Abstract
Low high-density lipoprotein cholesterol (HDL-C) levels are associated with incident cardiovascular events; however, many therapies targeting increases in HDL-C have failed to show consistent clinical benefit. Thus, focus has recently shifted toward measuring high-density lipoprotein (HDL) function. HDL is the key mediator of reverse cholesterol transport, the process of cholesterol extraction from foam cells, and eventual excretion into the biliary system. Cholesterol efflux from peripheral macrophages to HDL particles has been associated with atherosclerosis in both animals and humans. We review the mechanism of cholesterol efflux and the emerging evidence on the association between cholesterol efflux capacity and cardiovascular disease in human studies. We also focus on the completed and ongoing trials of novel therapies targeting different aspects of HDL cholesterol efflux.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lowering atherogenic low-density lipoprotein cholesterol (LDL-C) levels via lifestyle and pharmacotherapies, specifically HMG-CoA inhibitors, has clearly led to significant reductions in cardiovascular events [1, 2]. The recent approval of PCSK9 inhibitors, which further decrease LDL-C levels, may also result in clinical benefits [3, 4]. However, a significant residual risk remains and other lipids have also been targeted for therapeutic manipulation.
High-density lipoprotein (HDL), in contrast to LDL, is considered to be anti-atherogenic. HDL cholesterol (HDL-C) levels are inversely proportional to cardiovascular events [5–11] even after adequate LDL-C reduction is achieved [6]. However, therapies that are associated with increased HDL-C levels have not yielded consistent clinical benefit [12]. Niacin significantly increases HDL-C by 20–25 % yet failed to decrease future cardiovascular events in addition to statin therapy in two large randomized controlled trials [13, 14]. Cholesteryl ester transfer protein (CETP) inhibitors have been equally disappointing to date. Torcetrapib can increase HDL-C levels by almost 70 % but was associated with higher mortality rates and cardiovascular events [15]. Similarly, dalcetrapib did not significantly reduce recurrent cardiovascular events in patients with recent acute coronary syndromes [16•].
The failure of therapies targeting HDL-C levels has led to significant interest in directly evaluating HDL’s main anti-atherosclerotic function—the promotion of reverse cholesterol transport. Macrophage-specific cholesterol efflux is the first critical step of reverse cholesterol transport and can be readily measured in humans using high-throughput bioassays. Cholesterol efflux capacity (CEC) has gained significant momentum over the past few years as a potential target for therapy for further cardiovascular disease prevention. This review will briefly highlight the mechanism of cholesterol efflux and then focus on emerging evidence on the association between CEC and cardiovascular disease in human studies.
Mechanism of Reverse Cholesterol Transport and Cholesterol Efflux
Lipid-rich macrophages—foam cells—are induced by oxysterols delivered by LDL and form the core of atherosclerotic plaques in the arterial wall [17]. The apoptosis of macrophages starts an inflammatory cascade that leads to plaque rupture [17–19]. Oxysterols and free cholesterol efflux out of macrophages onto HDL particles, promoting plaque regression and reducing plaque instability [19], and are eventually excreted via the liver and biliary system. This process of reverse cholesterol transport is not only the main anti-atherosclerotic function of HDL but also the main pathway of HDL particle biogenesis and maturation.
HDL particles begin as lipid-poor apolipoprotein A-I (ApoA-I) synthesized by the liver and gut (Fig. 1). These lipid-poor ApoA-I particles (Prebeta-1 HDL) acquire free cholesterol from hepatic and peripheral tissue via ATP binding cassette transporter 1 (ABCA-1). Multiple ApoA-I molecules combine to serve as a protein “cage” for the lipid-rich interior of an HDL particle but only assume around 65 % of the protein mass of a mature HDL particle [18]. There is marked heterogeneity in the protein and phospholipid composition of HDL particles; thus, it is likely that HDL is an umbrella term for a variety of compositionally distinct particles that have a similar density [18, 20].
