Opinion Statement
Molecular heterogeneity has confounded attempts to target individual pathways in brain tumors. However, gliomas with BRAF mutations have been identified as being uniquely vulnerable to targeted therapies. Such mutations are predominantly seen in brain tumors of the adolescent and young adult population. Given that accurate and timely identification of such mutations is essential for offering appropriate treatment, treatment centers should offer both immunohistochemical and sequencing methods for detection of these mutations to guide treatment. Additional studies of these tumors at recurrence would also allow identification of breakthrough resistance mechanisms that may also be targetable for treatment. Due to the relative rarity of these tumors, multicenter collaborative studies will be essential in achieving long term control of these tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and Background
The identification of actionable mutations in cancer has heralded the development of highly effective targeted therapies that have made a dramatic impact on several cancers. One such target is BRAF, also known as v-raf murine sarcoma viral oncogene homolog B (B-raf), a proto-oncogene involved in the transduction of vital cellular signals via the mitogen-activated protein kinase (MAPK) pathway [1, 2]. BRAF aberrations cause abnormal cellular proliferation and survival, and are encountered in about 15% of all cancers [3]. These aberrations are relatively frequent in melanoma (66%), non-small-cell lung cancer (40%), colorectal cancer (12%), and hairy cell leukemia (100%) [1, 4]. Extensive genomic sequencing of brain tumors has revealed that although infrequent, BRAF aberrations do occur in these malignancies and provide an opportunity to target tumors in otherwise challenging locations that are not amenable to conventional treatments like surgery and radiation. In addition, recent insights into the mechanisms of resistance BRAF targeted treatments have allowed new approaches to be developed to enhance the activities of these agent with several clinical trials currently in progress evaluating such strategies in BRAF mutant tumors.
Structure and Biological Role of BRAF
The BRAF gene, located on chromosome 7q34 and consisting of 18 exons, encodes B-Raf, a 766 amino acid 94 kD cytoplasmic serine/threonine kinase—a member of the rapidly accelerated fibrosarcoma (Raf) kinase family. There are three isoforms in this family including B-Raf, C-Raf/Raf-1, and A-Raf which share common structural features, including three conserved regions (CR), CR1, CR2, and CR3, which are important for interaction of these proteins with their partners or encode their enzymatic function: CR1 is comprised a Ras-binding domain (RBD) and cysteine-rich domain (CRD) relevant to the Raf autoinhibition and has high homology across the isoforms, CR2 encompasses a conserved Akt phosphorylation site and is involved in negative regulation of Ras/raf activity, and CR3 consists of a catalytic domain which can be regulated by phosphorylation for kinase activation. Other than these three conserved regions, the Raf isoforms show little identity to each other and have different levels of ability to phosphorylate/activate MEK1/2 with the most active being B-Raf followed by C-Raf/Raf-1 and lastly A-Raf [5, 6]. The Raf kinases are components of the RAS/RAF/MEK/ERK/mitogen-activated protein kinase (MAPK) pathway [2], which is a critical signal transduction pathway that regulates several cellular functions such as proliferation, survival, differentiation, and senescence in response to activation of transmembrane tyrosine kinase (Fig. 1, left panel) [1, 2, 7, 8].

Reproduced from Zaman et al. Cancers 2019, 11(8), 1197, without modification under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/)
Illustration of MAPK pathway and mechanism of BRAF aberrations: in BRAF-driven cancers, mutant BRAF (BRAF*) can either act RAS independently as a monomer (class 1) and as a dimer (class 2) or act RAS dependently (class 3) to hyperactivate cellular growth.
Categories of BRAF Aberrations
In human cancers, approximately 200 different BRAF mutant alleles have been identified. BRAF gene aberrations include activating mutations or duplications/fusions that lead to constitutive kinase activity causing the downstream cellular effects such as proliferation and tumor growth [9]. Based on the evidence from BRAF-mutated cancers, in particular melanoma, thyroid, and colon cancers, recent studies have proposed three classes of BRAF mutations [10•, 11]. These classes are based upon the ability of mutant BRAF to transduce signal as monomers or dimers and their dependency on RAS and kinase activity. Understanding the mechanism of these mutant classes has implications for predicting therapeutic response from targeted therapies.
