Abstract
Purpose of Review
Today, statins are the first choice to lower LDL cholesterol and concomitantly the risk of atherosclerotic cardiovascular disease. There is a significant minority of statin-treated patients who are more susceptible to occasionally serious side effects that may increase morbidity and lead to compliance problems or the discontinuation of therapy. This review addresses the question of whether genetics can provide meaningful insights into the risk of statin side effects or therapy success.
Recent Findings
The use of genome-wide association studies has significantly reduced the number of predictive genetic markers for statin effects, and the isolated effect of the surviving markers is low; more promising are approaches to stratify patients with genetic risk scores.
Summary
Patients reveal a pronounced individual response to the administration of statins. The idea of being able to adequately describe this variability with single genetic markers has failed, genetic risk scores will be the method of choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When I began my research in a lipid laboratory nearly a quarter-century ago, patients were usually classified by their phenotype according to Fredrickson [1]. LDL-C levels of > 160 mg/dL were classified as high-risk LDL-C, those of 130 to 159 mg/dL as borderline-high-risk LDL-C, and those of < 130 mg/dL as desirable LDL-C [2]. Since then, we have entered the time of genomics with the option to sequence entire genomes; statins are first-line medication to lower LDL-C, with additional options like ezetimibe or PCSK9 inhibitors. Relying on LDL-C, the target is now heterogeneous: (a) the ACC/AHA guidelines abandoned the idea of absolute target levels and recommend high-intensity statin treatment to reduce LDL-C levels by ≥ 50% in patients with manifest atherosclerotic disease or high estimated risk, and to reduce LDL-C levels by 30–50% in patients with moderate risk [3], (b) the ESC/EAS task force recommends a target < 70 mg/dL for secondary prevention [4], (c) whereas the first organization in the USA has gone down to < 55 mg/dL for patients at extreme risk (e.g., progressive atherosclerotic cardiovascular disease including unstable angina in patients after achieving an LDL-C < 70 mg/dL) [5]. After the success of IMPROVE-IT [6] and FOURIER [7], the recommendation is inclining towards “the lower the better”, meaning that more patients will undergo high-intensity statin treatment.
Not only have scientific background, methodology, and treatment options changed in recent decades, the communication between patients, doctors, and interest groups also differs. The development of social media has opened channels for everyone to express her/his opinions that are frequently not based on scientific evidence but rather driven by fear or self-interest. Statins’ side effects are exaggerated, causing insecure patients to discontinue their medication. Lethal effects of the influence of disinformation are impressively demonstrated in a publication from Denmark [8]. Sune Nielsen and Borge Nordestgaard studied all individuals initiated on statin therapy from 1995 through 2010 in the entire Danish population (674,900), and followed them until 31 December 2011 for myocardial infarction and death from cardiovascular disease. Statin-related disinformation was associated with a significant increase in statin discontinuation. In line with strong evidence [9], the early discontinuation of statin therapy was associated with increased risk of myocardial infarction and death from cardiovascular disease [8].
The main adverse reactions to statin treatment include myalgia, myotoxicity, and new onset of diabetes (NOD). Statin-associated muscle symptoms (SAMS) are by far the most common adverse effects and one of the key reasons for discontinuing statin therapy. The management of statin intolerance is not the focus of this review, but it has been addressed in a very recent review by Peter Toth and colleagues [10•].
SAMS and Statin Drug-Drug Interactions
Before starting statin therapy, what can we do to identify those patients most likely to suffer from these considerable side effects? First, we must consider potential drug interactions. Thompson et al. [11] reported that approximately 60% of cases of rhabdomyolysis under a statin are associated with drug-drug interactions involving statin metabolism modification. A prominent example in the recent past is cerivastatin’s withdrawal from the world market due to a high rate of fatal rhabdomyolysis in patients who had been taking the full dose of cerivastatin (0.8 mg/day) and gemfibrozil concomitantly [12]. Two years ago, the American Heart Association published a comprehensive scientific statement listing the most important statin-drug interactions [13••]. In addition to describing the effects of combination therapies on the drug levels of common statins, the article also includes dosage recommendations for planned combinations, focusing on cardiovascular disease.
