Abstract
Purpose of Review
The current definition of heart failure is mainly based on an inappropriate measure of cardiac function, i.e., left ventricular ejection fraction (LVEF). The initial sole entity, heart failure with reduced ejection fraction (HFrEF, LVEF <40%), was complemented by the addition of heart failure with preserved ejection fraction (HFpEF, LVEF ≥50%) and most recently, heart failure with mid-range ejection fraction (HFmrEF, LVEF 40–49%). Initially, HFpEF was believed to be a purely left ventricular diastolic dysfunction. Pathophysiological concepts of HFpEF have changed considerably during the last years. In addition to intrinsic cardiac mechanisms, the heart failure pathogenesis is increasingly considered as driven by non-cardiac systemic processes including metabolic disorders, ischemic conditions, and pro-inflammatory/pro-fibrotic or immunological alterations. Presentation and pathophysiology of HFpEF is heterogeneous, and its management remains a challenge since evidence of therapeutic benefits is scarce. Up to now, there are no therapies improving survival in patients with HFpEF.
Recent Findings
Several results from clinical and preclinical interventions targeting non-cardiac mechanisms or non-pharmacological interventions including new anti-diabetic or anti-inflammatory drugs, mitochondrial-targeted anti-oxidants, anti-fibrotic strategies, microRNases incl. antagomirs, cell therapeutic options, and high-density lipoprotein-raising strategies are promising and under further investigation.
Summary
This review addresses mechanisms and available data of current best clinical practice and novel approaches towards HFpEF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current definition of heart failure (HF) is mainly based on an inappropriate measure of cardiac function, i.e., left ventricular ejection fraction (LVEF), mostly based on echocardiographic assessments. The initial sole entity, HF with reduced ejection fraction (HFrEF, LVEF <40%) was complemented by the addition of HF with preserved ejection fraction (HFpEF, LVEF ≥50%) 15 years ago, and most recently, HF with mid-range ejection fraction (HFmrEF, LVEF 40–49%) was added [1].
In the US alone, 5.7 million adults suffered from HF in 2012 [2]. Half of the patients with symptoms of HF have a preserved ejection fraction (HFpEF) and half of the patients have a reduced ejection fraction (HFrEF). These numbers are thought to increase in the future due to an expected rise in the prevalence of HFpEF in a constantly ageing population. This underlines the huge public health need for the development of therapies to alter the natural history of patients with HFpEF.
In the last decades, there has been a tremendous advance in treating patients with HFrEF, resulting in a declining mortality due to inhibition of the renin angiotensin aldosterone system (RAAS), β blockage, device therapy, and recently neprilysin inhibition [3]. Unfortunately, application of most of those therapies to patients with HFpEF has been unsuccessful in altering long-term results of these patients, where 5-year survival rates can be as poor as 50% [4]. The lack of efficacy of these therapies might underscore the fundamental differences between both these phenotypically distinct forms of HF as well as our incomplete understanding of the pathophysiology.
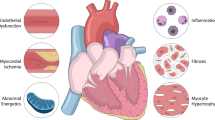
Initially, HFpEF was believed to be a purely LV diastolic dysfunction. Pathophysiological concepts of HFpEF have changed considerably during the last years: in addition to intrinsic cardiac mechanisms, HF pathogenesis is increasingly considered as driven by non-cardiac systemic processes including metabolic disorders, pro-inflammatory/pro-fibrotic or immunological alterations. Recently, a paradigm shift for HFpEF development has been proposed. The new paradigm presumes that a high prevalence of comorbidities such as overweight/obesity, diabetes mellitus, chronic obstructive pulmonary disease, and salt-sensitive hypertension induce a systemic pro-inflammatory state causing coronary microvascular endothelial inflammation and vascular rarefication. Coronary microvascular endothelial inflammation then reduces nitric oxide (NO) bioavailability, cyclic guanosine monophosphate content, and protein kinase G (PKG) activity in adjacent cardiomyocytes. Low PKG activity then favors hypertrophy development and increases resting tension due to hypophosphorylation of titin. Finally, both stiff cardiomyocytes and interstitial fibrosis contribute to high diastolic left ventricular (LV) stiffness and HF development [5•,6••,7] (Fig. 1). None of the established heart failure medications like renin-angiotensin aldosterone inhibitors and beta blockers targeting a neuroendocrine activation were effective in clinical trials to overcome the involved pathophophysiological mechanisms. In the following, we summarize new pharmacological as well as cell and molecular-based HF therapy approaches for HFpEF.
New Developments Among Causal Therapy Strategies for HFpEF
Neurohumoral activation plays a central part in the pathology of HFpEF and has been the main focus in the initial treatment of HFpEF. In recent years, however, our understanding of the pathologies involved in the development of HFpEF evolved and includes now disorders in calcium homeostasis, regulation of the energy homeostasis, disorders in matrix regulation, inflammation, angiogenesis, and oxidative stress (Table 1).
Regulation of the Calcium Homeostasis
Dysregulation of the intracellular calcium homeostasis can lead to a significant LV systolic and diastolic dysfunction [31] by interfering with functions of the ryanodine receptor (RyR2) [32], SERCA2a or the sodium-potassium pump [33].
Although there are currently no patient data available, animal studies have shown that the RyR2 stabilizer, K201 [19], the sodium-potassium pump inhibitor, SES0400 [34], and strategies that improve the functions of SERCA2A [35], all can improve diastolic function.
Regulation of the Energy Homeostasis
It has been shown that in some HFpEF patients, chronically increased β-adrenergic stimulation and an insulin resistance is present, leading to an unfavorable cardiac metabolism situation in addition to a limited energy production [36]. A majority of HFpEF patients also suffer from diabetes. In this regard, incretins and SGLT2 inhibitors may possibly represent an additional therapeutic option in the future for diabetic and non-diabetic HFpEF patients.
Another strategy includes the restoration of mitochondrial energy metabolism by the so-called Szeto-Schiller (SS) peptides like elamipretide (MTP-131).
Incretins
The glucagon-like peptide 1 (GLP-1) is a hormone of the incretin family that is released out of the alimentary canal after sugar loading [37]. GLP receptors have also been shown to be present in the heart [38]. The stimulation of myocardial GLP receptors leads to an increased sugar assimilation of the heart activating especially myocyte glycolysis [39]. This metabolic pathway can be stimulated by two pharmacological therapy strategies: by GLP-1 analogues like exenatide, semaglutide, liraglutide, or by dipeptidyl peptidase 4 inhibitors (DPP-IV) such as sitagliptin, saxapliptin, or linagliptin.
