Abstract
Purpose
To examine the associations between physical activity, metabolic risk factors, and comorbidities in Korean cancer survivors.
Methods
We used multiple cross-sectional data sets from the 2007–2013 Korean National Health and Nutrition Examination Surveys (KNHANES) that included 1225 cancer survivors. Physical activity and comorbidities were self-reported. Metabolic risk factors were measured via blood analyses and included fasting glucose, insulin, total cholesterol, triglycerides, and blood pressure.
Results
The sample was 38.4% male with a mean age of 59.9 ± 12.4 years. The most common cancers were stomach (22.5%), cervical (14.6%), breast (14.4%), and colorectal (11.8%). Cancer survivors meeting aerobic physical activity guidelines, compared to those completely inactive, had significantly lower fasting glucose (p = .001), HbA1c (p = .006), and systolic blood pressure (p = .001), and significantly lower risks of hypertension (odds ratio [OR] = 0.55, 95% confidential interval [CI] = 0.32 to 0.93), diabetes (OR = 0.64, 95% CI = 0.43 to 0.95), and arthritis (OR = 0.64, 95% CI = 0.41 to 0.99). Moreover, cancer survivors meeting strength exercise guidelines, compared to those not meeting guidelines, had significantly lower levels of fasting glucose (p = .001), HbA1c (p < .001), and total cholesterol (p = .031), and significantly lower risks of arthritis (OR = 0.42, 95% CI = 0.25 to 0.85) and back pain (OR = 0.50, 95% CI = 0.30 to 0.83).
Conclusion
Aerobic physical activity and strength exercise were significantly associated with lower risks of metabolic disturbances and comorbidities in Korean cancer survivors.
Implications for Cancer Survivors
Cancer survivors should engage in at least 150 min/week of aerobic exercise and at least 2 days/week of strength exercise to lower their risk of metabolic disturbances and comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer survivors experience poorer health than their non-cancer counterparts. For example, Hewitt et al. compared 95,615 individuals with or without a history of cancer and found that cancer survivors were three times more likely to report poor health than individuals without a history of cancer [1]. Moreover, cancer survivors are more susceptible to having metabolic risk factors such as elevated levels of glucose, total cholesterol (TC), triglycerides (TG), and blood pressure (BP) [2], and comorbidities such as type 2 diabetes, hypertension, and cardiovascular disease [3,4,5]. These undesirable health conditions may negatively affect cancer prognosis [6] as well as psychological health in cancer survivors [7]. Furthermore, cancer survivors may experience other musculoskeletal or physical function-related diseases such as arthritis and back pain after cancer treatments [8]. Managing these health conditions among cancer survivors has become an important part of post-treatment care.
There is substantial evidence examining the associations of physical activity (PA) with health-related fitness [9], patient-reported outcomes [10], and cancer outcomes [11]; however, only a few studies have investigated the associations between PA and metabolic risk factors or comorbidities in cancer survivors [12,13,14]. These studies have been limited, however, because of the narrow range of comorbidities examined and the failure to distinguish between aerobic and strength exercise. The purpose of the current study was to examine the associations between aerobic PA, strength exercise, and a wide range of metabolic risk factors and comorbidities in Korean cancer survivors. Considering that PA is beneficial to preventing many chronic metabolic conditions and various diseases in healthy populations [15], we hypothesized that cancer survivors would also demonstrate inverse associations between aerobic PA, strength exercise, and metabolic risk factors and comorbidities.
Materials and methods
Study participants
We used the data from the 2007–2013 Korean National Health and Nutrition Examination Surveys (KNHANES). The KNHANES is an annual cross-sectional national survey consisting of the health examination, health behavior, and nutrition survey. The surveys are conducted by interview or questionnaire. Each year, approximately 8000 individuals are sampled using a stratified cluster sampling method, which included the stratification criteria (province and city, residential area, and house type). Based on a total of 55,386 who participated in the surveys between 2007 and 2013, 1225 cancer survivors were eligible for this study. A participant who had ever been diagnosed with any type of cancer was defined as a cancer survivor. This survey was approved by the Korea Centers for Disease Control and Prevention Institutional Review Board, and written informed consent was obtained from all participants.