The importance of considering statins’ interactions with other drugs is impressively demonstrated by very recent work by Deljehier et al. [14]. They report on a 51-year-old patient with a severe case of rhabdomyolysis. He was on 80 mg of atorvastatin once a day when admitted to their care, having previously taken systemic fusidic acid (500 mg three times a day) and ofloxacin for osteitis. A comprehensive literature review added 29 case reports of rhabdomyolysis after combination therapies involving statins and systemic fusidic acid: 28% of those patients did not survive. Seeking another source, namely the WHO ViGiBASE, Deljehier et al. identified another 182 cases, revealing a 24% mortality rate. Their observations led the authors to conclude that there is substantial risk of developing rhabdomyolysis after a relatively long duration of combined statin and fusidic acid treatment, with a high mortality rate between 24 and 28%. If there is no alternative to fusidic acid, the authors suggest discontinuing the use of statins for the duration of the fusidic acid treatment and re-starting them 1 week after the end of fusidic acid therapy.
SAMS and Pharmacogenetics of Statins
Initial candidate genes for statin pharmacogenetics and SAMS were genes involved in the transport, metabolism, and clearance of statins. The most prominent example for this group is the solute carrier organic anion transporter family member 1B1 (SLCO1B1 or OATP1B1), which is expressed on the sinusoidal membrane of human hepatocytes and facilitates the hepatic uptake of many endogenous compounds such as bile acids, bilirubin, steroid hormone conjugates, and of drugs like rifampicin, cyclosporine, and most statins. Several polymorphisms in the gene encoding SLCO1B1, SLCO1B1, have been identified. Some of them, in particular c.521C > T (Val174Ala; rs4149056), are associated with reduced SLCO1B1 activity in vitro and markedly increased plasma concentrations of statins. Whereas the SLCO1B1 521C variant has only a minor effect on the lipid-lowering potency of statins in vivo, it is associated with an increased risk to develop statin myopathy. Heterozygous carriers of the genetic variant exhibit a 4.5-fold and homozygous carriers a 17-fold higher risk of myopathy taking 80 mg of simvastatin daily (for review see Reference [15]). In 2011, the U.S. Food and Drug Administration added warnings to the simvastatin product label to recommend against initiating simvastatin at 80 mg/day due to the risk of myopathy. As a consequence, prescribing recommendations for simvastatin have been established that are based on myopathy-risk categories (low, intermediate, or high) defined by SLCO1B1 genotype [16]. An ongoing trial (NCT02871934) enrolling 400 statin-naïve primary care patients will determine whether a genetic test for this genotype can help patients and providers choose the right type and dose of cholesterol-lowering statin medications to lower the risk of cardiovascular disease, while minimizing the muscle pain side effects that sometimes occur with statins. In the meantime, the possibility to switch to other generic statins possessing higher potency diminishes the need to screen patients for this polymorphism prior to treatment.
Other candidate genes involved in the pharmacokinetics of statins that might promote the development of SMAS are ABCB1 (rs1128503, rs2032582, rs1045642), encoding a transport protein responsible for hepato-biliary and renal–urinary transport of statins and their metabolites, and several cytochrome P450 genes like CYP3A (CYP3A4*22, rs35599367; CYP3A5*3, rs776746) [15]. Candidate genes associated with SAMS, which might be directly involved in the pathophysiology of SAMS are COQ2 (rs4693075 and rs4693570) encoding an enzyme involved in the biosynthesis of coenzyme Q10 and GATM (variant rs9806699) which encodes the rate-limiting enzyme glycine amidinotransferase in the creatine biosynthesis pathway [15]. In contrast to the SLCO1B1 genotype, the data on all these genes are inconsistent and require further evaluation. Last year, a new gene appeared as following a classical candidate-gene approach, namely the leukocyte immunoglobulin-like receptor subfamily-B (LILRB5) [17]. The missense variant Asp247Gly (rs12975366) is associated with lower creatine phosphokinase and lactate dehydrogenase levels, both biomarkers for muscle injury. The authors analyzed the impact of the variant on statin intolerance defined by two phenotypes in the GoDARTS cohort, and replicated their results in three independent studies looking for statin-induced myopathy (SIM) and myalgia (CPRD-STAGE SIM, PREDICTION-ADR SIM, JUPITER myalgia). Homozygous carriers of the Asp247 genotype carry a higher risk for all analyzed outcomes (OR1.34; 95% CI: 1.16–1.54). Of course, those findings will need to be confirmed by further investigations. The direct involvement of LILRB5 in the development of muscle pathology is unclear, but there might be a link to the immune system. It would come as no surprise if other genes from the immune system were revealed in our search for the cause of SAMS.
