Abstract
The increased availability of noninvasive breath tests, each with limitations, has led to widespread testing for small intestinal bacterial overgrowth (SIBO) in patients with non-specific gastrointestinal complaints. The lactulose breath test (LBT) is based upon an incorrect premise and therefore incorrect interpretations which has resulted in the over-diagnosis of SIBO and the excessive use of antibiotics in clinical practice. Despite limitations, the glucose breath test (GBT) should be exclusively employed when considering SIBO in appropriately chosen patients. This review suggests guidelines for the optimal use and appropriate interpretation of the GBT for suspected SIBO. The LBT should be discarded from future use, and the literature based upon the LBT should be discounted accordingly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The syndrome associated with small intestinal bacterial overgrowth (SIBO) was first characterized over a century ago [1], and by the mid-twentieth century, the ability to treat this syndrome with antibiotics was well recognized [2]. This syndrome was recognized as being a complication arising from a variety of different gastrointestinal disorders and postoperative states. It was understood to be a chronic condition causing considerable morbidity and requiring ongoing treatment if the underlying disease process could not be reversed. Since these initial descriptions, the definition of SIBO has become the subject of much controversy, including what defines the condition, which tests should be used to establish the diagnosis, and what are the appropriate treatment options. Initially considered a relatively rare entity with serious metabolic consequences, the number of patients receiving this diagnosis as an explanation for what were previously thought to be functional disorders has grown exponentially in the past few decades.
There appear to be several factors driving this growth in the diagnosis of SIBO. The first has been the increased availability of noninvasive and relatively inexpensive breath tests, which has lowered the threshold to test for this condition. Second, such testing has increasingly been employed to evaluate patients who have gastrointestinal symptoms without evidence of having the metabolic derangements and/or underlying conditions associated with the classic presentation of SIBO syndrome. Third, a failure to recognize the performance characteristics and limitations of available breath testing technology has resulted in patients with functional disorders erroneously being diagnosed as having SIBO. Finally, the symptomatic response to antibiotic therapy of a minority of patients with irritable bowel syndrome (IBS) has been conflated with the results of erroneous breath test interpretation to incorrectly infer that the etiology for their symptoms is SIBO. In clinical practice, these factors have led to widespread use of breath testing in patients exhibiting different, non-specific symptoms such as bloating, diarrhea, abdominal cramps, and flatus (often despite not fulfilling Rome III criteria for IBS). This in turn has led to the increased use of antibiotics in patients with a falsely positive breath test result.
The focus of this review is not to discuss the prevalence of SIBO in patients with IBS nor is it to assess the rapidly evolving concept of intestinal dysbiosis and its possible mechanistic role in functional gastrointestinal disorders. Rather, it will focus on the utility of breath tests in clinical practice to identify or exclude patients as having SIBO syndrome. While there is common acknowledgement that the performance characteristics of these tests are not optimal, they continue to be used by healthcare providers to make important clinical decisions in many patients with gastrointestinal symptoms. We will ultimately make suggestions about when such breath testing should (and should not) be requested, the appropriate test to perform, and how best to interpret test results in a clinical setting.
Definitions of SIBO Syndrome and SIBO
In its historically recognized form, SIBO syndrome consists of a clinical condition in which there is an abnormal proliferation of bacteria within the lumen of the small intestine, such that their metabolism of the luminal contents alters the normal processes of digestion and absorption to a clinically significant degree. The classic abnormality has been vitamin B12 deficiency with associated megaloblastic anemia, but other consequences have included fat malabsorption, protein loss, various nutritional deficiencies, and intestinal pneumatosis. Common gastrointestinal manifestations have included the expected symptoms of malabsorption and excess bacterial fermentation, such as diarrhea, bloating, excessive flatus, and weight loss, while specific nutrient deficiencies could result in other manifestations, such as peripheral edema and polyneuropathy.
A distinction needs to be made between the historically recognized syndrome associated with SIBO and the presence of SIBO itself, which may or may not have the metabolic consequences of the syndrome. In its simplest form, SIBO has been defined as the presence of excessive numbers of coliform bacteria in the small intestine. The most commonly accepted gold standard test for assessing the presence of SIBO has been by aspiration of fluid from the small bowel lumen, which then undergoes quantitative culture under both aerobic and anaerobic conditions [3]. The traditional cutoff value has been > 105 colony forming units per milliliter (cfu/ml) from the duodenum or jejunum, with the emphasis on coliform organisms similar to those found in the colon. A lower diagnostic level of ≥ 103 cfu has been advocated by some [4], based on the fact that asymptomatic healthy subjects infrequently have values above this [5]. However, the clinical issue is not to distinguish symptomatic patients from healthy subjects, but to distinguish, from among symptomatic patients, those whose symptoms are manifestations of the condition in question. In this regard, the lower cutoff value, for instance, distinguishes IBS patients from healthy subjects but not from disease controls [6].
