Abstract
Purpose of Review
This review aims to discuss the effect of alcohol consumption on various cardiovascular (CV) diseases and CV mortality.
Recent Findings
Alcohol intake has consistently shown a J- or U-shaped relationship with several cardiovascular diseases. Light to moderate alcohol intake has been associated with lower risk of coronary artery disease, heart failure (HF), as well as CV mortality. On the other hand, heavy consumption has been associated with deleterious CV outcomes including increased mortality. However, the evidence is based from observational and population-based studies where risk of confounding cannot be excluded even after meticulous methodological approaches. This is compounded by conflicting data such as higher risk of certain CV diseases like HF in former drinkers compared to abstainers. Further, Mendelian randomization studies using genetic polymorphisms in enzymes have recently questioned the beneficial association of low-moderate drinking with CV system.
Summary
There has been substantial and consistent evidence that light to moderate alcohol consumption have beneficial effect on overall cardiovascular profile and mortality. However, there are considerable limitations in the reported literature to determine a strong causality of a protective effect of moderate alcohol consumption by itself. Further robust studies or possibly a well-structured randomized controlled could bring an end to this debate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol has been an integral part of human culture since the beginning of recorded history. While moderate alcohol consumption might be associated with overall beneficial health effects, excess and binge drinking is one of the leading causes of mortality worldwide [1,2,3,4]. The same correlation holds true for alcohol and cardiovascular diseases [5••, 6]. It is suggested that whereas moderate amount of alcohol is protective against coronary artery disease (CAD), higher cardiovascular morbidity and mortality is observed among abstainers and heavy drinkers [7]. There have been multiple observational studies and meta-analyses demonstrating a J- or U-shaped association between alcohol consumption and all-cause mortality [5••, 6,7,8,9,10,11]. However, there is a growing skepticism around this observation, with recent studies pointing out several methodological shortcomings in the evidence on which the U-shaped association is based [12, 13]. In addition, age, ethnicity, gender, type and pattern of alcoholic beverage, and other confounding biases were not taken into account while arriving at these conclusions. The purpose of this review is to discuss the effect of alcohol consumption on cardiovascular mortality and coronary artery disease (CAD), the shortcomings of the reported studies, the cardioprotective mechanism of alcohol and the disparities due to age, sex, ethnicity, pattern, and type of beverage consumed.
What Is Light, Moderate, Heavy and Binge Drinking?
As per the Center for Disease Control (CDC), a standard drink contains 0.6 oz (14.0 g or 1.2 tablespoons) of pure alcohol. Generally, this amount of pure alcohol is found in 12-oz of beer (5% alcohol content), 8 oz of malt liquor (7% alcohol content), 5 oz of wine (12% alcohol content), and 1.5 oz of 80 proof (40% alcohol content) distilled spirits or liquor (e.g., gin, rum, vodka, whiskey) [12]. The Dietary Guidelines for Americans define moderate drinking as up to one drink per day for women and up to two drinks per day for men, and light drinking as any amount less than moderate drinking [12]. Heavy drinking is defined as consuming 8 or more drinks per week for women and 15 or more drinks per week for men. Binge drinking, the most common form of excessive drinking, is defined as consuming four or more drinks during a single occasion for women and five or more drinks during a single occasion for men, respectively [12] (Fig. 1).
What is excessive alcohol use? (from the National Center for Chronic Disease Prevention and Health Promotion and Division of Population Health; see https://www.cdc.gov/alcohol/pdfs/excessive_alcohol_use.pdf)
Alcohol and Cardiovascular Mortality
Studies have consistently reported a J-shaped or U-shaped curve to describe the relationship between alcohol use and total cardiovascular (CV) mortality observational and prospective studies showing a lower risk for CV diseases in light to moderate drinkers compared to abstainers, and highest risk among heavy drinkers [14,15,16,17,18]. This observation was supported by a meta-analysis of 34 prospective studies by Di Castelnuovo et al. [14] involving more than one million individuals that reported inverse relationship between mortality and consumption of alcohol, up to four drinks per day in men and two drinks per day in women, was inversely associated with total mortality [14]. The maximum protection was noted at one half to one drink daily for women (18% decrease in total mortality) and one to two drinks daily for men (total mortality decrease of 17%). However, intakes above 2.5 drinks per day in women and 4 drinks per day in men were associated with progressively higher death rates in a dose-dependent relationship.
Gaziano et al. examined the relationship between light-to-moderate alcohol consumption and cause-specific mortality in a prospective cohort of 89,299 US men from the Physicians’ Health Study enrollment cohort who were free of known myocardial infarction (MI), stroke, cancer, or liver disease at baseline [15]. The authors reported a U-shaped relationship between light-to-moderate alcohol intake and risk of total mortality. A decreased total mortality risk of up to 26% was seen among those who consumed 1 to less than 14 drinks per week. Similarly, Grønbaek et al. assessed relationship between stable alcohol intake and total mortality in a longitudinal study of 6644 men and 8010 women, age 25 to 98 years, who had attended at least two health surveys with a 5-year interval between them [16]. Stable drinkers demonstrated U-shaped all-cause mortality, with relative risks of 1.29 (95% confidence interval [CI] = 1.13–1.48) for nondrinkers (< 1 drink per week) and 1.32 (1.15–1.53) for heavy drinkers (> 13 drinks per week) compared with light drinkers (1 to 6 drinks per week). The authors also found that the stable abstainers had a relative risk of 1.32 (0.97–1.79) for developing coronary artery disease as compared with stable light drinkers. Cancer mortality was also increased in all groups of heavy drinkers [16]. Thun et al. published the results of a very large trial of 490,000 men and women (mean age, 56 years; range, 30 to 104) who were followed for 9 years. Forty-six thousand people died during 9 years of follow-up [17]. The authors compared the cause-specific rates of death across categories of baseline alcohol consumption, adjusting for other risk factors, and related drinking and smoking habits to the cumulative probability of dying between the ages of 35 and 69 years. The overall cardiovascular mortality was lower among men and women who reported consuming at least one drink daily than among nondrinkers. The all-cause mortality increased as the level of alcohol consumption increased with the highest mortality among heavy drinkers, particularly among adults less than 60 years of age. In the middle-aged and elderly population, moderate alcohol consumption slightly reduced overall mortality which was offset by smoking which approximately doubled this risk.