Statins and NOD
The increased risk of contracting diabetes while on statin treatment has long been overlooked. The JUPITER trial, a double-blind randomized primary prevention study of 17,802 subjects assigned to rosuvastatin 20 mg or placebo, was the first to report the increased incidence of diabetes (27%) with statins [18]. Various meta-analyses of randomized control trials supported this observation, demonstrating a greater risk of NOD associated with statins ranging from 9 to 13%, suggesting a dose-related effect. Patients at increased risk tended to be older, had higher BMI, higher fasting blood-glucose levels, higher triglycerides, and metabolic syndrome at baseline—all established diabetes risk factors [19]. A very recent meta-analysis focusing on observational studies instead of RCTs reported an even higher risk of 44%, varying from 38% in simvastatin users up to 61% in rosuvastatin users [20]. Pitavastatin, which this meta-analysis did not analyze, seems to be the only statin without a diabetogenic effect [21]. On the other hand, the follow-up in most pitavastatin studies was short. To close this gap, the LESS-DM trial will investigate the impact of 4 mg pitavastatin in comparison to 20 mg atorvastatin on the development of NOD in patients with metabolic syndrome with a 2-year follow-up [22].
Although the underlying cellular mechanisms have not been thoroughly evaluated, they range from effects on calcium channels in pancreatic ß-cells that control insulin secretion to the involvement of glucose transporter 4 (GLUT4) translocation and changes in intracellular signaling [23].
Over the last 3 years, several Mendelian randomization studies have demonstrated a direct connection between various genes involved in cholesterol metabolism and the risk of type 2 diabetes. In their cohort of over 220.000 individuals, Swerdlow et al. studied variants of the gene coding for the 3-hydroxy-methylglutaryl-CoA reductase (HMGCR), the target of the statins [24•]. They found that a common variant (rs17238484-G) responsible for lower LDL-C levels (2.3 mg/dL per allele) is associated with greater body weight and an approximately 5% higher risk for type 2 diabetes, mimicking the aforementioned association between statin usage and diabetes. Their results were confirmed by Ference et al. [25], who analyzed over 110,000 individuals. Instead of single SNP, they applied a genetic score that included six variants; they also analyzed the gene coding for PCSK9, thereby creating a score based on seven variants. Both variants in PCSK9 and HMGCR were associated with very similar effects on the increased risk of diabetes per unit decrease in LDL-C. They also found that these effects were independent and additive. The increased risk for diabetes appeared confined to persons with pathological fasting glucose levels [25]. Another study with more than 550,000 individuals and 51,623 cases of type 2 diabetes concentrated on variants in PCSK9 [26]. Schmidt et al. analyzed four independent PCSK9 variants (rs11583680, rs11591147, rs2479409, and rs11206510), and found an association between decreased LDL-C and increased fasting glucose, bodyweight, waist-to-hip ratio, and risk for type 2 diabetes. However, their results were dominated by the rarest variant, rs11591147 (minor allele frequency 0.01), which has the strongest influence on LDL-C. The genetic data on PCSK9 stands in contrast to the clinical trial data on PCSK9 inhibitors. The FOURIER trial investigators detected no differences between evolocumab and placebo in either NOD development or glycemic control [27]. Alirocumab delivered similar results in a pooled analysis of ten phase-III trials [28]. The PCSK9 inhibitor trials’ follow-ups were brief in comparison to the experiences with statins; therefore, it is too early to absolve the PCSK9 inhibitors. To close the circle of LDL-C lowering drugs, Lotta et al. analyzed variants in the gene NPC1L1 in > 300,000 individuals, coding for the molecular target of ezetimibe, NPC1 like intracellular cholesterol transporter 1 [29]. They confirmed previous findings concerning the increased diabetes risk for carriers of specific HMGCR and PCSK9 variants. For NPC1L1 they showed that LDL-C-lowering variants are associated with an odds ratio of 2.42 for type 2 diabetes per a genetically-predicted reduction of 1 mmol/L (38.7 mg/dL) in LDL-C. In contrast to the HMGCR locus and PCSK9 locus, they observed no significant association with glycemic or anthropometric parameters. Interestingly, when adjusted for a similar reduction in LDL-C, the association with type 2 diabetes differed by gene, implying different biochemical mechanisms. In contrast to LDL-C-lowering variants in HMGCR, PCSK9, and NPC1L1, patients with familial hypercholesterolemia carrying mutations in the genes for low density lipoprotein receptor (LDLR) or apolipoprotein B (APOB) reveal a significantly lower prevalence of type 2 diabetes than in their unaffected relatives (1.75 versus 2.93%) [30]. The authors also observed an inverse dose-response relationship between the severity of the mutation and prevalence of type 2 diabetes, being the lowest in LDLR-negative patients.