Exenatide was found to be able to improve cardiac diastolic function in diabetic patients [21, 22] and two large phase III trials showed the improvement in prognosis in diabetic patients with cardiovascular risk with semaglutide [23] and liraglutide [24]. Similarly, DPP-IV inhibitors are under investigation with respect to LV diastolic function. In a small study focusing on non-diabetic patients having non-ischemic cardiomyopathy, it was observed that sitagliptin improved myocardial glucose assimilation [25]. Linagliptin and sitagliptin were also able to improve diastolic function in diabetic HFpEF patients with chronic kidney disease [26]. Studies will have to be awaited in order to check whether or not an incretin-based therapy approach with diabetic and/or non-diabetic patients having HFpEF can lead to any improvement of the symptoms or prognosis.
Sodium-Glucose Cotransporter 2 Inhibitors
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, including empagliflocin, dapagliflozin, and canagliflozin, are now widely approved anti-hyperglycemic therapies. Moreover, the results of the EMPA-RREG OUTCOME trial revealing a relative risk reductions of 38% in cardiovascular mortality, 35% reduction in hospitalization for HF, and a 32% reduction in death from any cause using empagliflocin in patients with type 2 diabetes risk have raised the possibility that mechanisms beyond the anti-hyperglycemic actions were observed in the trial [27]. It has been shown that under conditions of mild, persistent hyperketonemia, similar to those during treatment with SGLT2 inhibitors, the heart freely takes up β-hydroxybutyrate and oxidizes it in preference to fatty acids [40]. This in turn improves the transduction of oxygen consumption into work efficiency at the mitochondrial level. In addition, SGLT2 inhibition is typically followed by hemoconcentration and this in turn enhances oxygen release to the tissues, thereby establishing a powerful synergy with the metabolic substrate shift. Empagliflozin is now recommended in diabetic HF patients by the ESC in combination with metformin (IIA recommendation; [41]). Studies are ongoing in non-diabetic patients with HFrEF and HFpEF.
Mitochondria-Targeting Peptides
HF represents a mismatch between supply and demand of ATP. This mismatch may result from damaged mitochondria, decreased mitochondrial production of ATP including increased workload to the myocardium following ischemia, hypertension, or diastolic dysfunction [42, 43]. Damaged mitochondria can augment the generation of ROS. Dysfunction of mitochondria increases the risk for a large number of human diseases, including HF following ischemic heart disease, cardiomyopathies, and cardiac hypertrophy [28]. Current treatments all rely on “energy sparing” by decreasing workload. Targeting mitochondrial plasticity to improve ATP supply may provide an alternative approach to the treatment of HF including HFpEF.
Elamipretide
New mitochondria-targeted antioxidant peptides were developed able to restore the mitochondrial electron transport chain to optimize efficiency of electron transport and restore cellular bioenergetics [44, 45]. The first of these compounds (SS-31; also named MTP-131, elamipretide (Bendavia™)) has entered into clinical development and is studied in phase II clinical trials for HFrEF and HFpEF. However, elamipretide was not able to reduce infarct size in a phase II trial in patients with acute ST-elevation myocardial infarction (EMBRACE STEMI study [28]).
Matrix Regulation
Changes in the structures within the extracellular matrix (ECM) can also affect diastolic function. The myocardial ECM is composed of three important constituents, fibrillar protein, proteoglycans, and basement membrane proteins, whereby it has been shown that the most important component within the ECM that contributes to the development of HFpEF is fibrillar collagen [46]. The regulatory control of collagen biosynthesis and degradation has at least three major determinants: transcriptional regulation, posttranslational regulation, including collagen cross-linking, and enzymatic degradation by matrix metalloproteinases (MMPs) [47]. Pharmacological attempts at MMP inhibition have been found to be over-simplistic and unsuccessful. Future strategies must recognize the diversity of this matrix proteolytic system including its regulation by endogenous inhibitors (TIMPs) [48].
Cross-Link Breakers
Advanced glycation end products (AGEs), molecules formed during a non-enzymatic reaction between proteins and sugar residues, which accumulate in the human body with age, diabetes, renal failure, and enhanced states of oxidative stress, form “cross-links” between matrix proteins like collagen, laminin, and elastin [49], leading to increased rigidity and diastolic dysfunction. Alagebrium chloride, a cross-link breaker, was examined in a small study involving 23 older patients having HFpEF and showed an improvement of diastolic function after 16 weeks [29]. Whether or not these results can also be confirmed subsequently depends on the undertaking of larger studies.
Lysyl Oxidase-Like 2 Inhibition
Lysyl oxidase-like 2 (LOXL2) belongs to the LOX family, which comprises copper-dependent extracellular enzymes that catalyze lysine-derived cross-links of collagen and elastin. Dysregulation of LOXL2 has been linked to many diseases, including cancer, pro-oncogenic angiogenesis, fibrosis, and heart diseases. LOXL2 is essential for interstitial fibrosis and mechanical dysfunction of stressed hearts. Particularly, increased LOXL2 expression leads to upregulated TGF-β2 production, triggering the formation and migration of myofibroblasts with enhanced collagen deposition and cross-linking in the hypertrophic regions of stressed hearts. Antibody-mediated inhibition of LOXL2 in mice has been shown to greatly reduce stress-induced cardiac fibrosis and chamber dilatation, improving systolic and diastolic functions [30]. Further studies are in preparation to prove different concept strategies of cross-link breaking in HFpEF.
Nitric Oxide Metabolism and Vascular Homeostasis
Recently, it was shown that disorders of intracellular nitrogen monoxide-cGMP-PKG (NO-cGMP-PKG) signal cascade which are brought on by oxidative stress are present in HFpEF [50] and lead to the development of concentric remodelling, increased cardiomyocyte stiffness, and an increase of cardiac fibrosis [50, 51]. These findings might lead to the development of new therapy options by specifically intervening in this mechanism via NO donors, phosphodiesterase-5 inhibitors, orally available soluble guanylate cyclase stimulators, or by an additional neprilysin inhibition.
eNOS Enhancer, Sodium Nitrite, Sodium Nitrate
However, activators of endothelial NO synthase (eNOS), like the eNOS transcription amplifier AVE3085, have been examined at least in animal experiments and yielded promising results [8]. In contrast to organic nitrates, the inorganic nitrate-nitrite pathway represents an important alternative route to restore NO signalling in HFpEF [9]. Acute infusion of sodium nitrite was shown in a placebo-controlled trial of patients with HFpEF to preferentially reduce diastolic LV pressures and pulmonary artery pressures during exercise while restoring cardiac output reserve towards normal. Part of this benefit was mediated by vasodilation, but evidence for a direct myocardial benefit, such as increased stroke work, was also observed [52]. Similar effects were seen by inhaled sodium nitrate [10]. Another recent study found that inorganic nitrate (precursor to nitrite), delivered as 1 week of once-daily beetroot juice consumption, improved submaximal exercise endurance [11].