Therefore, a critical question is what concentration and what type of bacteria are necessary to produce the metabolic consequences and symptoms associated with SIBO syndrome. In early studies of patients with conditions associated with SIBO such as stagnant loop syndromes or different types of partial gastrectomy, malabsorption of vitamin B12, bile acids, and fat were strongly associated with the presence of coliform organisms. Most such patients had much higher bacteria concentrations, in the range of 107–109 cfu/ml [7]. When lower bacteria concentrations are used to define SIBO, fewer patients are found to have an underlying condition historically associated with SIBO. Furthermore, with lower cutoff concentrations for determining SIBO, symptoms do not correlate strongly with the presence of SIBO [8], and patients are not observed to have additional clinical benefit from antibiotic therapy [9]. An additional concern comes from recent findings suggesting that bacterial concentrations ≥ 105 can be observed in the proximal small bowel of healthy subjects consuming a high fiber diet [8]. This observation raises additional questions regarding how to interpret quantitative cultures without accounting for the subject’s diet.
Pathogenesis and Etiologies of SIBO Syndrome
Although there are many potential factors that act to suppress the growth of bacteria and other organisms in the small intestine, the most important factor is the ability of the small intestine to clear intraluminal contents via propulsion, particularly in the fasting state via phase 3 of the migrating motor complex (MMC). Practically speaking, the two most common conditions to suspect SIBO involve disorders of intestinal motility and anatomical alterations which promote stasis in blind loops or conditions that are associated with intestinal obstruction. Examples of the former include systemic sclerosis (scleroderma), diabetic autonomic neuropathy, chronic opiate use, and intestinal pseudo-obstruction. Examples of the latter include blind intestinal loops, gastrocolic and jejunocolic fistula, small bowel strictures from Crohn’s disease, radiation or surgical procedures, small intestinal diverticulosis, and surgically constructed anatomical alterations such as Billroth 2 gastrectomy and end-to-side intestinal anastomosis. Other potential mechanisms and associated etiologies for SIBO syndrome include reduced bacterial killing (profound achlorhydria and immune deficiencies) as well as increased nutrient availability from underlying maldigestion/malabsorption (chronic pancreatitis). Not all patients with these conditions will have SIBO or SIBO syndrome. However, those patients exhibiting symptoms or typical metabolic derangements would be expected to have a higher pretest probability of having SIBO syndrome.
The Breath Testing Process and Sources of Measurable GAS Production
The premise behind breath testing is that human metabolism does not generate hydrogen or methane. Thus, the detection of these freely diffusible gases in expired air indicates the presence of active microbial metabolism of carbohydrates. Recent work employing novel gas-sensing capsules has demonstrated that ongoing fermentation of dietary constituents can be detected within the lumen of both the small and large intestine of healthy subjects [10]. However, most of the gas production by far arises within the colonic lumen. This is not surprising, as the microbial concentrations within the colon are orders of magnitude greater than those within the small intestine. Even in a patient with very high concentrations of bacteria within the small intestine, greater degrees of intraluminal hydrogen production occur when carbohydrate is instilled in the colonic lumen than in the small bowel lumen [11]. Detectable colon fermentation could result from passage of the test substrate into the colon before breath samples are collected or from previously ingested components of the normal diet that had failed to clear the colon by the time the breath test begins.
Methanogens (Methanobrevibacter smithii) are not bacteria but belong to the domain Archaea. Using new PCR-based detection methods, they have been found to be nearly ubiquitous in healthy subjects [12]. These predominantly reside in the colon, where they account for about 10% of all anaerobic organisms, but could also be present in the small intestine in conditions predisposing to SIBO. As the production of methane requires metabolism of hydrogen, this might result in lower or even absent levels of hydrogen being recorded during breath testing. This would be a concern for breath tests only examining hydrogen production [13]. Because of this consideration, measurement of both hydrogen and methane concentrations during carbohydrate breath testing has become the standard in the field.