Data collection
The KNAHNES data were collected by research staff using either self-reported questionnaires, face-to-face interviews, or objective measurements. The detailed data resource profile is described elsewhere [16]. In brief, demographic, socioeconomic, and PA data were obtained using self-reported questionnaires. Comorbidities and cancer-related data were collected through face-to-face interviews conducted by KNHANES research staff. BMI, blood pressure, and metabolic risk factors were objectively measured using weight/height measures, sphygmomanometers, and blood lab tests, respectively.
Study variables
Physical activity
The KNHANES used the International Physical Activity Questionnaire Short-Form (IPAQ-SF), which has been translated into Korean and tested for validity and reliability [17, 18]. The IPAQ-SF was used to estimate the number of minutes per week spent in vigorous aerobic PA, moderate aerobic PA, and walking. Each question included all types of activities that occur at work, leisure, or for transportation that lasted for at least 10 min. Total aerobic PA per week was calculated by adding the minutes spent in moderate aerobic PA per week and the doubled minutes spent in vigorous aerobic PA per week. Walking was categorized as low-intensity PA and not counted in the total minutes of aerobic PA. Aerobic PA was then categorized into three groups based on the American College of Sport Medicine (ACSM) [19]/American Cancer Society (ACS) [20] aerobic PA guidelines: (1) completely inactive (0 min of moderate-to-vigorous aerobic PA per week), (2) insufficiently active (1–149 min of moderate-to-vigorous aerobic PA per week), or (3) meeting PA guidelines (≥ 150 min of moderate-to-vigorous aerobic PA per week). In addition to the items from the original IPAQ-SF, participants were also asked to report the number of days they engaged in strength exercise during the past week. Strength exercise was categorized into meeting or not meeting the ACSM/ACS strength exercise guidelines (≥ 2 days per week).
Cancer variables
Cancer variables included the following four self-reported questions: (1) history of cancer diagnosis, (2) currently having cancer and (3) currently undergoing treatment, and (4) age at diagnosis used to calculate the time since diagnosis. Whether a patient was having cancer or treatment was recorded a dichotomic value (yes or no). These four questions were asked for each of the following cancer sites: stomach, liver, colorectal, breast, cervical, lung, thyroid, and other cancers.
Metabolic risk factors
Metabolic risk factors included plasma levels of fasting glucose, insulin, hemoglobin A1c (HbA1c), triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-c), systolic blood pressure (SBP), and diastolic blood pressure (DBP). Blood samples were obtained from an antecubital vein of each participant after a 12-h overnight fast and analyzed at the Central Testing Institute in Seoul, Korea. Plasma concentrations of glucose, HDL-c, TC, and TG were measured by an enzymatic method using the Hitachi Automatic Analyzer 7600 (Hitachi, Japan). HbA1c was analyzed using a sodium lauryl sulfate (SLS) hemoglobin detection method and flow cytometry by using the XE-2100D semiconductor laser (Sysmex, Japan). Insulin was measured by an immunoradiometric assay using the 1470 WIZARD Gamma-counter (PerkinElmer, Finland). Blood pressure was assessed using a standard mercury sphygmomanometer (Baumanometer, USA) and repeated three times. The average of the second and third trials was used as the score.
Comorbidities
Comorbidities were assessed by self-report and included hypertension, type 2 diabetes, metabolic syndrome, cardiovascular diseases, stroke, arthritis, and back pain. Hypertension was defined as SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or taking antihypertensive medication. Type 2 diabetes was defined as fasting glucose ≥ 126 mg/dL or taking anti-hyperglycemic medication, taking injections of insulin, or physician’s diagnosis. Metabolic syndrome followed the National Cholesterol Education Program Adult Treatment Panel (NCEP ATP) III criteria as having at least three of the following risk factors: (1) waist circumference ≥ 90 cm for men and ≥ 85 cm for women, (2) TG ≥ 150 mmHg, (3) HDL-c < 40 mg/dL for men and < 50 mg/dL for women, (4) SBP ≥ 130 mmHg or DBP ≥ 85 mmHg, and/or (5) fasting glucose ≥ 100 mg/dL. Cardiovascular diseases included any heart-related diseases or symptoms such as myocardial infarction or angina. Stroke and arthritis were determined based on the history of diagnosis, and back pain was defined as having back pain for at least 30 days over the last 3 months from the time of data collection.
