Abstract
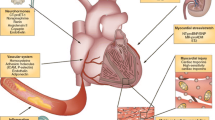
Biomarkers are increaingly being used in the management of heart failure not only for the purpose of screening, diagnosis, and risk stratification, but also as a guide to evaluate the response to treatment in the individual patient and as an entry criterion and/or a surrogate marker of efficacy in clinical trials testing novel drugs. In this chapter, we review the role of established biomarkers for heart failure management, according to the main classification of HF phenotypes, based on the measurement of left ventricular ejection fraction, including heart failure with reduced (<40%), preserved (≥50%), and, as recently proposed, mid-range (40-49%) ejection fraction.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Early diagnostic and therapeutic interventions counteracting pathophysiological mechanisms of heart failure (HF) progression, such as drugs inhibiting the renin-angiotensin-aldosterone system (RAAS) and adrenergic system activation, as well as device implantation in selected patients positively influence its clinical course, impacting on the arrhythmic burden and hemodynamics. Notwithstanding, outcome is still characterized by a high morbidity and mortality. Interest is therefore growing in the optimization of HF management and in the identification and validation of novel therapeutical tools. With these premises, research has focused on the use of biomarkers not only for the purpose of screening, diagnosis, and risk stratification, but also as a guide to the assessment of response to treatment in the individual patient, and finally as an entry criterion and/or a surrogate marker of efficacy in clinical trials testing novel drugs (Braunwald 2008; Braunwald 2013; Emdin et al. 2009).
In 2001, a National Institute of Health working group defined a biomarker as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” and identified different classes of biomarkers according to their role and potential utility in disease management. In particular, biomarkers were classified as antecedent biomarkers (i.e., those identifying the risk of developing a disease), screening biomarkers (those able to screen for subclinical disease), diagnostic biomarkers (recognizing clinically overt disease), staging biomarkers (those reflecting disease severity), or prognostic biomarkers (predicting the future course of the disease and response to pharmacological and non-pharmacological approaches) (Biomarkers Definitions Working Group 2001; Vasan 2006).
A number of biomarkers have been proposed for HF management purposes in the last years; nonetheless only a very few of them (namely B-type natriuretic peptides) are routinely used in current clinical practice. Indeed, several characteristics are requested for a circulating biomarker to be of real clinical value, related to (pre)analytical, biological, feasibility, and cost-effectiveness issues. In particular, the ideal biomarker for HF management should reflect the cardiovascular response to a specific pathogenic noxa; provide early information on cardiac involvement in preclinical stages (screening in HF stages A–B) and/or guide HF diagnosis when cardiac origin of symptoms is doubtful (HF stage C); be influenced by clinical modification in the disease history; and stratify patients’ risk and help in therapeutic decision making (Table 1). Still, novel biomarkers are clearly required to improve risk prediction already offered by existing models, with the mere demonstration of a statistically significant association with a prespecified end-point not being enough (Pencina et al. 2008). Further to c-statistic and receiver-operating-characteristic curve (AUC) measure (Pencina et al. 2010), providing estimate of the discriminative ability of the model (i.e., the capacity to separate subject developing/not developing the outcome), and measures of calibration (indicating how close are predicted and observed risks in different groups of observations, e.g., by means of the Hosmer-Lemeshow test) and of reclassification (indicating the ability of the model to reclassify individuals into a different risk category, e.g., by calculating the net reclassification improvement, NRI) are required to adequately assess the clinical utility of novel biomarkers (McGeechan et al. 2008; Parikh and Vasan 2007).
In this chapter, current evidences on the role of established and candidate biomarkers for HF management are discussed, according to the main classification of HF phenotypes, based on the measurement of left ventricular ejection fraction (LVEF), including HF with reduced EF (HFrEF, LVEF <40%), HF with preserved EF (HFpEF, LVEF ≥50%), and the recently proposed category HF with mid-range EF (HFmrEF, LVEF 40–49%) (Ponikowski et al. 2016).
2 Biomarkers of Heart Failure with Reduced Ejection Fraction
2.1 B-type Natriuretic Peptides in Heart Failure with Reduced Ejection Fraction (HFrEF): Standing on the Shoulders of Giants
Human brain natriuretic peptide (BNP) and the amino-terminal fragment of proBNP (NT-proBNP) are produced in equimolar fashion from the cleavage of their 108-amino acid precursor proBNP by proprotein convertases, such as corin and furin. The biologically active BNP is rapidly degraded in vivo by several peptidases, such as dipeptidyl peptidase IV and neutral endopeptidases (NEP, neprilysin) (Clerico and Emdin 2004; Pankow et al. 2007; Vanderheyden et al. 2009). BNP, together with NT-proBNP, is mainly product of ventricular myocytes in response to increased myocardial wall stress due to volume or pressure overload states and plays a major role in HF pathophysiology, given its diuretic, natriuretic, vasodilator, and anti-hypertrophic properties (Motiwala and Januzzi 2013).
Since the beginning of the twenty-first century, several studies have accumulated showing the clinical utility of B-type natriuretic peptide testing, supporting the use of a circulating biomarker to diagnose and assess severity of HF (Januzzi et al. 2005; Maisel et al. 2002; Troughton et al. 2000). At present, BNP and NT-proBNP are routinely used for HF management in a large variety of clinical settings. Strong evidence exists supporting the use of natriuretic peptide testing to diagnose (and rule out) HF in patients presenting with dyspnea. The Breathing Not Properly and the ProBNP Investigation of Dyspnea (PRIDE) trials have shown that BNP and NT-proBNP, respectively, can diagnose HF in patients admitted to the emergency department for breathlessness, with a high accuracy and a significant negative predictive value for levels of BNP <100 ng/L (Januzzi et al. 2005; Maisel et al. 2002). Although with lower cut points, the diagnostic value of natriuretic peptides has been confirmed in ambulatory settings (Wright et al. 2003). Moreover, in a cohort of around 800 patients with chronic HF, they have been shown to be associated with the presence of LV systolic dysfunction (defined as LVEF <40%) with an AUC of 0.803 (95% CI 0.757–0.849) and 0.730 (0.681–0.778) for BNP and NT-proBNP, respectively (Moertl et al. 2009). In stable patients with HFrEF, BNP circulating levels reflect disease severity, and increase with worsening symptoms (NYHA class) (Emdin et al. 2004). The assay of natriuretic peptides is currently recommended for diagnostic purposes by all major scientific societies, including the American College of Cardiology, the American Heart Association, the Heart Failure Society of America, and the European Society of Cardiology (Lindenfeld et al. 2010; Ponikowski et al. 2016; Yancy et al. 2013); however, no single diagnostic cutoff exists and natriuretic peptide levels often fall into a “grey zone.” Further, both BNP and NT-proBNP are influenced by gender, age, and comorbidities (in particular by renal function); therefore their interpretation must take into account the overall clinical assessment (Passino et al. 2008; van Kimmenade et al. 2008).
In adjunct to diagnostic properties, there is overwhelming evidence that natriuretic peptides hold prognostic value in HFrEF in both acute and chronic settings over other clinical factors. In >19,000 patients with HFrEF form the ADHERE (Acute Decompensated Heart Failure National Registry), admission BNP levels were near-linearly associated with in-hospital mortality, independently from other major clinical and laboratory risk factors (Fonarow et al. 2007). In a systematic review of studies performed in different clinical settings, Doust and colleagues have demonstrated that each 100 ng/L increase in BNP is associated with a relative 35% increase in risk (Doust et al. 2005). NT-proBNP predicts as well both short- and long-term prognosis after hospitalization for acute HF, with values >986 ng/L predicting 1-year death (Januzzi et al. 2006a, b). Although most studies have investigated the prognostic role of admission natriuretic peptide levels, there is evidence that discharge BNP and NT-proBNP, and their change during hospitalization, also predict outcome of patients with HFrEF. Data from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) show that the addition of discharge BNP to a clinical model significantly improved risk classification for 1-year mortality with an NRI of 5.5% (Kociol et al. 2011), thus suggesting that serial natriuretic peptide testing may be useful in predischarge clinical decision making (Januzzi et al. 2012). A post hoc analyses of the Valsartan Heart Failure Trial (Val-HeFT), enrolling patients with chronic symptomatic HF with LVEF <40% and LV diameter in diastole adjusted for body surface area ≥2.9 cm/m2, demonstrated that BNP and NT-proBNP similarly predicted all-cause mortality, while NT-proBNP outperformed BNP for the prediction of mortality and morbidity or hospitalization for HF (Masson et al. 2006). Moreover, experience from the Val-HeFT indicates that changes over time in natriuretic peptides, too, hold a prognostic value in stable HF, envisaging a role for serial BNP and NT-proBNP testing in patient monitoring and in the evaluation of response to therapeutical strategies (Masson et al. 2008; Richards 2008).
2.2 B-type Natriuretic Peptide-Guided Therapy
Circulating levels of B-type natriuretic peptides are influenced by most of the pharmacological and non-pharmacological therapeutical approaches in acute, acutely decompensated, and chronic HF. Indeed, in the acute setting, treatment with furosemide and the inodilator levosimendan decreases BNP (Cohen-Solal et al. 2009; Farmakis et al. 2010; Palazzuoli et al. 2014). Moreover, a reduction >30% from baseline values following levosimendan administration has been associated with an improvement in either short- (31 days) or long-term (180 days) mortality (Cohen-Solal et al. 2009). Other therapeutic strategies acting on hemodynamics and cardiac remodeling have been demonstrated to elicit similar effects on natriuretic peptides in stable HFrEF, including angiotensin-converting enzyme inhibitors (Rosenberg et al. 2008), angiotensin-receptor blockers (Anand et al. 2003), mineralocorticoid receptor antagonists (Berry et al. 2007), and, at a lower extent, β-blockers, whose initiation may also cause a transient increase in BNP and NT-proBNP, which subsequently decrease (Davis et al. 2006; Rosenberg et al. 2008). Evidence for a beneficial effect on natriuretic peptides also exists for other non-pharmacological tools, such as aerobic training and cardiac resynchronization therapy (Fruhwald et al. 2007; Passino et al. 2006). More recently, the first-in-class neprilysin/angiotensin receptor inhibitor sacubitril valsartan (LCZ696) has been proved effective in reducing the risks of death and of hospitalization in patients with HFrEF compared to enalapril in the PARADIGM-HF trial (McMurray et al. 2014). Such beneficial effects are possibly due, at least in part, to the inhibition of BNP degradation exerted by sacubitril, while its precursor and NT-proBNP are virtually resistant to degradation (Semenov and Katrukha 2016), as also supported by the observation that after LCZ696 initiation, circulating levels of NT-proBNP decrease, while BNP slightly increases (Packer et al. 2015). It has been therefore questioned that assessing the clinical significance of BNP in the era of LCZ696 may be challenging and that NT-proBNP may be preferred over BNP for biochemical monitoring of patients with HF, in order to assess its effectiveness on hemodynamic status (Lippi and Sanchis-Gomar 2016).