In a prospective epidemiological study, Goldberg et al. investigated health effects of alcohol consumption in middle-aged (aged 51 to 64 years) and elderly men (aged 65 to 75 years) of Japanese-American origin who were participating in the Honolulu Heart Program and were free from coronary heart disease, cerebrovascular disease, and cancer at baseline examination and at subsequent re-examination 6 years later [18]. The authors found that even after adjusting for several potential confounding factors, overall mortality exhibited a J-shaped pattern with the alcohol consumption. In another large and statistically rigorous study of 245,000 US adults, alcohol intakes of both light (3 drinks per week or less) and moderate (4 to 7 drinks per week for women, 4 to 14 drinks per week for men) levels were associated with lower CV mortality compared with either heavy users (> 7 drinks per week in women or > 14 drinks per week in men) or lifetime abstainers [19].
Alcohol and Coronary Artery Disease
Alcohol has been shown to have a favorable effect on the development of CAD. Studies have reported that moderate alcohol use is linked with a decreased atherosclerotic burden as assessed by coronary angiography [20], computerized tomography-detected coronary calcium [21], and carotid ultrasound [22]. Several observational studies have shown reduced risk of acute MI and CAD death in moderate drinkers compared to abstainers [23,24,25]. Similar to mortality, meta-analyses have also shown a U-curve or J-curve association between increasing alcohol intake and CAD, with lifelong abstainers as the referent. In the INTER-HEART case-control study [26], involving 27,000 patients from 52 countries, regular alcohol consumption was associated with a reduced incidence of MI in all adult age groups and in both genders. Light to moderate drinking was associated with improved CV health in higher-risk individuals, such as those with known CAD and/or diabetes, but it also reduced CV risk in lower-risk individuals. The Health Professionals Follow-Up Study [27] focused on effects of alcohol in 8867 men (mean age 57 years) taken from the total cohort of 51,529 health professionals who followed all four of the major healthy lifestyle behaviors (abstention from smoking, maintaining a body mass index 25 kg/m2, exercising at least 30 min daily, and eating a healthy diet) and were followed up for 16 years. The health professionals consuming 15.0 to 29.9 g/day of alcohol (i.e., 2 drinks per day) were associated with the lowest risk for MI, with higher intake associated with intermediate risk [27]. A larger study of 22, 071 male physicians in the USA confirmed that compared to men who had less than one drink per week, those who drank one drink per day had a lower relative risk of developing angina pectoris (relative risk 0.69; 95% CI, 0.59 to 0.81) and MI (0.65; 95% CI, 0.52 to 0.81) [28]. Several other epidemiological studies have also shown that light to moderate drinkers as compared to nondrinkers or heavy drinkers have lower rates of nonfatal acute MI and coronary deaths [19, 29].
Interestingly, light to moderate alcohol intake has also been shown to improve outcomes in patients with established CV disease. Mukamal et al. studied the effect of prior alcohol consumption on long-term mortality among early survivors of acute MI [30]. In a prospective cohort study of 1913 adults hospitalized with AMI, all-cause mortality was compared by self-reported average weekly consumption of alcohol in the year before the acute coronary event, over a median follow-up of 3.8 years looking. The authors concluded that moderate alcohol consumption during the prior year, as measured at the time of index AMI, was associated with lower subsequent mortality following AMI. The association was similar for among both men and women and with total and cardiovascular mortality, and among different types of alcoholic beverages [30]. In another prospective study, 1351 patients with established CAD who had undergone coronary artery bypass surgery were followed for 4.3 years. The authors found that the patients who had a moderate amount of alcohol consumption, i.e., between 7 and 13 drinks per week had a 30% reduction in clinical events as compared with abstainers or patients who consumed small amount [31]. In a meta-analysis of 8 prospective studies involving 16,351 patients with a history of CV disease, the familiar J-shaped curve was observed with maximal protection by alcohol at approximately 26 g/day (or about two drinks daily) [32]. Other studies evaluating alcohol’s effects on patients who have had a MI also report the typical J-shaped relationship between drinking and adverse events or total mortality [33, 34].