Covariates
The study covariates were selected based on the previous literature reporting demographic and socioeconomic factors [21] and BMI [22] as important determinants of metabolic risk factors and/or comorbidities. Socioeconomic variables were household income and education. Monthly household income was categorized by quartile. Educational attainment was categorized into elementary or less (≤ 6 years), middle school (7–9 years), high school (10–12 years), and college and above (≥ 13 years), then re-categorized into two groups for the analyses: high school graduate or less and post-secondary graduate or more. Demographic variables included age, sex, body mass index (BMI), and marital status. BMI was calculated using measured weight and height (BMI = weight (kg)/height2 (cm)). Marital status was categorized as never married, married and living with a spouse, and previously married (i.e., divorced, separation by death, or other). Cancer-related variables including cancer type, time since cancer diagnosis, and current status of having cancer and/or receiving treatment were also included as covariates [23].
Statistical analysis
Since the KNHANES data were collected using the stratified cluster sampling method, all statistical analyses were conducted using a complex sample procedure. Data were weighted based on the year of survey and the stratification and cluster variables by creating a complex sample analysis plan file based on sample weights provided by the KNHANES. Sociodemographic and medical characteristics, as well as PA were analyzed using weighted means and standard errors for continuous data and weighted percentages for categorical data. Complex sample general linear models (CSGLM) were conducted to examine the associations between aerobic PA or strength exercise variables and each metabolic risk factor. Complex sample logistic regression analyses (CSLOGISTIC) were performed to determine whether there were any associations between PA and comorbidities using both unadjusted and multivariable-adjusted analysis. P-trend for the association between aerobic PA categories and metabolic risk factors or comorbidities are also analyzed using CSGLM and CSLOGISTIC. IBM SPSS 23.0 was used for all analyses. All tests of statistical significance were two-sided with a p-value of 0.05.
Results
Participant characteristics
Sociodemographic, anthropometric, and medical characteristics of the cancer survivors are described in Table 1. In brief, 38.4% were men, the mean age was 59.9 ± 0.5, the mean BMI was 23.4 ± 0.1, 56.7% had one or more comorbidities, 15.0% had college or higher education, 76.5% were married, and 49.7% were low-mid or mid-high income. Stomach cancer was most prevalent (22.5%) followed by cervical cancer (14.6%), breast cancer (14.4%), colorectal cancer (11.8%), and other cancers (e.g., liver, lung, and thyroid). The mean time since cancer diagnosis was 7.9 ± 0.3 years and 68.8% had completed treatment at the time of the survey. In terms of comorbidities, 34.7% reported hypertension, 13.6% diabetes, 18.8% metabolic syndrome, 4.5% CVD, 3.0% stroke, 24.4% arthritis, and 16.3% back pain.
Physical activity participation
Table 2 shows the levels of PA participation in cancer survivors. The average time spent in aerobic PA was 215 ± 21 min/week. In terms of the aerobic PA guidelines, 61.5% were completely inactive, 8.8% were insufficiently active, and 29.7% were meeting guidelines. As for strength exercise, 75.5% were not participating in any strength exercises, and 19.3% were meeting the strength exercise guidelines.
Physical activity and metabolic risk factors
Associations between PA and metabolic risk factors in cancer survivors are presented in Table 3. For aerobic PA, individuals who were completely inactive showed a significantly higher level of fasting glucose than those who were insufficiently active or those who were meeting PA guidelines (102.6 ± 1.3 vs. 97.8 ± 1.2 vs. 95.8 ± 1.7 mg/dL, respectively, p = .002) after adjustment for age, sex, BMI, household income, education level, marital status, and cancer-related variables. HbA1c was higher in completely inactive survivors compared to insufficiently active and meeting PA guidelines (6.3 ± 0.1 vs. 5.9 ± 0.1 vs. 5.9 ± 0.1, respectively, p = .007). SBP was significantly lower in those who were meeting PA guidelines compared to those who were completely inactive (118.0 ± 1.1 vs. 122.3 ± 0.8, p < .002). For strength exercise, compared to those who were not meeting guidelines, those who were meeting guidelines showed lower fasting glucose (102.0 ± 1.1 vs. 96.9 ± 1.1 mg/dL, p = .001), HbA1c (6.3 ± 0.1 vs. 5.8 ± 0.1%, p < .001), and TC (189.9 ± 1.8 vs. 182.7 ± 2.9 mg/dL, p = .031). Insulin, TG, HDL-c, and DBP were not associated with aerobic PA or strength exercise guidelines. Complex sample multiple logistic regression analyses showed that there was no effect of sex on the associations between PA and metabolic risk factors.