As discussed before, natriuretic peptides perform well for diagnostic and prognostic purposes and are associated with disease severity and, importantly, their circulating levels change in response to evidence-based therapies for HF. Based on these premises, several studies have tested the (cost)effectiveness of strategies of treatment titration guided by natriuretic peptide circulating levels, the so-called biomarker-guided therapy. In the BATTLESCARED, the first of these studies, 364 HF patients were randomly allocated to therapy guided by NT-proBNP levels (with adjustments in medications and additional follow-up visits triggered by an NT-proBNP level >150 pmol/l) or by intensive clinical management, or according to usual care (Lainchbury et al. 2009). NT-proBNP-guided treatment was associated with a significant reduction in a primary end-point of death and/or readmission with heart failure in younger population (age ≤75 years), who also presented more often with HFrEF (61% vs. 47% in patients aged >75 years). In the same year results from the TIME-CHF trial, enrolling only patients with LVEF ≤45%, were published, showing that patients with therapy titration based on NT-proBNP (target: <400 ng/L in patients aged <75 years and <800 ng/L in patients ≥75 years) had improved 18-month survival free of hospitalizations for HF (Pfisterer et al. 2009). Following these pivotal trials, other studies using either BNP or NT-proBNP have provided mixed outcomes (Kim and Januzzi 2010). Some systematic reviews have addressed the issue of the effects on hard end-points, such as all-cause mortality, demonstrating a benefit from natriuretic peptide-guided therapy (Don-Wauchope and McKelvie 2015), and a meta-analysis by Felker has demonstrated a 30% improvement in survival, without an increase in therapy-related adverse events (Felker et al. 2009). As a general view, the use of natriuretic peptide to tailor HF therapy is likely to be more effective when lower target values are applied (i.e., <100 ng/L and <1,000 ng/L for BNP and NT-proBNP, respectively) (Januzzi et al. 2011; Jourdain et al. 2007; Troughton et al. 2000). Nonetheless, evidence is still scarce to support a general recommendation and some issues still need to be addressed, including the most appropriate use of biomarker with this respect (disease management vs. monitoring), the choice of the end-point, and the cost-effectiveness of such a strategy (Pruett et al. 2015).
2.3 Back to the de Bold’s “Atrial Natriuretic Factor”: MR-proANP
Although B-type natriuretic peptides represent the most widely studied cardiac hormones, both in the experimental and clinical field, atrial natriuretic peptide (ANP) was first described in early 1980s, as a substance secreted from atrial granules with endocrine functions, by Adolfo de Bold (de Bold 1981). ANP assay has with time been substituted by assays of B-type natriuretic peptides both for analytical and clinical reasons (Clerico 2006). More recently, the potential clinical applications of the mid-regional pro-atrial natriuretic peptide (MR-proANP), with a longer half-life than ANP, have been tested. Data from the Biomarker in the Acute Heart Failure (BACH) and the PRIDE study have demonstrated a good performance of MR-proANP for diagnostic and prognostic purposes in acute HF, even in addition to NT-proBNP (Maisel et al. 2011a; b, c; Shah et al. 2012). MR-proANP also revealed a significant prognostic value in 1237 patients with chronic HF enrolled in the Gruppo Italiano per lo Studio della Sopravvivenza nell’Insufficienza Cardiaca-Heart Failure (GISSI-HF) study (proposed cutoff 278 pmol/L, AUC 0.74, 0.71–0.77), outperforming other established and candidate biomarkers (including copeptin and mid-regional proadrenomedullin, MR-proADM, and C-terminal proendothelin-1) and beyond NT-proBNP and a set of clinical variables (NRI = 0.06) (Masson et al. 2010a).
2.4 Cardiac Troponins
Cardiac troponins are released into the circulation following the disruption of cardiomyocyte membrane due to cardiac injury, namely after cardiac necrosis, and have become the standard of care biomarker for diagnosis of myocardial infarction. Nonetheless, elevation of circulating troponins has been reported also in non-acute settings, including chronic HF, due to mechanisms still to be fully elucidated, possibly involving inflammation, neurohormonal activation, myocardial stretch, hypoxia, and cytotoxicity (Gaggin and Januzzi 2013). With the improvement in troponin assays and the rise of high-sensitivity troponins (hsTn), detectable circulating troponin is now observed in a large proportion of HF patients and several studies have explored its use in clinical practice as an additional biomarker for disease management. In 140 patients with acute HF, TnI was found to be increased in about 1/3 of cases and to independently predict 90-day mortality and readmission. Further, increase in TnI during hospitalization was also associated with a worse outcome (Xue et al. 2011). In the RELAX-AHF trial, hs-TnT was elevated above the 99% upper reference limit in most of the AHF patients. Baseline, peak, and peak change hs-cTnT were associated with worse outcomes, in particular with 180-day cardiovascular mortality (Felker et al. 2015). In the ADHERE study, patient with TnI elevation had significantly higher in-hospital mortality when treated with intravenous inotropic therapy as compared with intravenous vasodilator therapy (Peacock et al. 2008).
As in acute settings, circulating Tn is associated with prognosis also in chronic HF. In an analysis performed in >4000 patients enrolled in the Val-HeFT, TnT was detectable in about 10% of patients using a conventional assay, while 92% showed detectable Tn when the hsTnT assay was used. In the same cohort, hsTnT was associated with the risk of death and LV remodeling, and improved prognostic discrimination when added to a baseline model including BNP (Latini et al. 2007). The prognostic utility of serial Tn measurement in chronic HF has been investigated in patients from both the Val-HeFT and the GISSI-HF study. In this cohort, although increase in hsTnT over 3 to 4 months was strongly associated with all-cause mortality after adjustment for clinical risk factors, baseline levels, and NT-proBNP, it only modestly improved prognostic discrimination (Masson et al. 2012).
Previous reports show an association between the use of ACEi and beta-blockers with lower circulating Tn levels (Horwich et al. 2003; Masson et al. 2012), thus suggesting that guideline-recommended therapy may mitigate the risk in subsets with elevated Tn. More recently, in the PARADIGM-HF trial, treatment with LCZ696 led to a significant and sustained reduction in hsTnT that was not observed in the enalapril arm (Packer et al. 2015). Still, the issue of a Tn-guided therapy in chronic HF remains to be explored.
2.5 Candidate Biomarkers of HFrEF
Natriuretic peptides represent nowadays a fundamental aid to the clinical management of HF; nonetheless circulating levels of either BNP or NT-proBNP increase following each generic insult to the cardiovascular system. Therefore, while they are highly sensitive in the detection of ongoing damage, they are not able to provide clinically significant information concerning the nature of the noxa. The development and progression of the HF syndrome result from a complex interplay between different pathogenic determinants sustaining the ongoing myocardial damage and (mal)adaptive mechanisms. As a consequence, biomarkers providing insights into the extent of activation of specific axes of disease progression may help the clinician in the process of disease (and patient) characterization and of treatment tailoring.
A huge number of biomarkers have been tested or are currently under investigation for HF which may be classified according to he pathophysiological mechanism of damage they are considered to reflect. As previously suggested, biomarkers of sympathetic and RAAS activation, inflammation, fibrosis, and comorbidities can be distinguished (Braunwald 2013; Emdin et al. 2009).
2.5.1 Sympathetic Activation
Activation of the sympathetic, and inhibition of the parasympathetic system, represents one of the first (mal)adaptive mechanisms in disease onset and progression and one of the bases of the neuroendocrine model of HF, given its vasoconstrictive, profibrotic, and arrhythmogenic effects (Leimbach et al. 1986). Circulating norepinephrine increases with disease severity (Emdin et al. 2004), and, in a seminal paper by Cohn, it was the only independent predictor of mortality in 106 patients with moderate to severe HF, although such finding was not confirmed later on in more contemporary series (Cabassi et al. 2013; Cohn et al. 1984). Data from the Val-HeFT have shown that treatment with valsartan can blunt the increase in norepinephrine compared to placebo, while it was not affected by the mineralocorticoid receptor antagonist (MRA) spironolactone (Latini et al. 2002; Rousseau et al. 2002).
Together with catecholamines, chromogranin A is a component of chromaffin granules in the adrenal glands and, although its biological effects on the cardiovascular system remain to be elucidated, it seems to be involved in the regulation of adrenergic system (Tota et al. 2014). Limited evidence exists that circulating chromogranin A is increased in either acute or chronic HF and that may have some prognostic value (Dieplinger et al. 2009a; Røsjø et al. 2010).
2.5.2 Renin-Angiotensin-Aldosterone System Activation
RAAS is a complex endocrine system participated by the kidney, liver, vascular endothelium, and adrenal cortex regulating salt/water homeostasis and vasomotion. Either systemic or tissue RAAS are involved in tissue remodeling after damage, and can promote fibrosis, hypertrophy, and apoptosis. All the effectors of RAAS are increased in chronic HF (Emdin et al. 2004) and RAAS activation is an indirect or direct target of most effective pharmacological treatments in heart failure, such as beta-blockers, inhibitors of angiotensin-converting enzyme, angiotensin receptor blockers, direct renin inhibitors, mineralocorticoid receptor blockers, and angiotensin receptor/neprilysin inhibitors. Circulating biomarkers of RAAS activation are currently available, such as plasma renin activity (PRA), renin, angiotensin II, and aldosterone, although with different feasibility and accuracy, and some of them are well-recognized prognostic factors, even in patients with optimal therapy. Notably, chronic use of drugs acting on RAAS induces, per se, neurohormonal reactivation (Lee et al. 1999; Rousseau et al. 2002).
PRA has been demonstrated to hold an independent prognostic value in a systolic HF cohort on evidence-weighted treatment, with and without significant renal comorbidity (Poletti et al. 2013; Vergaro et al. 2011), thus potentially qualifying as a tool to identify patients with persistent RAAS activation despite adequate neurohormonal antagonism and to select subsets at higher risk for cardiovascular events. Further, aldosterone was shown to be a predictor of all-cause mortality in ≈300 patients with HF (most of them with systolic dysfunction), independently from other clinical and biohumoral variable including NT-proBNP (Güder et al. 2007). Specifically, the increase in circulating aldosterone following the initiation of RAAS acting therapy, a phenomenon termed “aldosterone breakthrough,” may hold clinical relevance, given the growing evidence on non-mineralocorticoid receptor-mediated effects of aldosterone. Further, in a small group of patients with systolic HF, increased PRA predicted ACE inhibitor-induced natriuresis (Lim et al. 2000).
The above-mentioned data support the rationale for the use of biomarkers of RAAS activation as a guide for treatment monitoring and tailoring, as well as a rule-in variable for trials in HF setting, a role up to now discarded as for the case of trials with the direct renin inhibitor aliskiren.
2.5.3 Inflammation and Immunity
There is growing information on the role of inflammatory cells and pathways during acute cardiovascular injury and in the reparative process that is subsequently activated. Elevation of inflammatory biomarkers, including C-reactive protein (CRP), members of the interleukin family (e.g., IL-1, IL-6, and IL-18), and TNF-α, is a hallmark feature of chronic ischemic and non-ischemic HF, although whether inflammation is causative to disease progression is not yet clear (Mann 2015). Moreover, viral infection is thought to participate in the development of dilated cardiomyopathy, sustaining acute and chronic inflammation (Kühl et al. 1996).
The Val-HeFT study demonstrated a direct correlation between elevated CRP level and HF severity (Anand et al. 2005); further, CRP predicts the risk of death and early readmission in acutely decompensated HF (Lourenço et al. 2010). Anti-inflammatory properties have been described for statins and their effect has been tested in HF settings. Data from the CORONA study show that subjects with HF of ischemic etiology and elevated baseline high sensitivity-CRP (≥2 mg/L) exhibited a greater benefit from statin therapy in terms of reduction of the primary end-point of cardiovascular death, myocardial infarction, and stroke (McMurray et al. 2009), while controversial results come from studies performed on patients with HF of non-ischemic origin (Bleske et al. 2006; Sola et al. 2006).