Reverse cholesterol transport. LCAT lecithin-cholesterol acyltransferase, CETP cholesteryl ester transfer protein, FC free cholesterol, CE cholesterol ester, TF triglycerides, LDL-R LDL receptor (with kind permission from Springer Science + Business Media, Fig. 1 [41])
Lecithin-cholesterol acyltransferase (LCAT) mediates conversion of free cholesterol to cholesteryl ester within the HDL particle. This activity maintains a free cholesterol gradient between the periphery and circulating HDL, promoting continual cholesterol efflux. CETP mediates transfer of these cholesteryl esters to other lipoproteins.
Mature HDL particles can further promote cholesterol efflux in a unidirectional manner via macrophage ATP binding cassette transporter G-1 (ABCG-1) [18–21]. Scavenger receptor class B type 1 (SR-B1) mediates cholesterol efflux and influx between macrophages and mature HDL particles in a bidirectional fashion [18, 19]. Lastly, passive aqueous diffusion of cholesterol is a significant component of cholesterol efflux from the macrophage to mature HDL. The cholesteryl ester in HDL can be delivered to the liver via direct binding to hepatic SR-B1 receptors, with subsequent excretion into the biliary system and out of the body. The complexity of the reverse cholesterol transport pathway allows for multiple putative therapeutic targets; however, animal studies clearly demonstrate that macrophage-specific cholesterol efflux, the first critical step of reverse cholesterol transport, plays a key role in preventing atherosclerosis. Therefore, recent efforts on interrogating HDL function in humans have focused on evaluating the clinical relevance of CEC.
Over the past decade, several assays for measuring CEC have been developed. They all measure the movement of radiolabeled cholesterol from specific cell types to a chosen extracellular acceptor. Extracellular acceptor media vary from ApoB-depleted plasma to whole plasma and can make a large impact on the assay specificity for HDL-mediated CEC [22].
Cholesterol Efflux Capacity and Atherosclerosis
The inverse relationship between CEC and atherosclerosis has been well documented in animal models [19, 21, 23]; however, only recently has this association been explored in human populations. Among the low-risk groups, the first cohort study evaluated CEC in 204 healthy white males undergoing carotid intima media thickness (CIMT) evaluation [24]. CEC was found to be inversely proportional to CIMT, a surrogate marker that is associated with increased atherosclerotic disease risk [25, 26], independent of HDL-C and ApoA-I levels. Interestingly, HDL-C levels were significantly correlated with CEC (r = 0.58, p < 0.0001) but failed to correlate with CIMT. These findings further the notion that the relationship between CEC and atherosclerosis is not completely explained by HDL-C levels. Another study explored the relationship between CEC and coronary atherosclerosis via CT angiography in patients with psoriasis without known coronary artery disease (CAD) [27]. Low CEC was associated with a higher coronary plaque burden— specifically non-calcified plaque—independent of cardiovascular risk factors, including hyperlipidemia.
Both studies assessed CEC in low-risk groups. The first had a relatively low LDL-C level (mean 123 mg/dL) and a relatively low atherosclerotic burden (CIMT 0.66 ± 0.13 mm) for average age [28]. The psoriasis cohort had an average pooled cohort equation risk estimate of less than 3 % and an average LDL-C of 100 mg/dL, with only a minority of patients on statin therapy. HDL function is not part of our current cardiovascular risk assessment model; however, these human studies show that even in the setting of few traditional risk factors, HDL function can still be abnormal and reflect a propensity for atherosclerosis.
The relationship between CEC and coronary atherosclerosis has also been assessed in higher-risk cohorts undergoing coronary angiography. In the first large series, CEC was inversely associated with both presence and severity of angiographic coronary disease, defined as a luminal stenosis >50 % in a major coronary vessel, independent of HDL-C and ApoA-I levels [24]. This landmark study established the association between CEC and coronary atherosclerosis. A similar relationship was reported in a smaller Japanese cohort [29]. In contrast to these studies, another large angiographic cohort revealed no significant association between CEC and angiographic CAD after adjustment for risk factors and HDL-C [30••].
These studies suggest that in lower-risk cohorts, low efflux is associated with prevalent coronary and peripheral atherosclerosis independent of HDL composition but this association is inconsistent in higher-risk individuals presenting for coronary angiogram.
