Abstract
Handan has been experiencing severe air pollution with significantly high fine particulate matter (PM2.5) and ozone (O3) levels in recent decades, but its health and economic outcomes have not been well understood. In this study, health effects due to PM2.5 and O3 by exposure-response functions during 2015 to 2017 were quantified. The corresponding economic loss was evaluated based on the value of statistical life (VSL). The years of life lost (YLL) due to PM2.5 exposure was also estimated. Annual average O3 concentration increased by 35.1% from 2015 to 2017 compared to 2015, while PM2.5 concentration decreased by 6.6%. Premature mortality of PM2.5 exposures due to cerebrovascular disease (CEVD, 6209) was the highest, followed by ischemic heart disease (IHD, 3476), lung cancer (LC, 1415), and chronic obstructive pulmonary disease (COPD, 1265) in 2017. The estimated total premature deaths in Handan due to PM2.5 were 12,361 (CI95: 5897–16,388), 11,802 (CI95: 5524–15,853), and 12,365 (CI95: 5848–16,528) people in 2015–2017. The total years of life lost (YLLtotal) attributed to PM2.5 exposures was 119,028, 113,826, and 118,239 in 2015, 2016, and 2017, respectively. The premature deaths and total YLL of female due to PM2.5 exposures were 5317 and 47,529, and those of male were 7049 and 70,710 in 2017. O3-associated COPD premature mortalities and YLLtotal in 2017 were 2.16 and 2.14 times more compared to 2016. Economic losses associated with PM2.5 and O3 exposures were 18.0, 19.3, and 22.8 billion Chinese Yuan (CNY), accounting for 5.73%, 5.78%, and 6.21% of Handan’s gross domestic product (GDP) in 2015, 2016, and 2017, respectively. Premature mortality and YLL due to PM2.5 exposures would be reduced by 84.7% and 85.0% when PM2.5 was reduced to WHO Air Quality Guidelines (AQG) of 10 μgm−3. This study improves the understanding of adverse health and economic effects of high pollution and indicates that Handan needs to adopt more stringent measures to decrease PM2.5 and avoid O3 increase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Air pollution is associated with human health, ecosystem, and climate effects. Fine particulate matter (PM2.5) and ground-level ozone (O3) are two major contributors to hazardous air pollution. PM2.5 is a complex mixture of directly emitted components such as organic carbon and elemental carbon and secondarily formed components including nitrate, sulfate, ammonium, and secondary organic aerosol with aerodynamic diameter of 2.5 μm or less. O3 is a reactive gaseous pollutant and strong oxidant formed by photochemical reactions involving volatile organic compounds and nitrogen oxides in the presence of sunlight (ultraviolet radiation) (Gao et al. 2017). Epidemiological studies establish related relationships between long-term exposure to PM2.5 and premature human mortality due to cerebrovascular disease (CEVD), ischemic heart disease (IHD), lung cancer (LC), and chronic obstructive pulmonary disease (COPD), and thereby substantially reducing life expectancy (Apte et al. 2015; Burnett et al. 2014; Hajizadeh et al. 2020; Lelieveld et al. 2013; Lelieveld et al. 2015). O3 is the second major contributor to hazardous air quality with health risk by respiratory disease, including COPD linked to increased O3 (Abdolahnejad et al. 2018; Carey et al. 2013; Jerrett et al. 2009; Lelieveld et al. 2015).
PM2.5 and O3 have attracted much attention in China. Besides the investigations of high concentrations of PM2.5 and O3, the adverse health effects have been estimated. By adopting the integrated exposure-response (IER) function (Burnett et al. 2014) to the global burden of disease due to PM2.5 exposure (GBD 2013), Lelieveld et al. (2015) reported 1.36 million premature mortalities attributed to PM2.5 and O3. A number of studies proved the adverse effects of PM2.5 on premature mortality (Hu et al. 2017; Lin et al. 2016; Liu et al. 2016; Shang et al. 2013; Song et al. 2017; Xie et al. 2016) in national and regional scales domestically. For instance, Liu et al. (2016) and Hu et al. (2017) estimated that adult premature deaths linked to PM2.5 exposure in China. In addition to premature mortality, years of life lost (YLL) is also very meaningful for estimations of the health burden due to PM2.5 pollution and environmental policy decision. There are some studies analyzed PM2.5-/O3-related YLL (Ghude et al. 2016; Guo et al. 2018; Guo et al. 2013; Nie et al. 2018; Pope III et al. 2009), and most of them mainly focus on estimating health impacts on national/regional scales. The estimation of health effects at the city level was relatively less.
