from acute HF. In addition, they found that a separate panel of metabolites, consisting of the dimethylarginine/arginine ratio, butyrylcarnitine, spermidine, and total essential amino acid amount, provided significant prognostic value in patients with stages B and C HF. The prognostic value of this second metabolite panel was actually greater than that of BNP in the stage B and C HF patients.
Another strategy is to utilize targeted metabolomics to identify novel pathways relevant to cardio-renal disease progression. For example, our group has identified an obligatory role for gut microbes in trimethylamine N-oxide (TMAO) generation measured by mass spectrometry. Elevated TMAO was associated with more advanced LV diastolic dysfunction and portended poor long-term prognosis in a large cohort of patients with a history of chronic HF independent of cardiorenal indices [79, 80]. To date, evidence supports that HF is associated with metabolic dysfunction [81], yet the clinical utility of metabolomics in HF remains unclear because of differences in study design and statistical methodology and a diverse array of molecular profiles reflecting the heterogeneity of HF phenotypes. Therefore, further studies of metabolomics in HF could have the clinical utility of characterizing unique metabolic phenotypes in HF leading to the identification of specific patient subgroups that may respond better to certain treatment strategies. In addition, the combination of metabolomics with other “omic” biomarkers may offer a robust phenotypic classification system in HF.
Proteomics
Proteomics is the study of the large-scale expression, function, and interaction of all proteins present in the cell [82]. Proteomics analyses have developed from basic protein separation by two-dimensional electrophoresis to mass spectrometry (MS)-based approaches [82]. Proteomics differs from genomics since proteomics has dynamic variability that can reveal the details of functioning within the cell, but genomics is relatively constant. Therefore, proteomic technologies offer potential tools for examining alterations in protein expression in cardiovascular disease and HF that may provide insights into underlying cellular mechanisms. In HF, the proteomics approach may help discover novel biomarkers for diagnosis, prevention, and the identification of specific therapeutic targets. Because of the diverse complexity and highly dynamic range of protein expression, current research in proteomics remains insufficient for a comprehensive understanding of the cellular mechanisms underlying HF and, therefore, the ability to target therapeutics in HF syndrome [83]. There is a clear need for technologic advancements and further well-designed studies robust in proteomic analyses to identify specific proteins unique to specific HF phenotypes.
Advances in Multidimensional Analytical Approaches
Phenotypic heterogeneity is a major problem in contemporary HF patient populations with both HFpEF and HFrEF [84, 85]. Contemporary clinical trials in HF focus on specific populations selected by inclusion/exclusion criteria that do not take into account the heterogeneity of HF phenotypes, which can lead to a mixed phenotypic population and unproductive results. The increasing use of “omics” studies may have the potential to identify unique molecular signatures and targeted treatment approaches and responses in HF. Therefore, the combination of omics biomarkers with other variables and the use of phenotype-based cluster analysis may allow for the characterization of more robust clinical phenotypes on the basis of underlying molecular biology. This will allow us to match more specific treatments with more specific patient subgroups, improving efficacy and cutting costs to patients and hospitals.
The advent of sophisticated phenotyping tools (e.g., cluster analysis) can improve phenotypic characterization in complex and heterogeneous syndromes such as HF. This analysis uses a combination of phenotypic variables to define subgroups based on differences (or similarities) in individually measured characteristics and clusters them, with strong associations between members of the same cluster and weak associations between members of different clusters. Cluster analysis using a big data-driven strategy has the potential to identify complex phenotypes and address the heterogeneity of the HF population. A recent study in HFrEF patients identified four patient clusters using a combination of 45 clinical variables including demographics, comorbidities, cardiac variables, cardiopulmonary exercise testing (CPET), and biomarkers. Each of these four clusters had differing prognoses as well as different responses to exercise training [85]. Similarly, a prospective study of 379 patients with HFpEF used 67 continuous phenotypic variables comprising demographics, and clinical, laboratory, electrocardiographic, and comprehensive echocardiographic findings identified 3 phenotypic classifications an unbiased phenotype mapping algorithm (“phenomapping”) [84].