Age, Sex, Ethnicity, and Type of Beverage Consumed
Age
The cardioprotective benefit of moderate alcohol intake appears to be more favorable for middle-aged and older people compared with younger individuals. In a pooled analysis of eight prospective studies by Hvidtfeldt el al [35] including 192,067 women and 74,919 men, an inverse association was found between alcohol intake and risk of CAD events. However, the absolute reductions in CAD were not clinically significant for people younger than 50 years of age [35]. Mukamal et al. looked at the relationship between alcohol use and coronary heart disease in 4410 adults aged > 65 years and free of cardiovascular disease at baseline [36]. Intriguingly, consumption of 14 or more drinks per week was associated with the lowest risk of coronary heart disease thereby supporting that alcohol intake is beneficial even in an older population group. Younger individuals are at a much lower risk for CAD but are more likely to engage in excessive and/or binge drinking and are therefore at higher risk of alcohol-related accidents, violence, and overdoses [37]. Thus, the risks of regular drinking especially heavy drinking may outweigh the cardiovascular benefits for younger population.
Sex
Given differences in volume of distribution, first-pass metabolism, and overall body size between the two genders, women experience toxic effects of alcohol at approximately half the daily dose of men [38]. However, the beneficial cardiovascular effects of moderate alcohol consumption in women are similar to those seen in men [39, 40]. In the Nurses’ Health study of 87,526 female nurses aged 34 to 59 years, moderate alcohol consumption decreased the risks of CAD and ischemic stroke during 334,382 person-years of follow-up, compared with nondrinkers [7]. Freiberg et al. conducted a prospective study among 10,576 black and 105,610 white postmenopausal women from the Women’s Health Initiative (WHI), without a history of cancer or cardiovascular disease. During a mean 8-year follow-up period, moderate drinking was associated with a lower risk of total mortality among Caucasian women regardless of hypertensive status, and hypertensive but not nonhypertensive African-American women [41]. Further, in another WHI Observational Study of 3198 postmenopausal women, both frequency and quantity of alcohol intake were inversely associated with the risk of developing CAD, irrespective of the beverage type [42]. Similarly, in the Swedish Women’s Lifestyle and Health Study of 47,921 women, aged 30–49 years, a substantial inverse relationship was seen between light to moderate drinking and total mortality which was predominantly driven by a reduction in cardiovascular mortality [43].
Ethnicity
The cardioprotective effect of moderate alcohol consumption might not be universal and vary according to different ethnicities. Most of the reported literature on the beneficial effects of alcohol has been studied in western world. In the INTERHEART study of acute MI patients, alcohol consumption in South Asians was not protective against CAD as was observed in other countries [26]. These results were supported in a study by Roy et al. involving 4465 Indian participants aged 20–69 years of age, in which the subjects with current and/or past alcohol use had a higher risk of CAD compared with alcohol abstainers [44]. In contrast with other studies, there was an inverse association suggesting possible harm of alcohol for coronary risk in Indian men. Similarly, Schooling et al. conducted a study in an older Chinese population in Hong Kong and found that moderate alcohol use had no effect on ischemic heart disease mortality in older men [45].
Type of Alcohol Consumed (the French Paradox)
The term French paradox was first used in 1992 to describe a relatively lower incidence of CV disease in the French population despite a relatively high dietary intake of saturated fatty acids. This paradox was postulated to be due to consumption of a moderate amount of red wine by the study population [46]. Although red wine has been shown to have higher levels of bioflavonoids which have antioxidant, anti-endothelin-1, and antiplatelet effects compared with white wine and other forms of alcohol, the ethanol itself rather than a specific type (wine, beer, liquor) appears to be the major factor in conferring the health benefits [47, 48]. Most of the observational and prospective studies have shown equal protection from all types of alcohol suggesting that the specific alcoholic beverage is less important than the quantity and pattern of the alcohol intake [49, 50]. A differential cardioprotective effect of wine is probably confounded by the fact that wine drinkers have more favorable CAD risk profile and also as compared to beer or liquor, wine is more often used in moderation.
Controversies Regarding the Cardioprotective Effect of Alcohol
The beneficial effects of alcohol have long been scientifically debated in part due to the lack of the control group and the observational/cross sectional nature of the studies. No randomized controlled trials with CAD outcome data have been conducted so far due to ethical and logistics reasons. Therefore, confounding cannot be completely ruled out and uncertainty remains about the causal nature of the association. Most of the studies that evaluated the relationship between alcohol consumption and CAD have used current abstainers and did not differentiate between lifetime abstainers and sick quitters, i.e., the former drinkers who gave up drinking due to health reasons [51]. Including sick quitters into control group might confound the results by falsely indicating a protective effect of light or moderate drinking. However, in few studies where the comparisons were made with lifetime abstainers only, the protective effect of moderate alcohol consumption persisted [9, 52]. But it should be taken in to account that these lifetime abstainers are people in high-income societies and often differs from the general population in socioeconomic status, drinking and nutritional habits, and therefore, these results should be interpreted with caution. Moreover, alcohol might have different influence on CV risk acutely as compared to long-term period. In a meta-analysis of 23 studies, even moderate alcohol consumption was associated with an immediate elevated CV risk while a benefit against MI and stroke was confirmed after 24 h [53]. Further, a “healthy drinker” hypothesis suggests that people who drink alcohol in moderation usually have healthier life style as compared to heavy and binge drinkers. Heavy and binge drinkers are likely to smoke more, do less exercise and follow worse diets as compared to their counterparts which might explain higher cardiovascular mortality.
Although there are numerous modifiable risk factors identified for ischemic heart disease, smoking is one of the most important risk factors and several studies have proven its influence on alcohol and CAD relationship. Some studies reported an inverse relationship, some a threshold relationship, and some no clear relationship [53,54,55,56]. There is the possibility that the detrimental association from alcohol consumption is overestimated because of uncontrolled confounding from smoking.