Some trials have addressed TNF-α elevation in HF, which is associated with worsened prognosis. Two large clinical studies, the Randomized Etanercept North American Strategy to Study Antagonism of Cytokines (RENAISSANCE) and the Research into Etanercept Cytokine Antagonism in Ventricular Dysfunction (RECOVER), were stopped because of lack of clinical benefit, and patients receiving the highest dose had increased adverse cardiac outcomes (Mann et al. 2004). Similar results were observed in the Anti-TNF-α in Congestive Heart Failure (ATTACH) trial, testing humanized neutralizing antibodies (infliximab) instead of the soluble receptor etanercept (Chung et al. 2003). The negative results of such trials may be, at least in part, explained by the inappropriate blockade of “physiological” inflammation that may be required for tissue-reparative processes.
2.5.4 Fibrosis
Galectin-3
In recent years galectin-3 (Gal-3), a soluble β-galactoside-binding lectin, has been found to play an important mechanistic role in the development of cardiac fibrosis and remodeling and to identify high-risk subsets in HF cohorts, thus qualifying both as a risk marker and a risk factor (de Boer et al. 2009). There is a growing amount of evidence that Gal-3 is essential for migration and phagocytic activity of macrophages. Macrophage-derived Gal-3 may then act on fibroblast proliferation and on collagen synthesis, by increasing collagen I and reversing the collagen I-to-collagen III ratio (Henderson and Sethi 2009). Together with liver and kidney fibrosis, Gal-3 has been strictly linked to the development of cardiac fibrosis, a key determinant of cardiac remodeling and HF progression, possibly by interacting with mechanisms of aldosterone-mediated damage (Vergaro et al. 2016). Further, circulating levels of Gal-3 are associated with biomarkers of extracellular matrix turnover (including PIIINP, TIMP-1, and MMP-2), after adjustment for several clinical variables in a population 106 patients with systolic HF (Lin et al. 2009).
The experimental demonstration of a mechanistic involvement of Gal-3 in fibrotic, inflammatory, and remodeling processes in heart disease led to a novel interest in the potential use of Gal-3 assayed in plasma, as a biomarker. van Kimmenade and colleagues in 2006 first compared NT-proBNP, apelin, and Gal-3 in the management of acute HF patients (van Kimmenade et al. 2006). Out of 599 acutely dyspneic patients, 209 were later diagnosed with HF. Although Gal-3 showed a limited diagnostic accuracy in identifying acute HF, it was the strongest predictor of early events (60-day re-hospitalization for HF or all-cause mortality). Later on, Gal-3 was also demonstrated to predict long-term outcome (4-year mortality) in another cohort of acute HF patients (proposed cutoff: 14.97 ng/mL), independently of echocardiographic indices of cardiac structure and function (LV end-diastolic/systolic diameter, EF and right ventricular pressure) (Shah et al. 2010). In the following years the prognostic role of Gal-3 in HF settings has been investigated in some substudies from larger clinical trials. Gal-3 levels were determined in 232 NYHA III–IV chronic HF patients enrolled in the Deventer-Alkmaar HF (DEAL-HF) study, who were then followed up for a period of 6.5 years (Lok et al. 2010). Baseline Gal-3 (cutoff: 17.6 ng/ml) predicted all-cause mortality after adjustment for age, gender, creatinine clearance, and NT-proBNP. By dichotomizing the population according to NT-proBNP and Gal-3 levels, the authors also demonstrated an additive prognostic power for Gal-3, since patients with elevation of both biomarkers had a 1.5- to 2-fold higher mortality rate compared to patients in other subgroups. In a larger population of 895 chronic HF patients from the HF-ACTION (Heart Failure: A Controlled Trial Investigating Outcomes of Exercise TraiNing) study with LVEF <35%, Gal-3 lost its univariate prognostic value in predicting the composite outcome of all-cause death or re-hospitalization, when corrected for peak oxygen consumption at cardiopulmonary test or NT-proBNP (Felker et al. 2012).
Despite this wide amount of data confirming its prognostic role in HF, there is still limited information on whether Gal-3 assay may help in adjusting therapeutical strategies. Current knowledge is indeed limited to a benefit from statin therapy in patients with chronic HF of ischemic cause and low Gal-3 level (Gullestad et al. 2012) and to the lack of power in predicting response to mineralocorticoid receptor antagonists or to cardiac resynchronization therapy (Gandhi et al. 2015; Lopez-Andrès et al. 2012).
Recently, measurement of Gal-3 has received a class IIb recommendation in acute decompensated (level of evidence A) and in chronic (level of evidence B) HF for risk stratification purposes in the 2013 ACCF/AHA Guideline for the Management of Heart Failure (Yancy et al. 2013).
sST2
Suppression of tumorigenicity 2 protein (ST2) is a member of the Toll-like/interleukin-1 receptor superfamily, which is expressed together with its ligand interleukin-33 (IL-33) following myocardial stretch and cardiovascular injury. The IL-33/ST2 interaction exerts positive effects in terms of blunting prohypertrophic and profibrotic signals (Kakkar and Lee 2008; Pascual-Figal and Januzzi 2015; Yancy et al. 2013). Indeed, the transmembrane receptor for IL-33 (ST2 ligand, ST2L) is one of ST2 isoforms. Among others, a soluble isoform of ST2 exists, sST2, arising from a dual-promoter system driving differential mRNA expression. There is evidence that sST2 may act as a decoy receptor competing with ST2L for IL-33 binding. For example, administration of IL-33 to cultured rat neonatal cardiomyocytes inhibited the prohypertrophic signals of angiotensin II or phenylephrine, these effects being reversed by sST2 (Sanada et al. 2007). Reflecting these experimental evidences, serum levels of sST2 have been associated to LV systolic function and remodeling, as well as to a more decompensated hemodynamic profile (Shah et al. 2009). Of interest, sST2 concentration does not appear to be influenced by age, kidney function, or body mass index, unlike natriuretic peptides (Dieplinger et al. 2009b).
sST2 assay has been tested for diagnostic and prognostic purposes in either acute or chronic HF populations. Data from the ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) study have shown higher sST2 concentration in subjects with acute HF compared to those with dyspnea of non-cardiac origin (Januzzi et al. 2007). In the same cohort, sST2 was reported to be the best predictor of 1-year death, outperforming NT-proBNP (hazard ratios equal to 4.6 and 2.3, respectively) (Januzzi et al. 2010). Interestingly, in a population of acute HF patients, most of them with LV systolic dysfunction, sST2 provided additional prognostic value over NT-proBNP in the prediction of death, even in subset with lower NT-proBNP (Rehman et al. 2008). Fewer studies have explored the prognostic value of sST2 in chronic HF. In a well-treated subset of patients enrolled in the HF-ACTION trial, with LVEF <35%, ST2 was only modestly associated with functional capacity while it was significantly associated with outcomes (death or hospitalization, cardiovascular death or HF hospitalization, and all-cause mortality). In the larger study in chronic HF patients, a post hoc analysis of the Val-HeFT, baseline sST2 levels added significant information to the Cox regression model of first morbid events composed of 23 clinical variables including NT-proBNP and the treatment allocation (Anand et al. 2014). In the same study, sST2 values were also available at 4 and 12 months and patients randomized to the valsartan arm showed a milder increase in sST2 over time compared to those assigned to placebo. Further, sST2 was the only circulating biomarker, in an analysis including also growth differentiation factor-15 (GDF-15) and hs-TnT to add prognostic information to baseline concentration and to predict the occurrence of reverse remodeling when serially tested in chronic systolic HF patients (Gaggin et al. 2014). Based on these data, and on the association of neurohormonal antagonism therapy with lower sST2 concentrations, sST2 is particularly promising as a tool for patient monitoring and therapeutic optimization (Januzzi et al. 2015). Further, as for Gal-3, sST2 measurement has received a class IIb recommendation in acute decompensated (level of evidence A) and in chronic (level of evidence B) HF for risk stratification purposes in the latest American guidelines (Yancy et al. 2013).
2.5.5 Cardiorenal Syndrome
Renal impairment and worsening renal function are very common in HF, and represent a key element in disease pathophysiology, thus constituting an aspect of the clinical spectrum of HF – configuring the so-called cardiorenal syndrome – rather than a mere comorbidity. In this view, the clinical utility of both markers of renal function and of renal damage has been tested in HF patients. Although kidney dysfunction generally reflects a loss of glomerular filtration rate (GFR), it is participated by alteration in renal hemodynamics, sodium and water retention, and glomerular and tubulo-interstitial function. Biomarkers have been proposed (and tested) in HF settings to investigate each of these aspects.
Chronic kidney disease, as assessed by either GFR or serum creatinine, is strongly associated with a worse outcome in HF patients (Dries et al. 2000; Hillege et al. 2000). Worsening renal function is also frequent in HF, sometimes associated with the initiation of RAAS-acting therapy. This phenomenon, termed “pseudo-worsening renal function,” is likely to have scarce effects on prognosis and may be associated with beneficial effects of ACE inhibitors in patients with LV systolic dysfunction (Clark et al. 2014; van Veldhuisen et al. 2015). Cystatin C is a small (13 kDa) protein produced by all nucleated cells, filtered and then catabolized by tubular cells, that can be considered an alternative tool to estimate renal function. A prognostic value has been demonstrated for cystatin C in chronic HF population (Damman et al. 2012) but it has never been used as a guide for HF treatment yet.
Albuminuria and proteinuria both reflect loss of integrity and damage to the glomerular membrane. Analyses from >2000 patients with chronic HF enrolled in the GISSI-HF study have shown an increasing mortality rate in subjects with normal albumin excretion, microalbuminuria or albuminuria, even after adjustment for other clinical risk factors (Masson et al. 2010b), with additive prognostic properties over GFR (Damman et al. 2011).
Some markers of tubular damage, including neutrophil-gelatinase-associated lipocalin (NGAL), kidney injury molecule (KIM)-1, and N-acetyl β-(d)-glucosaminidase (NAG), have been used for (early) detection of acute kidney injury. NGAL is a siderophore-binding protein expressed by various epithelial cells which is over-expressed in kidney injury and can be dosed in either serum or urine. Serum NGAL may be of help for prediction of acute kidney injury and in risk stratification in acute HF (Aghel et al. 2010; Maisel et al. 2011b). In patients with chronic HFrEF enrolled in the CORONA study, plasma NGAL did not add significant prognostic information when included in a model with NT-proBNP and GFR (Nymo et al. 2012). Also KIM-1 and NAG are increased in chronic HFrEF and may provide clinical aid in the prediction of worsening renal function in HF, while solid evidences on their prognostic value are still lacking (Jungbauer et al. 2011).
2.5.6 Comorbidities and Cachexia
HF is a systemic syndrome and peripheral organ dysfunction may either contribute to the disease onset and progression or represent a consequence of primitive cardiac abnormalities.
Thyroid hormones are crucial for cardiovascular homeostasis and even subclinical alteration of thyroid function is associated with worsened outcome in HF patients, independently from natriuretic peptides (Passino et al. 2009). Low-triiodothyronine syndrome is a recognized entity in HFrEF but, despite some promising results from animal studies and small-scale supplementation trials, general recommendation is still lacking (Gerdes and Iervasi 2010). Among hematologic conditions, anemia is prevalent in acute and chronic HF and low hemoglobin levels hold significant prognostic value, additive to NT-proBNP (Baggish et al. 2007). Further, ferritin and transferrin saturation assessment is of key importance to identify subgroups of patients with iron deficiency, which is coming up as a therapeutical target in patients with HFrEF, as confirmed in a recent meta-analysis (Qian et al. 2016).
Cachexia and wasting frequently develop in later stages of HF, as a consequence of a complex interplay among (neuro)hormonal, immune, inflammatory dysregulation and anabolic/catabolic imbalance. Ghrelin and adiponectin are peptide hormones involved in energy balance, and are both increased in cachectic chronic HF patients. Some evidence exists that adiponectin predicts mortality in systolic HF and that treatment with the beta-blocker carvedilol decreases circulating levels of adiponectin (Tsutamoto et al. 2007; Yamaji et al. 2009).