Physical activity and comorbidities
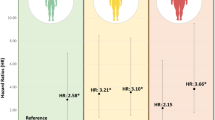
Table 4 describes the associations between PA and comorbidities in cancer survivors. Compared to those who were completely inactive, the risk of hypertension was lower in those who were insufficiently active (odds ratio [OR] = 0.60, 95% confidence interval [CI] = 0.39 to 0.92, p = .019) and those who were meeting aerobic PA guidelines (OR = 0.55, 95% CI = 0.32 to 0.93, p = .025) after adjustment for demographic and medical covariates. Those who were meeting aerobic PA guidelines also showed lower risks of diabetes (OR = 0.64, 95% CI = 0.43 to 0.95, p = .016) and arthritis (OR = 0.46, 95% CI = 0.19 to 0.96, p = .039) compared to those who were completely inactive. For strength exercise, those who were meeting guidelines showed a lower risk of arthritis (OR = 0.64, 95% CI = 0.41 to 0.99, p = .046) and back pain (OR = 0.50, 95% CI = 0.30 to 0.83, p = .031). Complex sample multiple logistic regression analyses showed that there was no effect of sex on the associations between PA and comorbidities.
Discussion
This cross-sectional study indicated the potential importance of both moderate-to-vigorous aerobic PA (e.g., brisk walking to running) and strength exercise (e.g., weight training) in improving metabolic risk factors and lowering the risks of comorbidities in Korean cancer survivors. Specifically, we found that more aerobic PA was associated with lower fasting glucose, HbA1c, TC, and SBP, and lower risks of hypertension, diabetes, and arthritis. Meeting strength exercise guidelines was associated with lower fasting glucose, HbA1c, and TG; and lower risks of arthritis and back pain.
Several epidemiological studies have investigated the associations between PA and comorbidities in cancer survivors. For instance, one cross-sectional study in breast cancer survivors reported that total PA was not associated with the comorbidity score; however, hours walked was inversely associated [14]. This study was limited, however, by a very small sample size (n = 40) and the use of a total score of comorbidities. Another retrospective cohort study with 1526 cancer survivors reported that, compared to the least physically active cancer survivors, those who were moderately or highly active had 35 to 45% lower risks of having CVD risk factors (e.g., diabetes and/or hypertension) [13] but it did not examine other comorbidities. Finally, a prospective cohort study of 1696 breast cancer survivors showed that moderate exercise (e.g., 30 min of walking per day) was associated with 31% lower prevalence of metabolic syndrome [12] but also did not examine other comorbidities. Together, most findings from these studies showed that there are inverse associations between PA and several comorbidities such as diabetes, hypertension, and metabolic syndrome in cancer survivors, consistent with the findings of our study. These studies, however, were limited in terms of the breadth of comorbidities and type of PA examined. Our study adds to these findings by examining associations between different comorbid conditions by exercise type (aerobic or strength) and dose (completely inactive vs. insufficiently active vs. meeting exercise guidelines).
Elevated blood glucose is related to poorer cancer prognosis [24] although the relationships vary according to cancer site [25]. Jeon et al. reported that colorectal cancer survivors with diabetes mellitus had an approximately 20% lower disease-free survival compared to those without diabetes [26]. For breast, prostate, and bladder cancer, a negative impact of diabetes on cancer prognosis has also been found [25]. Our study found an inverse relationship between aerobic PA and fasting glucose level, showing that completely inactive cancer survivors had a higher fasting glucose level (102.6 ± 1.3 mg/dL) in the prediabetes range (100–125 mg/dL) whereas those meeting aerobic PA guidelines had a lower level of fasting glucose (95.8 ± 1.7 mg/dL) falling in the normal range (< 100 mg/dL). We further found that those who were meeting aerobic PA guidelines had lower rates of diabetes by approximately 35% compared with those who were not participating in any PA. These results are in accordance with well-documented evidence on the positive effects of PA on diabetes and blood glucose control [27]. The physiological mechanisms underlying the association between PA and cancer prognosis are not fully understood. PA may help to systemically regulate glucose and insulin levels in blood [28, 29] which in turn may restrict cancer cells from glucose uptake for their growth, and may subsequently play a role in tumor anti-proliferation by inhibiting direct or indirect pathways relating to glucose and insulin on tumor growth [30, 31].
