Abstract
Background
High-mobility group box 2 (HMGB2) is considered as oncogene in non-small cell lung cancer (NSCLC), while its clinical implication is still unknown. This study aimed to explore the correlation of HMGB2 with clinicopathological characteristics and prognosis in NSCLC patients.
Methods
A total of 133 NSCLC patients who received radical excision were enrolled. HMGB2 expression in the tumor specimens and paired adjacent tissue specimens was determined by immunohistochemical assay (for protein expression) and reverse transcription quantitative polymerase chain reaction assay (for gene expression), respectively.
Results
HMGB2 protein expression was higher in tumor tissue compared with adjacent tissue, and it could distinguish tumor tissue from adjacent tissue (area under the curve (AUC): 0.775, 95%confidence interval (95%CI): 0.720–0.830). Meanwhile, tumor HMGB2 protein high expression correlated with lymph node (LYN) metastasis and advanced TNM stage. Additionally, tumor HMGB2 protein high expression associated with worse disease-free survival (DFS), while HMGB2 protein expression did not correlate with overall survival (OS). Besides, HMGB2 mRNA expression was raised in tumor tissue compared with adjacent tissue, and it had a good value in differentiating tumor tissue from adjacent tissue (AUC: 0.875, 95% CI: 0.834–0.915). Furthermore, tumor HMGB2 mRNA high expression correlated with higher Eastern Cooperative Oncology Group performance status score, LYN metastasis, and advanced TNM stage. Meanwhile, tumor HMGB2 mRNA high expression associated with shorter DFS and OS.
Conclusion
HMGB2 could be a biomarker that reflects disease features and prognosis of NSCLC, which is beneficial to improve clinical efficacy in NSCLC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-small cell lung cancer (NSCLC) is one of the most common cancers globally, with high morbidity and mortality, which represents approximately 85% of all lung cancer cases [1, 2]. Currently, due to lack of effective detecting methods, only a minority of NSCLC patients could be diagnosed at the early stage, while massive NSCLC patients are diagnosed at advanced stage [3, 4]. Meanwhile, although the advances in surgery, chemoradiotherapy, immunotherapy, and molecular-targeted therapy have improved clinical outcomes to some degree, the prognosis in NSCLC patients is poor with 5-year survival rate less than 18% mainly owing to tumor metastasis, relapse, drug resistance, and treatment-related toxicity [5, 6]. Thus, the exploration of potential biomarkers is needed to reflect the progression and prognosis of NSCLC, which is beneficial to improve treatment strategy for NSCLC patients.
High-mobility group box (HMGB) family involves four family members, including HMGB1, 2, 3, and 4, which is closely implicated in various biological processes via DNA replication, recombination, transcription, and repair [7,8,9,10]. Among these four members, HMGB2 plays an essential role in the regulation of transcription and DNA duplicate, which impacts cell proliferation, apoptosis, invasion, and migration in various tumors [11,12,13]. For example, HMGB2 enhances cell proliferation via AKT signaling pathway in cervical cancer [13]. Meanwhile, knockdown of HMGB2 reduces cell proliferation while overexpression of HMGB2 suppresses cisplatin- and etoposide-induced cell death in hepatocellular carcinoma [11]. In the clinical aspects, HMGB2 is recognized as a biomarker in cervical cancer and hepatocellular carcinoma [11, 13]. For instance, overexpression of HMGB2 is associated with distant metastasis and poor prognosis in hepatocellular carcinoma [11]. Regarding mechanism of HMGB2 in NSCLC, HMGB2 is recognized as oncogene for NSCLC, involving in cell proliferation and invasion of NSCLC [14]. However, clinical significance of HMGB2 is unknown in NSCLC patients.
Therefore, in this study, 133 NSCLC patients were retrospectively selected, and their tumor specimens and paired adjacent tissue specimens were obtained; then HMGB2 expression was determined by immunohistochemistry (IHC) assay and reverse transcription quantitative polymerase chain reaction (RT-qPCR) assay, aiming to investigate the correlation of HMGB2 with clinicopathological characteristics and prognosis in NSCLC patients.
