Abstract
Background
Small intestinal bacterial overgrowth (SIBO) is still difficult to diagnose. Quantitative culture of small intestine aspirate is recommended to be the gold standard. The methane and hydrogen breath tests are easily repeatable, sufficiently sensitive and highly specific for SIBO diagnosis. Our goal is to contrast the diagnostic value of the breath tests with jejunal aspiration cultures.
Methods
40 adult outpatients (age < 60) were enrolled in our study. Randomly, within 2 days, both the methane and the hydrogen breath test and jejunal aspiration culture were performed on each patient and the results of both tests were evaluated and contrasted.
Results
The jejunal culture was positive (105CFU / mL) in 14/40(35%) subjects, the lactulose breath test (LBT) was positive in 18/40 (45%) subjects, and the glucose breath test (GBT) was positive in 12/40 (30%). The GBT showed good agreement (κ = 0.659) and LBT showed poor agreement (κ = 0.588) with the jejunal aspirate culture. The sensitivity, specificity, positive and negative predictive values of LBT/GBT were 85.7/71.4%,76.9/92.3%, 66.6/83.3% and 90.9/85.7%, respectively.
Conclusions
35% of patients with suspected SIBO are identified using jejunal aspirate cultures. For the identification of SIBO, GBT is more specific than LBT, but has a lower sensitivity. In individuals with suspected SIBO, the breath test should be initially due to its good agreement with the jejunal aspirate culture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Small intestinal bacterial overgrowth (SIBO) describes an increase in the number or variety of bacteria in the small intestine as a result of organic or functional stasis. Although some patients with SIBO exhibit abdominal symptoms such as abdominal pain, bloating or diarrhea, others are asymptomatic [1]. Early diagnosis of SIBO is difficult due to limited diagnostic techniques or lack of specific symptoms. Abnormal structure or motility of the small intestine, decreased immune function, drugs such as proton pump inhibitors(PPIs) or aspirin may lead to SIBO [2]. Quantitative culture of small intestine aspiration, although invasive, is considered the gold standard for the diagnosis of SIBO [3]. The test is technically difficult and can only detect bacteria in the proximal small intestine. There is no strong evidence to support the current guidelines for SIBO cut-off values for bacterial colony counts [4].
Methane and hydrogen breath tests are non-invasive techniques based on the detection of metabolic products from bacteria in expired air [5], which presents several advantages: easily repeatable, sufficiently sensitive and highly specific for the diagnosis of SIBO [6, 7]. The glucose breath test (GBT) and the lactulose breath test (LBT) have been promoted for the past few years due to their convenience and safety. However, their performance in the diagnosis of SIBO is still controversial. As a result of the heterogeneity of the substrates used, the hydrogen and methane levels cut-offs, and the time interval used for measurement, the interpretation of their results is somewhat unclear [6].
The aim of this study was to assess the incidence of SIBO in patients using jejunal aspirate culture, GBT, and LBT to evaluate the diagnostic accuracy of these methods.
Methods
Study subjects
Between October 2016 and September 2019, 40 adult outpatients (age < 60) with gastrointestinal symptoms that included diarrhoea, bloating, gas, or unexplained abdominal discomfort were enroled at outpatient department of Gastroenterology, the Second Medical Center, Chinese PLA General Hospital, Beijing, China, after obtaining informed consent from them. No patient had metabolic problems or had taken PPIs, probiotics, or antibiotics within the previous four weeks. In the four weeks prior to the trial, no patient had taken any medication that could affect gastrointestinal motility or increase the risk of developing bacterial overgrowth, such as prokinetic medications or narcotics. Patients with active inflammation, cardiac, respiratory, hepatic, renal, or thyroid disease, Crohn’s disease or ulcerative colitis, hepatobiliary and pancreatic disease, or immunological disease were excluded from the study. The study protocol was approved by the IRB of Chinese PLA General Hospital (S2018-081-02).
Jejunal aspirate culture
Doctors and nurses wore sterile gloves before aspiration. The catheter (Freka-Trelumina CH 16/9,150cm) was slowly inserted from the nasal cavity under aseptic techniques, passed through the esophagus, the stomach and the duodenum, finally entered the jejunum. The guide wire was removed, and the catheter was fixed under the earlobe with the tape outside the nasal cavity, so that the pipe could be naturally bent and relaxed. X-ray photography was performed 24 h after intubation to confirm the arrival of the tube to the upper jejunum. The small intestine content was aspirated with a sterile vacuum pressure syringe and transferred to a sterile tube.