2.5.7 Adrenomedullin
Adrenomedullin (ADM) is a peptide hormone acting as a potent vasodilator expressed by all human tissues. Circulating ADM is increased in HF and correlates with disease severity. Nonetheless, ADM is highly unstable and, recently, a novel assay measuring the mid-region of the more stable prohormone (MR-proADM) has been developed, with similar behavior in HF patients (Shah et al. 2012). Prognostic value of ADM has been tested in a cohort of 297 patients with HFrEF of ischemic origin. In this study ADM predicted the risk of mortality and of HF hospitalization independently from other clinical variables (Richards et al. 2001). Interestingly, an interaction with carvedilol therapy was reported in the same paper.
2.5.8 GDF-15
Growth differentiation factor 15 (GDF15) is a member of the TGF-ß cytokine superfamily which is highly expressed during inflammatory stress. GDF circulating levels are increased in HF patients and correlate with the extent of myocardial fibrosis (Lok et al. 2012). Both baseline and repeated measurements of GDF-15 have additional prognostic value over hsTnT and NT-proBNP in patients with HFrEF (Chan et al. 2016). In an analysis from the Val-HeFT study, an independent, although weak, predictive value of GDF-15 for all-cause mortality was also shown, with GDF-15 levels increasing over time independently from the assignment to the placebo or the valsartan arm (Anand et al. 2010).
2.5.9 Copeptin
Arginine vasopressin (AVP), also known as antidiuretic hormone, is involved in the regulation of free water clearance, plasma osmolality, and vasomotricity. It is known since a long time that circulating AVP is elevated in HF settings (Goldsmith et al. 1983), but its assay is challenging. Copeptin, the c-terminal segment of the precursor of provasopressin, is a reliable surrogate marker for AVP and has been proved to independently predict mortality in acute HF, especially in subsets with hyponatremia (Maisel et al. 2011c). In 195 patients with chronic HFrEF, copeptin predicted 5-year all-cause mortality, although with poor additive prognostic accuracy over NT-proBNP (IDI 9.3%, NRI 8.2%) (Pozsonyi et al. 2015).
2.5.10 miRNAs
MicroRNAs (miRNAs) are non-coding RNAs which are involved in different cell processes by repressing messenger RNA translation. miRNAs have been shown to participate in several pathophysiological processes related to heart failure, including cardiac fibrosis and hypertrophy. Several circulating miRNAs have been tested for diagnostic and prognostic purposes either in acute or in chronic HF (Vegter et al. 2016). For example, Tijsen has reported that miR-423-5p is differentially expressed between HF patients, healthy controls, and patients with dyspnea of non-cardiac origin (Tijsen et al. 2010). In a small cohort of patients with chronic HF, miR-126 and miR-508-5p are associated with cardiovascular death in subsets with ischemic and non-ischemic HF, respectively (Qiang et al. 2013). Interestingly, there is experimental evidence that circulating miRNAs fluctuate in response to pharmacological HF treatment (e.g., by ACE inhibitors) and that miRNAs may represent, themselves, a therapeutical target (Vegter et al. 2016).
3 Biomarkers of Heart Failure with Mid-Range and Preserved Ejection Fraction
Among HF patients, a significant proportion exists presenting with preserved or only slightly impaired EF, especially in the elderly population. As mentioned above, these clinical entities have been defined as HFpEF and as HFmrEF in the latest European guidelines for the management of acute and chronic HF. Although specific EF cutoff has been proposed in these recommendations, in previous studies different definitions of “preserved” EF have been considered, ranging from 40 to 55%. There is therefore consistent overlap among HFpEF and HFmrEF; thus we will consider them on a whole in the following section.
Independent from its definition, HFpEF is associated with high rates of morbidity and mortality both in ambulatory and in-hospital settings, comparable to HFrEF (Senni et al. 2014). Nonetheless, while in the last few decades, several pharmacological and non-pharmacological approaches have been validated for HFrEF, up to now no single intervention has been demonstrated to modify the clinical course of HFpEF, possibly due to a consistent phenotypic variability and to the enrolment of heterogeneous population in large clinical trials (Butler et al. 2014). Different pathophysiological mechanisms indeed underlie the development of the clinical syndrome of HFpEF and the role of comorbidities is likely more relevant than in HFrEF. In the effort toward individualization that is therefore required for the management of HFpEF, circulating biomarkers – tracking specific damage pathways – may represent fundamental tools.
3.1 Natriuretic Peptides
As discussed above, natriuretic peptides are the cornerstone biomarkers in HFrEF. Nonetheless, their clinical value has been demonstrated across the whole spectrum of LV systolic function. Although to a lower extent as compared to patients with more severe reduction in EF, both BNP and NT-proBNP are increased and are key elements in the diagnosis of HFpEF. Moreover, their levels increase with more severe cardiac morphological and functional abnormalities (including hypertrophy, fibrosis, and diastolic dysfunction) (Tschope et al. 2005). Still, a clear cutoff does not exist to distinguish HFpEF from HFrEF (Parekh and Maisel 2009; van Veldhuisen et al. 2013). Further, prognostic properties of BNP are maintained independently from the extent of LV dysfunction, since, for a given BNP level, the risk of death and HF hospitalization of patients with HFpEF is as poor as in those with reduced LVEF (van Veldhuisen et al. 2013). The prognostic value of NT-proBNP has also emerged in HFpEF patients (defined as LVEF ≥45%) from the i-PRESERVE study, showing that baseline (proposed cutoff 339 pg/mL) and changes in NT-proBNP improve the prediction of mortality and HF re-hospitalization (Anand et al. 2011; Jhund et al. 2015).
As for the case of HFrEF, circulating levels of natriuretic peptides are influenced by several cardiac and extra-cardiac conditions (including female sex and advanced age), which is even more important in HFpEF, given the high prevalence of comorbidities. For example, a fivefold increase in NT-proBNP has been reported in subjects with HFpEF and atrial fibrillation, compared to those in sinus rhythm (McKelvie et al. 2010); likewise, renal function has been reported to significantly influence natriuretic peptide concentration (McCullough et al. 2003).
A few studies have specifically explored the effectiveness of a natriuretic peptide-guided therapy in HFpEF. Maeder and colleagues enrolled 123 patients with HF and LVEF >45%, who were randomized to medical therapy titrated to reduce symptoms to NYHA ≤ II or also to reduce NT-proBNP below the inclusion threshold (>400 or >800 ng/L depending on age). Differently from patients with HFrEF, NT-proBNP-guided management tended to worsen 18-month outcomes in HFpEF (Maeder et al. 2013), thus questioning the clinical benefit of such approach, as later confirmed in a recent individual patient meta-analysis (Brunner-La Rocca et al. 2015).
3.2 Other Biomarkers in HFpEF
As mentioned before, HFrEF and HFpEF are likely sustained by a different pathophysiology, thus explaining the variable response to pharmacological and non-pharmacological treatment. Analyses of data from the Trial of Intensified versus standard medical therapy in elderly patients with congestive heart failure (TIME-CHF) have shown a different circulating biomarker profile in patients with LVEF ≤40% (n = 458) vs. those with LVEF ≥50% (n = 112). After adjustment for other clinical variables accounting for heterogeneity between populations, patients with HFpEF displayed significantly higher levels of sST2, hs-CRP, and cystatin-C. On the other hand, HFrEF patients presented higher NT-proBNP, hs-TnT, and hemoglobin (Sanders-van Wijk et al. 2015). These results suggest that markers of myocardial damage and loading are activated in HFrEF, while elevation of biomarkers of inflammation and fibrosis characterizes HFpEF.
3.2.1 sST2
Among markers of inflammation and fibrosis, sST2 seems to be promising in the clinical management of HFpEF. First data came from a prognostic study showing that sST2, although not correlating with echocardiographic indices of diastolic function, was the only biohumoral marker predicting mortality in 200 patients with dyspnea and normal LV systolic function (Shah et al. 2011). These data have been confirmed in further studies, demonstrating that prognostic value of sST2 in HFpEF was comparable to that in HFrEF, especially in acute settings (Manzano-Fernández et al. 2011).
3.2.2 Gal-3
Gal-3 has also been mechanistically involved in the proceses of cardiovascular inflammation and fibroblast proliferation and fibrosis, which are thought to be at play in the development of HFpEF. In 2011 de Boer has shown that in HFpEF patients from the Coordinating study evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) (with LVEF >40%), Gal-3 appeared to have a particularly strong predictive value, compared to HFrEF patients (de Boer et al. 2011). Gal-3 also yielded significant reclassification indices in one of the largest biomarker studies in HFpEF so far, conducted in a cohort of 419 HF patients with LVEF >45% (Carrasco-Sánchez et al. 2013). The Aldo-DHF trial explored the effects of spironolactone 25 mg vs. placebo in chronic HFpEF patients. Gal-3 was associated with functional performance and quality of life, and its increase in serial measurements predicted all-cause death or hospitalization independently from NT-proBNP. However, no specific interaction between treatment arm and Gal-3 levels could be observed (Edelmann et al. 2015).
3.2.3 GDF-15
As previously discussed, GDF-15 is a marker of cell injury and inflammation that has been shown to circulate in higher concentrations in patients with HFpEF compared to controls (Stahrenberg et al. 2010). Diagnostic and prognostic properties have been advocated for GDF-15 in HFpEF. For example, the NT-proBNP/GDF-15 ratio has been shown to properly distinguish between HFpEF and HFrEF (AUC 0.709) (Santhanakrishnan et al. 2012); further, higher GDF-15 is associated with increased risk of death and HF hospitalization in HFpEF patients, providing additional prognostic information over hsTnT and NT-proBNP (Chan et al. 2016). Although not conclusive, these data strongly support a putative role of GDF-15 – both a determinant and marker of risk – as a useful tool for HFpEF management, as well as a possible therapeutical target (Putko et al. 2014a, b).
3.2.4 Inflammatory Biomarkers
Activation of pro-inflammatory pathways is a fundamental element in HFpEF pathophysiology (Paulus 2000). Elevated levels of inflammatory cytokines, such as TNF-α, IL1, IL6, IL8, and CRP, are often observed in HFpEF patient; interestingly, circulating levels of TNF-α receptors (TNFR1 and TNFR2) are associated with the severity of diastolic dysfunction and of symptoms (Putko et al. 2014a, b). Still, scarce evidence on their prognostic role is currently available.
3.2.5 Directions
Other biomarkers have been tested for the management of HFpEF in the past years, yielding different (in some case promising) results. For example, ADM levels have been correlated to diastolic dysfunction (Yu et al. 2001), and MR-proADM, which is also emerging in HFrEF, may help in identifying new-onset HFpEF (Brouwers et al. 2014). Von Willebrand factor has been shown to additive prognostic value over NT-proBNP in 457 patients with HFpEF enrolled in the LUdwigshafen Risk and Cardiovascular Health (LURIC) study (Kleber et al. 2015). In a small study, no significant difference in microRNA levels was identified between HFrEF and HFpEF.
RAAS activation is associated with most of the pathophysiological mechanisms leading to cardiac phenotypes commonly observed in HFpEF, including hypertrophy, apoptosis, and fibrosis; therefore, from a theoretical standpoint, biomarkers of RAAS should provide useful information for disease management and, possibly, for therapeutic optimization. Two trials, Aldo-DHF and TOPCAT, have investigated the effects of spironolactone in HFpEF patients showing no significant effect on outcome, despite a beneficial effect on diastolic function (Edelmann et al. 2013; Pitt et al. 2014). Also LCZ696 has been demonstrated to reduce left atrial volume in HFpEF (Solomon et al. 2012), but its prognostic effect is still under investigation in the phase III PARAGON-HF trial.