Class I Mutations
These mutations are independent and do not require an upstream RAS activation or dimerization [11]. Point mutations leading to exchange of valine to a different amino acid comprise this class. Most commonly described mutation is c.1799T>A leading to substitution of valine by glutamic acid at position 600 (p.V600E) (Fig. 1, right panel). This leads to conformational change that permits BRAF monomers to an active configuration by releasing the auto inhibitory domain, and ultimately allowing activation of downstream effectors (MEK1/2) without the need for dimerization [11, 12].
Class II Mutations
This category comprises mutation of codons other than V600E with high or intermediate BRAF kinase activity undergoing constitutive, RAS-independent dimerization [10•]. BRAF fusion mutants, other point mutations, and deletions comprise this class (Fig. 1, right panel). A common fusion encountered is KIAA1549-BRAF. In this mutation, the N-terminal dimerization domain of KIAA fuses with C-terminal kinase domain of BRAF leading to loss of the regulatory domain of BRAF that promotes increase affinity for dimerization and independent BRAF kinase activity [13].
Class III Mutations
These mutations require an upstream input and are dependent on RAS for their activity (Fig. 1, right panel). These either have impaired or at times absent kinase activity. The mutant protein causes increased activity by binding tightly to activate RAS compared to the wild-type BRAF and upon dimerization leads to increased activation of the wild-type binding partner [14, 15].
BRAF Aberrations in Brain Tumors
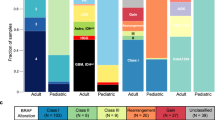
Analysis of data from a large cohort (n = 1320) of adult and pediatric brain tumor patients demonstrated that BRAF aberrations are seen, in order of frequency, in pleomorphic xanthoastrocytoma (PXA) (66%), PXA with anaplasia (65%), ganglioglioma (18%), and pilocytic astrocytoma (PA) (9%) and less frequently in other glial tumors (< 3%) [16]. Another report analyzing a cohort of 969 patients with various types of brain tumors identified 36 cases (4%) with immunohistochemically positive BRAF V600E mutation [17]. Approximately 10% of PA harbor a BRAF V600E mutation (class I) and over 60–70% have KIAA 1549-BRAF fusions (class II) [18,19,20]; mutations and fusion aberrations are noted to be mutually exclusive in PA. PAs with a BRAFV600E mutations typically arise in a non-cerebellar location with a recent systematic review reporting presence of BRAF mutations within exon 18 in 158 cases: the frequency of BRAF mutations in different types of tumors included PA (24/187; 13%), ganglioglioma (54/115; 47%), PXA (49/81; 60%), PXA with anaplasia (9/24; 37%), and epithelioid GBM (22/38; 58%). On the other hand, the KIAA 1549-BRAF fusion was reported in 139 cases, with the following frequency: in PA (120/191; 63%), pilomyxoid astrocytoma (10/13; 77%) and ganglioglioma (9/49; 18%) [21]. Brastianos et al. identified BRAFV600E mutation in 95% all the papillary craniopharyngiomas (CP) in a cohort of 39 patients [22••]. Another report of 73 CP patients identified BRAFV600E mutations in 24.6% and all being papillary CPs [23]. BRAF mutations have been reported in 8.13% of glioma patients, with 6.5% of patients having the canonical BRAFV600E mutation [16, 19•]. Of the 1579 patients queried from various datasets, a BRAF aberration was seen in 116 (7%) with a somatic mutation reported in 6% [24, 25] (data from lower grade glioma: TCGA, PanCancer Atlas; low-grade gliomas: UCSF, 2014; glioma: MSKCC, 2018; glioblastoma: TCGA, PanCancer Atlas; anaplastic oligodendroglioma and anaplastic oligoastrocytoma: MSKCC, 2017; medulloblastoma: Broad Institute, 2012; medulloblastoma: ICGC, 2012; medulloblastoma: PCGP, 2012; medulloblastoma: Sick Kids, 2016; pilocytic astrocytoma: ICGC, 2013) on cBioPortal (Fig. 2).