The sum of the genetic studies suggests that, regardless of the chosen means of reducing LDL-C by drugs, a slight increase in the diabetes risk is probable. Whether carriers of the above-mentioned variants carry a higher risk for NOD than non-carriers when taking LDL-C lowering drugs needs to be confirmed.
The risk for each individual must be carefully assessed so as to prevent whenever possible NOD, given that the risk of developing diabetes under a high-dose statin is minor, and their benefit so profound by reducing dramatically the number of cardiovascular events. The JUPITER trial showed that in patients with no major diabetes risk, > 84 events were prevented without their having contracted NOD following statin therapy, whereas in patients with diabetes risk factors, one will contract NOD while 2.5 cardiac events have been avoided [31]. Diabetic patients are not only characterized by their increased cardiovascular risk—they can also suffer other complications such as the need for additional drugs that can complicate drug adherence (a major problem in secondary prevention) and worse quality of life. Especially in high-risk patients, special attention is required to diet and lifestyle measures to reduce the NOD risk.
Pharmacogenetics of Statins: Effects on Lipid Lowering
As recently impressively demonstrated by an exome-wide association study in over 300,000 individuals, plasma lipids are affected by at least 250 loci [32•]. This is a broad field reflected in the numerous candidate genes for statin pharmacogenetics studied in the last 20 years, namely over 300. Most of those studies focused on genes related to lipid or drug metabolism, and the majority of the reported associations were not confirmed in independent investigations [33•]. Our review focuses on the most prominent candidates, confirmed by the latest genome-wide association studies, summarized in Table 1 [34, 35, 36••].
Apolipoprotein E is a ligand for several lipoprotein receptors and appears in three major phenotypes: apoE2, apoE3, and apoE4. These phenotypes are produced by APOE gene variants rs7412 (c.472C > T, Cys158Arg) and rs429358 (c.334 T > C, Cys112Arg). In comparison to the other phenotypes, apoE2 exhibits very weak binding affinity for the LDL receptor. This leads to greater hepatic cholesterol synthesis, which may predispose to more strongly inhibited cholesterol synthesis via statin treatment. In fact, the rare apoE2 allele (Cys112, Cys158) is associated with 4–6% greater LDL-C lowering than is the case in non-carriers [34, 35, 36••]. However, the apoE2 allele is associated with a lower off-statin LDL-C level, so the absolute reduction is smaller. LPA encodes for high polymorphic apolipoprotein (a), eponymous component of the LDL-like particle Lp(a). Lp(a) is an independent risk factor for cardiovascular disease and despite its similarity to LDL, cannot be lowered by statin therapy [37]. Nevertheless, SNP in LPA (rs10455872 and rs3798220) are associated with a lower statin-caused LDL-C reduction. This does not indicate a direct effect on LDL-C, but it does highlight weaknesses in the measurement of LDL-C. Both SNPs are closely associated with the plasma Lp(a) level, and because most LDL-C assays are incapable of sufficiently discriminating cholesterol residing in Lp(a) from that in LDL, the presence of higher Lp(a) levels attenuates the measured LDL-C response to statins. Two studies added loci at SORT1/CELSR2/PSRC1 (rs646776 and rs12740374) to the list [35, 36••]. SORT1 encodes the intracellularly-trafficking protein sortilin, which is involved in the metabolism of apoB-containing lipoproteins. The minor allele of rs646776 is preferentially associated with lower levels of small and very small LDL leading to approximately 1.5% greater LDL-C lowering in response to statins than non-carriers [36••].
Although the individual SNPs are robustly associated with the statin response, the small effect size limits their applicability.