Retrospective analysis of existing datasets from completed HF clinical trials that used phenotype-based cluster analysis may provide insights into the underlying pathophysiology of HF and address phenotypic heterogeneity issues [86]. Unlike the above mentioned cluster analysis that used continuous variables, studies looking at dichotomous variables from large HFpEF trials identified six subgroups that differed significantly in profiles of key characteristics and event-free survival. Interestingly, only those characterized by a high prevalence of obesity, hyperlipidemia, diabetes mellitus, anemia, and renal insufficiency, had a nominally improved outcome with irbesartan (hazard ratio 0.72, P = 0.046).
All three of the abovementioned studies used the machine learning algorithm to define clusters of patients based on phenotypic variables (phenotype-based cluster analysis), to classify a heterogeneous HF population into more homogeneous clusters. They were also able to identify subgroups that significantly differed in characteristics and prognoses (Table 1). However, there are several limitations in this approach, especially the fact that these three studies did not include omics, such as genomics biomarkers, as phenotypic variables in the cluster analysis. Since it is unclear whether patients stay within their assigned cluster over time, the clinical applicability of cluster analysis to identify subgroups that will be responsive to specific treatments remains unclear.
Future Outlook
Future advances in therapeutic management of HF will rely heavily on departing from the trajectory of drug and device development over the past four decades: (1) the need to discover (and visualize) novel therapeutic targets that are currently overlooked; (2) the need to improve precision in diagnostic and prognostic criteria to identify patients that may benefit from prioritizing specific therapeutic options, especially at early stages of the disease; and (3) to tackle heart failure before it develops.
Identify Novel and Specific Therapeutic Targets
Specific targeting of genetic or biomarker functions using specific inhibitors (e.g., direct Gal-3 inhibitors or anti-mRNAs) may be another useful approach to identify individual HF patients who may respond better to targeted treatment. This “proof-of-concept” should be incorporated into prospective studies, such as cluster-based or genotype-based RCTs, to identify individuals or specific subgroups of HF patients who may respond to targeted treatment. Like oncologic therapeutics, future clinical trials should account for the heterogeneity of HF when considering study design and should consider subgroup analysis to identify a specific HF phenotype that may respond to a particular treatment. It is important to recognize that few if any genetic polymorphisms have been clinically indicated to benefit from identifying targeted treatment. Nevertheless, this does not preclude the potential benefit of targeting specific genotypes for drug efficacy or to tailor drugs based on their pharmacokinetic profiling.
Improving Diagnostic Precision by Better Identify Phenotypic Variables
The underlying comorbidities and phenotypic heterogeneity in HFpEF are likely much greater than in HFrEF [2, 87], which may be a key reason for a lack of positive result in many large clinical trials. Improved phenotypic classification of the HF syndrome using a combination of variables, such as demographics, comorbidities, biomarkers, comprehensive imaging modalities, and omics approaches (genomics, proteomics, and metabolomics), is likely to aid in identifying more homogeneous HFpEF phenotype and the matching of appropriate targeted treatment. In fact, such analyses may also reveal that subsets of HFpEF may have absolutely no cardiac relevance at all.
Preventing Heart Failure by Targeting At-Risk Population
There have been major efforts to raise awareness among at-risk patients to prevent HF, including a reclassification of staging to denote a concept of disease progression with antecedent at-risk profiles [2]. Increasing attention has been focused on modifiable risk factors and the development of risk scores to help predict the incidence of HF and provide time to implement prevention strategies [2]. There is an unmet need to predict risk at an earlier time point, and HF risk has yet to be determined by genomic sequencing. There is also a major logistic and knowledge gaps in instituting more timely intervention of promising approaches. For example, the use of CMR (both T1 mapping and LGE) to identify intrinsic myocardial damage and arrhythmogenesis [88, 89]. There is also evidence to support that targeting rise in NP with therapeutic adjustments is associated with better outcomes and lower rates of detecting cardiac dysfunction over time [90].