BRAF Targeted Therapies in the Brain
Targeted approaches include selective inhibition of the BRAFV600E mutant, which has become the standard treatment of BRAF mutant melanoma, NSCLC, Erdheim–Chester disease, among others [26,27,28]. There are three FDA-approved drugs in this class: vemurafenib, dabrafenib, and encorafenib. Since reactivation of ERK signaling is a common mechanism of resistance to RAF inhibitors, RAF inhibitors have been combined with MEK inhibitors in patients with BRAF V600E-mutated tumors. FDA-approved MEK inhibitors include cobimetinib, trametinib, and binimetinib. MEK inhibition alone, on the other hand, is used for tumors with BRAF duplication/fusion [29].
Outcomes/Response Associated with the Targeted Therapies in Brain Tumors
Adult Glioma
VE-BASKET is a phase 2, non-randomized histology-agnostic study that included patients with BRAFV600 mutation-positive tumor types [30•]. The study included seven cohorts of patients with NSCLC, ovarian, colorectal, breast cancers, cholangiocarcinoma, multiple myeloma, and “other tumors.” Patients with brain tumors were required to have histologically confirmed glioma (any grade) and confirmation of BRAF V600E mutation. Patients received vemurafenib 960 mg twice per day continuously in 4-week cycles. Twenty-four patients with gliomas were enrolled: 11 with malignant diffuse glioma (6 with GBM and 5 with anaplastic astrocytoma), 7 with PXA, 2 with pilocytic astrocytoma, 3 with anaplastic ganglioglioma, and 1 with a high-grade glioma, not otherwise specified. One complete response (CR) was observed in a patient with PXA, and five patients achieved partial response (PR): two with PXA, one with anaplastic astrocytoma, one with anaplastic ganglioglioma, and one with pilocytic astrocytoma. The overall response rate in the group was 25% (95% CI 10% to 47%). CR lasted 25.9 months or more (censored at last assessment), and PRs lasted 13.1, 9.9, 7.5, 3.4, and 2.4 months. One patient achieved a PR in the diffuse malignant glioma subgroup and five patients had stable disease.
Wen et al. presented preliminary CNS results of a phase 2, open-label trial of dabrafenib and trametinib in patients with rare tumor types harboring the BRAF V600E mutation [31]. For the high-grade glioma cohort, eligible patients had histologically confirmed recurrent or progressive WHO grade 3 or 4 glioma (including PXA) and had prior treatment with radiotherapy and chemotherapy. The primary endpoint was investigator-assessed overall response rate (ORR) by RANO criteria. An abstract was presented with data on 31 of 37 patients. ORR was 26% (8/31; 95% CI 12–45%), including 1 complete response (CR). Five of 8 responding patients had a duration-of-response ≥ 12 months.
Gangliogliomas
In addition to the VE-BASKET trial summarized above that included three patients with anaplastic gangliogliomas, one of whom achieved a partial response, the evidence of activity of BRAF inhibitors in gangliogliomas is limited to case reports. One review of the literature estimated a complete response in 15% (3/20) and partial response in 50% (10/20) of reported pediatric and adult cases with ganglioglioma/anaplastic ganglioglioma at a median of 3.2 months after starting treatment and an estimated progression-free survival of 14 months. Some of those cases were treated with BRAF monotherapy, while others were treated with BRAF/MEK dual inhibition or a BRAF inhibitor and chemotherapy [32].