Pharmacogenetics of Statins: Effects on Cardiovascular Risk Reduction
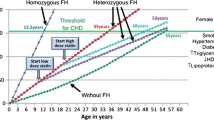
In many cases, the effects of individual variants are small and only lead to a phenotype when added up to arrive at a genetic risk score (GRS). This approach was used by Mega et al. in a re-analysis of primary (JUPITER/ASCOT) and secondary (CARE/PROVE IT-TIMI 22) statin prevention trials following risk stratification based on a GRS consisting of 27 SNPs associated with CAD [38••]. The sample size of 48,421 individuals with 3477 cardiac events was stratified into low, intermediate, and high GRS for CAD. Their study showed that statins reduced the absolute risk of CAD to a greater extent in individuals at higher than lower genetic risk. Correspondingly, the number needed to treat (NNT) to reduce CHD events via statin therapy differed according to the GRS. For example in JUPITER, the NNT to prevent one CHD event over 10 years for those individuals with low, intermediate, and high GRS was 66, 42, and 25. The interaction between cardiovascular risk and statin therapy was not because of greater LDL-C lowering among individuals with greater genetic risk or other potential clinical characteristics, as demonstrated in multivariate analysis [38••]. The result that people with a higher GRS benefit most from statin therapy was confirmed in another primary prevention study analysis namely, the WOSCOPS (West of Scotland Coronary Prevention Study), using an expanded GRS based on 57 SNPs [39•]. The high risk group exhibited a 44% risk reduction versus a relative risk reduction of 24% in others. The NNT to prevent one coronary event with statin therapy in the high risk group was 13 versus 38 among all others. The authors also analyzed the association between GRS and coronary artery calcification (Coronary Artery Risk Development in Young Adults – CARDIA, n = 1.154) and carotid artery plaque burden (BioImage, n = 4.392), showing an increased burden of atherosclerosis in both coronary and carotid arteries for those in the high risk group. They concluded that the association with a subclinical atherosclerosis burden may highlight a potential reason why those at high genetic risk derive enhanced clinical benefit from primary preventive statin therapy [39•]. Thus, stratifying by genetic risk appears to be a promising approach to identify a subset of patients who can derive the greatest benefit from statin therapy.
Conclusion
Reliable genetic markers for SAMS have been sought for many years, but the yield has been limited and has not really contributed to the predictive diagnostics of SAMS, perhaps with SLCO1B1 and simvastatin being the only exceptions. One reason for this is certainly the heterogeneity of the diagnoses and the low number of patients in the studies. The search for genetic markers may be the wrong path because it might be that individual and rare mutations are what characterize these patients, and not common variants [40]; thus, more focus should be targeted on metabolic markers that may better reflect anomalies in the muscles. The same applies to NOD. There is strong evidence that genetically-induced changes in LDL-C are associated with an increased risk of diabetes, but no predictive genetic markers exist for NOD. Here one should rely on the classical markers of glucose metabolism to identify patients at risk. Several genetic associations of variants in lipid-related genes and LDL-C lowering effect of statins have been described, but in general the effect is low in comparison to the LDL-C lowering capacity of statins, and it is questionable whether the analysis of single variants will improve clinical decision-making substantially. On the other hand, there is strong evidence that applying genetic risk scores is a good opportunity to assess a patient’s individual cardiovascular risk and to select those patients likely to benefit most from statin therapy. In this context, the study by Kera et al. [41••] is worth mentioning. Using a GRS of up to 50 SNPs in > 55,000 individuals to prospectively stratify them for their cardiovascular risk, the authors showed that a high risk score is not an unalterable fate. Of course, participants with a high genetic risk score had a significantly higher risk of cardiovascular events (91%), but a healthy lifestyle (no current smoking, no obesity, regular physical activity, and a healthy diet) in this group resulted in a nearly 50% reduction in risk compared to participants with a less healthy lifestyle.