The jejunal aspirate was then diluted and injected into different culture mediums using the serial dilution method. The aerobic culture media used were Nutrient agar, MacConkey agar, 5% sheep blood agar, and Salmonella Shigella agar. The samples were placed on agar plates and kept there for 24 h at 37 °C. The anaerobic culture media employed were lactobacilli MRS agar, gut microbiota medium (GMM) and bifidobacterium medium. The jejunal aspirate was plated in anaerobic medium at 37 °C for 24–48 h. In our study, SIBO was considered to exist when there were 105 CFU/ml of bacteria in the small intestine.
Methane and hydrogen breath test
The instrument used in this study was the BreathTracker SC expiratory gas analyser made in Quintron Company (USA) with its hydrogen and methane concentration expressed as parts per million (ppm), the detection range defined as 0-500 ppm, with a sensitivity of 1 ppm and an accuracy of ± 5%.
Milk products, soybean products, roughage and fermented foods were prohibited from the day before methane and hydrogen breath test and patients were required to have a cooked rice diet plus a small volume of protein in dinner. The time from the day before the breath test to the day of the breath test was 14 h, during which the patients could drink boiled water, but not beverages in which hydrogen was produced due to bacterial decomposition. The patients were asked to defecate and brush their teeth but not to do strenuous exercise. Smoking was prohibited at 2 h before and during the breath test. The patients were asked to remain conscious and quiet and not do any strenuous exercise during methane and hydrogen LBT. Standard curves were plotted to maintain the stability of the BreathTracker SC expiratory gas analyser after adjustment. The expiratory gas in resting state was collected into a bag for the measurement of methane and hydrogen concentrations. The patients were given 75g of glucose or 10g of lactulose dissolved in 200 ml of water and asked to exhale the gas into the bag every 20 min from the time the substrates were given and repeated 9 times to measure methane and hydrogen concentrations in the expiratory gas. GBT and LBT were performed on two separate days.
Diagnosis of SIBO
After the expiratory gas was tested, curves for the time-hydrogen concentration and the time-methane concentration in the expiratory gas were plotted with the time as abscissa, the methane and hydrogen concentration as the ordinate. Following glucose ingestion, a sustained increase in breath hydrogen of 20 ppm over the basal level was regarded as SIBO evidence. SIBO was defined as an increase in hydrogen in breath of 20 ppm over basal values within 90 min after lactulose treatment. A positive methane breath test was defined as a methane level ≥ 10 ppm at any time point in the study [8].
Culture results analysis
The results were considered SIBO-positive if one or more organisms (aerobic or anaerobic) were cultured with a colony count of 105 CFU/ml. Additionally, we measured the incidence of SIBO at a cut-off value of 103 CFU/ml.
Statistics
Data were analyzed with SPSS software, version 25.0 for Windows. Categorical variables were analyzed using the χ2 test and Fisher’s exact test as applicable. Nonparametric continuous data were analysed using the Mann–Whitney test. P-values below 0.05 were considered significant. Sensitivity, specificity, positive and negative predictive values, and diagnostic precision were calculated using standard formulas. The agreement between various methods for the diagnosis of SIBO was assessed by κstatistics. Values for κ of at least 0.81 were considered to show excellent agreement, 0.61–0.80 as good, and below 0.60 as poor.
Results
Demographics
In total, 40 adult outpatients were evaluated in the study. Subjects aged 28–57 (40.3 ± 8.4) years old, with positive methane and hydrogen LBT/GBT rate of 45%/30% respectively. We contrasted patients with small bowel colony counts of ≥ 105 CFU/ml and < 105 CFU/ml in terms of symptoms and GSRS scores. There was no difference between both groups. Furthermore, there was no change in the variables between patients with bacterial colony counts greater than 103 CFU/ml and less.
Breath test
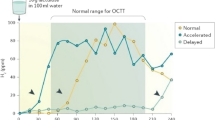
LBT and GBT were performed in all patients, with 18/40(45%) positive in LBT and 12/40(30%) positive in GBT. We contrasted the predetermined cutoff value of 105 CFU/ml by jejunal aspirate culture with the results of LBT or GBT and found that the sensitivity, specificity, positive and negative predictive values of LBT/GBT were 85.7/71.4%,76.9/92.3%, 66.6/83.3% and 90.9/85.7%, respectively. A total of 10/14 (71.4%) with and 6/26 (23.1%) without SIBO in culture had high hydrogen on LBT (sensitivity 71.4%, specificity 76.9%).A total of 8/14 (57.1%) with and 4/26 (15.4%) without SIBO on culture had high methane on LBT (sensitivity 57.1%, specificity 84.6%) (Fig. 1). GBT showed good agreement (κ = 0.659) and LBT showed poor agreement (κ = 0.588) with jejunal aspirate culture. The agreement between LBT and GBT was also good (κ = 0.687).