4 Conclusions
BNP and NT-proBNP have first demonstrated how biomarkers can dramatically influence the everyday management of HF patients, providing information to the clinician far exceeding initial expectations. Despite recent advances, HF still remains a syndrome with unacceptable morbidity and mortality, possibly reflecting a complex pathophysiology and an extremely heterogeneous presentation which is only partly counterbalanced by a “one-size-fits-all” therapeutic strategy. Novel biomarkers addressing specific disease phenotypes and paths of damage will be of help for treatment tailoring and to move toward a more rational use of drugs and devices in HF. Research has recently focused on the clinical value of Gal-3 and sST2, which are both markers and effectors of cardiovascular damage, but currently, still there is no clear indication for therapeutic driving or optimization based on circulating levels of such biomarkers and, more generally, on a single HF biomarker.
For prognostic purposes, it seems reasonable that the use of multiple markers reflecting the activation of different pathophysiological pathways may more accurately identify high-risk subjects. This hypothesis has been recently tested, for example, in a large cohort of decompensated HF patients who were tested for several (novel) HF biomarkers. Elevation of at least three among MR-proADM, hs-TnT, combined free light chains, hsCRP, and sST2 provided incremental prognostic value when added to a multivariable model including BNP (NRI 32.5%) (Jackson et al. 2016). Nonetheless, the feasibility and the cost-effectiveness of multimarker strategies remain to be elucidated.
During the last years, a growing number of biomarkers have been proposed as potentially useful in HF patients, but no one of them still resembles the characteristics of the “ideal biomarker.” A single marker will hardly perform for screening, diagnostic, prognostic, and therapeutic management purposes; therefore, a rational use of biomarkers will likely contemplate different analytes for different purposes. Moreover, the pathophysiological and clinical significance of biomarkers may depend on the presentation, stage, and severity of the disease (e.g., on etiology, presence/extent of LV systolic dysfunction, comorbidities). In this view, one could envisage specific sets of biomarker with different performances in HFpEF, HFmrEF, and HFrEF, especially as concerns prediction of the future course of the disease and of LV adverse/reverse remodeling.
Biomarkers are likely the most promising tools to make a step toward individualized therapy in HF. In the next future, a lot will depend on the quality (even more than on results) of clinical studies aimed at improving current diagnostic and prediction models and of studies using biomarkers to tailor therapeutics.
References
Aghel A, Shrestha K, Mullens W, Borowski A, Tang WH (2010) Serum neutrophil gelatinase-associated lipocalin (NGAL) in predicting worsening renal function in acute decompensated heart failure. J Card Fail 16:49–54
Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP, Glazer RD, Tognoni G, Cohn JN (2003) Val-HeFT Investigators. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation 107:1278–1283
Anand IS, Latini R, Florea VG, Kuskowski MA, Rector T, Masson S, Signorini S, Mocarelli P, Hester A, Glazer R, Cohn JN, Val-HeFT Investigators (2005) C-reactive protein in heart failure: prognostic value and the effect of valsartan. Circulation 112:1428–1434
Anand IS, Kempf T, Rector TS, Tapken H, Allhoff T, Jantzen F, Kuskowski M, Cohn JN, Drexler H, Wollert KC (2010) Serial measurement of growth-differentiation factor-15 in heart failure: relation to disease severity and prognosis in the Valsartan Heart Failure Trial. Circulation 122:1387–1395
Anand IS, Rector TS, Cleland JG et al (2011) Prognostic value of baseline plasma amino-terminal pro-brain natriuretic peptide and its interactions with irbesartan treatment effects in patients with heart failure and preserved ejection fraction: findings from the I-PRESERVE trial. Circ Heart Fail 4:569–577
Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN (2014) Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 7:418–426
Baggish AL, van Kimmenade R, Bayes-Genis A, Davis M, Lainchbury JG, Frampton C, Pinto Y, Richards MA, Januzzi JL (2007) Hemoglobin and N-terminal pro-brain natriuretic peptide: independent and synergistic predictors of mortality in patients with acute heart failure. Results from the International Collaborative of NT-proBNP (ICON) Study. Clin Chim Acta 381:145–150
Berry C, Murphy NF, De Vito G, Galloway S, Seed A, Fisher C, Sattar N, Vallance P, Hillis WS, McMurray J (2007) Effects of aldosterone receptor blockade in patients with mild-moderate heart failure taking a beta-blocker. Eur J Heart Fail 9:429–434
Bleske BE, Nicklas JM, Bard RL, Brook RD, Gurbel PA, Bliden KP, Rajagopalan S, Pitt B (2006) Neutral effect on markers of heart failure, inflammation, endothelial activation and function, and vagal tone after high-dose HMG-CoA reductase inhibition in non-diabetic patients with non-ischemic cardiomyopathy and average low-density lipoprotein level. J Am Coll Cardiol 47:338–341
Braunwald E (2008) Biomarkers in heart failure. N Engl J Med 358:2148–2159
Braunwald E (2013) Heart failure. J Am Coll Cardiol 1:1–20
Brouwers FP, van Gilst WH, Damman K, van den Berg MP, Gansevoort RT, Bakker SJ, Hillege HL, van Veldhuisen DJ, van der Harst P, de Boer RA (2014) Clinical risk stratification optimizes value of biomarkers to predict new-onset heart failure in a community-based cohort. Circ Heart Fail 7:723–731
Brunner-La Rocca HP, Eurlings L, Richards AM, Januzzi JL, Pfisterer ME, Dahlström U, Pinto YM, Karlström P, Erntell H, Berger R, Persson H, O’Connor CM, Moertl D, Gaggin HK, Frampton CM, Nicholls MG, Troughton RW (2015) Which heart failure patients profit from natriuretic peptide guided therapy? A meta-analysis from individual patient data of randomized trials. Eur J Heart Fail 17:1252–1261
Butler J, Fonarow GC, Zile MR, Lam CS, Roessig L, Schelbert EB, Shah SJ, Ahmed A, Bonow RO, Cleland JG, Cody RJ, Chioncel O, Collins SP, Dunnmon P, Filippatos G, Lefkowitz MP, Marti CN, McMurray JJ, Misselwitz F, Nodari S, O’Connor C, Pfeffer MA, Pieske B, Pitt B, Rosano G, Sabbah HN, Senni M, Solomon SD, Stockbridge N, Teerlink JR, Georgiopoulou VV, Gheorghiade M (2014) Developing therapies for heart failure with preserved ejection fraction: current state and future directions. JACC Heart Fail 2:97–112
Cabassi A, de Champlain J, Maggiore U, Parenti E, Coghi P, Vicini V, Tedeschi S, Cremaschi E, Binno S, Rocco R, Bonali S, Bianconcini M, Guerra C, Folesani G, Montanari A, Regolisti G, Fiaccadori E (2013) Prealbumin improves death risk prediction of BNP-added Seattle Heart Failure Model: results from a pilot study in elderly chronic heart failure patients. Int J Cardiol 168:3334–3339
Carrasco-Sánchez FJ, Aramburu-Bodas O, Salamanca-Bautista P, Morales-Rull JL, Galisteo-Almeda L, Páez-Rubio MI, Arias-Jiménez JL, Aguayo-Canela M, Pérez-Calvo JI (2013) Predictive value of serum galectin-3 levels in patients with acute heart failure with preserved ejection fraction. Int J Cardiol 169:177–182
Chan MM, Santhanakrishnan R, Chong JP, Chen Z, Tai BC, Liew OW, Ng TP, Ling LH, Sim D, Leong KT, Yeo PS, Ong HY, Jaufeerally F, Wong RC, Chai P, Low AF, Richards AM, Lam CS (2016) Growth differentiation factor 15 in heart failure with preserved vs reduced ejection fraction. Eur J Heart Fail 18:81–88
Chung ES, Packer M, Lo KH, Fasanmade AA, Willerson JT (2003) Anti-TNF Therapy Against Congestive Heart Failure Investigators. Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: results of the anti-TNF Therapy Against Congestive Heart Failure (ATTACH) trial. Circulation 107:3133–3140
Clark H, Krum H, Hopper I (2014) Worsening renal function during renin-angiotensin-aldosterone system inhibitor initiation and long-term outcomes in patients with left ventricular systolic dysfunction. Eur J Heart Fail 16:41–48
Clerico A, Emdin M (2004) Diagnostic accuracy and prognostic relevance of the measurement of cardiac natriuretic peptides: a review. Clin Chem 50:33–50
Clerico A, Recchia FA, Passino C, Emdin M. Cardiac endocrine function is an essential component of the homeostatic regulation network: physiological and clinical implications (2006) Am J Physiol Heart Circ Physiol 290:H17–29
Cohen-Solal A, Logeart D, Huang B, Cai D, Nieminen MS, Mebazaa A (2009) Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is associated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 53:2343–2348
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311:819–823
Damman K, Masson S, Hillege HL, Maggioni AP, Voors AA, Opasich C, van Veldhuisen DJ, Montagna L, Cosmi F, Tognoni G, Tavazzi L, Latini R (2011) Clinical outcome of renal tubular damage in chronic heart failure. Eur Heart J 32:2705–2712
Damman K, van der Harst P, Smilde TD, Voors AA, Navis G, van Veldhuisen DJ, Hillege HL (2012) Use of cystatin C levels in estimating renal function and prognosis in patients with chronic systolic heart failure. Heart 98:319–324
Davis ME, Richards AM, Nicholls MG, Yandle TG, Frampton CM, Troughton RW (2006) Introduction of metoprolol increases plasma B-type cardiac natriuretic peptides in mild, stable heart failure. Circulation 113:977–985
de Bold AJ, Borenstein HB, Veress AT, Sonnenberg H (1981) A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci 28:89–94
de Boer RA, Voors AA, Muntendam P, van Gilst WH, van Veldhuisen DJ (2009) Galectin-3: a novel mediator of heart failure development and progression. Eur J Heart Fail 11:811–817
de Boer RA, Lok DJ, Jaarsma T et al (2011) Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann Med 43:60–68
Dieplinger B, Gegenhuber A, Struck J, Poelz W, Langsteger W, Haltmayer M, Mueller T (2009a) Chromogranin A and C-terminal endothelin-1 precursor fragment add independent prognostic information to amino-terminal proBNP in patients with acute destabilized heart failure. Clin Chim Acta 400:91–96
Dieplinger B, Januzzi JL Jr, Steinmair M, Gabriel C, Poelz W, Haltmayer M, Mueller T (2009b) Analytical and clinical evaluation of a novel high-sensitivity assay for measurement of soluble ST2 in human plasma--the Presage ST2 assay. Clin Chim Acta 409:33–40
Don-Wauchope AC, McKelvie RS (2015) Evidence based application of BNP/NT-proBNP testing in heart failure. Clin Biochem 48:236–246
Doust JA, Pietrzak E, Dobson A, Glasziou P (2005) How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ 330:625
Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW (2000) The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 35:681–689
Edelmann F, Wachter R, Schmidt AG, Kraigher-Krainer E, Colantonio C, Kamke W, Duvinage A, Stahrenberg R, Durstewitz K, Löffler M, Düngen HD, Tschöpe C, Herrmann-Lingen C, Halle M, Hasenfuss G, Gelbrich G, Pieske B, Aldo-DHF Investigators (2013) Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA 309:781–791
Edelmann F, Holzendorf V, Wachter R, Nolte K, Schmidt AG, Kraigher-Krainer E, Duvinage A, Unkelbach I, Düngen HD, Tschöpe C, Herrmann-Lingen C, Halle M, Hasenfuss G, Gelbrich G, Stough WG, Pieske BM (2015) Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 17:214–223
Emdin M, Passino C, Prontera C, Iervasi A, Ripoli A, Masini S, Zucchelli GC, Clerico A (2004) Cardiac natriuretic hormones, neuro-hormones, thyroid hormones and cytokines in normal subjects and patients with heart failure. Clin Chem Lab Med 42:627–636
Emdin M, Vittorini S, Passino C, Clerico A (2009) Old and new biomarkers of heart failure. Eur J Heart Fail 11:331–335
Farmakis D, Parissis JT, Bistola V, Paraskevaidis IA, Iliodromitis EK, Filippatos G, Kremastinos DT (2010) Plasma B-type natriuretic peptide reduction predicts long-term response to levosimendan therapy in acutely decompensated chronic heart failure. Int J Cardiol 139:75–79
Felker GM, Hasselblad V, Hernandez AF, O’Connor CM (2009) Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials. Am Heart J 158:422–430
Felker GM, Fiuzat M, Shaw LK, Clare R, Whellan DJ, Bettari L, Shirolkar SC, Donahue M, Kitzman DW, Zannad F, Piña IL, O’Connor CM (2012) Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 5:72–78
Felker GM, Mentz RJ, Teerlink JR, Voors AA, Pang PS, Ponikowski P, Greenberg BH, Filippatos G, Davison BA, Cotter G, Prescott MF, Hua TA, Lopez-Pintado S, Severin T, Metra M (2015) Serial high sensitivity cardiac troponin T measurement in acute heart failure: insights from the RELAX-AHF study. Eur J Heart Fail 17:1262–1270
Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M, ADHERE Scientific Advisory Committee and Investigators (2007) Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 49:1943–1950
Fruhwald FM, Fahrleitner-Pammer A, Berger R, Leyva F, Freemantle N, Erdmann E, Gras D, Kappenberger L, Tavazzi L, Daubert JC, Cleland JG (2007) Early and sustained effects of cardiac resynchronization therapy on N-terminal pro-B-type natriuretic peptide in patients with moderate to severe heart failure and cardiac dyssynchrony. Eur Heart J 28:1592–1597
Gaggin HK, Januzzi JL Jr (2013) Biomarkers and diagnostics in heart failure. Biochim Biophys Acta 1832:2442–2450
Gaggin HK, Szymonifka J, Bhardwaj A, Belcher A, De Berardinis B, Motiwala S, Wang TJ, Januzzi JL Jr (2014) Head-to-head comparison of serial soluble ST2, growth differentiation factor-15, and highly-sensitive troponin T measurements in patients with chronic heart failure. JACC Heart Fail 2:65–72
Gandhi PU, Motiwala SR, Belcher AM, Gaggin HK, Weiner RB, Baggish AL, Fiuzat M, Brunner-La Rocca HP, Januzzi JL Jr (2015) Galectin-3 and mineralocorticoid receptor antagonist use in patients with chronic heart failure due to left ventricular systolic dysfunction. Am Heart J 169:404–411
Gerdes AM, Iervasi G (2010) Thyroid replacement therapy and heart failure. Circulation 122:385–393
Goldsmith SR, Francis GS, Cowley AW Jr, Levine TB, Cohn JN (1983) Increased plasma arginine vasopressin levels in patients with congestive heart failure. J Am Coll Cardiol 1:1385–1390
Group BDW (2001) Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 69(89–95)
Güder G, Bauersachs J, Frantz S, Weismann D, Allolio B, Ertl G, Angermann CE, Störk S (2007) Complementary and incremental mortality risk prediction by cortisol and aldosterone in chronic heart failure. Circulation 115:1754–1761
Gullestad L, Ueland T, Kjekshus J, Nymo SH, Hulthe J, Muntendam P, Adourian A, Böhm M, van Veldhuisen DJ, Komajda M, Cleland JG, Wikstrand J, McMurray JJ, Aukrust P, on behalf of the CORONA Study Group (2012) Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Eur Heart J 33:2290–2296
Henderson NC, Sethi T (2009) The regulation of inflammation by galectin-3. Immunol Rev 230:160–171
Hillege HL, Girbes AR, de Kam PJ, Boomsma F, De ZD, Charlesworth A, Hampton JR, van Veldhuisen DJ (2000) Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation 102:203–210
Horwich TB, Patel J, MacLellan WR, Fonarow GC (2003) Cardiac troponin I is associated with impaired hemodynamics, progressive left ventricular dysfunction, and increased mortality rates in advanced heart failure. Circulation 108:833–838
Jackson CE, Haig C, Welsh P, Dalzell JR, Tsorlalis IK, McConnachie A, Preiss D, Anker SD, Sattar N, Petrie MC, Gardner RS, McMurray JJ (2016) The incremental prognostic and clinical value of multiple novel biomarkers in heart failure. Eur J Heart Fail [Epub ahead of print]
Januzzi JL Jr, Camargo CA, Anwaruddin S et al (2005) The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol 95:948–954
Januzzi JL, van Kimmenade R, Lainchbury J, Bayes-Genis A, Ordonez-Llanos J, Santalo-Bel M, Pinto YM, Richards M (2006a) NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J 27:330–337
Januzzi JL Jr, Sakhuja R, O’donoghue M, Baggish AL, Anwaruddin S, Chae CU, Cameron R, Krauser DG, Tung R, Camargo CA Jr, Lloyd-Jones DM (2006b) Utility of amino-terminal pro-brain natriuretic peptide testing for prediction of 1-year mortality in patients with dyspnea treated in the emergency department. Arch Intern Med 166:315–320
Januzzi JL Jr, Peacock WF, Maisel AS, Chae CU, Jesse RL, Baggish AL, O’Donoghue M, Sakhuja R, Chen AA, van Kimmenade RR, Lewandrowski KB, Lloyd-Jones DM, Wu AH (2007) Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 50:607–613
Januzzi JL Jr, Rehman S, Mueller T, van Kimmenade RR, Lloyd-Jones DM (2010) Importance of biomarkers for long-term mortality prediction in acutely dyspneic patients. Clin Chem 56:1814–1821
Januzzi JL Jr, Rehman SU, Mohammed AA, Bhardwaj A, Barajas L, Barajas J, Kim HN, Baggish AL, Weiner RB, Chen-Tournoux A, Marshall JE, Moore SA, Carlson WD, Lewis GD, Shin J, Sullivan D, Parks K, Wang TJ, Gregory SA, Uthamalingam S, Semigran MJ (2011) Use of amino-terminal pro-B-type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 58:1881–1889
Januzzi JL Jr, Maisel AS, Silver M, Xue Y, DeFilippi C (2012) Natriuretic peptide testing for predicting adverse events following heart failure hospitalization. Congest Heart Fail 18(Suppl 1):S9–S13
Januzzi JL, Pascual-Figal D, Daniels LB (2015) ST2 testing for chronic heart failure therapy monitoring: the International ST2 Consensus Panel. Am J Cardiol 115(7 Suppl):70B–75B
Jhund PS, Anand IS, Komajda M et al (2015) Changes in N-terminal pro-B-type natriuretic peptide levels and outcomes in heart failure with preserved ejection fraction: an analysis of the I-Preserve study. Eur J Heart Fail 17:809–817
Jourdain P, Jondeau G, Funck F, Gueffet P, Le Helloco A, Donal E, Aupetit JF, Aumont MC, Galinier M, Eicher JC, Cohen-Solal A, Juillière Y (2007) Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol 49:1733–1739
Jungbauer CG, Birner C, Jung B, Buchner S, Lubnow M, von Bary C, Endemann D, Banas B, Mack M, Boger CA, Riegger G, Luchner A (2011) Kidney injury molecule-1 and N-acetyl-beta-D-glucosaminidase in chronic heart failure: possible biomarkers of cardiorenal syndrome. Eur J Heart Fail 13:1104–1110
Kakkar R, Lee RT (2008) The IL-33/ST2 pathway: therapeutic target and novel biomarker. Nat Rev Drug Discov 7:827–840
Kim HN, Januzzi JL Jr (2010) Biomarkers in the management of heart failure. Curr Treat Options Cardiovasc Med 12:519–531
Kleber ME, Koller L, Goliasch G, Sulzgruber P, Scharnagl H, Silbernagel G, Grammer TB, Delgado G, Tomaschitz A, Pilz S, März W, Von NA (2015) Willebrand factor improves risk prediction in addition to N-terminal pro-B-type natriuretic peptide in patients referred to coronary angiography and signs and symptoms of heart failure and preserved ejection fraction. Circ Heart Fail 8:25–32
Kociol RD, Horton JR, Fonarow GC, Reyes EM, Shaw LK, O’Connor CM, Felker GM, Hernandez AF (2011) Admission, discharge, or change in B-type natriuretic peptide and long-term outcomes: data from Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) linked to Medicare claims. Circ Heart Fail 4:628–636
Kühl U, Noutsias M, Seeberg B, Schultheiss HP (1996) Immunohistological evidence for a chronic intramyocardial inflammatory process in dilated cardiomyopathy. Heart 75:295–300
Lainchbury JG, Troughton RW, Strangman KM, Frampton CM, Pilbrow A, Yandle TG, Hamid AK, Nicholls MG, Richards AM (2009) N-terminal pro-B-type natriuretic peptide-guided treatment for chronic heart failure: results from the BATTLESCARRED (NT-proBNP-Assisted Treatment To Lessen Serial Cardiac Readmissions and Death) trial. J Am Coll Cardiol 55:53–60
Latini R, Masson S, Anand I, Judd D, Maggioni AP, Chiang YT, Bevilacqua M, Salio M, Cardano P, Dunselman PH, Holwerda NJ, Tognoni G, Cohn JN, Valsartan Heart Failure Trial Investigators (2002) Effects of valsartan on circulating brain natriuretic peptide and norepinephrine in symptomatic chronic heart failure: the Valsartan Heart Failure Trial (Val-HeFT). Circulation 106:2454–2458
Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, Angelici L, Barlera S, Parrinello G, Maggioni AP, Tognoni G, Cohn JN, Val-HeFT Investigators (2007) Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 116:1242–1249
Lee AF, MacFadyen RJ, Struthers AD (1999) Neurohormonal reactivation in heart failure patients on chronic ACE inhibitor therapy: a longitudinal study. Eur J Heart Fail 1:401–406
Leimbach WN, Wallin BG, Victor RG, Alyward PE, Sundlof G, Mark AL (1986) Direct evidence from intraneural recordings for increased central sympathetic outflow in patients with heart failure. Circulation 73:913–919
Lim PO, MacFadyen RJ, Struthers AD (2000) Is there a role for renin profiling in selecting chronic heart failure patients for ACE inhibitor treatment? Heart 83:257–261
Lin YH, Lin LY, Wu YW, Chien KL, Lee CM, Hsu RB, Chao CL, Wang SS, Hsein YC, Liao LC, Ho YL, Chen MF (2009) The relationship between serum galectin-3 and serum markers of cardiac extracellular matrix turnover in heart failure patients. Clin Chim Acta 409:96–99
Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN (2010) HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail 16:e1–e194
Lippi G, Sanchis-Gomar F (2016) Monitoring B-type natriuretic peptide in patients undergoing therapy with neprilysin inhibitors. An emerging challenge? Int J Cardiol 219:111–114