Abbreviations
- ACC:
-
American College of Cardiology
- AHA:
-
American Heart Association
- ALA:
-
Alanine
- APOB:
-
Apolipoprotein B
- APOE:
-
Apolipoprotein E
- ASCOT:
-
Anglo-Scandinavian Cardiac Outcomes Trial
- ASCVD:
-
Atherosclerotic cardiovascular disease
- ASP:
-
Aspartate
- CAD:
-
Coronary artery disease
- CARDIA:
-
Coronary Artery Risk Development in Young Adults
- CARE:
-
Cholesterol and Recurrent Events
- CHD:
-
Coronary heart disease
- CYP:
-
Cytochrom P
- COQ2:
-
Coenzyme Q2, polyprenyltransferase
- CPRD-STAGE:
-
Clinical Practice Research Datalink-STATin-Induced Muscle Toxicity: Exploration Using the UK GEmeal Practice Research Database
- EAS:
-
European Atherosclerotic Society
- ESC:
-
European Society of Cardiology
- FOURIER:
-
Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk
- GATM:
-
Glycine Amidinotransferase
- GIST consortium:
-
Genomic Investigation of Statin Therapy consortium
- GLUT4:
-
Glucose transporter 4
- GLY:
-
Glycine
- GoDARTS:
-
Genetics of Diabetes and Audit Research Tayside Study
- GRS:
-
Genetic risk score
- HMGCR:
-
3-hydroxy-methylglutaryl-CoA reductase
- IMPROVE-IT:
-
Improved Reduction of Outcomes: Vytorin Efficacy International Trial
- JUPITER:
-
Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin
- LDL-C:
-
Low-density lipoprotein cholesterol
- LDLR:
-
Low-density lipoprotein receptor
- LESS-DM:
-
Long-term Effects of high-doSe pitavaStatin on Diabetogenicity in comparison with atorvastatin in patients with Metabolic syndrome
- LILRB5:
-
Leukocyte immunoglobulin-like receptor subfamily-B 5
- Lp(a):
-
Lipoprotein (a)
- NNT:
-
Number needed to treat
- NOD:
-
New onset of diabetes
- NPC1L1:
-
Niemann-Pick C1-Like 1
- PREDICTION-ADR:
-
Personalization of tREatment In Cardiovascular disease adverse drug reaction
- PROVE IT-TIMI 22:
-
Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22
- PCSK9:
-
Proprotein convertase subtilisin/kexin Type 9
- RCT:
-
Randomized controlled trials
- SAMS:
-
Statin-associated muscle syndromes
- SIM:
-
Statin-induced myopathy
- SLCO1B1:
-
Solute carrier organic anion transporter family member 1B1
- SORT1:
-
Sortilin
- SNP:
-
Single nucleotide polymorphism
- Val:
-
Valine
- WHO:
-
World Health Organization
- WOSCOPS:
-
West of Scotland Coronary Prevention Study
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fredrickson DS, Lees RSA. System for phenotyping Hyperlipoproteinemia. Circulation. 1965;31:321–7.
National Cholesterol Education Program. Second report of the expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel II). Circulation. 1994;89(3):1333–445.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S1–45. https://doi.org/10.1161/01.cir.0000437738.63853.7a.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. European guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81. https://doi.org/10.1093/eurheartj/ehw106.
Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease. Endocr Pract. 2017;23(Suppl 2):1–87. https://doi.org/10.4158/EP171764.APPGL.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97. https://doi.org/10.1056/NEJMoa1410489.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–22. https://doi.org/10.1056/NEJMoa1615664.
Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37(11):908–16. https://doi.org/10.1093/eurheartj/ehv641.
De Vera MA, Bhole V, Burns LC, Lacaille D. Impact of statin adherence on cardiovascular disease and mortality outcomes: a systematic review. Br J Clin Pharmacol. 2014;78(4):684–98.
• Toth PP, Patti AM, Giglio RV, Nikolic D, Castellino G, Rizzo M, et al. Management of statin intolerance in 2018: still more questions than answers. Am J Cardiovasc Drugs. 2018; https://doi.org/10.1007/s40256-017-0259-7. This review focuses on the definition of statin intolerance and on the development of clinical and therapeutic strategies for its management, including emerging alternative therapies.
Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289(13):1681–90. https://doi.org/10.1001/jama.289.13.1681.
Furberg CD, Pitt B. Withdrawal of cerivastatin from the world market. Curr Control Trials Cardiovasc Med. 2001;2(5):205–7.
•• Wiggins BS, Saseen JJ, Page RL 2nd, Reed BN, Sneed K, Kostis JB, et al. Recommendations for management of cccclinically significant drug-drug interactions with statins and select agents used in patients with cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2016;134(21):e468–e95. https://doi.org/10.1161/CIR.0000000000000456. This statement of the AHA reviews the basics of drug-drug interactions, the pharmacological differences in the various statins and the significance of statins DDIs with select medications used in patients with CVD.
Deljehier T, Pariente A, Miremont-Salame G, Haramburu F, Nguyen L, Rubin S, et al. Rhabdomyolysis after co-administration of a statin and fusidic acid: an analysis of the literature and of the WHO database of adverse drug reactions. Br J Clin Pharmacol. 2018;84:1057–63. https://doi.org/10.1111/bcp.13515.
Kitzmiller JP, Mikulik EB, Dauki AM, Murkherjee C, Luzum JA. Pharmacogenomics of statins: understanding susceptibility to adverse effects. Pharmacogenomics Pers Med. 2016;9:97–106. https://doi.org/10.2147/PGPM.S86013.