AT1 Receptor Antagonism and Neprilysin Inhibition by LCZ696
LCZ696, a molecule consisting of the AT1 receptor antagonist valsartan and a neprilysin inhibitor, has been shown to stimulate the NO-cGMP-PKG signal cascade and might therefore play an important role in the pathomechanism of HFpEF. Furthermore, neprilysin inhibition prevents also the degradation of GLP-1, which allows the hypothesis that LCZ696 may affect also cardiac metabolism. The PARAMOUNT study [12], a phase II study, investigated the role of LCZ696. The primary endpoint, a decline in NT-proBNP levels after 12 weeks was reached in the LCZ696 group, and in addition after 36 weeks, a reduction of the atrium volumes and an improvement in the NYHA classification were observed. At the moment, the effect of LCZ696 on the mortality of HFpEF patients is being investigated in the phase III PARAGON-HF trial.
Phosphodiesterase-5 Inhibitors
Patients having a pulmonary hypertension often also have a diastolic dysfunction of the left ventricle most probably due to a septum shift from right to left [53]. Not only an improvement of the pulmonary pressure but also of the diastolic function was observed in 44 patients having HFpEF (>50%) and primary pulmonary hypertension after 1 year of phosphodiesterase-5 inhibitor sildenafil treatment [13]. However, these results could not be confirmed in the placebo-controlled RELAX study in which older HFpEF patients without primary pulmonary arteriopathy had been treated with sildenafil [54]. After a treatment of 24 weeks, no improvement of the strain capacity, neither of the diastolic function nor of left ventricular remodelling, could be observed. The application of sildenafil in HFpEF patients without additional primary pulmonary hypertension can therefore not recommended.
cGMP Stimulators
Novel classes of drugs were discovered which enhance cGMP production by targeting the NO receptor soluble guanylate cyclase (sGC). These compounds, the so-called sGC stimulators and sGC activators, are able to increase the enzymatic activity of sGC to generate cGMP independently of NO and have been developed to target this important signalling cascade in the cardiovascular system. One advantage of using this entails the finding that cGMP can be produced even where there is a diminished bioavailability of NO. Available clinical data with, e.g., riociguat and vericiguat, novel direct sGC stimulators, look promising in the treatment of HFrEF [55]. The DILATE-1 trial examined the use of riociguat in patients with HFpEF and pulmonary hypertension [15]. The primary outcome was peak decrease in mean PAP up to 6 h after administration. While there was no significant change in the primary outcome (P = 0.6), riociguat 2 mg significantly increased SV and cardiac index and decreased systolic blood pressure and right ventricular end-diastolic area. Recently, it was shown that vericiguat was well tolerated in HFpEF patients and did not change NT-proBNP at 12 weeks compared with placebo but was associated with improvements in quality of life. Further studies are ongoing to investigate the effects of this drug class in HFpEF [56].
Endothelin Antagonists
Endothelin (ET) receptors have been shown to be able to increase LV hypertrophy and to cause matrix accumulation. ET antagonists have been successfully used in the treatment of pulmonary hypertension and their potential role in the treatment of HFpEF has recently been evaluated. In a phase 2 study, the ETA antagonist sitaxsentan was investigated for a period of 24 weeks. Although there were no improvements in either diastolic function or in LV mass, there was a significant improvement in the exercise tolerance of the patients [16]. Interestingly, in a recent animal study, the dual ETA and ETB antagonist macicentan led to an improvement in diastolic function by abrogating adverse cardiac remodelling via anti-hypertrophic mechanisms and by reducing stiffness [17]. Further studies are pending to determine whether ETA/B receptor antagonists may be useful in the treatment of HFpEF.
Inflammation
Patients with HFpEF exhibit signs of chronic myocardial inflammation [57]. Endothelial activation enables immigration of activated inflammation cells that can activate the local cytokine cascade. Increased cardiac expression of TGF-β stimulates the formation of pro-inflammatory myofibroblasts, which release collagens and chemokines [58,59,60]. In the small D-HART study, the effect of the IL-1 inhibitor anakinra was examined over a period of 14 days in 12 HFpEF patients, who had increased plasma C-reactive protein levels (>2 mg/dl). In this study, load capacity and C-reactive protein levels improved compared to placebo [18]. Whether HFpEF patients without signs of systemic inflammation may benefit from such intervention remains to be shown. Similarly, new adhesion molecule antagonists targeting integrins (ICAM or VCAM) are under investigation as well as the role of colchicine to prevent myocardial invasion of inflammatory cells. Colchicine, traditionally used to treat gout [61], has recently been shown to be successful for the treatment of different inflammatory cardiac disorders, including stable coronary artery disease [62] and postpericarditomy syndrome [63]. Its broad anti-inflammatory actions, comprising the inhibition of neutrophil chemotaxis, adhesion and mobilization, the reduction in superoxide production and the inhibition of inflammasomes and IL-1β production, together with its anti-fibrotic and endothelial-protective features [64], make colchicine an attractive therapeutic agent for the treatment of HFpEF.
New Non-Pharmacological Therapy Approaches for HFpEF
Cell Therapy
T Regulatory Cells
T regulatory cells, a subpopulation of CD4+ cells, constituting 5–10% of the peripheral T cells, play a pivotal role in the induction and maintenance of immune homeostasis and tolerance [65]. Studies in HF [66] and in comorbidities underlying HFpEF such as diabetes mellitus [67], obesity [68], and chronic obstructive pulmonary disease [69] have demonstrated that T regulatory cells can be quantitatively and/or qualitatively impaired and/or were insufficient to balance the immune system. Experimental studies in mouse models of HF [70, 71] have shown the potential of adoptive transfer of T regulatory cells to reduce cardiac inflammation and fibrosis. New technologies make adoptive transfer of T regulatory cells as therapeutic option feasible in patients [72], opening the avenue for T regulatory cell therapy in HFpEF patients.
Mesenchymal Stromal Cells, PLX, and CardAPs
The pathophysiological mechanisms underlying HFpEF [50, 51] on the one hand and the broad spectrum of cardioprotective effects of mesenchymal stromal cells (MSC) on the other hand, including their pro-angiogenic [73], endothelial-protective [74], immunomodulatory [75,76,77,78], and anti-fibrotic features [76], and their ability to be used allogenically [79], make MSC an attractive cell type for the treatment of HFpEF. MSC are most commonly derived from the bone marrow but can be isolated from almost any organ. Placental-derived MSC, termed PLX, are stable adhesive stromal cells isolated from full-term human placentae, cultured on carriers, and expanded in a bioreactor [80]. They have been successfully used for the treatment of experimental hindlimb ischemia [74] and myocardial infarction [73]. Cardiac-derived proliferating cells (CardAPs, former CAPs) are endomyocardial biopsy-derived stromal cells [81] with MSC-like properties [82,83,84]. Intravenous application of both MSC (PLX) and CardAPs is associated with limited cardiac MSC/CardAPs engraftment and induces systemic immunomodulation. These findings together with the existence of the cardiosplenic axis, i.e., the homing of immune cells from the spleen towards the heart and their subsequent role in cardiac remodelling [85], support the hypothesis that the cardioprotective effects of MSC/CardAPs following intravenous application are partly due to their systemic immunomodulatory effects (Fig. 2), a hypothesis which also accounts for regulatory T cells (see infra). The relevance of low-grade inflammation in HFpEF [86] and in comorbidities underlying HFpEF [87] further stresses the benefit of a systemic/intravenous over a solely cardiac-directed cell approach. So far, intracoronary application of cardiosphere-derived cells, heart cell products with anti-fibrotic, anti-inflammatory, and angiogenic properties [88] has been shown to reverse HFpEF in rats by decreasing cardiac fibrosis and cardiac inflammation (cardiac macrophages and leukocytes) despite persistent hypertension and cardiac hypertrophy [89]. Further studies investigating the potential of intravenous MSC/CardAPs in HFpEF models are warranted.