Lactulose-Based Breath Testing
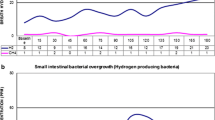
The lactulose hydrogen and methane breath test (LBT) is a noninvasive semi-qualitative test that was initially developed to measure orocecal transit time, taken as the time when an increase in hydrogen (or methane) in exhaled air above baseline was noted. This occurs when the non-absorbable saccharide reaches the cecum, where it is rapidly metabolized by coliform (hydrogen) or methanogenic (methane) organisms (Fig. 1) [14]. Lactulose can accelerate orocecal transit [15], so that normative values are not identical to other transit studies performed without lactulose. Early elevations of either gas over baseline can occur in two major circumstances: (1) patients with rapid orocecal transit and (2) those with SIBO. The critical issue with this test is the definition of “early” elevation.
Lactulose H2 breath test for measurement of orocecal transit time. Representative lactulose H2 breath tests (LHBTs) are shown for accelerated (30 min), normal (75 min), and delayed (225 min) orocecal transit times (OCTTS). The test requires H2 measurements at regular intervals after ingestion of lactulose. H2 values of>10 ppm over basal values followed by at least two subsequent increments (arrows) indicate cecal delivery of the nonabsorbable substrate bacterial metabolism. This increase in H2 exhalation normally occurs 50-200 min after ingestion of the marker substance (normal range for OCTT marked in grey). From Ref. [14] with permission
It has been proposed that when a significant elevation of breath hydrogen or methane values occurs within 90 min of lactulose ingestion, this should be interpreted as being positive for the presence of SIBO [16]. When the patient has an underlying condition that can promote small intestinal stasis, as previously cited, such a rise of hydrogen and/or methane has a higher likelihood of resulting from SIBO. In the absence of such conditions, the pretest probability of SIBO syndrome is lower, and a “positive” test result has a higher likelihood of being falsely positive due to accelerated orocecal transit. This is particularly likely to occur in patients presenting with common and non-specific symptoms, such as bloating, gas, abdominal cramping, and altered bowel habits, in whom prior evaluation has uncovered no evidence of a condition that would predispose to SIBO syndrome. In such patients, a “positive test” cannot be interpreted properly without a concomitant test of orocecal transit. This point was convincingly demonstrated by Yu and associates, who found in patients with IBS that, in those with an abnormal rise in breath hydrogen during an LBT, this occurred after the bolus had reached the cecum in 88% [17]. Notably, the mean orocecal transit time in this group was 71 min, confirming the error of assuming that hydrogen or methane production observed before 90 min emanates from the small intestine. In an editorial review of the utility of breath tests to diagnose SIBO, Sellin concluded that “These findings demonstrate convincingly the futility of diagnosing SIBO with the lactulose breath test on the basis of presumed intestinal transit times [18].” This conclusion has also been echoed by others [19].
Yet, despite these and similar critiques [20,21,22], the LBT continues to be widely employed in clinical practice. In a recent meta-analysis of SIBO and IBS [6], the LBT was used in 44% of all cited studies reported from the USA. Studies using the LBT reported a higher prevalence SIBO in IBS than studies using the glucose breath test (62 vs. 21%), but with more heterogeneity in the findings. Moreover, the prevalence of a positive LBT test was approximately 35% in control subjects! As the use of the LBT has expanded to more patients with non-specific symptoms, and with no objective evidence of intestinal stasis, the likelihood is that most positive test results are false positives. The utility of the LBT to assess individual patients for suspected SIBO in clinical practice cannot be defended unless accompanied by a concurrent scintigraphic transit study; this is unacceptable as a standard practice in terms of cost, exposure of patients to radioactivity, and lack of testing resources in many clinical settings.
Glucose-Based Breath Testing
The concept behind glucose-based breath testing (GBT) is that ingested glucose normally leaves the stomach at a relatively slow and linear rate of 1–4 kcal/min [23]. This theoretically should result in complete absorption of glucose by the small intestine before the solution can reach the cecum and be fermented by colonic bacteria. Thus, when a rise in breath hydrogen or methane occurs following ingestion of glucose, the assumption has been that this results from the metabolism by abnormal concentrations of bacteria in the small intestine, effectively competing with the human intestine for intake and metabolism of this energy source. Such a competition was congruent with clinical features of the classically described SIBO syndrome, where patients suffered weight loss, malnutrition, and reduction in absorption of nutrients such as vitamin B12.
The dose of glucose used for the test has generally ranged from 50 to 80 g [24], with one study suggesting fewer false negative tests with a higher dosage [25]. Most commercially available breath test kits contain 75 g (300 kcal) of glucose. The rise in hydrogen concentration above baseline that is used to determine a positive test has ranged from 10 to 20 ppm, with different guidelines recommending values ranging from 12 to 20 ppm [4, 24]. Higher cutoff values will increase the specificity while reducing the sensitivity [26, 27]. Far more important for the diagnostic accuracy of GBT are the sources for false negative and false positive results, as discussed below.