Methods
Patients
This was a retrospective study which collected 133 NSCLC patients who received radical excision in the hospital from July 2015 to June 2020. Before being included in the study analysis, each patient’s clinicopathologic data, including pathology report, clinic examination report, and operative report, were reviewed to confirm the eligibility. All eligible patients met the following inclusion criteria: (a) pathological diagnosis of NSCLC; (b) age at diagnosis more than 18 years; (c) intraoperative fresh-frozen tumor specimen and adjacent tissue specimen were well-preserved and available for immunohistochemical (IHC) staining and RNA detection analysis; (d) no preoperative therapy for NSCLC; (e) no history of other malignancies; (f) main clinical data and survival data were intact for study analysis. The Institutional Review Board approved the current study.
Data collection
Patients’ characteristics were abstracted from the pathology report, clinic examination report, and operative report, including age, gender, history of smoke, history of drink, hypertension, hyperlipidemia, diabetes, Eastern Cooperative Oncology Group performance status (ECOG PS) score, histological subtype, pathological differentiation, tumor size, lymph node (LYN) metastasis status, TNM stage, preoperative carcinoembryonic antigen (CEA) level, and preoperative carbohydrate antigen 125 (CA125) level. The duration of follow-up was 2.0–60.0 months, median 33.0 months. Survival-related data were extracted from the clinic visits and telephone follow-up records, for evaluation of disease-free survival (DFS) and overall survival (OS).
HMGB2 detection by IHC assay
HMGB2 protein expression in the 133 fresh-frozen tumor specimens and paired adjacent tissue specimens was determined by IHC assay. Experimental process of IHC staining was carried out as described previously [15]. The HMGB2 polyclonal antibody (Invitrogen, Carlsbad, California, USA) was used as primary antibody in a 1:200 dilution. The goat anti-Rabbit IgG (H + L) secondary antibody (Invitrogen, Carlsbad, California, USA) was served as secondary antibody in a dilution of 1:60. Based on the IHC staining intensity and density, semi-quantitative analysis for the HMGB2 protein expression was performed, which was also carried out referring to the previous study [15]. A final semi-quantitative IHC score was the product of intensity score and positive cell percentage score. The IHC score > 3 was considered as HMGB2 protein high expression, and IHC score ≤ 3 was considered as HMGB2 protein low expression [16].
HMGB2 detection by RT-qPCR assay
HMGB2 mRNA expression in the 133 fresh-frozen tumor specimens and paired adjacent tissue specimens was determined by reverse transcription quantitative polymerase chain reaction assay. The total RNA was extracted by TRIzol™ Reagent (Invitrogen, Carlsbad, California, USA). Next, the RNA was converted to complementary DNA using PrimeScript™ RT reagent Kit with gDNA Eraser (Takara, Dalian, Liaoning, China). Then, qPCR was conducted using QuantiNova SYBR Green PCR Kit (Qiagen, Duesseldorf, Nordrhein-Westfalen, Germany). GAPDH was selected as the internal reference for HMGB2 mRNA expression. Finally, HMGB2 mRNA expression was calculated by 2−ΔΔCt method. Primers were designed referring to a previous study [17]: HMGB2, Forward: 5′-GGGGAAGAAAAAGGACCCCA-3′; Reverse: 5′-GCTGACTGCTCAGACCACAT-3′; GAPDH, Forward: 5′-GACCACAGTCCATGCCATCAC-3′; Reverse: 5′-ACGCCTGCTTCACCACCTT-3′. In the correlation analysis, tumor HMGB2 mRNA was categorized as high expression and low expression by the median expression value (2.526) of HMGB2 in total tumor specimens.