Cholesterol Efflux Capacity and Cardiovascular Events
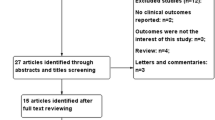
Not only has CEC been assessed with prevalent CAD but also longitudinally with incident atherosclerotic cardiovascular disease (ASCVD) (Fig. 2). Our group studied CEC and incident ASCVD events in 2924 American individuals without known CAD from the Dallas Heart Study [31••]. The average age of this low-risk population cohort was 42, with almost 50 % Blacks, and the median LDL-C was 104 mg/dL. ASCVD was defined as myocardial infarction, stroke, coronary revascularization, or cardiovascular death. Baseline HDL-C was not associated with ASCVD after adjustment for risk factors and total HDL particle (HDL-P) concentration by NMR (hazards ratio (HR) = 1.08, 95 % confidence interval (CI) = 0.59–1.99). CEC was associated with increasing lipid levels but very few other traditional risk factors. The correlation between CEC and HDL-C was weak (r = 0.07, p < 0.05) and modest with HDL-P concentration (r = 0.15, p < 0.05). CEC was inversely associated with ASCVD with no attenuation of the point estimate after adjustment for risk factors, HDL-C, or HDL-P concentration (HR for quartile 4 vs. 1 = 0.33, 95 % CI = 0.19–0.55). This inverse association was graded across increasing quartiles and was similar for the hard end point of nonfatal and fatal myocardial infarction and stroke. The hazard for 1 standard deviation increase in continuous CEC was 0.68 (95 % CI = 0.55–0.84).
Cholesterol efflux capacity (CEC) and risk of incident cardiovascular events. The relationship between increasing cholesterol efflux capacity and incident cardiovascular events is shown for three cohorts. The depicted hazards ratio (HR) and odds ratio (OR) with 95 % CI are adjusted for traditional risk factors. Q quartile, T tertile
A similar study was conducted in the EPIC-Norfolk cohort, using a prospective nested case-control sample of European Caucasians [32••]. There were 1745 cases, defined as those who were hospitalized or died from unstable angina, stable angina, or myocardial infarction. A total of 1749 participants were in the control group, free of coronary disease at follow-up. The 1745 incident cases at baseline were older and more overweight, had worse lipid profiles, and were more likely to have diabetes, hypertension, or a history of smoking. Among the controls, CEC was associated with female sex, total cholesterol, and alcohol intake and inversely associated with measures of adiposity and diabetes. CEC was moderately correlated with HDL-C (r = 0.40, p < 0.05), in contrast with a minimal correlation in the Dallas Heart Study, and modestly correlated with ApoA-I (r = 0.22, p < 0.05) among the controls. Despite this differing correlation between CEC and HDL-C, a similar inverse dose-response relationship with events was found: increasing tertiles of CEC were associated with reduced incidence of coronary heart disease, without attenuation from risk factor adjustment, including HDL-C (odds ratio (OR) tertile 3 vs. 1 = 0.64, 95 % CI = 0.51–0.80). Similar findings were seen with adjustment for ApoA-I levels. The odds ratio for 1 standard deviation increase in continuous CEC was also similar to that seen in the Dallas Heart Study (OR per 1 SD = 0.80, 95 % CI = 0.70–0.90).
The Dallas Heart Study and the EPIC-Norfolk study both studied low-risk populations free of heart disease at baseline. Despite some differences, including CEC assay methodology, levels of risk factors, and ethnicity makeup, both studies revealed similar inverse associations with incident ASCVD. The end points in the Dallas Heart Study included stroke and all CV deaths, whereas those in the EPIC-Norfolk study were specific to coronary ischemia or myocardial infarction. Taken together, these large longitudinal studies extend prior cross-sectional associations with prevalent coronary disease by showing that low baseline CEC predicts incident ASCVD.