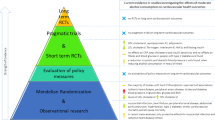
More recently, Mendelian randomization studies have looked at the association between alcohol and cardiovascular disease [57]. These studies are centered on the fact that genetic variants affecting alcohol metabolism are allocated randomly which theoretically comprises a form of “natural” randomized controlled trial [58]. Some evidence has suggested that individuals with an alcohol dehydrogenase polymorphism (ADH1C) resulting in “slow metabolism” of alcohol may obtain more cardiovascular benefit [59], thus supporting a causal relationship between the protective effect of light–moderate drinking on CAD. However, subsequent Mendelian randomization analyses have yielded conflicting results. For example, a Danish study showed that increasing alcohol intake was associated with decreasing risk of MI, but the association was not modified by ADH1B and ADH1C genotypes [60]. In contrast, a recent meta-analysis of 56 studies showed that individuals with the ADH1B polymorphism who were more likely to be abstainers had decreased CV risk and thus reduction of alcohol consumption might be beneficial for CV health even in light and moderate drinkers [57].
There are other considerations, such as the effect of underestimated consumption by the drinkers [61], or the effects of ingredients other than ethanol on the risks of development of CV disease [62], especially in unrecorded consumption [63]. However, these potential biases have received much less attention compared to the potential biases in the estimation of beneficial effects of alcohol.
Mechanism of Cardioprotective Action of Alcohol
There are several mechanisms that have been proposed to explain the beneficial effects of moderate alcohol consumption on CV diseases which include an increase in high-density lipoprotein (HDL) cholesterol, increased insulin sensitivity, favorable effects mediated by alterations in protein kinase C (PKC), anti-inflammatory effect, increase adiponectin, increase fibrinolysis, decrease in platelet aggregation, and coagulation and improved endothelial function [64,65,66] (Fig. 2). As these mechanisms are interconnected through complex metabolic pathways, the exact contribution of an individual component is difficult to assess. HDL cholesterol is an important factor for maintaining appropriate concentrations of low-density lipoprotein (LDL) cholesterol in vascular and other cells throughout the body. Additionally, HDL reduces expression of adhesion molecules and inhibits oxidation of LDL, migration of inflammatory cells into endothelium, and thus thrombosis. Moderate alcohol intake is associated with an increase in HDL and apolipoprotein (Apo) A1, the major HDL carrier protein in a dose-dependent fashion [67, 68]. Epidemiological studies support that a significant decrease in CAD risk in alcohol drinkers is mediated by higher HDL levels [69, 70].
Moderate alcohol consumption is also associated with increase in insulin sensitivity and glucose metabolism by suppression of fatty acid release from adipose tissue and elevation of adiponectin levels [71, 72]. This reduction in fatty acids decreases substrate competition in the Krebs cycle of skeletal muscles, thereby facilitating glucose metabolism [73]. One or two drinks per day reduce triglycerides modestly (7–10%), decrease abdominal obesity and improve the overall CV risk profile which is of significance in patients with metabolic syndrome [74, 75]. Therefore, an inverse relationship is seen in heavy drinkers, which lead to worsening of metabolic syndrome and raised homocysteine levels, and ultimately increased CV mortality [76, 77].
Evidence from human and animal studies has also suggested a possible role of alcohol as a CV preconditioning agent [64]. Moderate alcohol consumption mimics classic cardiac preconditioning and protects against ischemia-reperfusion injury, as evidenced by reduced infarct size and decreased hypoxia induced cell death. The mechanism of benefit involves the PKC family of isoforms which are activated by myocardial ischemia. Alcohol shares many of the same signal transduction pathways and effector molecules that have been implicated in conventional and/or pharmacologic preconditioning [78, 79]. Alcohol is also believed to have anti-inflammatory properties that are likely mediated through changes in cytokine profiles and cell signaling pathways. Recent data have shown that acute alcohol consumption may exert beneficial effects on the vascular system by suppressing production of proinflammatory cytokines such as tumor necrosis factor-alpha, interleukin-1 receptor antagonist, interleukin-5, interleukin-6, and C-reactive protein [80,81,82]. Moreover, alcohol has shown to have several antithrombotic effects including inhibition of platelet adhesion and lowered fibrinogen levels. As thrombosis in atherosclerotic arteries plays a key role in major CAD events, these effects may be important factors in the protective effect of alcohol however no human studies have confirmed a causal relationship.
Alcohol and Blood Pressure
The effects of alcohol consumption on blood pressure (BP) are less certain. Although low to moderate alcohol intake has no immediate effect on BP response, binge drinking has been shown to cause acute rise in systolic BP by mean of 4–6 mm Hg [83]. Moreover, different studies conflict in regard to association between long-term impact of light–moderate and heavy alcohol consumption and hypertension (HTN) incidence. In the CARDIA study, stratification of patients based on different levels of alcohol intake did not reveal an association with increase in incident HTN over a period of 20 years even after adjusting for several potential confounders [84]. In contrast, two meta-analyses studying effect of different doses of alcohol intake demonstrated differential association with risk of HTN in men and women [85, 86]. While, a J-shaped curve was observed in women with reduced risk of HTN for < 10 g intake and increasing risk for > 20 g intake/day, men had a more linear increase in BP response with intake > 30 g/day. Endothelial cellular dysfunction, oxidative stress, and imbalances in neurohormonal pathways are the most plausible pathways involved in ethanol-induced HTN. To consolidate these findings, both men and women have increased risk of HTN with alcohol intake greater than moderate levels.