Conclusions
There is an immediate need to refine the clinical use of current treatment options in order to significantly reduce iatrogenic adverse consequences (i.e., not to assume that current approaches are already optimal). In the future, the identification of robust phenotypic variables, in combination with advanced analytic approaches using computer algorithms, will likely assign HF patients to a unique cluster phenotype—a sort of “cluster fingerprint”—that may respond better to targeted treatment (Fig. 1). In the meantime, important building blocks for such precision medicine needed to be established, with a departure from the current conceptual framework.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–52.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004.
Swedberg K, Komajda M, Bohm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376(9744):875–85.
Braunwald E. Heart failure. JACC Heart Fail. 2013;1(1):1–20.
Shah SJ, Katz DH, Deo RC. Phenotypic spectrum of heart failure with preserved ejection fraction. Heart Fail Clin. 2014;10(3):407–18.
Januzzi Jr JL, Felker GM. Surfing the biomarker tsunami at JACC: heart failure. JACC Heart Fail. 2013;1(3):213–5.
Ahmad T, Fiuzat M, Pencina MJ, et al. Charting a roadmap for heart failure biomarker studies. JACC Heart Fail. 2014;2(5):477–88.
Eurlings LW, van Pol PE, Kok WE, et al. Management of chronic heart failure guided by individual N-terminal pro-B-type natriuretic peptide targets: results of the PRIMA (can PRo-brain-natriuretic peptide guided therapy of chronic heart failure improve heart failure morbidity and mortality?) study. J Am Coll Cardiol. 2010;56(25):2090–100.
Pfisterer M, Buser P, Rickli H, et al. BNP-guided vs symptom-guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients with Congestive Heart Failure (TIME-CHF) randomized trial. JAMA. 2009;301(4):383–92.
Berger R, Moertl D, Peter S, et al. N-terminal pro-B-type natriuretic peptide-guided, intensive patient management in addition to multidisciplinary care in chronic heart failure a 3-arm, prospective, randomized pilot study. J Am Coll Cardiol. 2010;55(7):645–53.
Jourdain P, Jondeau G, Funck F, et al. Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP multicenter study. J Am Coll Cardiol. 2007;49(16):1733–9.
Persson H, Erntell H, Eriksson B, Johansson G, Swedberg K, Dahlstrom U. Improved pharmacological therapy of chronic heart failure in primary care: a randomized study of NT-proBNP Guided Management of Heart Failure—SIGNAL-HF (Swedish Intervention study—Guidelines and NT-proBNP Analysis in Heart Failure). Eur J Heart Fail. 2010;12(12):1300–8.
Januzzi Jr JL, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B-type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol. 2011;58(18):1881–9.
Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: a meta-analysis. Arch Intern Med. 2010;170(6):507–14.
Januzzi Jr JL. The role of natriuretic peptide testing in guiding chronic heart failure management: review of available data and recommendations for use. Arch Cardiovasc Dis. 2012;105(1):40–50.
•• Felker GM, Ahmad T, Anstrom KJ, et al. Rationale and design of the GUIDE-IT study: guiding evidence based therapy using biomarker intensified treatment in heart failure. JACC Heart Fail. 2014;2(5):457–65. An important validation study for the use of natriuretic peptide testing to guide therapy.
Weinberg EO, Shimpo M, Hurwitz S, Tominaga S, Rouleau JL, Lee RT. Identification of serum soluble ST2 receptor as a novel heart failure biomarker. Circulation. 2003;107(5):721–6.
Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest. 2007;117(6):1538–49.
Weinberg EO, Shimpo M, De Keulenaer GW, et al. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation. 2002;106(23):2961–6.
Seki K, Sanada S, Kudinova AY, et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail. 2009;2(6):684–91.
Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail. 2011;4(2):180–7.
Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol. 2014;63(2):158–66.
Wang YC, Yu CC, Chiu FC, et al. Soluble ST2 as a biomarker for detecting stable heart failure with a normal ejection fraction in hypertensive patients. J Card Fail. 2013;19(3):163–8.