Aspirate culture
In the study, 22(55.0%), 4(10.0%), and 14(35.0%) patients, respectively, exhibited bacterial colony counts of ≤ 103, > 103 to 105 and ≥ 105 CFU/ml. Among patients with colony counts ≥ 105 CFU/ml,8 (57.1%) had positive aerobic cultures and 6(42.9%) had both positive aerobic and anaerobic cultures (Fig. 2). Anaerobic cultures that were positive alone did not emerge in any of the patients. The most frequently isolated microorganisms included Alpha-haemolytic streptococcus, Klebsiella species, and Neisseria spp (Table 1).
Discussion
The diagnosis of SIBO remains controversial. Since the gold standard is not available for the diagnosis of SIBO, the number of bacteria in proximal duodenal and jejunal aspiration and culture 105CFU / ml is therefore the widely accepted diagnostic technique for SIBO [9]. However, this technique is invasive, difficult to operate, time-consuming, expensive, false positive because of bacterial contamination, and is thus not widely used in clinical practice. The methane and hydrogen breath test is recommended as the best technique for the diagnosis of SIBO because it is a feasible, simple, noninvasive and radiation-free technique [10, 11].
In this study, we evaluated and contrasted the jejunal aspirate culture with the methane and hydrogen breath test in patients with gastrointestinal symptoms. While 33.3% of the patients had positive GBT and 45.0% of the patients had positive LBT, 35.0% of the patients had positive jejunal cultures. The most typical organisms identified from cultures included Alpha-haemolytic streptococcus, Klebsiella species, and Neisseria spp. 42.9% had both positive aerobic and anaerobic culture, while 57.1% only showed a positive aerobic culture. Therefore, the sensitivity and specificity of LBT/GBT were 85.7/71.4%,76.9/92.3%, respectively. What cutoff is better suitable for determining an abnormal level of bacterial growth is up for debate. We compared the results of different cutoff values in our study and found that the positive culture rate was 45% at ≥ 103 CFU/ml and 35% at ≥ 105 CFU / ml. Depending on the criteria used to identify a positive culture and the characteristics of the patients, the positive rate may change [12]. In healthy subjects, the proximal jejunum can contain up to 104 CFU/mL of bacteria [4, 13]. 0.12% of healthy individuals had bacteria counts in the proximal jejunum ranging from 0 to 103 CFU/ml [14]. There is no standardisation of aspiration and culture. Compared to our method of inserting a sterile catheter into the jejunum, some used endoscopic suction to collect duodenal juice, which can cause a high risk of contamination.
Because of variations in the dose and species of drugs employed, the cut-off for determining a positive breath test, and the features of the patients, the outcomes of the former studies have been inconsistent [15]. 0.30%/45% of the participants in our study who had no gastrointestinal symptoms tested positive for GBT/LBT. GBT was positive in 31% [16] and LBT was positive in 34.3–84% [17, 18] of patients with IBS. GBT was positive in 26.7%, LBT in 18.3% and culture (≥ 105CFU/ml) in 39.5% of patients with malabsorption in another study [7].
With a cut-off value of 106 CFU/ml, a study that cultured proximal jejunum fluid at two different locations reported that GBT had a sensitivity and specificity of 62% and 83%, respectively [19]. The specificity for a positive GBT was usually 76–85%, although there had been considerable variation in sensitivity based on different cutoff values, aspiration site, technique, and bacterial concentration. While the low sensitivity of GBT may attribute to quick absorption or lack of availability as a substrate in the distal small intestine, it was made reliable by the high specificity of the test [20]. The shortcomings of our research include a poor sample size of only 40 subjects. Our aspiration was carried out from the proximal jejunum, and it was not known whether the aspiration performed in the distal jejunum or some other site of the small intestine could have resulted in a higher positive cultures was unsure. Despite the aseptic methods we focus on, we could not completely rule out the possibility of oral bacteria.