Pediatric Low-Grade Astrocytoma
In an abstract presented in 2016, Kieran et al. reported outcomes of treatment with dabrafenib in 32 pediatric patients with relapsed or refractory low-grade glioma [33]. Investigator confirmed overall response was 1 CR and 22 PRs (ORR 72% [95% CI 53–86%]). There were 13 patients with stable disease of ≥ 6 months. The Pediatric Brain Tumor Consortium then reported the results of a multi-center phase 2 study using the MEK1/2 inhibitor selumetinib in 25 patients with recurrent or progressive BRAF-aberrant or NF-1-associated low-grade glioma [34•]. Selumetinib was provided orally at 25 mg/m2 twice daily in 4-week cycles. Nine of 25 patients (36%, [95% CI 18–57]) with pilocytic astrocytomas with BRAF fusion or V600E mutation achieved a partial response with a median follow-up of 36.4 months. Ten of 25 patients (40%, 95% CI [21–61]) with NF-1-associated low-grade glioma achieved a partial response with a median follow-up of 48.6 months. Drobysheva et al. reported two cases of disseminated pilocytic astrocytoma with BRAF V600E and BRAF V600D mutations, treated with dabrafenib or dabrafenib and trametinib, respectively [35]. The former patient had resolution of her leptomeningeal disease after 3 months of therapy. The latter patient had stable disease after 11 months of the combination therapy.
Brain Metastases
The BREAK-MB phase 2 study first examined dabrafenib in 74 and 65 patients with BRAF-V600E mutant melanoma and brain metastases that were treatment naïve or previously treated, respectively. Twenty-nine (39%) and 20 (30%) achieved an overall intracranial response [36]. A pilot study then reported on 19 patients with previously treated symptomatic melanoma brain metastases treated with vemurafenib (960 mg twice daily): 7 patients (37%) achieved > 30% intracranial tumor regression. Three patients (16%) achieved intracranial PR and 13 achieved intracranial stable disease [37]. COMBI-MB is a phase 2 multicenter trial that looks at four cohorts of patients with melanoma and brain metastases [38••]. Preliminary results after a median follow-up of 8.5 months showed that 44 (58%) of 76 patients in cohort A [BRAFV600E-positive, asymptomatic melanoma brain metastases, with no previous local brain therapy, and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1] achieved an intracranial response. Intracranial response by investigator assessment was also achieved in 9 (56%) of 16 patients in cohort B (BRAFV600E-positive, asymptomatic melanoma brain metastases, with previous local brain therapy, and an ECOG performance status of 0 or 1), 7 (44%) of 16 patients in cohort C (BRAFV600D/K/R-positive, asymptomatic melanoma brain metastases, with or without previous local brain therapy, and an ECOG performance status of 0 or 1), and 10 (59%; 33–82) of 17 patients in cohort D (BRAFV600D/E/K/R-positive, symptomatic melanoma brain metastases, with or without previous local brain therapy, and an ECOG performance status of 0, 1, or 2). There have also been reports of response to BRAF or BRAF/MEK inhibition in BRAF V600E mutant non-small-cell lung cancer metastatic to the brain (reported to occur in 1–4% of cases) [39, 40], as well as Erdheim–Chester Disease involving the brain [28].
Mechanisms of Resistance to BRAF Targeted Therapy
Mechanistically three different BRAF targeted therapy resistance patterns have been described in cancers harboring a BRAF aberration. These include intrinsic, adaptive, and acquired resistance mechanisms [41]. Presence of additional aberrations like copy number amplifications results in intrinsic resistance which results in lack of any response to initial treatment. Adaptive resistance or a partial response to the therapy can be seen due to de novo cellular epigenetic and transcription pathway alterations which may manifest as a partial and transient response with subsequent progression. Acquired resistance could result from selective pressures imposed by targeted therapy and resultant emergence of alternative clones within the tumor cell population with heterogeneous genetic alteration that can result in recurrence. It remains to be clarified whether all these resistance mechanisms are applicable to BRAF mutated brain tumor targeted treatments. In cases of PXA and PXA with anaplasia, resistance to targeted therapy with small molecule inhibitors like vemurafenib has been described. The typical BRAF mutation (class I) is often associated with sensitivity to targeted therapies; however, structural variations in the kinase domain such as β3-αC deletions and non-canonical BRAF mutations have been associated with resistant to such therapies [42, 43••]. For example, Wang et al. described that the emergence of secondary mutations in BRAF in addition to the canonical BRAFV600E mutation can confer resistance to dabrafenib in certain brain tumors (ganglioglioma) [44]. In this instance, the tumor showed initial response to dabrafenib but at progression, whole exome sequencing led to the identification of a new BRAF L514V mutation in addition to the initial V600E mutation that was not evident in the pretreatment tumor. The L514 residue is situated in the αC-β4-loop of the BRAF kinase domain. The BRAF kinase domain has a αC-β4-loop within the dimer interface that is crucial for the movements between α C-helix-in and α C-helix-out conformations [45]. This change represents an acquired resistance to targeted RAF inhibitor by inducing ERK signaling, promoting RAF dimer formation and thus promoting tumor growth. Resistance to RAF inhibitors has also been described in a cohort of PA cases due a novel recurrent BRAF insertion (p.V504_R506dup) [46].