Economic losses arising from PM2.5- and O3-related health burden are also of great interest. A number of studies on value of statistical life (VSL) were conducted in different regions (Bayat et al. 2019; Gao et al. 2015; Ghude et al. 2016; Hammitt et al. 2019; Huang and Zhang 2013; Lu et al. 2016; Viscusi and Masterman 2017; Zeng et al. 2019). Using the Benefits Mapping and Analysis Program (BenMap) model, Zeng et al. (2019) estimated that the total economic losses due to premature deaths, hospital admissions, and morbidity were 126.25 billion Chinese Yuan (CNY), about 1.53% of China’s GDP. Lu et al. (2016) presented that economic loss of premature death and morbidity attributable to NO2, SO2, O3, and PM10 using the VSL and cost of illness (COI) methods. The economic loss was 91,458 to 156,714 million CNY and was about1.4–2.3% of the annual GDP in 2013. Gao et al. (2015) assessed that the economic loss of health impacts was 1571.8 (95% CI: 1054.0, 2051.1) million CNY during the January 2013 haze in Beijing and might be 0.08% of the local GDP.
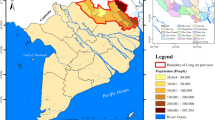
Handan, located in the south of Hebei province in the North China Plain, suffers with severe PM2.5 concentrations. Unlike other regions in the country, in addition to slower decrease of PM2.5 concentrations in recent years, O3 concentration is increasing gradually. However, the health and economic effects of high PM2.5 and O3 in Handan have not been well understood.
Therefore, this study aims (1) to investigate the characteristics of PM2.5 and O3; (2) to estimate premature mortalities (cause-specific and age-specific) and YLL linked to PM2.5 and O3 exposures for adults by applying integrated exposure-response functions in Handan for 2015–2017; (3) to assess the economic losses resulted from PM2.5 and O3 pollution; and (4) to examine the potential health benefits of PM2.5 concentrations in five reduction targets. In particular, this is the first study assessing health damage of O3 and related economic loss in Handan. This study also focused on health benefits of both PM2.5 and O3 at city level. This study should be of important value to the government for designing comprehensive goals and measures in reducing air pollution in Handan.
Data and methods
PM2.5 and O3 concentrations
PM2.5 hourly concentrations and O3 daily maximum 8-h concentrations in 2015–2017 in four air quality monitoring sites in Handan were downloaded from the website of the Chinese Environmental Protection Bureau (http://www.cnemc.cn/). The sites are Cong Tai Park, East Sewage Treatment Plant, Environmental Protection Bureau (all loaded in Cong Tai District), and Handan Mining Institute (loaded in Han Shan District) (Fig. S3). Strict quality control and assurance have been conducted by the Chinese Ministry of Environmental Protection before pollutant concentrations publication, following the Technical Guideline on Environmental Monitoring Quality Management (HJ 630-2011). The 8-h peak ozone concentrations were calculated based on hourly concentrations. The daily average concentrations of each pollutant were calculated when these data are valid (considering more than 16 h) for analysis.
Estimation of premature mortality
The premature mortalities for PM2.5- and O3-related diseases were estimated according to the human health impact function given in Eq. (1) (Anenberg et al. 2010).
where ΔMort is premature deaths for a given disease due to PM2.5/O3 exposure; y0 is the baseline mortality rate attributed to a given disease for a certain population in Handan as given in Table S1-S3. The baseline mortalities of sex 10-year age groups in 2015–2017 were from the China Public Health and Family Planning Statistical Yearbook 2016–2018. The RR is relative risk for a given disease due to long-term exposure, and the expression (RR−1)/RR represents the attributable fractions (AFs), which is the fraction of mortality for a given disease. The Pop is the population for given age group, and the age distributions in 2015–2017 (see Table S4) were obtained from the China Statistical Yearbook.
The RRs of premature deaths attribute to CEVD, IHD, LC, and COPD linked with long-term exposure to PM2.5 pollution are obtained based on the integrated exposure-response (IER) model concluded by Burnett et al. (2014) as shown in Eqs. 2 and 3. Burnett et al. considered much higher PM2.5 exposure concentration in the model, which may adapt those countries with higher PM2.5 (such as East and South Asia). It is assumed that PM2.5 toxicity depends on concentration instead of sources or chemical compositions.
where Ccf is the threshold concentration under which there is no additional risk and C is the mean PM2.5 concentration. A total of 1000 sets of α, γ, δ, and Ccf values were used in Monte Carlo simulations for four diseases category for adult. Dataset is obtained from the Global Health Data Exchange website (http://ghdx.healthdata.org/sites/default/files/record-attached-files/IHME_CRCurve_parameters.csv, last access: 14 March 2018). In this study, RR is estimated for the total population above the age of 25. We also adopted the bounds to represent the 95% confidence interval (CI) of RR based on the contents above.