Gaggin HK, Szymonifka J, Bhardwaj A, et al. Head-to-head comparison of serial soluble ST2, growth differentiation factor-15, and highly-sensitive troponin T measurements in patients with chronic heart failure. JACC Heart Fail. 2014;2(1):65–72.
Manzano-Fernandez S, Januzzi JL, Pastor-Perez FJ, et al. Serial monitoring of soluble interleukin family member ST2 in patients with acutely decompensated heart failure. Cardiology. 2012;122(3):158–66.
Gaggin HK, Motiwala S, Bhardwaj A, Parks KA, Januzzi Jr JL. Soluble concentrations of the interleukin receptor family member ST2 and beta-blocker therapy in chronic heart failure. Circ Heart Fail. 2013;6(6):1206–13.
Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure trial. Circ Heart Fail. 2014;7(3):418–26.
Maisel A, Xue Y, van Veldhuisen DJ, et al. Effect of spironolactone on 30-day death and heart failure rehospitalization (from the COACH study). Am J Cardiol. 2014;114(5):737–42.
Januzzi Jr JL, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol. 2007;50(7):607–13.
Tang WH, Wu Y, Grodin JL, et al. Prognostic value of baseline and changes in circulating soluble ST2 levels and the effects of nesiritide in acute decompensated heart failure. JACC Heart Fail. 2016;4(1):68–77.
Xue Y, Clopton P, Peacock WF, Maisel AS. Serial changes in high-sensitive troponin I predict outcome in patients with decompensated heart failure. Eur J Heart Fail. 2011;13(1):37–42.
de Boer RA, Daniels LB, Maisel AS, Januzzi Jr JL. State of the art: newer biomarkers in heart failure. Eur J Heart Fail. 2015;17(6):559–69.
Yang RY, Rabinovich GA, Liu FT. Galectins: structure, function and therapeutic potential. Expert Rev Mol Med. 2008;10:e17.
Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation. 2004;110(19):3121–8.
Yu L, Ruifrok WP, Meissner M, et al. Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circ Heart Fail. 2013;6(1):107–17.
de Boer RA, Lok DJ, Jaarsma T, et al. Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann Med. 2011;43(1):60–8.
Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail. 2015;17(2):214–23.
Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail. 2010;12(8):826–32.
Calvier L, Miana M, Reboul P, et al. Galectin-3 mediates aldosterone-induced vascular fibrosis. Arterioscler Thromb Vasc Biol. 2013;33(1):67–75.
Gandhi PU, Motiwala SR, Belcher AM, et al. Galectin-3 and mineralocorticoid receptor antagonist use in patients with chronic heart failure due to left ventricular systolic dysfunction. Am Heart J. 2015;169(3):404–411.e403.
Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Eur Heart J. 2012;33(18):2290–6.
Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail. 2013;15(5):511–8.
AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (phosphodiesterase-5 inhibition to improve clinical status and exercise capacity in diastolic heart failure). JACC Heart Fail. 2015;3(3):245–52.
Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc. 2012;1(5):e000760.
Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol. 2011;108(3):385–90.
Damman K, Testani JM. The kidney in heart failure: an update. Eur Heart J. 2015;36(23):1437–44.
Shlipak MG, Matsushita K, Arnlov J, et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med. 2013;369(10):932–43.
Brisco MA, Testani JM. Novel renal biomarkers to assess cardiorenal syndrome. Curr Heart Fail Rep. 2014;11(4):485–99.
Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail. 2015;3(1):40–9.
Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail. 2012;14(6):597–604.
Aghel A, Shrestha K, Mullens W, Borowski A, Tang WH. Serum neutrophil gelatinase-associated lipocalin (NGAL) in predicting worsening renal function in acute decompensated heart failure. J Card Fail. 2010;16(1):49–54.
Shrestha K, Shao Z, Singh D, Dupont M, Tang WH. Relation of systemic and urinary neutrophil gelatinase-associated lipocalin levels to different aspects of impaired renal function in patients with acute decompensated heart failure. Am J Cardiol. 2012;110(9):1329–35.