Alcohol and Cardiomyopathy
Alcohol consumption may have a bimodal response with heavy intake leading to both increased risk of developing heart failure (HF) as well as progression of established HF. A meta-analysis of eight studies assessing the dose-response relationship between alcohol consumption and HF showed a decreased risk of HF in patients with light to moderate (3–10 drinks/week) alcohol intake as compared to abstainers [87••]. In another study, elderly patients > 65 years age had a U-shaped response with light (1–6 drinks/week) and moderate (7–13 drinks/week) alcohol consumptions associated with a lower risk of HF as compared to abstainers [88]. However, former drinkers had a higher risk of HF compared to abstainers raising questions about protective effects of alcohol on HF. Further, higher risk of HF has been observed in men with heavy intake (> 28 drinks/week) and in lifetime abstainers compared to light drinkers [89].
Alcohol cardiomyopathy (ACM) is a type of dilated cardiomyopathy with reduced ejection fraction (EF) associated with long-term heavy alcohol consumption. The exact burden of ACM remains unknown but has been reported to account for 23–40% of cases with cardiomyopathy [90]. As seen with relationship of alcohol and other CV diseases, ACM might develop early and at a lower consumption in women as compared to men [91]. Potential mechanisms of ACM include free radical generation and oxidative stress, apoptosis, protein breakdown, and alterations of fatty acid metabolism. Thus, while light to moderate alcohol consumption might confer some benefit from HF risk in early to middle life, heavy drinkers especially elderly patients have much higher risk of developing HF.
Alcohol and Diabetes Mellitus
Light to moderate alcohol consumption appears to protect against development of CAD and the risk of coronary death in diabetic men and women [39, 92]. In addition, moderate alcohol consumption may lower the risk of developing type 2 diabetes [93] and the metabolic syndrome which are both strong risk factors for coronary disease. The finding of a U-shaped relationship between alcohol consumption and type 2 diabetes risk is similar with the previously demonstrated relationship with cardiovascular diseases and may partly share underlying mechanisms.
Conclusion
There is substantial and consistent evidence from observational and short-term experimental studies that having one to two drinks per day without episodic heavy drinking have a beneficial effect on the development of coronary artery disease as compared to lifetime abstainers. However, these studies suffer from either methodological issue, confounding biases, misclassification of alcohol consumption, excluding drinking patterns, the inclusion of sick quitters in reference groups and ethnicity differences. Therefore, it is impossible to determine causality of a protective effect of moderate alcohol consumption on ischemic heart disease by itself. Further robust studies or possibly a well-structured randomized controlled could bring an end to this debate. In our view, physicians should inform patients that low to moderate alcohol consumption (one drink/day for women or up to two drinks/day for men) should not be dangerous to their health. However, life-long abstaining individuals should not be encouraged to start drinking; owing to the fact that scenario has not been assessed even in observational studies and there is no way to predict if a person would consume only in moderation after starting drinking. Heavy or binge drinking can have adverse health outcomes [2, 3] and should be strongly discouraged. The physician should be aware that regular, moderate alcohol consumption, in the context of a healthy lifestyle, good dietary habits, and adequate drug therapy would substantially lower their cardiovascular or mortality risk than either abstainers or heavy/binge drinkers. The cardiovascular benefit of moderate alcohol intake must be balanced in the individual against the adverse effects of alcohol. Furthermore, the net risk-benefit balance associated with moderate alcohol consumption differs in various age groups and populations. The American Heart Association (AHA) actually recommends against advising people who do not currently drink to initiate light alcohol use [94]).
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
World Health Organization Management of Substance Abuse Team. Global status report on alcohol and health. Geneva: World Health Organization; 2011. 85
Centers for Disease Control and Prevention (CDC). Alcohol-related disease impact (ARDI). Atlanta: CDC.
Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis. 2014;11:130293.
Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med. 2015;49(5):e73–9.
•• Fernández-Solà J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat Rev Cardiol. 2015;12:576–87. This is an excellent review article discussing the beneficial effects of moderate alcohol consumption on cardiovascular mortality.
Mukamal KJ, Rimm EB. Alcohol consumption: risks and benefits. Curr Atheroscler Rep. 2008;10:536–43.
Stampfer MJ, Colditz GA, Willett WC, Speizer FE, Hennekens CH. A prospective study of moderate alcohol consumption and the risk of coronary disease and stroke in women. N Engl J Med. 1988;319(5):267–73.
Roerecke M, Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: a systematic review and meta-analysis. Addiction. 2012;107:1246–60.
Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med. 2014;12:182.
Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671.
O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health: the razor-sharp double-edged sword. J Am Coll Cardiol. 2007;50:1009–14.
Chikritzhs T, Stockwell T, Naimi T, Andreasson S, Dangardt F, Liang W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed? Addiction. 2015;110:726–7.
Fekjaer HO. Alcohol-a universal preventive agent? A critical analysis. Addiction. 2013;108:2051–7.
Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women. Arch Intern Med. 2006;166:2437–45.