Along with diabetes, high blood pressure or hypertension is another common comorbidity in cancer survivors [32, 33]. Although the evidence of the relationship between high blood pressure and cancer prognosis is limited to certain types of cancers [32, 34], regulating high blood pressure is important in that increased blood pressure can increase the risk of death from cardiovascular disease competing with cancer-specific death [35,36,37]. For cancer survivors who underwent chemotherapy using angiogenesis inhibitors, the use of anti-vascular endothelial growth factor increases the risks of hypertension and potentially cardiovascular disease (CVD) [38]. In our study, those who were meeting aerobic PA guidelines compared to those who were completely inactive showed a lower SBP (122.3 ± 0.8 vs. 118 ± 1.1 mmHg) and a 45% decreased risk of hypertension; however, the risk of CVD was not significantly different between groups. This may be because CVD tends to occur later than other comorbidities such as diabetes and hypertension [39]. In our sample, the total number of CVD events was only 55 out of 1226 whereas the number of participants with diabetes or hypertension was 366 and 166, respectively. Given that PA is proven to significantly lower blood pressure [40, 41], cancer survivors should participate in sufficient levels of PA to prevent high blood pressure and hypertension.
In addition to metabolic comorbidities, musculoskeletal diseases can be of concern in cancer survivors. For example, many cancer survivors report that they suffer from substantial arthropathy or joint pain during and/or after chemotherapy or hormone therapy [42, 43]. Another common symptom that cancer survivors may experience is a back pain [44]. Similarly, in our study, approximately one third of cancer survivors had experienced arthritis and/or back pain. Although we were not able to determine how many cancer survivors underwent chemotherapy or hormone therapy, there may be a substantial number of cancer survivors who experience musculoskeletal pain, which should be properly prevented or treated. We found from our study that the risk of having arthritis was 46% lower in those who were meeting aerobic PA guidelines compared to those who were completely inactive. Furthermore, those who were meeting strength exercise guidelines showed a significantly reduced risk of arthritis by 68% and back pain by 50%. PA, especially strength exercise, may prevent or mitigate musculoskeletal diseases such as arthritis and back pain, especially in cancer survivors treated with chemotherapy or hormone therapy.
Considering the potential impact of aerobic PA and strength exercise on the health of cancer survivors, the reported levels of PA are discouraging. Our study found that only 29.7% of Korean cancer survivors were meeting the aerobic PA guideline and only 19.3% were meeting the strength exercise guideline. Min et al. also reported that compared to a matched non-cancer population, the probability of Korean cancer survivors meeting the PA guidelines was 83% lower (OR 0.17, 95% CI 4.46–8.90) [45]. Research into the determinants of PA in Korean cancer survivors is needed. It is possible that the high rate of stomach cancer in Korea has a negative effect on PA levels in cancer survivors. PA levels might also be affected by increased fatigue, lack of time, and low physical fitness/poor health [46] as well as loss of muscle, anemia, peripheral neuropathy, and various other side effects from treatments [47].
There are several limitations associated with this study. First, the data from the KNHANES is cross-sectional. KNHANES surveys a different population each year and the data analyzed in this study were accumulated from each cross-sectional assessment; thus, causation on the observed associations cannot be inferred. Second, the PA questionnaire used in the KNHANES has potential reporting biases in healthy populations [48]. In particular, PA levels using the IPAQ-SF were likely to be over-reported compared to the actual time spent in PA. In our study, average moderate-to-vigorous PA was over 200 min per week, which was substantially higher than the PA time from another study that measured PA using an accelerometer [49]. Moreover, vigorous PA was reported as high as moderate PA in our study, which is rare, and may have resulted in increased total PA minutes. Third, our study did not conduct subgroup analysis according to cancer type due to the small sample sizes of each single cancer site. It is possible that the associations between PA and comorbidities may vary by cancer type; consequently, future studies should obtain larger sample sizes and stratify the analysis by cancer type. Fourth, the lack of detailed cancer-related medical information, including disease stage and type of treatment, may have limited the interpretation of the results. Last, it should be noted that the findings of this study may not be generalizable to cancer survivors in other countries due to the unique distribution of cancer types as well as differences in cultural, socioeconomic, and environmental/lifestyle factors in Korean cancer survivors.