The exposure-response function recommended by Ostro (2004) was used to calculate O3-related COPD:
where C0 refers to the threshold concentration of 37.6 ppb suggested by Lim et al. (2012). The β(0.1521) is the coefficient to show the association between concentration and RR obtained from Lim et al. (2012). Uncertainties and sensitivity of the shape of exposure-response functions were briefly discussed in previous studies (Burnett et al. 2014; Lim et al. 2012).
Estimation of years of life lost
YLL is an important part of disability-adjusted life year (DALY). As a precise term to evaluate the burden of diseases, YLL also helps to explain the health effects of PM2.5 pollution. YLL can be predicted by the DALY calculation template (http://www.who.int/healthinfo/global_burden_disease/tools_national/en/). There are four diseases (CEVD, IHD, LC, and COPD) involved in estimating total YLL in this study. The YLL per 1000 people (YLL/1000) is calculated by Eq. (5):
where YLLtotal is the YLL of male and female for specific group, and Poptotal is the total population for given year.
Economic loss assessment
The VSL was used to further assess economic losses due to PM2.5- and O3-related premature death in Handan from 2015 to 2017. VSL is a measure of total monetary value of individual mortality risk reduction and is widely used in economic assessment of environmental health and safety risk policies. In this work, the unit economic loss of health impacts comes from historical research results. Authoritative results from previous publications of similar study scopes or years were selected to provide reliable benchmarks for estimating economic benefits. Equation (6) (Mu and Zhang 2015; Zeng et al. 2019) shows the procedure used to estimate VSL of Handan. The benchmark unit economic cost of death was obtained from Huang and Zhang (2013) whose estimations were successfully applied on the Beijing-Tianjin-Hebei region and the value is 0.908 million CNY for the base year of 2010.
where VSLn indicates the unit value of statistical life in the year of n, income is the per capita disposable income, VSLbase is the value of a statistical life of the base year (2010), and β is the income elasticity (β = 1.4).
Health benefits of PM2.5 reduction
Based on WHO PM2.5 guidelines, five reduction PM2.5 standards were selected to estimate the potentially avoidable premature mortality and YLL by reducing PM2.5 concentrations in Handan, i.e., WHO IT1 of 35 μgm−3 (or Chinese Ambient Air Quality Standard (CAAQS) grade II), WHO IT2 of 25 μgm−3, WHO IT3 of 15 μgm−3 (CAAQS grade I), the US Ambient Air Quality Standards (US AAQS) of 12 μgm−3, and WHO Air Quality Guidelines (AQG) of 10 μgm−3, respectively. We considered 8-h mean concentration of 100 μgm−3 (46.7 ppb) for O3. We assume that the cause-specific premature death rates are independent of PM2.5 concentrations. The age distribution and population were unchanged in all circumstances.
Results and discussions
PM2.5 and O3 characteristics and RRs
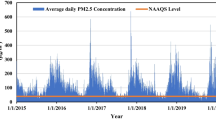
Figure 1 and Figure S1 list the monthly and seasonal variations of PM2.5 and O3 in 2015–2017. Annual average PM2.5 concentrations these years were 91 (± 43), 81 (± 46), and 86 (± 38) μgm−3, much higher than the CAAQS grade II of 35 μgm−3. Especially, December 2015, December 2016, and January 2017 had severe pollution with concentrations of 173, 234, and 170 μgm−3, respectively. PM2.5 concentrations in spring (from March to May), summer (from June to August), and fall (from September to November) in 2017 were higher than those in 2016, while it was lower in winter (from December to February) 2017 than in 2016 with extremely high value of 116 μg/m3. The changing trends suggested that the efforts were not enough to effectively cut air pollution as requested by the local air pollution action plan. PM2.5 in Handan rebounded in 2017 while it decreased in the Beijing-Tianjin-Hebei region (9.9%) and the whole country (4.5%).
A remarkable seasonal variation of PM2.5 was found with the highest value of 116 μgm−3 in winter and the lowest of 64 μgm−3 in summer in 2017. Higher PM2.5 concentrations in winter were likely attributed to more frequently stagnant weather with weak wind, relatively low boundary layer height, and higher anthropogenic emissions in Handan. New particle formations and secondary aerosol productions could further lead to increase of PM2.5 (Chen et al. 2008; Guo et al. 2014; Huang et al. 2014; Zhang and Cao 2015). PM2.5 was at lowest level in summer because of reducing fossil fuel and biomass burning of domestic heating. Higher atmospheric mixing layer could also result in stronger dilution effect of atmosphere (Yoo et al. 2014; Zhang and Cao 2015).