Ramsey LB, Johnson SG, Caudle KE, Haidar CE, Voora D, Wilke RA, et al. The clinical pharmacogenetics implementation consortium guideline for SLCO1B1 and simvastatin-induced myopathy: 2014 update. Clin Pharmacol Ther. 2014;96(4):423–8. https://doi.org/10.1038/clpt.2014.125.
Siddiqui MK, Maroteau C, Veluchamy A, Tornio A, Tavendale R, Carr F, et al. A common missense variant of LILRB5 is associated with statin intolerance and myalgia. Eur Heart J. 2017;38(48):3569–75. https://doi.org/10.1093/eurheartj/ehx467.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207. https://doi.org/10.1056/NEJMoa0807646.
Kohli P, Knowles JW, Sarraju A, Waters DD, Reaven G. Metabolic markers to predict incident diabetes mellitus in statin-treated patients (from the treating to new targets and the stroke prevention by aggressive reduction in cholesterol levels trials). Am J Cardiol. 2016;118(9):1275–81. https://doi.org/10.1016/j.amjcard.2016.07.054.
Casula M, Mozzanica F, Scotti L, Tragni E, Pirillo A, Corrao G, et al. Statin use and risk of new-onset diabetes: a meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2017;27(5):396–406. https://doi.org/10.1016/j.numecd.2017.03.001.
Vallejo-Vaz AJ, Kondapally Seshasai SR, Kurogi K, Michishita I, Nozue T, Sugiyama S, et al. Effect of pitavastatin on glucose, HbA1c and incident diabetes: a meta-analysis of randomized controlled clinical trials in individuals without diabetes. Atherosclerosis. 2015;241(2):409–18. https://doi.org/10.1016/j.atherosclerosis.2015.06.001.
Park JB, Jung JH, Yoon YE, Kim HL, Lee SP, Kim HK, et al. Long-term effects of high-doSe pitavaStatin on diabetogenicity in comparison with atorvastatin in patients with metabolic syndrome (LESS-DM): study protocol for a randomized controlled trial. Trials. 2017;18(1):501. https://doi.org/10.1186/s13063-017-2229-4.
Brault M, Ray J, Gomez YH, Mantzoros CS, Daskalopoulou SS. Statin treatment and new-onset diabetes: a review of proposed mechanisms. Metab Clin Exp. 2014;63(6):735–45. https://doi.org/10.1016/j.metabol.2014.02.014.
• Swerdlow DI, Preiss D, Kuchenbaecker KB, Holmes MV, Engmann JE, Shah T, et al. HMG-coenzyme a reductase inhibition, type 2 diabetes, and bodyweight: evidence from genetic analysis and randomised trials. Lancet. 2015;385(9965):351–61. https://doi.org/10.1016/S0140-6736(14)61183-1. The first publication from a series of articles that has attempted a genetic approach to explain the development of diabetes among patients treated with statins.
Ference BA, Robinson JG, Brook RD, Catapano AL, Chapman MJ, Neff DR, et al. Variation in PCSK9 and HMGCR and risk of cardiovascular disease and diabetes. N Engl J Med. 2016;375(22):2144–53. https://doi.org/10.1056/NEJMoa1604304.
Schmidt AF, Swerdlow DI, Holmes MV, Patel RS, Fairhurst-Hunter Z, Lyall DM, et al. PCSK9 genetic variants and risk of type 2 diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol. 2017;5(2):97–105. https://doi.org/10.1016/S2213-8587(16)30396-5.
Sabatine MS, Leiter LA, Wiviott SD, Giugliano RP, Deedwania P, De Ferrari GM, et al. Cardiovascular safety and efficacy of the PCSK9 inhibitor evolocumab in patients with and without diabetes and the effect of evolocumab on glycaemia and risk of new-onset diabetes: a prespecified analysis of the FOURIER randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5(12):941–50. https://doi.org/10.1016/S2213-8587(17)30313-3.
Leiter LA, Muller-Wieland D, Baccara-Dinet MT, Letierce A, Samuel R, Cariou B. Efficacy and safety of alirocumab in people with prediabetes vs those with normoglycaemia at baseline: a pooled analysis of 10 phase III ODYSSEY clinical trials. Diabet Med. 2018;35(1):121–30. https://doi.org/10.1111/dme.13450.