Statistical analysis
Variables were descried as mean with standard deviation (SD), median with interquartile range (IQR), or count with percentage. HMGB2 expression difference in the tumor tissue and adjacent tissue was checked by paired t test or Wilcoxon matched-pairs signed rank test. Receiver operating characteristic (ROC) analysis was performed to evaluate the effect of HMGB2 in distinguishing tumor from adjacent tissue. Correlation of tumor HMGB2 expression with clinicopathological characteristics was analyzed by Kruskal-Wallis H rank sum test or chi-square test. The DFS was calculated from the time of surgery to the time of disease relapse, progression, or patient’s death. The OS was calculated from the time of surgery to the time of patient’s death. Survival curve was shown by Kaplan-Meier method and checked using Log-rank (Mantel-Cox) test. Data analysis was carried out with the use of SPSS 22.0 statistical software (IBM, Chicago, Illinois, USA). Diagram was completed using GraphPad Prism 8.01 graphing software (GraphPad Software Inc., San Diego, California, USA). P value no more than 0.05 was regarded as there was statistical significance.
Results
NSCLC patients’ features
In the NSCLC patients, the mean age was 63.1 ± 11.9 years, and there were 110 (82.7%) males/23 (17.3%) females (Table 1). Furthermore, 79 (59.4%) patients had history of smoke. Regarding to histological subtype, 74 (55.6%), 50 (37.6%), and 9 (6.8%) patients presented with adenocarcinoma (ADC), squamous cell carcinoma (SCC), and adenosquamous carcinoma (ASC), respectively. In addition, 20 (15.0%), 78 (58.6%), and 35 (26.4%) patients exhibited well, moderate, and poor pathological differentiation, respectively. In terms of tumor size-lymph node-metastasis (TNM) stage, 43 (32.4%), 49 (36.8%), and 41 (30.8%) patients were at TNM stage I, II, and III, respectively. Meanwhile, the median CEA was 6.3 (2.5–30.2) (ng/mL), and the median CA125 was 32.8 (13.5–79.2) (U/mL). Other detailed characteristics of NSCLC patients were displayed in Table 1.
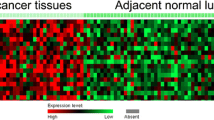
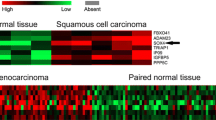
HMGB2 protein expression
HMGB2 protein expression in NSCLC patients was examined by IHC staining. IHC staining examples of adjacent HMGB2 expression, tumor HMGB2 expression (patients with LYN negative), and tumor HMGB2 expression (patients with LYN positive) are shown in Fig. 1a. HMGB2 IHC score was increased in tumor tissue compared with adjacent tissue (P < 0.001) (Fig. 1b). Subsequently, ROC curve analysis revealed that HMGB2 IHC score could distinguish tumor tissue from adjacent tissue (AUC: 0.775, 95% CI 0.720–0.830). The best cut-off point was the point where the IHC score was 2.5, the sensitivity was 91.0%, and specificity was 54.9%.
Comparison of HMGB2 protein expression between tumor tissue and adjacent tissue. IHC staining images showed HMGB2 expression of adjacent tissue, tumor tissue (patients with LYN negative), and tumor tissue (patients with LYN positive) in NSCLC. a Comparison of HMGB2 IHC score between tumor tissue and adjacent tissue. b ROC analysis of HMGB2 IHC score for distinguishing tumor tissue from adjacent tissue. c LYN lymph node, HMGB2 high mobility group box-2 protein, IHC immunohistochemistry, NSCLC non-small-cell lung cancer, ROC receiver operating characteristic, AUC area under the curve, CI confidence interval
Correlation of tumor HMGB2 protein expression with disease features
Tumor HMGB2 protein high expression correlated with LYN metastasis (P = 0.006) and advanced TNM stage (P = 0.033), while there was no correlation of HMGB2 protein expression with ECOG PS score (P = 0.196), histological subtype (P = 0.440), pathological differentiation (P = 0.798), tumor size (P = 0.224), CEA (P = 0.385), or CA125 (P = 0.330) (Table 2).
Correlation of tumor HMGB2 protein expression with DFS and OS
Shorter DFS was observed in tumor HMGB2 protein high expression patients compared with tumor HMGB2 protein low expression patients (P = 0.011) (Fig. 2a), while there was no difference of OS between tumor HMGB2 protein low expression patients and tumor HMGB2 protein high expression patients (Fig. 2b).