Hypothetical scheme illustrating how mesenchymal stromal cells, PLX, CardAPs, and regulatory T cells following intravenous application exert cardioprotective effects in HFpEF. Mesenchymal stromal cells (MSC), PLX, CardAPs, and regulatory T cells (Tregs) exert cardioprotective effects after intravenous application via (1) direct cardioprotective and systemic immunomodulation which involves (2) modulation of the cardiosplenic axis, i.e., reduction of homing of pro-inflammatory cells towards the heart. The impact of MSC, PLX, CardAPs, and regulatory T cells (Tregs) on low-grade inflammation in non-cardiac tissues including the lung, gut, adipose tissue, and skeletal muscle cannot be excluded and warrants further investigation
MicroRNAs
MicroRNAs (miRNAs) are a class of conserved small non-coding RNA (21–25 nucleotides in length) that regulate gene expression by base-pairing to the complementary mRNA sequences resulting in transcript degradation or translational inhibition [90]. miRNA are important epigenetic regulators of cardiac function. They are implicated in cardiac development and influence genes that are important for HF [91]. Circulating miRNA profiles have been identified to differ between HFpEF from HFrEF (miR-30c, miR-146a, miR-221, miR-328, and miR-375 [130]; miR-125a-5p, miR-190a, miR-550a-5p, and miR-638 [92, 93]). However, the role of circulating miRNAs as biomarkers in HFpEF is still not clear [94]. miRNAs can be in vivo targeted by synthetic molecules (antagomirs and miRNA mimics) [95, 96]. Their potential as therapeutic target for the treatment of HF and specifically HFpEF is currently under investigation [97]. Patient-specific iPS-induced cardiomyocytes offer a model disease system to determine miRNA-mediated mechanisms towards the disease phenotype [98].
High-Density Lipoprotein-Raising Strategies
Epidemiological and clinical studies have consistently demonstrated an inverse correlation between high-density lipoprotein (HDL) cholesterol levels and the incidence of ischemic cardiovascular diseases [99]. The primary mechanism for this protective effect of HDL has been attributed to its role in reverse cholesterol transport, i.e., the centripetal transport of excess cholesterol from peripheral tissue towards the liver for excretion into bile or to steroidogenic organs for steroid hormone synthesis. However, the cardiovascular-protective effects of HDL are reaching far beyond. HDL have direct anti-inflammatory [100, 101], anti-oxidative [102], anti-apoptotic [100, 103], pro-angiogenic [104, 105], anti-fibrotic [100, 106], immunomodulatory [107], and anti-diabetic [108] features, so-called pleiotropic effects, which may contribute in their protective effect against atherosclerosis and ischemic heart disease and explain their protective potential in endothelial dysfunction and non-ischemic heart disease. Low plasma HDL is in fact an independent predictor of endothelial dysfunction in healthy individuals and diabetic patients [109] and a common biomarker for several inflammatory disorders including diabetes mellitus, obesity, atherosclerosis, systemic lupus erythematosus, and rheumatoid arthritis, indicating a link between HDL and immunity. The broad spectrum of protective effects of HDL including their immunomodulatory properties [107] makes HDL-raising strategies interesting to prevent or counteract HFpEF. An increase of HDL via gene transfer with apolipoprotein A-I, the main apolipoprotein of HDL, has been shown to improve diastolic function in LDL receptor-deficient mice involving an increase in endothelial progenitor cell and an improved myocardial vascularity [105]. The failing clinical trials with HDL-raising pharmaca [110], the complexity of the HDL proteome and dysfunctionality of HDL under stress and diabetic conditions [108], and the success of LDL cholesterol-lowering proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors has dempered the HDL field and the development of novel HDL-raising pharmaca. In the attendance for further HDL-increasing treatment options, non-pharmacological strategies including exercise [111] and Mediterranean diet [112] known to increase HDL levels form an attractive alternative counteracting the development of HFpEF.
Conclusion
The management of and clinical research in patients with HFpEF remains an ongoing challenge. HFpEF is a heterogeneous syndrome. Therefore, clinical management and future clinical trials mandate an individualized, phenotype-specific approach instead of a “one-size-fits-all” strategy. Options to improve patients’ symptoms and quality of life include control of fluid overload, heart rate, risk factors, and comorbidities.
Recently, our understanding of the pathological processes involved in HFpEF has led to the discovery of new treatment targets and holds promise for more specific treatment options of HFpEF in the future (Table 1). Some strategies, such as LCZ696, have already been successfully studied in a phase-II trial [12]; other potential treatment targets, e.g., involving cGMP stimulation, mitochondria-targeted antioxidant peptides, new devices, or the role of anti-diabetic drugs like empagliflozin in normoglycaemic patients are currently investigated. The results of these studies will have an important contribution to our understanding of the pathophysiology of HFpEF and will help in generating new hypothesis and new future treatment strategies.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–200.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi:10.1161/01.cir.0000441139.02102.80.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. doi:10.1016/j.jacc.2013.05.019.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9. doi:10.1056/NEJMoa052256.
• Paulus WJ, Tschope C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–71. doi:10.1016/j.jacc.2013.02.092. The new paradigm for HFPEF identifying a systemic proinflammatory state induced by comorbidities as the cause of myocardial structural and functional alterations is decribed in detail
•• Shah SJ, Kitzman DW, Borlaug BA, van Heerebeek L, Zile MR, Kass DA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation. 2016;134(1):73–90. doi:10.1161/CIRCULATIONAHA.116.021884. Due to the phenotypic diversity in HFpEF, personalized therapeutic strategies are proposed and described in detail.
Perez Del Villar C, Savvatis K, Lopez B, Kasner M, Martinez-Legazpi P, Yotti R, et al. Impact of acute hypertension transients on diastolic function in patients with heart failure with preserved ejection fraction. Cardiovasc Res. 2017; doi:10.1093/cvr/cvx047.
Westermann D, Riad A, Richter U, Jager S, Savvatis K, Schuchardt M, et al. Enhancement of the endothelial NO synthase attenuates experimental diastolic heart failure. Basic Res Cardiol. 2009;104(5):499–509. doi:10.1007/s00395-009-0014-6.