Mechanisms for a False Negative Glucose Hydrogen Breath Test
Substandard operating performance of the breath testing system and failure to follow appropriate test protocols are obvious reasons for a false negative test. Calibration protocols for the test system need to be followed carefully. Hyperventilation, such as with vigorous exercise, can reduce concentrations of expelled gas in the breath samples [28, 29]. Antibiotics and bowel purges may have a similar effect, although this has been more clearly demonstrated with colonic than small bowel flora [30]. Some patients may not be able to provide an adequate breath sample. Specimens that have been collected remotely for later analysis may have experienced leakage. Breath testing systems that have the capability to measure carbon dioxide in the sample can detect substandard specimens. These considerations apply to the LBT as well.
Another possible mechanism for a false negative breath test is the delayed delivery or bypass of the glucose solution to the location in the small bowel where clinically relevant bacterial overgrowth is located. This could occur potentially in such conditions as achalasia, partial gastric outlet obstruction, and proximal enterocutaneous fistula. Negative breath tests in the presence of such conditions should probably be discounted. This also applies to the LBT.
There is also concern that glucose could be absorbed in the small intestine before reaching a region of luminal bacterial overgrowth confined to more distal location. While theoretically plausible, there are no studies employing quantitative cultures from the distal ileum to confirm whether, or how often, this is a clinical concern in patients with SIBO syndrome.
As mentioned previously, there is concern that hydrogen metabolism by methanogens in the gut could cause a false negative breath test if only hydrogen is measured. Studies reporting this phenomenon have only examined reduced hydrogen levels during colonic fermentation of non-absorbed carbohydrates, such as lactulose or lactose, rather than effects on hydrogen production or measurement within the small intestine [31, 32]. Even in the clinical scenario of colonic fermentation of malabsorbed carbohydrates, the presence of methanogenic fermentation does not necessarily impair breath test interpretation [33], and very few individuals with methanogens have been shown to have completely and consistently absent hydrogen production if given sufficient fermentable substrate [32, 34, 35]. There are no studies that have convincingly demonstrated a high prevalence of false negative GBT as a result of methane production in the small bowel (i.e., when a colonic source of methane production has been excluded).
Mechanisms for a False Positive Glucose Hydrogen Breath Test
Several recommended guidelines for breath testing protocols, if not adhered to, can result in false positive GBT. Smoking during the test can raise measured hydrogen values substantially [29, 36] as can oral flora when interacting with glucose [29, 37, 38]. Ingestion of a variety of foods and drinks containing fermentable substrates can result in elevated breath hydrogen levels several hours later [39, 40]. Failure to follow an appropriate pre-procedure diet and fasting before the procedure results in elevated basal and peak hydrogen values, due to fermentation of previously ingested substrates, rather than the glucose ingested for the test [35, 41, 42]; an early rise in hydrogen is likely related to passage of retained ileal contents into the colon, for fermentation at that location [41]. Again, these factors also apply to the LBT.
A major source for false positive hydrogen GBT is the incomplete absorption of the test substrate within the small bowel, resulting in delivery of glucose to and subsequent fermentation in the colon. This was identified during the development of breath testing, in which patients with partial gastrectomy exhibited hydrogen production when more than 25 g of glucose was ingested [43]. A subsequent case series identified a cohort of patients without surgical alterations of the gut who also had abnormal glucose breath tests as a result of a rapid orocecal transit time delivering unabsorbed glucose to the cecum [44].
In a larger series of 139 patients undergoing concurrent GBT with scintigraphy, 48% had a false positive breath test resulting from rapid delivery of glucose to the colon [27]. The frequency of this finding depended upon whether the patients had a history of prior upper GI tract surgery. Among patients with such surgery, 69% had an abnormal breath test result, but in 65% of these, this was a false positive result due to a rapid orocecal transit time (mean 16 min). This finding also calls into question studies showing high rates of bacterial overgrowth in patients following foregut surgery, based on results of breath tests performed without scintigraphy [45,46,47,48]. Even in patients without such a surgical history, 13% had a false positive breath test due to colonic fermentation from rapid orocecal transit (mean 38 min) [27]. Patients with negative GBT or presumptive true positive tests for bacterial overgrowth had similar orocecal transit times (mean 86 and 79 min, respectively), which were significantly longer than those with a false positive test. These findings demonstrate convincingly that a positive GBT cannot be interpreted without knowing the orocecal transit time.