Figure 1 also shows monthly variations of O3 in Handan from 2015 to 2017. Annual average O3 concentrations were 37 ± 13, 43 ± 13, and 50 ± 14 ppb, respectively, with a significant increasing rate of 7 ppb/year. The increase of O3 with slightly decrease of PM2.5 from 2015 to 2017 indicates that more comprehensive efforts are needed in pollution control. Since O3 is formed through photochemical reactions that are largely affected by strong solar radiation and high temperatures (Pu et al. 2017), monthly O3 increased gradually from the beginning of year and decreased after summer, reaching maximum level in July. Since there were no major meteorological variations during 2015–2017, monthly variations were consistent in the 3 years and were prominent in warm months. It should be noted that low concentrations PM2.5 while high O3 concentrations from April to October are partially related in addition to the nature of their sources and formation pathways. PM2.5 could reduce solar radiation and acts as sink of photochemical species; thus, high PM2.5 usually limits high O3 concentrations (Li et al. 2019).
The peak values in July of the 3 years were 54, 69, and 92 ppb, respectively. The significantly high concentration in July 2017 emphasizes the importance of considering O3 in health analysis. O3 concentrations exceeded the WHO standard of 46.7 ppb from May to September. O3 concentration was relatively low from October to March in cold months with the lowest levels of 14, 15, and 21 ppb in December. The increase of O3 was similar across the country (8.0%) and in the Beijing-Tianjin-Hebei region (15.6%).
Figure 2 shows monthly variations of RR due to PM2.5-associated COPD, IHD, LC, and CEVD from 2015 to 2017. The RR (1.92, 1.89, and 1.90) of CEVD due to PM2.5 was highest, followed by IHD and LC, while RR of COPD was the lowest in different months. The RRs of four diseases were higher in winter and lower in summer. As shown in Fig. 3, RRs of O3-associated COPD were significantly high from May to September especially in July. In contrast, RRs from Oct. to Feb. were less than 1, which was regarded as no health risk. O3-related RRs in 2017 were generally higher than the corresponding data in 2015 and 2016 due to increase of O3 concentration. It is implied that more attention should be paid to O3 pollution in summer and more reasonable control policies should be taken in Handan for reduction of both PM2.5 and O3.
Premature mortality and YLL
RRs for disease-specific mortalities were given based on the IER model (Table S5). Among the four diseases, CEVD had the highest RR value, indicating the particularly strong association between PM2.5 exposures and excess cerebrovascular disease mortality. The trends for RRs of IHD and COPD were similar. The AFs (%) of the premature mortality associated with PM2.5 for CEVD, IHD, LC, and COPD were 47% (95% CI 17–57%), 31% (95% CI 22–49%), 32% (95% CI 11–42%), and 25% (95% CI 13–34%) in 2017, respectively (Table S6). The AFs were generally consistent among these 3 years. CEVD had highest AF value followed by IHD and LC while COPD had the lowest estimation. Results were in well accord with previous studies (Apte et al. 2015; Cohen et al. 2017; Evans et al. 2013; Hu et al. 2017; Liu et al. 2016). AFs would significantly decrease if the Handan government improves ambient air quality to meet the WHO IT1, IT2, IT3, and AQG standards. When PM2.5 was lower than 15 μgm−3, IHD had the highest AF and became the major disease rather than CEVD.
The total premature deaths for adults (≥ 25 years old) attributed to COPD, LC, IHD, and CEVD are shown in Table 1. High PM2.5-associated premature mortality occurred in Handan with high population density. The premature mortality associated with PM2.5 from 2015 to 2017 was approximately 12,361 with CI95 of 5897–16,388, 11,802 with CI95 of 5524–15,853, and 12,365 with CI95 of 5848–16,528, respectively.
The disease-specific deaths associated with CEVD, IHD, LC, and COPD in 2015 were 6258, 3263, 1414, and 1425, respectively. The deaths caused by PM2.5 were slightly decreased to 5992, 3246, 1313, and 1251 due to slight reductions of AF in 2016. However, the disease-specific deaths increased to 6209 (CI95 2286–7489), 3475 (CI95 2420–5440), 1415 (CI95 479–1867), and 1265 (CI95 663–1733) in 2017, respectively. This indicates that pollution control measures should be strengthened in Handan. As shown in Table 1, CEVD had the highest PM2.5-related premature mortality, followed by IHD. These outcomes matched with the results from previous estimations (Guo et al. 2018; Hu et al. 2017; Nie et al. 2018). It is implied that the effects of PM2.5 on cerebrovascular diseases were larger than on respiratory diseases. In addition, there were significant differences in death among male and female (Fig. 4) with higher disease-specific deaths in males than in females when ages were lower than 84. The differences mainly resulted from gender-specific baseline mortality rates. Especially, the age group ranged from 65 to 74 revealed the largest differences of disease deaths caused by gender. Premature death for the old females (> 85) was higher than that for old males. It is mainly because of greater female populations in this age group. Figure 4 also provides the total of premature death in different age groups. The aged (> 65) accounted for large percentages of total premature mortality, and premature mortalities at 55–64 group in male were relatively high (1000 people/year), while the younger people less than 44 years old had slightly lower mortality. The differences in baseline mortality rates among age groups resulted in the differences in mortalities. In all diseases attributed to PM2.5 exposures, premature deaths of male were larger than those of female from 2015 to 2017, mainly because of higher all-cause mortalities (COPD, LC, IHD, and CEVD) rates (y0) in males. For example, premature mortality of male was 3493 (CEVD), 1823 (IHD), 987 (LC), and 745 (COPD), while mortality of female was 2716 (CEVD), 1652 (IHD), 428 (LC), and 520 (COPD), respectively in 2017. Moreover, CEVD had the most significant effect on premature mortalities.