Lok DJ, Van Der Meer P, de la Porte PW, Lipsic E, Van Wijngaarden J, Hillege HL, van Veldhuisen DJ (2010) Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 99:323–328
Lok SI, Winkens B, Goldschmeding R, van Geffen AJ, Nous FM, van Kuik J, van der Weide P, Klöpping C, Kirkels JH, Lahpor JR, Doevendans PA, de Jonge N, de Weger RA (2012) Circulating growth differentiation factor-15 correlates with myocardial fibrosis in patients with non-ischaemic dilated cardiomyopathy and decreases rapidly after left ventricular assist device support. Eur J Heart Fail 14:1249–1256
Lopez-Andrès N, Rossignol P, Iraqi W, Fay R, Nuée J, Ghio S, Cleland JG, Zannad F, Lacolley P (2012) Association of galectin-3 and fibrosis markers with long-term cardiovascular outcomes in patients with heart failure, left ventricular dysfunction, and dyssynchrony: insights from the CARE-HF (Cardiac Resynchronization in Heart Failure) trial. Eur J Heart Fail 14:74–81
Lourenço P, Paulo Araújo J, Paulo C, Mascarenhas J, Friões F, Azevedo A, Bettencourt P (2010) Higher C-reactive protein predicts worse prognosis in acute heart failure only in noninfected patients. Clin Cardiol 33:708–714
Maeder MT, Rickenbacher P, Rickli H, Abbühl H, Gutmann M, Erne P, Vuilliomenet A, Peter M, Pfisterer M, Brunner-La Rocca HP, TIME-CHF Investigators (2013) N-terminal pro brain natriuretic peptide-guided management in patients with heart failure and preserved ejection fraction: findings from the Trial of Intensified versus standard medical therapy in elderly patients with congestive heart failure (TIME-CHF). Eur J Heart Fail 15:1148–1156
Maisel AS, Krishnaswamy P, Nowak RM, et al., Breathing Not Properly Multinational Study Investigators (2002) Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347:161–167
Maisel A, Mueller C, Nowak RM, Peacock WF, Ponikowski P, Mockel M, Hogan C, Wu AH, Richards M, Clopton P, Filippatos GS, Di Somma S, Anand I, Ng LL, Daniels LB, Neath SX, Christenson R, Potocki M, McCord J, Hartmann O, Morgenthaler NG, Anker SD (2011a) Midregion prohormone adrenomedullin and prognosis in patients presenting with acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol 58:1057–1067
Maisel AS, Mueller C, Fitzgerald R, Brikhan R, Hiestand BC, Iqbal N, Clopton P, van Veldhuisen DJ (2011b) Prognostic utility of plasma neutrophil gelatinase-associated lipocalin in patients with acute heart failure: the NGAL EvaLuation Along with B-type NaTriuretic Peptide in acutely decompensated heart failure (GALLANT) trial. Eur J Heart Fail 13:846–851
Maisel A, Xue Y, Shah K, Mueller C, Nowak R, Peacock WF, Ponikowski P, Mockel M, Hogan C, Wu AH, Richards M, Clopton P, Filippatos GS, Di Somma S, Anand IS, Ng L, Daniels LB, Neath SX, Christenson R, Potocki M, McCord J, Terracciano G, Kremastinos D, Hartmann O, von Haehling S, Bergmann A, Morgenthaler NG, Anker SD (2011c) Increased 90-day mortality in patients with acute heart failure with elevated copeptin: secondary results from the Biomarkers in Acute Heart Failure (BACH) study. Circ Heart Fail 4:613–620
Mann DL (2015) Innate immunity and the failing heart: the cytokine hypothesis revisited. Circ Res 116:1254–1268
Mann DL, McMurray JJ, Packer M, Swedberg K, Borer JS, Colucci WS, Djian J, Drexler H, Feldman A, Kober L, Krum H, Liu P, Nieminen M, Tavazzi L, van Veldhuisen DJ, Waldenstrom A, Warren M, Westheim A, Zannad F, Fleming T (2004) Targeted anticytokine therapy in patients with chronic heart failure: results of the Randomized Etanercept Worldwide Evaluation (RENEWAL). Circulation 109:1594–1602
Manzano-Fernández S, Mueller T, Pascual-Figal D, Truong QA, Januzzi JL (2011) Usefulness of soluble concentrations of interleukin family member ST2 as predictor of mortality in patients with acutely decompensated heart failure relative to left ventricular ejection fraction. Am J Cardiol 107:259–267
Masson S, Latini R, Anand IS, Vago T, Angelici L, Barlera S, Missov ED, Clerico A, Tognoni G, Cohn JN, Val-HeFT Investigators (2006) Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: the Valsartan Heart Failure (Val-HeFT) data. Clin Chem 52:1528–1538
Masson S, Latini R, Anand IS, Barlera S, Angelici L, Vago T, Tognoni G, Cohn JN, Val-HeFT Investigators (2008) Prognostic value of changes in N-terminal pro-brain natriuretic peptide in Val-HeFT (Valsartan Heart Failure Trial). J Am Coll Cardiol 52:997–1003
Masson S, Latini R, Carbonieri E, Moretti L, Rossi MG, Ciricugno S, Milani V, Marchioli R, Struck J, Bergmann A, Maggioni AP, Tognoni G, Tavazzi L, GISSI-HF Investigators (2010a) The predictive value of stable precursor fragments of vasoactive peptides in patients with chronic heart failure: data from the GISSI-heart failure (GISSI-HF) trial. Eur J Heart Fail 12:338–347
Masson S, Latini R, Milani V, Moretti L, Rossi MG, Carbonieri E, Frisinghelli A, Minneci C, Valisi M, Maggioni AP, Marchioli R, Tognoni G, Tavazzi L, GISSI-HF Investigators (2010b) Prevalence and prognostic value of elevated urinary albumin excretion in patients with chronic heart failure: data from the GISSI-Heart Failure trial. Circ Heart Fail 3:65–72
Masson S, Anand I, Favero C, Barlera S, Vago T, Bertocchi F, Maggioni AP, Tavazzi L, Tognoni G, Cohn JN, Latini R, Valsartan Heart Failure Trial (Val-HeFT), Gruppo Italiano per lo Studio della Sopravvivenza nell’Insufficienza Cardiaca–Heart Failure (GISSI-HF) Investigators (2012) Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 125:280–288
McCullough PA, Duc P, Omland T, McCord J, Nowak RM, Hollander JE, Herrmann HC, Steg PG, Westheim A, Knudsen CW, Storrow AB, Abraham WT, Lamba S, Wu AH, Perez A, Clopton P, Krishnaswamy P, Kazanegra R, Maisel AS, Breathing Not Properly Multinational Study Investigators (2003) B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis 41:571–579
McGeechan K, Macaskill P, Irwig L, Liew G, Wong TY (2008) Assessing new biomarkers and predictive models for use in clinical practice: a clinician’s guide. Arch Intern Med 168:2304–2310
McKelvie RS, Komajda M, McMurray J et al (2010) Baseline plasma NT-proBNP and clinical characteristics: results from the irbesartan in heart failure with preserved ejection fraction trial. J Card Fail 16:128–134
McMurray JJ, Kjekshus J, Gullestad L, Dunselman P, Hjalmarson A, Wedel H, Lindberg M, Waagstein F, Grande P, Hradec J, Kamenský G, Korewicki J, Kuusi T, Mach F, Ranjith N, Wikstrand J, CORONA Study Group (2009) Effects of statin therapy according to plasma high-sensitivity C-reactive protein concentration in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA): a retrospective analysis. Circulation 120:2188–2196
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, PARADIGM-HF Investigators and Committees (2014) Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371:993–1004
Moertl D, Berger R, Struck J, Gleiss A, Hammer A, Morgenthaler NG, Bergmann A, Huelsmann M, Pacher R (2009) Comparison of midregional pro-atrial and B-type natriuretic peptides in chronic heart failure: influencing factors, detection of left ventricular systolic dysfunction, and prediction of death. J Am Coll Cardiol 53:1783–1790
Motiwala SR, Januzzi JL (2013) The role of natriuretic peptides as biomarkers for guiding the management of chronic heart failure. Clin Pharmacol Ther 93:57–67
Nymo SH, Ueland T, Askevold ET, Flo TH, Kjekshus J, Hulthe J, Wikstrand J, McMurray J, Van Veldhuisen DJ, Gullestad L, Aukrust P, Yndestad A (2012) The association between neutrophil gelatinase-associated lipocalin and clinical outcome in chronic heart failure: results from CORONA*. J Intern Med 271:436–443
Packer M, McMurray JJ, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile M, Andersen K, Arango JL, Arnold JM, Bělohlávek J, Böhm M, Boytsov S, Burgess LJ, Cabrera W, Calvo C, Chen CH, Dukat A, Duarte YC, Erglis A, Fu M, Gomez E, Gonzàlez-Medina A, Hagège AA, Huang J, Katova T, Kiatchoosakun S, Kim KS, Kozan Ö, Llamas EB, Martinez F, Merkely B, Mendoza I, Mosterd A, Negrusz-Kawecka M, Peuhkurinen K, Ramires FJ, Refsgaard J, Rosenthal A, Senni M, Sibulo AS Jr, Silva-Cardoso J, Squire IB, Starling RC, Teerlink JR, Vanhaecke J, Vinereanu D, Wong RC, PARADIGM-HF Investigators and Coordinators (2015) Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation 131:54–61
Palazzuoli A, Pellegrini M, Ruocco G, Martini G, Franci B, Campagna MS, Gilleman M, Nuti R, McCullough PA, Ronco C (2014) Continuous versus bolus intermittent loop diuretic infusion in acutely decompensated heart failure: a prospective randomized trial. Crit Care 18:R134
Pankow K, Wang Y, Gembardt F, Krause E, Sun X, Krause G, Schultheiss HP, Siems WE, Walther T (2007) Successive action of meprin A and neprilysin catabolizes B-type natriuretic peptide. Circ Res 101:875–882
Parekh N, Maisel AS (2009) Utility of B-natriuretic peptide in the evaluation of left ventricular diastolic function and diastolic heart failure. Curr Opin Cardiol 24:155–160
Parikh NI, Vasan RS (2007) Assessing the clinical utility of biomarkers in medicine. Biomark Med 1:419–436
Pascual-Figal DA, Januzzi JL (2015) The biology of ST2: the International ST2 Consensus Panel. Am J Cardiol 115:3B–7B
Passino C, Severino S, Poletti R, Piepoli MF, Mammini C, Clerico A, Gabutti A, Nassi G, Emdin M (2006) Aerobic training decreases B-type natriuretic peptide expression and adrenergic activation in patients with heart failure. J Am Coll Cardiol 47:1835–1839
Passino C, Poletti R, Fontana M, Vergaro G, Prontera C, Gabutti A, Giannoni A, Emdin M, Clerico A (2008) Clinical relevance of non-cardiac determinants of natriuretic peptide levels. Clin Chem Lab Med 46:1515–1523
Passino C, Pingitore A, Landi P, Fontana M, Zyw L, Clerico A, Emdin M, Iervasi G (2009) Prognostic value of combined measurement of brain natriuretic peptide and triiodothyronine in heart failure. J Card Fail 15:35–40
Paulus WJ (2000) Cytokines and heart failure. Heart Fail Monit 1:50–56
Peacock WF 4th, De Marco T, Fonarow GC, Diercks D, Wynne J, Apple FS, Wu AH, ADHERE Investigators (2008) Cardiac troponin and outcome in acute heart failure. N Engl J Med 358:2117–2126
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172
Pencina MJ, D’Agostino RB, Vasan RS (2010) Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med 48:1703–1711
Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, Rickenbacher P, Vuillomenet A, Jeker U, Dubach P, Beer H, Yoon SI, Suter T, Osterhues HH, Schieber MM, Hilti P, Schindler R, Brunner-La Rocca HP, TIME-CHF Investigators (2009) BNP-guided vs symptom-guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA 301:383–392