Tumor HMGB2 protein expression correlated with DFS but not OS in NSCLC. Comparison of DFS between tumor HMGB2 protein high expression patients and tumor HMGB2 protein low expression patients. a Comparison of OS between tumor HMGB2 protein high expression patients and tumor HMGB2 protein low expression patients. b DFS disease-free survival; OS overall survival OS; HMGB2 high mobility group box-2 protein, NSCLC non-small-cell lung cancer
HMGB2 mRNA expression
HMGB2 mRNA expression was determined by RT-qPCR, which observed that it was increased in tumor tissue compared with adjacent tissue (P < 0.01) (Fig. 3a). The following ROC curve analysis showed that HMGB2 mRNA expression had a good value in differentiating tumor tissue from adjacent tissue (AUC: 0.875, 95% CI: 0.834–0.915) (Fig. 3b). The best cut-off point was the point where the IHC score was 1.85, the sensitivity was 75.2%, and specificity was 86.5%.
HMGB2 mRNA expression between tumor tissue and adjacent tissue. Comparison of HMGB2 mRNA expression between tumor tissue and adjacent tissue. a ROC analysis of HMGB2 mRNA expression for distinguishing tumor tissue from adjacent tissue. b HMGB2 high mobility group box-2 protein, NSCLC non-small-cell lung cancer, ROC receiver operating characteristic, AUC area under the curve, CI confidence interval
Correlation of tumor HMGB2 mRNA expression with disease features
Tumor HMGB2 mRNA high expression correlated with higher ECOG PS score (P = 0.032), LYN metastasis (P = 0.006), and advanced TNM stage (P = 0.002), while there was no correlation of tumor HMGB2 mRNA expression with histological subtype (P = 0.118), pathological differentiation (P = 0.395), tumor size (P = 0.133), CEA (P = 0.547), or CA125 (P = 0.192) (Table 3).
Correlation of tumor HMGB2 mRNA expression with DFS and OS
Worse DFS was found in tumor HMGB2 mRNA high expression patients compared with tumor HMGB2 mRNA low expression patients (P < 0.001) (Fig. 4a). Meanwhile, shorter OS was also observed in tumor HMGB2 mRNA high expression patients compared with tumor HMGB2 mRNA low expression patients (P = 0.027) (Fig. 4b).
Tumor HMGB2 mRNA expression correlated with DFS and OS in NSCLC. Comparison of DFS between tumor HMGB2 mRNA high expression patients and tumor HMGB2 mRNA low expression patients. a Comparison of OS between tumor HMGB2 mRNA high expression patients and tumor HMGB2 mRNA low expression patients. b DFS disease-free survival, OS overall survival, HMGB2 high mobility group box-2 protein, NSCLC non-small-cell lung cancer
Discussion
In our study, the main findings were that (1) HMGB2 expression was higher in tumor tissue than adjacent tissue, and it could differentiate tumor tissue from adjacent tissue in NSCLC patients. (2) Tumor HMGB2 high expression correlated with LYN metastasis and advanced TNM stage in NSCLC patients. (3) Tumor HMGB2 high expression correlated with shorter DFS and OS in NSCLC patients.
Previous studies illustrate that HMGB2 is highly expressed in tumor tissues of several cancers [12, 13, 18,19,20]. However, no study investigates the difference of HMGB2 expression between tumor tissue and adjacent tissue in NSCLC. Our study retrospectively selected 133 NSCLC patients and compared HMGB2 expression between tumor tissue and adjacent tissue. Subsequently, we found that HMGB2 expression was higher in tumor tissue than adjacent tissue, and it could differentiate tumor tissue from adjacent tissue; these findings were also consistent with previous studies in other cancers [12, 13]. The possible reasons might be as follows: (1) regarding the cellular function of HMGB2 in other cancers, HMGB2 enhanced tumor cell proliferation by AKT signaling pathway, which might promote the NSCLC occurrence [13]. (2) HMGB2 inhibited cell growth and Warburg effect by modulating LDHB and FBP1 activities, so that was considered as basic in development and progression of tumor [12]. Therefore, increased HMGB2 expression was found in tumor tissue compared with adjacent tissue in NSCLC patients.