Shah AM, Claggett B, Loehr LR, Chang PP, Matsushita K, Kitzman D, et al. Heart failure stages among older adults in the community: the atherosclerosis risk in communities study. Circulation. 2016; doi:10.1161/CIRCULATIONAHA.116.023361.
Simon MA, Vanderpool RR, Nouraie M, Bachman TN, White PM, Sugahara M, et al. Acute hemodynamic effects of inhaled sodium nitrite in pulmonary hypertension associated with heart failure with preserved ejection fraction. JCI Insight. 2016;1(18):e89620. doi:10.1172/jci.insight.89620.
Eggebeen J, Kim-Shapiro DB, Haykowsky M, Morgan TM, Basu S, Brubaker P, et al. One week of daily dosing with beetroot juice improves submaximal endurance and blood pressure in older patients with heart failure and preserved ejection fraction. JACC Heart Fail. 2016;4(6):428–37. doi:10.1016/j.jchf.2015.12.013.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380(9851):1387–95. doi:10.1016/S0140-6736(12)61227-6.
Guazzi M, Vicenzi M, Arena R, Guazzi MD. PDE5 inhibition with sildenafil improves left ventricular diastolic function, cardiac geometry, and clinical status in patients with stable systolic heart failure: results of a 1-year, prospective, randomized, placebo-controlled study. Circ Heart Fail. 2011;4(1):8–17. doi:10.1161/CIRCHEARTFAILURE.110.944694.
Koller B, Steringer-Mascherbauer R, Ebner CH, Weber T, Ammer M, Eichinger J, et al. Pilot study of endothelin receptor blockade in heart failure with diastolic dysfunction and pulmonary hypertension (BADDHY-Trial). Heart Lung Circ. 2016; doi:10.1016/j.hlc.2016.09.004.
Bonderman D, Pretsch I, Steringer-Mascherbauer R, Jansa P, Rosenkranz S, Tufaro C, et al. Acute hemodynamic effects of riociguat in patients with pulmonary hypertension associated with diastolic heart failure (DILATE-1): a randomized, double-blind, placebo-controlled, single-dose study. Chest. 2014;146(5):1274–85. doi:10.1378/chest.14-0106.
Zile MR, Bourge RC, Redfield MM, Zhou D, Baicu CF, Little WC. Randomized, double-blind, placebo-controlled study of sitaxsentan to improve impaired exercise tolerance in patients with heart failure and a preserved ejection fraction. JACC Heart Fail. 2014;2(2):123–30. doi:10.1016/j.jchf.2013.12.002.
Valero-Munoz M, Li S, Wilson RM, Boldbaatar B, Iglarz M, Sam F. Dual endothelin-A/endothelin-B receptor blockade and cardiac remodeling in heart failure with preserved ejection fraction. Circ Heart Fail. 2016;9(11). doi:10.1161/CIRCHEARTFAILURE.116.003381.
Van Tassell BW, Arena R, Biondi-Zoccai G, McNair Canada J, Oddi C, Abouzaki NA, et al. Effects of interleukin-1 blockade with anakinra on aerobic exercise capacity in patients with heart failure and preserved ejection fraction (from the D-HART pilot study). Am J Cardiol. 2014;113(2):321–7. doi:10.1016/j.amjcard.2013.08.047.
Sacherer M, Sedej S, Wakula P, Wallner M, Vos MA, Kockskamper J, et al. JTV519 (K201) reduces sarcoplasmic reticulum Ca(2)(+) leak and improves diastolic function in vitro in murine and human non-failing myocardium. Br J Pharmacol. 2012;167(3):493–504. doi:10.1111/j.1476-5381.2012.01995.x.
van der Meer RW, Rijzewijk LJ, de Jong HW, Lamb HJ, Lubberink M, Romijn JA, et al. Pioglitazone improves cardiac function and alters myocardial substrate metabolism without affecting cardiac triglyceride accumulation and high-energy phosphate metabolism in patients with well-controlled type 2 diabetes mellitus. Circulation. 2009;119(15):2069–77. doi:10.1161/CIRCULATIONAHA.108.803916.
Wang XH, Han LN, Yu YR, Wang C, Wang B, Wen XR, et al. Effects of GLP-1 agonist exenatide on cardiac diastolic function and vascular endothelial function in diabetic patients. Sichuan Da Xue Xue Bao Yi Xue Ban. 2015;46(4):586–90.
Scalzo RL, Moreau KL, Ozemek C, Herlache L, McMillin S, Gilligan S, et al. Exenatide improves diastolic function and attenuates arterial stiffness but does not alter exercise capacity in individuals with type 2 diabetes. J Diabetes Complicat. 2016; doi:10.1016/j.jdiacomp.2016.10.003.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44. doi:10.1056/NEJMoa1607141.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. doi:10.1056/NEJMoa1603827.
Witteles RM, Keu KV, Quon A, Tavana H, Fowler MB. Dipeptidyl peptidase 4 inhibition increases myocardial glucose uptake in nonischemic cardiomyopathy. J Card Fail. 2012;18(10):804–9. doi:10.1016/j.cardfail.2012.07.009.
Connelly KA, Bowskill BB, Advani SL, Thai K, Chen LH, Kabir MG, et al. Dipeptidyl peptidase-4 inhibition improves left ventricular function in chronic kidney disease. Clin Invest Med. 2014;37(3):E172.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28. doi:10.1056/NEJMoa1504720.
Gibson CM, Giugliano RP, Kloner RA, Bode C, Tendera M, Janosi A, et al. EMBRACE STEMI study: a phase 2a trial to evaluate the safety, tolerability, and efficacy of intravenous MTP-131 on reperfusion injury in patients undergoing primary percutaneous coronary intervention. Eur Heart J. 2016;37(16):1296–303. doi:10.1093/eurheartj/ehv597.
Little WC, Zile MR, Kitzman DW, Hundley WG, O'Brien TX, Degroof RC. The effect of alagebrium chloride (ALT-711), a novel glucose cross-link breaker, in the treatment of elderly patients with diastolic heart failure. J Card Fail. 2005;11(3):191–5.
Yang J, Savvatis K, Kang JS, Fan P, Zhong H, Schwartz K, et al. Targeting LOXL2 for cardiac interstitial fibrosis and heart failure treatment. Nat Commun. 2016;7:13710. doi:10.1038/ncomms13710.
Lompre AM, Hajjar RJ, Harding SE, Kranias EG, Lohse MJ, Marks AR. Ca2+ cycling and new therapeutic approaches for heart failure. Circulation. 2010;121(6):822–30. doi:10.1161/CIRCULATIONAHA.109.890954.
Currie S, Elliott EB, Smith GL, Loughrey CM. Two candidates at the heart of dysfunction: the ryanodine receptor and calcium/calmodulin protein kinase II as potential targets for therapeutic intervention—an in vivo perspective. Pharmacol Ther. 2011;131(2):204–20. doi:10.1016/j.pharmthera.2011.02.006.