In contrast to these consistent relationships between CEC and incident ASCVD among the low-risk cohorts, findings have been mixed in higher-risk cohorts. In a study that prospectively followed 1150 patients without acute coronary syndrome who underwent coronary angiography, 871 patients met criteria for CAD, defined as luminal stenosis >50 % in a major coronary vessel [30••]. Of note, CEC was not associated with prevalent angiographic CAD in this study population after risk factor adjustment. The highest tertile of CEC exhibited an increased risk of both incident nonfatal myocardial infarction, stroke, and cardiovascular death and just incident nonfatal myocardial infarction and stroke, retaining significance in fully adjusted models (HR = 1.85, 95 % CI = 1.11–3.06, and HR = 2.19, 95 % CI = 1.02–4.74, respectively).
Conversely, in the LUdwigshafen RIsk and Cardiovascular Health (LURIC) study of 2450 patients undergoing coronary angiography, there was an inverse correlation between CEC and cardiovascular mortality [33]. This cohort was truly high risk with ∼15 % (N = ∼350) experiencing cardiovascular death. The inverse correlation remained significant after adjustment for traditional cardiovascular risk factors (HR tertile 3 vs. 1 = 0.65, 95 % CI = 0.48–0.88). Both angiographic cohort studies used the same CEC assay methodology. The angiographic cohort showing a positive association with incident events did not exhibit a dose-response relationship between CEC and events, as did the LURIC study and other reports. It remains unclear if patient factors or other aspects of study design led to the differential findings, but it may be that the relationship between efflux and incident cardiovascular events among the high-risk cohorts may vary, whereas the inverse relationship seen among low-risk cohorts has been thus far consistent.
Therapies Targeting HDL Metabolism
LCAT
LCAT mediates esterification of free cholesterol within the HDL particle and is thought to promote efflux by maintaining a free cholesterol gradient between the periphery and HDL molecules. Murine models have shown that LCAT overexpression does not increase CEC [34], and LCAT deficiency only reduced CEC by 50 % [35]. Plasma LCAT levels were measured in a case-control study of the EPIC-Norfolk cohort but did not differ by CAD status [36]. Another case-control study of LCAT activity and incident cardiovascular disease also found no relationship [37]. Thus, it remains unclear if targeting LCAT activity or levels will impact CAD risk; however, recombinant LCAT molecules and LCAT promoter modulators are currently under investigation and further studies in animal and human models are needed [38].
Niacin
The combination of niacin and statin therapy, when compared to statin therapy alone, failed to decrease the risk of recurrent cardiovascular events in the Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglycerides: Impact on Global Health Outcomes (AIM-HIGH) and HPS2-THRIVE clinical trials [13, 14], despite an increase in HDL-C levels. Though niacin does have a modest effect on ABCG-1-specific CEC [39], the overall effect on CEC was likely due to increases in HDL-C concentration. Niacin has not been shown to have a significant effect on ABCA-1-specific efflux, especially in patients already on statin therapy [40, 41]. In addition, the combination of niacin and statin therapy in the AIM-HIGH trial minimally increased ApoA-I levels compared to statin therapy alone. Overall, niacin does not decrease the risk of future cardiovascular events in addition to statin therapy, perhaps partially explained by the lack of significant modulation of CEC—specifically ABCA-1-specific efflux. An intriguing question would be to clarify whether there would be any clinical benefits of niacin in those with low total efflux and HDL-C levels, allowing a more targeted approach.
CETP Inhibitors
CETP inhibitors have not reduced cardiovascular outcomes in large, randomized controlled trials [15, 16•]. In the Dal-ACUTE trial [42••], 300 patients were randomized to 600 mg/day of dalcetrapib or placebo, within 1 week of an acute coronary syndrome. While HDL-C was increased by almost 34 % at 4 weeks in the dalcetrapib arm, CEC was only increased by 9.5 %. Importantly, this increase in CEC was mostly via non-ABCA-1-specific efflux.
Yvan-Charvet et al. compared torcetrapib 60 versus 120 mg/day dosing in a small sample of patients without cardiovascular disease (n = 8 in each arm) for 8 weeks [43]. At the 60 mg daily dosing, no significant difference in CEC was noted at 8 weeks; however, the 120 mg daily dosing did significantly raise CEC. The ILLUMINATE trial used 60 mg daily dosing to evaluate the efficacy of torcetrapib, but it was stopped early due a high rate of adverse outcomes [15]. As noted with dalcetrapib, a significant proportion (40–50 %) of torcetrapib’s effect on cholesterol efflux was non-ABCA-1 specific.