Damman K, Masson S, Hillege HL, et al. Clinical outcome of renal tubular damage in chronic heart failure. Eur Heart J. 2011;32(21):2705–12.
Damman K, Van Veldhuisen DJ, Navis G, et al. Tubular damage in chronic systolic heart failure is associated with reduced survival independent of glomerular filtration rate. Heart. 2010;96(16):1297–302.
Emmens JE, Ter Maaten JM, Matsue Y, et al. Plasma kidney injury molecule-1 in heart failure: renal mechanisms and clinical outcome. Eur J Heart Fail. 2016;18(6):641–9.
Grodin JL, Perez AL, Wu Y, et al. Circulating kidney injury molecule-1 levels in acute heart failure: insights from the ASCEND-HF trial (acute study of clinical effectiveness of nesiritide in decompensated heart failure). JACC Heart Fail. 2015;3(10):777–85.
Ky B, French B, Levy WC, et al. Multiple biomarkers for risk prediction in chronic heart failure. Circ Heart Fail. 2012;5(2):183–90.
Wang TJ, Wollert KC, Larson MG, et al. Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham Heart Study. Circulation. 2012;126(13):1596–604.
Sanders-van Wijk S, van Empel V, Davarzani N, et al. Circulating biomarkers of distinct pathophysiological pathways in heart failure with preserved vs. reduced left ventricular ejection fraction. Eur J Heart Fail. 2015;17(10):1006–14.
Watkins H, Ashrafian H, Redwood C. Inherited cardiomyopathies. N Engl J Med. 2011;364(17):1643–56.
Oni-Orisan A, Lanfear DE. Pharmacogenomics in heart failure: where are we now and how can we reach clinical application? Cardiol Rev. 2014;22(5):193–8.
Smith JG, Felix JF, Morrison AC, et al. Discovery of genetic variation on chromosome 5q22 associated with mortality in heart failure. PLoS Genet. 2016;12(5):e1006034.
Perez MV, Pavlovic A, Shang C, et al. Systems genomics identifies a key role for hypocretin/orexin receptor-2 in human heart failure. J Am Coll Cardiol. 2015;66(22):2522–33.
Meder B, Ruhle F, Weis T, et al. A genome-wide association study identifies 6p21 as novel risk locus for dilated cardiomyopathy. Eur Heart J. 2014;35(16):1069–77.
Villard E, Perret C, Gary F, et al. A genome-wide association study identifies two loci associated with heart failure due to dilated cardiomyopathy. Eur Heart J. 2011;32(9):1065–76.
Cappola TP, Matkovich SJ, Wang W, et al. Loss-of-function DNA sequence variant in the CLCNKA chloride channel implicates the cardio-renal axis in interindividual heart failure risk variation. Proc Natl Acad Sci U S A. 2011;108(6):2456–61.
Small EM, Frost RJ, Olson EN. MicroRNAs add a new dimension to cardiovascular disease. Circulation. 2010;121(8):1022–32.
Liebetrau C, Mollmann H, Dorr O, et al. Release kinetics of circulating muscle-enriched microRNAs in patients undergoing transcoronary ablation of septal hypertrophy. J Am Coll Cardiol. 2013;62(11):992–8.
Wang GK, Zhu JQ, Zhang JT, et al. Circulating microRNA: a novel potential biomarker for early diagnosis of acute myocardial infarction in humans. Eur Heart J. 2010;31(6):659–66.
Tijsen AJ, Creemers EE, Moerland PD, et al. MiR423-5p as a circulating biomarker for heart failure. Circ Res. 2010;106(6):1035–9.
Wong LL, Armugam A, Sepramaniam S, et al. Circulating microRNAs in heart failure with reduced and preserved left ventricular ejection fraction. Eur J Heart Fail. 2015;17(4):393–404.