Recent studies disclose that tumor HMGB2 expression is associated with advanced tumor features in several cancers such as osteosarcoma and renal tumor [11, 13, 20, 21]. For example, HMGB2 is associated with advanced Enneking staging, larger tumor size, and metastasis in osteosarcoma [20]. In terms of the correlation of tumor HMGB2 with clinical characteristics in NSCLC, little knowledge is known in this area. In this study, we found that tumor HMGB2 high expression correlated with LYN metastasis and advanced TNM stage in NSCLC, which is consistent with relevantly previous studies about other cancers [11,12,13, 20, 21]. Our findings could be explained by (1) previous studies showing that HMGB2 impeded cell apoptosis while promoted cell proliferation and invasion via the β-catenin pathway through regulating miR-329 in melanoma [22]. Meanwhile, in glioblastoma multiforme (GBM), HMGB2 over-expression was involved in cell migration and invasion by regulating the activity of P53 protein [23]. In addition, HMGB2 overexpression facilitated the migration and invasion abilities of renal tumor ACHN cells [21]. In addition, HMGB2 knockdown inhabited migration and invasion abilities of osteosarcoma cells [20]. Thus, HMGB2 possibly had similar functions in the regulation of invasion and migration in NSCLC. (2) The overexpression of HMGB2 could increase the expression level of p-AKT while decreasing that of p21 and p27 (cyclin/kinase inhibitors) [13], which promoted cancer cell cycle progression and cell proliferation, which might accelerate the development and progression of NSCLC. Therefore, HMGB2 high expression associated with LYN metastasis and advanced TNM stage in NSCLC.
Based on previous studies, tumor HMGB2 high expression is correlated with decreased DFS and OS in breast cancer, hepatocellular carcinoma, and cervical cancer, indicating that HMGB2 could be a potential prognostic biomarker in patients with these cancers [11, 12, 18,19,20,21]. Similarly, we found tumor HMGB2 high expression correlated with shorter DFS and OS in NSCLC patients. There were some explanations for our findings: (1) our previous findings revealed that HMGB2 high expression correlated with LYN metastasis and advanced TNM stage in NSCLC, which indirectly resulted in poorer prognosis. (2) Overexpression of HMGB2 decreased the sensitivity of the head and neck squamous cell carcinoma cell lines to cisplatin and 5-fluorouracil, which indicated HMGB2 could facilitate drug resistance in cancer, leading to worse treatment response [24]. Thus, we found tumor HMGB2 high expression correlated with poor prognosis in NSCLC patients.
Nonetheless, some limitations existed in this study. First of all, the detailed mechanisms of HMGB2 in the pathogenesis of NSCLC were not investigated, and further experimental studies were needed. Secondly, the sample size was relatively small in this study, causing decreased statistical power of the analyses, so further studies with larger sample size should be considered to validate our findings. In addition, our study was a retrospective research, which existed bias, so prospective study is needed in the future.
In conclusion, HMGB2 is highly expressed in tumor tissue, which is associated with LYN metastasis, advanced TNM stage, and worse DFS and OS in NSCLC patients. These findings support that HMGB2 serves as a potential biomarker which assists disease management and optimizes personalized treatment to improve clinical outcome in NSCLC patients.