Two new agents in this class are currently undergoing evaluation. We await the results of the ongoing phase 3 trial, REVEAL, in which cardiovascular outcomes are being studied in response to therapy with anacetrapib 100 mg daily in addition to statin therapy (clinicaltrials.gov, identifier: NCT01252953). Anacetrapib has been shown to increase HDL-C by up to 100 % [39]. Perhaps more importantly, this study of 20 patients given 300 mg of anacetrapib showed that at 8 weeks, there was up to a 2.4-fold increase in CEC when compared to the control groups [39]. Furthermore, the increased efflux potential seen with anacetrapib was partly dependent on ABCA-1 expression.
Another phase 3 trial in progress, ACCELERATE, is evaluating the effect of evacetrapib on cardiovascular risk (clinicaltrials.gov, identifier: NCT01687998). Evacetrapib therapy alone increases HDL-C by 54–129 % in a dose-dependent fashion [44] and has been shown to increase total CEC by 28 % and ABCA-1-specific efflux by 17 % [45].
In contrast to torcetrapib and dalcetrapib, anacetrapib and evacetrapib seem to increase both global CEC and ABCA-1-specific efflux. It remains to be seen whether these differential effects on the various efflux pathways will translate into clinical benefit. However, due to the variety of lipid effects of CETP inhibitors, including a reduction in LDL, it may be difficult to assess the specific clinical effects of modulating CEC via CETP inhibition.
ApoA-I
ApoA-I accepts cholesterol from the periphery and forms Prebeta-1 HDL, considered as the primary acceptor of cholesterol via ABCA-1. ApoA-I levels have been inversely associated with incident cardiovascular events [46]. ApoA-I mimetics have been studied in murine and human models, stimulate CEC [47, 48], and have atheroprotective effects [49–52].
The ERASE trial [53] in 2007 randomized 183 patients with recent acute coronary syndromes to placebo or different doses of CSL-111, a recombinant HDL particle consisting of human ApoA-I and phosphatidylcholine. Coronary angiography with IVUS was performed at a time of incident event and at a mean of 44 days later. Though there was a 3.4 % improvement in the primary end point—atheroma volume, as measured by intravascular ultrasound—this was not significant compared to placebo. There was a significant improvement in plaque characterization index and coronary score in the CSL-111-treated arm.
AEGIS-1 is an ongoing phase 2B, randomized placebo-controlled study investigating recurrent cardiovascular event rates with a newer recombinant HDL particle, CSL-112, therapy in 1200 patients with recent acute coronary syndrome (clinicaltrials.gov, identifier: NCT02108262). CSL-112 has been associated with increases in HDL-C levels, Prebeta-1 HDL particles [50], and ABCA-1-specific CEC [47, 48].
RVX-208 is a novel agent that selectively upregulates ApoA-I synthesis and has been shown in animal models to increase ApoA-I levels and ABCA-1-specific and non-ABCA-1-specific cholesterol efflux as well as promote a shift in HDL particle size distribution [54]. This prompted a phase 1 study of patients receiving RVX-208 infusions for 7 days, showing significant increases in ApoA-I levels and ABCA-1-specific cholesterol efflux without significant increases in HDL-C levels [54]. A phase II trial investigated 299 patients with stable CAD on statin therapy [55]. After 12 weeks of RVX-208 infusion, both increases in ApoA-I and HDL-C levels were noted.
The ApoA-I Synthesis Stimulation and Intravascular Ultrasound for Coronary Atheroma Regression Evaluation (ASSURE) and The Study of Quantitative Serial Trends in Lipids with Apolipoprotein A-I Stimulation (SUSTAIN) trials are completed phase 2B trials of RVX-208 [56]. In the ASSURE trial, 310 patients with low HDL-C and angiographic evidence of CAD (at least one stenosis >20 % in an epicardial coronary artery on a clinically indicated coronary angiogram) were randomized to RVX-208 or placebo for 26 weeks. The primary outcome was intravascular ultrasound-guided assessment of atheroma volume. There was no significant difference in atheroma volume in the treated cohort versus placebo [57]. In the SUSTAIN trial, 172 patients with low HDL-C already on statin therapy were randomized to RVX-208 or placebo, with change in HDL-C levels as the primary efficacy marker. Both of these trials analyzed the incidence of major adverse cardiovascular events (MACE) as a secondary outcome. Preliminary results report a 55 % relative risk reduction in MACE (p = 0.02) in the RVX-208 cohort, with a larger beneficial effect in those with diabetes (77 % relative risk reduction, p = 0.01) [58].