Constipation has recently been demonstrated to be a potential source of a false positive hydrogen GBT [49]. This appears to be the result of release of pre-formed hydrogen within retained stool, as a response of mixing of intestinal content. Half of severely constipated patients generated a positive breath test simply with the ingestion of a non-fermentable PEG-electrolyte solution. These abnormal findings resolved after correction of constipation.
Diagnostic Utility of Basal Breath Hydrogen Values
Because patients with profound intestinal stasis can have ongoing retention and thus fermentation of carbohydrates, the presence of a high fasting hydrogen level alone is considered to be diagnostic of SIBO by some. A major difficulty with such a conclusion is that baseline breath hydrogen values are greatly influenced by the diet leading up to the breath test [50]. If the pretest protocol does not require a diet low in fermentable substrates, or such a diet is not followed, high baseline hydrogen values likely represent fermentation of these dietary constituents in the colon rather than SIBO. In a patient with slow transit constipation, several days of a low fermentation diet may be required to reduce fasting levels of breath hydrogen to normal. High baseline values also occur in untreated celiac disease [51, 52]. In our experience, patients with SIBO syndrome associated with luminal stasis and high fasting hydrogen levels show dramatic elevations in hydrogen values above this baseline following glucose administration. Unless the patient is known to have significant problems with stasis, breath tests with baseline elevations of hydrogen only should be considered technically unsatisfactory and uninterpretable [21].
Diagnostic Utility of Methane Levels
Healthy subjects frequently harbor methanogenic organisms as components of their microbiome, although the presence of such organisms can vary over time [53]. The vast proportion of methane production from these organisms observed on breath testing arises in the colon. Baseline methane values are highly variable among healthy subjects and can rise in response to ingestion of non-fermentable oral intake [32]. Furthermore, methane concentrations vary considerably, both during single breath testing session and on repeat testing [54, 55]. In our experience, the vast majority of patients with a positive glucose breath test for methane are also positive for hydrogen, and concurrent measures of orocecal transit time remain necessary to avoid false positive results when only methane levels are elevated [27].
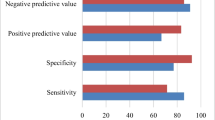
Small Bowel Quantitative Cultures Versus Glucose Breath Testing
The performance of glucose breath testing has usually been compared to the findings of quantitative cultures obtained from small bowel aspirates, which are taken to be the gold standard for diagnosing SIBO. In such analyses, glucose breath testing has generally been found to have suboptimal sensitivity and specificity [3]. There are difficulties with regarding quantitative cultures as the gold standard, aside from concerns of quality control in processing the specimens. The region of small bowel from which specimens are obtained may not represent bacteria counts in the region where bacterial overgrowth is actually present (false negative test). When the concept of SIBO syndrome is tested in patients with known conditions predisposing to such overgrowth, most patients so diagnosed had much higher concentrations, in the range of 107-109 CFU/ml. Indeed, when higher counts are used as the gold standard, the glucose breath test has a higher sensitivity [26].
Conclusions
-
1.
We believe that most of the literature on SIBO performed with lactulose-based testing is fundamentally flawed, as it is based on an incorrect premise and therefore incorrect conclusions. This has resulted in the over-diagnosis of SIBO and the excessive use of antibiotics in clinical practice.
-
2.
The LBT should not be performed to test patients for suspected SIBO syndrome in the absence of a concomitant measurement of orocecal transit. Since this approach is impractical for previously stated reasons, the LBT should be discarded.
-
3.
Despite its limitations, GBT should be the preferred noninvasive test at the present time for the evaluation of patients with suspected SIBO. However, when the test is positive, strong consideration should be given for repeating the test with a concomitant scintigraphic transit study. This is necessary to determine whether elevations of hydrogen and/or methane occur prior to the arrival of the glucose bolus to the terminal ileum or cecum. This is particularly so if there is a history of previous upper gastrointestinal surgery, due to the high prevalence of rapid orocecal transit times. This step is likely unnecessary if the patient has a condition where a delayed orocecal transit time is expected, such as with systemic sclerosis.
-
4.
We believe that changes in methane levels alone during GBT should not be used to diagnose SIBO syndrome. This is because most methane production occurs in the colon, baseline production is highly variable, and in constipated patients, methane production can reflect metabolism of colonic contents ingested several days before testing. These factors result in an unacceptably high rate of false positive test results when the test is positive only for methane.