For mortalities associated with O3-related COPD, the premature mortalities increased with baseline mortality rate and maximum increase was found for ≥ 60 years old. The premature mortalities were about 42 for 65–74 group, 79 for 75–84 group, and 73 people for ≥ 85 years old, respectively. The greatest premature deaths were found in 75–84 group with large population and high baseline mortality rate. It is revealed that premature age-specific mortalities attributed to O3 exposure showed similarity to those for PM2.5. The aggregated estimation of O3-related COPD premature mortality was about 99 and 214 in 2016 and 2017, respectively. The O3 concentration in 2015 was lower than the threshold concentration, and the premature death was regarded as zero.
Table 2 shows that total YLLs for CEVD, IHD, LC, and COPD attributed to PM2.5 exposures were 119,028, 113,826, and 118,239 years, respectively. The lost years were higher in males than in females, which is mainly because of higher all-cause mortality rates in males. The contribution of ambient PM2.5 was the highest to YLLs for CEVD followed by IHD, LC, and COPD and the risk of cardiovascular system diseases (CEVD and IHD) was higher than that of respiratory system diseases (LC and COPD). YLLT/1000 values (Eq. (5)) for CEVD, IHD, LC, and COPD were 8.81, 4.61, 2.49, and 1.44 years in 2017, respectively. Same as the premature mortality, 65–74 age group had the largest YLL in all groups (Fig. 4). There was small difference in YLL among genders for age groups of 75–84 and 25–34. YLLs of elder females (> 85) were higher than that of males, while YLLs of elder males were higher than elder female among 35–74 years. The estimated total YLLs (> 25 years old) in Handan were 1785 years per 100,000 (in 2015), higher than the estimations from Nie et al. (2018). The YLLs per 100,000 were also much higher than that of the developed countries in 2015 (Cohen et al. 2017), such as 337.1 years for DALY per 100,000 in the USA and 261.7 years in Japan. YLLs caused by CEVD, IHD, LC, and COPD were 59,989, 31,432, 16,983, and 9835 in 2017, respectively. YLLs of COPD attributed to O3 exposure were 777 and 1663 in 2016 and 2017, respectively. The premature deaths and YLLs due to PM2.5 and O3 exposure were very high and more rigorous pollution control policies should be taken in Handan.
Economic losses
The economic losses were calculated for premature deaths due to both PM2.5 and O3 exposures. Established VSL for 2015–2017 was 1.46, 1.62, and 1.81 million CNY, respectively (Table S7). The economic costs of premature death associated with PM2.5 were 18.0, 19.1, and 22.4 billion CNY among three years, and those for O3 exposure were 0.16 (2016) and 0.39 (2017) billion CNY, respectively (Table 3). The total economic losses of O3 and PM2.5 were 18.0, 19.3, and 22.8 billion CNY, accounting for 5.73%, 5.78%, and 6.21% of Handan’s GDP from 2015 to 2017.
It should be noted that the range of VSL was relatively broad and using different values would give different results. Thus, other published methods for calculating VSL were also used and compared for more comprehensive understanding (Table S7). In the recommended method by Organization for Economic Co-operation and Development (OECD) (2014), VSL is estimated in cost-benefit analysis and used for higher income and low-pollution countries or districts as the USA and Europe. This method is calculated country-specific VSL and adjusted by the benefits transfer approach (mainly adjusting the differences in income or national per capita output). As for Lu et al. (2016), method is simplified form for OECD formula, only considering the influence of consumer price index (CPI). The other methods are the same expression form with the different choices of two key factors, being the baseline of VSL and income elasticity (β). The estimated VSL (19.0, 21.8, 23.7 million CNY) for Handan was largest after adjusting the differences in income and GDP per capita suggested by OECD in 2014. This method was used to calculate the national VSL evaluation with the base year of 2005. Similar to Lu et al. (2016), VSL for China in 2010 (0.975 million USD) was selected as the baseline and only considered the consumer price index. The established VSL for Handan was 1.12, 1.21, and 1.26 million USD in 2015, 2016, and 2017, respectively. Hammitt et al. (2019) reported that VSL of Chengdu was 0.55 million USD with β of 1.0–3.0 in 2016 by contingent value method. Using this value as baseline, VSL of Handan was 0.38, 0.41, and 0.41 million USD (β = 1.0) from 2015 to 2017, respectively. If β is 3.0, the VSL would be 0.18, 0.22, and 0.22 million USD, respectively. It should be noted that VSL baseline and income elasticity were critical data and their reliability would affect the assessment of economic losses.