Matsumoto S, Sakata Y, Suna S, et al. Circulating p53-responsive microRNAs are predictive indicators of heart failure after acute myocardial infarction. Circ Res. 2013;113(3):322–6.
Gurha P, Abreu-Goodger C, Wang T, et al. Targeted deletion of microRNA-22 promotes stress-induced cardiac dilation and contractile dysfunction. Circulation. 2012;125(22):2751–61.
Montgomery RL, Hullinger TG, Semus HM, et al. Therapeutic inhibition of miR-208a improves cardiac function and survival during heart failure. Circulation. 2011;124(14):1537–47.
Senn T, Hazen SL, Tang WH. Translating metabolomics to cardiovascular biomarkers. Prog Cardiovasc Dis. 2012;55(1):70–6.
Wang TJ, Gupta DK. Metabolite profiles in heart failure: looking for unique signatures in a heterogeneous syndrome. J Am Coll Cardiol. 2015;65(15):1521–4.
Cheng ML, Wang CH, Shiao MS, et al. Metabolic disturbances identified in plasma are associated with outcomes in patients with heart failure: diagnostic and prognostic value of metabolomics. J Am Coll Cardiol. 2015;65(15):1509–20.
Tang WH, Wang Z, Shrestha K, et al. Intestinal microbiota-dependent phosphatidylcholine metabolites, diastolic dysfunction, and adverse clinical outcomes in chronic systolic heart failure. J Card Fail. 2015;21(2):91–6.
Tang WH, Wang Z, Fan Y, et al. Prognostic value of elevated levels of intestinal microbe-generated metabolite trimethylamine-N-oxide in patients with heart failure: refining the gut hypothesis. J Am Coll Cardiol. 2014;64(18):1908–14.
Doehner W, Frenneaux M, Anker SD. Metabolic impairment in heart failure: the myocardial and systemic perspective. J Am Coll Cardiol. 2014;64(13):1388–400.
Tunon J, Martin-Ventura JL, Blanco-Colio LM, Lorenzo O, Lopez JA, Egido J. Proteomic strategies in the search of new biomarkers in atherothrombosis. J Am Coll Cardiol. 2010;55(19):2009–16.
Gregorich ZR, Chang YH, Ge Y. Proteomics in heart failure: top-down or bottom-up? Pflugers Arch. 2014;466(6):1199–209.
Shah SJ, Katz DH, Selvaraj S, et al. Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation. 2015;131(3):269–79.
Ahmad T, Pencina MJ, Schulte PJ, et al. Clinical implications of chronic heart failure phenotypes defined by cluster analysis. J Am Coll Cardiol. 2014;64(17):1765–74.
Kao DP, Lewsey JD, Anand IS, et al. Characterization of subgroups of heart failure patients with preserved ejection fraction with possible implications for prognosis and treatment response. Eur J Heart Fail. 2015;17(9):925–35.
Shah AM, Solomon SD. Phenotypic and pathophysiological heterogeneity in heart failure with preserved ejection fraction. Eur Heart J. 2012;33(14):1716–7.
Shah DJ, Kim HW, James O, et al. Prevalence of regional myocardial thinning and relationship with myocardial scarring in patients with coronary artery disease. JAMA. 2013;309(9):909–18.
Klem I, Weinsaft JW, Bahnson TD, et al. Assessment of myocardial scarring improves risk stratification in patients evaluated for cardiac defibrillator implantation. J Am Coll Cardiol. 2012;60(5):408–20.
Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66–74.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Vichai Senthong and Jennifer L. Kirsop declare that they have no conflict of interest.
W.H. Wilson Tang has received grants from the National Institutes of Health (R01HL103931, P20HL113452, R01DK106000, R01HL126827) outside of the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Biomarkers of Heart Failure
Rights and permissions
About this article
Cite this article
Senthong, V., Kirsop, J.L. & Tang, W.H.W. Clinical Phenotyping of Heart Failure with Biomarkers: Current and Future Perspectives. Curr Heart Fail Rep 14, 106–116 (2017). https://doi.org/10.1007/s11897-017-0321-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-017-0321-4