-
5.
We believe that GBT should be performed predominantly in patients with known conditions predisposing to SIBO syndrome (high pretest probability), given the suboptimal performance characteristics of the test, and the costs and risks associated with treating false positive test results.
-
6.
Stricter attention needs to be paid to the pre-procedure diet than has often been the case in clinical practice, with stricter adherence to a diet low in fermentable substrates in the 24 h preceding the test. We believe that patients should bring in a written account of their dietary intake for the 24 h preceding the test. Patients with severe constipation should have this corrected before performing a GBT.
-
7.
We suggest following approach, outlined in Table 1, when healthcare providers consider GBT to evaluate patients for SIBO syndrome.
Table 1 Requesting and interpreting breath tests for suspected SIBO syndrome
References
Barker WH, Hummel LE. Macrocytic anemia in association with intestinal strictures and anastomoses. Bull Johns Hopkins Hosp. 1939;46:215–254.
Ellis H, Smith AD. The blind-loop syndrome. Monogr Surg Sci. 1967;4:193–215.
Corazza GR, Menozzi MG, Strocchi A, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology. 1990;98:302–309. https://doi.org/10.1016/0016-5085(90)90818-l.
Pimentel M, Saad RJ, Long MD, Rao SSC. ACG clinical guideline: small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115:165–178. https://doi.org/10.14309/ajg.0000000000000501.
Posserud I, Stotzer PO, Bjornsson ES, Abrahamsson H, Simren M. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut. 2007;56:802–808. https://doi.org/10.1136/gut.2006.108712.
Shah A, Talley NJ, Jones M, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis of case-control studies. Am J Gastroenterol. 2020;115:190–201. https://doi.org/10.14309/ajg.0000000000000504.
Tabaqchali S, Okubadejo OA, Neale G, Booth CC. Influence of abnormal bacterial flora on small intestinal function. Proc R Soc Med. 1966;59:1244–1246.
Saffouri GB, Shields-Cutler RR, Chen J, et al. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019;10:2012. https://doi.org/10.1038/s41467-019-09964-7.
Franco DL, Disbrow MB, Kahn A, et al. Duodenal Aspirates for small intestine bacterial overgrowth: yield, PPIs, and outcomes after treatment at a tertiary academic medical center. Gastroenterol Res Pract. 2015;2015:971582. https://doi.org/10.1155/2015/971582.
Berean KJ, Ha N, Ou JZ, et al. The safety and sensitivity of a telemetric capsule to monitor gastrointestinal hydrogen production in vivo in healthy subjects: a pilot trial comparison to concurrent breath analysis. Aliment Pharmacol Ther. 2018;48:646–654. https://doi.org/10.1111/apt.14923.
Levitt MD. Production and excretion of hydrogen gas in man. N Engl J Med. 1969;281:122–127. https://doi.org/10.1056/nejm196907172810303.
Dridi B, Henry M, El Khéchine A, Raoult D, Drancourt M. High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol. PLoS ONE. 2009;4:e7063. https://doi.org/10.1371/journal.pone.0007063.
Bjorneklett A, Jenssen E. Relationships between hydrogen (H2) and methane (CH4) production in man. Scand J Gastroenterol. 1982;17:985–992.
Keller J, Bassotti G, Clarke J, et al. Expert consensus document: advances in the diagnosis and classification of gastric and intestinal motility disorders. Nat Rev Gastroenterol Hepatol. 2018;15:291–308. https://doi.org/10.1038/nrgastro.2018.7.
Miller MA, Parkman HP, Urbain JL, et al. Comparison of scintigraphy and lactulose breath hydrogen test for assessment of orocecal transit: lactulose accelerates small bowel transit. Dig Dis Sci. 1997;42:10–18. https://doi.org/10.1023/a:1018864400566.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American Consensus. Am J Gastroenterol. 2017;112:775–784. https://doi.org/10.1038/ajg.2017.46.
Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut. 2011;60:334–340.
Sellin JH. A breath of fresh air. Clin Gastroenterol Hepatol. 2016;14:209–211. https://doi.org/10.1016/j.cgh.2015.10.027.
Paterson W, Camilleri M, Simren M, Boeckxstaens G, Vanner SJ. Breath testing consensus guidelines for SIBO: RES IPSA LOCQUITOR. Am J Gastroenterol. 2017;112:1888–1889. https://doi.org/10.1038/ajg.2017.233.