Hasenfuss G, Pieske B. Calcium cycling in congestive heart failure. J Mol Cell Cardiol. 2002;34(8):951–69.
Kamimura D, Ohtani T, Sakata Y, Mano T, Takeda Y, Tamaki S, et al. Ca2+ entry mode of Na+/Ca2+ exchanger as a new therapeutic target for heart failure with preserved ejection fraction. Eur Heart J. 2012;33(11):1408–16. doi:10.1093/eurheartj/ehr106.
Sedej S, Schmidt A, Denegri M, Walther S, Matovina M, Arnstein G, et al. Subclinical abnormalities in sarcoplasmic reticulum Ca(2+) release promote eccentric myocardial remodeling and pump failure death in response to pressure overload. J Am Coll Cardiol. 2014;63(15):1569–79. doi:10.1016/j.jacc.2013.11.010.
Ashrafian H, Frenneaux MP, Opie LH. Metabolic mechanisms in heart failure. Circulation. 2007;116(4):434–48. doi:10.1161/CIRCULATIONAHA.107.702795.
Drucker DJ. Glucagon-like peptides. Diabetes. 1998;47(2):159–69.
Wei Y, Mojsov S. Tissue-specific expression of the human receptor for glucagon-like peptide-I: brain, heart and pancreatic forms have the same deduced amino acid sequences. FEBS Lett. 1995;358(3):219–24.
Inzucchi SE, McGuire DK. New drugs for the treatment of diabetes: part II: incretin-based therapy and beyond. Circulation. 2008;117(4):574–84. doi:10.1161/CIRCULATIONAHA.107.735795.
Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME trial: a “thrifty substrate” hypothesis. Diabetes Care. 2016;39(7):1108–14. doi:10.2337/dc16-0330.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975. doi:10.1002/ejhf.592.
Shi J, Dai W, Hale SL, Brown DA, Wang M, Han X, et al. Bendavia restores mitochondrial energy metabolism gene expression and suppresses cardiac fibrosis in the border zone of the infarcted heart. Life Sci. 2015;141:170–8. doi:10.1016/j.lfs.2015.09.022.
Dai DF, Chen T, Szeto H, Nieves-Cintron M, Kutyavin V, Santana LF, et al. Mitochondrial targeted antioxidant peptide ameliorates hypertensive cardiomyopathy. J Am Coll Cardiol. 2011;58(1):73–82. doi:10.1016/j.jacc.2010.12.044.
Sabbah HN, Gupta RC, Kohli S, Wang M, Hachem S, Zhang K. Chronic therapy with elamipretide (MTP-131), a novel mitochondria-targeting peptide, improves left ventricular and mitochondrial function in dogs with advanced heart failure. Circ Heart Fail. 2016;9(2):e002206. doi:10.1161/CIRCHEARTFAILURE.115.002206.
Nickel AG, von Hardenberg A, Hohl M, Loffler JR, Kohlhaas M, Becker J, et al. Reversal of mitochondrial transhydrogenase causes oxidative stress in heart failure. Cell Metab. 2015;22(3):472–84. doi:10.1016/j.cmet.2015.07.008.
Covell JW. Factors influencing diastolic function. Possible role of the extracellular matrix. Circulation. 1990;81(2 Suppl):III155–8.
Spinale FG, Coker ML, Bond BR, Zellner JL. Myocardial matrix degradation and metalloproteinase activation in the failing heart: a potential therapeutic target. Cardiovasc Res. 2000;46(2):225–38.
Spinale FG, Villarreal F. Targeting matrix metalloproteinases in heart disease: lessons from endogenous inhibitors. Biochem Pharmacol. 2014;90(1):7–15. doi:10.1016/j.bcp.2014.04.011.
Hartog JW, Voors AA, Bakker SJ, Smit AJ, van Veldhuisen DJ. Advanced glycation end-products (AGEs) and heart failure: pathophysiology and clinical implications. Eur J Heart Fail. 2007;9(12):1146–55. doi:10.1016/j.ejheart.2007.09.009.
Tschope C, Van Linthout S. New insights in (inter)cellular mechanisms by heart failure with preserved ejection fraction. Curr Heart Fail Reps. 2014;11(4):436–44. doi:10.1007/s11897-014-0219-3.
Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28(20):2539–50. doi:10.1093/eurheartj/ehm037.
Borlaug BA, Koepp KE, Melenovsky V. Sodium nitrite improves exercise hemodynamics and ventricular performance in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2015;66(15):1672–82. doi:10.1016/j.jacc.2015.07.067.
Kasner M, Westermann D, Steendijk P, Drose S, Poller W, Schultheiss HP, et al. Left ventricular dysfunction induced by nonsevere idiopathic pulmonary arterial hypertension: a pressure-volume relationship study. Am J Respir Crit Care Med. 2012;186(2):181–9. doi:10.1164/rccm.201110-1860OC.
Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA J Am Med Assoc. 2013;309(12):1268–77. doi:10.1001/jama.2013.2024.
Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, et al. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA J Am Med Assoc. 2015;314(21):2251–62. doi:10.1001/jama.2015.15734.
Pieske B, Maggioni AP, Lam CSP, Pieske-Kraigher E, Filippatos G, Butler J, et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur Heart J. 2017;38(15):1119–27. doi:10.1093/eurheartj/ehw593.
Westermann D, Lindner D, Kasner M, Zietsch C, Savvatis K, Escher F, et al. Cardiac inflammation contributes to changes in the extracellular matrix in patients with heart failure and normal ejection fraction. Circ Heart Fail. 2011;4(1):44–52. doi:10.1161/CIRCHEARTFAILURE.109.931451.
Lindner D, Zietsch C, Tank J, Sossalla S, Fluschnik N, Hinrichs S, et al. Cardiac fibroblasts support cardiac inflammation in heart failure. Basic Res Cardiol. 2014;109(5):428. doi:10.1007/s00395-014-0428-7.
Van Linthout S, Miteva K, Tschope C. Crosstalk between fibroblasts and inflammatory cells. Cardiovasc Res. 2014;102(2):258–69. doi:10.1093/cvr/cvu062.
Van Tassell BW, Seropian IM, Toldo S, Mezzaroma E, Abbate A. Interleukin-1beta induces a reversible cardiomyopathy in the mouse. Inflamm Res. 2013;62(7):637–40. doi:10.1007/s00011-013-0625-0.
Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440(7081):237–41. doi:10.1038/nature04516.
Deftereos S, Giannopoulos G, Papoutsidakis N, Panagopoulou V, Kossyvakis C, Raisakis K, et al. Colchicine and the heart: pushing the envelope. J Am Coll Cardiol. 2013;62(20):1817–25. doi:10.1016/j.jacc.2013.08.726.