Clinical Trials Currently Investigating BRAF Targeted Therapies for Brain Tumors
Presently, there are six clinical trials registered on ClinicalTrials.gov that are either active or in the recruiting stage evaluating BRAF targeted therapies in various primary and secondary brain tumors (ref: www.clinicaltrials.gov) summarized below (Table 1).
Summary and Future Directions
Certain subtypes of brain tumors, such as gangliogliomas and craniopharyngiomas, can be genetically simple and driven only by a BRAF V600E alteration. Higher grade gliomas, on the other hand, constitute a genetically complex disease with the hallmark of heterogeneity. Targeted therapy has had better success in simpler single-mutation-driven tumors, and more thoughtful data-driven combination approaches are needed for the more complex mutation-bearing tumors. Regardless, in light of the aggressiveness and lack of therapeutic options for high-grade gliomas, the presence of BRAF alterations does provide a unique potential for targeted therapy that has otherwise not been generally successful in gliomas. Due to the relative rarity of these events, multicenter collaborative studies will be essential in accruing sufficient numbers of patients and in assessing the potential for combination therapies in the setting of BRAF alterations in these tumors. Similarly, basket trials that are tumor agnostic have created an opportunity to study cancer patients with such rare mutations. Future basket trials and longitudinal natural history studies will be essential for better understanding of the prognosis and therapeutic implications of BRAF-altered gliomas in the pediatric and adult populations.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54. https://doi.org/10.1038/nature00766 (published Online First: 18 June 2002).
Chong H, Vikis HG, Guan KL. Mechanisms of regulating the Raf kinase family. Cell Signal. 2003;15(5):463–9. https://doi.org/10.1016/s0898-6568(02)00139-0 (published Online First: 18 March 2003).
El-Osta H, Falchook G, Tsimberidou A, et al. BRAF mutations in advanced cancers: clinical characteristics and outcomes. PLoS ONE. 2011;6(10): e25806. https://doi.org/10.1371/journal.pone.0025806 (published Online First: 1 Nov 2011).
Tiacci E, Trifonov V, Schiavoni G, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011;364(24):2305–15. https://doi.org/10.1056/NEJMoa1014209 (published Online First: 15 June 2011).
Pritchard CA, Samuels ML, Bosch E, et al. Conditionally oncogenic forms of the A-Raf and B-Raf protein kinases display different biological and biochemical properties in NIH 3T3 cells. Mol Cell Biol. 1995;15(11):6430–42. https://doi.org/10.1128/mcb.15.11.6430 (published Online First: 1 Nov 1995).
Marais R, Light Y, Paterson HF, et al. Differential regulation of Raf-1, A-Raf, and B-Raf by oncogenic ras and tyrosine kinases. J Biol Chem. 1997;272(7):4378–83. https://doi.org/10.1074/jbc.272.7.4378 (published Online First: 14 Feb 1997).
Daum G, Eisenmann-Tappe I, Fries HW, et al. The ins and outs of Raf kinases. Trends Biochem Sci. 1994;19(11):474–80. https://doi.org/10.1016/0968-0004(94)90133-3 (published Online First: 1 Nov 1994).
Pearson G, Robinson F, Beers Gibson T, et al. Mitogen-activated protein (MAP) kinase pathways: regulation and physiological functions. Endocr Rev. 2001;22(2):153–83. https://doi.org/10.1210/edrv.22.2.0428 (published Online First: 11 April 2001).