Therapies mimicking ApoA-I or targeting ApoA-I metabolism more directly modulate CEC without significant effects on other lipids and will potentially be able to answer the critical question of whether targeting efflux capacity can lead to clinical benefit.
Conclusions
Reverse cholesterol transport is a key anti-atherosclerotic function of HDL and its main protein, ApoA-I. Interrogation of the first critical step of reverse cholesterol transport, macrophage-specific CEC, has revealed significant inverse associations with coronary heart disease in multiple human cohorts. Modulation of CEC, and more specifically, ABCA-1-specific CEC, may prove to be an attractive therapeutic target to reduce cardiovascular risk.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stone NJ et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–S45.
Cholesterol Treatment Trialists, C et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90.
Sabatine MS et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372(16):1500–9.
Robinson JG et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372(16):1489–99.
Assmann G et al. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. 1996;124 Suppl:S11–20.
Barter P et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357(13):1301–10.
Emerging Risk Factors, C et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993–2000.
Gordon T et al. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62(5):707–14.
Prospective Studies Collaboration, Lewington S, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370(9602):1829–39.
Sharrett AR et al. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2001;104(10):1108–13.
Turner RC et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ. 1998;316(7134):823–8.
Keene D et al. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients. BMJ. 2014;349:g4379.
Group, H.T.C. et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–12.
The AIM-HIGH Investigators et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67.
Barter PJ et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–22.
Schwartz GG et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99. Dal-OUTCOMES was a randomized controlled trial studying the effects of CETP inhibition on recurrent cardiovascular events. Over 15,000 patients were randomized to dalcetrapib or placebo and followed for a median of 31 months. Despite a significant increase in HDL-C in the dalcetrapib group, there was no significant reduction in recurrent cardiovascular events. This study emphasized that targeting HDL-C reduction may not reduce cardiovascular events.
Terasaka N et al. High-density lipoprotein protects macrophages from oxidized low-density lipoprotein-induced apoptosis by promoting efflux of 7-ketocholesterol via ABCG1. Proc Natl Acad Sci U S A. 2007;104(38):15093–8.
Rosenson RS et al. Cholesterol efflux and atheroprotection: advancing the concept of reverse cholesterol transport. Circulation. 2012;125(15):1905–19.
Tall AR et al. HDL, ABC transporters, and cholesterol efflux: implications for the treatment of atherosclerosis. Cell Metab. 2008;7(5):365–75.
Rader DJ et al. The role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis. J Lipid Res. 2009;50(Suppl):S189–94.
Out R et al. Combined deletion of macrophage ABCA1 and ABCG1 leads to massive lipid accumulation in tissue macrophages and distinct atherosclerosis at relatively low plasma cholesterol levels. Arterioscler Thromb Vasc Biol. 2008;28(2):258–64.
Rohatgi A. High-density lipoprotein function measurement in human studies: focus on cholesterol efflux capacity. Prog Cardiovasc Dis. 2015;58(1):32–40.
Yvan-Charvet L et al. Combined deficiency of ABCA1 and ABCG1 promotes foam cell accumulation and accelerates atherosclerosis in mice. J Clin Invest. 2007;117(12):3900–8.
Khera AV et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364(2):127–35.
Bauer M et al. Carotid intima-media thickness as a biomarker of subclinical atherosclerosis. Swiss Med Wkly. 2012;142:w13705.
Taylor AJ et al. Progression of calcified coronary atherosclerosis: relationship to coronary risk factors and carotid intima-media thickness. Atherosclerosis. 2008;197(1):339–45.