Gaziano JM, Gaziano TA, Glynn RJ, Sesso HD, Ajani UA, Stampfer MJ, et al. Light-to-moderate alcohol consumption and mortality in the Physicians’ Health Study enrollment cohort. J Am Coll Cardiol. 2000;35:96–105.
Grønbaek M, Johansen D, Becker U, Hein HO, Schnohr P, Jensen G, et al. Changes in alcohol intake and mortality: a longitudinal population study. Epidemiology. 2004;15:222–8.
Thun MJ, Peto R, Lopez AD, Monaco JA, Henley SJ, Heath CW, et al. Alcohol consumption and mortality among middle-aged and elderly US adults. N Engl J Med. 1997;337:1705–14.
Goldberg RJ, Burchfiel CM, Reed DM, Wergowske G, Chiu D. A prospective study of the health effects of alcohol consumption in middle-aged and elderly men: the Honolulu Heart Program. Circulation. 1994;89:651–9.
Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55(13):1328–35.
Femia R, Natali A, L’Abbate A, Ferrannini E. Coronary atherosclerosis and alcohol consumption: angiographic and mortality data. Arterioscler Thromb Vasc Biol. 2006;26:1607–12.
Vliegenthart R, Oei HHS, van den Elzen APM, van Rooij FJA, Hofman A, Oudkerk M, et al. Alcohol consumption and coronary calcification in a general population. Arch Intern Med. 2004;164:2355–60.
Schminke U, Luedemann J, Berger K, Alte D, Mitusch R, Wood WG, et al. Association between alcohol consumption and subclinical carotid atherosclerosis: the Study of Health in Pomerania. Stroke. 2005;36:1746–52.
Renaud S, Criqui MH, Farchi G, Veenstra J. Alcohol drinking and coronary heart disease. In: Verschuren PM, editor. Health issues related to alcohol consumption. Washington: ILSI Press; 1993. p. 81–124.
Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000;95:1505–23.
Gunzerath L, Faden V, Zakhari S, Warren K. National Institute on Alcohol Abuse and Alcoholism report on moderate drinking. Alcohol Clin Exp Res. 2004;28:829–49.
Yusuf S, Hawken S, Ounpuu S, et al. INTER-HEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTER-HEART study): case-control study. Lancet. 2004;364:937–52.
Mukamal KJ, Chiuve SE, Rimm EB. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch Intern Med. 2006;166:2145–50.
Camargo CA Jr, Stampfer MJ, Glynn RJ, Grodstein F, Gaziano JM, Manson JE, et al. Moderate alcohol consumption and risk for angina pectoris or myocardial infarction in U.S. male physicians. Ann Intern Med. 1997;126:372–5.
Agarwal DP, Srivastava LM. Does moderate alcohol intake protect against coronary heart disease? Indian Heart J. 2001;53:224–30.
Mukamal K, Maclure M, Muller JE, Sherwood JB, Mittleman MA. Prior alcohol consumption and mortality following acute myocardial infarction. JAMA. 2001;285:1965–70.
Mukamal KJ, Girotra S, Mittleman MA. Alcohol consumption, atherosclerotic progression, and prognosis among patients with coronary artery bypass grafts. Am Heart J. 2006;151:368–72.
Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Alcohol consumption and mortality in patients with cardiovascular disease: a meta-analysis. J Am Coll Cardiol. 2010;55(13):1339–47.
Marfella R, Cacciapuoti F, Siniscalchi M, Sasso FC, Marchese F, Cinone F, et al. Effect of moderate red wine intake on cardiac prognosis after recent acute myocardial infarction of subjects with type 2 diabetes mellitus. Diabet Med. 2006;23(9):974–81.
Carter MD, Lee JH, Buchanan DM, Peterson ED, Tang F, Reid KJ, et al. Comparison of outcomes among moderate alcohol drinkers before acute myocardial infarction to effect of continued versus discontinuing alcohol intake after the infarct. Am J Cardiol. 2010;105(12):1651–4.
Hvidtfeldt UA, Tolstrup JS, Jakobsen MU, Heitmann BL, Gronbaek M, O'Reilly E, et al. Alcohol intake and risk of coronary heart disease in younger, middle-aged, and older adults. Circulation. 2010;121(14):1589–97.
Mukamal KJ, Chung H, Jenny NS, Kuller LH, Longstreth WT Jr, Mittleman MA, et al. Alcohol consumption and risk of coronary heart disease in older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54(1):30–7.
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33.
Baraona E, Abittan CS, Dohmen K, Moretti M, Pozzato G, Chayes ZW, et al. Gender differences in pharmacokinetics of alcohol. Alcohol Clin Exp Res. 2001;25(4):502–7.
Solomon CG, Hu FB, Stampfer MJ, Colditz GA, Speizer FE, Rimm EB, et al. Moderate alcohol consumption and risk of coronary heart disease among women with type 2 diabetes mellitus. Circulation. 2000;102:494–9.
Janszky I, Mukamal KJ, Orth-Gomer K, Romelsjo A, SchenckGustafsson K, Svane B, et al. Alcohol consumption and coronary atherosclerosis progression: the Stockholm Female Coronary Risk Angiographic Study. Atherosclerosis. 2004;176:311–9.
Freiberg MS, Chang YF, Kraemer KL, Robinson JG, Adams-Campbell LL, Kuller LL. Alcohol consumption, hypertension, and total mortality among women. Am J Hypertens. 2009;22(11):1212–8.