Premature mortality benefits of PM2.5 reduction
The benefits of reducing PM2.5 concentrations were analyzed to encourage more effects in pollution control. Figure 5 shows the normalized premature mortality with proportional reductions (every 10%) in PM2.5 concentrations relative to 2017 concentrations for Handan. The benefits of PM2.5 reductions to total premature mortality increased as PM2.5 concentrations decreased. For example, 10%, 40%, and 80% reductions in PM2.5 in Handan caused 3%, 16%, and 65% reduction in premature deaths assuming the population stay unchanged. A 20% and 50% reduction of PM2.5 concentrations would lead to 4%, 7%, 12%, and 12% and 19%, 21%, 35%, and 35% reductions in premature deaths for CEVD, IHD, LC, and COPD, respectively. The reductions of premature mortality associated with four diseases were 71%, 49%, 71%, and 70% when PM2.5 concentrations reduced by 80%. The benefits of reducing PM2.5 for COPD and LC were higher than those for CEVD and IHD. The benefits trend of COPD and LC was almost identical in eight reduction scenarios. The benefits of reducing PM2.5 for CEVD were smaller than that for IHD at low fraction reduction (< 50%), while the benefits for CEVD were larger than that for IHD when PM2.5 was reduced by larger than 50%.
Figure S2 illustrates the premature death and YLL when PM2.5 concentrations in Handan were reduced to five different standards. Figure 6 shows the potentially avoidable premature deaths, avoidable YLL, and relative changes. When PM2.5 was reduced to 35 μgm−3(CAAQS grade II), the premature mortalities were decreased by 31.4% to 8486 and corresponding total YLLs were reduced by 31.6% to 80,917 years. For CAAQS grade I of 15 μgm−3, premature death and corresponding total YLLs were reduced by 70.2% to 3689 and by 70.5% to 34,830 years, respectively. When PM2.5 was dropped to AQG of 10 μgm−3, premature deaths between 2015 and 2017 due to PM2.5 exposure were reduced by 85.2% from 12,361 to 1824, by 84.6% from 11,802 to 1822, and by 84.7% from 12,365 to 1895 people, respectively, and the avoidable YLLs were reduced by 85.6%, 84.9%, and 85.0%, respectively. This indicates that reduction of PM2.5 has great potential in protecting human health and stricter policies are needed to decrease health impacts of PM2.5 and O3.
Conclusions
High PM2.5 and O3 concentrations caused significant health effects in Handan. Annual PM2.5 concentrations were 91 ± 43, 81 ± 46, and 86 ± 38 μgm−3 in 2015–2017, and annual O3 concentrations were 37 ± 13, 43 ± 13, and 50 ± 14 ppb, respectively. PM2.5 decreased slightly while O3 increased gradually. The total premature mortalities due to O3 exposure were 99 and 214 people, and the corresponding total YLLs were 777 and 1663 years and YLLs per 1000 people were 0.11 and 0.24 years in 2016 and 2017, respectively. The premature deaths and total YLL of female due to PM2.5 exposures were lower than those of male. The premature mortality and YLL due to PM2.5 exposure were 12,365 and 118,239 in 2017, respectively. The economic losses due to PM2.5-associated premature mortality were 18.0–22.4 billion CNY and due to O3 were 0.16–0.39 billion CNY. The total losses accounted for about 6.0% GDP in Handan. CEVD was the main cause of mortality, followed by IHD, COPD, and LC. Reducing PM2.5 concentrations led to great health benefits. When PM2.5 concentrations met the WHO IT1, IT2, IT3, US AAQS, and AQG, mortality benefits were 31.4%, 46.9%, 70.2%, 78.5%, and 84.6% of the total premature mortalities in 2017, respectively. It is recommended that more efforts are needed for protection of human health through keeping lowering PM2.5 and avoiding O3 increases in Handan.