Riordan SM, McIver CJ, Walker BM, Duncombe VM, Bolin TD, Thomas MC. The lactulose breath hydrogen test and small intestinal bacterial overgrowth. Am J Gastroenterol. 1996;91:1795–1803.
Simrén M, Stotzer PO. Use and abuse of hydrogen breath tests. Gut. 2006;55:297–303. https://doi.org/10.1136/gut.2005.075127.
Yao CK, Tuck CJ, Barrett JS, Canale KE, Philpott HL, Gibson PR. Poor reproducibility of breath hydrogen testing: Implications for its application in functional bowel disorders. Unit Eur Gastroenterol J. 2017;5:284–292. https://doi.org/10.1177/2050640616657978.
Brener W, Hendrix TR, McHugh PR. Regulation of the gastric emptying of glucose. Gastroenterology. 1983;85:76–82.
Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther. 2009;29:1–49. https://doi.org/10.1111/j.1365-2036.2009.03951.x.
King CE, Toskes PP. Comparison of the 1-gram [14C]xylose, 10-gram lactulose-H2, and 80-gram glucose-H2 breath tests in patients with small intestine bacterial overgrowth. Gastroenterology. 1986;91:1447–1451. https://doi.org/10.1016/0016-5085(86)90199-x.
Erdogan A, Rao SS, Gulley D, Jacobs C, Lee YY, Badger C. Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil. 2015;27:481–489. https://doi.org/10.1111/nmo.12516.
Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol. 2016;14:203–208. https://doi.org/10.1016/j.cgh.2015.07.032.
Perman JA, Modler S, Engel RR, Heldt G. Effect of ventilation on breath hydrogen measurements. J Lab Clin Med. 1985;105:436–439.
Thompson DG, Binfield P, De Belder A, O’Brien J, Warren S, Wilson M. Extra intestinal influences on exhaled breath hydrogen measurements during the investigation of gastrointestinal disease. Gut. 1985;26:1349–1352. https://doi.org/10.1136/gut.26.12.1349.
Gilat T, Ben Hur H, Gelman-Malachi E, Terdiman R, Peled Y. Alterations of the colonic flora and their effect on the hydrogen breath test. Gut. 1978;19:602–605. https://doi.org/10.1136/gut.19.7.602.
Corazza G, Strocchi A, Sorge M, Bentai G, Gasbarrini G. Prevalence and consistency of low breath H2 excretion following lactulose ingestion. Possible implications for the clinical use of the H2 breath test. Dig Dis Sci.. 1993;38:2010–2016. https://doi.org/10.1007/bf01297077.
Corazza GR, Benati G, Strocchi A, Malservisi S, Gasbarrini G. The possible role of breath methane measurement in detecting carbohydrate malabsorption. J Lab Clin Med. 1994;124:695–700.
Montes RG, Saavedra JM, Perman JA. Relationship between methane production and breath hydrogen excretion in lactose-malabsorbing individuals. Dig Dis Sci. 1993;38:445–448. https://doi.org/10.1007/bf01316497.
Rana SV, Sinha SK, Sharma S, Kaur H, Bhasin DK, Singh K. Effect of predominant methanogenic flora on outcome of lactose hydrogen breath test in controls and irritable bowel syndrome patients of north India. Dig Dis Sci. 2009;54:1550–1554. https://doi.org/10.1007/s10620-008-0532-3.
Strocchi A, Corazza G, Ellis CJ, Gasbarrini G, Levitt MD. Detection of malabsorption of low doses of carbohydrate: accuracy of various breath H2 criteria. Gastroenterology. 1993;105:1404–1410. https://doi.org/10.1016/0016-5085(93)90145-3.
Tadesse K, Eastwood M. Breath-hydrogen test and smoking. Lancet. 1977;2:91. https://doi.org/10.1016/s0140-6736(77)90098-8.
Thompson DG, O’Brien JD, Hardie JM. Influence of the oropharyngeal microflora on the measurement of exhaled breath hydrogen. Gastroenterology. 1986;91:853–860. https://doi.org/10.1016/0016-5085(86)90686-4.
Mastropaolo G, Rees WD. Evaluation of the hydrogen breath test in man: definition and elimination of the early hydrogen peak. Gut. 1987;28:721–725. https://doi.org/10.1136/gut.28.6.721.
Anderson IH, Levine AS, Levitt MD. Incomplete absorption of the carbohydrate in all-purpose wheat flour. N Engl J Med. 1981;304:891–892. https://doi.org/10.1056/nejm198104093041507.