Salahuddin T, Natarajan B, Playford MP, Joshi AA, Teague H, Masmoudi Y, et al. Cholesterol efflux capacity in humans with psoriasis is inversely related to non-calcified burden of coronary atherosclerosis. Eur Heart J. 2015;36(39):2662–5.
Lim TK et al. Normal value of carotid intima-media thickness—a surrogate marker of atherosclerosis: quantitative assessment by B-mode carotid ultrasound. J Am Soc Echocardiogr. 2008;21(2):112–6.
Ishikawa T et al. High-density lipoprotein cholesterol efflux capacity as a relevant predictor of atherosclerotic coronary disease. Atherosclerosis. 2015;242(1):318–22.
Li XM et al. Paradoxical association of enhanced cholesterol efflux with increased incident cardiovascular risks. Arterioscler Thromb Vasc Biol. 2013;33(7):1696–705. This study prospectively followed 1150 patients with high cardiovascular risk after measuring baseline CEC. The highest tertile of CEC exhibited an increased risk of both incident nonfatal myocardial infarction and cardiovascular death. These results are in contrast with other observational studies.
Rohatgi A et al. HDL cholesterol efflux capacity and incident cardiovascular events. N Engl J Med. 2014;371(25):2383–93. This study analyzed almost 3000 patients in the Dallas Heart Study, a low-risk population free of cardiovascular disease. Baseline CEC was shown to be inversely proportional to ASCVD, even after adjustment for HDL-C levels. This study established that baseline HDL function associates with incident cardiovascular disease.
Saleheen D et al. Association of HDL cholesterol efflux capacity with incident coronary heart disease events: a prospective case-control study. Lancet Diabetes Endocrinol. 2015;3(7):507–13. In this analysis of the EPIC-Norfolk cohort, a low-risk population, increasing tertiles of baseline CEC were associated with a reduced incidence of coronary heart disease. This association did not attenuate after adjustment for HDL-C levels. This study also showed that baseline CEC associates with incident events.
Ritsch A, Scharnagl H, Marz W. HDL cholesterol efflux capacity and cardiovascular events. N Engl J Med. 2015;372(19):1870–1.
Calabresi L, Franceschini G. Lecithin:cholesterol acyltransferase, high-density lipoproteins, and atheroprotection in humans. Trends Cardiovasc Med. 2010;20(2):50–3.
Tanigawa H et al. Lecithin: cholesterol acyltransferase expression has minimal effects on macrophage reverse cholesterol transport in vivo. Circulation. 2009;120(2):160–9.
Holleboom AG et al. Plasma levels of lecithin:cholesterol acyltransferase and risk of future coronary artery disease in apparently healthy men and women: a prospective case-control analysis nested in the EPIC-Norfolk population study. J Lipid Res. 2010;51(2):416–21.
Dullaart RP et al. High plasma lecithin:cholesterol acyltransferase activity does not predict low incidence of cardiovascular events: possible attenuation of cardioprotection associated with high HDL cholesterol. Atherosclerosis. 2010;208(2):537–42.
Rousset X et al. Lecithin cholesterol acyltransferase: an anti- or pro-atherogenic factor? Curr Atheroscler Rep. 2011;13(3):249–56.
Yvan-Charvet L et al. Cholesterol efflux potential and antiinflammatory properties of high-density lipoprotein after treatment with niacin or anacetrapib. Arterioscler Thromb Vasc Biol. 2010;30(7):1430–8.
Khera AV et al. The addition of niacin to statin therapy improves high-density lipoprotein cholesterol levels but not metrics of functionality. J Am Coll Cardiol. 2013;62(20):1909–10.
Mani P, Rohatgi A. Niacin therapy, HDL cholesterol, and cardiovascular disease: is the HDL hypothesis defunct? Curr Atheroscler Rep. 2015;17(8):521.
Ray KK et al. The effect of cholesteryl ester transfer protein inhibition on lipids, lipoproteins, and markers of HDL function after an acute coronary syndrome: the Dal-ACUTE randomized trial. Eur Heart J. 2014;35(27):1792–800. Dal-ACUTE studied 300 patients who were randomized to dalcetrapib or placebo within 1 week of an acute coronary syndrome. Only a modest increase in CEC was noted in the dalcetrapib group and mostly via a non-ABCA-1-mediated pathway. These results demonstrated the effects of dalcetrapib on specific efflux pathways.