Rajpathak SN, Freiberg MS, Wang C, Wylie-Rosett J, Wildman RP, Rohan TE, et al. Alcohol consumption and the risk of coronary heart disease in postmenopausal women with diabetes: Women's Health Initiative observational study. Eur J Nutr. 2010;49(4):211–8.
Behrens G, Leitzmann MF, Sandin S, Löf M, Heid IM, Adami HO, et al. The association between alcohol consumption and mortality: the Swedish women's lifestyle and health study. Eur J Epidemiol. 2011;26(2):81–90.
Roy A, Prabhakaran D, Jeemon P, Thankappan KR, Mohan V, Ramakrishnan L, et al. Impact of alcohol on coronary heart disease in Indian men. Atherosclerosis. 2010;210(2):531–5.
Schooling CM, Sun W, Ho SY, et al. Moderate alcohol use and mortality from ischemic heart disease: a prospective study in older Chinese people. PLoS One. 2008;3(6):e2370.
Renaud S, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339(8808):1523–6.
Mukamal KJ, Jensen MK, Grønbæk M, et al. Drinking frequency, mediating biomarkers, and risk of myocardial infarction in women and men. Circulation. 2005;112:1406–13.
Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA Jr, Stampfer MJ, Willett WC, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348:109–18.
Corder R, Mullent W, Khan NQ, et al. Red wine procyanidins and vascular health. Nature. 2006;444:566.
Ellison RC. Importance of pattern of alcohol consumption. Circulation. 2005;112:3818–9.
Shaper A, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2:1267–73.
Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol. 2014;64:281–9.
Inoue M, Nagata C, Tsuji I, Sugawara Y, Wakai K, Tamakoshi A, et al. Impact of alcohol intake on total mortality and mortality from major causes in Japan: a pooled analysis of six large-scale cohort studies. J Epidemiol Community Health. 2012;66:448–56.
Hart CL, Davey Smith G, Gruer L, Watt GC. The combined effect of smoking tobacco and drinking alcohol on cause-specific mortality: a 30 year cohort study. BMC Public Health. 2010;10:789.
Ebbert JO, Janney CA, Sellers TA, Folsom AR, Cerhan JR. The association of alcohol consumption with coronary heart disease mortality and cancer incidence varies by smoking history. J Gen Intern Med. 2005;20:14–20.
Zaridze D, Lewington S, Boroda A, Scélo G, Karpov R, Lazarev A, et al. Alcohol and mortality in Russia: prospective observational study of 151,000 adults. Lancet. 2014;383:1465–73.
Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. Br Med J. 2014;349:g4164.
Frick U, Rehm J. Can we establish causality with statistical analyses? The example of epidemiology. In: Wiedermann W, von Eye A, et al., editors. Statistics and causality: methods for applied empirical research. Hoboken: Wiley; 2016. p. 407–32.
Heidrich J, Wellmann J, Doring A, Illig T, Keil U. Alcohol consumption, alcohol dehydrogenase and risk of coronary heart disease in the MONICA/KORA-Augsburg cohort 1994/ 1995–2002. Eur J Cardiovasc Prev Rehabil. 2007;14:769–74.
Tolstrup JS, Grønbaek M, Nordestgaard BG. Alcohol intake, myocardial infarction, biochemical risk factors, and alcohol dehydrogenase genotypes. Circ Cardiovasc Genet. 2009;2:507–14.
Butt P, Beirness D, Cesa F, Gliksman L, Paradis C, Stockwell T. Alcohol and health in Canada: a summary of evidence and guidelines for low-risk drinking. Ottawa: Canadian Centre on Substance Abuse; 2011.
Pflaum T, Hausler T, Baumung C, Ackermann S, Kuballa T, Rehm J, et al. Carcinogenic compounds in alcoholic beverages: an update. Arch Toxicol. 2016;90:2349–67.
Rehm J, Kailasapillai S, Larsen E, Rehm MX, Samokhvalov AV, Shield KD, et al. A systematic review of the epidemiology of unrecorded alcohol consumption and the chemical composition of unrecorded alcohol. Addiction. 2014;109:880–93.
Krenz M, Korthuis RJ. Moderate ethanol ingestion and cardiovascular protection: from epidemiologic associations to cellular mechanisms. J Mol Cell Cardiol. 2012;52(1):93–104.
Perissinotto E, Buja A, Maggi S, Enzi G, Manzato E, Scafato E, et al. Alcohol consumption and cardiovascular risk factors in older lifelong wine drinkers: the Italian Longitudinal Study on Aging. Nutr Metab Cardiovasc Dis. 2010;20(9):647–55.
Wakabayashi I. Associations between alcohol drinking and multiple risk factors for atherosclerosis in smokers and nonsmokers. Angiology. 2010;61(5):495–503.
De Oliveira Silva ER, Foster D, McGee Harper M, et al. Alcohol consumption raises HDL cholesterol levels by increasing the transport rate of apolipoproteins A-I and A-II. Circulation. 2000;102(19):2347–52.
Mukamal KJ, Mackey RH, Kuller LH, Tracy RP, Kronmal RA, Mittleman MA, et al. Alcohol consumption and lipoprotein subclasses in older adults. J Clin Endocrinol Metab. 2007;92(7):2559–66.
Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. Br Med J. 1999;319:1523–8.
Criqui MH, Golomb BA. Epidemiologic aspects of lipid abnormalities. Am J Med. 1998;105(1A):48S–57S.