References
Abdolahnejad A, Jafari N, Mohammadi A, Miri M, Hajizadeh Y (2018) Mortality and morbidity due to exposure to ambient NO2, SO2, and O3 in Isfahan in 2013–2014. Int J Prev Med 9:11
Anenberg SC, Horowitz LW, Tong DQ, West JJ (2010) An estimate of the global burden of anthropogenic ozone and fine particulate matter on premature human mortality using atmospheric modeling. Environ Health Pers 118:1189–1195
Apte JS, Marshall JD, Cohen AJ, Brauer M (2015) Addressing global mortality from ambient PM2.5. Environ Sci Technol 49:8057–8066
Bayat R, Ashrafia K, Motlagh MS, Hassanvan MS, Daroudi R, Fink G, Künzli N (2019) Health impact and related cost of ambient air pollution in Tehran. Environ Res 176:108547
Burnett RT, Pope CA III, Ezzati M, Olives C, Lim SS, Mehta S, Shin HH, Singh G, Hubbell B, Brauer M, Anderson HR, Smith KR, Balmes JR, Bruce NG, Kan H, Laden F, Prüss-Ustün A, Turner MC, Gapstur SM, Diver WR, Cohen A (2014) An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Persp 122:397–403
Carey IM, Atkinson RW, Kent AJ, van Staa T, Cook DG, Anderson HR (2013) Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am J Respir Crit Care Med 187:1226–1233
Chen ZH, Cheng SY, Li JB, Guo XR, Wang WH, Chen DS (2008) Relationship between atmospheric pollution processes and synoptic pressure patterns in northern China. Atmos Environ 42:6078–6087
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA III, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH (2017) Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389:1907–1918
Evans J, van Donkelaar A, Martin RV, Burnett R, Rainham DG, Birkett NJ, Krewski D (2013) Estimates of global mortality attributable to particulate air pollution using satellite imagery. Environ Res 120:33–42
Gao M, Guttikunda SK, Carmichael GR, Wang Y, Liu Z, Stanier CO, Saide PE, Yu M (2015) Health impacts and economic losses assessment of the 2013 severe haze event in Beijing area. Sci Total Environ 511:553–561
Gao W, Tie X, Xu J, Huang R, Mao X, Zhou G, Chang L (2017) Long-term trend of O3 in a mega City (Shanghai), China: characteristics, causes, and interactions with precursors. Sci Total Environ 603-604:425–433
Ghude SD, Chate DM, Jena C, Beig G, Kumar R, Barth MC, Pfister GG, Fadnavis S, Pithani P (2016) Premature mortality in India due to PM2.5 and ozone exposure. Geophys Res Lett 43:4650–4658
Guo Y, Li S, Tian Z, Pan X, Zhang J, Williams G (2013) The burden of air pollution on years of life lost in Beijing, China, 2004-08: retrospective regression analysis of daily deaths. BMJ 347:f7139
Guo S, Hu M, Zamora ML, Peng J, Shang D, Zheng J, du Z, Wu Z, Shao M, Zeng L, Molina MJ, Zhang R (2014) Elucidating severe urban haze formation in China. P Natl Acad Sci USA 111:17373–17378
Guo H, Kota SH, Chen K, Sahu SK, Hu J, Ying Q, Wang Y, Zhang H (2018) Source contributions and potential reductions to health effects of particulate matter in India. Atmos Chem Phys 18:15219–15229
Hajizadeh Y, Jafari N, Mohammadi A, Momtaz SM, Fanaei F, Abdolahnejad A (2020) Concentrations and mortality due to short- and long-term exposure to PM2.5 in a megacity of Iran (2014–2019). Environ Sci Pollut Res 27:38004–38014
Hammitt JK, Geng F, Guo X, Nielsen CP (2019) Valuing mortality risk in China: comparing stated-preference estimates from 2005 and 2016. J Risk Uncertainty 58:167–186
Hu J, Huang L, Chen M, Liao H, Zhang H, Wang S, Zhang Q, Ying Q (2017) Premature mortality attributable to particulate matter in China: source contributions and responses to reductions. Environ Sci Technol 51:9950–9959
Huang D, Zhang S (2013) Health benefit evaluation for PM2.5 pollution control in Beijing-Tianjin-Hebei region of China. China Environ Sci 33:166–174
Huang R-J, Zhang Y, Bozzetti C, Ho KF, Cao JJ, Han Y, Daellenbach KR, Slowik JG, Platt SM, Canonaco F, Zotter P, Wolf R, Pieber SM, Bruns EA, Crippa M, Ciarelli G, Piazzalunga A, Schwikowski M, Abbaszade G, Schnelle-Kreis J, Zimmermann R, An Z, Szidat S, Baltensperger U, Haddad IE, Prévôt ASH (2014) High secondary aerosol contribution to particulate pollution during haze events in China. Nature 514:218–222
Jerrett M, Burnett RT, Pope CA III, Ito K, Thurston G, Krewski D, Shi Y, Calle E, Thun M (2009) Long-term ozone exposure and mortality. New Engl J Med 360:1085–1095