Erickson J, Wang Q, Slavin J. White grape juice elicits a lower breath hydrogen response compared with apple juice in healthy human subjects: a randomized controlled trial. J Acad Nutr Dietet. 2017;117:908–913. https://doi.org/10.1016/j.jand.2017.01.020.
Read NW, Al-Janabi MN, Bates TE, et al. Interpretation of the breath hydrogen profile obtained after ingesting a solid meal containing unabsorbable carbohydrate. Gut. 1985;26:834–842. https://doi.org/10.1136/gut.26.8.834.
Avallone EV, De Carolis A, Loizos P, Corrado C, Vernia P. Hydrogen breath test–diet and basal H2 excretion: a technical note. Digestion. 2010;82:39–41. https://doi.org/10.1159/000277630.
Bond JH, Jr., Levitt MD. Use of pulmonary hydrogen (H 2) measurements to quantitate carbohydrate absorption. Study of partially gastrectomized patients. J Clin Investig. 1972;51:1219-25. https://doi.org/10.1172/jci106916.
Sellin JH, Hart R. Glucose malabsorption associated with rapid intestinal transit. Am J Gastroenterol. 1992;87:584–589.
Iivonen MK, Ahola TO, Matikainen MJ. Bacterial overgrowth, intestinal transit, and nutrition after total gastrectomy. Comparison of a jejunal pouch with Roux-en-Y reconstruction in a prospective random study. Scand J Gastroenterol. 1998;33:63–70. https://doi.org/10.1080/00365529850166220.
Paik CN, Choi MG, Lim CH, et al. The role of small intestinal bacterial overgrowth in postgastrectomy patients. Neurogastroenterol Motility. 2011;23:e191–e196. https://doi.org/10.1111/j.1365-2982.2011.01686.x.
Perez Aisa A, Garcia Gavilan MC, Alcaide Garcia J, et al. Small intestinal bacterial overgrowth is common after gastrectomy but with little impact on nutritional status. Gastroenterol Hepatol. 2019;42:1–10. https://doi.org/10.1016/j.gastrohep.2018.07.001.
Mouillot T, Rhyman N, Gauthier C, et al. Study of small intestinal bacterial overgrowth in a cohort of patients with abdominal symptoms who underwent bariatric surgery. Obes Surg. 2020;30:2331–2337. https://doi.org/10.1007/s11695-020-04477-5.
Di Stefano M, Mengoli C, Bergonzi M, Miceli E, Pagani E, Corazza GR. Hydrogen breath test in patients with severe constipation: the interference of the mixing of intestinal content. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society.. 2014;26:1754–1760. https://doi.org/10.1111/nmo.12456.
Brummer RJ, Armbrecht U, Bosaeus I, Dotevall G, Stockbruegger RW. The hydrogen (H2) breath test. Sampling methods and the influence of dietary fibre on fasting level. Scand J Gastroenterol.. 1985;20(8):1007–1013. https://doi.org/10.3109/00365528509088863.
Di Stefano M, Miceli E, Missanelli A, Malservisi S, Strocchi A, Corazza GR. Fermentation of endogenous substrates is responsible for increased fasting breath hydrogen levels in celiac disease. J Lab Clin Med. 2004;143:163–168. https://doi.org/10.1016/j.lab.2003.11.006.
Rana SV, Sharma S, Sinha SK, Kaur J, Prasad KK, Singh K. Influence of previously ingested wheat on fasting breath hydrogen in celiac patients. Dig Dis Sci. 2009;54:1276–1279. https://doi.org/10.1007/s10620-008-0496-3.
Strocchi A, Ellis CJ, Furne JK, Levitt MD. Study of constancy of hydrogen-consuming flora of human colon. Dig Dis Sci. 1994;39:494–497. https://doi.org/10.1007/bf02088333.
Jonderko K, Gabriel-Jasniok A, Szymszal M, Kasicka-Jonderko A, Blonska-Fajfrowska B. Unreliability of breath methane as a candidate indicator of functional bowel disorders. Gut Liver. 2008;2:180–185. https://doi.org/10.5009/gnl.2008.2.3.180.
Harvie RM, Tuck CJ, Schultz M. Evaluation of lactulose, lactose, and fructose breath testing in clinical practice: a focus on methane. JGH Open. 2020;4:198–205. https://doi.org/10.1002/jgh3.12240.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Massey, B.T., Wald, A. Small Intestinal Bacterial Overgrowth Syndrome: A Guide for the Appropriate Use of Breath Testing. Dig Dis Sci 66, 338–347 (2021). https://doi.org/10.1007/s10620-020-06623-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06623-6