Ebrahim S, Lawlor DA, Shlomo YB, Timpson N, Harbord R, Christensen M, et al. Alcohol dehydrogenase type 1C (ADH1C) variants, alcohol consumption traits, HDL-cholesterol and risk of coronary heart disease in women and men: British Women’s Heart and Health Study and Caerphilly cohorts. Atherosclerosis. 2008;196(2):871–8.
Sierksma A, Patel H, Ouchi N, Kihara S, Funahashi T, Heine RJ, et al. Effect of moderate alcohol consumption on adiponectin, tumor necrosis factor-alpha, and insulin sensitivity. Diabetes Care. 2004;27(1):184–9.
Greenfield JR, Samaras K, Jenkins AB, Kelly PJ, Spector TD, Campbell LV. Moderate alcohol consumption, estrogen replacement therapy, and physical activity are associated with increased insulin sensitivity: is abdominal adiposity the mediator? Diabetes Care. 2003;26(10):2734–40.
Davies MJ, Baer DJ, Judd JT, Brown ED, Campbell WS, Taylor PR. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women: a randomized controlled trial. JAMA. 2002;287(19):2559–62.
Gigleux I, Gagnon J, St-Pierre A, Cantin B, Dagenais GR, Meyer F, et al. Moderate alcohol consumption is more cardioprotective in men with the metabolic syndrome. J Nutr. 2006;136:3027–32.
Fan AZ, Russell M, Dorn J, Freudenheim JL, Nochajski T, Hovey K, et al. Lifetime alcohol drinking pattern is related to the prevalence of metabolic syndrome: the Western New York Health Study (WNYHS). Eur J Epidemiol. 2006;21:129–38.
Robinson G, Narasimhan S, Weatherall M, Beasley R. Raised plasma homocysteine levels in alcoholism: increasing the risk of heart disease and dementia? N Z Med J. 2005;118:U1490.
Pagel PS, Toller WG, Gross ER, Gare M, Kersten JR, Warltier DC. KATP channels mediate the beneficial effects of chronic ethanol ingestion. Am J Physiol Heart Circ Physiol. 2000;279:H2574–9.
Zhou HZ, Karliner JS, Gray MO. Moderate alcohol consumption induces sustained cardiac protection by activating PKC- and Akt. Am J Phys. 2002;283:H165–74.
Nelson S, Kolls JK. Alcohol, host defense and society. Nat Rev Immunol. 2002;2:205–9.
Stoltz DA, Nelson S, Kolls JK, et al. In vitro ethanol suppresses alveolar macrophage TNF-alpha during simian immunodeficiency virus infection. Am J Respir Crit Care Med. 2000;161:135–40.
Szabo G. Consequences of alcohol consumption on host defense. Alcohol Alcohol. 1999;43:830–41.
Seppä K, Sillanaukee P. Binge drinking and ambulatory blood pressure. Hypertension. 1999;33(1):79–82.
Halanych JH, Safford MM, Kertesz SG, Pletcher MJ, Kim YI, Person SD, et al. Alcohol consumption in young adults and incident hypertension: 20-year follow-up from the Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol. 2010;171(5):532–9.
Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich). 2012;14(11):792–8.
Taylor B, Irving HM, Baliunas D, Roerecke M, Patra J, Mohapatra S, et al. Alcohol and hypertension: gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction. 2009;104(12):1981–90.
•• Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose-response meta-analysis of prospective studies. Eur J Heart Fail. 2015;17(4):367–73. This is an excellent meta-analysis looking at the effects of alcohol and risk of heart failure development.
Bryson CL, Mukamal KJ, Mittleman MA, Fried LP, Hirsch CH, Kitzman DW, et al. The association of alcohol consumption and incident heart failure. J Am Coll Cardiol. 2006;48:305–31.
Larsson SC, Wallin A, Wolk A. Contrasting association between alcohol consumption and risk of myocardial infarction and heart failure: two prospective cohorts. Int J Cardiol. 2017;231:207–10.
Piano MR, Phillips SA. Alcoholic cardiomyopathy: pathophysiologic insights. Cardiovasc Toxicol. 2014;14(4):291–308.
Fernández-Solà J, Estruch R, Nicolás JM, Paré JC, Sacanella E, Antúnez E, et al. Comparison of alcoholic cardiomyopathy in women versus men. Am J Cardiol. 1997;80(4):481–5.
Tanasescu M, Hu FB, Willett WC, Stampfer MJ, Rimm EB. Alcohol consumption and risk of coronary heart disease among men with type 2 diabetes mellitus. J Am Coll Cardiol. 2001;38(7):1836–42.
Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28(3):719–25.
Goldberg IJ, Mosca L, Piano MR, Fisher EA, Nutrition Committee, Council on Epidemiology and Prevention, and Council on Cardiovascular Nursing of the American Heart Association. AHA science advisory: wine and your heart: a science advisory for healthcare professionals from the Nutrition Committee, Council on Epidemiology and Prevention, and Council on Cardiovascular Nursing of the American Heart Association. Circulation. 2001;103(3):472–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Abhishek Sharma, Sunny Goel, and Aakash Garg declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Goel, S., Sharma, A. & Garg, A. Effect of Alcohol Consumption on Cardiovascular Health. Curr Cardiol Rep 20, 19 (2018). https://doi.org/10.1007/s11886-018-0962-2
Published:
DOI: https://doi.org/10.1007/s11886-018-0962-2