References
Duma N, Santana-Davila R, Molina JR (2019) Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc 94(8):1623–1640
Goldstraw P, Ball D, Jett JR et al (2011) Non-small-cell lung cancer. Lancet 378(9804):1727–1740
Reck M, Rabe KF (2017) Precision diagnosis and treatment for advanced non-small-cell lung cancer. N Engl J Med 377(9):849–861
Field JK, Oudkerk M, Pedersen JH, Duffy SW (2013) Prospects for population screening and diagnosis of lung cancer. Lancet 382(9893):732–741
Cheema PK, Rothenstein J, Melosky B et al (2019) Perspectives on treatment advances for stage III locally advanced unresectable non-small-cell lung cancer. Curr Oncol 26(1):37–42
Zappa C, Mousa SA (2016) Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res 5(3):288–300
Niu L, Yang W, Duan L et al (2020) Biological functions and theranostic potential of HMGB family members in human cancers. Ther Adv Med Oncol 12:1758835920970850
Grasser KD, Launholt D, Grasser M (2007) High mobility group proteins of the plant HMGB family: dynamic chromatin modulators. Biochim Biophys Acta 1769(5–6):346–357
Taniguchi N, Kawakami Y, Maruyama I, Lotz M (2018) HMGB proteins and arthritis. Hum Cell 31(1):1–9
Kucirek M, Bagherpoor AJ, Jaros J et al (2019) HMGB2 is a negative regulator of telomerase activity in human embryonic stem and progenitor cells. FASEB J 33(12):14307–14324
Kwon JH, Kim J, Park JY et al (2010) Overexpression of high-mobility group box 2 is associated with tumor aggressiveness and prognosis of hepatocellular carcinoma. Clin Cancer Res 16(22):5511–5521
Fu D, Li J, Wei J et al (2018) HMGB2 is associated with malignancy and regulates Warburg effect by targeting LDHB and FBP1 in breast cancer. Cell Commun Signal 16(1):8
Zhang P, Lu Y, Gao S (2019) High-mobility group box 2 promoted proliferation of cervical cancer cells by activating AKT signaling pathway. J Cell Biochem 120(10):17345–17353
Li S, Yang J, Xia Y et al (2018) Long noncoding RNA NEAT1 promotes proliferation and Invasion via targeting miR-181a-5p in non-small cell lung cancer. Oncol Res 26(2):289–296
Hu Z, Gu X, Zhong R, Zhong H (2018) Tumor-infiltrating CD45RO(+) memory cells correlate with favorable prognosis in patients with lung adenocarcinoma. J Thorac Dis 10(4):2089–2099
Tian Y, Zhao K, Yuan L et al (2018) EIF3B correlates with advanced disease stages and poor prognosis, and it promotes proliferation and inhibits apoptosis in non-small cell lung cancer. Cancer Biomark 23(2):291–300
Pu J, Tan C, Shao Z et al (2020) Long noncoding RNA PART1 promotes hepatocellular carcinoma progression via targeting miR-590-3p/HMGB2 axis. Onco Targets Ther 13:9203–9211
Cai X, Ding H, Liu Y et al (2017) Expression of HMGB2 indicates worse survival of patients and is required for the maintenance of Warburg effect in pancreatic cancer. Acta Biochim Biophys Sin (Shanghai) 49(2):119–127
Cui G, Cai F, Ding Z, Gao L (2019) HMGB2 promotes the malignancy of human gastric cancer and indicates poor survival outcome. Hum Pathol 84:133–141
Yang S, Ye Z, Wang Z, Wang L (2020) High mobility group box 2 modulates the progression of osteosarcoma and is related with poor prognosis. Ann Transl Med 8(17):1082
He ZH, Guo F, Hu XX et al (2020) Knockdown of HMGB2 inhibits proliferation and invasion of renal tumor cells via the p-38MAPK pathway. Eur Rev Med Pharmacol Sci 24(9):4729–4737
Tang C, Yang Z, Chen D et al (2017) Downregulation of miR-130a promotes cell growth and epithelial to mesenchymal transition by activating HMGB2 in glioma. Int J Biochem Cell Biol 93:25–31
Wu ZB, Cai L, Lin SJ et al (2013) High-mobility group box 2 is associated with prognosis of glioblastoma by promoting cell viability, invasion, and chemotherapeutic resistance. Neuro Oncol 15(9):1264–1275
Syed N, Chavan S, Sahasrabuddhe NA et al (2015) Silencing of high-mobility group box 2 (HMGB2) modulates cisplatin and 5-fluorouracil sensitivity in head and neck squamous cell carcinoma. Proteomics 15(2–3):383–393
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The Institutional Review Board approved the current study.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Lou, N., Zhu, T., Qin, D. et al. High-mobility group box 2 reflects exacerbated disease characteristics and poor prognosis in non-small cell lung cancer patients. Ir J Med Sci 191, 155–162 (2022). https://doi.org/10.1007/s11845-021-02549-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02549-8