Tran NH, Wu X, Frost JA. B-Raf and Raf-1 are regulated by distinct autoregulatory mechanisms. J Biol Chem. 2005;280(16):16244–53. https://doi.org/10.1074/jbc.M501185200 (published Online First: 16 Feb 2005).
• Yao Z, Torres NM, Tao A, et al. BRAF mutants evade ERK-dependent feedback by different mechanisms that determine their sensitivity to pharmacologic inhibition. Cancer Cell. 2015;28(3):370–83. https://doi.org/10.1016/j.ccell.2015.08.001 (published Online First: 8 Sep 2015). Identified mechanisms of resistance of BRAF mutant malignant cells to BRAF inhibitors.
Yao Z, Yaeger R, Rodrik-Outmezguine VS, et al. Tumours with class 3 BRAF mutants are sensitive to the inhibition of activated RAS. Nature. 2017;548(7666):234–8. https://doi.org/10.1038/nature23291 (published Online First: 8 Aug 2017).
Cutler RE Jr, Stephens RM, Saracino MR, et al. Autoregulation of the Raf-1 serine/threonine kinase. Proc Natl Acad Sci USA. 1998;95(16):9214–9. https://doi.org/10.1073/pnas.95.16.9214 (published Online First: 5 Aug 1998).
Jones DT, Kocialkowski S, Liu L, et al. Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res. 2008;68(21):8673–7. https://doi.org/10.1158/0008-5472.CAN-08-2097 (published Online First: 1 Nov 2008).
Wan PT, Garnett MJ, Roe SM, et al. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell. 2004;116(6):855–67. https://doi.org/10.1016/s0092-8674(04)00215-6 (published Online First: 24 March 2004).
Ikenoue T, Hikiba Y, Kanai F, et al. Functional analysis of mutations within the kinase activation segment of B-Raf in human colorectal tumors. Cancer Res. 2003;63(23):8132–7 (published Online First: 18 Dec 2003).
Schindler G, Capper D, Meyer J, et al. Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol. 2011;121(3):397–405. https://doi.org/10.1007/s00401-011-0802-6 (published Online First: 29 Jan 2011).
Behling F, Barrantes-Freer A, Skardelly M, et al. Frequency of BRAF V600E mutations in 969 central nervous system neoplasms. Diagn Pathol. 2016;11(1):55. https://doi.org/10.1186/s13000-016-0506-2 (published Online First: 29 June 2016).
Johnson A, Severson E, Gay L, et al. Comprehensive genomic profiling of 282 pediatric low- and high-grade gliomas reveals genomic drivers, tumor mutational burden, and hypermutation signatures. Oncologist. 2017;22(12):1478–90. https://doi.org/10.1634/theoncologist.2017-0242 (published Online First: 16 Sep 2017).
• Lassaletta A, Zapotocky M, Mistry M, et al. Therapeutic and prognostic implications of BRAF V600E in pediatric low-grade gliomas. J Clin Oncol. 2017;35(25):2934–41. https://doi.org/10.1200/JCO.2016.71.8726 (published Online First: 21 July 2017). Important study that identified the efficacy of BRAF inhibitors against pediatric BRAF mutant gliomas.
Zhang J, Wu G, Miller CP, et al. Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet. 2013;45(6):602–12. https://doi.org/10.1038/ng.2611 (published Online First: 16 April 2013).
Sugiura Y, Nagaishi M. Clinical relevance of BRAF status in glial and glioneuronal tumors: a systematic review. J Clin Neurosci. 2019;66:196–201. https://doi.org/10.1016/j.jocn.2019.05.014 (published Online First: 31 May 2019).
•• Brastianos PK, Taylor-Weiner A, Manley PE, et al. Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nat Genet. 2014;46(2):161–5. https://doi.org/10.1038/ng.2868 (published Online First: 15 Jan 2014). Important paper that reported high frequency of BRAF mutations in papillary craniopharyngiomas which has opened new avenues for treatment of these rare tumors.