In conclusion, we found that there were significant associations between PA, metabolic risk factors, and comorbidities in Korean cancer survivors. Specifically, those who met aerobic PA guidelines had a more favorable profile for several metabolic risk factors as well as comorbidities. Moreover, given that many cancer survivors experience arthropathy or joint problems after cancer treatment due to fatigue, immobilization, and/or toxicity of the drug, strength exercise appears to be important in preventing arthritis and back pain in cancer survivors. The findings of our study prompt future longitudinal studies and clinical trials to further investigate the effects PA on metabolic risk factors and risk of comorbidities in Korean cancer survivors. Given that approximately 61.5% of Korean cancer survivors were completely inactive and 75.5% reported no strength exercise, it may be important for health-care providers in clinical settings to encourage cancer survivors to participate in sufficient levels of aerobic PA and strength exercise for potential health benefits. Regardless, more research using rigorous study design (i.e., experimental, longitudinal) is required to build on our findings.
References
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58(1):M82–91.
Schultz PN, Beck ML, Stava C, Vassilopoulou-Sellin R. Health profiles in 5836 long-term cancer survivors. Int J Cancer. 2003;104(4):488–95.
Hong CC, Ambrosone CB, Goodwin PJ. Comorbidities and their management: potential impact on breast cancer outcomes. Adv Exp Med Biol. 2015;862:155–75.
Wu AH, Kurian AW, Kwan ML, John EM, Lu Y, Keegan TH, et al. Diabetes and other comorbidities in breast cancer survival by race/ethnicity: the California Breast Cancer Survivorship Consortium (CBCSC). Cancer Epidemiol Biomark Prev. 2015;24(2):361–8.
Ye F, Moon DH, Carpenter WR, Reeve BB, Usinger DS, Green RL, et al. Comparison of patient report and medical records of comorbidities: results from a population-based cohort of patients with prostate cancer. JAMA oncol. 2017;3(8):1035–42.
Sogaard M, Thomsen RW, Bossen KS, Sorensen H, Norgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013;5(Suppl 1):3–29.
Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–20.
Lustberg MB, Reinbolt RE, Shapiro CL. Bone health in adult cancer survivorship. J Clin Oncol. 2012;30(30):3665–74.
Speck RM, Courneya KS, Mâsse LC, Duval S, Schmitz KH. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2010;4(2):87–100.
Schmitz KH, Holtzman J, Courneya KS, Mâsse LC, Duval S, Kane R. Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. 2005;14(7):1588–95.
Friedenreich CM, Orenstein MR. Physical activity and cancer prevention: etiologic evidence and biological mechanisms. J Nutr. 2002;132(11):3456S–64S.
Bao PP, Zheng Y, Nechuta S, Gu K, Cai H, Peng P, et al. Exercise after diagnosis and metabolic syndrome among breast cancer survivors: a report from the Shanghai Breast Cancer Survival Study. Cancer Causes Control. 2013;24(9):1747–56.
Keats MR, Cui Y, Grandy SA, Parker L. Cardiovascular disease and physical activity in adult cancer survivors: a nested, retrospective study from the Atlantic PATH cohort. J Cancer Surviv. 2017;11(2):264–73.
Vardar-Yagli N, Sener G, Saglam M, Calik-Kutukcu E, Arikan H, Inal-Ince D, et al. Associations among physical activity, comorbidity, functional capacity, peripheral muscle strength and depression in breast cancer survivors. Asian Pac J Cancer Prev. 2015;16(2):585–9.
Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–9.
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int J Epidemiol. 2014;43(1):69–77.
Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J Korean Acad Fam Med. 2007;28(7):532–41.
Chun MY. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012;33(3):144–51.
Schmitz K, Courneya K, Matthews C, Demark-Wahnefried W, Galvao D, Pinto B, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26.
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):242–74.
Fuchs VR. Reflections on the socio-economic correlates of health. J Health Econ. 2004;23(4):653–61.
Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan LM, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91(8):2906–12.
Geraci JM, Escalante CP, Freeman JL, Goodwin JS. Comorbid disease and cancer: the need for more relevant conceptual models in health services research. J Clin Oncol. 2005;23(30):7399–404.
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol. 2004;159(12):1160–7.