Lelieveld J, Barlas C, Giannadaki D, Pozzer A (2013) Model calculated global, regional and megacity premature mortality due to air pollution. Atmos Chem Phys 13:7023–7037
Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A (2015) The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 525:367–371
Li K, Jacob DJ, Liao H, Zhu J, Shah V, Shen L, Bates KH, Zhang Q, Zhai S (2019) A two-pollutant strategy for improving ozone and particulate air quality in China. Nat Geosci 12:906–910
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng ATA, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FGR, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Memish ZA, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CDH, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJC, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJL, Ezzati M (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2224–2260
Lin H, Liu T, Xiao J, Zeng W, Li X, Guo L, Zhang Y, Xu Y, Tao J, Xian H, Syberg KM, Qian Z(M), Ma W (2016) Mortality burden of ambient fine particulate air pollution in six Chinese cities: results from the Pearl River Delta study. Environ Int 96:91–97
Liu J, Han Y, Tang X, Zhu J, Zhu T (2016) Estimating adult mortality attributable to PM2.5 exposure in China with assimilated PM2.5 concentrations based on a ground monitoring network. Sci Total Environ 568:1253–1262
Lu X, Yao T, Fung JCH, Lin C (2016) Estimation of health and economic costs of air pollution over the Pearl River Delta region in China. Sci Total Environ 566-567:134–143
Mu Q, Zhang S (2015) Assessment of the trend of heavy PM2.5 pollution days and economic loss of health effects during 2001–2013. Acta Sci Nat Univ Pekin 51:694–706
Nie D, Chen M, Wu Y, Ge X, Hu J, Zhang K, Ge P (2018) Characterization of fine particulate matter and associated health burden in Nanjing. Int J Environ Res Public Health 15:602
OECD (2014) The cost of air pollution: Health impacts of road transport:1–83
Ostro B (2004) Outdoor air pollution: assessing the environmental burden of disease at national and local levels. Environmental Burden of Disease Series, No 5, WHO, Geneva
Pope CA III, Ezzati M, Dockery DW (2009) Fine-particulate air pollution and life expectancy in the United States. New Engl J Med 360(4):376–386
Pu X, Wang TJ, Huang X, Melas D, Zanis P, Papanastasiou DK, Poupkou A (2017) Enhanced surface ozone during the heat wave of 2013 in Yangtze River Delta region, China. Sci Total Environ 603-604:807–816
Shang Y, Sun Z, Cao J, Wang X, Zhong L, Bi X, Li H, Liu W, Zhu T, Huang W (2013) Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int 54:100–111
Song C, He J, Wu L, Jin T, Chen X, Li R, Ren P, Zhang L, Mao H (2017) Health burden attributable to ambient PM2.5 in China. Environ Pollut 223:575–586
Viscusi WK, Masterman CJ (2017) Income elasticities and global values of a statistical life. J Benefit-Cost Analy 8:226–250
Xie Y, Dai H, Dong H, Hanaoka T, Masui T (2016) Economic impacts from PM2.5 pollution-related health effects in China: a provincial-level analysis. Environ Sci Technol 50:4836–4843
Yoo J-M, Lee YR, Kim D, Jeong MJ, Stockwell WR, Kundu PK, Oh SM, Shin DB, Lee SJ (2014) New indices for wet scavenging of air pollutants (O3, CO, NO2, SO2, and PM10) by summertime rain. Atmos Environ 82:226–237
Zeng X, Ruan F, Peng Y (2019) Health effects’ spatial distribution analysis of PM2.5 pollution in China based on spatial grid scale China. Environ Sci 39:2624–2632
Zhang YL, Cao F (2015) Fine particulate matter (PM2.5) in China at a city level. Scientific Reports 5:14884
Funding
The work is partly supported by open fund by Jiangsu Key Laboratory of Atmospheric Environment Monitoring and Pollution Control (KHK1906), Key Scientific Research Projects of General Institutions of Higher Education in Hebei Province (ZD2020135), Overseas Talents Introduction Funded Project of Hebei Province (C20200308), and the Young Talent Plan of Hebei Province 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 1003 kb)
Rights and permissions
About this article
Cite this article
Gao, A., Wang, J., Luo, J. et al. Health and economic losses attributable to PM2.5 and ozone exposure in Handan, China. Air Qual Atmos Health 14, 605–615 (2021). https://doi.org/10.1007/s11869-020-00964-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-020-00964-x