Imazio M, Trinchero R, Brucato A, Rovere ME, Gandino A, Cemin R, et al. COlchicine for the prevention of the post-pericardiotomy syndrome (COPPS): a multicentre, randomized, double-blind, placebo-controlled trial. Eur Heart J. 2010;31(22):2749–54. doi:10.1093/eurheartj/ehq319.
Leung YY, Yao Hui LL, Kraus VB. Colchicine—update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015; doi:10.1016/j.semarthrit.2015.06.013.
Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol. 2008;8(7):523–32. doi:10.1038/nri2343.
Tang TT, Ding YJ, Liao YH, Yu X, Xiao H, Xie JJ, et al. Defective circulating CD4CD25+Foxp3+CD127(low) regulatory T-cells in patients with chronic heart failure. Cell Physiol Biochem. 2010;25(4–5):451–8. doi:10.1159/000303050.
Bayry J, Gautier JF. Regulatory T cell immunotherapy for type 1 diabetes: a step closer to success? Cell Metab. 2016;23(2):231–3. doi:10.1016/j.cmet.2016.01.010.
Ilan Y, Maron R, Tukpah AM, Maioli TU, Murugaiyan G, Yang K, et al. Induction of regulatory T cells decreases adipose inflammation and alleviates insulin resistance in ob/ob mice. Proc Natl Acad Sci U S A. 2010;107(21):9765–70. doi:10.1073/pnas.0908771107.
Tan DB, Fernandez S, Price P, French MA, Thompson PJ, Moodley YP. Impaired function of regulatory T-cells in patients with chronic obstructive pulmonary disease (COPD). Immunobiology. 2014;219(12):975–9. doi:10.1016/j.imbio.2014.07.005.
Shi Y, Fukuoka M, Li G, Liu Y, Chen M, Konviser M, et al. Regulatory T cells protect mice against coxsackievirus-induced myocarditis through the transforming growth factor beta-coxsackie-adenovirus receptor pathway. Circulation. 2010;121(24):2624–34. doi:10.1161/CIRCULATIONAHA.109.893248.
Weirather J, Hofmann UD, Beyersdorf N, Ramos GC, Vogel B, Frey A, et al. Foxp3+ CD4+ T cells improve healing after myocardial infarction by modulating monocyte/macrophage differentiation. Circ Res. 2014;115(1):55–67. doi:10.1161/CIRCRESAHA.115.303895.
Abou-El-Enein M, Volk HD, Reinke P. Clinical development of cell therapies: setting the stage for academic success. Clin Pharmacol Ther. 2017;101(1):35–8. doi:10.1002/cpt.523.
Roy R, Brodarac A, Kukucka M, Kurtz A, Becher PM, Julke K, et al. Cardioprotection by placenta-derived stromal cells in a murine myocardial infarction model. J Surg Res. 2013;185(1):70–83. doi:10.1016/j.jss.2013.05.084.
Prather WR, Toren A, Meiron M, Ofir R, Tschope C, Horwitz EM. The role of placental-derived adherent stromal cell (PLX-PAD) in the treatment of critical limb ischemia. Cytotherapy. 2009;11(4):427–34.
Van Linthout S, Savvatis K, Miteva K, Peng J, Ringe J, Warstat K, et al. Mesenchymal stem cells improve murine acute coxsackievirus B3-induced myocarditis. Eur Heart J. 2011;32(17):2168–78. doi:10.1093/eurheartj/ehq467.
Savvatis K, van Linthout S, Miteva K, Pappritz K, Westermann D, Schefold JC, et al. Mesenchymal stromal cells but not cardiac fibroblasts exert beneficial systemic immunomodulatory effects in experimental myocarditis. PLoS One. 2012;7(7):e41047. doi:10.1371/journal.pone.0041047.
Miteva K, Van Linthout S, Volk HD, Tschope C. Immunomodulatory effects of mesenchymal stromal cells revisited in the context of inflammatory cardiomyopathy. Stem Cells Int. 2013;2013:353097. doi:10.1155/2013/353097.
Miteva K, Pappritz K, El-Shafeey M, Dong F, Ringe J, Tschope C, et al. Mesenchymal stromal cells modulate monocytes trafficking in coxsackievirus B3-induced myocarditis. Stem Cells Transl Med. 2017; doi:10.1002/sctm.16-0353.
Hare JM, Traverse JH, Henry TD, Dib N, Strumpf RK, Schulman SP, et al. A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. J Am Coll Cardiol. 2009;54(24):2277–86.
Ramot Y, Meiron M, Toren A, Steiner M, Nyska A. Safety and biodistribution profile of placental-derived mesenchymal stromal cells (PLX-PAD) following intramuscular delivery. Toxicol Pathol. 2009;37(5):606–16. doi:10.1177/0192623309338383.
Haag M, Van Linthout S, Schroder SE, Freymann U, Ringe J, Tschope C, et al. Endomyocardial biopsy derived adherent proliferating cells—a potential cell source for cardiac tissue engineering. J Cell Biochem. 2010;109(3):564–75. doi:10.1002/jcb.22433.
Miteva K, Haag M, Peng J, Savvatis K, Becher PM, Seifert M, et al. Human cardiac-derived adherent proliferating cells reduce murine acute coxsackievirus B3-induced myocarditis. PLoS One. 2011;6(12):e28513. doi:10.1371/journal.pone.0028513.
Haag M, Stolk M, Ringe J, Linthout SV, Tschope C, Sittinger M, et al. Immune attributes of cardiac-derived adherent proliferating (CAP) cells in cardiac therapy. J Tissue Eng Regen Med. 2013;7(5):362–70. doi:10.1002/term.531.
Miteva K, Van Linthout S, Pappritz K, Muller I, Spillmann F, Haag M, et al. Human endomyocardial biopsy specimen-derived stromal cells modulate angiotensin II-induced cardiac remodeling. Stem Cells Transl Med. 2016;5(12):1707–18. doi:10.5966/sctm.2016-0031.
Ismahil MA, Hamid T, Bansal SS, Patel B, Kingery JR, Prabhu SD. Remodeling of the mononuclear phagocyte network underlies chronic inflammation and disease progression in heart failure: critical importance of the cardiosplenic axis. Circ Res. 2014;114(2):266–82. doi:10.1161/CIRCRESAHA.113.301720.
Van Linthout S, Tschöpe C. Inflammation—cause or consequence of heart failure or both? . Current Heart Failure Reports. 2017;In Press.
Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111–7. doi:10.1172/JCI57132.
Smith RR, Barile L, Cho HC, Leppo MK, Hare JM, Messina E, et al. Regenerative potential of cardiosphere-derived cells expanded from percutaneous endomyocardial biopsy specimens. Circulation. 2007;115(7):896–908. doi:10.1161/CIRCULATIONAHA.106.655209.