La Corte E, Younus I, Pivari F, et al. BRAF V600E mutant papillary craniopharyngiomas: a single-institutional case series. Pituitary. 2018;21(6):571–83. https://doi.org/10.1007/s11102-018-0909-z (published Online First: 7 July 2018).
Cerami E, Gao J, Dogrusoz U, et al. The cBio Cancer Genomics Portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–4. https://doi.org/10.1158/2159-8290.CD-12-0095 (published Online First: 17 May 2012).
Gao J, Aksoy BA, Dogrusoz U, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6(269):pl1. https://doi.org/10.1126/scisignal.2004088 (published Online First: 4 April 2013).
Ascierto PA, McArthur GA, Dreno B, et al. Cobimetinib combined with vemurafenib in advanced BRAF(V600)-mutant melanoma (coBRIM): updated efficacy results from a randomised, double-blind, phase 3 trial. Lancet Oncol. 2016;17(9):1248–60. https://doi.org/10.1016/S1470-2045(16)30122-X (published Online First: 3 Aug 2016).
Planchard D, Smit EF, Groen HJM, et al. Dabrafenib plus trametinib in patients with previously untreated BRAF(V600E)-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 2017;18(10):1307–16. https://doi.org/10.1016/S1470-2045(17)30679-4 (published Online First: 19 Sep 2017).
Diamond EL, Subbiah V, Lockhart AC, et al. Vemurafenib for BRAF V600-mutant Erdheim-Chester disease and Langerhans cell histiocytosis: analysis of data from the histology-independent, phase 2, open-label VE-BASKET study. JAMA Oncol. 2018;4(3):384–8. https://doi.org/10.1001/jamaoncol.2017.5029 (published Online First: 1 Dec 2017).
Bouffet E, Kieran M, Hargrave D, et al. LGG-46: trametinib therapy in pediatric patients with low-grade gliomas (LGG) with BRAF gene fusion: a disease-specific cohort in the first pediatric testing of trametinib. Neuro-Oncology. 2018;20(Suppl 2):i114–214. https://doi.org/10.1093/neuonc/noy059.387 (published Online First: 22 June 2018).
• Kaley T, Touat M, Subbiah V, et al. BRAF inhibition in BRAF(V600)-mutant gliomas: results from the VE-BASKET study. J Clin Oncol. 2018;36(35):3477–84. https://doi.org/10.1200/JCO.2018.78.9990 (published Online First: 24 Oct 2018). Important study that identified the efficacy of BRAF inhibitors against BRAF mutantgliomas.
Wen P, Alexander S, Yung-Jue B, et al. RARE-09: efficacy and safety of dabrafenib + trametinib in patients with recurrent/refractory BRAF V600E-mutated high-grade glioma (HGG). Neuro-Oncology. 2018;20(Suppl 6):vi238–338. https://doi.org/10.1093/neuonc/noy148.986 (published Online First: 5 Nov 2018).
Garnier L, Ducray F, Verlut C, et al. Prolonged response induced by single agent vemurafenib in a BRAF V600E spinal ganglioglioma: a case report and review of the literature. Front Oncol. 2019;9:177. https://doi.org/10.3389/fonc.2019.00177 (published Online First: 16 April 2019).
Kieran MW, Bouffet E, Tabori U, et al. LBA19_PR-CNS tumours: the first study of dabrafenib in pediatric patients with BRAF V600-mutant relapsed or refractory low-grade gliomas. Ann Oncol. 2016;27:vi557. https://doi.org/10.1093/annonc/mdw435.09.
• Fangusaro J, Onar-Thomas A, Young Poussaint T, et al. Selumetinib in paediatric patients with BRAF-aberrant or neurofibromatosis type 1-associated recurrent, refractory, or progressive low-grade glioma: a multicentre, phase 2 trial. Lancet Oncol. 2019;20(7):1011–22. https://doi.org/10.1016/S1470-2045(19)30277-3 (published Online First: 4 June 2019). Demonstrates the efficacy of MEK inhibition in treating BRAF aberrant and NF1-associated low-grade gliomas.