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Harty B, Heitner JF, Kenwood CT, Lewis EF, O’Meara E, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, Yang S, McKinlay SM, TOPCAT Investigators (2014) Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 370:1383–1392
Poletti R, Vergaro G, Zyw L, Prontera C, Passino C, Emdin M (2013) Prognostic value of plasma renin activity in heart failure patients with chronic kidney disease. Int J Cardiol 167:711–715
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force Members, Document Reviewers (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18:891–975
Pozsonyi Z, Förhécz Z, Gombos T, Karádi I, Jánoskuti L, Prohászka Z (2015) Copeptin (C-terminal pro arginine-vasopressin) is an independent long-term prognostic marker in heart failure with reduced ejection fraction. Heart Lung Circ 24:359–367
Pruett AE, Lee AK, Patterson JH, Schwartz TA, Glotzer JM, Adams KF Jr (2015) Evolution of biomarker guided therapy for heart failure: current concepts and trial evidence. Curr Cardiol Rev 11:80–89
Putko BN, Yogasundaram H, Oudit GY (2014a) The harbinger of mortality in heart failure with preserved ejection fraction: do GDF-15 levels reflect tandem, deterministic effects of fibrosis and inflammation? Can J Cardiol 30:264–266
Putko BN, Wang Z, Lo J, Anderson T, Becher H, Dyck JR, Kassiri Z, Oudit GY, Alberta HEART Investigators (2014b) Circulating levels of tumor necrosis factor-alpha receptor 2 are increased in heart failure with preserved ejection fraction relative to heart failure with reduced ejection fraction: evidence for a divergence in pathophysiology. PLoS One 9, e99495
Qian C, Wei B, Ding J, Wu H, Wang Y (2016) The efficacy and safety of iron supplementation in patients with heart failure and iron deficiency: a systematic review and meta-analysis. Can J Cardiol 32:151–159
Qiang L, Hong L, Ningfu W, Huaihong C, Jing W (2013) Expression of miR-126 and miR-508-5p in endothelial progenitor cells is associated with the prognosis of chronic heart failure patients. Int J Cardiol 168:2082–2088
Rehman SU, Mueller T, Januzzi JL Jr (2008) Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 52:1458–1465
Richards AM (2008) Serial measurements of plasma B-type natriuretic peptides: what do they tell us? J Am Coll Cardiol 52:1004–1005
Richards AM, Doughty R, Nicholls MG, MacMahon S, Sharpe N, Murphy J, Espiner EA, Frampton C, Yandle TG, Australia-New Zealand Heart Failure Group (2001) Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: prognostic utility and prediction of benefit from carvedilol in chronic ischemic left ventricular dysfunction Australia-New Zealand Heart Failure Group. J Am Coll Cardiol 37:1781–1787
Rosenberg J, Gustafsson F, Remme WJ, Riegger GA, Hildebrandt PR (2008) Effect of beta-blockade and ACE inhibition on B-type natriuretic peptides in stable patients with systolic heart failure. Cardiovasc Drugs Ther 22:305–311
Røsjø H, Masson S, Latini R, Flyvbjerg A, Milani V, La Rovere MT, Revera M, Mezzani A, Tognoni G, Tavazzi L, Omland T, GISSI-HF Investigators (2010) Prognostic value of chromogranin A in chronic heart failure: data from the GISSI-Heart Failure trial. Eur J Heart Fail 12:549–556
Rousseau MF, Gurné O, Duprez D, Van Mieghem W, Robert A, Ahn S, Galanti L, Ketelslegers JM, Belgian RALES Investigators (2002) Beneficial neurohormonal profile of spironolactone in severe congestive heart failure: results from the RALES neurohormonal substudy. J Am Coll Cardiol 40:1596–1601
Sanada S et al (2007) IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 117:1538–1549
Sanders-van Wijk S, van Empel V, Davarzani N, Maeder MT, Handschin R, Pfisterer ME, Brunner-La Rocca HP, TIME-CHF Investigators (2015) Circulating biomarkers of distinct pathophysiological pathways in heart failure with preserved vs reduced left ventricular ejection fraction. Eur J Heart Fail 17:1006–1014
Santhanakrishnan R, Chong JP, Ng TP, Ling LH, Sim D, Leong KT, Yeo PS, Ong HY, Jaufeerally F, Wong R, Chai P, Low AF, Richards AM, Lam CS (2012) Growth differentiation factor 15, ST2, high-sensitivity troponin T, and N-terminal pro brain natriuretic peptide in heart failure with preserved vs reduced ejection fraction. Eur J Heart Fail 14:1338–1347
Semenov AG, Katrukha AG (2016) Different susceptibility of B-type natriuretic peptide (BNP) and BNP precursor (proBNP) to cleavage by neprilysin: the N-terminal part does matter. Clin Chem 62:617–622
Senni M, Gavazzi A, Oliva F, Mortara A, Urso R, Pozzoli M, Metra M, Lucci D, Gonzini L, Cirrincione V, Montagna L, Di Lenarda A, Maggioni AP, Tavazzi L, IN HF Outcome Investigators (2014) In-hospital and 1-year outcomes of acute heart failure patients according to presentation (de novo vs. worsening) and ejection fraction. Results from IN-HF Outcome Registry. Int J Cardiol 173:163–169
Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL (2009) Serum levels of the interleukin-1 receptor family member ST2, cardiac structure and function, and long-term mortality in patients with acute dyspnea. Circ Heart Fail 2:311–319
Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL (2010) Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 12:826–832
Shah KB, Kop WJ, Christenson RH, Diercks DB, Henderson S, Hanson K, Li SY, de Filippi CR (2011) Prognostic utility of ST2 in patients with acute dyspnea and preserved left ventricular ejection fraction. Clin Chem 57:874–882
Shah RV, Truong QA, Gaggin HK, Pfannkuche J, Hartmann O, Januzzi JL Jr (2012) Mid-regional pro-atrial natriuretic peptide and pro-adrenomedullin testing for the diagnostic and prognostic evaluation of patients with acute dyspnoea. Eur Heart J 33:2197–2205
Sola S, Mir MQ, Lerakis S, Tandon N, Khan BV (2006) Atorvastatin improves left ventricular systolic function and serum markers of inflammation in nonischemic heart failure. J Am Coll Cardiol 47:332–337
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, Shi V, Bransford T, Takeuchi M, Gong J, Lefkowitz M, Packer M, McMurray JJ, Prospective comparison of ARNI with ARB on Management Of heart failUre with preserved ejectioN fracTion (PARAMOUNT) Investigators (2012) The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet 380:1387–1395
Stahrenberg R, Edelmann F, Mende M, Kockskämper A, Düngen HD, Lüers C, Binder L, Herrmann-Lingen C, Gelbrich G, Hasenfuss G, Pieske B, Wachter R (2010) The novel biomarker growth differentiation factor 15 in heart failure with normal ejection fraction. Eur J Heart Fail 12:1309–1316
Tijsen AJ, Creemers EE, Moerland PD, de Windt LJ, van der Wal AC, Kok WE, Pinto YM (2010) MiR423-5p as a circulating biomarker for heart failure. Circ Res 106:1035–1039
Tota B, Angelone T, Cerra MC (2014) The surging role of Chromogranin A in cardiovascular homeostasis. Front Chem 2:64
Troughton RW, Frampton CM, Yandle TG et al (2000) Treatment of heart failure guided by plasma amino-terminal brain natriuretic peptide (N-BNP) concentrations. Lancet 355:1126–1130
Tschope C, Kasner M, Westermann D, Gaub R, Poller WC, Schultheiss HP (2005) The role of NT- proBNP in the diagnostics of isolated diastolic dysfunction: correlation with echocardiographic and invasive measurements. Eur Heart J 26:2277–2284
Tsutamoto T, Tanaka T, Sakai H, Ishikawa C, Fujii M, Yamamoto T, Horie M (2007) Total and high molecular weight adiponectin, haemodynamics, and mortality in patients with chronic heart failure. Eur Heart J 28:1723–1730
van Kimmenade RR, Januzzi JL Jr, Ellinor PT, Sharma UC, Bakker JA, Low AF, Martinez A, Crijns HJ, MacRae CA, Menheere PP, Pinto YM (2006) Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 48:1217–1224
van Kimmenade RR, Pinto YM, Januzzi JL Jr (2008) Importance and interpretation of intermediate (gray zone) amino-terminal pro-B-type natriuretic peptide concentrations. Am J Cardiol 101:39–42
van Veldhuisen DJ, Linssen GC, Jaarsma T, van Gilst WH, Hoes AW, Tijssen JG, Paulus WJ, Voors AA, Hillege HL (2013) B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J Am Coll Cardiol 61:1498–1506
van Veldhuisen DJ, Ruilope LM, Maisel AS, Damman K (2015) Biomarkers of renal injury and function: diagnostic, prognostic and therapeutic implications in heart failure. Eur Heart J pii: ehv588 [Epub ahead of print]
Vanderheyden M, Bartunek J, Goethals M, Verstreken S, Lambeir AM, De Meester I, Scharpé S (2009) Dipeptidyl-peptidase IV and B-type natriuretic peptide. From bench to bedside. Clin Chem Lab Med 47:248–252
Vasan RS (2006) Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation 113:2335–2362
Vegter EL, van der Meer P, de Windt LJ, Pinto YM, Voors AA (2016) MicroRNAs in heart failure: from biomarker to target for therapy. Eur J Heart Fail 18:457–468
Vergaro G, Emdin M, Iervasi A, Zyw L, Gabutti A, Poletti R, Mammini C, Giannoni A, Fontana M, Passino C (2011) Prognostic value of plasma renin activity in heart failure. Am J Cardiol 108:246–251
Vergaro G, Prud’homme M, Fazal L, Merval R, Passino C, Emdin M, Samuel JL, Cohen Solal A, Delcayre C (2016) Inhibition of galectin-3 pathway prevents isoproterenol-induced left ventricular dysfunction and fibrosis in mice. Hypertension 67:606–612
Wright SP, Doughty RN, Pearl A, Gamble GD, Whalley GA, Walsh HJ, Gordon G, Bagg W, Oxenham H, Yandle T, Richards M, Sharpe N (2003) Plasma amino-terminal pro-brain natriuretic peptide and accuracy of heart-failure diagnosis in primary care: a randomized, controlled trial. J Am Coll Cardiol 42:1793–1800
Xue Y, Clopton P, Peacock WF, Maisel AS (2011) Serial changes in high-sensitive troponin I predict outcome in patients with decompensated heart failure. Eur J Heart Fail 13:37–42
Yamaji M, Tsutamoto T, Tanaka T, Kawahara C, Nishiyama K, Yamamoto T, Fujii M, Horie M (2009) Effect of carvedilol on plasma adiponectin concentration in patients with chronic heart failure. Circ J 73:1067–1073
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(e147–239)
Yu CM, Cheung BM, Leung R, Wang Q, Lai WH, Lau CP (2001) Increase in plasma adrenomedullin in patients with heart failure characterized by diastolic dysfunction. Heart 86:155–160
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Senni, M., D’Elia, E., Emdin, M., Vergaro, G. (2016). Biomarkers of Heart Failure with Preserved and Reduced Ejection Fraction. In: Bauersachs, J., Butler, J., Sandner, P. (eds) Heart Failure. Handbook of Experimental Pharmacology, vol 243. Springer, Cham. https://doi.org/10.1007/164_2016_86
Download citation
DOI: https://doi.org/10.1007/164_2016_86
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59658-7
Online ISBN: 978-3-319-59659-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)