Currie CJ, Poole CD, Jenkins-Jones S, Gale EA, Johnson JA, Morgan CL. Mortality after incident cancer in people with and without type 2 diabetes impact of metformin on survival. Diabetes Care. 2012;35(2):299–304.
Jeon JY, Jeong DH, Park MG, Lee J-W, Chu SH, Park J-H, et al. Impact of diabetes on oncologic outcome of colorectal cancer patients: colon vs. rectal cancer. PLoS One. 2013;8(2):e55196.
American Diabetes Association. Physical activity/exercise and diabetes. Diabetes Care. 2004;27(suppl 1):s58–62.
Hsu PP, Sabatini DM. Cancer cell metabolism: Warburg and beyond. Cell. 2008;134(5):703–7.
Cairns RA, Harris IS, Mak TW. Regulation of cancer cell metabolism. Nat Rev Cancer. 2011;11(2):85–95.
Yun J, Rago C, Cheong I, Pagliarini R, Angenendt P, Rajagopalan H, et al. Glucose deprivation contributes to the development of KRAS pathway mutations in tumor cells. Science. 2009;325(5947):1555–9.
Gillies RJ, Robey I, Gatenby RA. Causes and consequences of increased glucose metabolism of cancers. J Nucl Med. 2008;49(Suppl 2):24S–42S.
Mouhayar E, Salahudeen A. Hypertension in cancer patients. Tex Heart Inst J. 2011;38(3):263–5.
Dyer A, Berkson D, Stamler J, Lindberg H, Stevens E. High blood-pressure: a risk factor for cancer mortality? Lancet. 1975;305(7915):1051–6.
Grossman E, Messerli FH, Boyko V, Goldbourt U. Is there an association between hypertension and cancer mortality? Am J Med. 2002;112(6):479–86.
Hooning MJ, Botma A, Aleman BM, Baaijens MH, Bartelink H, Klijn JG, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99(5):365–75.
Haugnes HS, Wethal T, Aass N, Dahl O, Klepp O, Langberg CW, et al. Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study. J Clin Oncol. 2010;28(30):4649–57.
Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13(3):1–9.
VBd S, Silva EN, Ribeiro ML, WdA M. Hypertension in patients with cancer. Arq Bras Cardiol. 2015;104(3):246–52.
Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease an update. Hypertension. 2001;37(4):1053–9.
Arroll B, Beaglehole R. Does physical activity lower blood pressure: a critical review of the clinical trials. J Clin Epidemiol. 1992;45(5):439–47.
Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503.
Amiri AH, Jaferian S. Post-chemotherapy arthralgia and arthritis in lung cancer. South Asian J Cancer. 2012;1(2):72–5.
Amiri A, Rafiei A. Analysis of patients with post-chemotherapy arthralgia and arthritis in breast cancer. Indian J Med Sci. 2010;64(5):197–203.
Deyo RA, Diehl AK. Cancer as a cause of back pain. J Gen Intern Med. 1988;3(3):230–8.
Min JH, Kim JY, Justin JY. The characteristics Korean cancer patients’ physical activity participation: focus on five major cancers: the Korea National Health and Nutrition Examination Survey 2009-2013. Korean J Phys Educ. 2015;54(6):389–97.
Kang D-W, Chung JY, Lee MK, Lee J, Park J-H, Kim D-i, et al. Exercise barriers in Korean colorectal cancer patients. Asian Pac J Cancer Prev. 2014;15(18):7539–45.
Courneya KS, Friedenreich CM, Quinney HA, Fields AL, Jones LW, Vallance JK, et al. A longitudinal study of exercise barriers in colorectal cancer survivors participating in a randomized controlled trial. Ann Behav Med. 2005;29(2):147–53.
Lee PH, Macfarlane DJ, Lam T, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8(1):1.
Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N. Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006). Cancer Causes Control. 2010;21(2):283–8.
Acknowledgements
The authors fully acknowledge that the data in this study is acquired from the Korean National Health and Nutrition Examination Survey (KNHANES) conducted by the Korean Centers for Disease Control and Prevention (KCDC) between 2007 and 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This survey was approved by the Korea Centers for Disease Control and Prevention Institutional Review Board, and written informed consent was obtained from all participants.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kang, DW., Lee, EY., An, K.Y. et al. Associations between physical activity and comorbidities in Korean cancer survivors. J Cancer Surviv 12, 441–449 (2018). https://doi.org/10.1007/s11764-018-0683-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-018-0683-y