In conclusion, compared to LBT, GBT has a lower sensitivity but a higher specificity to detect SIBO. Due to the non-invasive nature and wide availability of this tests, breath test should be considered first in patients who have symptoms of SIBO. The agreement between jejunal culture and GBT was good. Both GBT and LBT might be necessary in some patients with high suspicion of SIBO.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Bushyhead D, Quigley EMM (2022) Small intestinal bacterial overgrowth—pathophysiology and its implications for definition and management. Gastroenterology 163:593–607. https://doi.org/10.1053/j.gastro.2022.04.002
Sun X, Wang F, Liu J et al (2022) Risk factors for small-intestinal mucosal breaks beyond aspirin. J Gastroenterol Hepatol 37:1596–1602. https://doi.org/10.1111/jgh.15892
Bures J, Cyrany J, Kohoutova D et al (2010) Small intestinal bacterial overgrowth syndrome. World J Gastroenterol 16:2978–2990. https://doi.org/10.3748/wjg.v16.i24.2978
Khoshini R, Dai SC, Lezcano S et al (2008) A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci 53:1443–1454. https://doi.org/10.1007/s10620-007-0065-1
Grace E, Shaw C, Whelan K et al (2013) Review article: small intestinal bacterial overgrowth–prevalence, clinical features, current and developing diagnostic tests, and treatment. Aliment Pharmacol Ther 38:674–688. https://doi.org/10.1111/apt.12456
Gasbarrini A, Corazza GR, Gasbarrini G et al (2009) Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther 29(Suppl 1):1–49. https://doi.org/10.1111/j.1365-2036.2009.03951.x
Ghoshal UC, Ghoshal U, Das K et al (2006) Utility of hydrogen breath tests in diagnosis of small intestinal bacterial overgrowth in malabsorption syndrome and its relationship with oro-cecal transit time. Indian J Gastroenterol 25:6–10
Rezaie A, Buresi M, Lembo A et al (2017) Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American Consensus. Am J Gastroenterol 112:775–784. https://doi.org/10.1038/ajg.2017.46
Ghoshal UC, Ghoshal U, Shah A et al (2023) Evaluation of small intestinal bacterial overgrowth. Expert Rev Gastroenterol Hepatol 17:461–467. https://doi.org/10.1080/17474124.2023.2207008
Losurdo G, Leandro G, Ierardi E et al (2020) Breath tests for the non-invasive diagnosis of small intestinal bacterial overgrowth: a systematic review with meta-analysis. J Neurogastroenterol Motil 26:16–28. https://doi.org/10.5056/jnm19113
Pimentel M, Saad RJ, Long MD et al (2020) ACG clinical guideline: small intestinal bacterial overgrowth. Am J Gastroenterol 115:165–178. https://doi.org/10.14309/ajg.0000000000000501
Erdogan A, Rao SS, Gulley D et al (2015) Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil 27:481–489. https://doi.org/10.1111/nmo.12516
Bardhan PK, Gyr K, Beglinger C et al (1992) Diagnosis of bacterial overgrowth after culturing proximal small-bowel aspirate obtained during routine upper gastrointestinal endoscopy. Scand J Gastroenterol 27:253–256. https://doi.org/10.3109/00365529208999959
Posserud I, Stotzer PO, Bjornsson ES et al (2007) Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut 56:802–808. https://doi.org/10.1136/gut.2006.108712
Hammer HF, Fox MR, Keller J et al (2022) European guideline on indications, performance, and clinical impact of hydrogen and methane breath tests in adult and pediatric patients: European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Neurogastroenterology and Motility, and European Society for Paediatric Gastroenterology Hepatology and Nutrition consensus. United European Gastroenterol J 10:15–40. https://doi.org/10.1002/ueg2.12133
Lupascu A, Gabrielli M, Lauritano EC et al (2005) Hydrogen glucose breath test to detect small intestinal bacterial overgrowth: a prevalence case-control study in irritable bowel syndrome. Aliment Pharmacol Ther 22:1157–1160. https://doi.org/10.1111/j.1365-2036.2005.02690.x
Rana SV, Sharma S, Kaur J et al (2012) Comparison of lactulose and glucose breath test for diagnosis of small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Digestion 85:243–247. https://doi.org/10.1159/000336174
Pimentel M, Chow EJ, Lin HC (2003) Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 98:412–419. https://doi.org/10.1111/j.1572-0241.2003.07234.x
Corazza GR, Menozzi MG, Strocchi A et al (1990) The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology 98:302–309. https://doi.org/10.1016/0016-5085(90)90818-l
Lin HC (2004) Small intestinal bacterial overgrowth: a framework for understanding irritable bowel syndrome. JAMA 292:852–858. https://doi.org/10.1001/jama.292.7.852
Funding
This work was supported by the Foundation of Healthcare Project of Military Logistics(17BJZ46), Clinical Research Support of PLA General Hospital(2017FC-TSYS-2020) and Tianjin Health Research Project(TJWJ2023MS069).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of Chinese PLA General Hospital (S2018-081-02) and with the 1964 Helsinki declaration and its subsequent amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, S., Li, J., Ma, J. et al. Comparison of jejunal aspirate culture and methane and hydrogen breath test in the diagnosis of small intestinal bacterial overgrowth. Ir J Med Sci 193, 699–703 (2024). https://doi.org/10.1007/s11845-023-03527-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03527-y