Gallet R, de Couto G, Simsolo E, Valle J, Sun B, Liu W, et al. Cardiosphere-derived cells reverse heart failure with preserved ejection fraction (HFpEF) in rats by decreasing fibrosis and inflammation. JACC Basic Transl Sci. 2016;1(1–2):14–28. doi:10.1016/j.jacbts.2016.01.003.
Ambros V. microRNAs: tiny regulators with great potential. Cell. 2001;107(7):823–6.
Ohtani K, Dimmeler S. Control of cardiovascular differentiation by microRNAs. Basic Res Cardiol. 2011;106(1):5–11. doi:10.1007/s00395-010-0139-7.
Watson CJ, Gupta SK, O'Connell E, Thum S, Glezeva N, Fendrich J, et al. MicroRNA signatures differentiate preserved from reduced ejection fraction heart failure. Eur J Heart Fail. 2015;17(4):405–15. doi:10.1002/ejhf.244.
Wong LL, Armugam A, Sepramaniam S, Karolina DS, Lim KY, Lim JY, et al. Circulating microRNAs in heart failure with reduced and preserved left ventricular ejection fraction. Eur J Heart Fail. 2015;17(4):393–404. doi:10.1002/ejhf.223.
Schmitter D, Voors AA, van der Harst P. HFpEF vs. HFrEF: can microRNAs advance the diagnosis? Eur J Heart Fail. 2015;17(4):351–4. doi:10.1002/ejhf.259.
Ucar A, Gupta SK, Fiedler J, Erikci E, Kardasinski M, Batkai S, et al. The miRNA-212/132 family regulates both cardiac hypertrophy and cardiomyocyte autophagy. Nat Commun. 2012;3:1078. doi:10.1038/ncomms2090.
Wahlquist C, Jeong D, Rojas-Munoz A, Kho C, Lee A, Mitsuyama S, et al. Inhibition of miR-25 improves cardiac contractility in the failing heart. Nature. 2014;508(7497):531–5. doi:10.1038/nature13073.
Nair N, Gupta S, Collier IX, Gongora E, Vijayaraghavan K. Can microRNAs emerge as biomarkers in distinguishing HFpEF versus HFrEF? Int J Cardiol. 2014;175(3):395–9. doi:10.1016/j.ijcard.2014.06.027.
Kriegel AJ, Gartz M, Afzal MZ, de Lange WJ, Ralphe JC, Strande JL. Molecular approaches in HFpEF: MicroRNAs and iPSC-derived cardiomyocytes. J Cardiovasc Transl Res. 2016; doi:10.1007/s12265-016-9723-z.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study Am J Med. 1977;62(5):707–14.
Van Linthout S, Spillmann F, Riad A, Trimpert C, Lievens J, Meloni M, et al. Human apolipoprotein A-I gene transfer reduces the development of experimental diabetic cardiomyopathy. Circulation. 2008;117(12):1563–73.
Van Linthout S, Spillmann F, Graiani G, Miteva K, Peng J, Van Craeyveld E, et al. Down-regulation of endothelial TLR4 signalling after apo A-I gene transfer contributes to improved survival in an experimental model of lipopolysaccharide-induced inflammation. J Mol Med (Berl). 2011;89(2):151–60. doi:10.1007/s00109-010-0690-6.
Van Linthout S, Spillmann F, Lorenz M, Meloni M, Jacobs F, Egorova M, et al. Vascular-protective effects of high-density lipoprotein include the downregulation of the angiotensin II type 1 receptor. Hypertension. 2009;53(4):682–7.
Spillmann F, Trimpert C, Peng J, Eckerle LG, Staudt A, Warstat K, et al. High-density lipoproteins reduce palmitate-induced cardiomyocyte apoptosis in an AMPK-dependent manner. Biochem Biophys Res Commun. 2015;466(2):272–7. doi:10.1016/j.bbrc.2015.09.034.
Feng Y, Jacobs F, Van Craeyveld E, Brunaud C, Snoeys J, Tjwa M, et al. Human ApoA-I transfer attenuates transplant arteriosclerosis via enhanced incorporation of bone marrow-derived endothelial progenitor cells. Arterioscler Thromb Vasc Biol. 2008;28(2):278–83.
Gordts SC, Van Craeyveld E, Muthuramu I, Singh N, Jacobs F, De Geest B. Lipid lowering and HDL raising gene transfer increase endothelial progenitor cells, enhance myocardial vascularity, and improve diastolic function. PLoS One. 2012;7(10):e46849. doi:10.1371/journal.pone.0046849.
Spillmann F, Miteva K, Pieske B, Tschope C, Van Linthout S. High-density lipoproteins reduce endothelial-to-mesenchymal transition. Arterioscler Thromb Vasc Biol. 2015;35(8):1774–7. doi:10.1161/ATVBAHA.115.305887.
Spillmann F, De Geest B, Muthuramu I, Amin R, Miteva K, Pieske B et al. Apolipoprotein A-I gene transfer exerts immunomodulatory effects and reduces vascular inflammation and fibrosis in ob/ob mice. J Inflamm (Lond). 2016;13:25. doi:10.1186/s12950-016-0131-6.
Van Linthout S, Spillmann F, Schultheiss HP, Tschope C. High-density lipoprotein at the interface of type 2 diabetes mellitus and cardiovascular disorders. Curr Pharm Des. 2010;16(13):1504–16.
Chan NN, Colhoun HM, Vallance P. Cardiovascular risk factors as determinants of endothelium-dependent and endothelium-independent vascular reactivity in the general population. J Am Coll Cardiol. 2001;38(7):1814–20.
Spillmann F, Schultheiss HP, Tschope C, Van Linthout S. High-density lipoprotein-raising strategies: update 2010. Curr Pharm Des. 2010;16(13):1517–30.
Lee BA, Oh DJ. Effect of regular swimming exercise on the physical composition, strength, and blood lipid of middle-aged women. J Exerc Rehabil. 2015;11(5):266–71. doi:10.12965/jer.150242.
Hernaez A, Castaner O, Elosua R, Pinto X, Estruch R, Salas-Salvado J, et al. Mediterranean diet improves high-density lipoprotein function in high-cardiovascular-risk individuals: a randomized controlled trial. Circulation. 2017;135(7):633–43. doi:10.1161/CIRCULATIONAHA.116.023712.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carsten Tschöpe reports Steering Committee or Speaker honoraria from AstraZeneca, Novartis, Berlin Chemie, Servier, Bristol-Meyers Squibb GmbH, Roche, Boeheringer Ingelheim, Bayer Healthcare, and Impulse Dynamics.
Sophie Van Linthout and Behrouz Kherad declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Tschöpe, C., Van Linthout, S. & Kherad, B. Heart Failure with Preserved Ejection Fraction and Future Pharmacological Strategies: a Glance in the Crystal Ball. Curr Cardiol Rep 19, 70 (2017). https://doi.org/10.1007/s11886-017-0874-6
Published:
DOI: https://doi.org/10.1007/s11886-017-0874-6