Yvan-Charvet L et al. Inhibition of cholesteryl ester transfer protein by torcetrapib modestly increases macrophage cholesterol efflux to HDL. Arterioscler Thromb Vasc Biol. 2007;27(5):1132–8.
Nicholls SJ et al. Effects of the CETP inhibitor evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial. JAMA. 2011;306(19):2099–109.
Rader DJ et al. Abstract 12252: effects of the cholesteryl ester transfer protein inhibitor, evacetrapib, administered as monotherapy or in combination with statins on cholesterol efflux and HDL particles in patients with dyslipidemia. Circulation. 2014;130 Suppl 2:A12252.
van der Steeg WA et al. High-density lipoprotein cholesterol, high-density lipoprotein particle size, and apolipoprotein A-I: significance for cardiovascular risk: the IDEAL and EPIC-Norfolk studies. J Am Coll Cardiol. 2008;51(6):634–42.
Diditchenko S et al. Novel formulation of a reconstituted high-density lipoprotein (CSL112) dramatically enhances ABCA1-dependent cholesterol efflux. Arterioscler Thromb Vasc Biol. 2013;33(9):2202–11.
Gille A et al. CSL112 enhances biomarkers of reverse cholesterol transport after single and multiple infusions in healthy subjects. Arterioscler Thromb Vasc Biol. 2014;34(9):2106–14.
Amar MJ et al. 5A apolipoprotein mimetic peptide promotes cholesterol efflux and reduces atherosclerosis in mice. J Pharmacol Exp Ther. 2010;334(2):634–41.
Krause BR, Remaley AT. Reconstituted HDL for the acute treatment of acute coronary syndrome. Curr Opin Lipidol. 2013;24(6):480–6.
Nissen SE et al. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290(17):2292–300.
Uehara Y et al. FAMP, a novel apoA-I mimetic peptide, suppresses aortic plaque formation through promotion of biological HDL function in ApoE-deficient mice. J Am Heart Assoc. 2013;2(3):e000048.
Tardif JC et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297(15):1675–82.
Bailey D et al. RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo. J Am Coll Cardiol. 2010;55(23):2580–9.
Nicholls SJ et al. Efficacy and safety of a novel oral inducer of apolipoprotein a-I synthesis in statin-treated patients with stable coronary artery disease a randomized controlled trial. J Am Coll Cardiol. 2011;57(9):1111–9.
Nicholls SJ et al. ApoA-I induction as a potential cardioprotective strategy: rationale for the SUSTAIN and ASSURE studies. Cardiovasc Drugs Ther. 2012;26(2):181–7.
Barylski M et al. Emerging therapies for raising high-density lipoprotein cholesterol (HDL-C) and augmenting HDL particle functionality. Best Pract Res Clin Endocrinol Metab. 2014;28(3):453–61.
Wong NC et al. Abstract 338: effects of RVX-208 a selective bromodomain extra-terminal protein inhibitor beyond raising ApoA-I/HDL. Arterioscler Thromb Vasc Biol. 2015;35 Suppl 1:A338.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Anish Bhatt declares no conflict of interest.
Anand Rohatgi declares grants from the National Heart, Lung, and Blood Institute (NIH under award number K08HL118131) and Merck, personal fees from Vascular Strategies and CSL Limited for consultant work, personal fees from Cleveland HeartLab for serving on the advisory board, personal fees from Astra Zeneca for the Speaker’s Bureau, and non-financial support from Eli Lilly for being a site PI for the ACCELERATE trial (evacetrapib).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Bhatt, A., Rohatgi, A. HDL Cholesterol Efflux Capacity: Cardiovascular Risk Factor and Potential Therapeutic Target. Curr Atheroscler Rep 18, 2 (2016). https://doi.org/10.1007/s11883-015-0554-1
Published:
DOI: https://doi.org/10.1007/s11883-015-0554-1