Lotta LA, Sharp SJ, Burgess S, Perry JRB, Stewart ID, Willems SM, et al. Association between low-density lipoprotein cholesterol-lowering genetic variants and risk of type 2 diabetes: a meta-analysis. JAMA. 2016;316(13):1383–91. https://doi.org/10.1001/jama.2016.14568.
Besseling J, Kastelein JJ, Defesche JC, Hutten BA, Hovingh GK. Association between familial hypercholesterolemia and prevalence of type 2 diabetes mellitus. JAMA. 2015;313(10):1029–36. https://doi.org/10.1001/jama.2015.1206.
Ridker PM, Pradhan A, MacFadyen JG, Libby P, Glynn RJ. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet. 2012;380(9841):565–71. https://doi.org/10.1016/S0140-6736(12)61190-8.
• Liu DJ, Peloso GM, Yu H, Butterworth AS, Wang X, Mahajan A, et al. Exome-wide association study of plasma lipids in >300,000 individuals. Nat Genet. 2017;49(12):1758–66. https://doi.org/10.1038/ng.3977. First exome-wide association study of plasma lipids adding several new loci associated with lipid levels.
• Leusink M, Onland-Moret NC, de Bakker PI, de Boer A, Maitland-van der Zee AH. Seventeen years of statin pharmacogenetics: a systematic review. Pharmacogenomics. 2016;17(2):163–80. https://doi.org/10.2217/pgs.15.158. A very comprehensive review, in which the studies are not only collected, but also critically evaluated in terms of their quality.
Chasman DI, Giulianini F, MacFadyen J, Barratt BJ, Nyberg F, Ridker PM. Genetic determinants of statin-induced low-density lipoprotein cholesterol reduction: the justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin (JUPITER) trial. Circ Cardiovasc Genet. 2012;5(2):257–64. https://doi.org/10.1161/CIRCGENETICS.111.961144.
Hopewell JC, Parish S, Offer A, Link E, Clarke R, Lathrop M, et al. Impact of common genetic variation on response to simvastatin therapy among 18705 participants in the heart protection study. Eur Heart J. 2013;34(13):982–92. https://doi.org/10.1093/eurheartj/ehs344.
•• Postmus I, Trompet S, Deshmukh HA, Barnes MR, Li X, Warren HR, et al. Pharmacogenetic meta-analysis of genome-wide association studies of LDL cholesterol response to statins. Nat Commun. 2014;5:5068. https://doi.org/10.1038/ncomms6068. So far the biggest meta-analysis for GWAS studies exploring the LDL-C lowering effect of statins.
Tsimikas S, Fazio S, Ferdinand KC, Ginsberg HN, Koschinsky ML, Marcovina SM, et al. NHLBI working group recommendations to reduce lipoprotein(a)-mediated risk of cardiovascular disease and aortic stenosis. J Am Coll Cardiol. 2018;71(2):177–92. https://doi.org/10.1016/j.jacc.2017.11.014.
•• Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield M, Devlin JJ, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385(9984):2264–71. https://doi.org/10.1016/S0140-6736(14)61730-X. The first application of a genetic risk score to stratify patients on statins for their cardiovascular risk in primary as well as secondary prevention.
• Natarajan P, Young R, Stitziel NO, Padmanabhan S, Baber U, Mehran R, et al. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation. 2017;135(22):2091–101. https://doi.org/10.1161/CIRCULATIONAHA.116.024436. In addition to the validity of a genetic risk score in statin treated patients, the authors have investigated the association with subclinical atherosclerosis by looking for coronary artery calcification and carotid artery plaque burden.
Vladutiu GD, Simmons Z, Isackson PJ, Tarnopolsky M, Peltier WL, Barboi AC, et al. Genetic risk factors associated with lipid-lowering drug-induced myopathies. Muscle Nerve. 2006;34(2):153–62. https://doi.org/10.1002/mus.20567.
•• Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375(24):2349–58. https://doi.org/10.1056/NEJMoa1605086. A very important study showing that healthy lifestyle can modify the impact of genetic risk on cardiovascular disease.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Hoffmann reports personal fees from Sanofi and Akcea, and non-financial support from Diasys.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lipid Abnormalities and Cardiovascular Prevention
Rights and permissions
About this article
Cite this article
Hoffmann, M.M. Towards a More Personalized Treatment of Dyslipidemias to Prevent Cardiovascular Disease. Curr Cardiol Rep 20, 56 (2018). https://doi.org/10.1007/s11886-018-0996-5
Published:
DOI: https://doi.org/10.1007/s11886-018-0996-5