Drobysheva A, Klesse LJ, Bowers DC, et al. Targeted MAPK pathway inhibitors in patients with disseminated pilocytic astrocytomas. J Natl Compr Cancer Netw. 2017;15(8):978–82. https://doi.org/10.6004/jnccn.2017.0139 (published Online First: 9 Aug 2017).
Long GV, Trefzer U, Davies MA, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(11):1087–95. https://doi.org/10.1016/S1470-2045(12)70431-X (published Online First: 12 Oct 2012).
Dummer R, Goldinger SM, Turtschi CP, et al. Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: final results of an open-label pilot study. Eur J Cancer. 2014;50(3):611–21. https://doi.org/10.1016/j.ejca.2013.11.002 (published Online First: 4 Dec 2013).
•• Davies MA, Saiag P, Robert C, et al. Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017;18(7):863–73. https://doi.org/10.1016/S1470-2045(17)30429-1 (published Online First: 9 June 2017). Breakthrough paper that demonstrates the effectiveness of combined BRAF and MEK inhibition in BRAF mutant melanoma brain metastases.
Yamamoto G, Sakakibara-Konishi J, Ikari T, et al. Response of BRAF(V600E)-mutant lung adenocarcinoma with brain metastasis and leptomeningeal dissemination to dabrafenib plus trametinib treatment. J Thorac Oncol. 2019;14(5):e97–9. https://doi.org/10.1016/j.jtho.2018.12.027 (published Online First: 28 April 2019).
Robinson SD, O’Shaughnessy JA, Cowey CL, et al. BRAF V600E-mutated lung adenocarcinoma with metastases to the brain responding to treatment with vemurafenib. Lung Cancer. 2014;85(2):326–30. https://doi.org/10.1016/j.lungcan.2014.05.009 (published Online First: 4 June 2014).
Holderfield M, Deuker MM, McCormick F, et al. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat Rev Cancer. 2014;14(7):455–67. https://doi.org/10.1038/nrc3760 (published Online First: 25 June 2014).
Pratt D, Camelo-Piragua S, McFadden K, et al. BRAF activating mutations involving the beta3-alphaC loop in V600E-negative anaplastic pleomorphic xanthoastrocytoma. Acta Neuropathol Commun. 2018;6(1):24. https://doi.org/10.1186/s40478-018-0525-1 (published Online First: 17 March 2018).
•• Foster SA, Whalen DM, Ozen A, et al. Activation mechanism of oncogenic deletion mutations in BRAF, EGFR, and HER2. Cancer Cell. 2016;29(4):477–93. https://doi.org/10.1016/j.ccell.2016.02.010 (published Online First: 22 March 2016). Identified the major mechanism by which alterations in BRAF activate oncogenesis.
Wang J, Yao Z, Jonsson P, et al. A secondary mutation in BRAF confers resistance to RAF inhibition in a BRAF(V600E)-mutant brain tumor. Cancer Discov. 2018;8(9):1130–41. https://doi.org/10.1158/2159-8290.CD-17-1263 (published Online First: 9 June 2018).
Tse A, Verkhivker GM. Exploring molecular mechanisms of paradoxical activation in the BRAF kinase dimers: atomistic simulations of conformational dynamics and modeling of allosteric communication networks and signaling pathways. PLoS ONE. 2016;11(11): e0166583. https://doi.org/10.1371/journal.pone.0166583 (published Online First: 20 Nov 2016).
Khater F, Langlois S, Cassart P, et al. Recurrent somatic BRAF insertion (p.V504_R506dup): a tumor marker and a potential therapeutic target in pilocytic astrocytoma. Oncogene. 2019;38(16):2994–3002. https://doi.org/10.1038/s41388-018-0623-3 (published Online First: 24 Dec 2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Appaji Rayi, Iyad Alnahhas, Shirley Ong and Vinay K. Puduvalli declare that they have no conflict of interest. Pierre Giglio owns stock in Vanguard S&P 500 ETF.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Rayi, A., Alnahhas, I., Ong, S. et al. Targeted Therapy for BRAF Mutant Brain Tumors. Curr. Treat. Options in Oncol. 22, 105 (2021). https://doi.org/10.1007/s11864-021-00901-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-021-00901-9